Abstract
Presently, there is a high paucity of bone grafts in the United States and worldwide. Regenerating bone is of prime concern due to the current demand of bone grafts and the increasing number of diseases causing bone loss. Autogenous bone is the present gold standard of bone regeneration. However, disadvantages like donor site morbidity and its decreased availability limit its use. Even allografts and synthetic grafting materials have their own limitations. As certain specific stem cells can be directed to differentiate into an osteoblastic lineage in the presence of growth factors (GFs), it makes stem cells the ideal agents for bone regeneration. Furthermore, platelet-rich plasma (PRP), which can be easily isolated from whole blood, is often used for bone regeneration, wound healing and bone defect repair. When stem cells are combined with PRP in the presence of GFs, they are able to promote osteogenesis. This review provides in-depth knowledge regarding the use of stem cells and PRP in vitro, in vivo and their application in clinical studies in the future.
Introduction
Regenerating the lost bone is of primary concern in diseases and conditions involving bone loss, such as periodontitis, tumors, fractures, and bony defects.1 Autogenous bone has long been held as the gold standard of bone grafting materials; however, donor site morbidity, difficulty in obtaining it, and the prolonged healing time are its limitations.2 In recent years, autologous bone has been administered for the regeneration of bony defects and structures.3 But, the risk of disease transmission and foreign body immune reaction associated with it is high.4 In addition, synthetic bone grafting materials have been created and produced to mimic bony structure and cellular morphology along with promoting osteoconduction;5 however, the primary expenses involved in fabricating and manufacturing these graft materials preclude their extensive application.6 Hence, it is imperative to advocate and implement newer techniques and entities in order to overcome these limitations.7 Bone tissue engineering is the field of medicine that involves the regeneration and replacement of the lost bony tissue and structure.4 Due to the increasing demand and the paucity of the presently existing bone grafts, it has now become imperative to devise novel materials that can achieve excellent regeneration as well as reduce the drawbacks of the presently existing grafting materials.8 It is very important to harness the potential of cellular and molecular technology in order to develop newer grafting materials and exploit its practical applications.9–11
A high volume of research in bone tissue engineering has been devoted to adult stem cells, which can be isolated from tissues such as a bone marrow or adipose tissue. Mesenchymal stem cells (MSCs) have been identified as the cells which adhere to plastic, lack of expression and absence of the hematopoietic and endothelial markers and their ability to differentiate into adipogenic, chondrogenic, and osteogenic lineages.12–14 Adult bone marrow-derived MSCs (BMSCs) have been the focus of most studies due to the inherent potential of these cells to differentiate into various cell types. In the past decade, MSCs have been employed in the regeneration of bone, especially because of its potential to differentiate into an osteogenic lineage, which is of prime importance in the process of bone growth.15–18 It is also known to influence the fate of other cells through the process of paracrine signaling thus providing an osteoinductive and osteoconductive environment for the differentiation of other surrounding cells in the associated region.19 Furthermore, it also governs the immune modulatory potential of the neighboring cells through the secretion of prostaglandins.20 For MSCs to develop into an osteogenic lineage, it is crucial to have the presence of a catalyst that can accelerate its differentiation and proliferative potential without affecting its cellular structure and biology.21 It is also important for the catalyst to be inexpensive, biocompatible, and osteoconductive in property.22,23
PRP (platelet-rich plasma) was first defined in 2007 as a preparation of platelets present in a small volume of plasma containing a large amount of growth factors (GFs), which is essential for bone growth and regeneration.24 There are more than 15 GFs present in the PRP with the primary ones consisting of platelet-derived growth factor (PDGF), Insulin-like growth factor (IGF) and Transforming growth factor-β (TGF-β) along with their isoforms.25 These GFs have their origin in the alpha granules of the platelets (50–80 per platelet).26 However, recent studies have observed not only the presence of GFs, but also the cytokines, enzymes, proteins, and fibrinolytic and anti-fibrinolytic proteins which are release upon the activation of the platelets through a mechanical or chemical pathway.27 The factors required for activation may include collagen, thromboxane, calcium, magnesium, serotonin, and other platelet aggregating factors.28 Activation leads to an immediate burst of these GFs, thereby leading to the exhaustion of all the factors within 24 h.29 The benefits involved in the application of PRP in the regeneration of bone involve its availability, ease of isolation, good handling and storage properties and its application in the field of bone tissue engineering.30 In addition, it is autologous which eliminates the risk of disease transmission and immune rejection.31
GFs like PDGF, TGF, and IGF are associated with bone regeneration and growth since they consists of proteins which are known to be present in the cells during wound healing and are hence known to mimic bone healing conditions.30 These factors are present in abundant in the platelets and can be applied with MSCs for the regeneration of bone.32 In the presence of these factors, the MSCs have a greater predilection toward developing into an osteogenic lineage.33 It may have greater applications in the regeneration of critical-sized bony defects due to its excessive osteoconductive and osteoinductive potential.
This paper briefly covers various types of stem cell sources that have been described in the scientific literatures for use in tissue engineering applications. The majority of these studies have focused on PRP and stem cells due to their high osteogenic potential and the prospect of PRP for bone tissue engineering.
Stem cells in bone regeneration
BMSCs are the most extensively studied stem cells for bone regeneration owing to their capacity to differentiate into an osteoblastic lineage in the presence of appropriate GFs as well as regenerate bone efficiently in vivo.34 Upon isolation from the bone marrow, these stem cells are characterized. These cells are generally easy to isolate and passage.35 However, the low yield of BMSCs potentiates the need for extensive in vitro expansion, which reduces the posttranslational survival and immunomodulatory properties of BMSCs.36 In addition, the age and health status of the donor is of critical importance with regard to obtaining these cells. In the mid-1960’s, Friedenstein et al.37,38 reviewed a series of experiments and hypothesized that BMSCs could be co-isolated in vitro alongside hematopoietic cells. BMSCs are generally referred to as MSCs, however, it should be noted that bone marrow usually consists of stromal cells which do not necessarily give rise to MSCs.39 Nevertheless, upon isolation, the purified BMSCs are referred to as MSCs as they are governed by the 2006 criteria and exhibit both plasticity and the ability to differentiate into chondrocytes, osteocytes, and adipocytes in vitro and in vivo.40 In 1997, Komori et al.41 proposed that marrow stromal cells express the master osteogenic transcription factor, runt-related transcription factor 2 (Runx2) and furthermore, regardless of differentiation, the BMSCs retain Runx2 expression, suggesting an ability to shift phenotype and redifferentiate into osteoblasts.
