Abstract
Management of atrial fibrillation in the elderly presents unique challenges, including deciding upon the best treatment strategy: rate control versus rhythm control. The decision to pursue one treatment strategy over another is based on understanding the underlying disorder: symptomatology from atrial fibrillation itself versus symptoms due to a rapid ventricular response from atrial fibrillation. The ablation strategies for the treatment of atrial fibrillation include atrioventricular junction ablation and pulmonary vein isolation. This review discusses the data on ablation of atrial fibrillation in the elderly, with an emphasis on issues regarding safety and efficacy in this population.
Introduction
Atrial fibrillation is expected to affect an estimated 12-15 million people in the United States by the year 2050.[1,2] This increasing incidence and prevalence is greatest amongst the elderly (patients greater than 70 years of age), with nearly 8% of those older than 70 carrying a diagnosis of atrial fibrillation.[3-6] Three out of four patients with atrial fibrillation are between the ages of 65 and 85.[7,8] Age carries particular risk amongst patients with atrial fibrillation, as evidenced by the increased stroke risk in patients greater than 75 years of age.[4,9-10] Management of atrial fibrillation in the elderly presents unique challenges, including issues related to bleeding, general debility, a greater incidence of underlying conduction system disease, and structural heart disease.
Decision making regarding the management of atrial fibrillation in the elderly includes issues related to anticoagulation and whether to focus on a rate versus rhythm control approach. Perhaps the most important question that needs to be answered in this patient population is whether they are symptomatic from atrial fibrillation as this may be the most important factor in favor of pursuing a rhythm control strategy. Symptomatology from atrial fibrillation itself needs to be differentiated from symptoms due to a rapid ventricular response associated with atrial fibrillation as the latter would entail an aggressive rate control strategy, which may include atrioventricular junction ablation and pacemaker implantation, while the former would entail an approach geared more towards rhythm control. The risk of tachycardia-bradycardia syndrome and sick sinus syndrome may also be more common in elderly patients and favor a rhythm control approach as a more desirable option in many patients.[11,12] The options for rhythm control include antiarrhythmic medications and pulmonary vein isolation. There is a lack of prospective data on the relative benefits of these different rhythm control strategies in the elderly population.[13-16] Antiarrhythmic drugs can be difficult to manage due to unpredictable metabolism in elderly patients and intolerance of side effects.[17] Thus, pulmonary vein isolation and ablation of non-pulmonary vein foci is an important alternative in the management of atrial fibrillation in the elderly.
Pathophysiology
Atrial fibrillation is thought to be triggered by foci of abnormal conduction that lead to fibrillatory conduction in the atria. One of the mechanisms underlying the pathogenesis of atrial fibrillation is thought to be atrial remodeling, whether due to chronic stress from factors such as high atrial pressures from diastolic or systolic failure or from loss of atrial muscle mass resulting in greater dispersion of atrial refractoriness.[18-20] Multiple studies have shown a role for fibrosis in the pathogenesis of atrial fibrillation.[19] In the elderly, multiple factors including diastolic dysfunction, hypertension, and age-related loss of muscle mass may lead to increased left atrial stretch and fibrosis with a greater predilection towards developing atrial fibrillation.[16] Furthermore, sinus node dysfunction and reduction of normal conduction velocities throughout the atria may occur more commonly in elderly patients, resulting in a greater likelihood for secondary foci to take control and degenerate into atrial fibrillation.
Epidemiology
The importance of recognition of atrial fibrillation in the elderly lies in both its association with increased risk of morbidity and mortality, and in its leading to significant healthcare costs related to recurrent hospitalizations and doctor’s visits for the primary arrhythmia and its secondary effects.[21,22] Atrial fibrillation has been associated with an increased risk of stroke, heart failure, and overall mortality, particularly in elderly patients. [2,22] Furthermore, due to the risk of stroke, employment of anticoagulation strategies may increase bleeding risk, which may be higher in elderly patients above the age of 80, and is also associated with the need for frequent monitoring.[23-25] Patients may present with symptoms related to rapid rates but also with heart failure exacerbation, stroke, or bleeding from concomitant anticoagulation use. Thus, close management of atrial fibrillation is necessary, but may also prove a significant challenge.
Ablation Strategies
Several ablation strategies exist for the treatment of atrial fibrillation, but may be separated grossly into rate control via atrioventricular junction ablation or rhythm control via ablation of focal triggers of atrial fibrillation.[26] The latter strategy involves isolation of the pulmonary veins by creating effective areas of electrophysiological silence surrounding the ostia of the pulmonary veins, thereby eliminating transmission of signals from these venous foci.[26] However, several non-pulmonary vein foci may also exist and may necessitate additional ablation at other sites. Atrioventricular junction ablation is definitive in its control of patients’ rates but results in 100% pacemaker dependence. This may cause issues related to the long-term need for pacemaker follow-up and care, the risk of heart failure related to chronic right ventricular pacing, and the limitations in rate-responsiveness algorithms that may not always offer the level of heart rate augmentation to a given set of external stimuli that would be seen in a natural state. Studies have suggested, however, that atrioventricular junction ablation to achieve rate control is both a safe and well tolerated option in many patients.[27-29] Atrioventricular junction ablation may be a reasonable option in elderly patients in whom rate control cannot be achieved with medical therapy and in whom the duration of chronic right ventricular pacing may not be sufficient enough to cause significant cardiomyopathy.
