Abstract
Metabolic syndrome, a constellation of conditions including obesity, dyslipidemia, hypertension and insulin resistance, has increased to epidemic proportions. Metabolic syndrome has been recognized as a risk factor for cardiovascular morbidity and is likely related to the epidemic of cardiovascular diseases. Perhaps not coincidentally, its growth in incidence has paralleled that of atrial fibrillation. Various components of metabolic syndrome have been known to have a role in the pathogenesis of atrial fibrillation. With the conglomeration of components seen in the metabolic syndrome, the risk for atrial fibrillation increases greatly. Several studies have elucidated the role of metabolic syndrome in the development of atrial fibrillation. Its role on the atrial substrate makes it an important determinant of progression of disease and failure of therapeutic strategies such as catheter ablation. Control of the various components of metabolic syndrome may ultimately lead to better outcomes in atrial fibrillation patients.
Introduction
Atrial fibrillation (AF), already the most common arrhythmia worldwide, continues its growth to epidemic proportions.[1,2] Perhaps not coincidentally, the conglomeration of insulin resistance, hypertension, dyslipidemia, and obesity known as the metabolic syndrome (MS) also has grown in prevalence to epidemic proportions, particularly in the adult U.S. population.[3] The association of AF with an increased risk for stroke[4] and mortality is well known. [5,6] However, the association of MS with cardiovascular disease is now becoming more evident.[7,8] The MS has been associated with increased prevalence of coronary heart disease and cerebrovascular disease.[7,9] It has also been associated with worsened coronary heart disease outcomes and cardiovascular mortality.[7] More recently, a body of evidence has linked the MS with both the incidence of AF and outcomes of management of AF. In this review, we present the evidence and potential underpinnings of this convergence of epidemics.
Definition of the MS
The American Heart Association / National Heart, Lung, and Blood Institute (AHA/NHLBI) 2005 scientific statement[10] defined the metabolic syndrome as the presence of at least three of the following criteria:
Waist circumference greater than or equal to 40 inches (102 cm) in men or 35 inches (88cm) in women
Triglycerides greater than or equal to 150 mg/dl (1.7 mmol/L) or on drug treatment for elevated triglycerides
High density lipoprotein (HDL) cholesterol less than 40 mg/dL (1.03 mmol/L) in men or 50 mg/dL (1.3 mmol/L) in women or on drug treatment for reduced HDL
Systolic blood pressure greater than or equal to 130 mmHg or diastolic blood pressure greater than or equal to 85 mmHg or on antihypertensive drug treatment in a patient with a history of hypertension
Fasting glucose greater than or equal to 100 mg/dL or on drug treatment for elevated glucose
Based on the more conservative ATP III definition (fasting glucose >= 110 mg/dL), the age-adjusted U.S. prevalence of MS was 24% with Mexican Americans having the highest prevalence overall (32%). 11 Prevalence increases with age such that those over 60 have an astounding 44% prevalence of MS.[11] Based on 2000 census data, nearly 50 million U.S. residents have the metabolic syndrome and its prevalence is only increasing with time.
The simultaneous epidemic of AF in the U.S. and worldwide populations prompts one to consider whether the two may be linked. There are several hypothetical reasons why this may be the case.
Why Could MS Lead to AF?
Various components of the MS are known risk factors for AF. These factors have been hypothesized to be involved in the pathogenesis of AF by various mechanisms (Figure 1). However, recent studies have shown that all these components of the MS together may have an additive effect on the risk for AF.[12]
Figure 1. Factors involved in the pathogenesis of Atrial fibrillation:
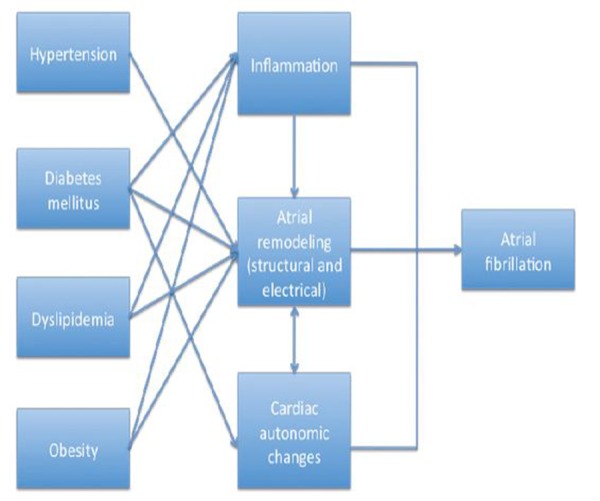
This figure summarizes the pathogenetic mechanisms for atrial fibrillation of the various components of the metabolic syndrome. Note the multiple effects of each component of metabolic syndrome.
According to our current understanding, the pathogenesis of AF involves a complex interplay of AF triggers and abnormal atrial substrate required to sustain the arrhythmia. Various components of the MS may act as risk factors for AF by their effect on AF triggers or the atrial substrate. Below we review the potential mechanisms for the MS components in the causation of AF.
