Abstract
Echocardiography plays a longstanding and vital role in the management of atrial fibrillation (AF). Advances in 2D imaging, Doppler echocardiography and strain imaging have all contributed to major progress in AF treatment. Echocardiographically measured left atrial (LA) volume is a powerful predictor of maintenance of sinus rhythm following cardioversion as well as risk of thrombus formation and thromboembolism. Doppler derived parameters of atrial mechanical function including atrial ejection force provide related prognostic information. Transesophageal echocardiocardiograpy (TEE) guided cardioversion of AF allows for rapid conversion to sinus rhythm without prolonged oral anticoagulation, and TEE serves as a useful tool during catheter ablation of AF and atrial flutter. Newer measures derived from speckle tracking offer great promise in further improving the care of patients with AF.
Introduction
Almost since its clinical introduction 50 years ago,echocardiography has played a vital role in the management of atrial fibrillation (AF).That role continues to expand as advances in both echocardiographic technology and arrhythmia treatment combine synergistically. The revolution in catheter based treatment of AF has increased the demand for more precise imaging from a variety of modalities,including transthoracic(TTE),transesophageal (TEE), Doppler echocardiography and speckle tracking. Increased precision in assessment of left atrial (LA) anatomy and function made possible by advances in these modalities has enhanced our understanding of the natural history of AF, and has provided superior tools for assessment of treatment efficacy.In the following pages, we undertake to review the many contributions of echocardiography to AF management and to highlight recent advances orgin echocardiographic imaging relevant to the management of this most common arrhythmia.
Estimation of LA size in the setting of AF
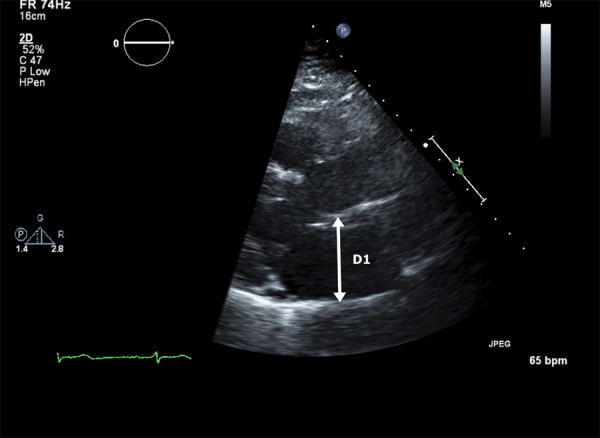
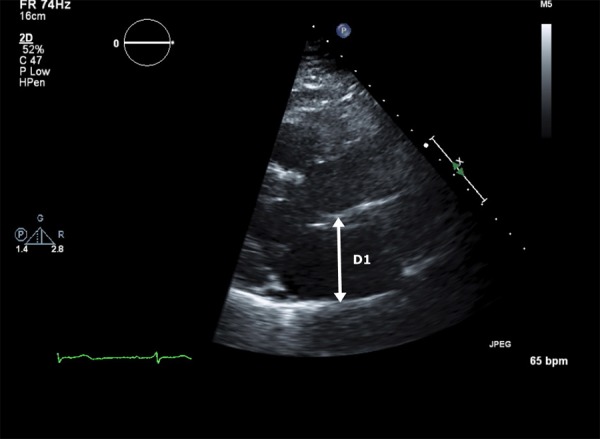
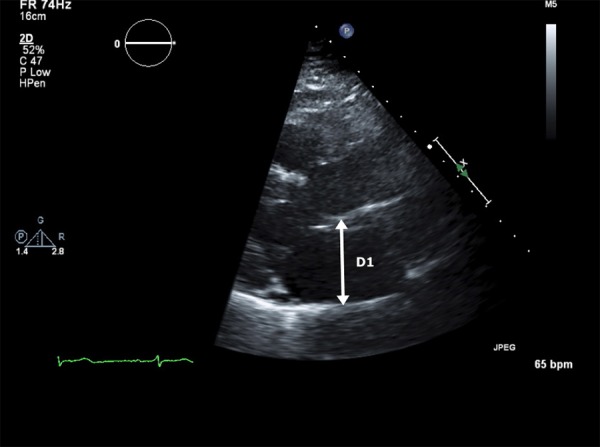
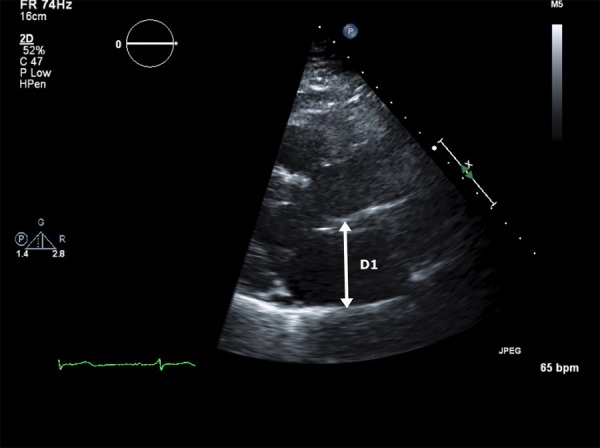
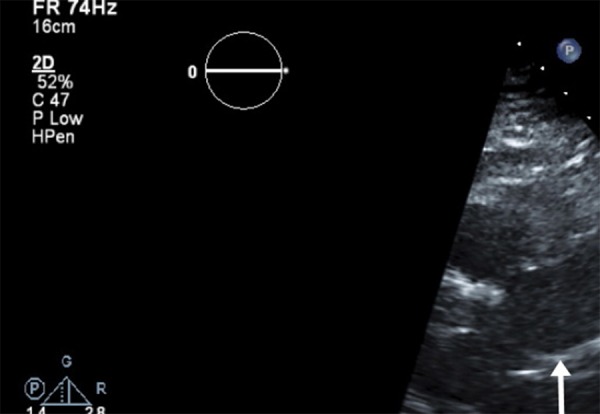
Quantification of atrial volumes using digitized images has produced major advances in our understanding of the relationship between LA size and both short and long-term outcome in patients with AF. LA volume may be estimated by several techniques.[1] The simplest but least accurate formula for calculation of LA volume assumes the chamber takes the shape of a sphere and cubes it along 3 axes using the AP dimension; LA-Cube = 4/3 π(APDimension/2)3.[2] This method’s major drawback is the inherent inaccuracy of the sphericity assumption, as well as the reality that any error in AP dimension will be multiplied 3-fold. An alternative ellipsoid model uses the LA M-mode AP dimension from the parasternal long axis view (D1), the LA minor diameter in the longaxis view (D2), and the length of the LA from roof to the center of the closed mitral valve at end systole from the apical four-chamber viewsas (4π/3)(L/2)(D1/2)(D2/2) (Figures 1a and 1b).
Figure 1a. The anteroposterior dimension (D1) obtained in the parasternal long axis view is used for the ellipsoidal estimation of left atrial (LA) volume.
