Abstract
Objective
The purpose of this study was to investigate the relationship between knowledge on arterial hypertension (AH) and its management, and adherence to pharmaceutical treatment.
Methods
The study included 233 patients diagnosed with AH and treated with hypotensive drugs for at least 1 year. The 8-item © Morisky Medication Adherence Scale (MMAS-8) and the Hypertension Knowledge-Level Scale (HK-LS) were used.
Results
Sixty-three percent of the patients had a low level of knowledge on AH, with the smallest proportion of correct answers provided for items related to non-pharmaceutical treatment, diet, hypertension definition, and drug adherence. When compared to patients with a high level of knowledge, those with a low knowledge had lower scores in the MMAS (6.45±1.45 vs 7.08±1.04; P=0.038). Multiple-factor analysis showed that statistically significant independent determinants of good adherence included a high level of knowledge (β=0.208; P=0.001), non-pharmaceutical treatment (β=0.182; P=0.006), and frequent blood pressure measurements (β=0.183; P=0.004). The most significant factor in MMAS was knowledge in the “drug adherence” domain (ρ=0.303; P<0.001).
Conclusion
Patients’ knowledge on hypertension is a significant independent determinant of good adherence. Other independent determinants include non-pharmaceutical treatment and regular blood pressure measurements.
Implication for practice
The identification of knowledge deficits as a factor contributing to lack of adherence and poor hypertension control remains a key challenge for multidisciplinary team caring for patients with hypertension.
Keywords: medication adherence, arterial hypertension, medical knowledge
Introduction
The prevalence of hypertension in the general population is ~30%–45% and increases with age. According to the World Health Organization (WHO) data, hypertension is found in 47% of the population in underdeveloped or developing countries and in 49% in developed countries.1 The number of adults with hypertension is predicted to increase by 60% by the year 2025, to a total of 1.56 billion adults.1
The population-wide effectiveness of hypertension treatment is still insufficient. The primary factor contributing to an unsatisfactory response to pharmaceutical treatment is poor medication adherence. The management and control of hypertension are possible with a combination of medication and strict lifestyle changes. Published studies indicate that ~60% of patients treated for hypertension discontinue treatment within 6 months.2 Apart from adverse effects and inadequate blood pressure (BP) control despite treatment, the most common causes of lack of adherence are believed to include a lack of patient involvement in the treatment process or motivation to continue it and a lack of information on the disease and its treatment, especially detailed information on dosage.3
An important component to control hypertension is knowledge, which is relative to lower rates of ceasing interventions, following the interventions behavior, and better control on disease by patients. As a result, careful evaluation of hypertension has been considered as an inseparable part of general care of the patients.
This results from poor awareness of the consequences of nontreatment, mistrust of the physician, and negating the necessity of treatment when symptoms are not present.4 Other than deficits in knowledge, factors of significance for adherence are reported to include sociodemographic and clinical (comorbidities, multidrug treatment) characteristics, as well as patients’ health-related beliefs.5,6
Observations indicate that patients with hypertension are least knowledgeable on normal BP values and on lifestyle changes required during the treatment process.7 The appropriate lifestyle changes are fundamental for preventing hypertension. Clinical studies prove that appropriate lifestyle modifications can have a hypotensive effect comparable to be seen with single-agent pharmaceutical treatment.8 Lifestyle changes may be a safe and effective way of preventing or delaying hypertension, avoiding or delaying pharmaceutical treatment in patients with grade 1 hypertension, and reducing BP in patients who are already treated, which allow dosages of hypotensive drugs to be reduced.9
European Society of Cardiology (ESC) guidelines include salt restriction, moderation of alcohol consumption, high consumption of vegetables and fruits and low-fat diet, weight reduction and maintenance, and regular physical exercise as lifestyle measures that have been shown to be capable of reducing BP.10
In Poland, hypotensive drug treatment is found to be effective in 28% of male and 29% of female patients.11 At the same time, as many as 39% of men and 29% of women diagnosed with hypertension do not start their treatment, which indicates poor awareness of long-term complications of hypertension.11 Epidemiological studies performed in Europe and in the United States demonstrate that a higher effectiveness of hypertension treatment – as high as 63% – is achievable. The European Society of Hypertension (ESH) and the Polish Society of Hypertension consider patient education aimed at enhancing their knowledge and motivation, and covering especially non-pharmaceutical treatment, to be a primary method of managing all patients with hypertension.12 Such patients should be managed by a therapeutic team. Nursing assistance may prove particularly significant in the process of lifestyle modification, where long-term adherence remains very low. Published studies demonstrate that team-based care is more effective than standard treatment, especially if it involves nurses and/or pharmacists.13 The beneficial effect of the involvement of pharmacists and nurses has been obtained when their tasks involved patient education, behavioral and medical counseling, assessment of adherence to treatment, and, for pharmacists, interaction with physicians in the area of guideline-based therapy.13–15
The papers on the level of knowledge of Polish patients prove the insufficient knowledge on arterial hypertension (AH) and its complications.16 The connection between sociodemographic variables and the level of knowledge on hypertension is widely discussed in the literature.17,18 However, there are small number of papers focusing on the association between the level of knowledge and the adherence to drug recommendations. Information on relationship between patients’ knowledge on hypertension and adherence may be helpful in the prevention of complication, treatment planning, and better patient health control.
The purpose of the study was to investigate the relationship between knowledge on hypertension and on its management, and adherence to pharmaceutical treatment in hypertension.
The investigation included the following questions:
What is the knowledge level of Polish patients with hypertension treated with at least one hypotensive drug?
How does adherence differ depending on knowledge regarding hypertension?
Does a correlation exist between knowledge and adherence, and what other variables affect adherence?
Materials and methods
Participants
The study was performed in the Kosmonautów health center in Wroclaw. Data were collected from January 2015 through November 2015. Eligible patients were consecutively selected by the physicians, who informed them of the study objectives and recruited all patients who agreed to participate. All the study participants gave informed consent. The survey included 233 patients (124 females) aged between 32 and 90 years (mean age 63±15 years) diagnosed with hypertension at least 1 year before (which is in line with the ESH guidelines),10 treated for hypertension with at least one hypotensive agent, and who had been patients of the health center for at least 6 months.