Hypertension
Hypertension is the commonest modifiable risk factor for AF.[13] It is seen in almost 60% of patients with AF.[14-16] Hypertension leads to left ventricular hypertrophy and diastolic dysfunction resulting in pathological remodeling of the left atrium predisposing to AF. Diastolic dysfunction results in left atrial stretching of enlargement,[17] important to the pathogenesis AF.[18] In animal models, hypertension has also been shown to induce structural changes including interstitial fibrosis.[19-21] In addition to mechanical remodeling and left atrial enlargement, electrical remodeling of the left atrium is known to occur with longstanding hypertension.[22] Global and regional conduction delays are seen in patients with longstanding systemic hypertension.[22] Moreover, changes in angiotensin II level leads to electrophysiological changes in the left atrial myocardium causing left atrial conduction delay. [23]
Insulin Resistance / Diabetes
Insulin resistance and diabetes are another risk factor associated with the development of AF. The Framingham Heart Study clearly established diabetes mellitus and glucose intolerance as a potential risk factor for AF.[13] Mechanistically diabetes mellitus predisposes to AF in a way similar to hypertension. Diabetes mellitus leads to left ventricular hypertrophy and diastolic dysfunction,[24] leading to mechanical and electrical remodeling of the atrium.[25] Apart from left ventricular hypertrophy and diastolic function, many other mechanisms of atrial remodeling in diabetes mellitus have been suggested based on animal experiments. Advanced glycation end-products (AGEs) and receptors for AGEs (RAGE) have been known to cause interstitial scarring in the left atrium.[26,27] Angiotensin II blockers are known to prevent anatomic and electrical remodeling likely by blocking AGE-RAGE.[28] In addition to structural remodeling, the atria of diabetic animals also demonstrate increased intra-atrial conduction time providing the electrical substrate for AF. Diabetes mellitus and the MS affect the cardiac autonomic system, which may contribute to arrhythmogenicity.[29,30] Finally, diabetes mellitus may lead to ischemic or non-ischemic cardiomyopathy also predisposing to AF through the resultant left atrial enlargement.
Dyslipidemia
Hypertriglyceridemia and low HDL-cholesterolemia are the lipid disorders seen with metabolic syndrome. Low HDL-cholesterol, has been found to increase the risk of AF by 20-40%.[15,31,32] However, data for hypertriglyceridemia are inconsistent. Proposed mechanisms of predisposition to AF due to the dyslipidemia are arrhythmogenicity due to altered membrane composition leading to altered excitability[33] as well as pro-inflammatory effects.[34]
Obesity
Obesity is an important component of the MS and is known to be associated with an increased risk for AF. Data from the Framingham heart study showed an increased risk of new-onset AF for obesity (BMI>=30) with an adjusted hazard ratio of 1.52 and 1.46 for men and women respectively compared to subjects with normal BMI.[35] A meta-analysis of 16 studies found a 49% increased risk of obese patients developing AF as compared to non-obese patients.[36] The role of obesity has been explained by multiple mechanisms. Obesity is a risk factor for insulin resistance and diabetes mellitus and hence is a potential pathway for predisposition to AF. A direct correlation has been seen between increasing BMI and left atrial size.[37] Left atrial enlargement may be the most important mechanism through which obesity increases the risk of AF, since after adjusting for left atrial enlargement obesity is no longer a risk factor for atrial fibrillation in the Framingham Heart Study cohort.[35] However, other mechanisms which have been suggested include the systemic inflammatory state seen with obesity. Inflammation is known to be a risk factor for AF [38] and obese patients are known to have elevated hsCRP levels, a marker of systemic inflammation.[39] Another factor which may predispose to AF in patients with obesity is obstructive sleep apnea, a well described risk factor for AF.[40-42]
All Together is Worse?
It is apparent that various components of MS predispose to AF in isolation. However, the combination of these components seen in the metabolic syndrome may act in a synergistic manner (Figure 1). The final common pathway in the pathogenesis of AF can be grouped as atrial structural and electrical remodeling, inflammatory processes, and cardiac autonomic changes.
Atrial structural and electrical remodeling is of paramount importance in providing the substrate for initiation and maintenance of AF. As described above, various components of MS cause atrial remodeling. Structural remodeling with interstitial fibrosis leads to heterogeneous electrical substrate with differences in conduction velocities promoting AF.[43] Fibroblasts in these areas of interstitial fibrosis may couple with cardiomyocytes electrically and promote reentry and ectopic activity.[44] Electrical remodeling alters ion channel function and calcium handling of the cells and promotes initiation and maintenance of atrial fibrillation.[45]
The cardiac autonomic nervous system is important in the pathogenesis of AF.[46] Vagal discharge,[47] beta-adrenoceptor activation[48] and atrial sympathetic hyperinnervation[49] have been implicated in the arrhythmogenesis of AF. Autonomic dysfunction is known to be associated with metabolic syndrome and has been shown to get worse with increasing number of MS factors present.[50]
Inflammation is considered one of the basic pathophysiological substrates in the causation and progression of AF. Atrial inflammation has been seen in the histological specimens of lone AF patients as opposed to patients with sinus rhythm.[51] Inflammation provides an anatomic and electrical substrate for AF. A vast body of evidence supporting the inflammation hypothesis of atrial fibrillation comes from studies of inflammatory biomarkers.[38] Moreover, inflammation has a role in early recurrence of atrial fibrillation after catheter ablation.[52] As previously discussed, several components of the MS (obesity, insulin resistance, dyslipidemia) have been shown to be proinflammatory.
Thus, various components of MS are known to affect these pathogenetic factors of AF. As these factors are affected by multiple components of MS, their role in the pathogenesis of AF becomes additive and complex. Recent studies have looked at the MS as a whole and the risk of AF.[53-56] It has been shown that as the number of components of AF increases, the risk of development of AF goes up.[53,57] The fact that AF is one of the important cardiovascular effects of metabolic syndrome has more recently been brought to notice by the studies detailed below.
