Abstract
Purpose: Hiatal hernia (HH) causes protrusion of the stomach into the chest cavity, directly impinging on the left atrium and possibly increasing predisposition to atrial arrhythmogenesis. However, such association has not been fully explored. The objective was to determine if an association between HH and atrial fibrillation (AF) exists and whether there are age- and sex-related differences.
Methods: Adult patients diagnosed with HH from 1976 to 2006 at Mayo Clinic Rochester, Minnesota, were evaluated for AF. The number of patients with AF and HH was compared to age- and sex-matched patients with AF reported in the general population. Long-term outcomes were compared to corresponding county and state populations.
Results: During the 30-year period, 111,429 patients were diagnosed with HH (mean age 61.4 ± 13.8 years, 47.9% male) and 7,865 patients (7.1%) also had a diagnosis of AF (mean age 73.1 ± 10.5 years; 55% male). In younger patients (<55 years), the occurrence of AF was 17.5-fold higher in men with HH and 19-fold higher in women with HH compared to the frequency of AF reported in the general population. Incidence of heart failure for patients with AF and HH was worse compared to the overall county population, but better than for those with AF. Similarly, mortality was worse in patients with AF and HH compared to the overall state population, but better than for those with AF in the county.
Conclusion: Hiatal hernia appears to be associated with increased frequency of AF in both men and women of all age groups, but particularly in young patients. Further studies are needed to investigate this possible association and underlying mechanism.
Keywords: Atrial Fibrillation, Hiatal hernia, Gastroesophageal reflux disease, Congestive heart failure, Stroke, Mortality
Introduction
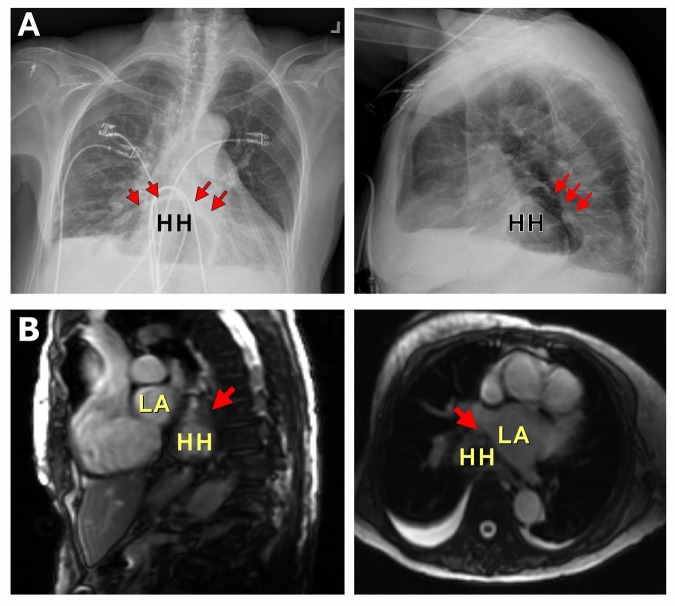
Hiatal hernia (HH) causes protrusion of the abdominal contents into the chest cavity, and can directly impinge on the left atrium (Figure 1).[1] The effect of this mechanical compression on the heart is not known. Cardiac compression from atrial masses is associated with various arrhythmias, and HH could potentially result in a similar effect.[2-6] The anatomical proximity of the left atrium to herniated gastric contents raises the possibility of mechanical irritation of the atria, autonomic neural connections or inflammation that may increase the risk for atrial fibrillation (AF). An association of esophagitis and frequent symptoms related to gastroesophageal reflux disease with the development of AF has been previously reported.[7-12] The reported reduction in frequency of recurrences of AF with the use of proton-pump inhibitors or following Nissen fundoplication also suggests a link between the gastrointestinal tract and atrial arrhythmias.[9,12]
Figure 1. A: Chest X-rays demonstrating large hiatal hernia (HH) (red arrows). Note close proximity to the left atrium (LA). B: Cardiac magnetic resonance imaging illustrating large HH (red arrows) in close proximity to the LA.