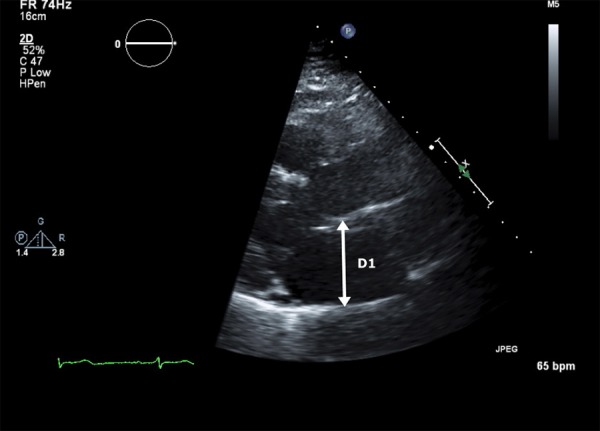
Figure 1b. The LA minor dimension (D2) and LA length from the roof of the atrium length (D3) obtained in the apical 4-chamber view complete the 3 axes required for the calculation; (4π/3) (L/2)(D1/2)(D2/2).
Both of these methods have largely been supplanted by either the area-length method[3] or the biplane method of discs (Simpson’s rule). The area-length method assumes an ellipsoidal shape to the LA and consequently applies the formula for calculation of an ellipse by measuring the LA area in the 4-chamber and in the 2-chamber views;LA volume(area-length) = (0.85 * LA area(4 chamber) * LA area(2 chamber))/Shortest LA length
The area-length method’s inherent disadvantage is its primary assumption of LA three-dimensional (3D) shape. For dilated or otherwise deformed LA, the method may either over or underestimate true LA volume.
Calculation of LA volume using Simpson’s rule, now available on most sonographs and off line analysis systems, represents the current gold standard for LA volume measurement (Figures 2a and 2b).[4] The method’s advantages are analogous to those appreciated for left ventricular (LV) volume estimation, as its accuracy does not depend upon geometry or symmetry of 3 dimensional LA shape. In contrast to the primary limitation to LV biplane measurements (inadequate endocardial visualization), poor blood tissue interface definition is less common given the thin walled nature of the LA. Although correlation between LA dimension and LA volume indexed for body surface area (LAVI) is significant (r=0.69, p<0.001), LAVI is increased in nearly 60% of patients with normal LA dimension.5 For patients in sinus rhythm, LA volumes can be measured throughout the cardiac cycle, and systolic and diastolic volumes can be subtracted for calculation of LA emptying volume.[6]
Figure 2a. LA volume calculated using the method of discs (Simpson’s rule) in the apical 4-chamber view. The calculation is performed using automated software.
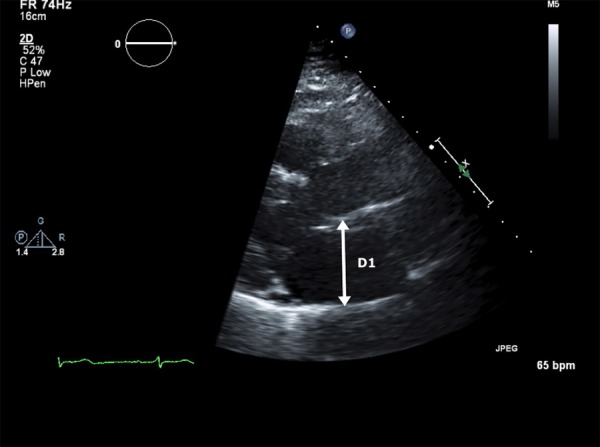
Figure 2b. LA volume calculated using the method of discs (Simpson’s rule) in the apical 2-chamber view. The biplane measurement is calculated using the diameters from both views to calculate the volume of each disc and then summing the volumes together.
In the setting of AF, increased LA size represents both cause and consequence. In longitudinal studies, increased LA dimension is an important predictor of risk for the development for AF.[7,8] Subsequently, both right atrial (RA) and LA size increase once AF occurs.[9] The increase in biatrial size is progressive and is directly related to AF duration.[10] Conversely, both RA and LA size decline within hours following cardioversion and maintenance of sinus rhythm.[1] The decline continues to progress for up to 8 months (if sinus rhythm is maintained).[12] Patients who convert spontaneously enjoy a faster rate of reduction in LA dimension compared to those who require either electrical or chemical cardioversion.[13]
Studies investigating the relation between LA size and the ability to maintain long term restoration of sinus rhythm following cardioversion have produced discrepant results. Several studies have reported reduced rates of maintenance of sinus rhythm in patients with LA anteroposterior dimension >45 mm.[14-16] Other observers have reported no relation between any echocardiographic descriptor of LA size[17-19] or any cutoff point predictive of long term success post cardioversion.[20] Studies representing both sides of this issue have often been limited by small sample size, heterogeneous populations and short term follow-up.In the largest (411 patients) and most recent study to date, patients maintaining sinus rhythm for at least 6 months had significantly smaller LA volumes (31.4 ml/m2) than those who did not maintain sinus rhythm (39.7 ml/m2).21Although the RA has not been studied as extensively, changes in RA size and function pre and post cardioversion appear to parallel those observed in the LA.[9,11,12]
Although 2D guided M-mode measurement of LA dimension has provided important clinical and prognostic information, the correlation between calculated LA volume and LA dimension is relatively poor,[22] and LA volume has been shown to be superior to the older measurement.[23,24] LAVI has emerged as a powerful predictor of outcome in a wide variety of settings including heart failure,[25,[26] myocardial infarction,[27] and ischemic stroke.[28] In a large (n=1655) prospective series, LAVI emerged as a highly significant predictor of the development new AF.[29] In patients with lone AF, increased LAVI predicts a higher frequency of adverse cardiac events.[30]
Functional Measures of LA Function Pre and Post Cardioversion
Interrogation of diastolic flow through the mitral valve using spectral Doppler provides a powerful measure of LA passive and mechanical function. Following cardioversion from AF, the presence of a p wave on the surface electrocardiogram demonstrates the return of atrial electrical activity. Return of atrial mechanical function, however, as demonstrated by the transmitral (and transtricuspid) time velocity integral (VTI) produced by atrial contraction (A wave) is often delayed.[31] The rate of return of atrial mechanical function is dependent on both the duration of AF prior to cardioversion[32,33] and the mode of cardioversion.[34] Biochemical function, as demonstrated by the progressive return of plasma atrial naturetic peptide, reappears coincident with A wave return.[35] Although initial A wavevelocities post cardioversion are not predictive of long term success,[31-[36] lack of A wave progression, and peak transmittal A wave velocity at 24 hours in patients who maintain sinus rhythm are higher compared to those return to AF post cardioversion.[37]
Atrial ejection force describes the force generated by the contracting atrium in terms of classical mechanics; force=mass x acceleration.[38] The mass of blood ejected by the LA is calculated as the product of blood volume ejected during the acceleration phase x blood density (ρ).The blood volume ejected during the acceleration phase is calculated as ½ the time velocity integral of the A wave x the mitral valve annular diameter, and acceleration is calculated as the 1st derivative of the change in A wave velocity, dA/dt, again during the acceleration phase.Combining the two variables cancels out the time factor and simplifies to:Atrial ejection force= 0.5 (mitral valve area) (peak A wave velocity )[2]
In a fashion analogous to peak A wave velocity, recovery and magnitude of atrial ejection force is a predictor of long term maintenance of normal sinus rhythm.[38]
For patients in AF, LA appendage (LAA) flow measured by transesophageaal echocardiography (TEE) guided pulse Doppler interrogation at the mouth of the LAA is a powerful predictor of both thromboembolic risk and rhythm outcome. The pattern produced by the LAA flow in AF differs distinctly from that seen in sinus rhythm; the characteristic 4 phase pattern of appendage filling and contraction (Figure 3a)[39] is replaced by an irregular chaotic series of waves of varying velocity (Figure 3b). As LAA function deteriorates, the morphology of the flow velocity becomes less distinct and peak velocity declines markedly (Figure 3c). Decreased mean LAA flow velocity (<40 cm/sec) is strongly correlated with a high frequency of spontaneous echo contrast,[40] increased incidence of LAA thrombus[41]-[43] and subsequent clinical thromboembolism.[44] Reduced LAA flow velocity (<20 cm/sec) is also a significant negative predictor of maintenance of sinus rhythm following cardioversion.[45-47] TTE has also been reported to be a useful modality for evaluation of LAA appendage size and function.[48] However, the utility of TTE for identification of AF patients who can be safely cardioverted without prolonged anticoagulation is unknown.