Increased Incidence of AF with MS
Several population-based studies have demonstrated the increased risk of incident AF among patients with the metabolic syndrome (Table 1). Umetani et al analyzed 592 hospitalized patients without structural heart disease. Among 21% of patients with metabolic syndrome, AF occurred in 9% compared with 4% of those without metabolic syndrome. In multivariable analyses, the OR for AF with metabolic syndrome was 2.8.[54] Watanabe et al studied 28,449 participants without baseline AF in the Niigata preventive medicine community-based study. The metabolic syndrome was present in 13% of participants. During a mean follow-up of 4.5 years, AF developed in 265 participants. The HR for AF among participants with MS, compared to those without MS, was 1.78.[55] Chamberlain et al analyzed the risk of AF in the Atherosclerosis Risk in Communities (ARIC) Study. Among 15,094 participants over a mean follow-up of 15.4 years, there were 1238 cases of incident AF. At baseline, 46% of black and 40% of white participants had the metabolic syndrome. The HR for AF among participants with, compared to those without, the metabolic syndrome was 1.67 and did not differ by race. In addition, the risk for incident AF increased with increasing number of MS components such that those with all 5 components had a HR of 4.4 compared to those with no components.[12] Echahidi et al analyzed the risk of post-operative AF after coronary artery bypass surgery among 5085 patients. Metabolic syndrome was present in 46% of patients and post-operative AF occurred in 27%. Among patients <=50 years old, MS was associated with a RR of 2.4 with development of post-operative AF. 58 Vyssoulis et al studied a population of over 15,000 patients with hypertension.[57] The prevalence of MS ranged from 32% to 48%, depending on the definition used. The odds of having AF in those with MS ranged from 1.61 to 1.99. Importantly, the prevalence of AF increased with each additional component of the MS. Altieri et al demonstrated a high incidence of AF (16%) in a population of Hispanic patients with metabolic syndrome.[59] The authors suggested mechanisms of this association may include sinus node remodeling, atrial fibrosis, and older age which are all seen in a population with MS.
Table 1. Studies Showing Association of Atrial Fibrillation with Metabolic Syndrome.
| Author, year | No. of patients | Findings |
|---|---|---|
| Umetani et al., 2007 [71] | 592 | 21% of hospitalized patients with MS; incident AF occurred more frequently in patients with MS (9% vs. 4%, OR 2.8) |
| Watanabe et al., 2008 [72] | 28,449 | 13% had MS. After a follow up of 4.5 years, subjects with MS at baseline were more likely to develop AF (HR 1.78) |
| Chamberlain et al, (ARIC study)[31] | 15,094 | 41% of participants had MS at baseline, HR for development of AF was 1.67 with MS. Risk for incidence of AF increased with increasing number of components of MS |
| Echahidi et al, [58] | 5085 | MS was present in 46% of patients post CABG and 27% developed post-operative AF. RR of AF 2.4 with MS |
| Vyssoulis et al, [57] | 15,075 | MS associated with presence of AF in patients with hypertension (odds ratio 1.61 to 1.99 depending on the definition of MS used). Prevalence of AF increased with number components of MS |
| Altieri et al, [59] | 173 | MS was present in 16% of patients with metabolic syndrome |
| Liu et al, [73] | 972 | Higher incidence of AF in hypertensive patients with MS than in them without MS (OR 1.853, 12.84% vs. 6.93%) |
| Tang et al, [74] | 741 | 46.3% of patients without structural heart disease coming for catheter ablation of AF had MS |
Worsened Outcomes of AF Treatment with MS
Atrial fibrillation is a progressive disease and various etiological factors provide substrate for its initiation as well as maintenance and progression. Hence patients with MS continue to develop substrate for AF even after treatment and are likely to have worsened outcomes (Table 2). Multiple studies have suggested that MS may influence the outcome of catheter ablation therapy. In a large prospective study of catheter ablation of AF, 1496 patients were followed up for a mean of 21 months. Patients with MS had a 39% recurrence rate compared to 32% for patients without MS (p = 0.005).[60] A study by Chang et al.[61] from Taiwan enrolled 282 patients undergoing catheter ablation for AF. The authors found a higher incidence of recurrent AF in patients with MS (55% vs. 24%, p < 0.001). Notably, it was more common to see recurrent atrial fibrillation originating from non-pulmonary veinous sites in patients with MS (45% vs. 20%, p=0.037), suggesting an effect of MS on left atrial substrate. In an analysis of predictors of late recurrence of AF after catheter ablation by Cai et al., MS was an independent predictor of late recurrence (OR = 4.41, 95% CI 1.56-12.46, p = 0.005).[62] Berkowitsch et al reported the results of pulmonary vein isolation in patients with AF with either cryo-balloon or by circumferential pulmonary vein isolation with radiofrequency catheter ablation in 702 consecutive patients with AF. The presence of MS was independently associated with a higher risk of recurrent AF (46.4% in patients with MS vs. 56.8% among patients without MS, p = 0.006) over 15.6 (inter-quartile range 12.7-42.3) months.[63]
Table 2. Studies Showing Increased Risk of Recurrent Atrial Fibrillation after Catheter Ablation in patients with Metabolic Syndrome .
| Author, year | No of patients | Findings |
|---|---|---|
| Mohanty et al., 2012 [60] | 1496; 485 with MS | Higher recurrence rate of AF after catheter ablation in patients with MS (39% vs. 32%, p=0.005; mean follow up 21 months). No difference in subgroup with paroxysmal AF |
| Tang et al., 2009 [75] | 654; 323 with MS | Patients with MS post catheter ablation had higher rate of recurrence (43.7% vs. 30.5%, p<0.001; mean follow up of 470 days) |
| Chang et al., 2009 [61] | 282; 53 with MS | Higher rate of recurrence of AF after catheter ablation in patients with MS (45% vs. 24%, p=0.037) |
| Cai et al., 2011 [62] | 186; 61 with MS | Metabolic syndrome was an independent predictor of late recurrence of AF (OR 4.41, 95% CI 1.56-12.46, p=0.005) after catheter ablation along with obesity, procedural failure and early recurrence of atrial fibrillation |
| Berkowitsch et al., 2012 [63] | 702; 276 with MS | Recurrence of AF after catheter ablation higher in patients with MS (56.4% vs 46.4%) |
What Can be Done?
Altered anatomic and electrical substrate is a major factor in the progression of AF and has an adverse effect on outcomes of medical and catheter ablation therapy. Atrial fibrillation is known to promote the structural and electrical remodeling of the atria and control of AF by medical therapy or catheter ablation should have a favorable effect on the substrate. However, evidence suggests that risk factors for AF such as MS have a direct effect on the creation and promotion of the arrhythmogenic substrate. Hence, control of these risk factors by optimum intervention may potentially slow the progression of the remodeling process. Data suggests that optimal control of blood pressure, maintenance of ideal body weight, control of lipid disorders and intervention for insulin resistance would help to control the arrhythmogenic substrate.
