Abstract
Due to several unfavorable epidemiological changes, chronic kidney disease (CKD) and treatment of its associated cardiovascular morbidity have become a worldwide problem. Thus, atrial fibrillation (AF) is the most common arrhythmia and frequently associated with renal impairment: prevalence for AF is up to 27% in long-term hemodialysis patients and in general more than 25% in all CKD patients 70 years and older. Thromboembolism and stroke are the major complications of AF. Two-year death rates for CKD patients after stroke range between 55% and 74%. Although treatment of AF in the general population is well defined, patients with CKD and AF are often undertreated due to lack of studies and guidelines. In this review recent data concerning incidence and prevalence of AF, stroke, and major bleedings in CKD patients are presented. Particular attention is paid to the available data about the different types of oral anticoagulation therapy with regard to CKD stage, including the new oral anticoagulant drugs dabigatran, rivaroxaban, and apixaban. Stratification algorithms for stroke risk in general, and individualized risk stratification for oral anticoagulation in CKD patients are discussed in detail.
Introduction
Chronic kidney disease (CKD), defined by the presence of either reduced estimated glomerular filtration rate (eGFR) and/or albuminuria/proteinuria,[1] affects currently about 30 million patients in the US.[2] Upon these, more than 530,000 CKD patients suffer from end-stage renal disease (ESRD) requiring renal replacement therapy, over 370,000 receive chronic dialysis.[2] As the population ages, the incidence for CKD and its risk factors, such as hypertension and diabetes mellitus, and the prevalence for CKD, ESRD, and its concomitant diseases will further increase[3] and become a global challenge.[4] Despite this unfavorable epidemiological development, data about associated risks and treatment strategies in CKD are limited yet and left many open issues. This concerns especially the most common arrhythmia in CKD which is atrial fibrillation.
Cardiovascular Events and CKD
It is well known that patients with CKD are more prone to develop coronary heart disease, chronic heart failure, peripheral artery disease, and venous thromboembolism independent of other risk factors.[5-8] CKD is also a key risk factor for cardiocerebrovascular events as stroke, and is associated with other important stroke risk factors such as diabetes mellitus, myocardial hypertrophy, hypertension-and atrial fibrillation.[9] Other key players which are altered by CKD, such as the renin-angiotensin-aldosterone system and sympathetic activation, have also been found to trigger AF.[8]
Atrial Fibrillation
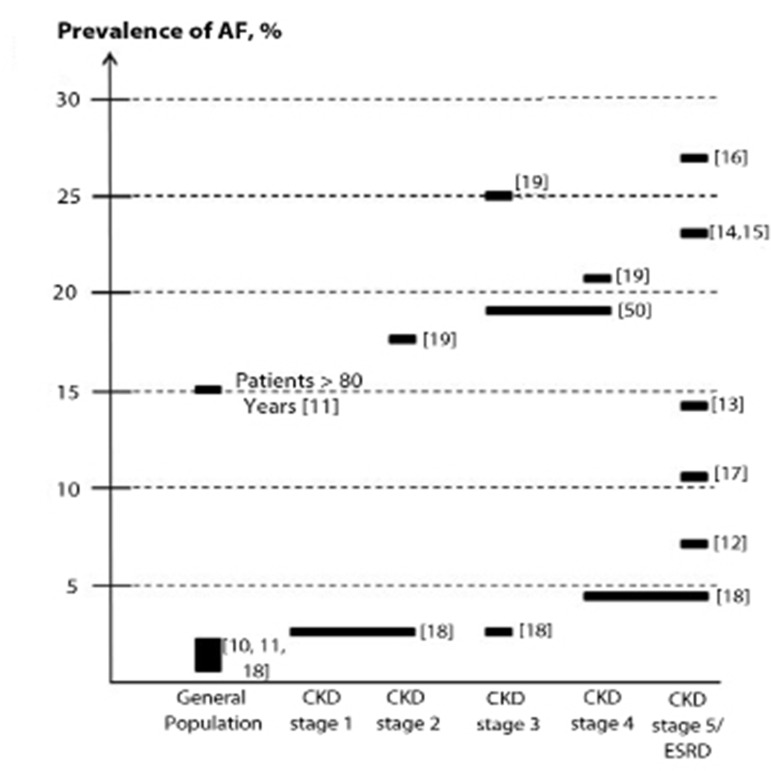
In general, the prevalence of AF increases with age: whereas about 0.4 - 2.0% in the general population suffer from atrial fibrillation, the prevalence rises up to 15% in patients over 80 years.[10,11] Regarding solely hemodialysis patients, the prevalence of AF is significantly higher: thus, possibly 7% up to 27% of ESRD patients suffer from AF [12-17] (figure 1).
Figure 1. Prevalence of atrial fibrillation is shown in the general population, and in patients with different stages of chronic kidney disease (CKD) including end-stage renal disease (ESRD). In some studies, different stages are pooled together which is indicated by wider srectangles above the CKD stages. CKD stage 1: eGFR ≥ 90 ml/min/1.73m2; CKD stage 2: eGFR 60-89 ml/min/1.73m2; CKD stage 3: eGFR 30-59 ml/min/1.73m2; CKD stage 4: eGFR 15-29 ml/min/1.73m2; CKD stage 5: eGFR <15 ml/min/1.73m2.
One recent epidemiological study with 26,917 US patients who were categorized by renal function demonstrated that CKD, regardless of its stage, was associated with a higher risk for AF: the prevalence for AF in patients with CKD stage 1 to 2 (eGFR ≥ 60 ml/min/1.73 m2 with albuminuria), CKD stages 3 (eGFR 30 to 59 ml/min/1.73 m2) and CKD stage 4 to 5 (eGFR < 30 ml/min/1.73 m2) was 2.8%, 2.7 % and 4.2%, respectively, compared to only 1.0% in patients without CKD.[18]
Soliman et al.[19] reported a prevalence for AF of more than 25% in CKD patients 70 years and older, but found no association of the development of AF with hypertension or diabetes. Another retrospective study with 1,010 consecutive CKD patients from two community-based hospitals found also a much higher prevalence for AF even at mild renal impairment: 17.9% of patients with CKD stage 2 (eGFR 60 to 89 ml/min/1.73m2), 25.2 % of CKD stage 3 patients (eGFR 30 to 59 ml/min/1.73 m2) and 20.8% of CKD stage 4 patients (eGFR 15 to 29 ml/min/1.73 m2) had AF.[20]
Interestingly, CKD appears to increase the risk of new onset of AF as well as AF increases the risk of developing renal disease. This bidirectional association was described for a large prospective community-based observational cohort study of 235,818 individuals in Japan. Therein, the hazard ratio for the development of AF were 1.32 for patients with eGFR of 30 to 59 ml/min/1.73m2, and 1.57 for patients with eGFR <30 ml/min/1.73m2 compared to patients with an eGFR>60 ml/min/1.73m2. Vice versa, in patients with atrial fibrillation at entry, the hazard ratio for the development of kidney dysfunction was 1.77. Interestingly, both associations remained significant independent of any existence or treatment of the concomitant comorbidities hypertension or diabetes mellitus.[21] The bidirectionalassociation between CKD and AF cannot simply be explained by increased mechanical stress in the atrium as a result of hypertension and high atrial pressure. There have to be other pathophysiologicprocesses which play a role in the development and perpetuation of both CKD and AF, e.g. inflammatory processes, and the renin-angiotensin-aldosteron system activation.