In this study, we sought to determine whether the presence of HH is associated with an increased risk for AF, particularly in young patients who lack the significant comorbidities that can otherwise increase predisposition of AF in the elderly. The overall prevalence of AF in patients with HH was compared to previously reported prevalence of AF in the general population.[13] Clinical outcomes of these patients with AF and HH also were compared to the expected outcomes of the corresponding county’s and state’s general populations and patients with AF.
Material and Methods
All patients older than 18 years with a Hospital International Classification of Disease Adaptation (HICDA) diagnosis code of HH who were seen at Mayo Clinic in Rochester, MN, in both the ambulatory and inpatient settings from Jan. 1, 1976, to Dec. 31, 2006, were assessed for the presence of AF. An electronic clinical database for patients who were given a HICDA diagnosis code for HH (05515 and 05535) and AF (04163 and 04164) during the specified time period and age group was maintained and reviewed. All patients who were given a coded diagnosis of AF, including lone, paroxysmal, persistent and permanent AF, as well as those who were given a diagnosis of HH by a physician were included in the study. The diagnosis of AF was confirmed by reviewing medical records. Detailed information about the severity of HH was not available. Patients were categorized by age and gender. The dates of initial diagnosis of HH, AF and cardiovascular events including heart failure, stroke and death were obtained. Patients given a diagnosis of AF after the diagnosis of HH were analyzed as well as the overall group of patients with both AF and HH. Risk factors that increase predisposition for AF – hypertension, diabetes mellitus, coronary artery disease, sleep apnea, valvular disease and heart failure at the time of diagnosis of HH – were identified (HICDA and International Classification of Diseases-9 codes 34128430, 02500000, 414.00, 780.58, 03950112, 04279113). The study population was compared to the prevalence of AF reported in the general population by Go et al. based on the similar age and gender breakdown.[13] Clinical outcomes, including heart failure and transient ischemic attack (TIA) or stroke, in the study population were assessed in a similar fashion using the HICDA codes documented by a physician. These outcomes then were compared to the expected events in the corresponding county’s general population. These events for patients with AF and HH then were compared to clinical outcomes reported in patients with AF.[14-16] Mortality was determined from medical records and the Social Security Death Index. All-cause mortality of the study population was compared to the expected death rate in the state population for age- and gender- matched controls. The study was approved by the Mayo Clinic Institutional Review Board.
Statistical Analysis
Data are summarized using frequencies and percentages for categorical variables and mean ± standard deviation for continuous variables. The Kaplan-Meier method was used to generate survival free-of-endpoint curves for stroke, heart failure and death in patients with AF and HH. Observed curves for each of these endpoints were compared to expected outcomes using one-sample log-rank tests. Expected curves were constructed using population-based studies of each of the outcomes. Expected mortality was constructed from the corresponding state death data.
Results
Hiatal Hernia Is Associated With Increased Frequency of Atrial Fibrillation
A total of 111,429 patients (mean age 61.4 ± 13.8 years, 53,430 males [47.9%]) with a diagnosis of HH were seen during the 30-year study period. Of these, 7,865 patients (7.1%; mean age 73.1 ± 10.5 years) also had a diagnosis of AF (4,337 [55%] men and 3,528 [45%] women). The baseline characteristics of patients with AF and HH compared to those with AF as reported in the general population by Go et al.[13] are summarized in Table 1. Despite a similar age range (mean age 73.1 ± 10.5 vs. 71.2 ± 12.2 years), the prevalence of common conditions, such as coronary artery disease, heart failure, valvular disease and hypertension that predispose to AF, was lower in the HH and AF group compared to the population with AF.
Table 1. Comparison of Baseline Characteristics of Patients With AF And HH vs. AF as Reported in the Literature.