In contrast, pulmonary vein isolation focuses on maintenance of sinus rhythm. While effective in up to 70% of all-comers with paroxysmal atrial fibrillation, the efficacy of this strategy in an elderly cohort has not been as well established.[30,31] Ablation aimed at maintenance of sinus rhythm may offer the benefit of maintaining atrio-ventricular synchrony while simultaneously limiting the need for potentially caustic antiarrhythmic or rate control agents that may often be poorly tolerated in elderly patients. Furthermore, in the absence of underlying sinus or atrioventricular nodal disease, patients will generally not need additional device therapy that may lead to additional long-term risks. However, many patients may require multiple ablation attempts to achieve long-term maintenance of sinus rhythm.[26]
Efficacy of Pulmonary Vein Isolation in the Elderly
As mentioned previously, the first step in the management of atrial fibrillation in the elderly is deciding whether a rate or rhythm control strategy is appropriate. While prior trials have suggested that rate and rhythm control strategies have equivalent survival, post hoc analyses have suggested that successful maintenance of sinus rhythm was an independent predictor of improved survival. Furthermore, comparison between rate and rhythm control strategies have always involved use of antiarrhythmic drugs, which often have poor side effect profiles and may be proarrhythmic in some patients. There are no published prospective trials to date comparing ablation-based rhythm control against a rate control strategy. However, it is clear that restoring and maintaining sinus rhythm in certain patients may confer both a morbidity and mortality benefit.[33] Thus, the decision to employ pulmonary vein isolation or trigger-focused ablation as a management strategy in elderly patients needs to take into account the goals of rhythm control and whether it may be as efficacious as in younger patients who comprise most of the cohorts studied to date.
Several studies have recently studied the efficacy and safety of pulmonary vein isolation in elderly patients, one of which was a prospective, nonrandomized trial comparing atrioventricular nodal ablation with pulmonary vein isolation.[15,34-40] Table 1 summarizes the data on atrial fibrillation ablation in the elderly including published trials to date, patient characteristics, and outcomes. Four of these studies focused on the efficacy and safety of pulmonary vein isolation in different age groups and the remaining studies focused on the relative overall safety of ablation in elderly patients. All studies involved segmental or circumferential pulmonary vein isolation with the addition of ablation of non-pulmonary vein triggers or linear ablation in the left atrium in some studies. The overall success rate across all studies, which included use of anti-arrhythmic drugs, was 80% and not age-dependent.Table 1
Table 1. Baseline Clinical Characteristics.
LV-EF: left ventricular ejection fraction AF: atrial fibrillation, CAD: coronary artery disease, DCM: dilatative cardiomiopathy, VHD: Valvular Heart Disease
| Study | Number | Quinidine | Propafenone | p-value | |
|---|---|---|---|---|---|
| Bhargava, et al[34] | 103 | >60 | 82% (vs 85%) | 6.8% (vs 2.8%) | AF Ablation in <50 years old |
| Hsieh, et al[35] | 37 | >65 | 81% (vs 100%)* | 0% (vs 0%) | AV nodal ablation + pacemaker |
| Zado, et al[36] | 32 | >75 | 87% (vs 89%) | 2.9% (vs 1.6%) | AF Ablation in <65 years old, |
| Corrado, et al[37] | 174 | >75 | 93% | 1.0% | N/A |
| Nademanee, et al[40] | 635 | >65 | 81% | 3.1% | N/A |
| Traub, et al[15] | 15 | >70 | 60% (vs 80%) | 6.7% (vs 4.4%) | AF Ablation in <70 years old |
| Kusumoto, et al[41] | 61 | >75 | 82% (vs 96%) | 0% (vs 1.1%) | AF Ablation in <65 years old |
| Bunch, et al[42] | 35 | >80 | 78% (vs 75%) | 5.7% (vs 3.1%) | AF Ablation in <80 years old |
| Hsu, et al[38] | 22 | >65 | 68% (vs 75% vs 71%) | 9.1% (vs 2% vs 0%) | AF Ablation in 45-65 years, <45 years |
| Oral, et al[39] | 24 | >70 | 80% | 12.5%* | N/A |
One of the key points of all the studies is that, despite the presumption that there may be greater amounts of fibrosis and atrial remodeling in elderly patients that limit efficacy of pulmonary vein isolation, there was no significant difference in success rates when compared with younger patients. [Table 1] However, most of these studies included patients with paroxysmal atrial fibrillation. One study did focus on patients presenting with permanent atrial fibrillation and did demonstrate an age-independent success rate of about 70%.[38]
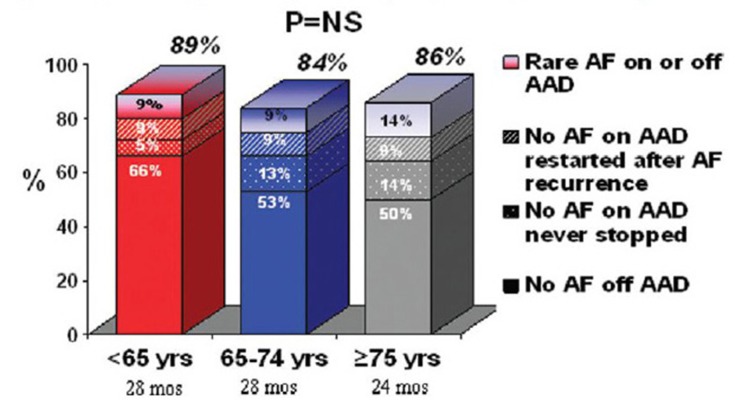
One limitation of the available data is that all of the studies, with the exception of the study by Corrado et al, have involved a single center with a high degree of experience. Also, decision making in retrospective analyses may be impacted by differences in choices related in how to achieve rhythm control. For example, in the study by Zado et al, patients over 75 years of age tended to undergo repeat ablation less often and more often remained on antiarrhythmic drugs than those less than 65 years of age despite similar overall success rates.([Figure 1]) Continued use of antiarrhythmic medications was also seen in studies by Traub et al and Kusumoto et al.[25,4] In the latter study, the similarity in the success of a rhythm control strategy in elderly patients compared to younger patients appeared due to the continued use of antiarrhythmic drugs rather than to the ablation strategy alone.