Thromboembolic Risk
Patients with AF have an increased risk for thromboembolism and therefore for transient ischemic attacks as well as ischemic strokes. Blood stasis in the left atrium and its appendage, endothelial injury of the vessel wall, and hypercoagulation, known as Virchow’s triad, contribute to thrombogenesis and the risk for thromboembolism.[22] Patients with renal impairment but with no AF are also at increased risk for thromboembolic events because of altered hemostasis, atherosclerosis and endothelial damage, altered protein C metabolism, increased levels of lipoprotein(a) and therefore inhibition of plasmin, as well as defects in the expression of glycoprotein GPIb.[9,23] Therefore, patients with AF and CKD are even more at advanced risk for stroke, and treatment with oral anticoagulation represents an important therapeutic option.
Stroke
Stroke is the major complication in patients with AF, and especially in CKD, too. Its incidence increases as kidney function declines. A Japanese community-based longitudinal observational study with 1,977 individuals showed that the hazard ratio for first symptomatic stroke was 1.9 for patients with creatinine clearance (CrCl) between 40 and 70 ml/min and 3.1 for patients with CrCl < 40 ml/min compared to patients with CrCl > 70 ml/min/[24]. The US Renal Data System report the stroke incidence to be 15.1 % in hemodialysis patients and 9.6 % in patients with less severe CKD compared to 2.6% in patients without CKD.[25]
The association of CKD with increasing risk of stroke was also proven by another Japanese study of 11.780 individuals. In patients with normal eGFR (≥ 90 ml/min) stroke occurred in 4.3% of men and 2.4% of women, whereas in patients with CKD, characterized by an eGFR < 60 ml/min, 13.1% of men and 7.6% of women experienced a stroke event. Men had a higher risk of hemorrhagic stroke and women of ischemic stroke. Furthermore, regularalcohol consumption markedly increased the rate of hemorrhagic stroke both in men and in women with CKD (5.3% and 6.1%, respectively) compared to never-drinkers with CKD (0.7% and 1.7%, respectively) and never-drinker without CKD (1.1% and 1.5%, respectively.[26] This is an important finding, since the amount of consumed alcohol was substantially lower than the current recommendation suggests for cardiocerebrovascular protection. Thus, in patients with CKD, mild to moderate alcohol consumption was associated with a higher risk for hemorrhagic stroke, at least in the Asian population. A strict alcohol prohibition for Asian patients with eGFR < 60ml/min might reduce the rate of hemorrhagic stroke.[27] Whether CKD independently increases the risk for ischemic stroke in patients with AF was investigated by Go et al. in the ATRIA study.[28] None of the included patients was treated with anticoagulation. With decreasing eGFR a graded, increased risk of stroke was proven: after adjustment for known risk factors for stroke, the hazard ratio was 1.16 for patients with eGFR between 45 and 59 ml/min/1.73m2, and 1.39 for patients with eGFR < 45 ml/min/1.73m[2] compared to patients with eGFR ≥ 60 ml/min/1.73m2.
In a meta-analysis of 21 articles, the relative risk for incident stroke was 1.43 (95% CI 1.31-1.57, P<0.001) among patients with an eGFR < 60 ml/min/1.73 m2 compared to patients with normal baseline eGFR.[29]
Vazques et al.[30] described a 9.8 fold increased risk for ischemic stroke in hemodialysis patients suffering from AF compared to hemodialysis patients who maintained sinus rhythm. In the Rotterdam study,[31] risk of hemorrhagic stroke was elevated with decreasing GFR, but not the risk of ischemic stroke.
In contrast, an Italian study with 476 hemodialysis patients did not find any significant differences in stroke rates regardless of AF or sinus rhythm.[32]
Differences in the various study results may be explained by different ages of the studied population, different length of follow-up, differences in the type and documentation of detected AF and anticoagulation treatment.[23]
Mortality
The direct impact of atrial fibrillation on the mortality rate of CKD patients is difficult to assess since there is a strong association between AF with structural heart disease.[9] In CKD patients, the risk of death increases as renal function declines.[5,6] In the large Kaiser Permanente Renal Registry, the adjusted hazard ratio for death was 1.2 fold higher in patients with eGFR between 45 and 59 ml/min/1.73m2 compared to patients with eGFR >59 ml/min/1.73m2 and rose to a 5.9 fold increase in patients with eGFR < 15 ml/min/1.73m2.[6]
Patients on hemodialysis suffering from AF were reported to have an annual mortality of 5% compared with only 2% in those without AF.[33]
One other longitudinal, single-center study with 190 individuals reported a dramatically increased four-year mortality rate of 81% in patients with AF and ESRD compared to 29% in patients without AF.[34] After a stroke, the cumulative two-year mortality rate for patients with CKD or ESRD is raised to 55% and 74%, respectively, whereas patients without CKD have a two-year mortality rate of 28%. Even after TIA, the cumulative two-year mortality rate for patients with CKD or ESRD is also significantly increased (41% and 62%; respectively) compared to patients with normal renal function (15%) .[25]
Major Bleeding
Patients with CKD and especially those with ESRD show an increased tendency for bleeding events especially from the gastrointestinal tract. Pathophysiological processes include altered platelet function and von Willebrand factor, reduced intracellular ADP and serotonin, enhanced intracellular cAMP and abnormal mobilization of platelet Ca2+ as well as abnormal platelet arachidonic acid metabolism.[9]
Gastrointestinal bleeding occurs markedly more often and is associated with higher mortality in renal patients: in ESRD patients, upper gastrointestinal bleeding accounts for 3-7% of all deaths.[23]
The risk for bleeding especially when taking oral anticoagulation increases as the degree of CKD worsens. In an analysis of a prospective cohort of 578 CKD patients treated with warfarin, the risk of major hemorrhage in patients with severe CKD (eGFR <30 ml/min/1.73 kg/m2) was 2.4-fold higher than that of patients with milder CKD.[35]
With regard to atrial fibrillation, anticoagulation therapy is used to reduce the thrombotic risk. A small single-center report of ESRD patients with AF showed that the relative risk of bleeding for dialysis patients on oral anticoagulation was 2.36 compared to the dialysis group not treated with anticoagulation; in contrast to the rate of 12.8 % with bleeding events in patients without anticoagulation, none of the bleeding events in the oral anticoagulation group was fatal.[36]
Outcomes with Oral Anticoagulation Depending on CKD Stage
CKD stage 2 and 3 (eGFR between 90 and 29 ml/min/1.73 m2): To our knowledge there are no studies investigating the risk for stroke under warfarin versus placebo or versus antiplatelet medication in patients with light to moderate renal impairment and AF.