Current research in MSCs not only aims at generating novel cell therapies but also enables in the development of cell models that facilitate the learning and study of the experiments for the basis of regeneration of tissues and the mechanisms involved.42 MSCs are generally obtained from the bone marrow and can be studied in vitro, which enables the convenient study of these tissue specific cells.43 MSCs are being used in in vivo studies because they are governed by the molecules in their environment where their anabolic capacity is modulated.44 There are various GFs present in the PRP which bring about the signaling of various processes leading to MSC proliferation, migration, and differentiation, and the development of an environment where healing of the tissues can occur.45 However, the use of MSCs is limited in a clinical setting due to the need for GFs for MSC growth and expansion, MSC low yield and the inherent heterogeneity they display in their multi-differentiation potential.46 This heterogeneity has been reported to occur within the same single-cell-derived colony, and no matter how pure the pure colony is, it will still result in a heterogeneous population upon passaging. In fact, these challenges and benefits from addressing emergent population heterogeneity are not limited to MSCs, and they can be considered for other tissue-derived stem cells and induced pluripotent cell populations and can be overcome by sorting by label-free biophysical markers or by biophysical or other characteristics.47 Because of the extremely low yields of BMSC progenitors (typically 0.001%–0.01%) obtained from bone marrow aspirates, large quantities of bone marrow must be procured, which can cause additional donor site morbidity.48 In addition, several passages are required in order to separate the hematopoietic population and other cell types from the pure BMSCs. Furthermore, passaging of the cells can result in the decreased potential of differentiation and this may potentiate the need for additional GFs in order to increase the differentiation and growth potential.49 These significant limitations have hindered the translation of BMSC into a clinical setting, leading investigators to seek alternative tissue sources from which to isolate MSCs. However, clinical studies have demonstrated that even with the pure preparations of these cells, only few of these cells can differentiate into an osteoblastic lineage.50 Even with seemingly pure preparations of BMSC, only 1% of BMSC in the population are susceptible to osteogenesis.51 It is also obvious that unfractionated BMSCs expanded in culture exhibit variable functional efficacy.52 Zuk et al.53,54 first discovered adipose stem cells (ASCs) in 2001 and ever since then, these cells have been used in the field of tissue engineering, especially in bone regeneration. It acts an excellent substitute to MSCs in bone formation, owing to its abundant supply, ease of isolation and because it is readily and safely accessible. Although, ASCs have been explored for their potential of bone formation, they have been able to yield very low amounts of bone in several studies. This could be attributed to the fact that they contain some populations of stromal and endothelial cells that could interfere with their whole potential towards osteogenesis.53 However, MSCs can be purified from ASC and be identified by checking for the expression of the cell markers CD73, CD90, CD44, and CD9. Moreover, ASCs have been shown to possess tri-lineage potential and to undergo osteogenic differentiation by itself as well as when treated with ascorbic acid, bone morphogenetic protein-2, and β-glycerophosphate.55,56
In, in vivo studies, ASC have been reported to repair critical-sized calvarial defects, to promote bone formation in appendicular defects,57 and to induce spinal fusion in murine models and they were able to promote bone formation for craniomaxillofacial repair in a large animal canine model.58 And although, large quantities of ASCs are implanted in vivo, these cells have to be passaged several times in order to decrease its contamination with other cell types. However, this could also reduce the osteogenic potential of the cell, decrease its viability and self-renewal as well as lower its multi-potency. ASCs are known to contain and release factors such as angiopoietin-like 1, Epidermal growth factor (EGF), Fibroblast growth factor (FGF), Hepatocyte growth factor (HGF), TGF-β, and CXC chemokine ligand 12(CXCL12), as well as the immunosuppressive cytokines prostaglandin E2 (PGE2) and indole amine 2,3-dioxygenase (IDO). However, while these factors may increase the growth and differential potential, their presence could also play a role in successfully regenerating bone without triggering a lymphocyte reaction.59 Overall, these cells possess tremendous potential for osteogenesis in the field of bone engineering. In 2003, Shi and Gronthos successfully isolated dental pulp stem cells from third molars with the use of the antibody STRO-1. These cells were characterized as cells with a high level of clonogenicity and proliferation and the ability to generate large calcified colonies and occasional nodules.60 MSC purified from the pulp of deciduous teeth is termed as DMSC (dental mesenchymal stem cell). The tooth is abundant in MSCs population and depending on the area source is termed as dental pulp stem cells (DPSCs), periodontal ligament stem cells (PDLSCs), apical papilla stem cells (SCAPs), dental follicle stem cells (DFSCs), and gingival tissue stem cells (GMSCs).61 The greatest advantage that lies with the use of DMSCs is its ease of isolation, and that despite the small size of the tooth, they are an abundant source of these cells.62 Also, extraction being a routine dental procedure, the isolation of these cells does not result into inconvenience to the patient.60
In vivo studies in literature have reported promising results of the use of DMSCs in bone regeneration. The use of DMSCs has been demonstrated to repair critical-size calvarial defects in mice by promoting the formation of new bone.63 In canine and swine models, the local implantation of DMSCs with β-TCP and HA/TCP scaffolds has been shown to induce successful bone regeneration in critical-sized orofacial bone defects.64 Ravindran et al. reported the occurrence of robust odontogenic differentiation and proliferation of tissue with the use of DPSCs, PDLSCs, and BMSCs to collagen/chitosan scaffolds without the use of external agents. Zhang et al. seeded 2×106 DPSCs/per silk fiber/collagen/hexafluoro-2-propanol (HFIP) scaffold and observed that they formed soft dental pulp.65 However, the disadvantages associated with these cells is their heterogeneity which can affect its osteogenic potential. Moreover, several investigators have also reported the limited potential of DMSCs to regenerate bone in vivo due to its inability to promote de novo bone formation in the form of cortical bone and not vascularized bone as noted in a human mandibular defect.66
Platelet-rich plasma