Figure 3a. The pulse spectral Doppler appearance of LA appendage (LAA) flow during sinus rhythm (Reprinted with permission from Silverman DI and Manning WJ, The Complete Guide to Echocardiography. Jones & Bartlett Learning 2001; Sudbury MA).
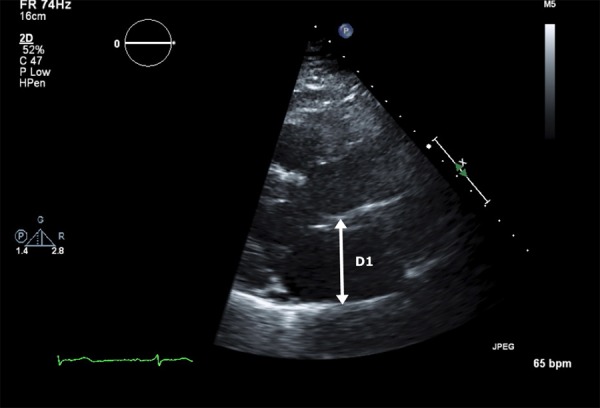
Figure 3b. LAA flow during atrial fibrillation. Flow velocities in this example are normal (>40 cm/sec).
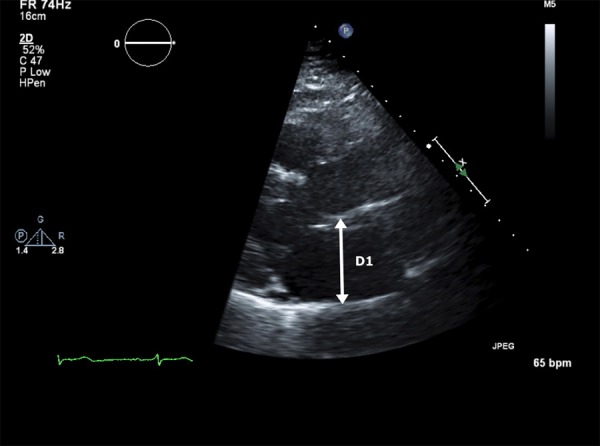
Figure 3c. LAA flow velocities are marked reduced in this example.
TEE Guided Cardioversion of AF and Its Role in Catheter Ablation
Since the first report of the use of TEE for identification of LAA thrombi in patients with AF, TEE guided cardioversion has endured as a therapeutic strategy for converting patients with AF (and atrial flutter) to sinus rhythm without the use of prolonged pre-cardioversion anticoagulation. Compared to the gold standard of open surgical visualization, the sensitivity of TEE for detection of LA thrombi is 100%, and the specificity is 99%.[49]-[53] To date, four prospective trials have documented an equivalent incidence of clinical thromboembolism following a negative TEE for thrombus, compared with the traditional approach of 4 weeks of therapeutic warfarin anticoagulation (International Normalized Ratio 2-3) (Table 1).[54]-[57] In addition, TEE guided cardioversion is associated with a reduced incidence of bleeding,[55] is cost effective,[58] and may be associated with an interval dependent improvement in the frequency of long term suppression of AF post cardioversion.[59] The efficacy of the technique depends crucially upon the use of anticoagulation (INR 2-3) in the peri-cardioversion and post-cardioversion period.Data demonstrate more impaired LAA ejection velocity post electrical, chemical and even spontaneous cardioversion. The majority of clinical thromboembolic events following a TEE negative for thrombus have occurred either in the setting of subtherapeutic anticoagulation or in the absence of anticoagulation altogether. Anectodal reports have also demonstrated apparent dissociation of function between the body of the LA (in sinus rhythm) and the LAA (in mechanical AF).[60]Administration of echo contrast has been reported to improve accuracy for LAA thrombus detection (Figures 4a and 4b).[61]
Table 1. Studies Evaluating Association of Diabetes with Atrial Fibrillation.
| Study | (%) (n) of Patients Enrolled | (%)(n) of Patients w/ A thrombi | % (n) of Embolic Events Post cardioversion |
|---|---|---|---|
| Manning(54) | 223 | 15(34) | 0(0) |
| Stoddard(56) | 206 | 18(37) | 0(0) |
| Seidl(57) | 719* | 7.7(55) | 0.8(6) |
| Klein(55) | 619* | 76(14) | 0.8(5) |
Figure 4a. Transesophageal echocardiography (TEE), midesophageal view in a patient reveals an indistinct haziness (arrow) in the body of the LAA.
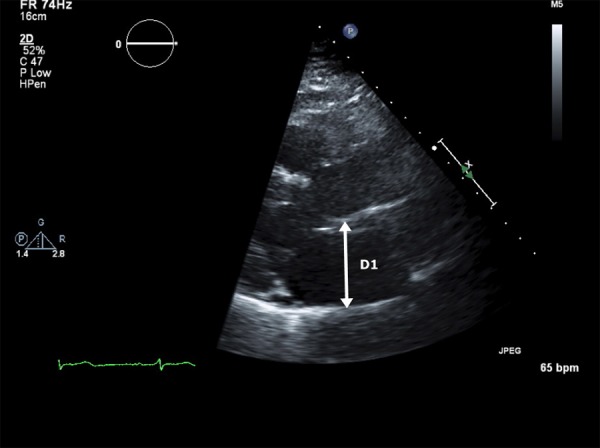
Figure 4b. Injection of 2 cc of echo contrast (?Definity) solution completely opacifies the LAA , providing convincing evidence that there is no thrombus.The patient underwent successful conversion to sinus rhythm a few moments later without complication.