The inclusion criteria were as follows: 1) clinically confirmed hypertension diagnosis, 2) the patient’s written informed consent, and 3) age ≥18 years. The exclusion criteria were as follows: 1) moderate to severe dementia (defined as mini-mental score ≤15),19 2) lack of consent, and 3) patients with severe concomitant diseases, which could affect adherence to therapeutic guidelines, were excluded from the study due to their complex treatment schemes and the possibility of adverse effects and reactions occurring as a result of the use of multiple medications. Patients were selected by a panel consisting of a physician and a nurse – specialist in the field of cardiac nursing. The sample group was homogeneous and could be subjected to statistical analysis.
Patients were divided into two groups based on their knowledge level. The patients’ knowledge was assessed using the Polish version of the Hypertension Knowledge-Level Scale (HK-LS). According to the asymmetrical answer distribution (Figure 1), the group was divided into two subgroups depending on the score:
≤17 points – low level of knowledge on hypertension (n=147);
between 18 and 22 points – high level of knowledge on hypertension (n=86).
Figure 1.
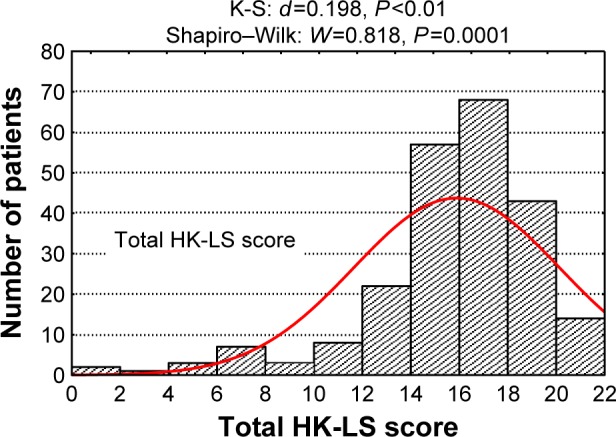
Histogram of hypertension knowledge scores obtained by 233 patients.
Abbreviations: HK-LS, Hypertension Knowledge-Level Scale; K-S, Kolmogorov-Smirnov test.
Ethical consideration
The study was approved by the Bioethics Committee (approval no KB 136/2015); all patients recruited to the study provided their informed and voluntary written consent to participate in the study.
Instruments
Two validated instruments were used: the 8-item © Morisky Medication Adherence Scale (MMAS-8) and the HK-LS. Furthermore, the patients were interviewed and their medical records were analyzed to gather detailed information. The instruments were distributed by a cardiac nurse during patients’ follow-up appointments for continuing hypotensive treatment.
Adherence
Self-reported medication adherence was assessed using the MMAS-8, previously translated and validated. Self-reported MMAS-8 is simple to administer and is feasible and economical in clinical practice. The MMSA-8 was designed to facilitate the identification of barriers to and behaviors associated with adherence to chronic medication.20,21 The tool has been confirmed as reliable and significantly associated with BP control in individuals with hypertension, as well as with antihypertensive medication pharmacy fill rates. MMAS-8 scores may range from 0 to 8, with scores of <6, 6–8, and 8 reflecting low, medium, and high adherence, respectively.22 The questionnaire has very good psychometric properties (Cronbach’ s alpha =0.81).
Knowledge
The HK-LS assessed respondents’ knowledge in defining hypertension, lifestyle, medical treatment, drug compliance, diet, and complication of hypertension. Each item was a full sentence that was either correct or incorrect. And each item was prepared as part of a standard answer (correct, incorrect, or do not know). To assess the content validity of the scale to identify whether items were or were not representative of the knowledge level of hypertension, the opinions of experts were requested through an assessment form. The expert opinions were Evaluated and in the Polish language version provided all the questions.
The scale included 22 items divided into six subdimensions. The expressions are incorrect in nine items. Each correct answer is worth 1 point. Incorrect statements are encoded inversely to the other items. The maximum score is 22 for the entire scale. The minimum score is zero for the entire scale and for all subdimensions.23 The questionnaire has adequate psychometric properties (Cronbach’s alpha =0.81).
Possible determinants of adherence
Variables that may affect the aspects of adherence studied include ESC hypertension grade, disease duration, type of treatment and of hypotensive drugs administered, presence of comorbidities, self-control and keeping a self-control journal, and sociodemographic factors (age, sex, living situation, and education).
Statistical analysis
The level of knowledge was evaluated by the HK-LS questionnaire. The maximum score was 22 points. The distribution of scores obtained is shown on the histogram in Figure 1. The distribution is highly asymmetrical, with a left skew, that is, a small proportion of low scorers. Therefore, at a further stage, the following classification criteria were used: ≤17 points – low level of knowledge on hypertension, points between 18 and 22 – high level of knowledge on hypertension.
For quantitative variables, the normality of empirical distributions was verified using the Shapiro–Wilk test. Subsequently, mean values and standard deviations were calculated, and mean values were compared between the two patient groups in one-way analysis of variance. If the null hypothesis of no differences between groups was rejected, post hoc tests were performed (multiple comparisons: least significant difference).
Qualitative and ordinal variables were grouped in contingency tables, with numbers (ni) and fractions calculated. The independence of qualitative characteristics was verified using Pearson’s chi-squared test. The strength of correlations was determined by calculating Spearman’s rank correlation coefficients (ρ) and significance levels (P).
The correlation of the independent variables of adherence was tested in multiple linear regression analysis using the forward stepwise method, after testing the applicability of the least squares method and performing analyses of outliers. For independent variables (knowledge and age), standardized coefficients and regression coefficients b were calculated. The statistical significance of variables in the model was verified using Student’s t-test. The quality of the proposed multiple linear regression model was evaluated using standard error of the estimate (SEe). Calculations were performed using the STATISTICA Version 10 software suite.
Results
Patient characteristics
In the group of 233 patients studied, 63% showed a low level of knowledge on hypertension. In the sociodemographic analysis, the only factor for which differences were found was the patients’ living situation. The majority of patients with a low level of knowledge on hypertension were living alone (83.7% vs 15.1%; P=0.045) (Table 1).
Table 1.