There is only one study which examines the incidence of thromboembolic stroke in patients with all (including the above) stages of CKD and AF treated with or without warfarin[37] (table 1). Independent of CKD stage, therein thromboembolic stroke occurred in 9% of patients treated with warfarin and 26% of patients without anticoagulation (P<0.001). The incidence of stoke in patients with CKD stage 2 and 3 under warfarin was half that of patients without warfarin (10% resp. 20%, P<0.05). Major bleeding was slightly but insignificantly increased in patients under warfarin treatment.
Table 1. Studies of Warfarin in CKD and Dialysis Patients.
USRDS DMMS indicates United States Renal Data System Dialysis Morbidity and Mortality Study; ANZDATA, Australia and New Zealand Dialysis and Transplant Registry; DOPPS, Dialysis Outcomes and Practice Patterns Study; AF, atrial fibrillation; INVOR, Incident Dialysis Patients in Vorarlberg; HR, hazard ratio; CI, confidence interval;
| Study (year, design) | Included CKD stages | Number of patients | Average follow-up | Results |
|---|---|---|---|---|
| 2001, retrospective study [47] | Hemodialysis patients | 430patients overall 61 (14.2%) with chronic AF 96 (22.3%) on warfarin or aspirin for various reasons |
Study covers a 22 year period | Overall incidence for stroke in dialysis patients was 3.78/100 patient-years. In patients on antithrombotic therapy (aspirin or warfarin) the overall rate of stroke was 8.33/100 patients-years compared to patients without antithrombotic therapy (2.6/100 patients-years, p=0.0002). Patients with AF and on warfarin or aspirin had a higher risk for stroke (4.46/100 patients-years) than AF patients without anticoagulation (1.0/100 patient-years). |
| 2003, retrospective cohort study using data of USRDS DMMS Wave II [48] | Dialysis patients | 3,374 patients overall
123 (3.6%) with newly diagnosed AF during follow-up 198 (5.9%) on warfarin, 10 of those for AF treatment |
2.92 ± 1.14 years | Baseline use of warfarin was associated with a lower risk of mortality after hospitalization for AF. |
| 2003, retrospective study [36] | Hemodialysis or peritoneal dialysis patients | 240 patients overall 29 (12.1%) on coumarin derivatives (warfarin), 7 of them with AF |
20 month for coumarin subgroup 21 month for non-coumarin subgroup | The relative risk for bleeding under coumarin was 2.36 (95% CI, 1.19-4.27) compared to the non-coumarin subgroup. The risk for bleeding in the coumarin subgroup was mainly in the digestive tract, no bleeding event was fatal. |
| 2007, retrospective study using data from ANZDATA [49] | Hemodialysis patients | 155 patients overall 40 (25.8%) with AF, 5 of them taking warfarin 11 (27.5%) on warfarin, 5 of them for AF treatment |
25.5 ± 8.4 months | No statistical significant difference in the incidence of cerebrovascular events or major hemorrhage between 1. patients taking warfarin and patients off warfarin. 2. the AF and the non-AF subgroup. Incidence of major hemorrhage was over three times that of cerebrovascular events in the whole population as well as in the AF and non-AF subgroup. |
| 2008, prospective multicenter study [32] | Hemodialysis patients | 476 patients overall 127 (26.7%) with preexisting AF 31 (24.4%) of the AF patients taking anticoagulation (warfarin) at enrollment |
3 years | No difference in stroke incidence in patients with AF compared to no-AF patients (15.4% vs. 12.4%, P=0.4) |
| 2009, retrospective study [41] | Hemodialysis patients | 1,671 patients overall with preexisting AF 508 (30.4%) patients on warfarin only 239 (14.3%) patients on warfarin and either clopidogrel or aspirin 480 (28.7%) patients on no anticoagulation or antiplatelet therapy |
1.6 years (maximum 5 years) | Warfarin doubles the risk for stoke (HR = 2.00; 95% CI 1.34-2.99, P = 0.001) compared to non-warfarin use. There was a positive relationship between increasing INR and increasing risk of stroke, which the highest risk for patients with no INR monitoring. |
| 2009, observational retrospective study [37] | CKD stage 3 CKD stage 4 CKD stage 5 Hemodialysis patients |
399 patients overall with AF 232 on warfarin, 167 without warfarin CKD stage 3: 115 (50%) on warfarin; 85 (51%) without warfarin CKD stage 4: 39 (17%) on warfarin, 28 (17%) without warfarin CKD stage 5: 78 (34%) on warfarin, 54 (32%) without warfarin Hemodialysis: 51 (22%) on warfarin, 42 (25%) without warfarin |
31 ± 34 months follow-up for patients on warfarin; 23 ± 30 months follow-up for patients without warfarin | Warfarin significantly reduced the incidence of new thromboembolic stroke in all investigated CKD stages and hemodialysis patients (CKD stage 3: 10% on warfarin vs. 20% without warfarin, P<0.05; CKD stage 4. 5% vs. 21%, P<0.05; CKD stage 5: 10% vs. 37%, P<0.001; hemodialysis: 10% vs 38%, P<0.005). |
| 2010, retrospective study using data from DOPPS [42] | Hemodialysis patients | 17,513 patients overall 2,188 patients with atrial fibrillation 350 (16%) of the AF patients taking warfarin |
Not reported | Warfarin use was associated with significantly higher stroke risk in patients > 75 yrs (HR = 2.17; 95% CI=1.04-4.53, P=0.04). |
| 2011, prospective single-center observational cohort study (INVOR)[46] | Incident dialysis patients | 235 patients overall 12 (5.1%) patients with AF at start of dialysis 40 (17.0%) patients with newly diagnosed AF during follow-up 46 (19.6%) patients under warfarin treatment, 30 (65.2%) of them for AF |
2.84 years | No stroke or fatal bleeding events occurred in patients under sufficient oral anticoagulation. The mortality risk for AF patients on warfarin was slightly, but not significantly lower than for patients without AF and without anticoagulation therapy (reference group). AF patients with contraindication for warfarin had a significantly higher mortality risk compared to the reference group (HR: 3.9, 95% CI=2.16-7.04, P<0.001) |
Three recent phase 3 studies compared new anticoagulant drugs to warfarin concerning safety and efficacy (table 2). In the RE-LY trial, the direct thrombin inhibitor dabigatran was given at two different doses (110 mg and 150 mg) twice daily; AF patients with CrCl of at least 30 ml/min were included. The lower dose was associated with comparable rates of stroke, systemic embolism, and major bleeding events to those under warfarin. The higher dabigatran dose was superior to warfarin in preventing stroke. Concerning patients with CrCl <50 ml/min, between 50 and 79 ml/min, and ≥80 ml/min, there was no significant difference in the treatment benefit of the studied anticoagulants.[38]
Table 2. Trials of oral anticoagulation in CKD.