Reduction in the risk of atrial fibrillation with treatment of hypertension has been well documented in various studies of antihypertensive therapy for hypertension. A meta-analysis of treatment of hypertension using renin- angiotensin system inhibitors showed a reduction in the relative risk of atrial fibrillation by 15-40%, however this benefit was limited to patients with left ventricular systolic dysfunction or left ventricular hypertrophy.[64] Other meta-analyses of studies using ARBs and ACEIs showed similar reduction in new onset atrial fibrillation as well better outcome with electrical cardioversion and lower recurrence later.[65,66]
Control of diabetes mellitus with treatment reduced the risk of atrial fibrillation in a large study.[67] Another study showed the reduction of risk of atrial fibrillation recurrence after catheter ablation in patients with diabetes mellitus and insulin resistance with the use of pioglitazone.[68] Use of lipid lowering drugs like statins has been shown to reduce the risk of atrial fibrillation.[69,70] However, use of pioglitazone or statin may reduce the risk of atrial fibrillation through their direct effect on inflammatory process rather than their effect on insulin resistance or dyslipidemia. Similarly, control of obesity may affect atrial fibrillation indirectly by its effect on insulin resistance and obstructive sleep apnea.
The above account suggests that those factors involved in the pathogenesis of AF work in an interactive manner. Therapeutic interventions have pleiotropic effect and their action on reduction of AF risk is frequently through multiple effects. Further evidence supporting the benefit of treatment for MS as a whole in reducing AF outcomes will improve our understanding in this area.
Conclusions
Metabolic syndrome, a constellation of associated conditions, has increased to epidemic proportions. It has been recognized as a risk factor for cardiovascular morbidity and is likely related to the epidemic of cardiovascular diseases. Recently it has been recognized that atrial fibrillation may be associated with the ongoing epidemic of metabolic syndrome. Various components of metabolic syndrome have been known to have a role in pathogenesis of atrial fibrillation. Recent studies have elucidated the role of metabolic syndrome in the causation of atrial fibrillation. Its role on the atrial substrate makes it an important determinant of progression of disease and failure of therapeutic strategies such as catheter ablation. Control of the various components of metabolic syndrome may ultimately lead to better outcomes in AF patients.
Disclosures
No disclosures relevant to this article were made by the authors.
References
- 1.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter P, Seward James B, Tsang Teresa S M. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006 Jul 11;114 (2):119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 2.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 3.Ford Earl S, Giles Wayne H, Mokdad Ali H. Increasing prevalence of the metabolic syndrome among u.s. Adults. Diabetes Care. 2004 Oct;27 (10):2444–9. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 4.Wolf P A, Abbott R D, Kannel W B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22 (8):983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 5.Kannel W B, Abbott R D, Savage D D, McNamara P M. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N. Engl. J. Med. 1982 Apr 29;306 (17):1018–22. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin E J, Wolf P A, D'Agostino R B, Silbershatz H, Kannel W B, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998 Sep 08;98 (10):946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 7.Mottillo Salvatore, Filion Kristian B, Genest Jacques, Joseph Lawrence, Pilote Louise, Poirier Paul, Rinfret Stéphane, Schiffrin Ernesto L, Eisenberg Mark J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010 Sep 28;56 (14):1113–32. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 8.Gami Apoor S, Witt Brandi J, Howard Daniel E, Erwin Patricia J, Gami Lisa A, Somers Virend K, Montori Victor M. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J. Am. Coll. Cardiol. 2007 Jan 30;49 (4):403–14. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 9.Li Wei, Ma Dongrui, Liu Ming, Liu Hua, Feng Shejun, Hao Zilong, Wu Bo, Zhang Shihong. Association between metabolic syndrome and risk of stroke: a meta-analysis of cohort studies. Cerebrovasc. Dis. 2008;25 (6):539–47. doi: 10.1159/000131672. [DOI] [PubMed] [Google Scholar]