Figure 1. Single center experience for patients completing at least 1 year of follow-up after ablationto.
While no comparisons were made with younger age groups, the one multi-center study reported by Corrado et al showed similar efficacy in achieving sinus rhythm (82%) to that seen in the other single center trials.[37] Thus, allowing for the limited numbers of patients included across trials and differences in techniques between trials, the efficacy of atrial fibrillation ablation in elderly patients appears to be similar to that of younger patients.
Safety of Pulmonary Vein Isolation in the Elderly
Another area of consideration when referring elderly patients for atrial fibrillation ablation is the safety of the procedure. Table 1 Elderly patients tend to have higher degrees of baseline stroke, hypertension, and structural heart disease than younger patients and thus, may be more prone to complications. One risk during pulmonary vein isolation is incidental cerebrovascular accident from coagulum formation and embolization during the procedure. Several older studies, including one multivariate analysis, have suggested that there are more major adverse clinical events in older patients, though these results have not necessarily borne out in more recent studies, which may be attributed to advances in catheter technology and more aggressive anticoagulation.[15] Bunch et al, however, did demonstrate a longer duration of hospital stay in those over 80 year of age after ablation.The overall risk between studies of periprocedural cerebrovascular accident, cardiac tamponade or pulmonary vein stenosis ranged from 0 to 12% between studies.
One limitation in assessing safety of pulmonary vein isolation lies in the definition of cerebrovascular accident. Small incidental strokes may not be clinically evident, as is often seen in cardiac catheterization patients when delineating between clinically significant stroke with grossly apparent clinical features and silent cerebrovascular accidents that may be seen on direct imaging but otherwise not clinically apparent. The long-term risk of these issues in terms of cognitive functioning, however, is unclear and would require longer term follow-up of these patients. Preexisting cerebral atherosclerosis has been associated with increased risk of periprocedural major complications, though this may be attributed to a higher incidence of comorbidities such as hypertension, structural heart disease, and prior stroke with already diminished baseline functioning in these patients.[32] Lastly, since all of the studies evaluating safety of ablation have been nonrandomized, the elderly patients who underwent ablation may have been a select population that is not representative of the general elderly population with atrial fibrillation.
Thus, the safety of pulmonary vein isolation, while not clearly different from younger patients, needs to be considered in the context of the limitations in existing studies and the presumed higher incidence of pre-existing conditions in elderly patients.
Atrioventricular Nodal Ablation Versus Pulmonary Vein Isolation
In certain patients, rate control of atrial fibrillation may be challenging and difficult to achieve with medications alone. Atrioventricular nodal ablation and pacemaker implantation may be used to achieve rate control in this population of patients. Several studies have demonstrated efficacy of this approach as being similar to that of antiarrhythmic drug use in terms of risk of sudden death or overall mortality. Furthermore, these patients tend to have survival rates similar to the general population.[27-29]
There has been one nonrandomized study directly comparing atrioventricular nodal ablation against pulmonary vein isolation in pharmacologically refractory elderly patients. While 100% of those patients with atrioventricular nodal ablation had control of their rates in atrial fibrillation, only 81% of those undergoing pulmonary vein isolation had rhythm or adequate rate control. However, 69% of patients undergoing atrioventricular nodal ablation still had persistent atrial fibrillation and 53% had congestive heart failure compared with 8% and 24% of patients undergoing pulmonary vein isolation respectively. In this study, patients undergoing atrioventricular nodal ablation and permanent pacing developed a higher incidence of heart failure, higher NYHA class, and a decreased left ventricular ejection fraction compared to the patients undergoing catheter ablation.