RE-LY: Randomized Evaluation of Long-Term Anticoagulation Therapy; ROCKET AF: Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation; ARISTOTLE: Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation; INR:international normalized ratio; CrCl: creatinine clearance Numbers in bold represent significant differences of the investigated medication compared to warfarin. a: for non-inferiority; b: for superiority
| RE-LY [38] | ROCKET AF [39] | ARISTOTLE [40] | |
|---|---|---|---|
| Drug | Dabigatran etexilate | Rivaroxaban | Apixaban |
| Study design | Phase 3, multicenter, prospective, open-label randomized trial: 18,113 patients with AF and one additional risk factor for stroke | Phase 3, multicenter, double-blind, double-dummy randomized trial: 14,264 patients with AF and elevated stroke risk | Phase 3, multicenter, double-blind, double-dummy randomized trial: 18,201 patients with AF and at least one additional risk factor for stroke |
| Dosage | 110 mg resp. 150 mg dabigatran etexilate twice daily versus warfarin adjusted to an INR of 2.0 to 3.0 | 20 mg rivaroxaban per day resp. 15 mg/day rivaroxaban for patients with CrCl 30-49 ml/min versus warfarin adjusted to an INR of 2.0 to 3.0 | 5 mg apixaban twice daily resp. 2.5 mg apixaban twice daily for patients with serum creatinine ≥ 1.5 mg/dl (approx. CrCl ≤ 50 ml/min) versus warfarin adjusted to an INR of 2.0 to 3.0 |
| Antiplatelet agents | Aspirin ≤100 mg per day Clopidogrel Ticlopidine Dipyridamole ASA/Dipyridamole | Aspirin ≤100 mg per day | Aspirin ≤165 mg per day Clopidogrel |
| Investigated CKD stages | CrCl <50 ml/min CrCl 50 - 79 ml/min CrCl ≥ 80 ml/min | CrCl 30 - 49ml/mg CrCl ≥ 50ml/min | CrCl ≤ 30 ml/min CrCl 30 - 50 ml/min CrCl <50 – 80 ml/min CrCl > 80 ml/min |
| Exclusion criteria with regard to creatinine clearance | <30 ml/min | <30 ml/min | <25 ml/min |
| Study Outcomes Primary efficacy outcome Primary safety outcome Secondary efficacy outcome |
|
|
|
| Study Results | |||
| Primary efficacy outcome | Dabigatran Warfarin 110 mg: 1.53%/yra 1.69%/yr 150 mg: 1.11%/yra,b | Rivaroxaban Warfarin 15 mg: 2.32%/yr 2.77%/yr 20 mg: 1.57 %/yr 2.00%/yr | Apixaban Warfarin 1.27%/yra,b 1.60%/yr |
| Primary safety outcome | Dabigatran 110 mg: 2.71%/yra Warfarin 150 mg: 3.11%/yr 3.36%/yr | Rivaroxaban Warfarin 15 mg: 17.82%/yr 18.28%/yr 20 mg: 14.24%/yr 13.67%/yr | Apixaban Warfarin 2.13%/yr 3.09%/yr |
| Secondary efficacy outcome | Mortality Rate: | ||
| Dabigatran Warfarin 110 mg: 3.75%/yr 4.13%/yr 150 mg: 3.64%/yr | Rivaroxaban Warfarin 15 mg: 5.58%/yr 6.54%/yr 20 mg: 3.55%/yr 4.16%/yr | Apixaban Warfarin 3.52%/yr 3.94%/yr | |
| Outcome with regard to CKD | No significant difference in the treatment effect could be observed in patients with renal impairment | Patients with moderate renal impairment (CrCl <50ml/min) have higher rates of stroke and bleeding under both rivaroxaban and warfarin compared to patients with normal renal function. No superiority or non-inferiority of rivaroxaben versus warfarin could be demonstrated for patients with CrCl 30-49 ml/min | Patients with moderate to severe renal impairment (CrCl ≤50 ml/min) showed an even greater reduction in major bleeding events under apixaban compared to warfarin. |
Rivaroxaban, a novel factor Xa inhibitor, was tested at two different doses depending on creatinine clearance against warfarin in the ROCKET-AFstudy39 (table 2). Patients with AF and CrCl ≥ 30 ml/min were included. The efficacy results showed that slightly but not significantly less stroke and systemic embolism events occurred in the rivaroxaban groups than in the warfarin group. Compared to warfarin there was no excess bleeding on rivaroxaban.
In the ARISTOTELE trial, another direct factor Xa inhibitor, apixaban, was studied versus warfarin in AF patients with CrCl of at least 25 ml/min 40(table 2). Apixaban was superior to warfarin in reducing stroke, systemic embolism events, and major hemorrhages. Especially patients with severe or moderate renal impairment suffered from significantly less major bleedings under apixaban than under warfarin (apixaban group: 3.2% versus warfarin group: 6.4%; P=0.03 for interaction).
CKD stage 4 (eGFR between 15 and 29 ml/min/1.73 m2): Only few trials with small numbers of CKD patients with eGFR between 15 and 29 ml/min/1.73 m2 are available. Limdi et al.[35] evaluated the influence of kidney function on warfarin dosage. With decreasing kidney function patients require significantly lower warfarin doses and are at higher risk for over-anticoagulation. Further, patients with severe CKD (eGFR < 30 ml/min/1.73m2) had a 2.4-fold increased risk of major hemorrhage.
As mentioned above, a recent retrospective study with 399 patients with CKD stages 3, 4 and 5 and AF investigated the incidence of thromboembolic stroke under treatment with or without warfarin. The incidence of thromboembolic stroke in patients with CKD stage 4 was only about a fourth of those in patients without anticoagulation (5% versus 21%, P<0.05).[37]
CKD stage 5 = ESRD (eGFR <15 ml/min/1.73 m2): Since anticoagulation therapy in patients with CKD stage 4 must be weight out carefully, this applies certainly even more to patients with ESRD. Few studies so far have evaluated the safety of warfarin in patients with eGFR < 15 ml/min/1.73 m2 with controversial results (table 1).