- 10.Grundy Scott M, Cleeman James I, Daniels Stephen R, Donato Karen A, Eckel Robert H, Franklin Barry A, Gordon David J, Krauss Ronald M, Savage Peter J, Smith Sidney C, Spertus John A. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary. Crit Pathw Cardiol. 2005 Dec;4 (4):198–203. doi: 10.1097/00132577-200512000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Ford Earl S, Giles Wayne H, Dietz William H. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002 Jan 16;287 (3):356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 12.Chamberlain Alanna M, Agarwal Sunil K, Ambrose Marietta, Folsom Aaron R, Soliman Elsayed Z, Alonso Alvaro. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 2010 May;159 (5):850–6. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kannel W B, Abbott R D, Savage D D, McNamara P M. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N. Engl. J. Med. 1982 Apr 29;306 (17):1018–22. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwlaat Robby, Capucci Alessandro, Camm A John, Olsson S Bertil, Andresen Dietrich, Davies D Wyn, Cobbe Stuart, Breithardt Günter, Le Heuzey Jean-Yves, Prins Martin H, Lévy Samuel, Crijns Harry J G M. Atrial fibrillation management: a prospective survey in ESC member countries: the Euro Heart Survey on Atrial Fibrillation. Eur. Heart J. 2005 Nov;26 (22):2422–34. doi: 10.1093/eurheartj/ehi505. [DOI] [PubMed] [Google Scholar]
- 15.Haywood L Julian, Ford Charles E, Crow Richard S, Davis Barry R, Massie Barry M, Einhorn Paula T, Williard Angela. Atrial fibrillation at baseline and during follow-up in ALLHAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial). J. Am. Coll. Cardiol. 2009 Nov 24;54 (22):2023–31. doi: 10.1016/j.jacc.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 16.Baseline characteristics of patients with atrial fibrillation: the AFFIRM Study. Am. Heart J. 2002 Jun;143 (6):991–1001. doi: 10.1067/mhj.2002.122875. [DOI] [PubMed] [Google Scholar]
- 17.Vaziri S M, Larson M G, Lauer M S, Benjamin E J, Levy D. Influence of blood pressure on left atrial size. The Framingham Heart Study. Hypertension. 1995 Jun;25 (6):1155–60. doi: 10.1161/01.hyp.25.6.1155. [DOI] [PubMed] [Google Scholar]
- 18.Tsang T S, Barnes M E, Bailey K R, Leibson C L, Montgomery S C, Takemoto Y, Diamond P M, Marra M A, Gersh B J, Wiebers D O, Petty G W, Seward J B. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin. Proc. 2001 May;76 (5):467–75. doi: 10.4065/76.5.467. [DOI] [PubMed] [Google Scholar]
- 19.Kistler Peter M, Sanders Prashanthan, Dodic Miodrag, Spence Steven J, Samuel Chrishan S, Zhao Chongxin, Charles Jennifer A, Edwards Glenn A, Kalman Jonathan M. Atrial electrical and structural abnormalities in an ovine model of chronic blood pressure elevation after prenatal corticosteroid exposure: implications for development of atrial fibrillation. Eur. Heart J. 2006 Dec;27 (24):3045–56. doi: 10.1093/eurheartj/ehl360. [DOI] [PubMed] [Google Scholar]
- 20.Lau Dennis H, Mackenzie Lorraine, Kelly Darren J, Psaltis Peter J, Worthington Michael, Rajendram Arumuga, Kelly Douglas R, Nelson Adam J, Zhang Yuan, Kuklik Pawel, Brooks Anthony G, Worthley Stephen G, Faull Randall J, Rao Mohan, Edwards James, Saint David A, Sanders Prashanthan. Short-term hypertension is associated with the development of atrial fibrillation substrate: a study in an ovine hypertensive model. Heart Rhythm. 2010 Mar;7 (3):396–404. doi: 10.1016/j.hrthm.2009.11.031. [DOI] [PubMed] [Google Scholar]
- 21.Lau Dennis H, Mackenzie Lorraine, Rajendram Arumuga, Psaltis Peter J, Kelly Douglas R, Spyropoulos Peter, Zhang Yuan, Olakkengil Santosh A, Russell Christine H, Brooks Anthony G, Faull Randall J, Saint David A, Kelly Darren J, Rao M Mohan, Worthley Stephen G, Sanders Prashanthan. Characterization of cardiac remodeling in a large animal "one-kidney, one-clip" hypertensive model. Blood Press. 2010 Apr;19 (2):119–25. doi: 10.3109/08037050903576767. [DOI] [PubMed] [Google Scholar]
- 22.Medi Caroline, Kalman Jonathan M, Spence Steven J, Teh Andrew W, Lee Geoffrey, Bader Ilona, Kaye David M, Kistler Peter M. Atrial electrical and structural changes associated with longstanding hypertension in humans: implications for the substrate for atrial fibrillation. J. Cardiovasc. Electrophysiol. 2011 Dec;22 (12):1317–24. doi: 10.1111/j.1540-8167.2011.02125.x. [DOI] [PubMed] [Google Scholar]
- 23.Matsuyama Narihisa, Tsutsumi Takeshi, Kubota Nami, Nakajima Toshiaki, Suzuki Hiroshi, Takeyama Youici. Direct action of an angiotensin II receptor blocker on angiotensin II-induced left atrial conduction delay in spontaneously hypertensive rats. Hypertens. Res. 2009 Aug;32 (8):721–6. doi: 10.1038/hr.2009.89. [DOI] [PubMed] [Google Scholar]
- 24.Velagaleti Raghava S, Gona Philimon, Chuang Michael L, Salton Carol J, Fox Caroline S, Blease Susan J, Yeon Susan B, Manning Warren J, O'Donnell Christopher J. Relations of insulin resistance and glycemic abnormalities to cardiovascular magnetic resonance measures of cardiac structure and function: the Framingham Heart Study. Circ Cardiovasc Imaging. 2010 May;3 (3):257–63. doi: 10.1161/CIRCIMAGING.109.911438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watanabe Masaya, Yokoshiki Hisashi, Mitsuyama Hirofumi, Mizukami Kazuya, Ono Taisuke, Tsutsui Hiroyuki. Conduction and refractory disorders in the diabetic atrium. Am. J. Physiol. Heart Circ. Physiol. 2012 Jul;303 (1):H86–95. doi: 10.1152/ajpheart.00010.2012. [DOI] [PubMed] [Google Scholar]
