Abstract
Atrial fibrillation (AF) presently affects over 2 million Americans, and the magnitude and population burden from AF continues to increase concomitant with the aging of the U.S. population. Chronic kidney disease (CKD) is present in 13% of individuals in the U.S., and the prevalence of CKD is also rapidly increasing. The increasing population burden of CKD and AF will profoundly affect the clinical and public health, since CKD and AF are both associated with lower quality of life, increased hospitalization rates, and a greater risk of heart failure, stroke, and total mortality. AF and CKD often co-exist, each condition predisposes to the other, and the co-occurrence of these disorders worsens prognosis relative to either disease alone. The shared epidemiology of CKD and AF may be explained by the strong pathophysiologic connections between these diseases. In order to promote a better understanding of CKD and AF, we have reviewed their shared epidemiology and pathophysiology and described the natural history of patients affected by both diseases.
Introduction
Atrial fibrillation (AF) is presently the most common sustained dysarrhythmia among Americans and the global burden of AF continues to grow.[1-3] The prevalence of AF increases dramatically with advancing age and this arrhythmia is present in nearly 1 in every 10 individuals by the age of 80 years.[3,4] The increasing population burden of AF has a profound impact on clinical and public health through its association with lower quality of life,[5,6] increased hospitalization rates, and a greater risk of heart failure,[7,8] stroke,[9] and all-cause mortality.[10-14]
Chronic kidney disease (CKD) affects approximately 13% of the U.S. population and the national prevalence of end-stage kidney disease more than doubled between 1991 and 2004.[15,16] Similar to the descriptive epidemiology of AF,[17] the incidence of CKD increases with advancing age and progression to end-stage renal disease (ESRD) adversely affects the quality of life and longevity of millions worldwide.[18] AF and CKD frequently coexist,[19] each condition predisposes to the other,[20] and the presence of concomitant AF and CKD worsens patient’s long-term prognosis relative to either disease alone.[21,22]
The shared epidemiology of CKD and AF may be explained by strong pathophysiologic connections between these two diseases (Table 1). Subclinical atrial remodeling, a process characterized by atrial structural and electrophysiological changes over time, is an important contributor to the initiation and maintenance of AF in many individuals.[23,24] Even mild renal impairment may promote or accelerate atrial remodeling by up regulating neurohumoral (e.g., TGF-β) and pro-inflammatory (C-reactive protein) signaling cascades, promoting volume retention and imposing hemodynamic stress on the atria.[25-27] CKD also results in chronic sympathetic nervous system activation, which may cause AF.[28-29] On the other hand, and reflecting the inter-connections between these 2 diseases, AF can promote or accelerate the progression of CKD by decreasing cardiac output, through its association with heart failure and thromboembolic events, and by promoting the development of the cardiorenal syndrome (Table 1).[30]
Table 1. Common Risk Factors and Mechanisms between Atrial Fibrillation and Chronic Kidney Disease.
MI = myocardial infarction, LV = left ventricular, LA = left atrial, TGF = tissue growth factor, CRP = C-reactive protein, TNF = tumor necrosis factor, IL = interleukin
| Common AF and CKD Risk Factors | Age, hypertension, obesity, diabetes mellitus, valvular heart disease, acute coronary syndrome, heart failure |
|---|---|
| Common Intermediate Phenotypes | LV hypertrophy, LA enlargement |
| Cardiac Remodeling Mechanisms in Chronic Kidney Disease | |
| Neurohumoral signaling mechanisms | Renin-angiotensin-aldosterone system, TGF-β1, sympathetic nervous system up-regulation |
| Inflammatory Mechanisms | Increased systemic inflammation – increased circulating levels of CRP, TNF-α, fibrinogen, IL-6, increased oxidative stress |
| Stretch-related Mechanisms | Abnormal calcium handling, shortened action potential duration, decreased refractoriness, dispersion of the refractory period |
| Fibrosis-related Mechanisms | Disrupted cell-cell junctions, areas of delayed conduction, facilitation of re-entry |
In light of the growing number of patients affected by both CKD and AF, we have undertaken this work to review the mechanistic and epidemiological parallels between these two diseases, and the strong connections between AF, CKD, and several important cardiovascular risk factors. We have also drawn from the published literature on the natural history of AF in order to promote the evidence-based treatment of AF among patients with concomitant CKD.
Epidemiology of Atrial Fibrillation in Patients with Chronic Kidney Disease
Our group and others have shown that reduced kidney function and the presence of albuminuria are strongly associated with an increased risk for developing AF.[18,31] Contemporary estimates suggest that individuals with ESRD and AF are 50% more likely to be hospitalized, and approximately two-thirds more likely to die, when compared to individuals in normal sinus rhythm.[11] The relationship between kidney dysfunction and risk for AF is J-shaped, with the lowest risk of AF seen among patients with the least significant reduction in kidney function (Figure 1).[18] However, the prevalence of AF is high even in patients with mild or moderate CKD, with contemporary estimates suggesting that nearly one in every five persons with Stage 1-2 CKD has AF.[19,32]
Figure 1. Cumulative incidence of Atrial Fibrillation by categories of estimated glomerular filtration rate in whites (top) and blacks (bottom).
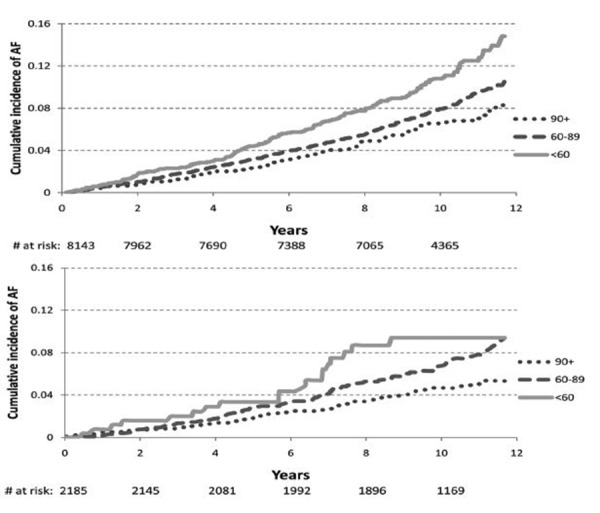
From the Atherosclerosis in Communities study. Reprinted with permission from Alonso, A. Circulation 2011
Epidemiology of Chronic Kidney Disease in Patients with Atrial Fibrillation
Although data are more limited with respect to the influence of AF on the incidence and progression of kidney dysfunction, AF is strongly and independently associated with incident CKD.[20] In an international study involving over 235,000 men and women recruited at an ambulatory clinic visit, AF was associated with 1.8-fold higher odds of developing kidney dysfunction and 2.2-fold higher odds of developing proteinuria over a 6-year follow-up period.20 Similar to the current “epidemic” of AF, the recent national increase in new cases of CKD may be secondary to the aging of the population and an increase in the prevalence of several common important comorbidities, including diabetes, hypertension, and coronary heart disease.[33-38]
Atrial Fibrillation in Chronic Kidney Disease: Shared Predisposing Factors
AF, like CKD, disproportionately affects older individuals, with approximately one-half of all AF cases occurring in persons 75 years and older.[4,39]AF shares strong epidemiologic associations with other cardiovascular diseases and risk factors, such as coronary artery disease, hypertension, valvular heart disease, heart failure, obesity, diabetes mellitus, and obstructive sleep apnea.[17,40] CKD also predominantly affects older Americans, and many of the chronic disease conditions and risk factors that predispose to AF are also associated with the development of CKD. Increasing rates of shared risk factors provide insights into the changing, and increasingly interwoven, epidemiology of AF and CKD.