AF = atrial fibrillation; CHF = congestive heart failure; HH = hiatal hernia; NR = not reported. *Data taken from ATRIA study, Go et al. JAMA 200113
| AF* (%) n=17,974 | AF and HH (%) n=7,865 | |
|---|---|---|
| Mean age (years) | 71.2 ± 12.2 | 73.1 ± 10.5 |
| Sex (male) | 57 | 55 |
| Hypertension | 49 | 40 |
| Hyperlipidemia | NR | 17 |
| Diabetes | 17 | 16 |
| Coronary artery disease | 35 | 20 |
| Sleep apnea | NR | 4 |
| CHF | 29 | 10 |
| Valvular disease | 5 | 2 |
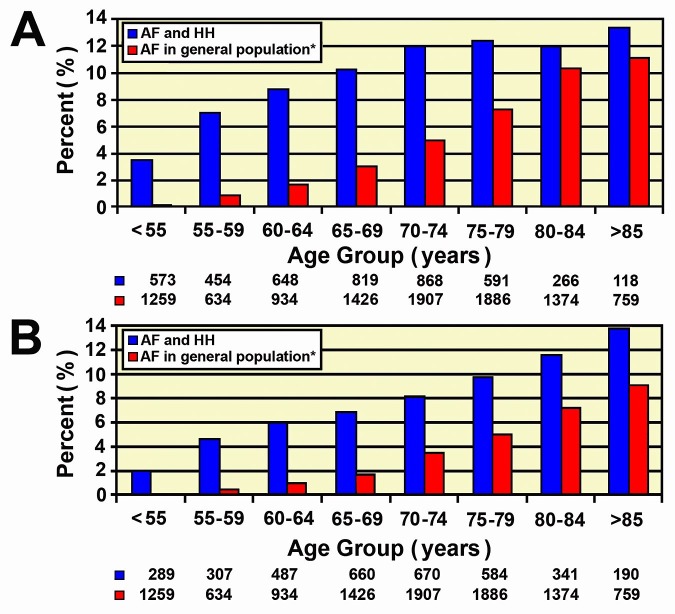
In both sexes, the number of individuals with AF was higher in patients with HH compared to what has been reported for the general population throughout all age groups (Figure 2).[13] In young men (<55 years) with HH, AF was present in 3.5%, a 17.5-fold higher prevalence compared to the 0.2% reported in this group by Go et al.13 (Figure 2). Other studies have found low prevalence rates for young patients with AF,17-20 similar to Go et al.[13] Likewise, the occurrence of AF in young women (<55 years) with HH was 19-fold higher than the prevalence of AF reported in the general population in the same age group (1.9% vs. 0.1%) (Figure 2). As illustrated in Figure 2, the higher prevalence of AF in patients with HH was consistently seen across all age groups in both men and women, although the differences diminished in the older age groups. Men with HH aged 55-59 years had a 7.8-fold increase in the prevalence of AF, 60-64 years a 5.2-fold increase, 65-69 years a 3.4-fold increase, 70-74 years a 2.4-fold increase, 80-84 years a 1.2-fold increase and > 85 years a 1.2-fold increase. Similarly, women with HH aged 55-59 years had an 11.7-fold increase in the prevalence of AF, 60-64 years a 5.9- fold increase, 65-69 years a 4-fold increase, 70-74 years a 2.4-fold increase, 75-79 years a 2-fold increase, 80-84 years a 1.6-fold increase and > 85 years a 1.5-fold increase.
Figure 2. A: Men with atrial fibrillation (AF) and hiatal hernia (HH) compared to AF reported in the general population* B: Women with AF and HH compared to AF reported in the general population*.