Respondents’ sociodemographic characteristics in relation to their knowledge level
| Nominal (qualitative) variables | Hypertension knowledge level
|
P-value | 1 − β | |||
|---|---|---|---|---|---|---|
| Low N=147 |
High N=86 |
|||||
| n | % | n | % | |||
| Sex | 0.638 | 0.071 | ||||
| Female | 76 | 51.7 | 48 | 55.8 | ||
| Male | 71 | 48.3 | 38 | 44.2 | ||
| Education | ||||||
| Primary | 36 | 24.5 | 27 | 31.4 | 0.254 | 0.171 |
| High school | 62 | 42.2 | 37 | 43.0 | 0.905 | 0.037 |
| College/university | 49 | 33.3 | 22 | 25.6 | 0.721 | 0.186 |
| Professional activity | 0.727 | 0.252 | ||||
| Active | 48 | 32.6 | 36 | 41.9 | ||
| Nonactive | 99 | 67.4 | 50 | 58.1 | ||
| Living situation | ||||||
| Living alone | 123 | 83.7 | 13 | 15.1 | <0.001 | 1.000 |
| Living with family/partner | 22 | 14.9 | 72 | 83.7 | <0.001 | 1.000 |
| Residential care institution | 3 | 1.4 | 1 | 1.2 | 0.898 | 0.010 |
| Age | 0.945 | 0.054 | ||||
| M ± SD | 62.9±15.2 | 63.3±14.8 | ||||
| Me (Q1; Q3) | 64 (55; 75) | 63.5 (54; 74) | ||||
| Min–Max | 22–90 | 20–90 | ||||
Abbreviations: Me, mean; SD, standard deviation; M, median; Q1, lower quartile; Q3, upper quartile; P, confidence level; 1 − β, test power; Min, minimum; Max, maximum.
Analysis of the patients’ clinical characteristics showed that the low knowledge level group had a higher rate of ischemic heart disease (31.3% vs 15.1%; P=0.01). A total of 56.5% patients with a low knowledge level and 27.9% patients with high knowledge level group had elevated BP (systolic ≥140 mmHg and/or diastolic ≥90 mmHg). Thirty-five percent of patients with a low knowledge level and fifty-eight percent of patients with high knowledge level had their BP controlled at least daily/weekly. Patients with low knowledge level had less often stated that they owned a BP meter than patients with high knowledge level (58.5% vs 77.1%) (Table 2).
Table 2.
Respondents’ clinical characteristics in relation to knowledge level
| Nominal (qualitative) variables | Hypertension knowledge level
|
P-value | 1 − β | |||
|---|---|---|---|---|---|---|
| Low N=147 |
High N=86 |
|||||
| n | % | n | % | |||
| BP ≥140 mmHg or ≥90 mmHg | 83 | 56.5 | 26 | 27.9 | 0.032 | 0.989 |
| ESC hypertension grade | ||||||
| Normal BP | 16 | 10.9 | 11 | 12.8 | 0.662 | 0.049 |
| Prehypertension | 26 | 17.7 | 16 | 18.6 | 0.863 | 0.036 |
| Grade 1 hypertension | 70 | 47.6 | 35 | 40.7 | 0.308 | 0.141 |
| Grade 2 hypertension | 35 | 23.8 | 24 | 27.9 | 0.488 | 0.083 |
| Comorbidities | ||||||
| Diabetes mellitus | 60 | 40.8 | 31 | 36.1 | 0.561 | 0.083 |
| COPD | 50 | 34.0 | 29 | 33.7 | 0.922 | 0.036 |
| Ischemic heart disease | 46 | 31.3 | 13 | 15.1 | 0.010 | 0.752 |
| Kidney failure | 34 | 23.1 | 26 | 30.2 | 0.298 | 0.184 |
| Medication | ||||||
| ACE inhibitors | 72 | 49.0 | 42 | 48.8 | 0.909 | 0.036 |
| Beta-adrenolytics | 25 | 17.0 | 18 | 20.9 | 0.569 | 0.088 |
| Angiotensin II receptor antagonists | 10 | 6.8 | 5 | 5.8 | 0.984 | 0.029 |
| Thiazide diuretics | 29 | 19.7 | 18 | 20.9 | 0.959 | 0.039 |
| Calcium channel blockers | 49 | 33.3 | 25 | 29.1 | 0.597 | 0.075 |
| Treatment type | ||||||
| Single-agent treatment | 93 | 63.2 | 56 | 65.1 | 0.959 | 0.043 |
| Combination treatment | 54 | 36.7 | 30 | 34.9 | ||
| Other hypertension treatment forms | 54 | 36.7 | 38 | 44.2 | 0.325 | 0.168 |
| Low-sodium/DASH diet | 41 | 27.9 | 26 | 30.2 | 0.817 | 0.049 |
| Weight reduction | 28 | 19.0 | 20 | 23.3 | 0.549 | 0.096 |
| Moderate physical activity | 36 | 24.5 | 23 | 26.7 | 0.821 | 0.048 |
| Keeping a self-control diary | 54 | 36.7 | 52 | 64.2 | 0.048 | 0.979 |
| Blood pressure control daily/weekly | 52 | 35.4 | 48 | 57.8 | 0.044 | 0.894 |
| Own blood pressure meter | 86 | 58.5 | 64 | 77.1 | 0.052 | 0.795 |
| Adherence score (MMAS-8) | ||||||
| Low | 29 | 19.7 | 7 | 8.1 | 0.019 | 0.596 |
| Moderate | 80 | 54.4 | 46 | 53.5 | 0.894 | 0.038 |
| High | 38 | 25.9 | 33 | 38.4 | 0.047 | 0.458 |
| Time from hypertension diagnosis M ± SD | 11.2±8.3 | 12.3±9.2 | 0.349 | 0.070 | ||
| MMAS-8 (score) M ± SD | 6.45±1.45 | 7.08±1.04 | 0.001 | 0.966 | ||
Note: Use of the ©MMAS is protected by US and International copyright laws. Permission for use is required. A license agreement is available from: Donald E Morisky, MMAS Research (MORISKY) 16636 159th Place SE, Renton WA 98058, dmorisky@gmail.com.
