Abstract
Background
Multiple studies have demonstrated strong associations between cardiorespiratory fitness and lower cardiovascular disease mortality. In contrast, little is known about associations of fitness with non-fatal cardiovascular events.
Methods and Results
Linking individual participant data from the Cooper Center Longitudinal Study with Medicare claims files, we studied 20,642 participants (21% women) with fitness measured at mean age 49 years and who survived to receive Medicare coverage from 1999 to 2009. Fitness was categorized into age- and sex-specific quintiles (Q) according to Balke protocol treadmill time with Q1 as low fitness. Fitness was also estimated in metabolic equivalents according to treadmill time. Associations between midlife fitness and hospitalizations for heart failure and acute myocardial infarction after age 65 were assessed by applying a proportional hazards model to the multivariate failure time data. After 133,514 person-years of Medicare follow-up, we observed 1,051 hospitalizations for heart failure and 832 hospitalizations for acute myocardial infarction. Compared to high fitness (Q4-5), low fitness (Q1) was associated with a higher rate of heart failure hospitalization (14.3% vs. 4.2%) and hospitalization for myocardial infarction (9.7% vs. 4.5%). After multivariable adjustment for baseline age, blood pressure, diabetes, body mass index, smoking status and total cholesterol, a 1 unit greater fitness level in metabolic equivalents (METs) achieved in midlife was associated with approximately a 20% lower risk for heart failure hospitalization after age 65 [Men, hazard ratio (95% confidence intervals): 0.79 (0.75-0.83), p<0.001; Women: 0.81 (0.68-0.96), P=0.01] but just a 10% lower risk for acute myocardial infarction in men [0.91 (0.87-0.95), p< 0.001] and no association in women [0.97 (0.83-1.13), p=0.68].
Conclusions
Fitness in healthy, middle-aged adults is more strongly associated with heart failure hospitalization than acute myocardial infarction outcomes decades later in older age.
Keywords: cardiorespiratory fitness, heart failure, acute myocardial infarction
Higher cardiorespiratory fitness (fitness) is a reflection of habitual physical activity in adults.1, 2 Fitness is strongly associated with lower cardiovascular disease mortality, with multiple studies demonstrating a consistent, inverse association between fitness and mortality even after adjustment for traditional risk factor burden.3-8 This association persists across the lifespan, with a single measurement of fitness in mid-life strongly associated with the lifetime risk for cardiovascular mortality decades later.9 However, the association between fitness and non-fatal cardiovascular events is not well understood,8, 10 reflecting the lack of data on non-fatal cardiovascular events among established cohorts with objectively measured fitness levels.
The mechanism through which low fitness associates with adverse cardiovascular outcomes across the lifespan likely reflects in part the subsequent development of traditional risk factors such as diabetes and hypertension. 11, 12 Although higher fitness is associated with lower levels subclinical atherosclerosis,13-15 exercise also has measurable, biological effects on cardiovascular structure and function16, 17 that are highly responsive to short-term changes in exercise.18, 19 In addition, lifelong exercise training appears to limit age-related cardiac stiffening, resulting in a more compliant left ventricle in older age and possibly reducing the risk of heart failure with preserved ejection fraction.17, 20 While much of the focus on the mechanisms of benefit of exercise and fitness have focused on prevention of atherosclerosis and its complications, the specific effects of exercise on cardiac structure and function suggest that low fitness might be particularly important for long-term heart failure risk. Therefore, we hypothesized that lower levels of fitness in healthy, middle-aged adults would be more strongly associated with heart failure hospitalization than with hospitalization for acute myocardial infarction.
In this study, we merged the Cooper Center Longitudinal Study with individual claims data from the Center for Medicare and Medicaid Statistics, allowing for the assessment of the correlation between midlife fitness and the long-term risk for heart failure and acute myocardial infarction.
Methods
Among 73,439 participants in the CCLS who received a complete clinical examination at the Cooper Clinic in Dallas, TX, between 1970 and 2009, 24,903 were eligible to receive Medicare coverage between 1999 and 2009 as described previously.21 After excluding 2,981 (12%) participants lacking traditional Medicare Fee-for-Service coverage (i.e. Medicare Advantage participants lacking claims files), 382 participants with a self-reported prior myocardial infarction at study entry, 844 participants whose CCLS examination occurred after enrollment into Medicare Fee-for Service, and 54 participants < age 65 (i.e. Medicare coverage for disability, end-stage renal disease, etc), we were left with a final study sample of 20,642 CCLS participants for the present analysis. No individual was excluded on the basis of his or her performance on the exercise treadmill portion of the examination.
CCLS Clinical Examination
Details of the clinical examination and the study cohort have been published previously.3, 4. Participants completed a comprehensive clinical examination which included a self-reported personal and family history, standardized medical examination by a physician, fasting blood levels of total cholesterol, triglycerides, and glucose, as well as a maximal treadmill exercise test. Body mass index was calculated from measured height and weight.