*Data taken from ATRIA study, Go et al. JAMA 2001 [13]
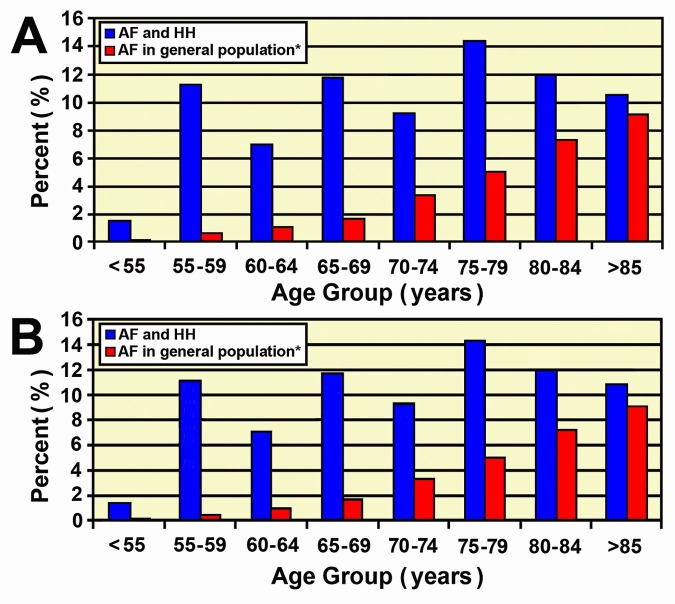
When comparing the occurrence of AF in patients with HH over the same one-year period (July 1, 1996, to Dec. 1, 1997) as Go et al.[13] there was a comparable trend (Figure 3). Men with HH aged < 55 years had a 21-fold increase in the prevalence of AF, 55-59 years a 12-fold increase, 60-64 years an 11-fold increase, 65-69 years a 7-fold increase, 70-74 years a 3-fold increase, 75-79 years a 2-fold increase, 80-84 years a 2-fold increase and > 85 years a 2-fold increase. Women with HH aged <55 years had a 16-fold increase in the prevalence of AF, 55-59 years a 28-fold increase, 60-64 years a 7-fold increase, 65-69 years a 7-fold increase, 70-74 years a 3-fold increase, 75-79 years a 3-fold increase, 80-84 years a 2-fold increase and > 85 years a 1-fold increase.
Figure 3. A: Men with atrial fibrillation (AF) and hiatal hernia (HH) compared to AF reported in the general population* from July 1, 1996, to Dec. 1, 1997 B: Women with AF and HH compared to AF reported in the general population* from July 1, 1996, to Dec. 1, 1997.
AF = atrial fibrillation; CHF = congestive heart failure; HH = hiatal hernia; NR = not reported. *Data taken from ATRIA study, Go et al. JAMA 200113
Cardiovascular Events in Patients With Atrial Fibrillation and Hiatal Hernia
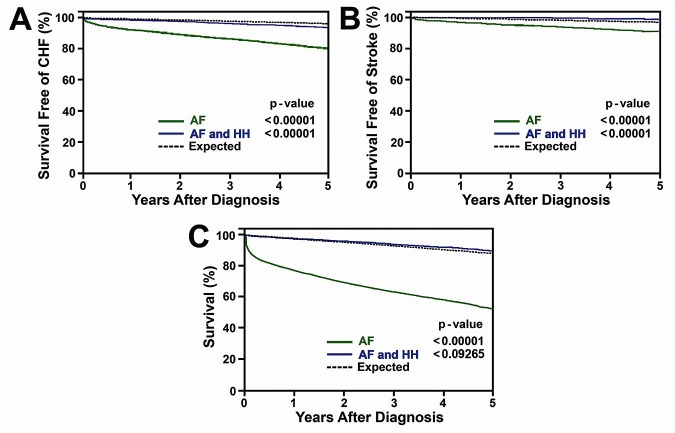
A total of 1,746 patients had heart failure, 810 patients with AF and HH developed TIA or stroke and 2,810 patients died during the 30-year follow-up period. Although the rate of heart failure development in patients with AF and HH was significantly higher (p<0.0001) when compared to the expected outcomes for the county’s general population, it was significantly better (p<0.00001) than for those with AF in this population (Figure 4).[15] At five years, survival free of stroke was 98.7% in the study population of AF and HH compared with 90.8% in the AF group and 96.6% in the expected county population. Survival free of heart failure at five years was 93.9% in the AF and HH group, 81% in the AF group, and 96.3% in the expected county group. The expected survival at five years was 90% in the AF and HH population, 55.4% in the AF population and 88.1% in the expected state population (Figure 4).