Although prospective data validating TEE for exclusion of LAA thrombi prior to catheter ablation are somewhat limited,[62] the technique has gained wide acceptance for that purpose.[63,64] Whether TEE is required for exclusion of thrombi in lower risk patients remains controversial,[65] as several observers have reported an incidence of LAA thrombi of <1.5% in patients with a CHADS2 score ≤1,[66,67]while Others have reported a small but persistent incidence of thrombi even in the presence of therapeutic anticoagulation.[68] TEE is also commonly employed in combination with alternate imaging modalities for identification of pulmonary vein anatomy and location, and for determination of pulmonary vein stenosis post procedure.[69] 3D TEE provides an important tool for catheter placement during transeptal puncture, especially in the presence of structural abnormalities not readily detected by conventional radiographic imaging techniques[70,71]
Measures of LA Function Derived from Tissue Doppler Imaging and Speckle Tracking
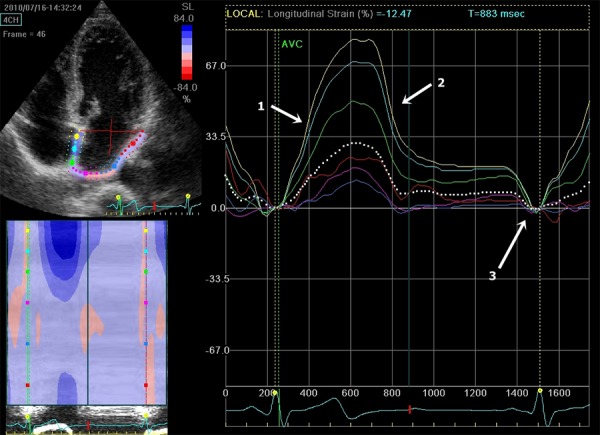
The application of techniques for measurement of atrial strain provides a novel technique for assessment of the relation between LA function and AF in a variety of settings. Strain describes the rate of myocardial deformation as the ratio of the difference in shortening of a particular segment to its initial length; L-L0/L0 where L0 =initial length and L=shortened length (Figures 5a). Systolic strain is thus by convention a negative value, as is its 1st derivative with respect to time, strain rate. Peak systolic strain can be calculated for any desired length and at any location along the blood tissue interface. While measurement of atrial strain and strain rate are still in their earliest phases, several intriguing findings have already been reported. Compared to LAA flow velocities, reduced atrial myocardial velocity, strain and strain rate are superior predictors of persistence of sinus rhythm after cardioversion.[46,72] Increased LA strain is also predictive of long term success post catheter ablation of AF [73-[75] and long term reduction in atrial volume post procedure.[76] Post cardioversion, atrial strain rate increases for up to 30 days and is correlated with increasing A wave velocity ( ).
Figure 5. Atrial strain mapped using speckle tracking.
Echocardiographic Predictors of Thromboembolism in AF
While the average annual stroke risk for unanticoagulated patients in AF approximates 5%,[78] individual risk varies greatly. In addition to well described clinical factors,[79] a number of echocardiographic variables have endured as consistent predictors of increased risk for thromboembolism. Reduced left ventricular ejection fraction (LVEF) (<35%) is considered such a powerful factor that its presence is an indication for anticoagulation regardless of other factors.[80] Mitral regurgitation appears to be protective [81]( TEE parameters of increased clinical thromboembolic risk [42,74] and mortality[51] include spontaneous echo contrast, decreased LAA fibrillatory wave velocity and LA thrombus (Figures 6), and complex aortic plaque.
Figure 6. TEE midesophageal view demonstrates LAA thrombus (arrow).
Although no single echocardiographic variable discriminates between the presence and absence of LAA thrombus, increased LA volume index, especially in combination with reduced LVEF is associated with increased frequency of LAA thrombus formation at every level of CHADS2 score.[42] Conversely, in low risk patients (CHADS2 score ≤1) a normal LVEF and normal LAVIare associated with the near absence of LAA thrombus.[42] We have observed similar results in a series of patients with AF and CHADS2 score ≤1, in which LAVI is significantly increased compared to age and sex matched controls (unpublished data). Atrial strain is reduced in patients with AF and previous stroke compared to stroke free controls[82] and decreased LA strain is associated with increased stroke risk as determined by CHADS2 scores.[83]
In summary echocardiography in all its manifestations plays an irreplaceable role in the management and prognosis of patients with AF. As it has in the past, we expect future advances in echocardiography will continue to strengthen this enduring partnership between imaging and arrhythmia.
References
- 1.Lang Roberto M, Bierig Michelle, Devereux Richard B, Flachskampf Frank A, Foster Elyse, Pellikka Patricia A, Picard Michael H, Roman Mary J, Seward James, Shanewise Jack S, Solomon Scott D, Spencer Kirk T, Sutton Martin St John, Stewart William J. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005 Dec;18 (12):1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Khankirawatana Banthit, Khankirawatana Suwanee, Porter Thomas. How should left atrial size be reported? Comparative assessment with use of multiple echocardiographic methods. Am. Heart J. 2004 Feb;147 (2):369–74. doi: 10.1016/j.ahj.2003.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Loperfido F, Pennestri F, Digaetano A, Scabbia E, Santarelli P, Mongiardo R, Schiavoni G, Coppola E, Manzoli U. Assessment of left atrial dimensions by cross sectional echocardiography in patients with mitral valve disease. Br Heart J. 1983 Dec;50 (6):570–8. doi: 10.1136/hrt.50.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kircher B, Abbott J A, Pau S, Gould R G, Himelman R B, Higgins C B, Lipton M J, Schiller N B. Left atrial volume determination by biplane two-dimensional echocardiography: validation by cine computed tomography. Am. Heart J. 1991 Mar;121 (3 Pt 1):864–71. doi: 10.1016/0002-8703(91)90200-2. [DOI] [PubMed] [Google Scholar]
- 5.Barbieri Andrea, Bursi Francesca, Zanasi Vera, Veronesi Benedetta, Cioni Elena, Modena Maria Grazia. Left atrium reclassified: application of the American Society of Echocardiography/European Society of Cardiology cutoffs to unselected outpatients referred to the echocardiography laboratory. J Am Soc Echocardiogr. 2008 May;21 (5):433–8. doi: 10.1016/j.echo.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 6.Erol Mustafa Kemal, Yilmaz Mustafa, Acikel Mahmut, Karakelleoglu Sule. Left atrial mechanical function in patients with essential hypertension. Acta Cardiol. 2002 Oct;57 (5):323–7. doi: 10.2143/AC.57.5.2005447. [DOI] [PubMed] [Google Scholar]