Gender and Race
Although the prevalence of CKD is higher among African Americans than among white individuals, the rate of progression from milder CKD to ESRD, and death rates from ESRD are higher among white as compared with non-white patients.[41] Even though CKD is more commonly observed in women, women with CKD have a more favorable prognosis than men with CKD.[42] It is notable that racial and sex differences in predisposition to AF also exist, with white individuals and men at higher risk for AF than African Americans and women, respectively.[33] Although the epidemiology of AF in African Americans and women with CKD is poorly characterized, we hypothesize that an increased prevalence of AF among men and whites with CKD may cause a more precipitous decline in renal function and clinical status when compared with women and non-white individuals with CKD.[32]
Diabetes Mellitus
Diabetes mellitus is associated with a markedly increased risk for AF in both American men and women.[33] Diabetes also accounts for upwards of 2 in every 5 new cases of kidney failure in the U.S.35 Treatment of diabetes with insulin-sensitizing thiazolidinedione therapy has been shown to reduce recurrences of AF.[44] In light of the association between increased adiposity, diabetes, AF and CKD, insulin resistance has been hypothesized to represent an important intermediate step in the progression to AF.[45] To date, however, data are conflicted with respect to the role of insulin resistance in mediating the increased risk for AF among persons with pre-diabetes and diabetes.[46]
Microalbuminuria is common in diabetics and relates strongly to the risk of developing CKD.[47-49] Acute or sustained hyperglycemia can cause microvascular damage in the kidney, leading to increased glomerular permeability and albuminuria.[50-51] Albuminuria has been identified as an independent predictor of AF, irrespective of renal dysfunction.[52] Since approximately one-half of patients with diabetes have at least some degree of albuminuria,[47] a high prevalence of proteinuria may explain the significant burden of AF in diabetic populations.[53] Hyperglycemic-induced renovascular disease promotes up-regulation of neurohumoral signaling cascades that also lead to development of pathological cardiac remodeling phenotypes associated with AF (Table 1).[50] Further investigations are needed to investigate the mechanisms underlying the associations between diabetes mellitus, albuminuria, and AF.
Coronary Artery Disease
Individuals with CKD are significantly more likely to have underlying coronary artery disdisease than men and women without impaired renal function,[54] and prevalent CKD is an independent risk factor for subsequent adverse cardiovascular events.[12] A history of prior coronary heart disease, and development of a myocardial infarction, are established risk factors for AF, conferring a 1.5 to 3-fold increased risk for AF.[55] Cardiogenic shock and left ventricular dysfunction are more commonly observed following acute myocardial infarction in patients with, than in those without, CKD, providing a potential hemodynamic link between prevalent CKD, coronary artery disease, and AF.[56]
Hypertension
Hypertension is both a cause and consequence of CKD, with the majority of CKD patients affected by systemic hypertension.[57] Moreover, with sodium retention, activation of the renin-angiotensin aldosterone system (RAAS), and sympathetic nervous system up-regulation, hypertension becomes increasingly refractory to treatment and more severe in advanced stages of CKD.[58] This has important implications for both the development and management of AF, since the duration and intensity of exposure to elevated systolic and pulse pressures are critical contributors to pathological atrial structural remodeling over adulthood.[23,59,60] Hypertension is associated with a markedly increased risk for AF and each 20-mmHg increase in pulse pressure may elevate the risk of AF by as much as one-quarter.[61,33] Notably, the concomitant presence of hypertension and diabetes mellitus may also have a synergistic effect on the likelihood of developing AF, as diabetes has been associated with a 1.5-fold higher risk of AF among individuals with hypertension.[62] It remains unclear, however, why the combination of diabetes and hypertension has such a profound effect on the risk for developing new-onset AF, but amplified activation of neurohumoral and catecholinergic signaling pathways common to CKD and AF is a likely explanation.
Obesity
The ongoing obesity epidemic in developed countries has important public health implications in light of the known relations of increased adiposity with CKD and several common cardiovascular diseases, including AF.[2,57,63-65] Poor kidney function is strongly associated with higher body mass, and each unit increment in body mass index increases the odds of CKD by approximately 5%.[65] Obesity indirectly contributes to the development of CKD through its association with several underlying risk factors and predisposing conditions including diabetes, hypertension, and atherosclerosis.[66] Obesity may also directly lead to the development of CKD; several epidemiologic investigations have shown that individuals with obesity are at a 3-fold higher risk for CKD, even after adjustment for blood pressure and presence of diabetes.[63]
Obese individuals are also at higher risk for AF, with each unit increase in body mass index conferring an approximate 4% increased risk for developing AF.[67] Atrial structural remodeling appears to play an important role in mediating the relation between increased adiposity and risk for AF.[67] The strong relations of the obesity-related disorder obstructive sleep apnea with CKD and AF also highlight the significant and complex associations between obesity, CKD, and AF. Sleep apnea is increasingly recognized as an important risk factor for AF and CKD,[68] and the obstructive sleep apnea syndrome is also related to the underlying progression of both diseases.[69] Mechanisms connecting obesity to the development of CKD and AF may be interlinked through crosstalk between fat, the kidney, the liver, and the heart through circulating signaling molecules such as fetuin A, adiponectin, resistin, and 5′-AMP activated protein kinase.[70,71]
Valvular Disease
Among patients with CKD, particularly those with end-stage renal disease, dystrophic vascular and valvular calcification is common and is likely secondary to chronic hyperphosphatemia.[72,73] Dystrophic valvular calcification can lead to mitral annular calcification and aortic stenosis, two valvular disorders strongly linked to left ventricular hypertrophy, atrial enlargement, and AF.[74] In fact, the presence of valvular heart disease increased AF risk by 3.4- and 1.8-fold in female and male Framingham Heart Study participants, respectively.[17] Since even mild aortic stenosis and mitral regurgitation impose hemodynamic stress on the atrium and ventricle, valvular heart disease may accelerate atrial structural and electrical remodeling and is another comorbid illness that promotes the development of AF in patients with CKD (Figure 2).
Figure 2. Mechanisms Linking Atrial Fibrillation to Chronic Kidney Disease.
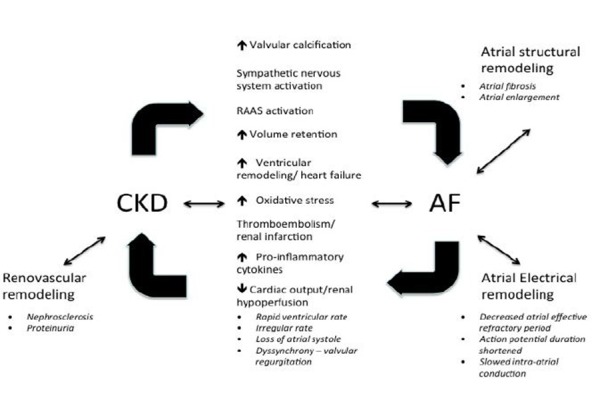
CKD = chronic kidney disease; AF = atrial fibrillation; RAAS = renin-angiotensin-aldosterone system
Heart Failure
The majority of individuals with heart failure have significant renal impairment, and worsen ing renal function in persons hospitalized with heart failure is associated with an increased risk for adverse cardiac events.[75-77] CKD is associated with a 1.4-fold and 2.4-fold higher risk for new-onset heart failure in men and women, respectively, compared to persons with normal renal function.[78] Although common risk factors such as diabetes and hypertension contribute to the association between CKD and heart failure, the incidence rates of heart failure are higher among patients with CKD than would be expected on the basis of risk factors alone.[79]
AF and HF also frequently coexist, with 30% of all individuals with HF affected by AF.[7,80] Individuals with AF are at significantly higher risk for developing HF in comparison to persons in normal sinus rhythm.[7,8,30,81] Conversely, the diagnosis of HF is associated with a greater than 5-fold increased risk for development of AF, highlighting the strong connection between these two increasingly prevalent disorders.[7] As we discuss in the next section, subclinical ventricular remodeling and clinical HF may represent a common pathway through which CKD promotes AF, and vice versa (Figure 2).