Figure 4. Five-year follow-up comparing patients with atrial fibrillation (AF), AF and HH, and expected population for A: congestive heart failure (CHF), B: stroke and C: mortality.
Discussion
The novel finding of our study is demonstration of an association between HH and AF, with a greater likelihood of developing AF in patients with HH. The prevalence of AF in the general population is age-dependent and generally reported as approximately 1%.[13] The occurrence of AF in patients with HH in our study was 7.1%. This difference was strikingly greater in younger age groups in both men and women. When broken down by age and gender, we found 17.5-fold and 19-fold higher prevalences of AF in men and women younger than 55 years with HH, respectively. A similar trend was found when comparing the occurrence of AF in patients with HH over the same one-year period used by Go et al.[13] with a 21-fold increase in men < 55 years and a 16-fold increase in women < 55 years, suggesting that secular differences over time with the 30-year follow-up were less of a factor. These differences in the prevalence of AF persisted with advancing age, but the magnitude of the difference between the HH group and the general population diminished, likely due to the presence of other comorbidities and factors in addition to HH that promote the development of AF (Table 1). The higher prevalence of AF in the young HH group, despite reduced prevalence of risk factors for AF such as hypertension, coronary artery disease and congestive heart failure as compared to the AF group, suggests that HH may increase the risk for AF.
Anatomically, the esophagus lies directly behind the left atrium and protrusion of abdominal contents into this limited space can predispose the atria to mechanical compression and stretch that increases the likelihood of developing AF (Figure 1). Hiatal hernias are frequently associated with gastroesophageal reflux and esophagitis,[21] which could lead to local inflammation of the esophagus and surrounding structures. The proximity of the esophagus, and consequently of the HH to the left atrium, could lead to extension of this inflammation that could contribute to the development of AF by mechanical or chemical/neural influences mediated through vagal or sympathetic nervous systems.[7,9,10,12,22-26] Huang et al. recently reported an increased risk of AF in patients with gastroesophageal reflux disease (GERD) as an independent predictor.[27] They postulated that the increased vagal tone observed in patients with GERD could lead to an increased risk of AF. The presence of a HH may exacerbate GERD and consequently a similar mechanism of vagal stimulation could be attributed to the increased prevalence of AF seen in patients with HH. The presence of cardiac masses has been associated with development of AF and atrial flutter, and similar atrial compression by the presence of HH, associated inflammation of the esophagus or irritation of the autonomic neural plexus present in this region, particularly after heavy meals, can influence the development of AF and other atrial arrhythmias.[03,5,6,28]
The hypothesis that presence of HH contributes to the development of AF is supported by previous reports. Schilling et al.[26] described a case of atrial flutter that resolved in a patient with a large paraesophageal hernia after surgical repair of the hernia. Duygu et al.[12] also reported a case of paroxysmal atrial flutter that was refractory to electrical cardioversion and calcium channel blockers in a patient with severe acid reflux and daily heartburn symptoms secondary to a large HH. However, after instituting proton-pump inhibitor therapy, normal sinus rhythm was restored and maintained at oneyear follow-up. In another patient with a large paraesophageal HH and postprandial AF, Nissen fundoplication suppressed recurrences of AF.[25] Other reports have demonstrated electrocardiographic changes, including ST-segment elevation, T-wave inversion and sinus bradycardia, that can occur in patients with HH.[4,29] Studies defining a definitive causal relationship with HH and mechanistic insights are warranted.