It is difficult to use the persistence of atrial fibrillation as an endpoint after atrioventricular nodal ablation given that this strategy involves primarily rate rather than rhythm control. However, the worsening of heart failure symptoms and decrease in ejection fraction are important considerations. There is some evidence that chronic right ventricular pacing may compromise cardiac function over time.However, another study that was not specific to elderly patients showed that atrioventricular nodal ablation plus biventricular pacemaker placement in patients with NYHA class II ablationto III symptoms tended to not see as great an improvement in heart failure symptoms as those who underwent pulmonary vein isolation (average age of patients = 60 + 8 years). Overall, these data suggest a rhythm control strategy in these patients may help overall functional status. However, the studies were nonrandomized, and programming of the pacemaker function was non-physiologic (all devices were programmed to VVI even in patients who later remained in sinus rhythm).
Thus, while several studies have demonstrated the safety and efficacy of atrioventricular nodal ablation with pacemaker implantation in managing ventricular rates and associated symptoms in atrial fibrillation, studies on effects on heart failure symptoms and further comparison with outcomes with pulmonary vein isolation are needed. It is still unclear if an atrioventricular nodal ablation approach is equivalent to a rhythm-control ablative strategy in terms of long-term morbidity and mortality.
Anticoagulation Management After Ablation Conversion rate
The risk of stroke in atrial fibrillation is generally attributed to clot formation in the left atrium due to stagnation of blood in the left atrial appendage. Age greater than 75 years is one major component of the CHADS2 risk stratification used to determine the need for anticoagulation to reduce stroke risk atrial fibrillation. Elderly patients have a greater risk of stroke than younger patients with atrial fibrillation, but several studies have highlighted the greater bleeding risk with warfarin in this cohort.[23,24] Two prior studies have suggested that if sinus rhythm is successfully maintained for up to 3-6 months after pulmonary vein isolation, anticoagulation may be discontinued.[50] In the study by Corrado et al, warfarin was discontinued in 96% of elderly patients after atrial fibrillation ablation after 5-6 months in sinus rhythm without any incident strokes, despite a CHADS2 score > 2 in 65% of these patients. Current practices, however, tend to vary with regards to the decision to discontinue anticoagulation, especially given the risk.[51] Ambulatory monitoring is often used to confirm sinus rhythm and the lack of recurrent, asymptomatic atrial fibrillation.[13,40] Studies that have demonstrated the safety of this approach in determining the discontinuation of anticoagulation have involved small numbers of patients and have not been randomized. Thus, the safety of anticoagulation discontinuation after presumed successful pulmonary vein isolation, particularly in elderly patients who are often at greater risk of stroke, is unclear and at this time this decision must be left in the hands of the electrophysiologist performing the procedure after taking into account the individual risk profile of each patient.
Conclusions
Several studies have suggested similar safety and efficacy of atrial fibrillation ablation in elderly patients when compared with younger patients. However, most of these studies have been single center trials with relatively small patient numbers. The potential benefits of achieving rhythm control in elderly patients relates to the maintenance of sinus rhythm, improvement in symptoms related to atrial fibrillation, and the potential for being able to discontinue anticoagulation. Several studies have demonstrated maintenance of sinus rhythm as a major determinant of improvement in outcomes and quality of life in patients with atrial fibrillation.[33,52] Recent data also suggests the benefit in terms of quality of life and cost-effectiveness of pulmonary vein isolation over pharmacologic management strategies. Furthermore, given the potential for bleeding in Reviewelderly patients, the possibility that anticoagulation may be discontinued should be considered.
Atrioventricular nodal ablation and pacemaker implantation is another strategy that may be safe in select patients. However, close attention to the type of pacemaker (biventricular versus single versus dual chamber), the programming, and the patient’s functional status is likely needed to select those who will benefit most. Furthermore, there is limited data comparing the relative efficacy of this approach, in which patients may remain in atrial fibrillation but with better controlled ventricular rates, with that of pulmonary vein isolation trigger-guided ablation, in which maintenance of sinus rhythm is the principal goal.
To date, published data support that ablative strategies are relatively safe and efficacious in elderly patients. Future randomized prospective trials are needed to further assess the safety and efficacy of pulmonary vein isolation in elderly patients. Elderly subsets of the CABANA trial may offer some insights into the relative efficacy of pulmonary vein isolation when compared with antiarrhythmic drugs in managing patients with atrial fibrillation. Further studies are needed to better evaluate the relative benefits and risks of different approaches aimed at rate versus rhythm control in the elderly population and specifically, the role and timing of ablation strategies.