As reported previously,3, 4 fitness was measured in the CCLS by a maximal treadmill exercise test using a Balke protocol. In this protocol, treadmill speed is set initially at 88 m/min. In the first minute, the grade is set at 0% followed by 2% in the second minute and an increase of 1% for every minute thereafter. After 25 minutes, the grade remains unchanged but the speed is increased 5.4 m/min for each additional minute until the test is terminated. Participants were encouraged not to hold onto the railing and were given encouragement to exert maximal effort. The test was terminated by volitional exhaustion reported by the participant or by the physician for medical reasons. As described previously, the test time using this protocol correlates highly with directly measured maximal oxygen uptake (r = 0.92).22
In accordance with standard approaches to the analysis of fitness data, 3, 4 treadmill times were compared with age- and sex-specific normative data on treadmill performance within the CCLS, allowing each individual's treadmill time to be classified into an age- and sex-specific quintile of fitness. These quintiles of fitness measures were then combined into three, mutually exclusive fitness groupings: “low fitness”: quintile 1; “intermediate fitness”: quintiles 2-3; “high fitness”: quintiles 4-5. Using well-characterized regression equations, treadmill times from the Balke protocol allow for estimation of fitness level in metabolic equivalents (METS).22
Medicare Claims Data
Medicare inpatient claims data were obtained from the Center for Medicare and Medicaid Services (CMS) for surviving participants who were 65 years of age or older and who were thus eligible for Medicare benefits during the period from 1999 — the first year CMS data are currently available for public use — through 2009. CMS data contain 100% of claims paid by Medicare for covered health care services. A beneficiary may be tracked over time to elicit a history of all the utilization of health care services. Inpatient hospitalization files from CMS provide all individual records for each medical service billed to Medicare, the date of service, primary diagnosis and up to eight secondary diagnoses (i.e. ICD-9 code), procedure (ICD-9 procedure code), beneficiary demographic information, and numerous additional data.
In accordance with standard approaches, heart failure hospitalization was defined as a primary diagnosis of heart failure as indicated by ICD-9 codes 428, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, and 404.93. Acute myocardial infarction was defined as the primary or secondary hospitalization as indicated by ICD-9 codes 410.0 to 410.9.
Statistical Analyses
The data contains Medicare claims on all CCLS patients who were age 65 or older during the period 1999-2009. The data is subject to censoring on the right and the left, with the possibility of multiple events per patient. Because of the unique structure of the Medicare claims files, we used attained age as the time scale. We estimated the association between fitness and hospitalization for acute myocardial infarction or heart failure by applying a proportional hazards model to the multivariate failure time data, as described by Prentice.23 In order to assess the association between fitness and either heart failure or myocardial infarction, participants were allowed to transition through multiple states: from healthy to heart failure, from healthy to acute myocardial infarction, and from acute myocardial infarction to heart failure, where healthy was defined as the absence of any prior hospitalization for heart failure or acute myocardial infarction. Separate risk sets were maintained for each possible transition. So, for example, a healthy participant was included in the risk set for transition to heart failure and the risk set for transition to myocardial infarction until either of these events or a censoring event occurred. We used the robust sandwich estimate of the covariance matrix to account for correlation of score residuals of the same participant in different strata.24 As noted below, only 10% of heart failure cases were associated with antecedent myocardial infarction resulting in limited statistical power for this analysis, particularly in women. Therefore, we do not report the association between fitness and the transition from acute myocardial infarction to heart failure.
Men and women were analyzed separately for each outcome in models adjusted for age, baseline fitness, systolic blood pressure, diabetes (yes/no), current smoking (yes/no), total cholesterol, and body mass index. In all analyses, death obtained from Medicare claims files was treated as a censoring event.
To assess the association between midlife fitness levels and risk for cardiovascular events across time, we constructed Kaplan Meier curves for each outcome separately in both men and women with age as the time scale. Failure was defined as the development of a heart failure hospitalization or acute myocardial infarction hospitalization in separate analyses. To compare the association between fitness levels measured at particular ages in midlife and subsequent heart failure risk, we stratified the analysis according to the age at which fitness was measured (i.e. age 40-49 years, 50-59 years, and 60-69 years). Finally, in order to determine the effects of absolute fitness differences in early middle-age, we compared the distribution of fitness levels measured at age 40-49 years between those with and without a subsequent hospitalization for heart failure at age 65 or older. We compared these distributions in men and women separately using the rank sum test. All statistical analyses were performed using SAS for Windows (release 9.2; SAS Institute, Inc., Cary, NC).
Results
Baseline characteristics for the study sample demonstrate a low level of traditional risk factors at entry into the Cooper Center Longitudinal Study in both men and women (Table 1). As expected, both estimated fitness levels and the level of most traditional risk factors were higher in men compared to women. In both men and women, higher fitness levels were associated with lower levels of all traditional risk factors.