PRP was discovered in 1914 by Dimond et al.,67 when it was prepared for intravenous transfusions. Around four decades ago, platelets were primarily known to be associated with the hematopoietic system, until recently, in 1974, when Ross et al.,68 while working on smooth muscle cell culture found that the addition of platelets and calcium or the extract from the platelets derived upon activation, to the serum, increased the mitogenic activity and proliferation of the cells. This led to a breakthrough in platelet research and opened new realms in this field that no longer limited the use of platelets to hemostatic cells. In 1978, PDGF was discovered by Witte et al.69 and in 1979, Kaplan et al.70 reported that PDGF resided within the alpha granules of the platelet cells. Following that, several other GFs like TGF-β was discovered by Assoian et al.71 in 1983 as well as IGF-1,by Karey et al.72 in 1989 and vascular endothelial growth factor (VEGF) by Banks et al.73 in 1998. Autologous PRP was first used in a heart surgery in 1987 by Ferrari et al., and did not report of any complications with its use.74 Autologous fibrin gel was first introduced by Gibble and Ness in 1990,75 at that time, this fibrin gel lacked the presence of platelets, and the addition of platelets to this fibrin gel arrived later. With the subsequent introduction of this PRP, the advent of its administration began in the world of bone-related surgeries especially due to the fact that the GFs, which were available but expensive and had a short span with inefficient local delivery to target cells.76–78 Recently, studies involving the use of PRP has gained momentum considering the cost effectiveness, availability of large quantities at a time, prolonged storage and the decreased rate of rejection as it is autogenous.79 PRP contains various GFs.80 There is currently an estimated of 600 GFs present in the PRP.81 These GFs are primarily responsible for inducing differentiation, enhancing healing and promote tissue regeneration.82 This molecular pool is released upon platelet activation that is the interaction of molecules such as collagen, thrombin, platelet-activating factor, serotonin, calcium, magnesium, thromboxane A2, and adenosine di-phosphate with platelet receptors.83 Also, mechanical disruption of platelets causes their activation and the subsequent release of the cellular contents. When platelets are activated, there is an initial burst of GFs that is lately stabilized and maintained in a sustained release.84
Recently, research in the use of PRP has been gaining momentum in the field of Bone regeneration and is being employed extensively in orthopedic surgery.79 PRP contains various important GFs that enable the growth of bone and even though the mechanism of the bone regeneration is not well understood presently, its ease of handling and application makes it a good agent in the orthopedic field.85 In addition, it reduces inflammation, provides excellent tissue healing and being autologous reduces the risk of disease transmission and immunogenic reactions.81
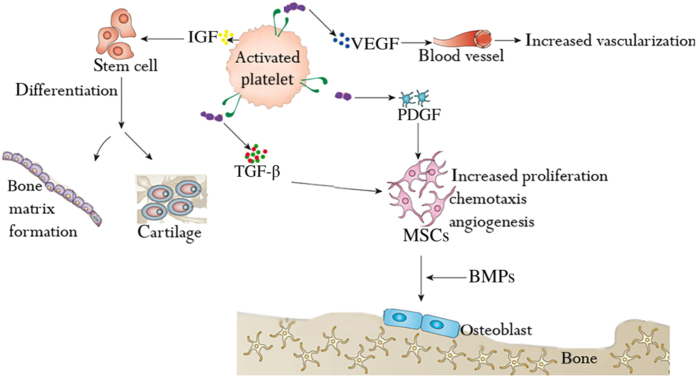
When integrated with biological or synthetic bone grafts, PRP has been reported to improve the aggregation and cohesiveness of particulate-based bone substitutes, thus helping bone formation or bone regeneration process, particularly due to the fact that most of the events involved in the formation of bone are triggered by the factors that are present in PRP.86 However, the doubt governing whether PRP is clinically effective or not is exacerbated by the inadequate knowledge concerning the bioavailability of PRP-derived GFs.87 The polypeptide GFs PDGF, TGF-β, IGF-1, VEGF, HGF, EGF, and FGF have each been identified within platelet alpha granules. Many of these factors share some common structural features and signaling mechanisms, which have been summarized in Table 1 and their actions on stem cells in Figure 1.
Table 1. GFs released from PRP.
| Growth factor | Source | Target | Function | Reference |
|---|---|---|---|---|
| Platelet-derived growth factor | Platelet, macrophages, monocytes, smooth muscle, degranulating platelets, endothelial cells, macrophages, osteoblasts, osteoclasts, mesenchymal stem cells. | Smooth muscle, fibroblasts, glial cell | Cell proliferation, neutrophil chemotaxis, inducing cells to migrate toward the wound, collagen production, blood vessel repair and regeneration, connective tissue healing, Increases mitogenesis in smooth muscle cells/glial cells/fibroblasts,angiogenesis and macrophage activation, Differentiation of fibroblasts, collagenase secretion | 88 |
| Transforming growth factor-beta | Platelet, T-lymphocyte, macrophage, neutrophil, osteoblasts, macrophages, platelets, bone matrix | Fibroblast, stem cell, endothelial cell, epithelial cell, pre-osteoblast, | Stimulation/inhibition of endothelial, osteoblastic and fibroblastic chemotaxis and angiogenesis, collagenase secretion, mitogenesis of other GFs, increase fibroblast and osteoblast mitosis, promotion of wound healing, bone matrix formation, growth and neurogenesis of epithelial cells, Regulation of the balance between fibrosis and myocyte regeneration, stimulation of proliferation of undifferentiated mesenchymal stem cells, inhibition of replication of most cells in vitro, inhibition of MMP production. | 89 |
| Insulin-like growth factor | Osteoblasts, monocytes, chondrocyte, Macrophage, Plasma stored in bone, epithelial cells, endothelial cells, smooth muscle cells,liver | Osteoblasts, fibroblast,chondrocyte | Bone matrix formation, increase cartilage growth, wound healing, proliferation of osteoprogenitor cells, mitogenic for osteoblasts, fibroblasts and endothelial cells, | 90 |
| Vascular endothelial growth factor | Platelet | Endothelial cells | Angiogenesis and increased capillary permeability, expression increased in presence of hypoxia, | 91 |
| Epidermal growth factor | Submaxillary gland, brunner’s gland. Macrophage and platelets. | Epidermal cells, | Epithelial cell proliferation, angiogenesis and promotion of wound healing, induction of basal membrane formation, keratinocyte migration and granulation tissue formation. | 92 |
| Fibroblast growth factor | Mast cells,Macrophage, osteoblasts and immature chondrocytes. | Fibroblasts, endothelial cells | Cell growth, tissue repair, collagen production, hyaluronic acid production | 93 |
| Keratinocyte growth factor | Platelets | keratinocytes | Proliferation, differentiation and regeneration of keratinocytes | 94 |
| Connective tissue growth factor | Platelets | vascular endothelial cells, epithelial cells, neuronal cells, vascular smooth muscle cells, and cells of supportive skeletal tissues | Increased wound healing, angiogenesis, chondrogenesis, osteogenesis, tissue repair fibrosis. | 95 |
| Interleukin-8 | Macrophages, epithelial cells, endothelial cells, smooth muscle cells,keratinocytes | Neutrophil, endothelial cells,macrophages, mast cells, and keratinocytes | Induction of chemotaxis in target cells and stimulate their migration toward site of infection, pro-inflammatory, recruiting fibroblasts and endothelial cells | 96 |
| Platelet derived angiogenesis growth factor | Platelet, endothelial cells | Endothelial cells | Angiogenesis, increased capillary permeability, stimulation of endothelial cells mitogenesis | 97 |
| Platelet factor-4 | Platelet | Neutrophil, fibroblasts | Chemotaxis of neutrophils and fibroblasts, potent anti-heparin agent | 98 |
Abbrevations: GF, growth factor; PRP, platelet-rich plasma.
Figure 1.
Role of PRP on stem cells in bone and cartilage formation.