The occurrence of heart failure, stroke or TIA and death during the five-year follow-up period after the diagnosis of HH was compared to the expected event rates for heart failure and stroke or TIA in the county and the overall mortality in the state. The event rates for patients with AF and HH also were compared to the overall rates in patients with AF in the county population.[14-16] The incidence of these complications was significantly less than that described in the overall AF population, suggesting that patients with AF associated with HH might have a better prognosis than patients with AF without HH (Figure 4). There are a few possibilities for this finding. Patients with AF and HH are more likely to seek medical attention given the presence of a hiatal hernia and related symptoms and, thus, may be treated more aggressively for their AF with medications such as anticoagulation. Another possibility may be that patients with AF and HH represent a unique subgroup of patients with AF that are actually less likely to develop AF-related complications due to a different mechanism for the AF. These patients may be more likely to have lone AF and less structural heart disease but still develop AF due to the mechanical/neural factors from the effect of the HH on the atria and, consequently, have a lower complication rate. Our study suggests that the natural history of AF in patients with HH may be different from AF associated with structural heart disease.
Limitations
The findings of this retrospective study should be considered in the context of the limitations of such a study design that cannot account for other confounding factors predisposing to AF not reported in the medical record. Our study encompassed all types of AF including lone, paroxysmal, persistent and permanent AF, which may affect the degree to which HH played a role in the development of AF. Although the diagnosis of AF was confirmed by reviewing medical records, the frequency and duration of AF episodes could not be assessed. Similarly, the severity of HH could not be assessed from the retrospective review of the records. Echocardiographic assessment was not performed or available in the majority of patients, and, therefore, the impact of HH on atrial function or dimensions or their contribution to the development of AF could not be determined. Further prospective studies investigating patients with HH and minimum risk factors for AF are needed to confirm the novel observations described here and to provide additional evidence to support the association between HH and AF.
Conclusions
We present a hypothesis-generating study that suggests the presence of hiatal hernia may trigger development of atrial fibrillation, particularly in younger patients. Further prospective investigation is needed to confirm this association and the underlying mechanisms.
Acknowledgements
The authors gratefully acknowledge Joe Grundle and Katie Klein for the editorial preparation of the manuscript and Brian Miller and Brian Schurrer for their help in preparing illustrations.
Disclosures
No disclosures relevant to this article were made by the authors.
References
- 1.Khouzam Rami N, Akhtar Asif, Minderman Daniel, Kaiser Jacqueline, D'Cruz Ivan A. Echocardiographic aspects of hiatal hernia: A review. J Clin Ultrasound. 2007 May;35 (4):196–203. doi: 10.1002/jcu.20312. [DOI] [PubMed] [Google Scholar]
- 2.Bolis S, Bregani E R, Rossini F, Schiavina R, Pogliani E M. Atrial flutter followed by sick sinus syndrome as presenting symptoms of B-cell malignant non-Hodgkin lymphoma involving the heart. Haematologica. 1993 Sep 1;78 (5):332–4. [PubMed] [Google Scholar]