Table 1. Baseline characteristics according to category of baseline fitness from data acquired at the baseline clinical examination.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Fitness Quintile 1 (N = 3,011) | Fitness Quintiles 2-3 (N = 6,851) | Fitness Quintiles 4-5 (N = 6,441) | Fitness Quintile 1 (N = 600) | Fitness Quintiles 2-3 (N = 1,631) | Fitness Quintiles 4-5 (N = 2,108) | |
| Baseline Age in CCLS, years | 46.0 (8.5) | 49.1 (8.6) | 51.0 (8.5) | 48.2 (9.4) | 50.6 (9.2) | 52.8 (8.2) |
| Age at Medicare Entry, years | 67.7 (4.8) | 68.0 (4.9) | 67.7 (4.8) | 68.2 (5.3) | 67.9 (5.1) | 67.0 (4.2) |
| Median (25%ile, 75%ile) Age at Medicare Entry* | 65 (65,69) | 65 (65,70) | 65 (65,69) | 65 (65,70) | 65 (65,69) | 65 (65,67) |
| Systolic blood pressure, mm Hg | 124.7 (14.6) | 122.6 (14.1) | 122.3 (14.3) | 119.3 (15.7) | 116.7 (15.6) | 116.7 (15.9) |
| Total cholesterol, mg/dL | 221.9 (41.5) | 216.4 (39.5) | 209.6 (37.5) | 213.9 (38.7) | 214.3 (40.2) | 209.8 (37.5) |
| Body mass index, kg/m2 | 28.6 (4.5) | 26.6 (3.2) | 25.1 (2.5) | 25.4 (5.5) | 23.6 (3.8) | 22.4 (2.9) |
| Smokers (%) | 31.2% | 19.3% | 8.7% | 17.3% | 9.9% | 5.3% |
| Diabetes (%) | 5.5% | 2.9% | 1.7% | 3.3% | 1.8% | 1.1% |
| METS | 8.4 (1.2) | 10.3 (1.2) | 13.0 (1.8) | 6.4 (0.9) | 7.9 (1.0) | 10.0 (1.5) |
Data presented as mean (SD) or % except as noted.
Data presented as median (25%ile, 75%ile)
METS: metabolic equivalents
After 133,514 person-years of Medicare exposure time, we observed 1,051 heart failure hospitalizations and 832 hospitalizations for acute myocardial infarction among 20,642 participants in the CCLS-Medicare cohort. In both men and women, heart failure hospitalization after acute myocardial infarction represented a minority of heart failure hospitalization events (men: 9.6%; women: 11.3%).
There were significant differences in the observed event rates of each outcome according to baseline fitness level (Table 2). In both men and women, compared to low fitness measured at baseline, the presence of high fitness was associated with approximately a 3-fold gradient in heart failure hospitalization rates [HR (95% CI) 0.31 (0.24-0.41) and 0.38 (0.20-0.71) in men and women, respectively]. In contrast, there was less than a 1-fold gradient in risk for acute myocardial infarction hospitalization [0.56 (0.43-0.71) and 0.62 (0.33-1.17)] in men and women, respectively; see Table 2 and Figures 1 and 2). When these data were stratified by age at entry, we observed a similar pattern of results across all quintiles of fitness levels measured at ages 40-49, 50-59, and 60-69 years (Figure 3).
Table 2. Rate of heart failure and acute myocardial infarction according to baseline fitness levels and results of Multivariable-adjusted Cox Proportional Hazards Models Examining the Association between Fitness and Heart Failure and Acute Myocardial Infarction among Participants in the Cooper Center Longitudinal Study.
| Men | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heart Failure | Acute MI | Total Mortality | |||||||||||
| Person- years | Events | Rate | Hazard ratio# (95% CI) | χ2 | P-value | Events | Rate | Hazard ratio (95% CI) | χ2 | P-value | Events | Rate | |
| Q1 (low Fit) | 19,378 | 331 | 17.1 | 1.0 | ----- | ---- | 204 | 10.5 | 1.0 | ----- | ---- | 677 | 34.9 |
| Q2-3 (Mod Fit) | 45,131 | 387 | 8.6 | 0.60 (0.49-0.75) | 20.7 | < 0.001 | 319 | 7.1 | 0.74 (0.59-0.92) | 7.6 | .006 | 1037 | 23.0 |
| Q4-5 (High Fit) | 41,346 | 189 | 4.6 | 0.31 (0.24-0.41) | 71.6 | < 0.001 | 206 | 5.0 | 0.56 (0.43-0.71) | 21.6 | < 0.001 | 674 | 16.3 |
| Fitness (per MET) | 0.79 (0.75-0.83) | 81.7 | < 0.001 | 0.91 (0.87-0.95) | 18.6 | < 0.001 | |||||||
| Women | |||||||||||||
| Q1 (low Fit) | 4,024 | 35 | 8.7 | 1.0 | ---- | ----- | 23 | 5.7 | 1.0 | ---- | ---- | 99 | 24.6 |
| Q2-3 (Mod Fit) | 10,862 | 72 | 6.6 | 0.53 (0.31-0.93) | 5.0 | .03 | 41 | 3.8 | 0.73 (0.40-1.32) | 1.1 | 0.29 | 177 | 16.3 |
| Q4-5 (High Fit) | 12,772 | 37 | 2.9 | 0.38 (0.20-0.71) | 9.1 | 0.003 | 39 | 3.1 | 0.62 (0.33-1.17) | 2.16 | 0.14 | 126 | 9.9 |
| Fitness (per MET) | 0.81 (0.68-0.96) | 6.1 | 0.01 | 0.97 (0.83-1.13) | 0.2 | 0.68 | |||||||
Rate per 1000 person-years;
Reference group for Hazard ratio calculation is High fit (Q4-5); METS: metabolic equivalents
Figure 1.