- 7.Vaziri S M, Larson M G, Benjamin E J, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994 Feb;89 (2):724–30. doi: 10.1161/01.cir.89.2.724. [DOI] [PubMed] [Google Scholar]
- 8.Aronow W S, Ahn C, Kronzon I. Echocardiographic findings associated with atrial fibrillation in 1,699 patients aged > 60 years. Am. J. Cardiol. 1995 Dec 01;76 (16):1191–2. doi: 10.1016/s0002-9149(99)80336-1. [DOI] [PubMed] [Google Scholar]
- 9.Sanfilippo A J, Abascal V M, Sheehan M, Oertel L B, Harrigan P, Hughes R A, Weyman A E. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation. 1990 Sep;82 (3):792–7. doi: 10.1161/01.cir.82.3.792. [DOI] [PubMed] [Google Scholar]
- 10.Petersen P, Kastrup J, Brinch K, Godtfredsen J, Boysen G. Relation between left atrial dimension and duration of atrial fibrillation. Am. J. Cardiol. 1987 Aug 01;60 (4):382–4. doi: 10.1016/0002-9149(87)90253-0. [DOI] [PubMed] [Google Scholar]
- 11.Gosselink A T, Crijns H J, Hamer H P, Hillege H, Lie K I. Changes in left and right atrial size after cardioversion of atrial fibrillation: role of mitral valve disease. J. Am. Coll. Cardiol. 1993 Nov 15;22 (6):1666–72. doi: 10.1016/0735-1097(93)90593-p. [DOI] [PubMed] [Google Scholar]
- 12.Van Gelder I C, Crijns H J, Van Gilst W H, Hamer H P, Lie K I. Decrease of right and left atrial sizes after direct-current electrical cardioversion in chronic atrial fibrillation. Am. J. Cardiol. 1991 Jan 01;67 (1):93–5. doi: 10.1016/0002-9149(91)90108-w. [DOI] [PubMed] [Google Scholar]
- 13.Mattioli A V, Sansoni S, Lucchi G R, Mattioli G. Serial evaluation of left atrial dimension after cardioversion for atrial fibrillation and relation to atrial function. Am. J. Cardiol. 2000 Apr 01;85 (7):832–6. doi: 10.1016/s0002-9149(99)00876-0. [DOI] [PubMed] [Google Scholar]
- 14.Henry W L, Morganroth J, Pearlman A S, Clark C E, Redwood D R, Itscoitz S B, Epstein S E. Relation between echocardiographically determined left atrial size and atrial fibrillation. Circulation. 1976 Feb;53 (2):273–9. doi: 10.1161/01.cir.53.2.273. [DOI] [PubMed] [Google Scholar]
- 15.Höglund C, Rosenhamer G. Echocardiographic left atrial dimension as a predictor of maintaining sinus rhythm after conversion of atrial fibrillation. Acta Med Scand. 1985;217 (4):411–5. doi: 10.1111/j.0954-6820.1985.tb02716.x. [DOI] [PubMed] [Google Scholar]
- 16.Brodsky M A, Allen B J, Capparelli E V, Luckett C R, Morton R, Henry W L. Factors determining maintenance of sinus rhythm after chronic atrial fibrillation with left atrial dilatation. Am. J. Cardiol. 1989 May 01;63 (15):1065–8. doi: 10.1016/0002-9149(89)90079-9. [DOI] [PubMed] [Google Scholar]
- 17.Dittrich H C, Erickson J S, Schneiderman T, Blacky A R, Savides T, Nicod P H. Echocardiographic and clinical predictors for outcome of elective cardioversion of atrial fibrillation. Am. J. Cardiol. 1989 Jan 15;63 (3):193–7. doi: 10.1016/0002-9149(89)90284-1. [DOI] [PubMed] [Google Scholar]
- 18.Grey E, Silverman D I. Efficacy of type 1C antiarrhythmic agents for treatment of resistant atrial fibrillation. Pacing Clin Electrophysiol. 1993 Dec;16 (12):2235–40. doi: 10.1111/j.1540-8159.1993.tb02329.x. [DOI] [PubMed] [Google Scholar]
- 19.Arnar D O, Danielsen R. Factors predicting maintenance of sinus rhythm after direct current cardioversion of atrial fibrillation and flutter: a reanalysis with recently acquired data. Cardiology. 1996 May 1;87 (3):181–8. doi: 10.1159/000177084. [DOI] [PubMed] [Google Scholar]
- 20.Volgman A S, Soble J S, Neumann A, Mukhtar K N, Iftikhar F, Vallesteros A, Liebson P R. Effect of left atrial size on recurrence of atrial fibrillation after electrical cardioversion: atrial dimension versus volume. Am J Card Imaging. 1996 Oct;10 (4):261–5. [PubMed] [Google Scholar]
- 21.Marchese Procolo, Bursi Francesca, Delle Donne Grazia, Malavasi Vincenzo, Casali Edoardo, Barbieri Andrea, Melandri Francesco, Modena Maria Grazia. Indexed left atrial volume predicts the recurrence of non-valvular atrial fibrillation after successful cardioversion. Eur J Echocardiogr. 2011 Mar;12 (3):214–21. doi: 10.1093/ejechocard/jeq176. [DOI] [PubMed] [Google Scholar]
- 22.Schabelman S, Schiller N B, Silverman N H, Ports T A. Left atrial volume estimation by two-dimensional echocardiography. Cathet Cardiovasc Diagn. 1981;7 (2):165–78. doi: 10.1002/ccd.1810070206. [DOI] [PubMed] [Google Scholar]
- 23.Wade M R, Chandraratna P A, Reid C L, Lin S L, Rahimtoola S H. Accuracy of nondirected and directed M-mode echocardiography as an estimate of left atrial size. Am. J. Cardiol. 1987 Nov 15;60 (14):1208–11. doi: 10.1016/0002-9149(87)90434-6. [DOI] [PubMed] [Google Scholar]
- 24.Lester S J, Ryan E W, Schiller N B, Foster E. Best method in clinical practice and in research studies to determine left atrial size. Am. J. Cardiol. 1999 Oct 01;84 (7):829–32. doi: 10.1016/s0002-9149(99)00446-4. [DOI] [PubMed] [Google Scholar]
- 25.Ristow Bryan, Ali Sadia, Whooley Mary A, Schiller Nelson B. Usefulness of left atrial volume index to predict heart failure hospitalization and mortality in ambulatory patients with coronary heart disease and comparison to left ventricular ejection fraction (from the Heart and Soul Study). Am. J. Cardiol. 2008 Jul 01;102 (1):70–6. doi: 10.1016/j.amjcard.2008.02.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rossi Andrea, Temporelli Pier Luigi, Quintana Miguel, Dini Frank L, Ghio Stefano, Hillis Graham S, Klein Allan L, Marsan Nina Ajmone, Prior David L, Yu Cheuk Man, Poppe Katrina K, Doughty Robert N, Whalley Gillian A. Independent relationship of left atrial size and mortality in patients with heart failure: an individual patient meta-analysis of longitudinal data (MeRGE Heart Failure). Eur. J. Heart Fail. 2009 Oct;11 (10):929–36. doi: 10.1093/eurjhf/hfp112. [DOI] [PubMed] [Google Scholar]
- 27.Moller Jacob E, Hillis Graham S, Oh Jae K, Seward James B, Reeder Guy S, Wright R Scott, Park Seung W, Bailey Kent R, Pellikka Patricia A. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003 May 06;107 (17):2207–12. doi: 10.1161/01.CIR.0000066318.21784.43. [DOI] [PubMed] [Google Scholar]
- 28.Fatema Kaniz, Bailey Kent R, Petty George W, Meissner Irene, Osranek Martin, Alsaileek Ahmed A, Khandheria Bijoy K, Tsang Teresa S, Seward James B. Increased left atrial volume index: potent biomarker for first-ever ischemic stroke. Mayo Clin. Proc. 2008 Oct;83 (10):1107–15. doi: 10.4065/83.10.1107. [DOI] [PubMed] [Google Scholar]