- 3.Fujisaki Joji, Tanaka Takahiro, Kato Jyundai, Saito Tetsuya, Yano Kohei, Shimizu Yutaka, Sada Toshikatsu, Kitazume Kouichi, Fujita Akira, Kira Yuji. Primary cardiac lymphoma presenting clinically as restrictive cardiomyopathy. Circ. J. 2005 Feb;69 (2):249–52. doi: 10.1253/circj.69.249. [DOI] [PubMed] [Google Scholar]
- 4.Hokamaki Jun, Kawano Hiroaki, Miyamoto Shinzo, Sugiyama Seigo, Fukushima Ryuichiro, Sakamoto Tomohiro, Yoshimura Michihiro, Ogawa Hisao. Dynamic electrocardiographic changes due to cardiac compression by a giant hiatal hernia. Intern. Med. 2005 Feb;44 (2):136–40. doi: 10.2169/internalmedicine.44.136. [DOI] [PubMed] [Google Scholar]
- 5.Linhart Markus, Lickfett Lars, Hammerstingl Christoph, Tiemann Klaus, Nickenig Georg, Lewalter Thorsten. Paroxysmal atrial flutter caused by cardiac lymphoma. Pacing Clin Electrophysiol. 2006 Jun;29 (6):682–4. doi: 10.1111/j.1540-8159.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 6.Thompson Michael A, Harker-Murray Amy, Locketz Adam J, Chareonthaitawee Panithaya. Unusual lymphoma manifestations: case 2. Myocardial lymphoma presenting as atrial flutter. J. Clin. Oncol. 2004 Feb 01;22 (3):558–60. doi: 10.1200/JCO.2004.12.100. [DOI] [PubMed] [Google Scholar]
- 7.Bunch T Jared, Packer Douglas L, Jahangir Arshad, Locke G Richard, Talley Nicholas J, Gersh Bernard J, Roy Ranjini R, Hodge David O, Asirvatham Samuel J. Long-term risk of atrial fibrillation with symptomatic gastroesophageal reflux disease and esophagitis. Am. J. Cardiol. 2008 Nov 01;102 (9):1207–11. doi: 10.1016/j.amjcard.2008.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kunz Jeffrey S, Hemann Brian, Edwin Atwood J, Jackson Jeffrey, Wu Timothy, Hamm Carolyn. Is there a link between gastroesophageal reflux disease and atrial fibrillation? Clin Cardiol. 2009 Oct;32 (10):584–7. doi: 10.1002/clc.20660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weigl Manuela, Gschwantler Michael, Gatterer Edmund, Finsterer Josef, Stöllberger Claudia. Reflux esophagitis in the pathogenesis of paroxysmal atrial fibrillation: results of a pilot study. South. Med. J. 2003 Nov;96 (11):1128–32. doi: 10.1097/01.SMJ.0000084294.77504.4B. [DOI] [PubMed] [Google Scholar]
- 10.Gerson Lauren B, Gerson Lauren, Friday Karen, Triadafilopoulos George. Potential relationship between gastroesophageal reflux disease and atrial arrhythmias. J. Clin. Gastroenterol. 2006 Oct;40 (9):828–32. doi: 10.1097/01.mcg.0000225571.42890.a5. [DOI] [PubMed] [Google Scholar]
- 11.Gordon Jackie, Saleem Syed M, Ngaage Dumbor L, Thorpe James A C. Swallow syncope associated with paroxysmal atrial fibrillation. Eur J Cardiothorac Surg. 2002 Mar;21 (3):587–90. doi: 10.1016/s1010-7940(01)01172-1. [DOI] [PubMed] [Google Scholar]
- 12.Duygu Hamza, Ozerkan Filiz, Saygi Serkan, Akyüz Serdar. Persistent atrial fibrillation associated with gastroesophageal reflux accompanied by hiatal hernia. Anadolu Kardiyol Derg. 2008 Apr;8 (2):164–5. [PubMed] [Google Scholar]
- 13.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 14.Miyasaka Yoko, Barnes Marion E, Bailey Kent R, Cha Stephen S, Gersh Bernard J, Seward James B, Tsang Teresa S M. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J. Am. Coll. Cardiol. 2007 Mar 06;49 (9):986–92. doi: 10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 15.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter, Seward James B, Iwasaka Toshiji, Tsang Teresa S M. Incidence and mortality risk of congestive heart failure in atrial fibrillation patients: a community-based study over two decades. Eur. Heart J. 2006 Apr;27 (8):936–41. doi: 10.1093/eurheartj/ehi694. [DOI] [PubMed] [Google Scholar]