GFs in PRP
Platelet-derived growth factor
PDGF was one of the earliest and first GFs to be discovered and its role and function is known to be primarily associated with all forms of wound healing by increasing the number of MSCs in the environment, by acting as a chemoattractant and recruiter of osteoprogenitor cells and by increasing the proliferation of cells at high level.99 PDGF has isoforms and exists as PDGFAA, PDGFBB, PDGFAB and PDGFCC. But the specific actions of each isoforms has yet to be determined.100 It works by binding to the transmembrane receptors.101 It is responsible for the mitogenesis of MSCs, endothelial mitoses into functioning capillaries, and macrophage activation for bone regeneration and wound healing.99 PDGFBB at amounts of 10-100 ng·mL−1 increased [3H] thymidine incorporation into the DNA and increased collagen and non-collagen synthesis in rat calvarias.102,103 PDGF can also increase bone collagen degradation, which is possibly related to its ability to increase collagenase production. PDGF is also known to stimulate production of several matrix molecules like fibronectin, collagen and hyaluronic acid.104 It is also known to stimulate the contraction of collagen matrices in vitro.105 It acts at the site of wound healing since it is released from macrophages, endothelial cells smooth muscle cells and fibroblasts cells. In some studies, it has been documented that the application of PDGF to the site of healing increased the glycosaminogycans, neovascularization and amount of granulation tissue, which implicates its role in the increase in the rate of wound healing and bone formation.105
Transforming growth factor-β
TGF-β is the second most prominent GF in PRP and is responsible for the cell differentiation and proliferation.106 TGF-β is secreted in a latent form that is activated outside of the cell.107 It acts by binding to heteromeric serine/threonine kinase receptors on the cell surface that transmit a signal to nucleus via Smad proteins to ultimately regulate changes in gene expression.107 At normal serum levels, TGF-β can promote mitogenesis and osteogenic differentiation of osteoprogenitor cells. However at altered levels, it can cause pathological conditions in bone.108 Ideally, in the platelets, TGF-β is secreted in a dormant form.109 It is then later activated via certain proteolytic or non-proteolytic pathways. It can regulate changes in the gene expression via Smad pathway, as well as inhibit mitogenesis and cell growth through the MAP kinase and cyclin dependent pathways. TGF-β can also regulate proliferation, differentiation, alteration in cell morphology, chemotaxis and adhesion of the osteogenic progenitor cells at the site of wound healing, which makes it an excellent agent in the promotion of fracture healing.110
IGF
IGF-1 is produced by osteoblasts that are generally controlled by the growth hormone and other factors. Their activity is regulated at several levels.111,112 They can enhance collagen synthesis as well as osteoblast differentiation and proliferation.113 The differentiation is dose and time dependent and functions through various signal transduction systems.114 With aging, there is an impaired osteoblastic function with reduced bone formation. IGF-1 has an essential role in the development of the growing skeleton and in the maintenance of bone mass during late adulthood and aging.115 Its mitogenic action selectively promotes cell multiplication in young differentiated clones.116 It can also stimulate tissue growth and has an important role in bone mass maintenance and acquisition.116 When administered with growth hormone, they have synergistic effect on bone modeling and regeneration.114
PRP isolation, activation, and delivery
PRP is obtained by centrifuging peripheral blood in order to obtain plasma, platelets and red blood cells. The plasma is abundant in cytokines, thrombin, and other GFs, with inherent biological and adhesive properties. PRP was first prepared in the 1970s.117 Several papers have later modified the protocols for PRP extraction by creating changes in the time, speed and distance, with reference to centrifugation physics and mechanics with gravity in the preparation and quantity of PRP.118–121 The process of isolation of PRP involves the use of anti-coagulation. Do Amaral et al.122 found that there was no difference between the use of EDTA, ACD (acid citrate dextrose) and sodium citrate as an anticoagulant; however, EDTA yielded higher platelet quantity, PRP obtained by citrate solution resulted in higher induction of MSC proliferation and smallest variation in MSC gene expression and ACD caused an increase in platelet recovery. There are two widely used protocols in the preparation of PRP: one step and two step PRP preparation. The effect of separation by these two methods is still controversial. The increase in commercial applications led to the development of PRP kits.123–125 However, GFs content has been established to be the same using the presently available methods of isolation. GFs can be released from the PRP upon activation via endogenous or exogenous pathway. Endogenous activation involves using freeze thaw cycles. However, the freeze thaw cycles would affect the release of the GFs due to destruction of the platelets. Another common method of activation is the use of calcium chloride and thrombin.126 GF release has shown no differences when activated with either calcium chloride or thrombin. Calcium chloride is preferred over thrombin due to thrombin’s ability to act as an anticoagulant and thereby precipitate undesired reactions.127 Furthermore, there have controversies over the use of leukocyte rich PRP and pure PRP. Yin et al.128 reported that Leukocytes in L-PRP may activate the NF-κB pathway via the increased pro-inflammatory cytokines to induce the inferior effects on bone regeneration of L-PRP compared with P-PRP, thus implying that pure PRP may be a safer option for use.
Upon activation, PRP can release several GFs that are essential for healing and bone regeneration.117 These GFs have a short life span of 24 h and hence, potentiate a need for delivering PRP via different biological materials that have lower degradation rates in order to prolong its effect on bone regeneration and healing. Several studies have defined the use of platelet gels (gel formed upon activation of PRP using calcium chloride and thrombin), certain salts like calcium phosphate, calcium sulfate, nano calcium sulfate, hydrogels-like gelatin, and alginate, nanofiber scaffolds and bioactive glass.118,129–131 The studies have been summarized in Table 2.
Table 2. Delivery of PRP for bone formation.
| Type of material | Animal model | Results | References |
|---|---|---|---|
| Activated PRP | Goat trabecular bone implants | Increased bone-to-implant surface contact. | 132–134 |
| Activated PRP with BMMSCs, porous hydroxyapatite (HA), | Canine trabeculae implants | Increased bone healing | 135 |
| Activated PRP with HA/collagen type I bead matrix within a polytetrafluoroethylene (PTFE) | Rabbit iliac crests | Increased mineralization | 136 |
| Activated PRP with DBM (demineralized bone matrix) | Athymic rats | Increased osteoconductivity | 137 |
| PRP gel | Diabetic fracture healing rats | Increased healing | 138–140 |
| PRP gel | 50-patient randomized clinical study for autograft positioning for ACL surgery | Increased cortical bone formation | 141,142 |
| PRP gel | Non-union long-bone regeneration | Lesser complications | 143 |
| PRP gel with autologous and/or allogeneic bone | Tibia fracture of a diabetic patient | Bridged bone defect | 144 |
| PRP gel with autologous and/or allogeneic bone | Rabbit tibia | Increased bone regeneration | 145 |
| Alginate hydrogel | MSCs in vitro | Increased alp and mineralization activity | 146 |
| Alginate beads and capsules | SaOS-2 osteoblast-like cell in vitro | Increased alp and proliferation | 147 |
| Alginate hydrogel | Mouse subcutaneous | Increased ectopic bone regeneration | 148 |
| Gelatin hydrogel/sponge | Rabbit ulna and calvarial defects | Increased bone regeneration | 149,150 |
| SEW2871, of a sphignosine-1 phosphate agonist and PRP were combined in micelles and incorporated into gelatin hydrogels | Rat | Increased recruited macrophages | 151 |
| Collagen sponges | Pig model with a critical-size defect (10×8 mm) | Increased bone regeneration | 152 |
| Biphasic calcium phosphate or deproteinized bovine bone | 20 patients with sinus augmentation | Increased osseointegration | 153 |
| Allogenic PRP+bone morphogenic protein 7 (BMP7)+CaP coated electrospun PCL | Full thickness diaphyseal segmental rat femoral defects | Significantly increased bone volume and biomechanical properties | 154 |
| Bioactive glass | Premolar defects in dogs | Improved bone formation | 155 |
| BMSCs+PRP | Intervertebral disc degeneration in rabbits | Increased regeneration of early degenerated discs | 156 |
Abbreviations: BMSC, bone marrow-derived mesenchymal stem cell; PRP, platelet-rich plasma.