- 26.Kato Takeshi, Yamashita Takeshi, Sekiguchi Akiko, Tsuneda Takayuki, Sagara Kouichi, Takamura Masayuki, Kaneko Shuichi, Aizawa Tadanori, Fu Long-Tai. AGEs-RAGE system mediates atrial structural remodeling in the diabetic rat. J. Cardiovasc. Electrophysiol. 2008 Apr;19 (4):415–20. doi: 10.1111/j.1540-8167.2007.01037.x. [DOI] [PubMed] [Google Scholar]
- 27.Kato Takeshi, Yamashita Takeshi, Sekiguchi Akiko, Sagara Kouichi, Takamura Masayuki, Takata Shigeo, Kaneko Shuichi, Aizawa Tadanori, Fu Long-Tai. What are arrhythmogenic substrates in diabetic rat atria? J. Cardiovasc. Electrophysiol. 2006 Aug;17 (8):890–4. doi: 10.1111/j.1540-8167.2006.00528.x. [DOI] [PubMed] [Google Scholar]
- 28.Kato Takeshi, Yamashita Takeshi, Sekiguchi Akiko, Tsuneda Takayuki, Sagara Kouichi, Takamura Masayuki, Kaneko Shuichi, Aizawa Tadanori, Fu Long-Tai. Angiotensin II type 1 receptor blocker attenuates diabetes-induced atrial structural remodeling. J Cardiol. 2011 Sep;58 (2):131–6. doi: 10.1016/j.jjcc.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Li Lihua, Huang Chenghui, Ai Jing, Yan Binbin, Gu He, Ma Zhuosai, Li Angie Y, Xinyan Shang, Harden Scott W, Hatcher Jeff T, Wurster Robert D, Cheng Zixi Jack. Structural remodeling of vagal afferent innervation of aortic arch and nucleus ambiguus (NA) projections to cardiac ganglia in a transgenic mouse model of type 1 diabetes (OVE26). J. Comp. Neurol. 2010 Jul 15;518 (14):2771–93. doi: 10.1002/cne.22363. [DOI] [PubMed] [Google Scholar]
- 30.Mabe Abigail M, Hoover Donald B. Remodeling of cardiac cholinergic innervation and control of heart rate in mice with streptozotocin-induced diabetes. Auton Neurosci. 2011 Jul 05;162 (1-2):24–31. doi: 10.1016/j.autneu.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Chamberlain Alanna M, Agarwal Sunil K, Ambrose Marietta, Folsom Aaron R, Soliman Elsayed Z, Alonso Alvaro. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 2010 May;159 (5):850–6. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Watanabe Hiroshi, Tanabe Naohito, Yagihara Nobue, Watanabe Toru, Aizawa Yoshifusa, Kodama Makoto. Association between lipid profile and risk of atrial fibrillation. Circ. J. 2011;75 (12):2767–74. doi: 10.1253/circj.cj-11-0780. [DOI] [PubMed] [Google Scholar]
- 33.Wu C C, Su M J, Chi J F, Wu M H, Lee Y T. Comparison of aging and hypercholesterolemic effects on the sodium inward currents in cardiac myocytes. Life Sci. 1997;61 (16):1539–51. doi: 10.1016/s0024-3205(97)00733-9. [DOI] [PubMed] [Google Scholar]
- 34.Siasos Gerasimos, Tousoulis Dimitris, Oikonomou Evangelos, Zaromitidou Marina, Stefanadis Christodoulos, Papavassiliou Athanasios G. Inflammatory markers in hyperlipidemia: from experimental models to clinical practice. Curr. Pharm. Des. 2011 Dec;17 (37):4132–46. doi: 10.2174/138161211798764780. [DOI] [PubMed] [Google Scholar]
- 35.Wang Thomas J, Parise Helen, Levy Daniel, D'Agostino Ralph B, Wolf Philip A, Vasan Ramachandran S, Benjamin Emelia J. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004 Nov 24;292 (20):2471–7. doi: 10.1001/jama.292.20.2471. [DOI] [PubMed] [Google Scholar]
- 36.Wanahita Nikolas, Messerli Franz H, Bangalore Sripal, Gami Apoor S, Somers Virend K, Steinberg Jonathan S. Atrial fibrillation and obesity--results of a meta-analysis. Am. Heart J. 2008 Feb;155 (2):310–5. doi: 10.1016/j.ahj.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 37.Ayer Julian G J, Almafragy Hamid S, Patel Anushka A, Hellyer Rachael L, Celermajer David S. Body mass index is an independent determinant of left atrial size. Heart Lung Circ. 2008 Feb;17 (1):19–24. doi: 10.1016/j.hlc.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Aviles Ronnier J, Martin David O, Apperson-Hansen Carolyn, Houghtaling Penny L, Rautaharju Pentti, Kronmal Richard A, Tracy Russell P, Van Wagoner David R, Psaty Bruce M, Lauer Michael S, Chung Mina K. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003 Dec 16;108 (24):3006–10. doi: 10.1161/01.CIR.0000103131.70301.4F. [DOI] [PubMed] [Google Scholar]
- 39.Visser M, Bouter L M, McQuillan G M, Wener M H, Harris T B. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999 Dec 08;282 (22):2131–5. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- 40.Gami Apoor S, Pressman Gregg, Caples Sean M, Kanagala Ravi, Gard Joseph J, Davison Diane E, Malouf Joseph F, Ammash Naser M, Friedman Paul A, Somers Virend K. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004 Jul 27;110 (4):364–7. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 41.Ng Chee Yuan, Liu Tong, Shehata Michael, Stevens Steven, Chugh Sumeet S, Wang Xunzhang. Meta-analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am. J. Cardiol. 2011 Jul 01;108 (1):47–51. doi: 10.1016/j.amjcard.2011.02.343. [DOI] [PubMed] [Google Scholar]