Vazquez[36] conducted a small observational study with 240 patients on hemodialysis, of whom 29 had received oral anticoagulant warfarin derivatives for a period of at least one month. Although the relative risk of bleeding with anticoagulation was more than 2-fold enhanced, none of the bleeding incidences, mainly in the digestive tract, was fatal.
Recently, two retrospective studies of hemodialysis patients with AF suggest that warfarin is associated with increased risk of stroke. In a retrospective cohort analysis of 1,671 hemodialysis patients the use of warfarin increased the risk for new stroke by 1.93 compared with nonuse. Furthermore, patients on warfarin who received no INR monitoring in the first 90 day had an even more advanced risk for stroke (hazard ration 2.79). On the other hand, there was no statistically significant increase in all-cause mortality or hospitalization under warfarin use.[41]
Data from the Dialysis Outcomes and Practice Patterns Study (DOPPS),[42] showed that warfarin given to hemodialysis patients with AF increased their stroke risk especially for elderly patients over 75 years (hazard ratio 2.17, 95% CI 1.04 – 4.53).
Controversially, Lai[37] reported a reduced stoke incidence in patients on warfarin compared to patients off warfarin: 10% of hemodialysis patients and 10% of patients with eGFR < 15 ml/min/1.73 m2 under warfarin treatment experienced a thromboembolic stroke versus 38% respectively 37% of patients without warfarin.
A retrospective analysis of 5,858 ESRD patients examined the long–term survival after cardiac valve surgery.[43] Patients received either mechanical prosthetic valves requiring lifetime anticoagulation or bio prosthetic valves with no medical need for subsequent anticoagulation. Although all dialysis patients had a poor long-term survival after cardiac surgery, there was no difference in the survival of the 4,944 patients with mechanical valves compared to that of the 848 patients with tissue valves. This is remarkable, since patients receiving mechanical valves need permanent anticoagulation whereas most of the patients with tissue valves probably did not take anticoagulation although there are no data given in the study.
Therapeutic Strategies
In general, oral anticoagulation is an effective therapy to prevent stroke in AF patients. Whether patients with impaired renal function benefit to thesame extent from an anticoagulant therapy, is the issue of only few studies so far. The problem with anticoagulation in CKD patients is their also increased risk of bleeding due to altered hemostasis. In consequence, with worsening kidney function, both the risk of stroke and the risk of bleeding events rise markedly.
To determine the risk of stroke in the general population, several stroke risk stratification algorithms have been developed. The simplest and most common risk assessment scheme, the CHADS2-score, is based on a point system in which one point is assigned for recent cardiac failure, hypertension, age > 75 years, and diabetes and two points are assigned for history of stroke or transient ischemic attacks (TIA). In routine care of the general population, oral anticoagulation is recommended for patients with a CHADS2-score ≥2.[11] Lately, the CHADS2-score has been modified to the CHA2DS2-VASc-score, giving two points to age > 75 years and an additional point for vascular disease, age 65-74 years, and female gender.[44] Thus, more risk factors for stroke are considered in the CHA2DS2-VASc-score. Again, oral anticoagulation is recommended for patients with a CHA2DS2-VASc-score of two or greater.[45]
In CKD and especially in ESRD, affected patients suffer from a prothrombotic state which is the result of a high risk for thromboembolism and a coagulopathy with an increased tendency for bleeding.[9] The management of chronic hemodialysis patients with AF is therefore difficult, and so far no current stroke risk stratification schemes consider the situation in CKD or ESRD patients.[23] An individual algorithm considering risk factors and persistent medication, as suggest by us previously,[9] might currently represent the most suitable approach for CKD patients until data from randomized trials will be available. Going briefly through this algorithm, all CKD patients with permanent, persistent, and paroxysmal atrial fibrillation should be considered to be prone to an increased risk for ischemic stroke. Based on the ESC guidelines[11] for atrial fibrillation, the patient’s major and clinically relevant non-major risk factors (table 3) should be assessed and the CHADS2- or CHA2DS2-VASc-score could be calculated. Since all the patients evaluated in this context have CKD as an additional but yet not concerned risk factor, there is wide consent that their true ischemic risk must be classified to be higher. If a patient has definitely no or only one moderate risk factor, anticoagulation with antiplatelet drugs, e.g. low-dose acetylsalicylic acid (ASS), can be considered as an efficient therapy.
Table 3. Major and clinically relevant non-major risk factors for stroke and thromboembolism in non-valvular AF [11].
TIA: transient ischemic attack; LV: left ventricular; EF: ejection fraction
| Major risk factors | Clinically relevant non-major risk factors |
|---|---|
| Prior stroke or TIA or thromboembolism | Heart failure or moderate to severe LV dysfunction (LV EF ≤ 40%) |
| Age ≥ 75 years | Hypertension |
| Mitral stenosis or prosthetic heart valves | Diabetes mellitus Female sex Age 65-74 years Vascular disease (prior myocardial infarction, peripheral artery disease, complex aortic plaque) |
Otherwise, for patients with two or more risk factors an oral anticoagulation therapy should be considered. If the patient has already taken oral anticoagulation for more than 3 months, there is evidence that he probably represents a positive selection with a lower risk for bleedings.[9] Nevertheless, the bleeding risk is higher in CKD patients; therefore during long-term treatment the INR should be controlled at least every 14 days and be adjusted within a precise target range of 2.0-2.5.
In patients without current oral anticoagulation or beginning of this therapy within the last 3 months, risk factors for bleedings e.g. previous hemorrhage, dementia, cancer, eGFR<30 ml/min/1.73 m2 or recurrent falls, should be carefully considered. If the decision towards oral anticoagulation is made, than the titration phase should be started carefully, with lower starting doses of the anticoagulant and small-meshed INR controls during the first 4 weeks, during which the highest bleeding rates in all patients especially those with increased risks occur. If the bleedings risk appears to be too high, then at least administration of antiplatelet drugs should be considered, even more if other vascular manifestations are present (coronary, peripheral or carotid artery disease).
Conclusions
Although it is well known that CKD and ESRD patients are at a markedly increased risk for cardiovascular events and mortality, only limited and conflicting data are available about treatment strategies in many fields. As a consequence, CKD patients are often undertreated compared to patients with normal renal function. Thus, the unfavorable prognosis of CKD and ESRD patients with AF is in part due to poor treatment which is the consequence of the poor data basis. In so far, CKD patients are hit twice: they suffer from a higher morbidity and are often treated worse.