- 29.Tsang T S, Barnes M E, Bailey K R, Leibson C L, Montgomery S C, Takemoto Y, Diamond P M, Marra M A, Gersh B J, Wiebers D O, Petty G W, Seward J B. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin. Proc. 2001 May;76 (5):467–75. doi: 10.4065/76.5.467. [DOI] [PubMed] [Google Scholar]
- 30.Osranek Martin, Bursi Francesca, Bailey Kent R, Grossardt Brandon R, Brown Robert D, Kopecky Stephen L, Tsang Teresa S, Seward James B. Left atrial volume predicts cardiovascular events in patients originally diagnosed with lone atrial fibrillation: three-decade follow-up. Eur. Heart J. 2005 Dec;26 (23):2556–61. doi: 10.1093/eurheartj/ehi483. [DOI] [PubMed] [Google Scholar]
- 31.Manning W J, Leeman D E, Gotch P J, Come P C. Pulsed Doppler evaluation of atrial mechanical function after electrical cardioversion of atrial fibrillation. J. Am. Coll. Cardiol. 1989 Mar 01;13 (3):617–23. doi: 10.1016/0735-1097(89)90602-5. [DOI] [PubMed] [Google Scholar]
- 32.Manning W J, Leeman D E, Gotch P J, Come P C. Pulsed Doppler evaluation of atrial mechanical function after electrical cardioversion of atrial fibrillation. J. Am. Coll. Cardiol. 1989 Mar 01;13 (3):617–23. doi: 10.1016/0735-1097(89)90602-5. [DOI] [PubMed] [Google Scholar]
- 33.Sparks P B, Jayaprakash S, Mond H G, Vohra J K, Grigg L E, Kalman J M. Left atrial mechanical function after brief duration atrial fibrillation. J. Am. Coll. Cardiol. 1999 Feb;33 (2):342–9. doi: 10.1016/s0735-1097(98)00585-3. [DOI] [PubMed] [Google Scholar]
- 34.Harjai K J, Mobarek S K, Cheirif J, Boulos L M, Murgo J P, Abi-Samra F. Clinical variables affecting recovery of left atrial mechanical function after cardioversion from atrial fibrillation. J. Am. Coll. Cardiol. 1997 Aug;30 (2):481–6. doi: 10.1016/s0735-1097(97)00173-3. [DOI] [PubMed] [Google Scholar]
- 35.Wozakowska-Kapłon Beata, Opolski Grzegorz. Concomitant recovery of atrial mechanical and endocrine function after cardioversion in patients with persistent atrial fibrillation. J. Am. Coll. Cardiol. 2003 May 21;41 (10):1716–20. doi: 10.1016/s0735-1097(03)00306-1. [DOI] [PubMed] [Google Scholar]
- 36.Dethy M, Chassat C, Roy D, Mercier L A. Doppler echocardiographic predictors of recurrence of atrial fibrillation after cardioversion. Am. J. Cardiol. 1988 Oct 01;62 (10 Pt 1):723–6. doi: 10.1016/0002-9149(88)91210-6. [DOI] [PubMed] [Google Scholar]
- 37.Grundvold Irene, Tveit Arnljot, Smith Pål, Seljeflot Ingebjørg, Abdelnoor Michael, Arnesen Harald. The predictive value of transthoracic echocardiographic variables for sinus rhythm maintenance after electrical cardioversion of atrial fibrillation. Results from the CAPRAF study, a prospective, randomized, placebo-controlled study. Cardiology. 2008;111 (1):30–5. doi: 10.1159/000113424. [DOI] [PubMed] [Google Scholar]
- 38.Manning W J, Silverman D I, Katz S E, Douglas P S. Atrial ejection force: a noninvasive assessment of atrial systolic function. J. Am. Coll. Cardiol. 1993 Jul;22 (1):221–5. doi: 10.1016/0735-1097(93)90838-r. [DOI] [PubMed] [Google Scholar]
- 39.Agmon Y, Khandheria B K, Gentile F, Seward J B. Echocardiographic assessment of the left atrial appendage. J. Am. Coll. Cardiol. 1999 Dec;34 (7):1867–77. doi: 10.1016/s0735-1097(99)00472-6. [DOI] [PubMed] [Google Scholar]
- 40.Fatkin D, Kelly R P, Feneley M P. Relations between left atrial appendage blood flow velocity, spontaneous echocardiographic contrast and thromboembolic risk in vivo. J. Am. Coll. Cardiol. 1994 Mar 15;23 (4):961–9. doi: 10.1016/0735-1097(94)90644-0. [DOI] [PubMed] [Google Scholar]
- 41.Santiago D, Warshofsky M, Li Mandri G, Di Tullio M, Coromilas J, Reiffel J, Homma S. Left atrial appendage function and thrombus formation in atrial fibrillation-flutter: a transesophageal echocardiographic study. J. Am. Coll. Cardiol. 1994 Jul;24 (1):159–64. doi: 10.1016/0735-1097(94)90557-6. [DOI] [PubMed] [Google Scholar]
- 42.Ayirala Srilatha, Kumar Simi, O'Sullivan David M, Silverman David I. Echocardiographic predictors of left atrial appendage thrombus formation. J Am Soc Echocardiogr. 2011 May;24 (5):499–505. doi: 10.1016/j.echo.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Rubin D N, Katz S E, Riley M F, Douglas P S, Manning W J. Evaluation of left atrial appendage anatomy and function in recent-onset atrial fibrillation by transesophageal echocardiography. Am. J. Cardiol. 1996 Oct 01;78 (7):774–8. doi: 10.1016/s0002-9149(96)00419-5. [DOI] [PubMed] [Google Scholar]
- 44.Kamp O, Verhorst P M, Welling R C, Visser C A. Importance of left atrial appendage flow as a predictor of thromboembolic events in patients with atrial fibrillation. Eur. Heart J. 1999 Jul;20 (13):979–85. doi: 10.1053/euhj.1998.1453. [DOI] [PubMed] [Google Scholar]
- 45.Antonielli Emanuele, Pizzuti Alfredo, Pálinkás Attila, Tanga Mattia, Gruber Noèmi, Michelassi Claudio, Varga Albert, Bonzano Alessandro, Gandolfo Nicola, Halmai László, Bassignana Antonia, Imran Muhammad Babar, Delnevo Fabrizio, Csanády Miklós, Picano Eugenio. Clinical value of left atrial appendage flow for prediction of long-term sinus rhythm maintenance in patients with nonvalvular atrial fibrillation. J. Am. Coll. Cardiol. 2002 May 01;39 (9):1443–9. doi: 10.1016/s0735-1097(02)01800-4. [DOI] [PubMed] [Google Scholar]
- 46.Di Salvo Giovanni, Caso Pio, Lo Piccolo Rosalia, Fusco Angela, Martiniello Alfonso R, Russo Maria G, D'Onofrio Antonio, Severino Sergio, Calabró Paolo, Pacileo Giuseppe, Mininni Nicola, Calabró Raffaele. Atrial myocardial deformation properties predict maintenance of sinus rhythm after external cardioversion of recent-onset lone atrial fibrillation: a color Doppler myocardial imaging and transthoracic and transesophageal echocardiographic study. Circulation. 2005 Jul 19;112 (3):387–95. doi: 10.1161/CIRCULATIONAHA.104.463125. [DOI] [PubMed] [Google Scholar]
- 47.Verhorst P M, Kamp O, Welling R C, Van Eenige M J, Visser C A. Transesophageal echocardiographic predictors for maintenance of sinus rhythm after electrical cardioversion of atrial fibrillation. Am. J. Cardiol. 1997 May 15;79 (10):1355–9. doi: 10.1016/s0002-9149(97)00139-2. [DOI] [PubMed] [Google Scholar]
- 48.Coletta Claudio, Infusino Tommaso, Sciarretta Sebastiano, Sestili Augusto, Trambaiolo Paolo, Cianfrocca Cinzia, De Marchis Elettra, Auriti Antonio, Salustri Alessandro. Transthoracic Doppler echocardiography for the assessment of left atrial appendage size and blood flow velocity: a multicentre study. J Cardiovasc Med (Hagerstown) 2008 Feb;9 (2):147–52. doi: 10.2459/JCM.0b013e3281053abd. [DOI] [PubMed] [Google Scholar]