Abbreviations: M, median; SD, standard deviation; MMAS-8, 8-item Morisky Medication Adherence Scale; COPD, chronic obstructive pulmonary disease; BP, blood pressure; ESC, European Cardiovascular Society; ACE, angiotensin-converting enzyme; 1 − β, test power.
Characteristics of adherence and knowledge
Most respondents had moderate adherence scores, but in group with low knowledge level, they have lower adherence than in group in high knowledge level MMAS (6.45±1.45 vs 7.08±1.04; P=0.038). However, the low knowledge level group included significantly more low-adherence patients than the group with a high level of knowledge (19.7% vs 8.1%; P=0.023) (Table 2).
The number (proportion) of correct answers to each HK-LS item are shown in Table 3. Patients with a low knowledge level answered correctly significantly less frequently than those with a high knowledge level (P<0.01), the only exception being item 6, with a similar proportion of correct answers in the two groups (P>0.05) (Table 3).
Table 3.
Number (proportions) of correct answers to HK-LS items in the two hypertension knowledge level subgroups
| Item (correct answer) | Hypertension knowledge level
|
P-value | 1 − β | |||
|---|---|---|---|---|---|---|
| Low N=147 |
High N=86 |
|||||
| n | % | n | % | |||
| 1. High diastolic or systolic blood pressure indicates increased blood pressure (yes) | 127 | 86.4 | 84 | 97.7 | 0.004 | 0.788 |
| 2. Increased diastolic blood pressure also indicates increased blood pressure (yes) | 123 | 83.7 | 81 | 94.2 | 0.023 | 0.580 |
| 3. Increased blood pressure is the result of aging, so treatment is unnecessary (no) | 107 | 72.8 | 80 | 93.0 | <0.001 | 0.971 |
| 4. If the medication for increased blood pressure can control blood pressure, there is no need to change lifestyles (no) | 78 | 53.1 | 71 | 82.6 | <0.001 | 0.997 |
| 5. If individuals with increased blood pressure change their lifestyles, there is no need for treatment (no) | 89 | 60.5 | 78 | 90.7 | <0.001 | 0.999 |
| 6. Individuals with increased blood pressure must take their medication in a manner that makes them feel good (no) | 22 | 15.0 | 22 | 25.6 | 0.068 | 0.447 |
| 7. Drugs for increased blood pressure must be taken every day (yes) | 117 | 79.6 | 81 | 94.2 | 0.005 | 0.842 |
| 8. Individuals with increased blood pressure must take their medication only when they feel ill (no) | 105 | 71.4 | 84 | 97.7 | <0.001 | 0.999 |
| 9. Individuals with increased blood pressure must take their medication throughout their life (yes) | 94 | 63.9 | 80 | 93.0 | <0.001 | 0.999 |
| 10. For individuals with increased blood pressure, the best cooking method is frying (no) | 98 | 66.7 | 81 | 94.2 | <0.001 | 0.999 |
| 11. For individuals with increased blood pressure, the best cooking method is boiling or grilling (yes) | 95 | 64.6 | 69 | 80.2 | 0.018 | 0.668 |
| 12. Individuals with increased blood pressure can eat salty foods as long as they take their drugs regularly (no) | 48 | 32.7 | 63 | 73.3 | <0.001 | 1.000 |
| 13. Individuals with increased blood pressure must eat fruits and vegetables frequently (yes) | 70 | 47.6 | 76 | 88.4 | <0.001 | 1.000 |
| 14. The best type of meat for individuals with increased blood pressure is red meat (no) | 26 | 17.7 | 50 | 58.1 | <0.001 | 1.000 |
| 15. The best type of meat for individuals with increased blood pressure is white meat (yes) | 46 | 31.3 | 64 | 74.4 | <0.001 | 1.000 |
| 16. Individuals with increased blood pressure must not smoke (yes) | 74 | 50.3 | 70 | 81.4 | <0.001 | 0.998 |
| 17. Individuals with increased blood pressure can drink alcoholic beverages (no) | 110 | 74.8 | 81 | 94.2 | <0.001 | 0.970 |
| 18. Increased blood pressure can cause strokes, if left untreated (yes) | 125 | 85.0 | 86 | 100.0 | <0.001 | 0.984 |
| 19. Increased blood pressure can cause heart diseases, such as heart attack, if left untreated (yes) | 125 | 85.0 | 85 | 98.8 | <0.001 | 0.940 |
| 20. Increased blood pressure can cause premature death if left untreated (yes) | 126 | 85.7 | 86 | 100.0 | <0.001 | 0.977 |
| 21. Increased blood pressure can cause kidney failure, if left untreated (yes) | 111 | 75.5 | 85 | 98.8 | <0.001 | 0.999 |
| 22. Increased blood pressure can cause visual disturbances, if left untreated (yes) | 108 | 73.5 | 82 | 95.3 | <0.001 | 0.993 |
|
| ||||||
| HK-LS questionnaire domains (M ± SD) |
Low N=147 |
High N=86 |
P-value | 1 − β | ||
|
| ||||||
| Definition | 1.70±0.65 | 1.92±0.28 | 0.012 | 0.948 | ||
| Treatment | 2.30±1.01 | 3.10±0.55 | <0.001 | 1.000 | ||
| Drug adherence | 2.19±1.14 | 3.40±0.69 | <0.001 | 1.000 | ||
| Lifestyle | 3.04±1.15 | 4.48±0.64 | <0.001 | 1.000 | ||
| Diet | 0.49±0.64 | 1.33±0.73 | <0.001 | 1.000 | ||
| Complications | 4.05±1.46 | 4.93±0.26 | <0.001 | 1.000 | ||
| Total score (M ± SD) | 13.8±3.7 | 19.1±1.1 | <0.001 | 1.000 | ||
Abbreviations: HK-LS, Hypertension Knowledge-Level Scale; M, median; SD, standard deviation; P, significance level; 1 − β, test power.