With regard to atrial fibrillation, there is a great insecurity whether the standard therapy whichis oral anticoagulation provides any benefit in patients with renal impairment and AF. CKD patients with AF who are closely monitored as seen in a recent study[46] appear have a comparable survival rate to patients without AF and without anticoagulation. Also, the stroke incidence can be dramatically reduced if an INR between 2.0 and 3.0 was achieved.[37] Other, non-randomized, retrospective studies did not support these positive findings.[41,42, 47] More studies evaluating CKD patients especially with CKD stages 4 and 5 and AF are strongly recommended to improve the medical therapy and to develop widely accepted risk stratification and treatment guidelines.
References
- 1.K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am. J. Kidney Dis. 2002 Feb;39 (2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 2.U S Renal Data System, USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. 2010;0:0–0. [Google Scholar]
- 3.Hsu Chi-yuan, Iribarren Carlos, McCulloch Charles E, Darbinian Jeanne, Go Alan S. Risk factors for end-stage renal disease: 25-year follow-up. Arch. Intern. Med. 2009 Feb 23;169 (4):342–50. doi: 10.1001/archinternmed.2008.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meguid El Nahas A, Bello Aminu K. Chronic kidney disease: the global challenge. Lancet. 2005 Jan 25;365 (9456):331–40. doi: 10.1016/S0140-6736(05)17789-7. [DOI] [PubMed] [Google Scholar]
- 5.Reinecke Holger, Trey Torsten, Matzkies Fritz, Fobker Manfred, Breithardt Günter, Schaefer Roland M. Grade of chronic renal failure, and acute and long-term outcome after percutaneous coronary interventions. Kidney Int. 2003 Feb;63 (2):696–701. doi: 10.1046/j.1523-1755.2003.00784.x. [DOI] [PubMed] [Google Scholar]
- 6.Go Alan S, Chertow Glenn M, Fan Dongjie, McCulloch Charles E, Hsu Chi-yuan. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004 Sep 23;351 (13):1296–305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 7.Wattanakit Keattiyoat, Cushman Mary, Stehman-Breen Catherine, Heckbert Susan R, Folsom Aaron R. Chronic kidney disease increases risk for venous thromboembolism. J. Am. Soc. Nephrol. 2008 Jan;19 (1):135–40. doi: 10.1681/ASN.2007030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alonso Alvaro, Lopez Faye L, Matsushita Kunihiro, Loehr Laura R, Agarwal Sunil K, Chen Lin Y, Soliman Elsayed Z, Astor Brad C, Coresh Josef. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011 Jun 28;123 (25):2946–53. doi: 10.1161/CIRCULATIONAHA.111.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reinecke Holger, Brand Eva, Mesters Rolf, Schäbitz Wolf-Rüdiger, Fisher Marc, Pavenstädt Hermann, Breithardt Günter. Dilemmas in the management of atrial fibrillation in chronic kidney disease. J. Am. Soc. Nephrol. 2009 Apr;20 (4):705–11. doi: 10.1681/ASN.2007111207. [DOI] [PubMed] [Google Scholar]
- 10.Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J , McGregor K, Metra M, Morais J, Osterspey A, Zamorano JL. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines. J. Am. Coll. Cardiol. . 2006;48:854–906. doi: 10.1016/j.jacc.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Camm A John, Kirchhof Paulus, Lip Gregory Y H, Schotten Ulrich, Savelieva Irene, Ernst Sabine, Van Gelder Isabelle C, Al-Attar Nawwar, Hindricks Gerhard, Prendergast Bernard, Heidbuchel Hein, Alfieri Ottavio, Angelini Annalisa, Atar Dan, Colonna Paolo, De Caterina Raffaele, De Sutter Johan, Goette Andreas, Gorenek Bulent, Heldal Magnus, Hohloser Stefan H, Kolh Philippe, Le Heuzey Jean-Yves, Ponikowski Piotr, Rutten Frans H. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010 Oct;12 (10):1360–420. doi: 10.1093/europace/euq350. [DOI] [PubMed] [Google Scholar]
- 12.Abe S, Yoshizawa M, Nakanishi N, Yazawa T, Yokota K, Honda M, Sloman G. Electrocardiographic abnormalities in patients receiving hemodialysis. Am. Heart J. 1996 Jun;131 (6):1137–44. doi: 10.1016/s0002-8703(96)90088-5. [DOI] [PubMed] [Google Scholar]
- 13.Vázquez E, Sánchez-Perales C, Borrego F, Garcia-Cortés M J, Lozano C, Guzmán M, Gil J M, Borrego M J, Pérez V. Influence of atrial fibrillation on the morbido-mortality of patients on hemodialysis. Am. Heart J. 2000 Dec;140 (6):886–90. doi: 10.1067/mhj.2000.111111. [DOI] [PubMed] [Google Scholar]
- 14.Fabbian F, Catalano C, Lambertini D, Tarroni G, Bordin V, Squerzanti R, Gilli P, Di Landro D, Cavagna R. Clinical characteristics associated to atrial fibrillation in chronic hemodialysis patients. Clin. Nephrol. 2000 Sep;54 (3):234–9. [PubMed] [Google Scholar]
- 15.Tsagalis George, Bakirtzi Nerantzoula, Manios Efstathios, Chouliaras Ioannis, Papagiannidou Parthenia, Stamellou Eleni, Akrivos Theodore, Makris Fotis, Psimenou Erasinia, Koutroubas George, Xinos Koustantinos, Vemmos Koustantinos. Atrial fibrillation in chronic hemodialysis patients: prevalence, types, predictors, and treatment practices in Greece. Artif Organs. 2011 Oct;35 (10):916–22. doi: 10.1111/j.1525-1594.2011.01229.x. [DOI] [PubMed] [Google Scholar]