- 16.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Seward James B, Bailey Kent R, Iwasaka Toshiji, Tsang Teresa S M. Time trends of ischemic stroke incidence and mortality in patients diagnosed with first atrial fibrillation in 1980 to 2000: report of a community-based study. Stroke. 2005 Nov;36 (11):2362–6. doi: 10.1161/01.STR.0000185927.63746.23. [DOI] [PubMed] [Google Scholar]
- 17.Heeringa Jan, van der Kuip Deirdre A M, Hofman Albert, Kors Jan A, van Herpen Gerard, Stricker Bruno H Ch, Stijnen Theo, Lip Gregory Y H, Witteman Jacqueline C M. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur. Heart J. 2006 Apr;27 (8):949–53. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- 18.Kannel W B, Wolf P A, Benjamin E J, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am. J. Cardiol. 1998 Oct 16;82 (8A):2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- 19.Onundarson P T, Thorgeirsson G, Jonmundsson E, Sigfusson N, Hardarson T. Chronic atrial fibrillation--epidemiologic features and 14 year follow-up: a case control study. Eur. Heart J. 1987 May;8 (5):521–7. doi: 10.1093/oxfordjournals.eurheartj.a062312. [DOI] [PubMed] [Google Scholar]
- 20.DeWilde S, Carey I M, Emmas C, Richards N, Cook D G. Trends in the prevalence of diagnosed atrial fibrillation, its treatment with anticoagulation and predictors of such treatment in UK primary care. Heart. 2006 Aug;92 (8):1064–70. doi: 10.1136/hrt.2005.069492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fujiwara Yasuhiro, Arakawa Tetsuo. Epidemiology and clinical characteristics of GERD in the Japanese population. J. Gastroenterol. 2009;44 (6):518–34. doi: 10.1007/s00535-009-0047-5. [DOI] [PubMed] [Google Scholar]
- 22.Issac Tim T, Dokainish Hisham, Lakkis Nasser M. Role of inflammation in initiation and perpetuation of atrial fibrillation: a systematic review of the published data. J. Am. Coll. Cardiol. 2007 Nov 20;50 (21):2021–8. doi: 10.1016/j.jacc.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 23.Shaker Reza. Gastroesophageal reflux disease: beyond mucosal injury. J. Clin. Gastroenterol. 2007 Jul;41 Suppl 2 ():S160–2. doi: 10.1097/MCG.0b013e318042d660. [DOI] [PubMed] [Google Scholar]
- 24.Hou Yinglong, Scherlag Benjamin J, Lin Jiaxiong, Zhang Ying, Lu Zhibing, Truong Kim, Patterson Eugene, Lazzara Ralph, Jackman Warren M, Po Sunny S. Ganglionated plexi modulate extrinsic cardiac autonomic nerve input: effects on sinus rate, atrioventricular conduction, refractoriness, and inducibility of atrial fibrillation. J. Am. Coll. Cardiol. 2007 Jul 03;50 (1):61–8. doi: 10.1016/j.jacc.2007.02.066. [DOI] [PubMed] [Google Scholar]
- 25.Gillinov A Marc, Rice Thomas W. Prandial atrial fibrillation: off-pump pulmonary vein isolation with hiatal hernia repair. Ann. Thorac. Surg. 2004 Nov;78 (5):1836–8. doi: 10.1016/S0003-4975(03)01434-6. [DOI] [PubMed] [Google Scholar]
- 26.Schilling R J, Kaye G C. Paroxysmal atrial flutter suppressed by repair of a large paraesophageal hernia. Pacing Clin Electrophysiol. 1998 Jun;21 (6):1303–5. doi: 10.1111/j.1540-8159.1998.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 27.Huang Chin-Chou, Chan Wan-Leong, Luo Jiing-Chyuan, Chen Yu-Chun, Chen Tzeng-Ji, Chung Chia-Min, Huang Po-Hsun, Lin Shing-Jong, Chen Jaw-Wen, Leu Hsin-Bang. Gastroesophageal reflux disease and atrial fibrillation: a nationwide population-based study. PLoS ONE. 2012;7 (10) doi: 10.1371/journal.pone.0047575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zaharia L, Gill P S. Primary cardiac lymphoma. Am. J. Clin. Oncol. 1991 Apr;14 (2):142–5. doi: 10.1097/00000421-199104000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Marks P, Thurston J G. Sinus bradycardia with hiatus hernia. Am. Heart J. 1977 Jan;93 (1):30–2. doi: 10.1016/s0002-8703(77)80168-3. [DOI] [PubMed] [Google Scholar]