Abstract
We present a rare complication of cardiac arrest from asystole in the setting of prolonged endoscopic retrograde cholangiopancreatography(ERCP) procedure. Cardiopulmonary complications of ERCP are rare but can be fatal. Therefore it is essential to closely monitor the patient during ERCP. Immediate access to resuscitation equipment facilitating prompt intervention in the unlikely event of fatal cardiovascular collapse should be a part of standard ERCP protocol to ensure life threatening complications are appropriately managed.
Keywords: Cardiac Asystole, Endoscopic Retrograde Cholangiopancreatography
Introduction
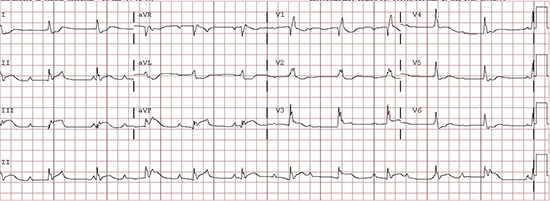
A 70 year old female with non obstructive coronary artery disease, hypertension, hyperlipidemia underwent endoscopic spincterotomy and biliary stent placement for papillary stenosis. Follow up studies revealed migration of the stent to right hepatic duct. The patient was then scheduled for repeat endoscopic retrograde cholangiopancreatography (ERCP) for stent removal. Her home medications included aspirin 81 mg daily, amlodipine 5 mg daily, simvastatin 20 mg daily and multivitamins. Laboratory studies revealed low levels of serum potassium (3.4 mmol/L (normal 3.5-5.1 mmol/L). Remaining tests were unremarkable. Baseline electrocardiogram revealed sinus rhythm with left bundle branch block (LBBB) pattern (Figure 1). She did not take any home medications on the day of procedure. She did not have any oral intake for 12 hours prior to the procedure. Induction of anesthesia and intubation were uneventful (150 mg of propofol, 100 mg of lidocaine and 100 mg of succinylcholine). Initially the patient was hemodynamically stable. Thirty minutes into the procedure as the biliary stent was being extracted, the patient became bradycardic (heart rate dropped from 52 to 32 beats per minute) and hypotensive. The end tidal carbon dioxide levels dropped from 30 to 10 mm Hg and rhythm changed from severe bradycardia changed to asystole (Figure 2). Cardiopulmonary resuscitation was initiated using ACLS protocol. The patient went into pulseless electrical activity. After three 1 mg doses of epinephrine and 50 mEq of intravenous sodium bicarbonate, spontaneous perfusion was restored. Electrocardiogram (ECG) showed complete atrio-ventricular block with ventricular rate of 66 beats per minute and ST segment elevation in leads III and avF with reciprocal changes in lateral leads(Figure 3). The patient was emergently transferred to cardiac catheterization laboratory. Temporary transvenous pacemaker was placed and cardiac catheterization showed moderate disease in right coronary artery and 1st diagonal branch of left anterior descending artery. Computed tomography angiogram did not reveal any evidence of pulmonary embolism. Two-dimensional echocardiogram showed left ventricular ejection fraction of 35% and septal hypokinesis. Serum electrolytes were unremarkable apart from low serum potassium (3.2 mmol/L). The patient was closely monitored in intensive care unit. Third-degree atrioventricular block resolved spontaneously and transvenous pacemaker was removed next day. The patient was successfully extubated on the fourth day after the procedure. Rest of the hospital stay was uneventful.
Figure 1. Electrocardiogram showing sinus rhythm with left bundle branch block pattern .
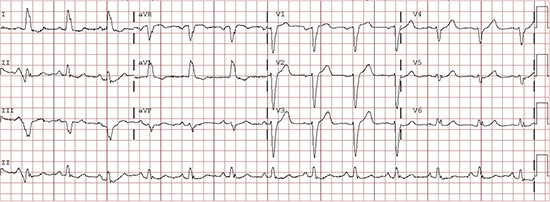
Figure 2. Electrocardiogram showing asystole.