Pathophysiology of Atrial Fibrillation as it relates to Chronic Kidney Disease
Chronic kidney disease imposes hemodynamic, inflammatory, catecholinergic, neurohumoral, and metabolic stress on the heart (Figure 2).[28,58,82,83] Subclinical phenotypes, such as left ventricular hypertrophy and atrial enlargement, are associated with CKD and develop in response to these stressors.[84-86] Although ventricular and atrial remodeling may appear to be adaptive, enabling the heart to compensate for increases in preload and/or afterload imposed by CKD, these compensatory mechanisms may eventually become maladaptive and lead to a decline in cardiac function. Not surprisingly, increased echocardiographic left ventricular wall thickness and electrocardiographic left ventricular hypertrophy, two markers of ventricular remodeling commonly seen in patients with CKD, are also strongly associated with atrial enlargement and AF.[59,85]
Renin-Angiotensin Aldosterone System
Chronic kidney disease activates a number of stress-signaling pathways, including the RAAS. RAAS up-regulation results in impaired vascular growth, interstitial myocardial fibrosis, and myocyte apoptosis.[87] Up-regulation of the RAAS may lead directly to AF through salt retention and atrial distension. Chronic RAAS activation also contributes to atrial remodeling independent of its hemodynamic effects in experimental studies of AF.[88] Key components of the RAAS, including Angiotensin-converting enzyme, Angiotensin II (AII) and transforming growth factor-beta 1 (TGF-β1), are up-regulated in a systemic and tissue-specific manner in patients with CKD.[87,89] The electrophysiologic and structural effects of chronic RAAS activation act in concert to promote the development of an atrial substrate that is vulnerable to AF (Figure 2).[89-91] Although the benefits of RAAS inhibition with respect to AF prevention have not been systematically studied, data support the hypothesis that RAAS inhibition may reduce the incidence of AF in high-risk subgroups, such as those with CKD.[89,92]
Oxidative Stress and Inflammation
It is well known that CKD is associated with increased levels of circulating pro-inflammatory cytokines,[26] perhaps because the accumulation of uremic toxins causes an endothelial inflammatory response.[93] Exposure of endothelium to uremic toxins leads to changes in endovascular cellular phenotypes and production of many pro-inflammatory molecules,[94-95] often leading to increased vascular stiffness, accelerated atherosclerosis, and the development of adverse cardiac remodeling phenotypes (Figure 2).[86]
Systemic inflammation and endothelial dysfunction play an important role in the pathogenesis of AF (Figure 2).[25,96] The key role of inflammation in the development of AF is highlighted by the fact that histologic evidence of inflammation is seen in two-thirds of patients who go on to develop this arrhythmia.[97] In particular, serum levels of interleukin-6, fibrinogen, and C-reactive protein, three important markers of inflammation that are elevated in patients with CKD,[98] are also predictive of future episodes of AF.[82,99] Over-expression of tumor necrosis factor-α (TNF-α), another inflammatory cytokine, is also associated with atrial fibrosis, ion channel dysfunction, and increased susceptibility to AF.[100] Consistent with this working hypothesis, several studies have shown that anti-inflammatory agents, such as glucocorticoids, and medications with anti-oxidative properties, such as statins, may prevent AF.[101] Further study into the anti-arrhythmic effects of several commonly used drugs with anti-inflammatory effects, particularly statins, in patients with CKD appears warranted.[102-104]
Sympathetic Nervous System Up-Regulation
CKD leads to chronic up-regulation of the sympathetic nervous system, as evidenced by the fact that kidney dysfunction is associated with lower heart rate recovery, an established marker of autonomic function, after exercise testing.[105-108] Since enhanced automaticity in the left atrium and pulmonary veins is considered a major contributor to the pathogenesis of AF, kidney dysfunction may lead to AF through its association with sympathetic nervous system up-regulation.[109] Enhanced autonomic tone during dialysis, along with acute changes in circulating volume and electrolyte concentrations, may explain why CKD patients on hemodialysis are at particularly high risk for AF (Figure 2).[110]
Chronic Kidney Disease and pathological atrial remodeling
Atrial remodeling – a process describing progressive atrial electrical and structural changes in response to chronic or repeated atrial injury– merits attention in understanding the pathogenesis of AF in the setting of CKD (Figure 2).[90,91] Experimental models of AF show that atrial remodeling often precedes development of AF.[90,91] Pathologic atrial remodeling is related to the presence and severity of CKD.[86] Chronic intra-atrial or intra-ventricular pressure overload from CKD activates stress signaling pathways, most notably the RAAS, yielding impaired myocardial vascular growth, myocyte apoptosis and interstitial fibrosis as discussed above.[23,31] Chronic RAAS activation, as evidenced by increased levels of circulating AII and TGF-β1, has been shown to contribute to atrial fibrosis and remodeling in AF experimental studies.[90] Experimental data also show that the RAAS up-regulation also influences ion channel function and action potential duration, predisposing to intra-atrial reentry and AF. Independent of its effects on the RAAS, CKD may also contribute to pathologic atrial remodeling through its associations with sympathetic nervous system up-regulation, systemic inflammation, and valvular heart disease.[8]
Natural History of Atrial Fibrillation in Individuals with Chronic Kidney Disease
CKD is an independent predictor of adverse cardiac events among patients with AF.[11] Long-term all-cause mortality rates, risk of non-fatal myocardial infarction and stroke, and hospitalizations for heart failure are markedly higher in individuals with AF and ESRD compared to those with ESRD alone.[9-12] Markers of subclinical cardiac remodeling that accompany AF, including echocardiographic atrial enlargement, are also associated with an increased risk of dying and adverse cardiovascular events among patients with CKD.[111] Although longitudinal data on the natural history of AF among patients with CKD not requiring renal replacement therapy are lacking, the presence of both CKD and AF identifies a subgroup of individuals at particularly high risk for thromboembolic events.[13] After adjustment for known stroke risk factors, the presence of proteinuria increases the risk of thromboembolism by more than 50%, and there is a graded, increased risk of stroke associated with progressively lower estimated glomerular filtration rate.[52] The association between CKD and stroke may be mediated by ongoing subclinical inflammation.[112]
Implications of Chronic Kidney Disease on the Treatment of Individuals with Atrial Fibrillation
Despite the fact that patients with both AF and CKD are at significantly higher risk of stroke than patients with either disease alone, renal insufficiency also increases the risk of bleeding with the use of antiplatelet and anticoagulant agents, and the optimal anticoagulation strategy for patients with AF and CKD remains unclear.[9,52,113,114] The debate over which anticoagulant to use for patients with AF and CKD is unlikely to be resolved soon, however, since patients with CKD have been systematically excluded from most clinical trials of anticoagulants used in the setting of AF.
CKD increases the risk of complications from anti-arrhythmic drugs, such as digoxin, sotalol or dofetilide, which undergo renal elimination.[115,116] CKD is also an independent predictor of arrhythmia recurrence after catheter ablation for AF.[117] This association may be mediated by the association between CKD and atrial structural remodeling.[117] CKD has also been identified as a major predictor of complications after catheter ablation in patients with underlying AF.[117] In a cohort of more than 1,600 patients undergoing ablation for AF as well as several other arrhythmias, renal insufficiency was associated with a 2.5-fold higher rate of major peri- and post-operative complications.[118] Additional prospective investigations of patients with CKD and AF are needed to determine how CKD affects treatment response and complications from catheter-based AF ablation.
Conclusions
In part due to the increasing prevalence of shared cardiovascular risk factors such as diabetes, obesity, and heart failure, and the aging of the population, the number of individuals in the U.S. and other developed countries affected by AF and CKD is growing rapidly. Independent of shared risk factors, patients with CKD are at increased risk for developing AF, and vice versa, suggesting strong mechanistic connections between these two conditions. Chronic activation of neurohumoral, pro-inflammatory, and catecholinergic signaling pathways in individuals with CKD promote cardiac structural and electrophysiologic changes over time, enhancing vulnerability to AF. Patients with both CKD and AF are at significantly increased risk for adverse cardiac events, including thromboembolism and death. In light of the fact that patients with CKD are often excluded from clinical studies involving patients with AF, the optimal strategy for managing patients with AF and concomitant CKD remains unclear. It is apparent, however, that patients with AF and CKD are at high risk for AF-related treatment failure and complications. Further longitudinal studies involving patients with CKD and AF are needed in order to determine how this important group of patients responds to contemporary AF treatments, including catheter ablation as well as novel anti-coagulants and anti-arrhythmic medications.