References
- 1.Feinberg W M, Blackshear J L, Laupacis A, Kronmal R, Hart R G. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch. Intern. Med. 1995 Mar 13;155 (5):469–73. [PubMed] [Google Scholar]
- 2.Aronow Wilbert S. Management of the older person with atrial fibrillation. J. Gerontol. A Biol. Sci. Med. Sci. 2002 Jun;57 (6):M352–63. doi: 10.1093/gerona/57.6.m352. [DOI] [PubMed] [Google Scholar]
- 3.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 4.Kamath Sridar, Lip Gregory Y H. Atrial fibrillation in the elderly: anticoagulation strategies and indications in the very elderly. Am J Geriatr Cardiol. 2002 Nov 6;11 (6):357–62. doi: 10.1111/j.1076-7460.2002.00070.x. [DOI] [PubMed] [Google Scholar]
- 5.Lip Gregory Y H, Kakar Puneet, Watson Timothy. Atrial fibrillation--the growing epidemic. Heart. 2007 May;93 (5):542–3. doi: 10.1136/hrt.2006.110791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter P, Seward James B, Tsang Teresa S M. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006 Jul 11;114 (2):119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 7.Kannel W B, Abbott R D, Savage D D, McNamara P M. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N. Engl. J. Med. 1982 Apr 29;306 (17):1018–22. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 8.Stewart Simon, Hart Carole L, Hole David J, McMurray John J V. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am. J. Med. 2002 Oct 01;113 (5):359–64. doi: 10.1016/s0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 9.Smith C L, Hammond G L. Ontogeny of corticosteroid-binding globulin biosynthesis in the rat. Endocrinology. 1991 Feb;128 (2):983–8. doi: 10.1210/endo-128-2-983. [DOI] [PubMed] [Google Scholar]
- 10.Wolf P A, Dawber T R, Thomas H E, Kannel W B. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology. 1978 Oct;28 (10):973–7. doi: 10.1212/wnl.28.10.973. [DOI] [PubMed] [Google Scholar]
- 11.C Berry, A Rae, J Taylor, AJ Brady. Atrial fibrillation in the elderly . Br J Cardiol. 2003;10:373–378. [Google Scholar]
- 12.Fang Margaret C, Chen Jane, Rich Michael W. Atrial fibrillation in the elderly. Am. J. Med. 2007 Jun;120 (6):481–7. doi: 10.1016/j.amjmed.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 13.Curtis Anne B, Rich Michael W. Atrial fibrillation in the elderly: mechanisms and management. Heart Rhythm. 2007 Dec;4 (12):1577–9. doi: 10.1016/j.hrthm.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 14.Williams Eric S, Hall Burr, Traub Darren, Bahnson Tristram, Hranitzky Patrick, Zareba Wojciech, Daubert James P. Catheter ablation of atrial fibrillation in the elderly. Curr. Opin. Cardiol. 2011 Jan;26 (1):25–9. doi: 10.1097/HCO.0b013e3283413978. [DOI] [PubMed] [Google Scholar]
- 15.Traub Darren, Daubert James P, McNitt Scott, Zareba Wojciech, Hall Burr. Catheter ablation of atrial fibrillation in the elderly: where do we stand? Cardiol J. 2009;16 (2):113–20. [PubMed] [Google Scholar]
- 16.Yamada Takumi, Kay G Neal. Catheter ablation of atrial fibrillation in the elderly. Pacing Clin Electrophysiol. 2009 Aug;32 (8):1085–91. doi: 10.1111/j.1540-8159.2009.02442.x. [DOI] [PubMed] [Google Scholar]
- 17.Dayer Mark, Hardman Suzanna M C. Special problems with antiarrhythmic drugs in the elderly: safety, tolerability, and efficacy. Am J Geriatr Cardiol. 2002 Nov 6;11 (6):370–5. doi: 10.1111/j.1076-7460.2002.0069.x. [DOI] [PubMed] [Google Scholar]
- 18.Tan Alex Y, Zimetbaum Peter. Atrial Fibrillation and Atrial Fibrosis. J. Cardiovasc. Pharmacol. 2010 Dec 04; () doi: 10.1097/FJC.0b013e3182073c78. [DOI] [PubMed] [Google Scholar]
- 19.Burstein Brett, Nattel Stanley. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J. Am. Coll. Cardiol. 2008 Feb 26;51 (8):802–9. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 20.Nattel Stanley, Shiroshita-Takeshita Akiko, Cardin Sophie, Pelletier Patricia. Mechanisms of atrial remodeling and clinical relevance. Curr. Opin. Cardiol. 2005 Jan;20 (1):21–5. [PubMed] [Google Scholar]