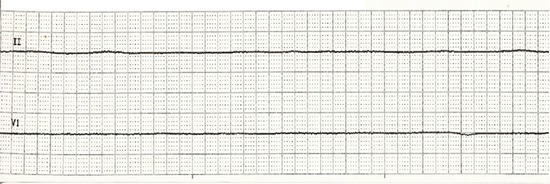
Figure 3. Electrocardiogram showing complete atrio-ventricular (AV) block with ventricular rate of 66 beats per minute and ST segment elevation in leads III and avF with reciprocal changes in lateral leads.
Discussion
We describe a patient with non-ischemic cardiomyopathy who developed a vasovagal event which led to asystole during a prolonged procedure under anesthesia. Case reports describing sudden cardiac arrest during ERCP due to possible air embolism have been published in the past.[1,2] Goins et al[3] described a case of 72-year-old lady who developed pulseless electrical activity during ERCP. Emergent trans-esophageal echocardiogram revealed large amount of air in the right ventricle, which was immediately aspirated with a pulmonary artery catheter and spontaneous circulation was restored. However, in our patient neither computed tomography angiogram nor echocardiography showed any trapped air. Heart block with propofol administration in a 9-year-old child has also been reported.[4] Propofol may have contributed to bradycardia in our patient. Supra-physiologic activation of sensory nerve endings of vagal nerve by prolonged ERCP manipulation may have resulted in intense vagal tone leading to bradycardia. Gonclaves described a patient who developed pulseless electrical activity leading to asystole during prolonged ERCP procedure(60 minutes).[05] Our patient had severe left ventricular dysfunction (EF 35% and LBBB, non -ischemic). The combination of impaired LV function, prolonged ERCP procedure and sedation probably resulted in bradycardia which led to cardiac asystole. EKG changes noted following resuscitation were most likely due to the non-significant RCA lesion which became significant in the setting of profound hypotension and use of epinephrine. In summary, we describe a rare complication of cardiac arrest from asystole in the setting of prolonged ERCP. In this case, cardiopulmonary resuscitation was immediately initiated and the patient survived without neurological deficits.
Conclusions
Cardiopulmonary complications of ERCP are rare but can befatal. Therefore it is essential to closely monitor the patient during ERCP. Immediate access to resuscitation equipment facilitating prompt intervention in the unlikely event of fatal cardiovascular collapse should be a part of standard ERCP protocol to ensure life threatening complications are appropriately managed.
Disclosures
None.
References
- 1.Bisceglia Michele, Simeone Anna, Forlano Rosario, Andriulli Angelo, Pilotto Alberto. Fatal systemic venous air embolism during endoscopic retrograde cholangiopancreatography. Adv Anat Pathol. 2009 Jul;16 (4):255–62. doi: 10.1097/PAP.0b013e3181aab793. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy C, Larvin M, Linsell J. Fatal hepatic air embolism following ERCP. Gastrointest. Endosc. 1997 Feb;45 (2):187–8. doi: 10.1016/s0016-5107(97)70246-3. [DOI] [PubMed] [Google Scholar]
- 3.Goins K M, May J M, Hucklenbruch C, Littlewood K E, Groves D S. Unexpected cardiovascular collapse from massive air embolism during endoscopic retrograde cholangiopancreatography. Acta Anaesthesiol Scand. 2010 Mar;54 (3):385–8. doi: 10.1111/j.1399-6576.2009.02144.x. [DOI] [PubMed] [Google Scholar]
- 4.Sochala C, Deenen D, Ville A, Govaerts M J. Heart block following propofol in a child. Paediatr Anaesth. 1999;9 (4):349–51. doi: 10.1046/j.1460-9592.1999.00373.x. [DOI] [PubMed] [Google Scholar]
- 5.Gonçalves D. Endoscopic procedure hazard--vagovagal syncope with heart standstill due to ERCP. Arq Gastroenterol. 1979 Oct 1;16 (4):200–2. [PubMed] [Google Scholar]