References
- 1.Wolf P A, Benjamin E J, Belanger A J, Kannel W B, Levy D, D'Agostino R B. Secular trends in the prevalence of atrial fibrillation: The Framingham Study. Am. Heart J. 1996 Apr;131 (4):790–5. doi: 10.1016/s0002-8703(96)90288-4. [DOI] [PubMed] [Google Scholar]
- 2.Chen Lin Y, Shen Win-Kuang. Epidemiology of atrial fibrillation: a current perspective. Heart Rhythm. 2007 Mar;4 (3 Suppl):S1–6. doi: 10.1016/j.hrthm.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 3.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 4.Go Alan S. The epidemiology of atrial fibrillation in elderly persons: the tip of the iceberg. Am J Geriatr Cardiol. 2005 Mar 24;14 (2):56–61. doi: 10.1111/j.1076-7460.2005.02278.x. [DOI] [PubMed] [Google Scholar]
- 5.Savelieva I, Paquette M, Dorian P, Lüderitz B, Camm A J. Quality of life in patients with silent atrial fibrillation. Heart. 2001 Feb;85 (2):216–7. doi: 10.1136/heart.85.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramaraj Radhakrishnan. Atrial fibrillation and quality of life. Am. Heart J. 2009 Nov;158 (5) doi: 10.1016/j.ahj.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Wang Thomas J, Larson Martin G, Levy Daniel, Vasan Ramachandran S, Leip Eric P, Wolf Philip A, D'Agostino Ralph B, Murabito Joanne M, Kannel William B, Benjamin Emelia J. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003 Jun 17;107 (23):2920–5. doi: 10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 8.McManus David D, Shaikh Amir Y, Abhishek Fnu, Vasan Ramachandran S. Atrial fibrillation and heart failure parallels: lessons for atrial fibrillation prevention. Crit Pathw Cardiol. 2011 Mar;10 (1):46–51. doi: 10.1097/HPC.0b013e31820e1a4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolf P A, Abbott R D, Kannel W B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22 (8):983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 10.Miyasaka Yoko, Barnes Marion E, Bailey Kent R, Cha Stephen S, Gersh Bernard J, Seward James B, Tsang Teresa S M. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J. Am. Coll. Cardiol. 2007 Mar 06;49 (9):986–92. doi: 10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 11.Genovesi Simonetta, Vincenti Antonio, Rossi Emanuela, Pogliani Daniela, Acquistapace Irene, Stella Andrea, Valsecchi Maria Grazia. Atrial fibrillation and morbidity and mortality in a cohort of long-term hemodialysis patients. Am. J. Kidney Dis. 2008 Feb;51 (2):255–62. doi: 10.1053/j.ajkd.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 12.Herzog Charles A, Asinger Richard W, Berger Alan K, Charytan David M, Díez Javier, Hart Robert G, Eckardt Kai-Uwe, Kasiske Bertram L, McCullough Peter A, Passman Rod S, DeLoach Stephanie S, Pun Patrick H, Ritz Eberhard. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011 Sep;80 (6):572–86. doi: 10.1038/ki.2011.223. [DOI] [PubMed] [Google Scholar]
- 13.Vázquez Eduardo, Sánchez-Perales Carmen, Lozano Cristóbal, García-Cortés Ma José, Borrego Francisco, Guzmán Manuel, Pérez Pilar, Pagola Carlos, Borrego Ma José, Pérez Vicente. Comparison of prognostic value of atrial fibrillation versus sinus rhythm in patients on long-term hemodialysis. Am. J. Cardiol. 2003 Oct 01;92 (7):868–71. doi: 10.1016/s0002-9149(03)00904-4. [DOI] [PubMed] [Google Scholar]
- 14.Benjamin E J, Wolf P A, D'Agostino R B, Silbershatz H, Kannel W B, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998 Sep 08;98 (10):946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 15.Coresh Josef, Selvin Elizabeth, Stevens Lesley A, Manzi Jane, Kusek John W, Eggers Paul, Van Lente Frederick, Levey Andrew S. Prevalence of chronic kidney disease in the United States. JAMA. 2007 Nov 07;298 (17):2038–47. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 16.Collins Allan J, Kasiske Bertram, Herzog Charles, Chavers Blanche, Foley Robert, Gilbertson David, Grimm Richard, Liu Jiannong, Louis Thomas, Manning Willard, Matas Arthur, McBean Marshall, Murray Anne, St Peter Wendy, Xue Jay, Fan Qiao, Guo Haifeng, Li Shuling, Li Suying, Roberts Tricia, Snyder Jon, Solid Craig, Wang Changchun, Weinhandl Eric, Arko Cheryl, Chen Shu-Cheng, Dalleska Frederick, Daniels Frank, Dunning Stephan, Ebben James, Frazier Eric, Johnson Roger, Sheets Daniel, Forrest Beth, Berrini Delaney, Constantini Edward, Everson Susan, Frederick Pamela, Eggers Paul, Agodoa Lawrence. Excerpts from the United States Renal Data System 2004 annual data report: atlas of end-stage renal disease in the United States. Am. J. Kidney Dis. 2005 Jan;45 (1 Suppl 1):A5–7, S1-280. doi: 10.1053/j.ajkd.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Kannel W B, Wolf P A, Benjamin E J, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am. J. Cardiol. 1998 Oct 16;82 (8A):2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- 18.Alonso Alvaro, Lopez Faye L, Matsushita Kunihiro, Loehr Laura R, Agarwal Sunil K, Chen Lin Y, Soliman Elsayed Z, Astor Brad C, Coresh Josef. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011 Jun 28;123 (25):2946–53. doi: 10.1161/CIRCULATIONAHA.111.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soliman Elsayed Z, Prineas Ronald J, Go Alan S, Xie Dawei, Lash James P, Rahman Mahboob, Ojo Akinlolu, Teal Val L, Jensvold Nancy G, Robinson Nancy L, Dries Daniel L, Bazzano Lydia, Mohler Emile R, Wright Jackson T, Feldman Harold I. Chronic kidney disease and prevalent atrial fibrillation: the Chronic Renal Insufficiency Cohort (CRIC). Am. Heart J. 2010 Jun;159 (6):1102–7. doi: 10.1016/j.ahj.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watanabe Hiroshi, Watanabe Toru, Sasaki Shigeru, Nagai Kojiro, Roden Dan M, Aizawa Yoshifusa. Close bidirectional relationship between chronic kidney disease and atrial fibrillation: the Niigata preventive medicine study. Am. Heart J. 2009 Oct;158 (4):629–36. doi: 10.1016/j.ahj.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 21.Horio Takeshi, Iwashima Yoshio, Kamide Kei, Tokudome Takeshi, Yoshihara Fumiki, Nakamura Satoko, Kawano Yuhei. Chronic kidney disease as an independent risk factor for new-onset atrial fibrillation in hypertensive patients. J. Hypertens. 2010 Aug;28 (8):1738–44. doi: 10.1097/HJH.0b013e32833a7dfe. [DOI] [PubMed] [Google Scholar]
- 22.Korantzopoulos Panagiotis, Kokkoris Stelios, Liu Tong, Protopsaltis Ioannis, Li Guangping, Goudevenos John A. Atrial fibrillation in end-stage renal disease. Pacing Clin Electrophysiol. 2007 Nov;30 (11):1391–7. doi: 10.1111/j.1540-8159.2007.00877.x. [DOI] [PubMed] [Google Scholar]
- 23.McManus David D, Xanthakis Vanessa, Sullivan Lisa M, Zachariah Justin, Aragam Jayashri, Larson Martin G, Benjamin Emelia J, Vasan Ramachandran S. Longitudinal tracking of left atrial diameter over the adult life course: Clinical correlates in the community. Circulation. 2010 Feb 09;121 (5):667–74. doi: 10.1161/CIRCULATIONAHA.109.885806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nattel Stanley, Burstein Brett, Dobrev Dobromir. Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol. 2008 Apr;1 (1):62–73. doi: 10.1161/CIRCEP.107.754564. [DOI] [PubMed] [Google Scholar]