The analysis of questionnaire answers showed that in the low knowledge level group, the largest proportion of wrong answers was provided for items on non-pharmaceutical hypertension treatment, and the lowest scores were obtained in the “diet” domain (0.49±0.64 vs 1.33±0.73; P<0.001), then in the “definition” (1.70±0.65 vs 1.92±0.28; P=0.012) and “drug adherence” (2.19±1.14 vs 3.40±0.69; P<0.001) domains. The highest scores were obtained in the “complications” domain (4.05±1.46 vs 4.93±0.26; P<0.001). The total score in the low knowledge level group was 13.8±3.7 and that in the high knowledge level group was 19.1±1.1 (Figure 2).
Figure 2.
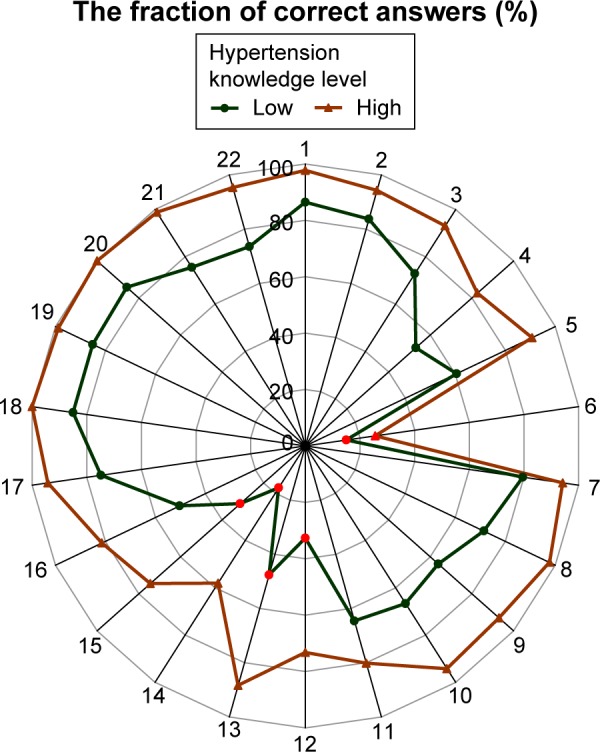
Comparison of correct answer proportions for each HK-LS item in the two groups differentiated by their level of knowledge on hypertension (items with <50% correct answers are marked in red).
Abbreviation: HK-LS, Hypertension Knowledge-Level Scale.
In the group of 233 patients, 71.5% of answers were correct, whereas in the subgroups the percentages were 62.6 (low knowledge level) and 86.5 (high knowledge level). In the low knowledge level group, the lowest proportion of correct answers was given in the “diet” (24.5% vs 66.3% in the high knowledge level group) and “drug adherence” (54.8% vs 84.9%) domains. In the low knowledge level group, the highest proportion of correct answers was given in the “definition” domain (85%), whereas in the high knowledge level group, the highest proportion of items answered correctly belonged to the “complications” domain (98.6%). The significance of differences was P<0.001 (Table 4) (Figure 3).
Table 4.
Proportions of correct answers in HK-LS domains for the two subgroups
| Domain | Total (%) | Group 1 (%) N=147 |
Group 2 (%) N=86 |
1 vs 2 P-value |
1 − β |
|---|---|---|---|---|---|
| Definition | 89.1 | 85.0 | 95.9 | 0.012 | 0.676 |
| Treatment | 65.9 | 57.5 | 77.6 | <0.001 | 0.857 |
| Drug adherence | 65.9 | 54.8 | 84.9 | <0.001 | 0.998 |
| Lifestyle | 70.7 | 60.8 | 87.7 | <0.001 | 0.995 |
| Diet | 39.9 | 24.5 | 66.3 | <0.001 | 1.000 |
| Complications | 87.5 | 81.0 | 98.6 | <0.001 | 0.988 |
| Total | 71.5 | 62.6 | 86.6 | <0.001 |
Abbreviations: HK-LS, Hypertension Knowledge-Level Scale; 1 − β, test power.
Figure 3.
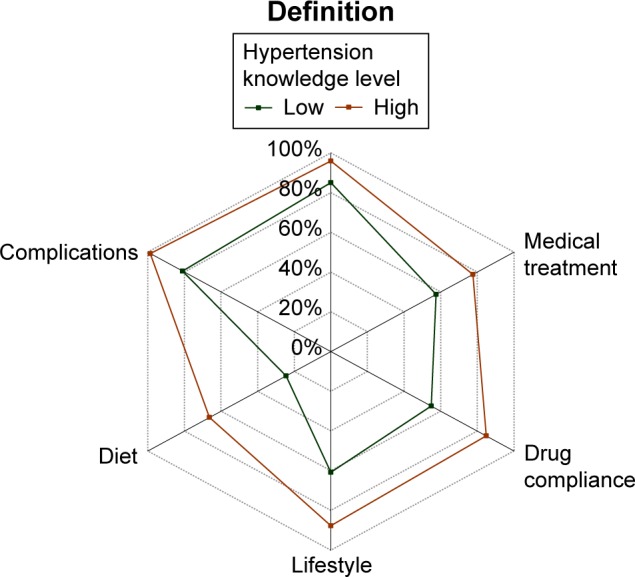
Comparison of correct answer percentages in the 6 HK-LS domains between the two groups differentiated by their level of knowledge on hypertension.
Abbreviation: HK-LS, Hypertension Knowledge-Level Scale.
Single-factor analysis – correlation on adherence of the characteristics studied (MMAS-8 score)
Subsequently, Spearman’s rank analysis was performed to evaluate the correlation of selected variables on adherence (MMAS-8 score). Table 5 shows correlation coefficients from the analysis. Correlation analysis showed that variables having a significant positive effect on adherence included regular BP measurement (ρ=0.171, P=0.009); keeping a self-control diary (ρ=0.017, P=0.007); adherence with non-pharmaceutical hypertension treatment (ρ=0.182; P=0.006); and a high level of knowledge on hypertension (HK-LS) (ρ=0.173; P=0.008) (Table 5).
Table 5.