Bone regeneration process
Bone growth is a combination of two pathways, that is, intramembranous and endochondral.157 After the condensation and merger of the MSCs has occurred, it serves as an architecture for the process of bone formation.158 Intramembranous bone formation consists of the process where the mesenchymal progenitor cells differentiate into osteoblastic cells and form the mandible, clavicle and other bones.159 Whereas, the process of endochondral bone formation involves the process of formation of most of the long bones in the body which is characterized by the differentiation of the mesenchymal progenitor cells into chondrocytes, thereby leading to the formation of a template made of cartilage which is later replaced by bone.160
The process of endochondral and intramembranous bone formation is regulated by various genes and proteins that are similar even though there are several differences in the structure and composition of the bone at various levels. Several proteins like the Indian Hedgehog (Ihh), parathyroid hormone related peptide (PTHrP), BMPs, and FGF are key regulators in both the processes of bone formation.161 However, the BMPs, Ihh, and PTHrP are extremely essential and are required for the co-ordination of the balance between chondrocyte proliferation and hypertrophy and regulate the thickness of the growth plate.162 As far as the intramembranous bone formation process is concerned, these key regulator proteins stimulate the undifferentiated mesenchymal progenitor cells to differentiate into pre-osteoblastic cells which co-express chondrocytic and osteoblastic markers simultaneously.163
Generally, the process of bone defect repair is similar to the process of intramembranous and endochondral bone formation which occurs by the initial development of a hematoma, accompanied by an inflammatory response and the combination of several cell signaling and key regulator protein molecules like ILs, TNF-α, FGF, BMPs, PDGF, and VEGF. Interestingly, the entire process is completed without the formation of scar tissue.164 The healing of the bony defect at the periosteum follows the process of intramembranous bone formation which occurs because of the role of the proteins on the mesenchymal progenitor cells, whereas the soft tissues stabilize the callus by the process of endochondral bone formation which involves the transition of the totipotent MSCs into chondrocytes, followed by maturation and mineralization, leading subsequently to the process of new bone formation and subsequent remodeling of the newly formed bone.165
Hence, it is imperative to develop techniques to combat and mimic the bone development process or the bone defect repair process. It is indeed necessary to place importance on both the processes since both the process are nearly similar and consists of an initial hematoma formation as well as the inflammatory response to healing and both the processes require the presence of the bone GFs and signaling molecules.166,167 The field of bone engineering should lay emphasis on the following factors:
Presence of totipotent stem cells
Signaling pathways, genes, and proteins
The presence of a good scaffold that is osteoinductive and osteoconductive
The understanding that normal tissue healing involves progressive remodeling and restructuring of pre-existing tissue structures
Angiogenesis and neo vascularization
The use of PRP in bone regeneration and cartilage formation have long been implicated.168 Marx had proposed the first protocol for the isolation of PRP using calcium and thrombin.29 Additional protocols have been proposed ever since which differ in the pathway of platelet activation and leukocyte concentration.120 It has been noted that the absence of leukocytes may prevent the release of pro-inflammatory cytokines which might increase the inflammation during wound healing thus decreasing and interfering with the mechanism of bone growth. However, Choukroun’s technique (L-PRF) has mentioned that the presence of leukocytes in the PRP enhance the host immune defense objective and role. Also, the enzyme, myeloperoxidase contained in the monocytes and neutrophils exhibit bactericidal properties that can decrease bacterial infections and contaminations associated with the wound healing process.118
PRP is activated using calcium and thrombin. The addition of calcium and thrombin activates the coagulation pathway to release the GFs.125 Thrombin is known to contain bovine factor V and its systemic use is associated with increased blood clotting and coagulopathies leading to cross reactivity between anti-bovine factor V antibodies with human factor V.169 However, studies have noted that the presence of thrombin in the circulatory system may lead to the formation of blood clots thereby provoking a myocardial infarction. Therefore, it is necessary to eliminate thrombin and activate the PRP using only calcium chloride. Studies have demonstrated that there is no difference in the concentration of GFs or the degree of activation when calcium chloride is used as an activator for the coagulation pathway as compared to the use of thrombin.132 However, the only disadvantage to using calcium chloride in the activation of PRP involves an increased period required for activation. A thrombin receptor agonist peptide (TRAP) can also be used in lieu of the thrombin which is similar in function. It has been noted that for in vitro studies, it is imperative to activate the PRP in order to release the GFs embedded in it.170 However, in vivo studies may not require the activation of the PRP.171
When PRP is employed in conjunction with MSCs in vitro, the findings have demonstrated that it tends to increase the cellular proliferation but decreases the osteogenic differentiation.172 PRP is generally seen to have suppressed the alkaline phosphatase activity in vitro, however increasing the cellular proliferative activity.173 The increased cellular proliferative activity may result in the altered morphology of the cell distribution result in the formation of pre-osteoblastic cells.174 BMP2 increases the osteogenic differentiation of MSCs and appears to have a role opposite to PRP, since in vitro studies have not shown an increased proliferative activity of MSCs with the use of BMP2 only.175 When BMP was used in conjunction with PRP, PRP could inhibit the activity of BMP, thus increasing the proliferation activity but decreasing the osteogenic potential of the MSCs.174 After the complete release of the GFs, the MSCs regains its responsiveness to the BMPs176 (Table 3).
Table 3. PRP application in vitro.
| Cell type | Application to culture | Outcome | Reference |
|---|---|---|---|
| Bone | |||
| Mouse BMSCs | PRP-BMP2 genetically modified MSCs(2.5%–5% PRP for in vitro and 10% for ex vivo) | Improve BMSCs proliferation and differentiation | 177 |
| Synovial fluid MSCs | SF-MSCs-alginate system (20%–50% PRP) 50% demonstrated highest activity | Promoted MSCs proliferation and chondrocyte differentiation | 178 |
| MSCs derived from canine umbilical cord | Co-cultured with PRP and demineralized bone matrix. | Induced osteogenesis in vitro of MSCs derived from the umbilical cord | 179 |
| BMSCs | BMSCs+PRP | Increased MSCs proliferation and differentiation | 176 |
| Human ASCs | Combination of chitosan-PRP and either Nano-hydroxyapatite or tricalcium phosphate | Enhanced MSCs proliferation and differentiation | 180 |
| Human DPSCs | PRP (1%, 5%, 10%, 20%) | 1%–10% PRP showed significant effect of promoting hDPSC osteogenic differentiation | 181 |
| DPSCs | DPSC+PRP | Increased DPSCs proliferation at 0.5% and 1% PRP concentration but decreased at 5% concentration. Long-term treatment with 1% PRP showed most significant enhancement at 96 h. | 182 |
| Human ASCs | culture medium containing 10 mL·L−1 PRP | Increased ASCs osteogenic differentiation and proliferation | 183 |
| Human MSCs | calcium phosphate scaffolds+PRP | Increased MSCs osteogenic differentiation and proliferation | 184 |
| Cartilage | |||
| Human MSCs | 10% PRP | Increased MSCs proliferation and chondrogenesis | 173 |
| Human BMSCs | 10% PRP | Increased MSCs migration and proliferation | 185 |
| Human ASCs | 10% PRP | Increased ASCs proliferation and preservation of immunophenotype and differentiation | 186 |
| Mouse MDSCs | 10% PRP | Upregulation of type II collagen and improved MDSCs proliferation | 187 |
| Nude rat MDSCs | PRP+VEGF antagonist+BMP-4 | Type II collagen increased | 188 |
| Sheep MDSCs | PRP | Increased MDSCs proliferation | 189 |
| Human ADSCs | PRP and insulin in 3D collagen scaffold | Increased chondrogenic and osteogenic differentiation of ASCs | 190 |
Abbrevations: BMSC, bone marrow-derived mesenchymal stem cell; DPSC, dental pulp stem cell; MDSC, muscle-derived stem cell; MSC, mesenchymal stem cell; PRP, platelet-rich plasma; VEGF, vascular endothelial growth factor.