- 42.Gami Apoor S, Hodge Dave O, Herges Regina M, Olson Eric J, Nykodym Jiri, Kara Tomas, Somers Virend K. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J. Am. Coll. Cardiol. 2007 Feb 06;49 (5):565–71. doi: 10.1016/j.jacc.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 43.Burstein Brett, Nattel Stanley. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J. Am. Coll. Cardiol. 2008 Feb 26;51 (8):802–9. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 44.Yue Lixia, Xie Jia, Nattel Stanley. Molecular determinants of cardiac fibroblast electrical function and therapeutic implications for atrial fibrillation. Cardiovasc. Res. 2011 Mar 01;89 (4):744–53. doi: 10.1093/cvr/cvq329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wakili Reza, Voigt Niels, Kääb Stefan, Dobrev Dobromir, Nattel Stanley. Recent advances in the molecular pathophysiology of atrial fibrillation. J. Clin. Invest. 2011 Aug;121 (8):2955–68. doi: 10.1172/JCI46315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chou Chung-Chuan, Chen Peng-Sheng. New concepts in atrial fibrillation: neural mechanisms and calcium dynamics. Cardiol Clin. 2009 Feb;27 (1):35–43, viii. doi: 10.1016/j.ccl.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kneller James, Zou Renqiang, Vigmond Edward J, Wang Zhiguo, Leon L Joshua, Nattel Stanley. Cholinergic atrial fibrillation in a computer model of a two-dimensional sheet of canine atrial cells with realistic ionic properties. Circ. Res. 2002 May 17;90 (9):E73–87. doi: 10.1161/01.res.0000019783.88094.ba. [DOI] [PubMed] [Google Scholar]
- 48.Dobrev Dobromir, Voigt Niels, Wehrens Xander H T. The ryanodine receptor channel as a molecular motif in atrial fibrillation: pathophysiological and therapeutic implications. Cardiovasc. Res. 2011 Mar 01;89 (4):734–43. doi: 10.1093/cvr/cvq324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gould Paul A, Yii Michael, McLean Catriona, Finch Samara, Marshall Tanneale, Lambert Gavin W, Kaye David M. Evidence for increased atrial sympathetic innervation in persistent human atrial fibrillation. Pacing Clin Electrophysiol. 2006 Aug;29 (8):821–9. doi: 10.1111/j.1540-8159.2006.00447.x. [DOI] [PubMed] [Google Scholar]
- 50.Gehi Anil K, Lampert Rachel, Veledar Emir, Lee Forrester, Goldberg Jack, Jones Linda, Murrah Nancy, Ashraf Ali, Vaccarino Viola. A twin study of metabolic syndrome and autonomic tone. J. Cardiovasc. Electrophysiol. 2009 Apr;20 (4):422–8. doi: 10.1111/j.1540-8167.2008.01363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo M A, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997 Aug 19;96 (4):1180–4. doi: 10.1161/01.cir.96.4.1180. [DOI] [PubMed] [Google Scholar]
- 52.Smit Marcelle D, Maass Alexander H, De Jong Anne Margreet, Muller Kobold Anneke C, Van Veldhuisen Dirk J, Van Gelder Isabelle C. Role of inflammation in early atrial fibrillation recurrence. Europace. 2012 Jun;14 (6):810–7. doi: 10.1093/europace/eur402. [DOI] [PubMed] [Google Scholar]
- 53.Chamberlain Alanna M, Agarwal Sunil K, Ambrose Marietta, Folsom Aaron R, Soliman Elsayed Z, Alonso Alvaro. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 2010 May;159 (5):850–6. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Umetani Ken, Kodama Yasushi, Nakamura Takamitsu, Mende Akira, Kitta Yoshinobu, Kawabata Kenichi, Obata Jun-ei, Takano Hajime, Kugiyama Kiyotaka. High prevalence of paroxysmal atrial fibrillation and/or atrial flutter in metabolic syndrome. Circ. J. 2007 Feb;71 (2):252–5. doi: 10.1253/circj.71.252. [DOI] [PubMed] [Google Scholar]
- 55.Watanabe Hiroshi, Tanabe Naohito, Watanabe Toru, Darbar Dawood, Roden Dan M, Sasaki Shigeru, Aizawa Yoshifusa. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study. Circulation. 2008 Mar 11;117 (10):1255–60. doi: 10.1161/CIRCULATIONAHA.107.744466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Echahidi Najmeddine, Mohty Dania, Pibarot Philippe, Després Jean-Pierre, O'Hara Gilles, Champagne Jean, Philippon François, Daleau Pascal, Voisine Pierre, Mathieu Patrick. Obesity and metabolic syndrome are independent risk factors for atrial fibrillation after coronary artery bypass graft surgery. Circulation. 2007 Sep 11;116 (11 Suppl):I213–9. doi: 10.1161/CIRCULATIONAHA.106.681304. [DOI] [PubMed] [Google Scholar]
- 57.Vyssoulis G, Karpanou E, Adamopoulos D, Kyvelou S-M, Tzamou V, Michaelidis A, Stefanadis C. Metabolic syndrome and atrial fibrillation in patients with essential hypertension. Nutr Metab Cardiovasc Dis. 2013 Feb;23 (2):109–14. doi: 10.1016/j.numecd.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 58.Echahidi Najmeddine, Mohty Dania, Pibarot Philippe, Després Jean-Pierre, O'Hara Gilles, Champagne Jean, Philippon François, Daleau Pascal, Voisine Pierre, Mathieu Patrick. Obesity and metabolic syndrome are independent risk factors for atrial fibrillation after coronary artery bypass graft surgery. Circulation. 2007 Sep 11;116 (11 Suppl):I213–9. doi: 10.1161/CIRCULATIONAHA.106.681304. [DOI] [PubMed] [Google Scholar]
- 59.Altieri Pablo I, Figueroa Yolanda, Banchs Héctor L, de Lamadrid José Hernández-Gil, Escobales Nelson, Crespo María. Higher incidence of atrial fibrillation in the metabolic syndrome: a Hispanic population study. Bol Asoc Med P R. 2012 Jun 29;103 (4):24–7. [PubMed] [Google Scholar]
- 60.Mohanty Sanghamitra, Mohanty Prasant, Di Biase Luigi, Bai Rong, Pump Agnes, Santangeli Pasquale, Burkhardt David, Gallinghouse Joseph G, Horton Rodney, Sanchez Javier E, Bailey Shane, Zagrodzky Jason, Natale Andrea. Impact of metabolic syndrome on procedural outcomes in patients with atrial fibrillation undergoing catheter ablation. J. Am. Coll. Cardiol. 2012 Apr 03;59 (14):1295–301. doi: 10.1016/j.jacc.2011.11.051. [DOI] [PubMed] [Google Scholar]