- 16.Genovesi Simonetta, Pogliani Daniela, Faini Andrea, Valsecchi Maria G, Riva Alessandra, Stefani Francesca, Acquistapace Irene, Stella Andrea, Bonforte Giuseppe, DeVecchi Amedeo, DeCristofaro Vincenzo, Buccianti Gherardo, Vincenti Antonio. Prevalence of atrial fibrillation and associated factors in a population of long-term hemodialysis patients. Am. J. Kidney Dis. 2005 Nov;46 (5):897–902. doi: 10.1053/j.ajkd.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 17.Winkelmayer Wolfgang C, Patrick Amanda R, Liu Jun, Brookhart M Alan, Setoguchi Soko. The increasing prevalence of atrial fibrillation among hemodialysis patients. J. Am. Soc. Nephrol. 2011 Feb;22 (2):349–57. doi: 10.1681/ASN.2010050459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baber Usman, Howard Virginia J, Halperin Jonathan L, Soliman Elsayed Z, Zhang Xiao, McClellan William, Warnock David G, Muntner Paul. Association of chronic kidney disease with atrial fibrillation among adults in the United States: REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circ Arrhythm Electrophysiol. 2011 Feb;4 (1):26–32. doi: 10.1161/CIRCEP.110.957100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soliman Elsayed Z, Prineas Ronald J, Go Alan S, Xie Dawei, Lash James P, Rahman Mahboob, Ojo Akinlolu, Teal Val L, Jensvold Nancy G, Robinson Nancy L, Dries Daniel L, Bazzano Lydia, Mohler Emile R, Wright Jackson T, Feldman Harold I. Chronic kidney disease and prevalent atrial fibrillation: the Chronic Renal Insufficiency Cohort (CRIC). Am. Heart J. 2010 Jun;159 (6):1102–7. doi: 10.1016/j.ahj.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ananthapanyasut Wanwarat, Napan Sirikarn, Rudolph Earl H, Harindhanavudhi Tasma, Ayash Husam, Guglielmi Kelly E, Lerma Edgar V. Prevalence of atrial fibrillation and its predictors in nondialysis patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010 Feb;5 (2):173–81. doi: 10.2215/CJN.03170509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watanabe Hiroshi, Watanabe Toru, Sasaki Shigeru, Nagai Kojiro, Roden Dan M, Aizawa Yoshifusa. Close bidirectional relationship between chronic kidney disease and atrial fibrillation: the Niigata preventive medicine study. Am. Heart J. 2009 Oct;158 (4):629–36. doi: 10.1016/j.ahj.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 22.Lip Gregory Y H, Tse Hung-Fat. Management of atrial fibrillation. Lancet. 2007 Aug 18;370 (9587):604–18. doi: 10.1016/S0140-6736(07)61300-2. [DOI] [PubMed] [Google Scholar]
- 23.Marinigh Ricarda, Lane Deirdre A, Lip Gregory Y H. Severe renal impairment and stroke prevention in atrial fibrillation: implications for thromboprophylaxis and bleeding risk. J. Am. Coll. Cardiol. 2011 Mar 22;57 (12):1339–48. doi: 10.1016/j.jacc.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Nakayama Masaaki, Metoki Hirohito, Terawaki Hiroyuki, Ohkubo Takayoshi, Kikuya Masahiro, Sato Toshinobu, Nakayama Keisuke, Asayama Kei, Inoue Ryusuke, Hashimoto Junichiro, Totsune Kazuhito, Hoshi Haruhisa, Ito Sadayoshi, Imai Yutaka. Kidney dysfunction as a risk factor for first symptomatic stroke events in a general Japanese population--the Ohasama study. Nephrol. Dial. Transplant. 2007 Jul;22 (7):1910–5. doi: 10.1093/ndt/gfm051. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Renal Data System, USRDS 2006 Annual Data Report: Atlas of End-Stage Renal Disease in6the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. 2006;0:0–0. [Google Scholar]
- 26.Shimizu Yuji, Maeda Kenji, Imano Hironori, Ohira Tetsuya, Kitamura Akihiko, Kiyama Masahiko, Okada Takeo, Ishikawa Yoshinori, Shimamoto Takashi, Yamagishi Kazumasa, Tanigawa Takeshi, Iso Hiroyasu. Chronic kidney disease and drinking status in relation to risks of stroke and its subtypes: the Circulatory Risk in Communities Study (CIRCS). Stroke. 2011 Sep;42 (9):2531–7. doi: 10.1161/STROKEAHA.110.600759. [DOI] [PubMed] [Google Scholar]
- 27.Schäbitz Wolf-Rüdiger, Reinecke Holger. Chronic kidney disease and alcohol consumption: are asians at particular risk for hemorrhagic stroke? Stroke. 2011 Sep;42 (9):2385–6. doi: 10.1161/STROKEAHA.111.626713. [DOI] [PubMed] [Google Scholar]
- 28.Go Alan S, Fang Margaret C, Udaltsova Natalia, Chang Yuchiao, Pomernacki Niela K, Borowsky Leila, Singer Daniel E. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. 2009 Mar 17;119 (10):1363–9. doi: 10.1161/CIRCULATIONAHA.108.816082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee Meng, Saver Jeffrey L, Chang Kuo-Hsuan, Liao Hung-Wei, Chang Shen-Chih, Ovbiagele Bruce. Low glomerular filtration rate and risk of stroke: meta-analysis. BMJ. 2010 Sep 30;341 () doi: 10.1136/bmj.c4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vazquez Eduardo, Sanchez-Perales Carmen, Garcia-Garcia Francisco, Castellano Patricia, Garcia-Cortes Maria-Jose, Liebana Antonio, Lozano Cristobal. Atrial fibrillation in incident dialysis patients. Kidney Int. 2009 Aug;76 (3):324–30. doi: 10.1038/ki.2009.185. [DOI] [PubMed] [Google Scholar]
- 31.Bos Michiel J, Koudstaal Peter J, Hofman Albert, Breteler Monique M B. Decreased glomerular filtration rate is a risk factor for hemorrhagic but not for ischemic stroke: the Rotterdam Study. Stroke. 2007 Dec;38 (12):3127–32. doi: 10.1161/STROKEAHA.107.489807. [DOI] [PubMed] [Google Scholar]
- 32.Genovesi Simonetta, Vincenti Antonio, Rossi Emanuela, Pogliani Daniela, Acquistapace Irene, Stella Andrea, Valsecchi Maria Grazia. Atrial fibrillation and morbidity and mortality in a cohort of long-term hemodialysis patients. Am. J. Kidney Dis. 2008 Feb;51 (2):255–62. doi: 10.1053/j.ajkd.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Renal Data System, USRDS 2005 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. 2005;0:0–0. [Google Scholar]
- 34.Vázquez Eduardo, Sánchez-Perales Carmen, Lozano Cristóbal, García-Cortés Ma José, Borrego Francisco, Guzmán Manuel, Pérez Pilar, Pagola Carlos, Borrego Ma José, Pérez Vicente. Comparison of prognostic value of atrial fibrillation versus sinus rhythm in patients on long-term hemodialysis. Am. J. Cardiol. 2003 Oct 01;92 (7):868–71. doi: 10.1016/s0002-9149(03)00904-4. [DOI] [PubMed] [Google Scholar]