- 49.Hwang J J, Chen J J, Lin S C, Tseng Y Z, Kuan P, Lien W P, Lin F Y, Chu S H, Hung C R, How S W. Diagnostic accuracy of transesophageal echocardiography for detecting left atrial thrombi in patients with rheumatic heart disease having undergone mitral valve operations. Am. J. Cardiol. 1993 Sep 15;72 (9):677–81. doi: 10.1016/0002-9149(93)90884-f. [DOI] [PubMed] [Google Scholar]
- 50.Olson J D, Goldenberg I F, Pedersen W, Brandt D, Kane M, Daniel J A, Nelson R R, Mooney M R, Lange H W. Exclusion of atrial thrombus by transesophageal echocardiography. J Am Soc Echocardiogr. 1992 Jan 1;5 (1):52–6. doi: 10.1016/s0894-7317(14)80103-x. [DOI] [PubMed] [Google Scholar]
- 51.Mu¨gge A, Daniel WG, Hausmann D, Godke J, Wagenbreth I, Lichtlen PR. Diagnosis of left atrial appendage thrombi by transesophageal echocardiography: clinical implications and follow-up. Am J Card Imaging. 1990;0:0–0. [Google Scholar]
- 52.Manning W J, Weintraub R M, Waksmonski C A, Haering J M, Rooney P S, Maslow A D, Johnson R G, Douglas P S. Accuracy of transesophageal echocardiography for identifying left atrial thrombi. A prospective, intraoperative study. Ann. Intern. Med. 1995 Dec 01;123 (11):817–22. doi: 10.7326/0003-4819-123-11-199512010-00001. [DOI] [PubMed] [Google Scholar]
- 53.Fatkin D, Scalia G, Jacobs N, Burstow D, Leung D, Walsh W, Feneley M. Accuracy of biplane transesophageal echocardiography in detecting left atrial thrombus. Am. J. Cardiol. 1996 Feb 01;77 (4):321–3. doi: 10.1016/s0002-9149(97)89406-4. [DOI] [PubMed] [Google Scholar]
- 54.Manning W J, Silverman D I, Keighley C S, Oettgen P, Douglas P S. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J. Am. Coll. Cardiol. 1995 May;25 (6):1354–61. doi: 10.1016/0735-1097(94)00560-D. [DOI] [PubMed] [Google Scholar]
- 55.Klein A L, Grimm R A, Murray R D, Apperson-Hansen C, Asinger R W, Black I W, Davidoff R, Erbel R, Halperin J L, Orsinelli D A, Porter T R, Stoddard M F. Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation. N. Engl. J. Med. 2001 May 10;344 (19):1411–20. doi: 10.1056/NEJM200105103441901. [DOI] [PubMed] [Google Scholar]
- 56.Stoddard M F, Dawkins P R, Prince C R, Longaker R A. Transesophageal echocardiographic guidance of cardioversion in patients with atrial fibrillation. Am. Heart J. 1995 Jun;129 (6):1204–15. doi: 10.1016/0002-8703(95)90405-0. [DOI] [PubMed] [Google Scholar]
- 57.Seidl Karlheinz, Rameken Monika, Drögemüller Axel, Vater Margit, Brandt Andreas, Schwacke Harald, Bergmeier Caroline, Zahn Ralf, Senges Jochen. Embolic events in patients with atrial fibrillation and effective anticoagulation: value of transesophageal echocardiography to guide direct-current cardioversion. Final results of the Ludwigshafen Observational Cardioversion Study. J. Am. Coll. Cardiol. 2002 May 01;39 (9):1436–42. doi: 10.1016/s0735-1097(02)01785-0. [DOI] [PubMed] [Google Scholar]
- 58.Seto T B, Taira D A, Tsevat J, Manning W J. Cost-effectiveness of transesophageal echocardiographic-guided cardioversion: a decision analytic model for patients admitted to the hospital with atrial fibrillation. J. Am. Coll. Cardiol. 1997 Jan;29 (1):122–30. doi: 10.1016/s0735-1097(96)00448-2. [DOI] [PubMed] [Google Scholar]
- 59.Manning W J, Silverman D I, Keighley C S, Oettgen P, Douglas P S. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J. Am. Coll. Cardiol. 1995 May;25 (6):1354–61. doi: 10.1016/0735-1097(94)00560-D. [DOI] [PubMed] [Google Scholar]
- 60.Seto T B, Buchholz W A, Douglas P S, Manning W J. When the body and appendage of the left atrium disagree: "Focal" atrial fibrillation-implications for atrial thrombus formation and risk of thromboembolism. J Am Soc Echocardiogr. 1999 Dec;12 (12):1097–100. [PubMed] [Google Scholar]
- 61.von der Recke Giso, Schmidt Harald, Illien Stefan, Lüderitz Berndt, Omran Heyder. Use of transesophageal contrast echocardiography for excluding left atrial appendage thrombi in patients with atrial fibrillation before cardioversion. J Am Soc Echocardiogr. 2002 Oct;15 (10 Pt 2):1256–61. doi: 10.1067/mje.2002.123961. [DOI] [PubMed] [Google Scholar]
- 62.Yamashita Eiji, Takamatsu Hiroto, Tada Hiroshi, Toide Hiroyuki, Okaniwa Hiroki, Takemura Naoki, Sasaki Takehito, Miki Yuko, Fuke Etsuko, Hayashi Tatsuya, Sakamoto Tamotsu, Nakamura Koki, Fukazawa Rie, Sato Chizuru, Goto Koji, Kaseno Kenichi, Kumagai Koji, Naito Shigeto, Hoshizaki Hiroshi, Oshima Shigeru. Transesophageal echocardiography for thrombus screening prior to left atrial catheter ablation. Circ. J. 2010 Jun;74 (6):1081–6. doi: 10.1253/circj.cj-09-1002. [DOI] [PubMed] [Google Scholar]
- 63.Wazni Oussama M, Beheiry Salwa, Fahmy Tamer, Barrett Conor, Hao Steven, Patel Dimpi, Di Biase Luigi, Martin David O, Kanj Mohamed, Arruda Mauricio, Cummings Jennifer, Schweikert Robert, Saliba Walid, Natale Andrea. Atrial fibrillation ablation in patients with therapeutic international normalized ratio: comparison of strategies of anticoagulation management in the periprocedural period. Circulation. 2007 Nov 27;116 (22):2531–4. doi: 10.1161/CIRCULATIONAHA.107.727784. [DOI] [PubMed] [Google Scholar]
- 64.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Natale Andrea, Packer Douglas, Skanes Allan, Ambrogi Federico, Biganzoli Elia. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010 Feb;3 (1):32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 65.Geller J Christoph, Brunelli Michele. Catheter ablation of atrial fibrillation without prior transoesophageal echocardiography: are we there yet? Europace. 2011 Apr;13 (4):453–4. doi: 10.1093/europace/eur030. [DOI] [PubMed] [Google Scholar]
- 66.Calvo N, Mont L, Vidal B, Nadal M, Montserrat S, Andreu D, Tamborero D, Pare C, Azqueta M, Berruezo A, Brugada J, Sitges M. Usefulness of transoesophageal echocardiography before circumferential pulmonary vein ablation in patients with atrial fibrillation: is it really mandatory? Europace. 2011 Apr;13 (4):486–91. doi: 10.1093/europace/euq456. [DOI] [PubMed] [Google Scholar]
- 67.Scherr Daniel, Dalal Darshan, Chilukuri Karuna, Dong Jun, Spragg David, Henrikson Charles A, Nazarian Saman, Cheng Alan, Berger Ronald D, Abraham Theodore P, Calkins Hugh, Marine Joseph E. Incidence and predictors of left atrial thrombus prior to catheter ablation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2009 Apr;20 (4):379–84. doi: 10.1111/j.1540-8167.2008.01336.x. [DOI] [PubMed] [Google Scholar]