- 21.Fuster Valentin, Rydén Lars E, Cannom David S, Crijns Harry J, Curtis Anne B, Ellenbogen Kenneth A, Halperin Jonathan L, Le Heuzey Jean-Yves, Kay G Neal, Lowe James E, Olsson S Bertil, Prystowsky Eric N, Tamargo Juan Luis, Wann Samuel, Smith Sidney C, Jacobs Alice K, Adams Cynthia D, Anderson Jeffery L, Antman Elliott M, Halperin Jonathan L, Hunt Sharon Ann, Nishimura Rick, Ornato Joseph P, Page Richard L, Riegel Barbara, Priori Silvia G, Blanc Jean-Jacques, Budaj Andrzej, Camm A John, Dean Veronica, Deckers Jaap W, Despres Catherine, Dickstein Kenneth, Lekakis John, McGregor Keith, Metra Marco, Morais Joao, Osterspey Ady, Tamargo Juan Luis, Zamorano José Luis. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006 Aug 15;114 (7):e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 22.Hurwitz Jodie Linda. Atrial fibrillation treatment in the elderly: are we getting closer to an answer? J. Cardiovasc. Electrophysiol. 2008 Aug;19 (8):812–4. doi: 10.1111/j.1540-8167.2008.01144.x. [DOI] [PubMed] [Google Scholar]
- 23.Copland M, Walker I D, Tait R C. Oral anticoagulation and hemorrhagic complications in an elderly population with atrial fibrillation. Arch. Intern. Med. 2001 Sep 24;161 (17):2125–8. doi: 10.1001/archinte.161.17.2125. [DOI] [PubMed] [Google Scholar]
- 24.Fihn S D, Callahan C M, Martin D C, McDonell M B, Henikoff J G, White R H. The risk for and severity of bleeding complications in elderly patients treated with warfarin. The National Consortium of Anticoagulation Clinics. Ann. Intern. Med. 1996 Jun 01;124 (11):970–9. doi: 10.7326/0003-4819-124-11-199606010-00004. [DOI] [PubMed] [Google Scholar]
- 25.Fang Margaret C. Antithrombotic therapy for the treatment of atrial fibrillation in the elderly. J Interv Card Electrophysiol. 2009 Jun;25 (1):19–23. doi: 10.1007/s10840-008-9334-y. [DOI] [PubMed] [Google Scholar]
- 26.Crandall Mark A, Bradley David J, Packer Douglas L, Asirvatham Samuel J. Contemporary management of atrial fibrillation: update on anticoagulation and invasive management strategies. Mayo Clin. Proc. 2009 Jul;84 (7):643–62. doi: 10.1016/S0025-6196(11)60754-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kay G N, Ellenbogen K A, Giudici M, Redfield M M, Jenkins L S, Mianulli M, Wilkoff B. The Ablate and Pace Trial: a prospective study of catheter ablation of the AV conduction system and permanent pacemaker implantation for treatment of atrial fibrillation. APT Investigators. J Interv Card Electrophysiol. 1998 Jun;2 (2):121–35. doi: 10.1023/a:1009795330454. [DOI] [PubMed] [Google Scholar]
- 28.Wood M A, Brown-Mahoney C, Kay G N, Ellenbogen K A. Clinical outcomes after ablation and pacing therapy for atrial fibrillation : a meta-analysis. Circulation. 2000 Mar 14;101 (10):1138–44. doi: 10.1161/01.cir.101.10.1138. [DOI] [PubMed] [Google Scholar]
- 29.Ozcan C, Jahangir A, Friedman P A, Patel P J, Munger T M, Rea R F, Lloyd M A, Packer D L, Hodge D O, Gersh B J, Hammill S C, Shen W K. Long-term survival after ablation of the atrioventricular node and implantation of a permanent pacemaker in patients with atrial fibrillation. N. Engl. J. Med. 2001 Apr 05;344 (14):1043–51. doi: 10.1056/NEJM200104053441403. [DOI] [PubMed] [Google Scholar]
- 30.Pappone Carlo, Augello Giuseppe, Sala Simone, Gugliotta Filippo, Vicedomini Gabriele, Gulletta Simone, Paglino Gabriele, Mazzone Patrizio, Sora Nicoleta, Greiss Isabelle, Santagostino Andreina, LiVolsi Laura, Pappone Nicola, Radinovic Andrea, Manguso Francesco, Santinelli Vincenzo. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF Study. J. Am. Coll. Cardiol. 2006 Dec 05;48 (11):2340–7. doi: 10.1016/j.jacc.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 31.Wilber David J, Pappone Carlo, Neuzil Petr, De Paola Angelo, Marchlinski Frank, Natale Andrea, Macle Laurent, Daoud Emile G, Calkins Hugh, Hall Burr, Reddy Vivek, Augello Giuseppe, Reynolds Matthew R, Vinekar Chandan, Liu Christine Y, Berry Scott M, Berry Donald A. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010 Jan 27;303 (4):333–40. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 32.Wyse D G, Waldo A L, DiMarco J P, Domanski M J, Rosenberg Y, Schron E B, Kellen J C, Greene H L, Mickel M C, Dalquist J E, Corley S D. A comparison of rate control and rhythm control in patients with atrial fibrillation. N. Engl. J. Med. 2002 Dec 05;347 (23):1825–33. doi: 10.1056/NEJMoa021328. [DOI] [PubMed] [Google Scholar]