A concentration of 2%–5% PRP is ideal for the osteogenic differentiation of the MSCs in vitro. Any concentration below or above inhibits the osteogenic potential of MSCs.191 Likewise, an increase in the concentration of MSCs increases the cell proliferative activity of the MSCs. However, conditions need to be optimized for clinical studies. L-PRF can stimulate the osteogenic differentiation and proliferation of the human MSCs in vitro in a dose-dependent manner as compared to PRP without leukocytes.192 When cultured with one PRF membrane, around 160%–210% proliferation rate can be expected in comparison to the use of two membranes,where 190%–380% can be achieved for up to 14 days in culture.184,193
MSCs, adipose- and muscle-derived stem cells (MDSCs) and human subchondral bone-derived progenitor cells are among the commonly employed stem cells in the field of cartilage engineering.194 Studies have reported that PRP can induce mitogenic effects on MSCs. And when MSCs were treated with PRP in vitro for 7 days, while both chondrogenic and osteogenic gene markers were upregulated and the chondrogenic markers, including Sox9 and aggrecan, increased much more (over 10-fold increase) than RUNX2 (less than 2-fold increase),195 a marker of early osteogenic differentiation. Furthermore, when muscle-derived MSCs were treated with PRP in vitro, their ability to proliferate, adhere and migrate was significantly promoted, however, the chondrogenic gene expression was not upregulated.188 Moreover, PRP could also stimulate the vertical migration of subchondral progenitors and cartilaginous matrix accumulation in vitro.196 These reports suggest that PRP might be able to enhance the migration of the subchondral progenitors to repair cartilage defects.
Bone tissue engineering consists of a combination of cell, GFs and a good scaffold that exhibits osteoinductive and osteoconductive properties. PRP was able to modify the properties of MSCs when seeded on a synthetic scaffold, owing to the fact that the GFs present in the PRP could provide a nutritive environment to the MSCs.197 It was noticed that the MSCs could adhere better to the scaffold in the presence of the PRP. However, the excellent adherence was limited to the high specific surface area of the calcium scaffold in comparison to the lower surface area counterparts of β-tricalcium phosphate. In the presence of hydroxyapatite and silica coated hydroxyapatite scaffolds, platelet poor plasma was able to stimulate the osteogenic differentiation of goat MSCs greater than the platelet lysates.198
MSCs can also be administered in conjunction with other bone grafting materials in order to increase its bone growth potential. Demineralized bone grafts can accelerate the cellular proliferative activity of human MSCs in vitro, but can alsodecrease osteogenic differentiation potential.199 On the contrary, when human MSCs are administered alongside freeze-dried bone allografts, they can significantly increase the osteogenic differentiation potential in vitro in an osteogenic media along with the GFs after 1–15 days.200,201
There are very few methods to evaluate the conformation of the conversion of MSCs into osteoblastic cells in vivo. Hence, Freidenstein proposed the first in vivo assay for the determination of the transition of MSCs into an osteoblastic lineage and used ‘diffusion chambers’ to study the differentiation potential of MSCs.202,203 The gold standard assay at present to study the differentiation potential of MSCs in vivo is implanting MSCs into a β-tricalcium phosphate scaffold in SCID mice by subcutaneous implantation since the heterogeneity of MSC cultures and considerable donor variability preclude standardized production of MSC and point on functional deficits for some human MSC populations, this assay was developed in order to predict the therapeutic capacity of human MSC before clinical transplantation.203,204
In critical-sized defects, MSCs combined with PRP and BMP2 have demonstrated the greatest bone formation effect.84 It has been observed that a single component alone cannot achieve good results as compared to the combination of MSCs BMP2 and PRP. The only problem is the optimizing the ratio of PRP to bone graft. PRP has been shown to promote the osteogenic differentiation of osteoblastic precursors. However, when implanted in vivo, it does not show to have a greater effect on the regeneration process of bone as compared to the use of MSCs alone. When implanted at an ectopic region in goats, MSCs with PRP did not seem to have any significant regenerative effect on the critical-sized defects as compared to MSCs alone when MSCs was seeded on scaffolds made of hydroxyapatite and β-tricalcium phosphate.191,205
In bone regeneration around the dental implants in the canine mandible, it was observed that the combination of MSCs with PRP led to excellent bone formation and vascularization which was comparable to bone regenerated by autologous bone alone.191 When MSC was combined with PRP fibrin gel and was used for alveolar augmentation in a canine model, the findings demonstrated the highest amount of dental osteointegration. A combination of MSCs, BMP2 and PRP in a gelatin, β–tricalcium phosphate scaffold demonstrated good regeneration in an equine cartilage defect repair within 16 weeks.206 PRP can thus, promote bone regeneration in the beginning stages of bone formation and bone healing. However, it does not seem to have an effect on the later stages on bone formation due to early dissolution of fibrin and GFs. PRP can also effectively increase bone formation when administered in a natural or synthetic scaffold like hydroxyapatite and β-tricalcium phosphate. But, the lack in the consistency of the results can be attributed to the heterogeneity of the studies (Table 4).
Table 4. PRP application in animal models.