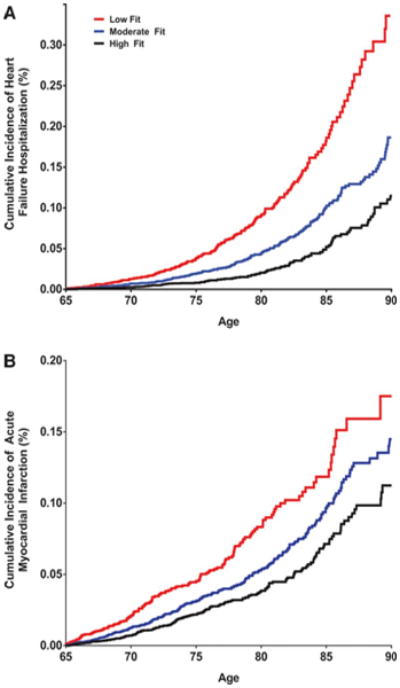
Cumulative Incidence of (a) heart failure and (b) acute myocardial infarction in Men at Age > 65 years According to Category of Midlife Physical Fitness Measured at Baseline Examination. Low fitness (quintile 1), Moderate fitness (quintiles 2-3), High Fitness (quintile 4-5).
Figure 2.
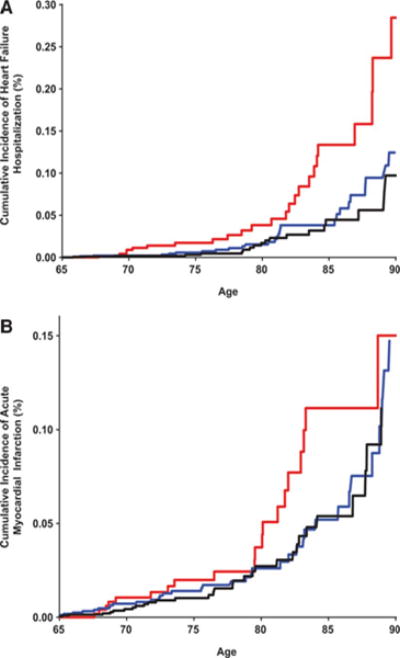
Cumulative Incidence of (a) heart failure and (b) acute myocardial infarction in Women at Age > 65 years According to Category of Midlife Physical Fitness Measured at Baseline Examination. Low fitness (quintile 1), Moderate fitness (quintiles 2-3), High Fitness (quintile 4-5)
Figure 3.
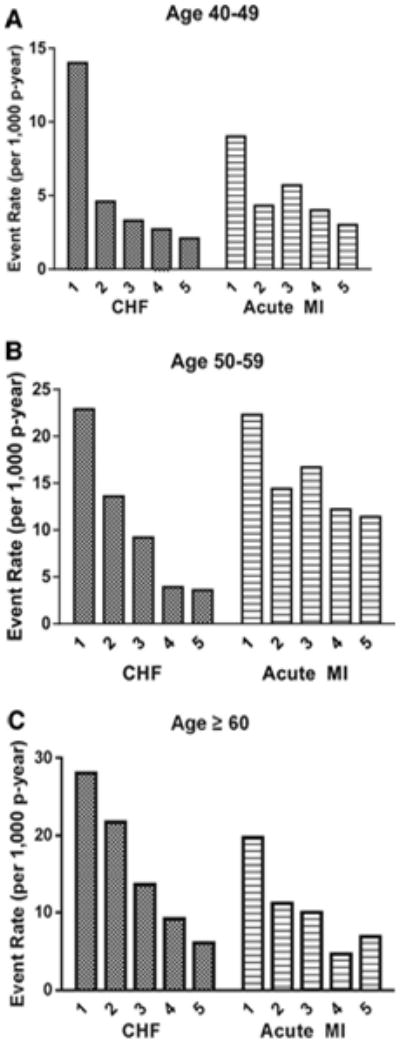
Association between fitness quintiles measured at age (a) 40-49 years, (b) 50-59 years, (c) and 60-69 years with heart failure and acute myocardial infarction hospitalization in men and women (combined) at Medicare age from the Cooper Center Longitudinal Study. Quintile 1: low fitness
There were significant differences in the distribution of fitness levels measured in early middle-age (i.e. age 40-49) between participants who did and did not develop heart failure at age ≥ 65 years. In particular, we observed a difference of 2 METs at age 40-49 years between those who did and did not develop heart failure at age ≥ 65 years (men: 10.3 vs. 12.3 METs; women: 7.6 vs. 9.7 METs; Figure 4, p< 0.001 for both).
Figure 4.