- 25.Aviles Ronnier J, Martin David O, Apperson-Hansen Carolyn, Houghtaling Penny L, Rautaharju Pentti, Kronmal Richard A, Tracy Russell P, Van Wagoner David R, Psaty Bruce M, Lauer Michael S, Chung Mina K. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003 Dec 16;108 (24):3006–10. doi: 10.1161/01.CIR.0000103131.70301.4F. [DOI] [PubMed] [Google Scholar]
- 26.Shlipak Michael G, Fried Linda F, Crump Casey, Bleyer Anthony J, Manolio Teri A, Tracy Russell P, Furberg Curt D, Psaty Bruce M. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003 Jan 07;107 (1):87–92. doi: 10.1161/01.cir.0000042700.48769.59. [DOI] [PubMed] [Google Scholar]
- 27.Singh David, Whooley Mary A, Ix Joachim H, Ali Sadia, Shlipak Michael G. Association of cystatin C and estimated GFR with inflammatory biomarkers: the Heart and Soul Study. Nephrol. Dial. Transplant. 2007 Apr;22 (4):1087–92. doi: 10.1093/ndt/gfl744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlaich Markus P. Sympathetic activation in chronic kidney disease: out of the shadow. Hypertension. 2011 Apr;57 (4):683–5. doi: 10.1161/HYPERTENSIONAHA.110.167189. [DOI] [PubMed] [Google Scholar]
- 29.Schlaich Markus P, Socratous Flora, Hennebry Sarah, Eikelis Nina, Lambert Elisabeth A, Straznicky Nora, Esler Murray D, Lambert Gavin W. Sympathetic activation in chronic renal failure. J. Am. Soc. Nephrol. 2009 May;20 (5):933–9. doi: 10.1681/ASN.2008040402. [DOI] [PubMed] [Google Scholar]
- 30.Ronco Claudio, Haapio Mikko, House Andrew A, Anavekar Nagesh, Bellomo Rinaldo. Cardiorenal syndrome. J. Am. Coll. Cardiol. 2008 Nov 04;52 (19):1527–39. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 31.McManus David D, Corteville David C M, Shlipak Michael G, Whooley Mary A, Ix Joachim H. Relation of kidney function and albuminuria with atrial fibrillation (from the Heart and Soul Study). Am. J. Cardiol. 2009 Dec 01;104 (11):1551–5. doi: 10.1016/j.amjcard.2009.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baber Usman, Howard Virginia J, Halperin Jonathan L, Soliman Elsayed Z, Zhang Xiao, McClellan William, Warnock David G, Muntner Paul. Association of chronic kidney disease with atrial fibrillation among adults in the United States: REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circ Arrhythm Electrophysiol. 2011 Feb;4 (1):26–32. doi: 10.1161/CIRCEP.110.957100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benjamin E J, Levy D, Vaziri S M, D'Agostino R B, Belanger A J, Wolf P A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994 Mar 16;271 (11):840–4. [PubMed] [Google Scholar]
- 34.Schaeffner Elke S, Kurth Tobias, Bowman Thomas S, Gelber Rebecca P, Gaziano J Michael. Blood pressure measures and risk of chronic kidney disease in men. Nephrol. Dial. Transplant. 2008 Apr;23 (4):1246–51. doi: 10.1093/ndt/gfm757. [DOI] [PubMed] [Google Scholar]
- 35.Beckles Gloria L, Zhu Julia, Moonesinghe Ramal. Diabetes - United States, 2004 and 2008. MMWR supplements. 2011 Jan 14;60 (1):90–3. [PubMed] [Google Scholar]
- 36.Chen Wei, Chen Weiqing, Wang Hui, Dong Xiuqing, Liu Qinghua, Mao Haiping, Tan Jiaqing, Lin Jianxiong, Zhou Feiyu, Luo Ning, He Huijuan, Johnson Richard J, Zhou Shu-Feng, Yu Xueqing. Prevalence and risk factors associated with chronic kidney disease in an adult population from southern China. Nephrol. Dial. Transplant. 2009 Apr;24 (4):1205–12. doi: 10.1093/ndt/gfn604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cutler Jeffrey A, Sorlie Paul D, Wolz Michael, Thom Thomas, Fields Larry E, Roccella Edward J. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008 Nov;52 (5):818–27. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 38.Cowie Catherine C, Rust Keith F, Byrd-Holt Danita D, Eberhardt Mark S, Flegal Katherine M, Engelgau Michael M, Saydah Sharon H, Williams Desmond E, Geiss Linda S, Gregg Edward W. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006 Jun;29 (6):1263–8. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 39.Feinberg W M, Blackshear J L, Laupacis A, Kronmal R, Hart R G. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch. Intern. Med. 1995 Mar 13;155 (5):469–73. [PubMed] [Google Scholar]
- 40.Rich Michael W. Epidemiology of atrial fibrillation. J Interv Card Electrophysiol. 2009 Jun;25 (1):3–8. doi: 10.1007/s10840-008-9337-8. [DOI] [PubMed] [Google Scholar]
- 41.Evans Kira, Coresh Josef, Bash Lori D, Gary-Webb Tiffany, Köttgen Anna, Carson Kathryn, Boulware L Ebony. Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol. Dial. Transplant. 2011 Mar;26 (3):899–908. doi: 10.1093/ndt/gfq473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kummer Sebastian, von Gersdorff Gero, Kemper Markus J, Oh Jun. The influence of gender and sexual hormones on incidence and outcome of chronic kidney disease. Pediatr. Nephrol. 2012 Aug;27 (8):1213–9. doi: 10.1007/s00467-011-1963-1. [DOI] [PubMed] [Google Scholar]
- 43.Borzecki Ann M, Bridgers D Keith, Liebschutz Jane M, Kader Boris, Kazis Lewis E, Berlowitz Dan R. Racial differences in the prevalence of atrial fibrillation among males. J Natl Med Assoc. 2008 Feb;100 (2):237–45. doi: 10.1016/s0027-9684(15)31212-8. [DOI] [PubMed] [Google Scholar]
- 44.Korantzopoulos Panagiotis, Kokkoris Stelios, Kountouris Evaggelos, Protopsaltis Ioannis, Siogas Konstantinos, Melidonis Andreas. Regression of paroxysmal atrial fibrillation associated with thiazolidinedione therapy. Int. J. Cardiol. 2008 Apr 25;125 (3):e51–3. doi: 10.1016/j.ijcard.2006.12.063. [DOI] [PubMed] [Google Scholar]
- 45.Meigs James B, Larson Martin G, Fox Caroline S, Keaney John F, Vasan Ramachandran S, Benjamin Emelia J. Association of oxidative stress, insulin resistance, and diabetes risk phenotypes: the Framingham Offspring Study. Diabetes Care. 2007 Oct;30 (10):2529–35. doi: 10.2337/dc07-0817. [DOI] [PubMed] [Google Scholar]
- 46.Fontes João D, Lyass Asya, Massaro Joseph M, Rienstra Michiel, Dallmeier Dhayana, Schnabel Renate B, Wang Thomas J, Vasan Ramachandran S, Lubitz Steven A, Magnani Jared W, Levy Daniel, Ellinor Patrick T, Fox Caroline S, Benjamin Emelia J. Insulin resistance and atrial fibrillation (from the Framingham Heart Study). Am. J. Cardiol. 2012 Jan 01;109 (1):87–90. doi: 10.1016/j.amjcard.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maharjan B R, Bhandary S, Risal P, Sedhain A, Shakya P R, Gautam M. Microalbuminuria and macroalbuminuria in type 2 diabetes. J Nepal Health Res Counc. 2010 Oct;8 (2):110–5. [PubMed] [Google Scholar]