| Cell type | Application | Animal model | Outcome | Reference |
|---|---|---|---|---|
| Rat BM-BMSCs | PRP gel/calcium phosphate particles | Rat femoral defect (2.5×5 mm)followed up at 4 weeks. | Increased BMSCs alp activity and proliferation | 207 |
| Equine MSCs | Gelatin/β-tricalcium phosphate (GT) sponge loaded with MSCs and BMP2 | Equine osteochondral defects | The GT with MSCs/BMP2 group showed significantly higher macroscopic scores than the control group. In addition, hyaline cartilaginous tissue was detected in the test group in areas larger than those in the control group. | 208 |
| Murine ADSCs | (ADSCs) combined with PRP, and implanted on bone mineral matrix (BMM) | Subcutaneous mouse | The highest relative expression of bone-related genes and osteocalcin expression was found at the 15th day of in vitro osteogenic induction of the ADSCs. Expression peaks of bone-related genes in implants were at 2 and 4 weeks, but they significantly decreased at 8 weeks. The signs of resorption, formation of callus-like tissue positive for osteocalcin and increased presence of bone cells were found in experimental sites compared with control sites. | 209 |
| ASCs from inguinal fat pads of F344 inbred rats | ASCs with 5% PRP | Rat calvarial defect model | Increased osteogenesis and augmentative effects in the ASCs with 5% PRP group on bone regeneration in vivo as compared with the control. | 210 |
| Human PDLSCs | (PDLSC) sheets and 1% PRP | Subcutaneous immunocompromised mice | Based on the production of extracellular matrix proteins, the results of scanning electron microscopy and the expression of the osteogenic genes ALP, Runx2, Col-1 and OCN, the provision of 1% PRP for PDLSC sheets was the most effective PRP administration mode for cell sheet formation as compared to without PRP intervention. | 211 |
| Rabbit osteogenic-induced MSCs | Ceramic block with osteogenic-induced MSCs & PRP | Critical-sized segmental tibia defect in rabbits | The experimental group tibiae achieved the highest compressive strength (43.50±12.72 MPa) compared to those treated with control (23.28±6.14 MPa). | 212 |
| Rat UC-MSCs | (UC-MSCs) with 10% PRP | Rat critical-sized calvarial defects | PRP enhanced UC-MSC proliferation, and 10% PRP caused the strongest ALP and Alizarin red staining. At 7 days, the expression levels of ALP, Collagen 1 (COL-1) and Runt-related transcription factor 2 (RUNX2) in the PRP group were higher than those in the FBS group. | 213 |
| Rabbit ADSCs | ADSCs+PRP in alginate microspheres | In vivo subcutaneous injection of New Zealand rabbits | A blood vessel network was found within the 10% PRP and 15% PRP-ADSC implants, which was associated with a significant increase inmineralization. | 214 |
| BMSCs | PRP/BMSCs gel membrane | Ectopic mouse model and rabbit segmental bone defect model | The cells secreted significant amounts ofsoluble proangiogenic factors, such as PDGFBB, VEGF, and interleukin-8 (IL-8) | 84 |
| Murine MSCs | MSC associated with 50.0 μL of plasma gel containing 1.0×109 autologous platelets | C57BL/6 gfpGFP(+) Mice and cranial defect of 6.0mm in diameter | At 10 days, the area of new bone formationwidened, at 30 days, was higher toward the center of the defect and at day 60, identified himself to the larger amount of bone tissue and more organized than had hitherto been observed | 215 |
| Canine DPSC, BMSC, and periosteal cells (PC) | DPSC, BMSC, and PC with PRP | Mandibular implants in dogs | DPSC showed the highest osteogenic potential around dental implants. | 216 |
| Angiopoietin 1 gene-transfected rabbit BMSCs | Angiopoietin 1 gene transfected BMSCs+PRP | Radial segmental bone defects (15 mm in length) were created in 20 3-month-old New Zealand rabbits | Callus formed at 4 weeks, partial bony union was observed at 8weeks, and complete union at 12 weeks. | 217 |
| Canine MSCs | A nanofiber scaffold, Pura Matrix (PM)+dMSCs+PRP | Implants in the region of first molar and all premolars in the mandibular regions of dogs | Bone-to-implant contact was highest in the PM, dMSCs, and platelet-rich plasma group at 55.64%. | 218 |
| Stem cells from deciduous teeth, dental pulp, and bone marrow | Stem cells from deciduous teeth (DTSCs), dental pulp (DPSCs), and bone marrow + PRP | Bone defects were prepared on both sides of the mandible canine mandible | Histologically, the cMSCs/PRP, cDPSCs/PRP, and cDTSCs/PRP groups had well-formed mature bone and neovascularization compared with the control (defect only) and PRP groups at 4 and 8 weeks, respectively, and the mineralized tissues in cMSCs/PRP, cDPSCs/PRP, and pDTSCs/PRP specimens were positive for osteocalcin at 8 weeks. | 219 |
| Human alveolar BMSCs (hABMSCs) | (hABMSCs)+0.5% PRF(platelet-rich fibrin) | Critical-sized defect in mice calvaria | Transplantation of the fresh PRF into the mouse calvarias enhanced regeneration of the critical-sized defect. | 220 |
| Dog MSCs (dMSCs) | dMSCs and/or PRP | Adult hybrid dog's mandible region | PM/dMSCs and PM/dMSCs/PRP groups showed a significant increase at all weeks compared with the control, PM, or PM/PRP in new bone formation. | 221 |
| MSCs | MSCs + PRP | Critical-size long-bone defects in diaphyseal rabbit model | PRP yielded better bone formation with CDHA scaffold as determined by both histology and micro-computer tomography (p<0.05) after 16 weeks. | 184 |
| MSCs | PRP | Sinus augmentation in minipigs | After 12 weeks, a significant increase in bone formation occurred in the Test sites compared with the control sites. In addition, BIC was significantly greater in the test sites compared with the control sites in the regenerated area | 222 |
| MSCs | Fibrin glue and PRP | Simultaneous implant placement and bone regeneration around dental implants in hybrid dogs | dMSCs/PRP/fibrin demonstrated the highest 53% bone implant contact at 8 weeks. | 223 |
| MDSCs | PRP | Osteoarthritis model for nude rats | Increase in type II collagen and decreased chondrocyte apoptosis. | 188 |
| MDSCs | PRP | New Zealand white rabbit(osteochondral defect) | Higher cartilage gene and protein expression. Improved immunohistochemical and histological characteristicsin association with the MDSCs with PRP group | 224 |
| Allogeneic ASCs | PRP | Equine superficial digital flexor tendonitis (SDFT) | At 24-month follow-up, reinjury rate was only 10.5%. Decreased pain. | 225 |
| Bone marrow aspirate concentrate | PRP | porcine osteochondral defect model | The Bone marrow aspirate concentrate group with PRP demonstrated increased collagen type II. Asignificant improvement of the histological characteristics. | 226 |
| Synovial membrane-derived MSCs | PRP | osteochondral defects in a new Zealandrabbit model | Increased type II collagen content, glycosaminoglycan content, cumulative histologic scores, and number of proliferating cells. | 227 |
| Autologous BMSCs | PRP | Equine tendonitis and desmitis | Implanted MSCs caused no adverse reactions and thirteen out of the 18 inoculated horses returned to race competitions. On the contrary, no improvement was seen in the twelve animals of group 2 treated with pin firing, that were not able to resume sport activity. | 228 |
| ASCs | Subcutaneous injection of the PRP alginate microspheres | Mouse subcutaneous | Blood vessel network was found within the 10% PRP and 15%PRP-ADSC implants. Significant increase in mineralization. | 214 |
| MSCs | PRP/deproteinized bone matrix (DPB) | 1.5-cm segmental radial defects in New Zealand whiterabbits | The implantation of allogeneic PRP/(DPB) constructs group demonstrated successful bridging of the 1.5-cm segmental radial defects in rabbits, achieving similar healing capacity as autologous MSC/DPB constructs (MSC+DPB), with greater bone formation and vascularization than DPB alone, shown by histomorphometric analysis, bone mineral density measurement, and radionuclide bone imaging. | 229 |
| BMSCs | PRP | 5 mm calvarial defects in New Zealand white rabbits | Substantial bone regeneration was observed at the calvarial defect restored with PRP incorporating the induced BMSCs at 8 weeks post implantation. In contrast, no bone regeneration was detected at the defects implanted with the whole blood incorporating BMSCs, whether the BMSCs were induced or not. | 199 |
| Rat BMSCs | PRP | Achilles tendon ruptures created surgically in Sprague Dawley rats | The use of rBMSC and PRP in the Achilles tendon ruptures when the tendon is in its weakest phase positively affected the recovery of the tendon in histopathologic, immunohistochemical, and biomechanical manners compared to the control group (P<0.05). The levels of pro-inflammatory cytokines TNF-α, IFNγ, and IL-1β were significantly low, the levels of anti-inflammatory cytokines and GFs playing key roles in tendon recovery, such as IL2, VEGF, TGF-β, and HGF, were significantly higher in the MSC group than those of the PRP and control groups (P<0.05). | 230 |
Abbrevations: ADSC, adipose-derived stem cell; BMSC, bone marrow-derived mesenchymal stem cell; DPSC, dental pulp stem cell; IFNγ, interferon-γ; IL-1β, interleukin-1β; MDSC, muscle-derived stem cell; MSC, mesenchymal stem cell; PRP, platelet-rich plasma; TGF-β, transforming growth factor-β; TNF-α, tumor necrosis factor-α; VEGF, vascular endothelial growth factor.