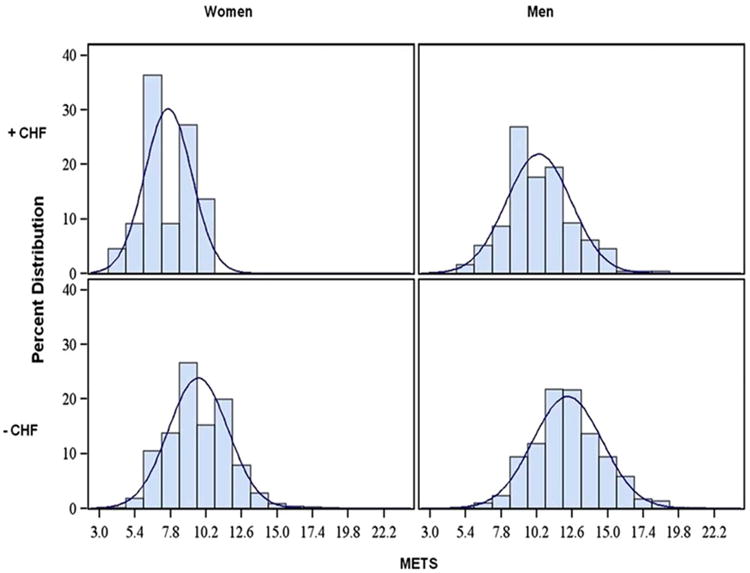
Histogram and overlying probability densities for fitness levels (in METs) measured at age 40-49 years among women with and without heart failure at age > 65 years (Mean: 7.6 vs. 9.7 METs; p-value <0.001), and men with and without heart failure at age > 65 years (Mean: 10.3 vs. 12.3 METs; p-value <0.001). The mean age difference between baseline visit and Medicare entry in this age group was similar for subjects with and without hospitalization for heart failure at a later age [23 vs. 21 years (Men); 21 vs. 20 years (Women)].
After multivariable adjustment, low fitness remained strongly associated with heart failure risk in both men and women. In contrast, the association between low fitness and acute myocardial infarction were less prominent (Table 2). When fitness was analyzed as a continuous variable (i.e. per MET), we observed a similar pattern of results. Although diabetes, systolic blood pressure, and higher body mass index were all associated with heart failure risk in both men and women, the association between body mass index and future heart failure risk appeared more prominent in women [HR 95% confidence intervals: 1.24 (1.03 – 1.49)] compared to men [1.11 (1.01 – 1.22)]. Similar findings were observed for diabetes and future risk for heart failure hospitalization, with more prominent associations for women [3.74 (1.57 – 8.92)] compared to men [1.71 (1.25 – 2.34)].
Discussion
In this study, lower fitness in healthy, middle-aged adults was associated with a marked increase in risk for heart failure hospitalization in later life. In addition, the magnitude of the association between low fitness and heart failure hospitalization was nearly twice that observed for the association between fitness and acute myocardial infarction. Finally, the association between fitness and heart failure was particularly prominent for fitness levels measured in early middle age, suggesting that heart failure in the elderly is associated with low levels of fitness throughout middle age. These findings suggest the potential contribution of exercise training in midlife for the prevention of heart failure in the elderly.
Our findings could have important public health implications. Heart failure affects an estimated 5.8 million people and accounts for an estimated annual healthcare cost of $34.8 billion.25 Heart failure is predominantly a disease of the elderly with more than 80% of all heart failure admissions occurring in those individuals over 65 years of age.26 In contrast to the marked decrease in the burden of coronary artery disease, the prevalence of heart failure remains relatively unchanged,25-27 reflecting diverse epidemiologic trends such as the aging population.
However, other than blood pressure treatment, relatively few strategies have been proposed for the prevention of heart failure in the elderly. In the present study, we observed that fitness levels measured in early middle age were strongly associated with heart failure risk decades later in older age. Furthermore, these differences in midlife fitness levels were not insignificant. For example, men and women with heart failure at age > 65 years had a mean fitness level at age 40 that was near the 20th percentile for the general population,28 suggesting that approximately one-half of all heart failure cases at age > 65 years had very low fitness levels in early life.
There are several potential mechanisms through which low physical fitness in healthy, middle-aged adults might be associated with the long-term risk for heart failure. Fitness is associated with downstream risk factors such as diabetes, hypertension, and obesity that might promote the development of heart failure in older age directly or indirectly through the development of interval myocardial infarction.11, 12, 29 Because only 10% of the heart failure events in the present study occurred after a hospitalization for acute myocardial infarction, the majority of heart failure risk among low fit individuals appears to follow a pathway independent of antecedent myocardial infarction.
There is also strong evidence to support a more direct association between midlife fitness and heart failure risk in older age. Multiple studies have observed that the heart stiffens with advanced age, resulting in decreased left ventricular compliance,20, 30, 31 and contributing to the development of heart failure with preserved ejection fraction in the elderly.30 However, individuals age >65 years who report lifelong endurance training have higher left ventricular compliance compared to sedentary older adults. 20 Furthermore, exercise training among sedentary older adults is beneficial in increasing fitness but translates into only trivial differences in LV compliance.17 Thus, exercise training throughout midlife appears to attenuate the age-related decrease in left ventricular compliance, potentially decreasing the risk for heart failure with preserved ejection fraction in later life.