- 48.Salles Gil F, Cardoso Claudia R L, Pereira Vinicius S, Fiszman Roberto, Muxfeldt Elizabeth S. Prognostic significance of a reduced glomerular filtration rate and interaction with microalbuminuria in resistant hypertension: a cohort study. J. Hypertens. 2011 Oct;29 (10):2014–23. doi: 10.1097/HJH.0b013e32834adb09. [DOI] [PubMed] [Google Scholar]
- 49.Jun Min, Perkovic Vlado, Cass Alan. Intensive glycemic control and renal outcome. Contrib Nephrol. 2011;170 ():196–208. doi: 10.1159/000325664. [DOI] [PubMed] [Google Scholar]
- 50.Campbell Duncan J, Somaratne Jithendra B, Jenkins Alicia J, Prior David L, Yii Michael, Kenny James F, Newcomb Andrew E, Schalkwijk Casper G, Black Mary J, Kelly Darren J. Impact of type 2 diabetes and the metabolic syndrome on myocardial structure and microvasculature of men with coronary artery disease. Cardiovasc Diabetol. 2011 Sep 19;10 () doi: 10.1186/1475-2840-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Swärd P, Rippe B. Acute and sustained actions of hyperglycaemia on endothelial and glomerular barrier permeability. Acta Physiol (Oxf) 2012 Mar;204 (3):294–307. doi: 10.1111/j.1748-1716.2011.02343.x. [DOI] [PubMed] [Google Scholar]
- 52.Go Alan S, Fang Margaret C, Udaltsova Natalia, Chang Yuchiao, Pomernacki Niela K, Borowsky Leila, Singer Daniel E. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. 2009 Mar 17;119 (10):1363–9. doi: 10.1161/CIRCULATIONAHA.108.816082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abdelhafiz Ahmed H, Ahmed Shameela, El Nahas Meguid. Microalbuminuria: marker or maker of cardiovascular disease. Nephron Exp. Nephrol. 2011;119 Suppl 1 ():e6–10. doi: 10.1159/000328015. [DOI] [PubMed] [Google Scholar]
- 54.Di Angelantonio Emanuele, Chowdhury Rajiv, Sarwar Nadeem, Aspelund Thor, Danesh John, Gudnason Vilmundur. Chronic kidney disease and risk of major cardiovascular disease and non-vascular mortality: prospective population based cohort study. BMJ. 2010 Sep 30;341 () doi: 10.1136/bmj.c4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saczynski Jane S, McManus David, Zhou Zheng, Spencer Frederick, Yarzebski Jorge, Lessard Darleen, Gore Joel M, Goldberg Robert J. Trends in atrial fibrillation complicating acute myocardial infarction. Am. J. Cardiol. 2009 Jul 15;104 (2):169–74. doi: 10.1016/j.amjcard.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Beattie J N, Soman S S, Sandberg K R, Yee J, Borzak S, Garg M, McCullough P A. Determinants of mortality after myocardial infarction in patients with advanced renal dysfunction. Am. J. Kidney Dis. 2001 Jun;37 (6):1191–200. doi: 10.1053/ajkd.2001.24522. [DOI] [PubMed] [Google Scholar]
- 57.Prevalence of chronic kidney disease and associated risk factors--United States, 1999-2004. MMWR Morb. Mortal. Wkly. Rep. 2007 Mar 02;56 (8):161–5. [PubMed] [Google Scholar]
- 58.Stinghen Andréa E M, Pecoits-Filho Roberto. Vascular damage in kidney disease: beyond hypertension. Int J Hypertens. 2011;2011 () doi: 10.4061/2011/232683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vaziri S M, Larson M G, Benjamin E J, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994 Feb;89 (2):724–30. doi: 10.1161/01.cir.89.2.724. [DOI] [PubMed] [Google Scholar]
- 60.Vaziri S M, Larson M G, Lauer M S, Benjamin E J, Levy D. Influence of blood pressure on left atrial size. The Framingham Heart Study. Hypertension. 1995 Jun;25 (6):1155–60. doi: 10.1161/01.hyp.25.6.1155. [DOI] [PubMed] [Google Scholar]
- 61.Mitchell Gary F, Vasan Ramachandran S, Keyes Michelle J, Parise Helen, Wang Thomas J, Larson Martin G, D'Agostino Ralph B, Kannel William B, Levy Daniel, Benjamin Emelia J. Pulse pressure and risk of new-onset atrial fibrillation. JAMA. 2007 Feb 21;297 (7):709–15. doi: 10.1001/jama.297.7.709. [DOI] [PubMed] [Google Scholar]
- 62.Aksnes Tonje Amb, Schmieder Roland E, Kjeldsen Sverre Erik, Ghani Sajda, Hua Tsushung Augie, Julius Stevo. Impact of new-onset diabetes mellitus on development of atrial fibrillation and heart failure in high-risk hypertension (from the VALUE Trial). Am. J. Cardiol. 2008 Mar 01;101 (5):634–8. doi: 10.1016/j.amjcard.2007.10.025. [DOI] [PubMed] [Google Scholar]
- 63.Ejerblad Elisabeth, Fored C Michael, Lindblad Per, Fryzek Jon, McLaughlin Joseph K, Nyrén Olof. Obesity and risk for chronic renal failure. J. Am. Soc. Nephrol. 2006 Jun;17 (6):1695–702. doi: 10.1681/ASN.2005060638. [DOI] [PubMed] [Google Scholar]
- 64.Flegal Katherine M, Carroll Margaret D, Ogden Cynthia L, Johnson Clifford L. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002 Oct 09;288 (14):1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 65.Gelber Rebecca P, Kurth Tobias, Kausz Annamaria T, Manson Joann E, Buring Julie E, Levey Andrew S, Gaziano J Michael. Association between body mass index and CKD in apparently healthy men. Am. J. Kidney Dis. 2005 Nov;46 (5):871–80. doi: 10.1053/j.ajkd.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 66.Kurukulasuriya L Romayne, Stas Sameer, Lastra Guido, Manrique Camila, Sowers James R. Hypertension in obesity. Endocrinol. Metab. Clin. North Am. 2008 Sep;37 (3):647–62, ix. doi: 10.1016/j.ecl.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 67.Wang Thomas J, Parise Helen, Levy Daniel, D'Agostino Ralph B, Wolf Philip A, Vasan Ramachandran S, Benjamin Emelia J. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004 Nov 24;292 (20):2471–7. doi: 10.1001/jama.292.20.2471. [DOI] [PubMed] [Google Scholar]
- 68.Iseki Kunitoshi, Tohyama Kazuyo, Matsumoto Tsuyoshi, Nakamura Hiroshi. High Prevalence of chronic kidney disease among patients with sleep related breathing disorder (SRBD). Hypertens. Res. 2008 Feb;31 (2):249–55. doi: 10.1291/hypres.31.249. [DOI] [PubMed] [Google Scholar]
- 69.Needleman Matthew, Calkins Hugh. The role of obesity and sleep apnea in atrial fibrillation. Curr. Opin. Cardiol. 2011 Jan;26 (1):40–5. doi: 10.1097/HCO.0b013e328341398e. [DOI] [PubMed] [Google Scholar]
- 70.McManus David D, Lyass Asya, Ingelsson Erik, Massaro Joseph M, Meigs James B, Aragam Jayashri, Benjamin Emelia J, Vasan Ramachandran S. Relations of circulating resistin and adiponectin and cardiac structure and function: the Framingham Offspring Study. Obesity (Silver Spring) 2012 Sep;20 (9):1882–6. doi: 10.1038/oby.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ix Joachim H, Sharma Kumar. Mechanisms linking obesity, chronic kidney disease, and fatty liver disease: the roles of fetuin-A, adiponectin, and AMPK. J. Am. Soc. Nephrol. 2010 Mar;21 (3):406–12. doi: 10.1681/ASN.2009080820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rufino Margarita, García Sagrario, Jiménez Alejandro, Alvarez Alejandra, Miquel Rosa, Delgado Patricia, Marrero Domingo, Torres Armando, Hernández Daniel, Lorenzo Victor. Heart valve calcification and calcium x phosphorus product in hemodialysis patients: analysis of optimum values for its prevention. Kidney Int. Suppl. 2003 Jun; (85):S115–8. doi: 10.1046/j.1523-1755.63.s85.27.x. [DOI] [PubMed] [Google Scholar]