- 33.Corley Scott D, Epstein Andrew E, DiMarco John P, Domanski Michael J, Geller Nancy, Greene H Leon, Josephson Richard A, Kellen Joyce C, Klein Richard C, Krahn Andrew D, Mickel Mary, Mitchell L Brent, Nelson Joy Dalquist, Rosenberg Yves, Schron Eleanor, Shemanski Lynn, Waldo Albert L, Wyse D George. Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation. 2004 Mar 30;109 (12):1509–13. doi: 10.1161/01.CIR.0000121736.16643.11. [DOI] [PubMed] [Google Scholar]
- 34.Bhargava Mandeep, Marrouche Nassir F, Martin David O, Schweikert Robert A, Saliba Walid, Saad Eduardo B, Bash Dianna, Williams-Andrews Michelle, Rossillo Antonio, Erciyes Demet, Khaykin Yaariv, Burkhardt J David, Joseph George, Tchou Patrick J, Natale Andrea. Impact of age on the outcome of pulmonary vein isolation for atrial fibrillation using circular mapping technique and cooled-tip ablation catheter:. J. Cardiovasc. Electrophysiol. 2004 Jan;15 (1):8–13. doi: 10.1046/j.1540-8167.2004.03266.x. [DOI] [PubMed] [Google Scholar]
- 35.Hsieh Ming-Hsiung, Tai Ching-Tai, Lee Shih-Huang, Tsao Huan-Ming, Lin Yung-Kuo, Huang Jin-Long, Chan Paul, Chen Yi-Jen, Kuo Jen-Yuan, Tuan Ta-Chuan, Hsu Tsui-Lieh, Kong Chi-Woon, Chang Shih-Lin, Chen Shih-Ann. Catheter ablation of atrial fibrillation versus atrioventricular junction ablation plus pacing therapy for elderly patients with medically refractory paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2005 May;16 (5):457–61. doi: 10.1111/j.1540-8167.2005.40632.x. [DOI] [PubMed] [Google Scholar]
- 36.Zado Erica, Callans David J, Riley Michael, Hutchinson Mathew, Garcia Fermin, Bala Rupa, Lin David, Cooper Joshua, Verdino Ralph, Russo Andrea M, Dixit Sanjay, Gerstenfeld Edward, Marchlinski Francis E. Long-term clinical efficacy and risk of catheter ablation for atrial fibrillation in the elderly. J. Cardiovasc. Electrophysiol. 2008 Jun;19 (6):621–6. doi: 10.1111/j.1540-8167.2008.01183.x. [DOI] [PubMed] [Google Scholar]
- 37.Corrado Andrea, Patel Dimpi, Riedlbauchova Lucie, Fahmy Tamer S, Themistoclakis Sakis, Bonso Aldo, Rossillo Antonio, Hao Steven, Schweikert Robert A, Cummings Jennifer E, Bhargava Mandeep, Burkhardt David, Saliba Walid, Raviele Antonio, Natale Andrea. Efficacy, safety, and outcome of atrial fibrillation ablation in septuagenarians. J. Cardiovasc. Electrophysiol. 2008 Aug;19 (8):807–11. doi: 10.1111/j.1540-8167.2008.01124.x. [DOI] [PubMed] [Google Scholar]
- 38.LF Hsu , P Jais , P Sanders, M Hocini, F Sacher, Y Takahashi, M Rotter, T Rostock, J Clementy, M Haissaguerre. Catheter ablation of permanent atrial fibrillation in the elderly. [Abstract] Heart Rhythm. 2005;0:0–0. [Google Scholar]
- 39.Oral Hakan, Chugh Aman, Lemola Kristina, Cheung Peter, Hall Burr, Good Eric, Han Jihn, Tamirisa Kamala, Bogun Frank, Pelosi Frank, Morady Fred. Noninducibility of atrial fibrillation as an end point of left atrial circumferential ablation for paroxysmal atrial fibrillation: a randomized study. Circulation. 2004 Nov 02;110 (18):2797–801. doi: 10.1161/01.CIR.0000146786.87037.26. [DOI] [PubMed] [Google Scholar]
- 40.Nademanee Koonlawee, Schwab Mark C, Kosar Erol M, Karwecki Margaret, Moran Michael D, Visessook Nithi, Michael Anthony Don, Ngarmukos Tachapong. Clinical outcomes of catheter substrate ablation for high-risk patients with atrial fibrillation. J. Am. Coll. Cardiol. 2008 Feb 26;51 (8):843–9. doi: 10.1016/j.jacc.2007.10.044. [DOI] [PubMed] [Google Scholar]
- 41.Kusumoto Fred, Prussak Karin, Wiesinger Melissa, Pullen Tammy, Lynady Cynthia. Radiofrequency catheter ablation of atrial fibrillation in older patients: outcomes and complications. J Interv Card Electrophysiol. 2009 Jun;25 (1):31–5. doi: 10.1007/s10840-008-9346-7. [DOI] [PubMed] [Google Scholar]
- 42.Bunch T Jared, Weiss J Peter, Crandall Brian G, May Heidi T, Bair Tami L, Osborn Jeffrey S, Anderson Jeffrey L, Lappe Donald L, Muhlestein J Brent, Nelson Jennifer, Day John D. Long-term clinical efficacy and risk of catheter ablation for atrial fibrillation in octogenarians. Pacing Clin Electrophysiol. 2010 Feb;33 (2):146–52. doi: 10.1111/j.1540-8159.2009.02604.x. [DOI] [PubMed] [Google Scholar]
- 43.Spragg David D, Dalal Darshan, Cheema Aamir, Scherr Daniel, Chilukuri Karuna, Cheng Alan, Henrikson Charles A, Marine Joseph E, Berger Ronald D, Dong Jun, Calkins Hugh. Complications of catheter ablation for atrial fibrillation: incidence and predictors. J. Cardiovasc. Electrophysiol. 2008 Jun;19 (6):627–31. doi: 10.1111/j.1540-8167.2008.01181.x. [DOI] [PubMed] [Google Scholar]