The association between low levels of fitness and an increased risk for both cardiovascular and non-cardiovascular disease death is well established.3-5, 7, 32, 33 However, the association between low physical fitness and non-fatal events is less well understood because few datasets with measured physical fitness have followed participants for non-fatal outcomes. In one smaller study of 1,166 men from the Kuopio Ischemic Risk Factor Study, higher levels of fitness were associated with a lower risk for acute myocardial infarction (44 total events).10 In another study, Sui et al showed association between fitness and non fatal cardiovascular events using Cooper clinic database.34 However this prior analysis focused on atherosclerotic cardiovascular disease events (MI, stroke and revascularization) and used mail back health survey responses to identify primary end point events. In the present study, we include 20,642 healthy men and women with objectively measured fitness and with 832 acute MI hospitalizations and 1,052 heart failure hospitalizations after long-term follow-up. Therefore, the present study represents a substantial contribution to the available literature on the association between fitness and non-fatal cardiovascular events, providing novel insights into the contribution of low fitness in midlife to cardiovascular risk at older ages.
Our findings are consistent with observational studies that have reported an independent association between self-reported physical activity and the subsequent risk of coronary artery disease35 and heart failure36-40. We extend these prior observations in several notable ways. First, we compare the association between low fitness—rather than self-reported physical activity—and subsequent risk for non-fatal cardiovascular events, providing an opportunity to compare the relative contribution of low fitness to both atherosclerotic and non-atherosclerotic cardiovascular outcomes. Second, because of our sample size and long-term follow-up, we were able to estimate separately the association between fitness levels measured at mid-life and both atherosclerotic and non-atherosclerotic non-fatal cardiovascular events decades later.
Several important limitations of our study should be acknowledged. First, participants in the Cooper Center Longitudinal Study represent a sample of well-educated individuals with a relatively high socioeconomic status and overall high level of fitness compared to the general population. However, we have recently shown that the association between traditional risk factor burden and lifetime risk observed in this study were strikingly similar to those obtained from a large, more representative cohort.9 Thus, although the levels of risk factors are lower than the general population, the effects of these risk factors are strikingly similar.
Second, we merged individual-level data with Medicare claims files to compare the association between fitness and cardiovascular outcomes at age ≥ 65 years. We were not able to capture cardiovascular outcomes that occurred between study entry and the onset of Medicare eligibility. Nevertheless, this approach has been used by other investigators in a parallel context, providing novel insight into the contribution of traditional risk factors and other Medicare outcomes.41-44 Importantly, we observed a similar pattern of results for fitness levels measured in early life (i.e. age 40 years) as well as in later life (i.e. age 60) and closer to Medicare eligibility, suggesting that the association between fitness and non-fatal events was insensitive to the time interval between fitness ascertainment and Medicare eligibility.
Third, additional factors like medication use were not included in our analysis because these data are limited in the CCLS. Although adjustment for this additional covariate may have influenced the association of fitness with risk of heart failure and myocardial infarction, we believe that the healthy nature of our cohort, exclusion of subjects with significant cardiovascular events at baseline, and long duration of follow up minimize the effect of missing medication data.
Fourth, because much of our data is derived from the 1970s, we do not have HDL- and LDL- cholesterol on as many participants as we have total cholesterol measurements. Prior literature suggests a more limited contribution of high-density lipoprotein cholesterol to risk prediction for CVD mortality.45 Furthermore, because our primary objective was to compare the association between fitness and non-fatal events across long periods of follow-up, we elected to use total cholesterol in our multivariable adjusted model so as to include participants from the beginning of the CCLS where LDL and HDL data are more limited. Finally, we used diagnoses from Medicare claims files rather than adjudicated clinical outcomes and therefore some events might not have been captured or might have been misclassified. However, measurement error tends to bias towards the null and encouragingly, the association between fitness and non-fatal cardiovascular events were present despite use of administrative data. Also, the use of administrative data for the study of heart failure hospitalization, 46-48 acute myocardial infarction49 is well established. Furthermore, nearly all prior studies on the association between fitness and cardiovascular outcomes are derived from administrative data (i.e. the National Death Index). In the present study, we have extended this prior approach by linking the Cooper Center Longitudinal Study with an additional source of administrative data, providing a novel and cost-effective approach to the study of fitness in healthy adults that would not be possible otherwise.
In summary, we observed that fitness in healthy, middle-aged adults was more strongly associated with heart failure hospitalization than with coronary artery disease outcomes in later life. These findings suggest the importance of midlife fitness levels and subsequent heart failure risk in later life.
Supplementary Material
Acknowledgments
Sources of Funding: Dr. Berry receives funding from (1) the Dedman Family Scholar in Clinical Care endowment at UT Southwestern Medical Center, (2) grant K23 HL092229 from the National Heart, Lung, and Blood Institute, and (3) grant 10BG1A4280091 from the American Heart Association. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication. All authors have read and agree to the manuscript as written.