- 73.Liu Yiwen, Shanahan Catherine M. Signalling pathways and vascular calcification. Front Biosci (Landmark Ed) 2011 Jan 01;16 ():1302–14. doi: 10.2741/3790. [DOI] [PubMed] [Google Scholar]
- 74.Das Manisha, Aronow Wilbert S, McClung John A, Belkin Robert N. Increased prevalence of coronary artery disease, silent myocardial ischemia, complex ventricular arrhythmias, atrial fibrillation, left ventricular hypertrophy, mitral annular calcium, and aortic valve calcium in patients with chronic renal insufficiency. Cardiol Rev. 2005 Dec 24;14 (1):14–7. doi: 10.1097/01.crd.0000148162.88296.9f. [DOI] [PubMed] [Google Scholar]
- 75.Verdiani Valerio, Lastrucci Vieri, Nozzoli Carlo. Worsening renal function in patients hospitalized with acute heart failure: risk factors and prognostic significances. Int J Nephrol. 2010 Oct 11;2011 () doi: 10.4061/2011/785974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Udani Suneel M, Koyner Jay L. The effects of heart failure on renal function. Cardiol Clin. 2010 Aug;28 (3):453–65. doi: 10.1016/j.ccl.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Patel Uptal D, Greiner Melissa A, Fonarow Gregg C, Phatak Hemant, Hernandez Adrian F, Curtis Lesley H. Associations between worsening renal function and 30-day outcomes among Medicare beneficiaries hospitalized with heart failure. Am. Heart J. 2010 Jul;160 (1):132–138.e1. doi: 10.1016/j.ahj.2010.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dhingra Ravi, Gaziano J Michael, Djoussé Luc. Chronic kidney disease and the risk of heart failure in men. Circ Heart Fail. 2011 Mar;4 (2):138–44. doi: 10.1161/CIRCHEARTFAILURE.109.899070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Spinar J, Ludka O, Dusek L, Vitovcova L, Sobotova D, Spinarova L, Tomandl J, Vitovec J. Neurohumoral activity, heart failure and prognosis in patients with end-stage renal disease treated by hemodialysis. Kidney Blood Press. Res. 2007;30 (5):347–57. doi: 10.1159/000107797. [DOI] [PubMed] [Google Scholar]
- 80.Stevenson W G, Stevenson L W. Atrial fibrillation in heart failure. N. Engl. J. Med. 1999 Sep 16;341 (12):910–1. doi: 10.1056/NEJM199909163411209. [DOI] [PubMed] [Google Scholar]
- 81.Seiler Jens, Stevenson William G. Atrial fibrillation in congestive heart failure. Cardiol Rev. 2009 Dec 17;18 (1):38–50. doi: 10.1097/CRD.0b013e3181c21cff. [DOI] [PubMed] [Google Scholar]
- 82.Witasp A, Carrero J J, Heimbürger O, Lindholm B, Hammarqvist F, Stenvinkel P, Nordfors L. Increased expression of pro-inflammatory genes in abdominal subcutaneous fat in advanced chronic kidney disease patients. J. Intern. Med. 2011 Apr;269 (4):410–9. doi: 10.1111/j.1365-2796.2010.02293.x. [DOI] [PubMed] [Google Scholar]
- 83.Ix Joachim H, Shlipak Michael G, Liu Haiying H, Schiller Nelson B, Whooley Mary A. Association between renal insufficiency and inducible ischemia in patients with coronary artery disease: the heart and soul study. J. Am. Soc. Nephrol. 2003 Dec;14 (12):3233–8. doi: 10.1097/01.asn.0000095642.25603.7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Masugata Hisashi, Senda Shoichi, Goda Fuminori, Yamagami Ayumu, Okuyama Hiroyuki, Kohno Takeaki, Hosomi Naohisa, Yukiiri Kazushi, Noma Takahisa, Imai Masanobu, Kiyomoto Hideyasu, Nishiyama Akira, Kohno Masakazu. Echocardiographic assessment of the cardio-renal connection: is left ventricular hypertrophy or diastolic function more closely correlated with estimated glomerular filtration rate in patients with cardiovascular risk factors? Clin. Exp. Hypertens. 2010 Jan;32 (2):113–20. doi: 10.3109/10641960902993145. [DOI] [PubMed] [Google Scholar]
- 85.Kimura Tomonori, Iio Ken-ichiro, Obi Yoshitsugu, Hayashi Terumasa. [Left ventricular hypertrophy in predialysis chronic kidney disease: impact of cardiomuscular stress markers]. Nihon Jinzo Gakkai Shi. 2007;49 (8):1007–13. [PubMed] [Google Scholar]
- 86.Mathenge R N, McLigeyo S O, Muita A K, Otieno L S. The spectrum of echocardiographic findings in chronic renal failure. East Afr Med J. 1993 Feb;70 (2):107–11. [PubMed] [Google Scholar]
- 87.Remuzzi Giuseppe, Perico Norberto, Macia Manuel, Ruggenenti Piero. The role of renin-angiotensin-aldosterone system in the progression of chronic kidney disease. Kidney Int. Suppl. 2005 Dec; (99):S57–65. doi: 10.1111/j.1523-1755.2005.09911.x. [DOI] [PubMed] [Google Scholar]
- 88.Korantzopoulos Panagiotis, Kolettis Theofilos, Kountouris Evaggelos, Siogas Konstantinos. Atrial remodeling in persistent atrial fibrillation: the potential role of aldosterone. Eur. Heart J. 2004 Jun;25 (12):1086; author reply 1086–7. doi: 10.1016/j.ehj.2003.12.033. [DOI] [PubMed] [Google Scholar]
- 89.Ehrlich Joachim R, Hohnloser Stefan H, Nattel Stanley. Role of angiotensin system and effects of its inhibition in atrial fibrillation: clinical and experimental evidence. Eur. Heart J. 2006 Mar;27 (5):512–8. doi: 10.1093/eurheartj/ehi668. [DOI] [PubMed] [Google Scholar]
- 90.Weber K T, Brilla C G, Janicki J S. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc. Res. 1993 Mar;27 (3):341–8. doi: 10.1093/cvr/27.3.341. [DOI] [PubMed] [Google Scholar]
- 91.Everett Thomas H, Olgin Jeffrey E. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm. 2007 Mar;4 (3 Suppl):S24–7. doi: 10.1016/j.hrthm.2006.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fukuda Yamato, Fukuda Nobuo, Morishita Satofumi, Tamura Yoshiyuki. Preventive effect of renin-angiotensin system inhibitor on left atrial remodelling in patients with chronic atrial fibrillation: long-term echocardiographic study. Eur J Echocardiogr. 2011 Apr;12 (4):278–82. doi: 10.1093/ejechocard/jeq193. [DOI] [PubMed] [Google Scholar]
- 93.Himmelfarb Jonathan. Uremic toxicity, oxidative stress, and hemodialysis as renal replacement therapy. Semin Dial. 2009 Dec 19;22 (6):636–43. doi: 10.1111/j.1525-139X.2009.00659.x. [DOI] [PubMed] [Google Scholar]
- 94.Hayden Melvin R, Goldsmith David, Sowers James R, Khanna Ramesh. Calciphylaxis: calcific uremic arteriolopathy and the emerging role of sodium thiosulfate. Int Urol Nephrol. 2008;40 (2):443–51. doi: 10.1007/s11255-008-9373-4. [DOI] [PubMed] [Google Scholar]
- 95.Sowers Kurt M, Hayden Melvin R. Calcific uremic arteriolopathy: pathophysiology, reactive oxygen species and therapeutic approaches. Oxid Med Cell Longev. 2010 Aug 19;3 (2):109–21. doi: 10.4161/oxim.3.2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Issac Tim T, Dokainish Hisham, Lakkis Nasser M. Role of inflammation in initiation and perpetuation of atrial fibrillation: a systematic review of the published data. J. Am. Coll. Cardiol. 2007 Nov 20;50 (21):2021–8. doi: 10.1016/j.jacc.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 97.Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo M A, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997 Aug 19;96 (4):1180–4. doi: 10.1161/01.cir.96.4.1180. [DOI] [PubMed] [Google Scholar]