Single- and multiple-factor regression analysis results for the variables studied against MMAS scores
| Nominal (qualitative) variables | Single-factor analysis
|
Multiple-factor analysis
|
||
|---|---|---|---|---|
| ρ/F (95% CI) | P-value | b | P-value | |
| Age, years | 0.019 (−0.106 to 0.146) | 0.772 | – | – |
| Female sex | 0.028 (−0.028 to 0.155) | 0.671 | – | – |
| Education | 0.107 (−0.016 to 0.232) | 0.104 | – | – |
| Professional activity – active | −0.012 (−0.137 to 0.116) | 0.861 | – | – |
| Living situation – living alone | −0.080 (−0.206 to 0.050) | 0.222 | – | – |
| ESC hypertension grade | 0.082 (−0.041 to 0.208) | 0.212 | – | – |
| Duration of hypertension in years | −0.013 (−0.138 to 0.115) | 0.848 | – | – |
| Regular BP measurements | 0.171 (0.049 to 0.294) | 0.009 | 0.183 (0.051 to 0.296) | 0.004 |
| Diary of self-control | 0.177 (0.055 to 0.300) | 0.007 | 0.115 (−0.008 to 0.240) | 0.089 |
| Concurrent non-pharmaceutical treatment | 0.182 (0.060 to 0.305) | 0.006 | 0.171 (0.049 to 0.294) | 0.006 |
| Ischemic heart disease | −0.184 (−0.065 to 0.3070) | 0.005 | −0.199 (−0.068 to 0.2980) | 0.001 |
| High level of knowledge on hypertension (HK-LS) | 0.173 (0.051 to 0.296) | 0.008 | 0.208 (0.087 to 0.330) | 0.001 |
Note: Use of the © MMAS is protected by US copyright laws. Permission for use is required. A license agreement is available from: Donald E. Morisky, ScD, ScM, MSPH, Professor, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772.
Abbreviations: MMAS, Morisky Medication Adherence Scale; ESC, European Society of Cardiology; BP, blood pressure; HK-LS, Hypertension Knowledge-Level Scale.
Statistically significant independent determinants of good adherence include a high level of knowledge on hypertension (β=0.208; P=0.001), non-pharmaceutical hypertension treatment (β=0.171; P=0.006); and regular BP measurements (β=0.183; P=0.004). The model is significant: F(4.228)=8.99; P<0.001, but only explains 36.9% of the variation in adherence scores.
Spearman’s rank analysis of the correlation of knowledge on specific HK-LS domains on medication adherence showed a statistically significant correlation between knowledge in the “drug adherence” domain and adherence measured by the MMAS questionnaire, especially in the low knowledge level group (ρ=0.303; P<0.001). In the entire study group, a significant correlation between knowledge and adherence was observed. Higher knowledge levels were correlated with better adherence, that is, higher MMAS-8 scores (ρ=0.179; P=0.007) (Table 6).
Table 6.
Spearman’s rank correlation coefficients (ρ) and significance values (P) for correlations between HK-LS domains and MMAS-8 scores
| Subdimension | Total
|
Low knowledge level
|
High knowledge level
|
|---|---|---|---|
| N=233 | N=147 | N=86 | |
| Definition | ρ=0.110 | ρ=0.062 | ρ=0.181 |
| P=0.094 | P=0.451 | P=0.095 | |
| Medical treatment | ρ=0.079 | ρ=0.028 | ρ=0.024 |
| P=0.230 | P=0.732 | P=0.826 | |
| Drug adherence | ρ=0.242 | ρ=0.303 | ρ=0.029 |
| P<0.001 | P<0.001 | P=0.789 | |
| Lifestyle | ρ=0.065 | ρ=−0.022 | ρ=−0.021 |
| P=0.320 | P=0.788 | P=0.845 | |
| Diet | ρ=0.058 | ρ=−0.024 | ρ=0.013 |
| P=0.378 | P=0.771 | P=0.901 | |
| Complications | ρ=0.068 | ρ=0.061 | ρ=−0.140 |
| P=0.301 | P=0.458 | P=0.197 | |
| Total score | ρ=0.179 | ρ=0.151 | ρ=0.028 |
| P=0.007 | P=0.068 | P=0.799 |
Note: Use of the © MMAS is protected by US copyright laws. Permission for use is required. A license agreement is available from: Donald E. Morisky, ScD, ScM, MSPH, Professor, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772.
Abbreviations: HK-LS, Hypertension Knowledge-Level Scale; MMAS-8, 8-item Morisky Medication Adherence Scale.
Discussion
Poorly controlled or untreated hypertension causes gradual irreversible organ damage, leading to life-threatening complications or even death. Hypertension treatment involves continued drug administration, as well as lifestyle modifications and adherence with a complex set of therapeutic recommendations: reduced salt and animal fat intake, weight reduction, and regular exercise. Poor knowledge on adherence to the treatment plan negatively affects patient awareness and behaviors and poses a significant problem in hypertension control. Knowledge and education are considered crucial for proper hypertension control.24 In the present study, as many as 63% of patients showed a low level of knowledge on the definition, treatment, and complications of hypertension. Other published studies confirm the poor knowledge on hypertension among patients25 and a lack of appropriate education promoting the understanding of hypertension.26,27
In the patients with hypertension group of the study, knowledge was poorest with regard to diet and adherence and best with regard to complications. In a study by Eshah and Al-Daken,28 the lowest knowledge levels were found in the “diet” domain, as in the present study, and in the “definition” domain, in contrast to this study. Furthermore, contrary to this study, other authors reported highest knowledge levels in the “lifestyle” and “drug adherence” domains.29 According to other authors, being hypertensive increases the patient’s level of knowledge regarding the illness30,31 and motivation to learn more. In the present study, all patients had been diagnosed with hypertension at least 1 year before, and more than half of them still showed an unsatisfactory level of knowledge on the definition, treatment, and complications of hypertension. In the low knowledge level group, only 62% of questionnaire items were answered correctly, with the lowest correct answer percentage in the “diet” domain – 24.5.