Footnotes
Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Paffenbarger RS, Jr, Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Medicine and science in sports and exercise. 1993;25:60–70. doi: 10.1249/00005768-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Nes BM, Janszky I, Aspenes ST, Bertheussen GF, Vatten LJ, Wisloff U. Exercise patterns and peak oxygen uptake in a healthy population: The hunt study. Medicine and science in sports and exercise. 2012;44:1881–1889. doi: 10.1249/MSS.0b013e318258b443. [DOI] [PubMed] [Google Scholar]
- 3.Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273:1093–1098. [PubMed] [Google Scholar]
- 4.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 5.Ekelund LG, Haskell WL, Johnson JL, Whaley FS, Criqui MH, Sheps DS. Physical fitness as a predictor of cardiovascular mortality in asymptomatic north american men. The lipid research clinics mortality follow-up study. N Engl J Med. 1988;319:1379–1384. doi: 10.1056/NEJM198811243192104. [DOI] [PubMed] [Google Scholar]
- 6.Erikssen G, Liestol K, Bjornholt J, Thaulow E, Sandvik L, Erikssen J. Changes in physical fitness and changes in mortality. Lancet. 1998;352:759–762. doi: 10.1016/S0140-6736(98)02268-5. [DOI] [PubMed] [Google Scholar]
- 7.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 8.Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 9.Berry JD, Willis B, Gupta S, Barlow CE, Lakoski SG, Khera A, Rohatgi A, de Lemos JA, Haskell W, Lloyd-Jones DM. Lifetime risks for cardiovascular disease mortality by cardiorespiratory fitness levels measured at ages 45, 55, and 65 years in men. The cooper center longitudinal study. J Am Coll Cardiol. 2011;57:1604–1610. doi: 10.1016/j.jacc.2010.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lakka TA, Venalainen JM, Rauramaa R, Salonen R, Tuomilehto J, Salonen JT. Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction. N Engl J Med. 1994;330:1549–1554. doi: 10.1056/NEJM199406023302201. [DOI] [PubMed] [Google Scholar]
- 11.Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA. 1984;252:487–490. [PubMed] [Google Scholar]
- 12.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 13.Lakka TA, Laukkanen JA, Rauramaa R, Salonen R, Lakka HM, Kaplan GA, Salonen JT. Cardiorespiratory fitness and the progression of carotid atherosclerosis in middle-aged men. Ann Intern Med. 2001;134:12–20. doi: 10.7326/0003-4819-134-1-200101020-00008. [DOI] [PubMed] [Google Scholar]
- 14.Lee CD, Jacobs DR, Jr, Hankinson A, Iribarren C, Sidney S. Cardiorespiratory fitness and coronary artery calcification in young adults: The cardia study. Atherosclerosis. 2009;203:263–268. doi: 10.1016/j.atherosclerosis.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rauramaa R, Rankinen T, Tuomainen P, Vaisanen S, Mercuri M. Inverse relationship between cardiorespiratory fitness and carotid atherosclerosis. Atherosclerosis. 1995;112:213–221. doi: 10.1016/0021-9150(94)05416-g. [DOI] [PubMed] [Google Scholar]
- 16.Fleg JL, Shapiro EP, O'Connor F, Taube J, Goldberg AP, Lakatta EG. Left ventricular diastolic filling performance in older male athletes. JAMA. 1995;273:1371–1375. [PubMed] [Google Scholar]
- 17.Fujimoto N, Prasad A, Hastings JL, Arbab-Zadeh A, Bhella PS, Shibata S, Palmer D, Levine BD. Cardiovascular effects of 1 year of progressive and vigorous exercise training in previously sedentary individuals older than 65 years of age. Circulation. 2010;122:1797–1805. doi: 10.1161/CIRCULATIONAHA.110.973784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saltin B, Blomqvist G, Mitchell JH, Johnson RL, Jr, Wildenthal K, Chapman CB. Response to exercise after bed rest and after training. Circulation. 1968;38:VII1–78. [PubMed] [Google Scholar]
- 19.Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358:1370–1380. doi: 10.1056/NEJMra072139. [DOI] [PubMed] [Google Scholar]
- 20.Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, Thomas JD, Palmer D, Levine BD. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110:1799–1805. doi: 10.1161/01.CIR.0000142863.71285.74. [DOI] [PubMed] [Google Scholar]
- 21.Willis BL, Gao A, Leonard D, Defina LF, Berry JD. Midlife fitness and the development of chronic conditions in later life. Archives of internal medicine. 2012:1–8. doi: 10.1001/archinternmed.2012.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pollock ML, Bohannon RL, Cooper KH, Ayres JJ, Ward A, White SR, Linnerud AC. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92:39–46. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 23.Prentice R, Williams B, Peterson A. On the regression analysis of multivariate failure time data. Biometrika. 1981;68:373–379. [Google Scholar]
- 24.Lin DY, Wei LJ. The robust inference for the cox proportional hazards model. Journal of the American Statistical Association. 1989;84:1074–1078. [Google Scholar]
- 25.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2011 update: A report from the american heart association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the u.S., 1979 to 2004. J Am Coll Cardiol. 2008;52:428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 27.Redfield MM. Heart failure — an epidemic of uncertain proportions. New England Journal of Medicine. 2002;347:1442–1444. doi: 10.1056/NEJMe020115. [DOI] [PubMed] [Google Scholar]
- 28.Wang CY, Haskell WL, Farrell SW, Lamonte MJ, Blair SN, Curtin LR, Hughes JP, Burt VL. Cardiorespiratory fitness levels among us adults 20-49 years of age: Findings from the 1999-2004 national health and nutrition examination survey. Am J Epidemiol. 2010;171:426–435. doi: 10.1093/aje/kwp412. [DOI] [PubMed] [Google Scholar]