- 68.Wallace Thomas W, Atwater Brett D, Daubert James P, Voora Deepak, Crowley Anna Lisa, Bahnson Tristram D, Hranitzky Patrick M. Prevalence and clinical characteristics associated with left atrial appendage thrombus in fully anticoagulated patients undergoing catheter-directed atrial fibrillation ablation. J. Cardiovasc. Electrophysiol. 2010 Aug 01;21 (8):849–52. doi: 10.1111/j.1540-8167.2010.01729.x. [DOI] [PubMed] [Google Scholar]
- 69.Stavrakis Stavros, Madden George W, Stoner Julie A, Sivaram Chittur A. Transesophageal echocardiography for the diagnosis of pulmonary vein stenosis after catheter ablation of atrial fibrillation: a systematic review. Echocardiography. 2010 Oct;27 (9):1141–6. doi: 10.1111/j.1540-8175.2010.01250.x. [DOI] [PubMed] [Google Scholar]
- 70.Silvestry Frank E, Kerber Richard E, Brook Michael M, Carroll John D, Eberman Karen M, Goldstein Steven A, Herrmann Howard C, Homma Shunichi, Mehran Roxana, Packer Douglas L, Parisi Alfred F, Pulerwitz Todd, Seward James Bernard, Tsang Teresa S M, Wood Mark A. Echocardiography-guided interventions. J Am Soc Echocardiogr. 2009 Mar;22 (3):213–31. doi: 10.1016/j.echo.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 71.Faletra Francesco F, Nucifora Gaetano, Ho Siew Yen. Imaging the atrial septum using real-time three-dimensional transesophageal echocardiography: technical tips, normal anatomy, and its role in transseptal puncture. J Am Soc Echocardiogr. 2011 Jun;24 (6):593–9. doi: 10.1016/j.echo.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 72.Wang Tian, Wang Mei, Fung Jeffrey W H, Yip Gabriel W K, Zhang Yan, Ho Pearl P Y, Tse Deco M K, Yu Cheuk Man, Sanderson John E. Atrial strain rate echocardiography can predict success or failure of cardioversion for atrial fibrillation: a combined transthoracic tissue Doppler and transoesophageal imaging study. Int. J. Cardiol. 2007 Jan 08;114 (2):202–9. doi: 10.1016/j.ijcard.2006.01.051. [DOI] [PubMed] [Google Scholar]
- 73.Schneider Carsten, Malisius Rainer, Krause Korff, Lampe Friedrun, Bahlmann Edda, Boczor Sigrid, Antz Matthias, Ernst Sabine, Kuck Karl-Heinz. Strain rate imaging for functional quantification of the left atrium: atrial deformation predicts the maintenance of sinus rhythm after catheter ablation of atrial fibrillation. Eur. Heart J. 2008 Jun;29 (11):1397–409. doi: 10.1093/eurheartj/ehn168. [DOI] [PubMed] [Google Scholar]
- 74.Mirza Mahek, Caracciolo Giuseppe, Khan Uzma, Mori Naoyo, Saha Samir K, Srivathsan Komandoor, Altemose Gregory, Scott Luis, Sengupta Partho, Jahangir Arshad. Left atrial reservoir function predicts atrial fibrillation recurrence after catheter ablation: a two-dimensional speckle strain study. J Interv Card Electrophysiol. 2011 Sep;31 (3):197–206. doi: 10.1007/s10840-011-9560-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hammerstingl Christoph, Schwekendiek Marieke, Momcilovic Diana, Schueler Robert, Sinning Jan-Malte, Schrickel Jan W, Mittmann-Braun Erica, Nickenig Georg, Lickfett Lars. Left atrial deformation imaging with ultrasound based two-dimensional speckle-tracking predicts the rate of recurrence of paroxysmal and persistent atrial fibrillation after successful ablation procedures. J. Cardiovasc. Electrophysiol. 2012 Mar;23 (3):247–55. doi: 10.1111/j.1540-8167.2011.02177.x. [DOI] [PubMed] [Google Scholar]
- 76.Tops Laurens F, Delgado Victoria, Bertini Matteo, Marsan Nina Ajmone, Den Uijl Dennis W, Trines Serge A I P, Zeppenfeld Katja, Holman Eduard, Schalij Martin J, Bax Jeroen J. Left atrial strain predicts reverse remodeling after catheter ablation for atrial fibrillation. J. Am. Coll. Cardiol. 2011 Jan 18;57 (3):324–31. doi: 10.1016/j.jacc.2010.05.063. [DOI] [PubMed] [Google Scholar]
- 77.Thomas L, McKay T, Byth K, Marwick T H. Abnormalities of left atrial function after cardioversion: an atrial strain rate study. Heart. 2007 Jan;93 (1):89–95. doi: 10.1136/hrt.2006.088609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hart R G, Benavente O, McBride R, Pearce L A. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann. Intern. Med. 1999 Oct 05;131 (7):492–501. doi: 10.7326/0003-4819-131-7-199910050-00003. [DOI] [PubMed] [Google Scholar]
- 79.Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch. Intern. Med. 1994 Jul 11;154 (13):1449–57. [PubMed] [Google Scholar]
- 80.Fuster Valentin, Rydén Lars E, Cannom David S, Crijns Harry J, Curtis Anne B, Ellenbogen Kenneth A, Halperin Jonathan L, Le Heuzey Jean-Yves, Kay G Neal, Lowe James E, Olsson S Bertil, Prystowsky Eric N, Tamargo Juan Luis, Wann Samuel, Smith Sidney C, Jacobs Alice K, Adams Cynthia D, Anderson Jeffery L, Antman Elliott M, Hunt Sharon Ann, Nishimura Rick, Ornato Joseph P, Page Richard L, Riegel Barbara, Priori Silvia G, Blanc Jean-Jacques, Budaj Andrzej, Camm A John, Dean Veronica, Deckers Jaap W, Despres Catherine, Dickstein Kenneth, Lekakis John, McGregor Keith, Metra Marco, Morais Joao, Osterspey Ady, Zamorano José Luis. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). J. Am. Coll. Cardiol. 2006 Aug 15;48 (4):854–906. doi: 10.1016/j.jacc.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 81.Blackshear J L, Pearce L A, Asinger R W, Dittrich H C, Goldman M E, Zabalgoitia M, Rothbart R M, Halperin J L. Mitral regurgitation associated with reduced thromboembolic events in high-risk patients with nonrheumatic atrial fibrillation. Stroke Prevention in Atrial Fibrillation Investigators. Am. J. Cardiol. 1993 Oct 01;72 (11):840–3. doi: 10.1016/0002-9149(93)91079-w. [DOI] [PubMed] [Google Scholar]
- 82.Shih Jhih-Yuan, Tsai Wei-Chuan, Huang Yao-Yi, Liu Yen-Wen, Lin Chih-Chan, Huang Yu-Shan, Tsai Liang-Miin, Lin Li-Jen. Association of decreased left atrial strain and strain rate with stroke in chronic atrial fibrillation. J Am Soc Echocardiogr. 2011 May;24 (5):513–9. doi: 10.1016/j.echo.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 83.Saha Samir K, Anderson Paula L, Caracciolo Giuseppe, Kiotsekoglou Anatoli, Wilansky Susan, Govind Satish, Mori Naoyo, Sengupta Partho P. Global left atrial strain correlates with CHADS2 risk score in patients with atrial fibrillation. J Am Soc Echocardiogr. 2011 May;24 (5):506–12. doi: 10.1016/j.echo.2011.02.012. [DOI] [PubMed] [Google Scholar]