Nearly 20% of patients with a low knowledge level and 8% of patients with a high knowledge level had low adherence scores. The present findings corroborate those by other authors, reporting lack of adherence among patients with hypertension at 25%31 and 28%,5 with better results among patients who were more knowledgeable on the disease.31
In the study by Karaeren et al,31 knowledge on the causes of hypertension and reasons for hypotensive treatment was positively correlated with medication adherence. In the present study, the overall knowledge score and the “drug adherence” domain score were positively correlated with medication adherence. In other studies, knowledge on hypertension complications was not found to be correlated with adherence, which is surprising, as it could be assumed to be the primary motivation for changes in behavior.31 In the present study, knowledge was the highest in the “complications” domain in both groups, and the score in this domain was a predictor of good adherence. In this aspect, the present findings differ from other published reports, where patients were interested in short-term problems related to hypertension (symptoms and adverse effects of treatment) rather than long-term complications.31–33 In the current study, single- and multiple-factor analyses showed significant correlation of knowledge in the “drug adherence” domain on actual medication adherence. The authors state that many patients with hypertension do not understand that hypotensive medication should be taken throughout their life, as opposed to medication during symptom exacerbations31,34 and discontinuation when BP values are normal. In a study by Kjellgren et al35 treatment side effects and disease symptoms were correlated with lack of adherence to treatment. In this study, the impact of adverse effects of treatment was not assessed; however, the “drug adherence” domain was a determinant of high adherence. Items comprised in the “drug adherence” domain are consistent with the correlation between non-pharmaceutical treatment for hypertension (salt restriction and exercise) and self-reported medication adherence, found in this study. Patients complying with non-pharmaceutical treatment recommendations were found to have better adherence to pharmaceutical treatment.
Blood pressure control involves such aspects as regular medication-taking, BP measurements, and keeping a diary of self-control.33 In the present study, regular BP measurements and diary of self-control keeping were confirmed to be predictors of high medication adherence.
Medication adherence is crucial to hypertension control and cardiovascular complication prevention. Concurrent ischemic heart disease is a significant independent negative determinant of medication adherence. In a study by Zhao et al,37 38.4% of patients with ischemic heart disease failed to comply with treatment, and poor knowledge on treatment and complications was correlated with poor medication adherence. The negative correlation between ischemic heart disease and patients with hypertension knowledge could, or should, be explained by the frequent occurrence of ischemic heart disease as a complication of untreated hypertension.36
It should be emphasized that no association between sociodemographic variables and the level of adherence to drug recommendations was discovered in our study. Only regular BP measurement and the concurrent non-pharmaceutical treatment as well as the high level of knowledge were statistically significant factors influencing the level of adherence to recommendations. Both in our study and in the literature the association between the lower level of BP control (or total lack of BP control) with lower level of adherence to recommendations was confirmed.38,39
During hypotensive therapy, the detection of non-adherence in patients with noncontrolled AH is very important before increasing the dosage of the drugs. In such a situation, increasing the dosage of the drugs might intensify the side effects of the medication and increase the level of non-adherence to recommendation. Only effective communication and education can influence the regular BP control and the adherence to therapeutic recommendations.
Conclusion
Patients with hypertension knowledge on their illness are insufficient, with the lowest levels of knowledge on diet and drug adherence.
Patients with a high level of knowledge also show better medication adherence.
Knowledge on hypertension is a significant independent determinant of good adherence. Other independent determinants include salt restriction and regular BP measurements.
Concurrent ischemic heart disease is a significant negative determinant.
Implication for practice
The identification of knowledge deficits as a factor contributing to lack of adherence and poor hypertension control remains a key challenge for clinicians caring for patients with hypertension.
A multidisciplinary approach and the development of intervention programs focused on promoting patient knowledge and healthy behaviors are significant components of care, contributing to better adherence and control.
Study limitations
The most important limitation is the fact that this study sample was recruited from a single center. Then, the method used for assessing adherence was a self-assessment questionnaire; however, the MMAS had been used in multiple studies on medication adherence in hypertension, showing good psychometric properties. Finally, no information on patients’ sources of knowledge was gathered.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization, International Society of Hypertension, Writing Group World Health Organization (WHO) International Society of Hypertension, (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Marcum ZA, Zheng Y, Perera S, et al. Prevalence and correlates of self-reported medication non-adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension. Res Social Adm Pharm. 2013;9:817–827. doi: 10.1016/j.sapharm.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jokisalo E, Kumpusalo E, Enlund H, Takala J. Patients’ perceived problems with hypertension and attitudes towards medical treatment. J Hum Hypertens. 2001;15:755–761. doi: 10.1038/sj.jhh.1001276. [DOI] [PubMed] [Google Scholar]
- 4.Szczęch R, Szyndler A, Wizner B, Narkiewicz K. Education of patients with hypertension [w:] In: Januszewicz A, Januszewicz W, Szczepańska-Sadowska E, Sznajderman M, editors. Arterial Hypertension. Kraków: Medycyna Praktyczna; 2007. pp. 1225–1230. [Google Scholar]
- 5.Altun B, Arici M, Nergizoğlu G, et al. Prevalence, awareness, treatment and control of hypertension in Turkey (The Patent Study) in 2003. J Hypertens. 2005;23:1817–1823. doi: 10.1097/01.hjh.0000176789.89505.59. [DOI] [PubMed] [Google Scholar]