- 44.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Natale Andrea, Packer Douglas, Skanes Allan, Ambrogi Federico, Biganzoli Elia. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010 Feb;3 (1):32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 45.Stygall J, Kong R, Walker J M, Hardman S M, Harrison M J, Newman S P. Cerebral microembolism detected by transcranial Doppler during cardiac procedures. Stroke. 2000 Oct;31 (10):2508–10. doi: 10.1161/01.str.31.10.2508. [DOI] [PubMed] [Google Scholar]
- 46.Kok Lai Chow, Mangrum J Michael, Haines David E, Mounsey J Paul. Cerebrovascular complication associated with pulmonary vein ablation. J. Cardiovasc. Electrophysiol. 2002 Aug;13 (8):764–7. doi: 10.1046/j.1540-8167.2002.00764.x. [DOI] [PubMed] [Google Scholar]
- 47.Kapa Suraj, Bruce Charles J, Friedman Paul A, Asirvatham Samuel J. Advances in cardiac pacing: beyond the transvenous right ventricular apical lead. Cardiovasc Ther. 2010 Dec;28 (6):369–79. doi: 10.1111/j.1755-5922.2010.00157.x. [DOI] [PubMed] [Google Scholar]
- 48.Tops Laurens F, Schalij Martin J, Bax Jeroen J. The effects of right ventricular apical pacing on ventricular function and dyssynchrony implications for therapy. J. Am. Coll. Cardiol. 2009 Aug 25;54 (9):764–76. doi: 10.1016/j.jacc.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 49.Khan Mohammed N, Jaïs Pierre, Cummings Jennifer, Di Biase Luigi, Sanders Prashanthan, Martin David O, Kautzner Josef, Hao Steven, Themistoclakis Sakis, Fanelli Raffaele, Potenza Domenico, Massaro Raimondo, Wazni Oussama, Schweikert Robert, Saliba Walid, Wang Paul, Al-Ahmad Amin, Beheiry Salwa, Santarelli Pietro, Starling Randall C, Dello Russo Antonio, Pelargonio Gemma, Brachmann Johannes, Schibgilla Volker, Bonso Aldo, Casella Michela, Raviele Antonio, Haïssaguerre Michel, Natale Andrea. Pulmonary-vein isolation for atrial fibrillation in patients with heart failure. N. Engl. J. Med. 2008 Oct 23;359 (17):1778–85. doi: 10.1056/NEJMoa0708234. [DOI] [PubMed] [Google Scholar]
- 50.Oral Hakan, Chugh Aman, Ozaydin Mehmet, Good Eric, Fortino Jackie, Sankaran Sundar, Reich Scott, Igic Petar, Elmouchi Darryl, Tschopp David, Wimmer Alan, Dey Sujoya, Crawford Thomas, Pelosi Frank, Jongnarangsin Krit, Bogun Frank, Morady Fred. Risk of thromboembolic events after percutaneous left atrial radiofrequency ablation of atrial fibrillation. Circulation. 2006 Aug 22;114 (8):759–65. doi: 10.1161/CIRCULATIONAHA.106.641225. [DOI] [PubMed] [Google Scholar]
- 51.Fang Margaret C, Go Alan S, Chang Yuchiao, Borowsky Leila H, Pomernacki Niela K, Udaltsova Natalia, Singer Daniel E. Warfarin discontinuation after starting warfarin for atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2010 Nov;3 (6):624–31. doi: 10.1161/CIRCOUTCOMES.110.937680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shah Ashok J, Haissaguerre Michel, Hocini Meleze, Jais Pierre. Comparison of rhythm restoration strategies in paroxysmal atrial fibrillation. Expert Rev Cardiovasc Ther. 2010 Jul;8 (7):903–6. doi: 10.1586/erc.10.66. [DOI] [PubMed] [Google Scholar]
- 53.Reynolds Matthew R, Walczak Joshua, White Sarah A, Cohen David J, Wilber David J. Improvements in symptoms and quality of life in patients with paroxysmal atrial fibrillation treated with radiofrequency catheter ablation versus antiarrhythmic drugs. Circ Cardiovasc Qual Outcomes. 2010 Nov;3 (6):615–23. doi: 10.1161/CIRCOUTCOMES.110.957563. [DOI] [PubMed] [Google Scholar]
- 54.Martin-Doyle William, Reynolds Matthew R. Is AF Ablation Cost Effective? J Atr Fibrillation. 2010 May 01;2 (1):727–739. doi: 10.4022/jafib.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marrouche Nassir F. Catheter ablation treatment for paroxysmal atrial fibrillation results in a longer time to treatment failure than anti-arrhythmic drugs and improves quality of life. Evid Based Med. 2010 Jun;15 (3):88–9. doi: 10.1136/ebm1072. [DOI] [PubMed] [Google Scholar]
- 56.Wokhlu Anita, Monahan Kristi H, Hodge David O, Asirvatham Samuel J, Friedman Paul A, Munger Thomas M, Bradley David J, Bluhm Christine M, Haroldson Janis M, Packer Douglas L. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J. Am. Coll. Cardiol. 2010 May 25;55 (21):2308–16. doi: 10.1016/j.jacc.2010.01.040. [DOI] [PubMed] [Google Scholar]