- 61.Chang Shih-Lin, Tuan Ta-Chuan, Tai Ching-Tai, Lin Yenn-Jiang, Lo Li-Wei, Hu Yu-Feng, Tsao Hsuan-Ming, Chang Chien-Jun, Tsai Wen-Chin, Chen Shih-Ann. Comparison of outcome in catheter ablation of atrial fibrillation in patients with versus without the metabolic syndrome. Am. J. Cardiol. 2009 Jan 01;103 (1):67–72. doi: 10.1016/j.amjcard.2008.08.042. [DOI] [PubMed] [Google Scholar]
- 62.Cai Liyun, Yin Yuehui, Ling Zhiyu, Su Li, Liu Zengzhang, Wu Jinjin, Du Huaan, Lan Xianbin, Fan Jinqi, Chen Weijie, Xu Yanping, Zhou Pei, Zhu Jifang, Zrenner Bernhard. Predictors of late recurrence of atrial fibrillation after catheter ablation. Int. J. Cardiol. 2013 Mar 20;164 (1):82–7. doi: 10.1016/j.ijcard.2011.06.094. [DOI] [PubMed] [Google Scholar]
- 63.Berkowitsch Alexander, Kuniss Malte, Greiss Harald, Wójcik Maciej, Zaltsberg Sergey, Lehinant Stefan, Erkapic Damir, Pajitnev Dimitri, Pitschner Heinz-Friedrich, Hamm Christian W, Neumann Thomas. Impact of impaired renal function and metabolic syndrome on the recurrence of atrial fibrillation after catheter ablation: a long term follow-up. Pacing Clin Electrophysiol. 2012 May;35 (5):532–43. doi: 10.1111/j.1540-8159.2012.03350.x. [DOI] [PubMed] [Google Scholar]
- 64.Healey Jeff S, Baranchuk Adrian, Crystal Eugene, Morillo Carlos A, Garfinkle Michael, Yusuf Salim, Connolly Stuart J. Prevention of atrial fibrillation with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysis. J. Am. Coll. Cardiol. 2005 Jun 07;45 (11):1832–9. doi: 10.1016/j.jacc.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 65.Kalus James S, Coleman Craig I, White C Michael. The impact of suppressing the renin-angiotensin system on atrial fibrillation. J Clin Pharmacol. 2006 Jan;46 (1):21–8. doi: 10.1177/0091270005283284. [DOI] [PubMed] [Google Scholar]
- 66.Schneider Markus P, Hua Tsushung A, Böhm Michael, Wachtell Kristian, Kjeldsen Sverre E, Schmieder Roland E. Prevention of atrial fibrillation by Renin-Angiotensin system inhibition a meta-analysis. J. Am. Coll. Cardiol. 2010 May 25;55 (21):2299–307. doi: 10.1016/j.jacc.2010.01.043. [DOI] [PubMed] [Google Scholar]
- 67.Dublin Sascha, Glazer Nicole L, Smith Nicholas L, Psaty Bruce M, Lumley Thomas, Wiggins Kerri L, Page Richard L, Heckbert Susan R. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med. 2010 Aug;25 (8):853–8. doi: 10.1007/s11606-010-1340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gu Jun, Liu Xu, Wang Xinhua, Shi Haifeng, Tan Hongwei, Zhou Li, Gu Jianing, Jiang Weifeng, Wang Yuanlong. Beneficial effect of pioglitazone on the outcome of catheter ablation in patients with paroxysmal atrial fibrillation and type 2 diabetes mellitus. Europace. 2011 Sep;13 (9):1256–61. doi: 10.1093/europace/eur131. [DOI] [PubMed] [Google Scholar]
- 69.Fauchier Laurent, Pierre Bertrand, de Labriolle Axel, Grimard Caroline, Zannad Noura, Babuty Dominique. Antiarrhythmic effect of statin therapy and atrial fibrillation a meta-analysis of randomized controlled trials. J. Am. Coll. Cardiol. 2008 Feb 26;51 (8):828–35. doi: 10.1016/j.jacc.2007.09.063. [DOI] [PubMed] [Google Scholar]
- 70.Liu Tong, Li Lijian, Korantzopoulos Panagiotis, Liu Enzhao, Li Guangping. Statin use and development of atrial fibrillation: a systematic review and meta-analysis of randomized clinical trials and observational studies. Int. J. Cardiol. 2008 May 23;126 (2):160–70. doi: 10.1016/j.ijcard.2007.07.137. [DOI] [PubMed] [Google Scholar]
- 71.Umetani Ken, Kodama Yasushi, Nakamura Takamitsu, Mende Akira, Kitta Yoshinobu, Kawabata Kenichi, Obata Jun-ei, Takano Hajime, Kugiyama Kiyotaka. High prevalence of paroxysmal atrial fibrillation and/or atrial flutter in metabolic syndrome. Circ. J. 2007 Feb;71 (2):252–5. doi: 10.1253/circj.71.252. [DOI] [PubMed] [Google Scholar]
- 72.Watanabe Hiroshi, Tanabe Naohito, Watanabe Toru, Darbar Dawood, Roden Dan M, Sasaki Shigeru, Aizawa Yoshifusa. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study. Circulation. 2008 Mar 11;117 (10):1255–60. doi: 10.1161/CIRCULATIONAHA.107.744466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu Hui-lan, Lu Xue-li, Guo Zhi-ping, Lin Jin-xiu. [Association between metabolic syndrome and incidence of atrial fibrillation in essential hypertensive patients without left ventricular hypertrophy]. Zhonghua Xin Xue Guan Bing Za Zhi. 2010 Jan;38 (1):15–9. [PubMed] [Google Scholar]
- 74.Tang Ri-bo, Gao Ling-yun, Dong Jian-zeng, Liu Xiao-hui, Liu Xing-peng, Wu Jia-hui, Long De-yong, Yu Rong-hui, Du Xin, Ma Chang-sheng. Metabolic syndrome in patients with atrial fibrillation in the absence of structural heart disease from a tertiary hospital in China. Chin. Med. J. 2009 Nov 20;122 (22):2744–7. [PubMed] [Google Scholar]
- 75.Tang Ri-Bo, Dong Jian-Zeng, Liu Xing-Peng, Long De-Yong, Yu Rong-Hui, Kalifa Jérôme, Ma Chang-Sheng. Metabolic syndrome and risk of recurrence of atrial fibrillation after catheter ablation. Circ. J. 2009 Mar;73 (3):438–43. doi: 10.1253/circj.cj-08-0832. [DOI] [PubMed] [Google Scholar]