- 6.Sanne S, Muntner P, Kawasaki L, Hyre A, DeSalvo KB. Hypertension knowledge among patients from an urban clinic. Ethn Dis. 2008;18:42–47. [PubMed] [Google Scholar]
- 7.Oliveria SA, Chen RS, McCarthy BD, Davis CC, Hill MN. Hypertension knowledge, awareness and attitudes in a hypertensive population. J Gen Intern Med. 2005;5:20219–20225. doi: 10.1111/j.1525-1497.2005.30353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 9.Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Beyond salt: lifestyle modifications and blood pressure. Eur Heart J. 2011;32:3081–3087. doi: 10.1093/eurheartj/ehr379. [DOI] [PubMed] [Google Scholar]
- 10.2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 11.Tykarski A, Posadzy-Małaczyńska A, Wyrzykowski B, et al. [Prevalence of hypertension and effectiveness of its treatment in adult residents of our country. Results of the WOBASZ program] Rozpowszechnienie nadciśnienia tętniczego oraz skuteczność jego leczenia u dorosłych mieszkańców naszego kraju. Wyniki programu WOBASZ. Kardiol Pol. 2005;63(6 Suppl 4):S614–S619. Polish. [PubMed] [Google Scholar]
- 12.Mancia G, Grassi G. Impact of new clinical trials on recent guidelines on hypertension management. Ann Med. 2011;43:124–132. doi: 10.3109/07853890.2010.543922. [DOI] [PubMed] [Google Scholar]
- 13.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169:1748–1755. doi: 10.1001/archinternmed.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;17:CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 15.Machado M, Bajcar J, Guzzo GC, Einarson TR. Sensitivity of patient outcomes to pharmacist interventions. Part II: systematic review and meta-analysis in hypertension management. Ann Pharmacother. 2007;41:1770–1781. doi: 10.1345/aph.1K311. [DOI] [PubMed] [Google Scholar]
- 16.Suligowska K, Gajewska M, Stokwiszewski J, et al. Insufficient knowledge of adults in Poland on criteria of arterial hypertension and its complications. Results of the NATPOL 2011 Survey. Arterial Hypertens. 2014;18(1):9–18. [Google Scholar]
- 17.Sanne S, Muntner P, Kawasaki L, Hyre A, DeSalvo KB. Hypertension knowledge among patients from an urban clinic. Ethn Dis. 2008;18(1):42–47. [PubMed] [Google Scholar]
- 18.Wizner B, Gryglewska B, Gasowski J, Kocemba J, Grodzicki T. Normal blood pressure values as perceived by normotensive and hypertensive subjects. J Hum Hypertens. 2003;17(2):87–91. doi: 10.1038/sj.jhh.1001516. [DOI] [PubMed] [Google Scholar]
- 19.Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. J Am Med Assoc. 1993;269:2386–2391. [PubMed] [Google Scholar]
- 20.Krousel-Wood MA, Islam T, Webber LS, Re RS, Morisky DE, Muntner P. New Medication Adherence Scale Versus Pharmacy Fill Rates in Seniors with Hypertension. Am J Manag Care. 2009;15(1):59–66. [PMC free article] [PubMed] [Google Scholar]
- 21.Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: Final response. J Clin Epidem. 2011;64:258–263. doi: 10.1016/j.jclinepi.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Erkoc SB, Isikli B, Metintas S, Kalyoncu C. Hypertension Knowledge-Level Scale (HK-LS): study on development, validity and reliability. Int J Environ Res Public Health. 2012;9:1018–1029. doi: 10.3390/ijerph9031018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han HR, Chan K, Song H, Nguyen T, Lee JE, Kim MT. Development and evaluation of a hypertension knowledge test for Korean hypertensive patients. J Clin Hypertens (Greenwich) 2011;13:750–757. doi: 10.1111/j.1751-7176.2011.00497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dzudie A, Kengne AP, Muna WF, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open. 2012;2(4) doi: 10.1136/bmjopen-2012-001217. pii:e001217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee HS, Park YM, Kwon HS, et al. Prevalence, awareness, treatment, and control of hypertension among people over 40 years old in a rural area of South Korea: the Chungju Metabolic Disease Cohort (CMC) study. Clin Exp Hypertens. 2010;32:166–178. doi: 10.3109/10641960903254497. [DOI] [PubMed] [Google Scholar]
- 27.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056–1065. doi: 10.1111/j.1532-5415.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- 28.Eshah NF, Al-Daken LI. Assessing publics’ knowledge about hypertension in a community-dwelling sample. J Cardiovasc Nurs. 2012;31:158–165. doi: 10.1097/JCN.0000000000000227. [DOI] [PubMed] [Google Scholar]
- 29.Zernike W, Henderson A. Evaluating the effectiveness of two teaching strategies for patients diagnosed with hypertension. J Clin Nurs. 1998;7:37–44. doi: 10.1046/j.1365-2702.1998.00128.x. [DOI] [PubMed] [Google Scholar]
- 30.Zafar SN, Gowani SA, Irani FA, Ishaq M. Awareness of the risk factors, presenting features and complications of hypertension amongst hypertensives and normotensives. J Pak Med Assoc. 2008;58:711–715. [PubMed] [Google Scholar]
- 31.Karaeren H, Yokuşoğlu M, Uzun S, et al. The effect of the content of the knowledge on adherence to medication in hypertensive patients. A Svenssonnadolu Kardiyol Derg. 2009;9:183–188. [PubMed] [Google Scholar]
- 32.Malik A, Yoshida Y, Erkin T, Salim D, Hamajima N. Hypertension related knowledge, practice and drug adherence among inpatients of hospital Insamarkand, Uzbekistan. Nagoya J Med Sci. 2014;76(3–4):255–263. [PMC free article] [PubMed] [Google Scholar]
- 33.Ghembaza MA, Senoussaoui Y, Tani MK, Meguenni K. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev. 2014;10:41–48. doi: 10.2174/157340211001141111160653. [DOI] [PubMed] [Google Scholar]
- 34.Neutel JM. Choosing among renin-angiotensin system blockers for the management of hypertension: from pharmacology to clinical efficacy. Curr Med Res Opin. 2010;26:213–222. doi: 10.1185/03007990903444434. [DOI] [PubMed] [Google Scholar]
- 35.Kjellgren KI, Svensson S, Ahlner J, Säljö R. Hypertensive patients’ knowledge of high blood pressure. Scand J Prim Health Care. 1997;15:188–192. doi: 10.3109/02813439709035026. [DOI] [PubMed] [Google Scholar]
- 36.Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299. [DOI] [PubMed] [Google Scholar]
- 37.Zhao S, Zhao H, Wang L, Du S, Qin Y. Education is critical for medication adherence in patients with coronary heart disease. Acta Cardiol. 2015;70:197–204. doi: 10.1080/ac.70.2.3073511. [DOI] [PubMed] [Google Scholar]
- 38.Morgado M, Rolo S, Macedo AF, Pereira L, Castelo-Branco M. Predictors of uncontrolled hypertension and antihypertensive medication nonadherence. J Cardiovasc Dis Res. 2010;1(4):196–202. doi: 10.4103/0975-3583.74263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al Ghobain M, Alhashemi H, Aljama A, et al. Nonadherence to antihypertensive medications and associated factors in general medicine clinics. Patient Prefer Adherence. 2016;10:1415–1419. doi: 10.2147/PPA.S100735. [DOI] [PMC free article] [PubMed] [Google Scholar]