- 35.Limdi Nita A, Beasley T Mark, Baird Melissa F, Goldstein Joyce A, McGwin Gerald, Arnett Donna K, Acton Ronald T, Allon Michael. Kidney function influences warfarin responsiveness and hemorrhagic complications. J. Am. Soc. Nephrol. 2009 Apr;20 (4):912–21. doi: 10.1681/ASN.2008070802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vázquez Eduardo, Sánchez-Perales Carmen, García-Cortes M-José, Borrego Francisco, Lozano Cristóbal, Guzmán Manuel, Gil José Manuel, Liébana Antonio, Pérez Pilar, Borrego M-José, Pérez Vicente. Ought dialysis patients with atrial fibrillation be treated with oral anticoagulants? Int. J. Cardiol. 2003 Feb;87 (2-3):135–9. doi: 10.1016/s0167-5273(02)00317-0. [DOI] [PubMed] [Google Scholar]
- 37.Lai Hoang M, Aronow Wilbert S, Kalen Phoenix, Adapa Sreedhar, Patel Kaushal, Goel Arvind, Vinnakota Ravi, Chugh Savneek, Garrick Renee. Incidence of thromboembolic stroke and of major bleeding in patients with atrial fibrillation and chronic kidney disease treated with and without warfarin. Int J Nephrol Renovasc Dis. 2009;2 ():33–7. doi: 10.2147/ijnrd.s7781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Connolly Stuart J, Ezekowitz Michael D, Yusuf Salim, Eikelboom John, Oldgren Jonas, Parekh Amit, Pogue Janice, Reilly Paul A, Themeles Ellison, Varrone Jeanne, Wang Susan, Alings Marco, Xavier Denis, Zhu Jun, Diaz Rafael, Lewis Basil S, Darius Harald, Diener Hans-Christoph, Joyner Campbell D, Wallentin Lars. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009 Sep 17;361 (12):1139–51. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 39.Fox Keith A A, Piccini Jonathan P, Wojdyla Daniel, Becker Richard C, Halperin Jonathan L, Nessel Christopher C, Paolini John F, Hankey Graeme J, Mahaffey Kenneth W, Patel Manesh R, Singer Daniel E, Califf Robert M. Prevention of stroke and systemic embolism with rivaroxaban compared with warfarin in patients with non-valvular atrial fibrillation and moderate renal impairment. Eur. Heart J. 2011 Oct;32 (19):2387–94. doi: 10.1093/eurheartj/ehr342. [DOI] [PubMed] [Google Scholar]
- 40.Granger Christopher B, Alexander John H, McMurray John J V, Lopes Renato D, Hylek Elaine M, Hanna Michael, Al-Khalidi Hussein R, Ansell Jack, Atar Dan, Avezum Alvaro, Bahit M Cecilia, Diaz Rafael, Easton J Donald, Ezekowitz Justin A, Flaker Greg, Garcia David, Geraldes Margarida, Gersh Bernard J, Golitsyn Sergey, Goto Shinya, Hermosillo Antonio G, Hohnloser Stefan H, Horowitz John, Mohan Puneet, Jansky Petr, Lewis Basil S, Lopez-Sendon Jose Luis, Pais Prem, Parkhomenko Alexander, Verheugt Freek W A, Zhu Jun, Wallentin Lars. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011 Sep 15;365 (11):981–92. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 41.Chan Kevin E, Lazarus J Michael, Thadhani Ravi, Hakim Raymond M. Warfarin use associates with increased risk for stroke in hemodialysis patients with atrial fibrillation. J. Am. Soc. Nephrol. 2009 Oct;20 (10):2223–33. doi: 10.1681/ASN.2009030319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wizemann Volker, Tong Lin, Satayathum Sudtida, Disney Alex, Akiba Takashi, Fissell Rachel B, Kerr Peter G, Young Eric W, Robinson Bruce M. Atrial fibrillation in hemodialysis patients: clinical features and associations with anticoagulant therapy. Kidney Int. 2010 Jun;77 (12):1098–106. doi: 10.1038/ki.2009.477. [DOI] [PubMed] [Google Scholar]
- 43.Herzog Charles A, Ma Jennie Z, Collins Allan J. Long-term survival of dialysis patients in the United States with prosthetic heart valves: should ACC/AHA practice guidelines on valve selection be modified? Circulation. 2002 Mar 19;105 (11):1336–41. doi: 10.1161/hc1102.100075. [DOI] [PubMed] [Google Scholar]
- 44.Lip Gregory Y H, Nieuwlaat Robby, Pisters Ron, Lane Deirdre A, Crijns Harry J G M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010 Feb;137 (2):263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 45.Yang Felix, Chou Denise, Schweitzer Paul, Hanon Sam. Warfarin in haemodialysis patients with atrial fibrillation: what benefit? Europace. 2010 Dec;12 (12):1666–72. doi: 10.1093/europace/euq387. [DOI] [PubMed] [Google Scholar]
- 46.Knoll Florian, Sturm Gisela, Lamina Claudia, Zitt Emanuel, Lins Friederike, Freistätter Otto, Kronenberg Florian, Lhotta Karl, Neyer Ulrich. Coumarins and survival in incident dialysis patients. Nephrol. Dial. Transplant. 2012 Jan;27 (1):332–7. doi: 10.1093/ndt/gfr341. [DOI] [PubMed] [Google Scholar]
- 47.Wiesholzer M, Harm F, Tomasec G, Barbieri G, Putz D, Balcke P. Incidence of stroke among chronic hemodialysis patients with nonrheumatic atrial fibrillation. Am. J. Nephrol. 2001 Mar 29;21 (1):35–9. doi: 10.1159/000046216. [DOI] [PubMed] [Google Scholar]
- 48.Abbott Kevin C, Trespalacios Fernando C, Taylor Allen J, Agodoa Lawrence Y. Atrial fibrillation in chronic dialysis patients in the United States: risk factors for hospitalization and mortality. BMC Nephrol. 2003 Jan 24;4 () doi: 10.1186/1471-2369-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.To Andrew Cy, Yehia Maha, Collins John F. Atrial fibrillation in haemodialysis patients: do the guidelines for anticoagulation apply? Nephrology (Carlton) 2007 Oct;12 (5):441–7. doi: 10.1111/j.1440-1797.2007.00835.x. [DOI] [PubMed] [Google Scholar]
- 50.Das Manisha, Aronow Wilbert S, McClung John A, Belkin Robert N. Increased prevalence of coronary artery disease, silent myocardial ischemia, complex ventricular arrhythmias, atrial fibrillation, left ventricular hypertrophy, mitral annular calcium, and aortic valve calcium in patients with chronic renal insufficiency. Cardiol Rev. 2005 Dec 24;14 (1):14–7. doi: 10.1097/01.crd.0000148162.88296.9f. [DOI] [PubMed] [Google Scholar]