- 29.Wei M, Gibbons LW, Mitchell TL, Kampert JB, Lee CD, Blair SN. The association between cardiorespiratory fitness and impaired fasting glucose and type 2 diabetes mellitus in men. Ann Intern Med. 1999;130:89–96. doi: 10.7326/0003-4819-130-2-199901190-00002. [DOI] [PubMed] [Google Scholar]
- 30.Aurigemma GP, Gaasch WH. Diastolic heart failure. New England Journal of Medicine. 2004;351:1097–1105. doi: 10.1056/NEJMcp022709. [DOI] [PubMed] [Google Scholar]
- 31.Bryg RJ, Williams GA, Labovitz AJ. Effect of aging on left ventricular diastolic filling in normal subjects. Am J Cardiol. 1987;59:971–974. doi: 10.1016/0002-9149(87)91136-2. [DOI] [PubMed] [Google Scholar]
- 32.Kokkinos P, Myers J, Kokkinos JP, Pittaras A, Narayan P, Manolis A, Karasik P, Greenberg M, Papademetriou V, Singh S. Exercise capacity and mortality in black and white men. Circulation. 2008;117:614–622. doi: 10.1161/CIRCULATIONAHA.107.734764. [DOI] [PubMed] [Google Scholar]
- 33.Mora S, Redberg RF, Sharrett AR, Blumenthal RS. Enhanced risk assessment in asymptomatic individuals with exercise testing and framingham risk scores. Circulation. 2005;112:1566–1572. doi: 10.1161/CIRCULATIONAHA.105.542993. [DOI] [PubMed] [Google Scholar]
- 34.Sui X, LaMonte MJ, Blair SN. Cardiorespiratory fitness as a predictor of nonfatal cardiovascular events in asymptomatic women and men. Am J Epidemiol. 2007;165:1413–1423. doi: 10.1093/aje/kwm031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sattelmair J, Pertman J, Ding EL, Kohl HW, 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: A meta-analysis. Circulation. 2011;124:789–795. doi: 10.1161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Hu G. Individual and joint associations of obesity and physical activity on the risk of heart failure. Congest Heart Fail. 2010;16:292–299. doi: 10.1111/j.1751-7133.2010.00189.x. [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Tuomilehto J, Jousilahti P, Antikainen R, Mahonen M, Katzmarzyk PT, Hu G. Occupational, commuting, and leisure-time physical activity in relation to heart failure among finnish men and women. J Am Coll Cardiol. 2010;56:1140–1148. doi: 10.1016/j.jacc.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 38.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation. 2010;121:237–244. doi: 10.1161/CIRCULATIONAHA.109.887893. [DOI] [PubMed] [Google Scholar]
- 39.Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119:44–52. doi: 10.1161/CIRCULATIONAHA.108.807289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in us men and women: Nhanes i epidemiologic follow-up study. Archives of internal medicine. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 41.Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to medicare costs. N Engl J Med. 1998;339:1122–1129. doi: 10.1056/NEJM199810153391606. [DOI] [PubMed] [Google Scholar]
- 42.Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Greenland P, Manheim LM, Dyer AR, Wang R, Lubitz J, Manning WG, Fries JF, Stamler J. Cardiovascular risk profile earlier in life and medicare costs in the last year of life. Archives of internal medicine. 2005;165:1028–1034. doi: 10.1001/archinte.165.9.1028. [DOI] [PubMed] [Google Scholar]
- 43.Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Wang R, Van Horn L, Manning WG, Manheim LM, Dyer AR, Greenland P, Stamler J. Relationship of fruit and vegetable consumption in middle-aged men to medicare expenditures in older age: The chicago western electric study. J Am Diet Assoc. 2005;105:1735–1744. doi: 10.1016/j.jada.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 44.Daviglus ML, Liu K, Yan LL, Pirzada A, Manheim L, Manning W, Garside DB, Wang R, Dyer AR, Greenland P, Stamler J. Relation of body mass index in young adulthood and middle age to medicare expenditures in older age. JAMA. 2004;292:2743–2749. doi: 10.1001/jama.292.22.2743. [DOI] [PubMed] [Google Scholar]
- 45.Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM. Estimation of ten-year risk of fatal cardiovascular disease in europe: The score project. European Heart Journal. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 46.Goff DC, Jr, Pandey DK, Chan FA, Ortiz C, Nichaman MZ. Congestive heart failure in the united states: Is there more than meets the i(cd code)? The corpus christi heart project. Archives of internal medicine. 2000;160:197–202. doi: 10.1001/archinte.160.2.197. [DOI] [PubMed] [Google Scholar]
- 47.Rector TS, Wickstrom SL, Shah M, Thomas Greeenlee N, Rheault P, Rogowski J, Freedman V, Adams J, Escarce JJ. Specificity and sensitivity of claims-based algorithms for identifying members of medicare+choice health plans that have chronic medical conditions. Health Serv Res. 2004;39:1839–1857. doi: 10.1111/j.1475-6773.2004.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DiMartino LD, Hammill BG, Curtis LH, Gottdiener JS, Manolio TA, Powe NR, Schulman KA. External validity of the cardiovascular health study: A comparison with the medicare population. Med Care. 2009;47:916–923. doi: 10.1097/MLR.0b013e318197b104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of medicare claims-based diagnosis of acute myocardial infarction: Estimating positive predictive value on the basis of review of hospital records. American Heart Journal. 2004;148:99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