- 98.Keller Christopher, Katz Ronit, Cushman Mary, Fried Linda F, Shlipak Michael. Association of kidney function with inflammatory and procoagulant markers in a diverse cohort: a cross-sectional analysis from the Multi-Ethnic Study of Atherosclerosis (MESA). BMC Nephrol. 2008 Aug 05;9 () doi: 10.1186/1471-2369-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fried Linda, Solomon Cam, Shlipak Michael, Seliger Stephen, Stehman-Breen Catherine, Bleyer Anthony J, Chaves Paolo, Furberg Curt, Kuller Lewis, Newman Anne. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J. Am. Soc. Nephrol. 2004 Dec;15 (12):3184–91. doi: 10.1097/01.ASN.0000146422.45434.35. [DOI] [PubMed] [Google Scholar]
- 100.Lee Shih-Huang, Chen Yao-Chang, Chen Yi-Jen, Chang Shih-Lin, Tai Ching-Tai, Wongcharoen Wanwarang, Yeh Hung-I, Lin Cheng-I, Chen Shih-Ann. Tumor necrosis factor-alpha alters calcium handling and increases arrhythmogenesis of pulmonary vein cardiomyocytes. Life Sci. 2007 Apr 17;80 (19):1806–15. doi: 10.1016/j.lfs.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 101.Yared J P, Starr N J, Torres F K, Bashour C A, Bourdakos G, Piedmonte M, Michener J A, Davis J A, Rosenberger T E. Effects of single dose, postinduction dexamethasone on recovery after cardiac surgery. Ann. Thorac. Surg. 2000 May;69 (5):1420–4. doi: 10.1016/s0003-4975(00)01180-2. [DOI] [PubMed] [Google Scholar]
- 102.Rahimi Kazem, Emberson Jonathan, McGale Paul, Majoni William, Merhi Amal, Asselbergs Folkert W, Krane Vera, Macfarlane Peter W. Effect of statins on atrial fibrillation: collaborative meta-analysis of published and unpublished evidence from randomised controlled trials. BMJ. 2011 Mar 16;342 () doi: 10.1136/bmj.d1250. [DOI] [PubMed] [Google Scholar]
- 103.Saso Srdjan, Vecht Joshua A, Rao Christopher, Protopapas Aristotle, Ashrafian Hutan, Leff Daniel, Darzi Ara, Athanasiou Thanos. Statin therapy may influence the incidence of postoperative atrial fibrillation: what is the evidence? Tex Heart Inst J. 2009;36 (6):521–9. [PMC free article] [PubMed] [Google Scholar]
- 104.Shiroshita-Takeshita Akiko, Brundel Bianca J J M, Burstein Brett, Leung Tack-Ki, Mitamura Hideo, Ogawa Satoshi, Nattel Stanley. Effects of simvastatin on the development of the atrial fibrillation substrate in dogs with congestive heart failure. Cardiovasc. Res. 2007 Apr 01;74 (1):75–84. doi: 10.1016/j.cardiores.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 105.Neumann Jutta, Ligtenberg Gerry, Klein Inge I, Koomans Hein A, Blankestijn Peter J. Sympathetic hyperactivity in chronic kidney disease: pathogenesis, clinical relevance, and treatment. Kidney Int. 2004 May;65 (5):1568–76. doi: 10.1111/j.1523-1755.2004.00552.x. [DOI] [PubMed] [Google Scholar]
- 106.Neumann Jutta, Ligtenberg Gerry, Klein Inge H T, Boer Peter, Oey P Liam, Koomans Hein A, Blankestijn Peter J. Sympathetic hyperactivity in hypertensive chronic kidney disease patients is reduced during standard treatment. Hypertension. 2007 Mar;49 (3):506–10. doi: 10.1161/01.HYP.0000256530.39695.a3. [DOI] [PubMed] [Google Scholar]
- 107.McManus David, Shlipak Michael, Ix Joachim H, Ali Sadia, Whooley Mary A. Association of cystatin C with poor exercise capacity and heart rate recovery: data from the heart and soul study. Am. J. Kidney Dis. 2007 Mar;49 (3):365–72. doi: 10.1053/j.ajkd.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Habicht Antje, Watschinger Bruno. [Sympathetic overactivity and the kidney]. Wien. Klin. Wochenschr. 2003 Sep 30;115 (17-18):634–40. doi: 10.1007/BF03040468. [DOI] [PubMed] [Google Scholar]
- 109.Haïssaguerre M, Jaïs P, Shah D C, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Métayer P, Clémenty J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 1998 Sep 03;339 (10):659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 110.Severi Stefano, Pogliani Daniela, Fantini Giulia, Fabbrini Paolo, Viganò Maria Rosa, Galbiati Eleonora, Bonforte Giuseppe, Vincenti Antonio, Stella Andrea, Genovesi Simonetta. Alterations of atrial electrophysiology induced by electrolyte variations: combined computational and P-wave analysis. Europace. 2010 Jun;12 (6):842–9. doi: 10.1093/europace/euq042. [DOI] [PubMed] [Google Scholar]
- 111.Chen Szu-Chia, Chang Jer-Ming, Liu Wan-Chun, Huang Jiun-Chi, Tsai Jer-Chia, Lin Ming-Yen, Su Ho-Ming, Hwang Shang-Jyh, Chen Hung-Chun. Echocardiographic parameters are independently associated with increased cardiovascular events in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2012 Mar;27 (3):1064–70. doi: 10.1093/ndt/gfr407. [DOI] [PubMed] [Google Scholar]
- 112.Hermida José, Lopez Faye L, Montes Ramón, Matsushita Kunihiro, Astor Brad C, Alonso Alvaro. Usefulness of high-sensitivity C-reactive protein to predict mortality in patients with atrial fibrillation (from the Atherosclerosis Risk In Communities [ARIC] Study). Am. J. Cardiol. 2012 Jan 01;109 (1):95–9. doi: 10.1016/j.amjcard.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang Thomas J, Massaro Joseph M, Levy Daniel, Vasan Ramachandran S, Wolf Philip A, D'Agostino Ralph B, Larson Martin G, Kannel William B, Benjamin Emelia J. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003 Aug 27;290 (8):1049–56. doi: 10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 114.Go Alan S, Hylek Elaine M, Chang Yuchiao, Phillips Kathleen A, Henault Lori E, Capra Angela M, Jensvold Nancy G, Selby Joe V, Singer Daniel E. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003 Nov 26;290 (20):2685–92. doi: 10.1001/jama.290.20.2685. [DOI] [PubMed] [Google Scholar]
- 115.Recurrent Torsades de Pointes After Sotalol Therapy for Symptomatic Paroxysmal Atrial Fibrillation in a Patient with End-Stage Renal Disease. J. Cardiovasc. Pharmacol. Ther. 1999 Apr;4 (2):129–134. doi: 10.1177/107424849900400208. [DOI] [PubMed] [Google Scholar]
- 116.Chan Kevin E, Lazarus J Michael, Hakim Raymond M. Digoxin associates with mortality in ESRD. J. Am. Soc. Nephrol. 2010 Sep;21 (9):1550–9. doi: 10.1681/ASN.2009101047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Naruse Yoshihisa, Tada Hiroshi, Sekiguchi Yukio, Machino Takeshi, Ozawa Mahito, Yamasaki Hiro, Igarashi Miyako, Kuroki Kenji, Itoh Yoko, Murakoshi Nobuyuki, Yamaguchi Iwao, Aonuma Kazutaka. Concomitant chronic kidney disease increases the recurrence of atrial fibrillation after catheter ablation of atrial fibrillation: a mid-term follow-up. Heart Rhythm. 2011 Mar;8 (3):335–41. doi: 10.1016/j.hrthm.2010.10.047. [DOI] [PubMed] [Google Scholar]
- 118.Bohnen Marius, Stevenson William G, Tedrow Usha B, Michaud Gregory F, John Roy M, Epstein Laurence M, Albert Christine M, Koplan Bruce A. Incidence and predictors of major complications from contemporary catheter ablation to treat cardiac arrhythmias. Heart Rhythm. 2011 Nov;8 (11):1661–6. doi: 10.1016/j.hrthm.2011.05.017. [DOI] [PubMed] [Google Scholar]