Clinical applications of stem cells and PRP in orthopedics
PRP is generally and extensively employed in the field of orthopedics for the regeneration of defects and fractures. PRP in conjunction with MSCs has been proposed for the treatment of unions of fractures, distraction osteogenesis, spinal fusions, and periodontal defects, post extraction bone regeneration and dental osteointegration (Table 5).The major advantage for using PRP is that PRP has antimicrobial effects in vitro. Low volume WBC containing PRP can reduce inflammation. No side effects have been reported in 146 patients that were treated with PRP for bone regeneration. Many studies have suggested safety, increased bone formation, wound healing and vascularization with the use of PRP; adverse effects are rare risks, and benefits have been thoroughly reviewed. Due to the early dissolution of PRP and fibrin resorption, the risk of developing an adverse reaction to PRP is rare.
Table 5. PRP application in the clinic.
| Sample size (patients) | Treatment | Time | Outcome | References |
|---|---|---|---|---|
| 44 | Open-wedge high tibia osteotomy (HTO) with or without Human MSC therapy and PRP injection. | 24–36 months | The MSC-PRP group showed significantly greater improvements in the KOOS subscales for pain and symptoms. Arthroscopic evaluation, at plate removal, showed that partial or even fibrocartilage coverage was achieved in 50% of the MSC-PRP group patients but in only 10% of the patients in the PRP-only group (P<0.001). | 231 |
| 24 | Delayed fracture union: PRP, sorted Human MSCs in suspension and DBM (Ignite ICS injectable scaffold) | 2, 6 weeks, 3, 6, 9 and 12 months. | No significant difference in VAS (visual analog scale), at 6-month time point, all fractures in the intervention group had healed, 25% of the control group experienced delayed union as their fractures did not unite by the 3-month follow-up. | 232 |
| 72 | Bone non-union: 6–8 mL platelet-rich plasma prepared by centrifugalizing venous blood and MSCs extracted from human umbilical cord. | 2 years | No loosening and breakage of internal fixation were observed in two groups at 2 years. The motility and function of hip, knee and ankle were good. Significantly higher healing rate in MSC+PRP group. | 233 |
| 6 | Human MSC+PRP −972 269 (range 524 480–2 033 000) in sinus augmentation and alveolar ridge augmentation. | 6 months | At 6 months after loading, as tested after removal of the prosthetic reconstruction, all implants maintained stability. Marginal bone resorption at 6 months after loading did not exceed 1.5 mm. | 234 |
| 23 | Injectable Human BMSCs and autologous PRP | 3, 6 months and 1 year | Increased bone formation and Osseointegration.The mean regenerated bone height was 8.2±1.6 mm and 8.0±1.4 mm, and the average alveolar bone height was 15.6±1.2 mm and 15.1±1.4 mm, at 3 and 6 months, respectively. There were significant differences between pre-operative values and post-operative ones (at 3 and 6 months). No perforations of the Schneider membrane were found and the inserted implants were successful after 1 year. | 235 |
| 01 | Human MSCs and PRP | 6 months | Re-examination at 6 months demonstrated that the application of MSCs-PRP gel at periodontal sites with angular defects, resulted in a 4-mm reduction in probing depths and a 4-mm clinical attachment gain, while bleeding and tooth mobility disappeared. Radiographic assessments showed that the bone defect had been reduced in depth. | 236 |
Abbrevations: BMSC, bone marrow-derived mesenchymal stem cell; DBM, demineralized bone matrix; MSC, mesenchymal stem cell; PRP, platelet-rich plasma.
Sinclair et al.237 in their systematic review paper described the effects of MSCs and PRP in fractures and non-unions, which included 39 papers involving trials on the effects of GFs and MSCs on non-unions or bone repair. They reported that MSCs and PRP when used as a single entity or combined together, significantly promoted fracture and non-union repair as well as synergistically enhance wound healing. When administered in conjunction, MSC and PRP demonstrated excellent implant success in titanium implants.11 Implants of β-TCP seeded with MSC and PRP for maxillary sinus floor augmentation were clinically stable 12 months after loading.238 In a randomized controlled study, it was noticed that PRP, if combined with MSC, increased the osteogenic potential of lyophilized bone chips.239 The strength of this clinical research was the randomization and the comparison among different treatments (freeze-dried bone allograft alone or in combination with PRP with or without MSC); its weakness was the lack of the evaluation of PRP effect in alone and of a clear primary outcome. However, more well designed protocols and studies and rigorous clinical trials using consistent techniques may lead to more conclusive general recommendations. Patients, suffering from achondroplasia (ACH), hypochondroplasia (HCH) or congenital pseudo arthrosis or distraction osteogenesis were given MSCs with PRP.240 The femoral lengthening showed significantly faster healing than did the tibial lengthening and transplantation of BMSCs and the PRP shortened the treatment period by accelerating new bone regeneration during distraction osteogenesis of the lower extremity in patients with ACH and HCH.240
Challenges
Although several reports have elaborated on the advantages of PRP in the fields of periodontal, bone and cartilage regeneration, there are still several challenges to be addressed.241 To begin with, we have not yet been able to obtain consistent results from the insufficient pre-clinical and clinical data on the immunogenicity and protective effects of stem cells.242 Also, several questions need to be answered before these procedures can be clinically translated.243 First, it is important to determine the molecular immune mechanisms and cells that are involved in these responses, the dynamic fate of these implanted ASCs, assessment of its clinical efficiency and factors that influence these inconsistent results.244
Another challenge is in obtaining a homogenous composition of PRP, since its composition displays relatively strong intra-patient variation.245 Moreover, its variation is correlated with age, sex, and patient comorbidities.246 Furthermore, it remains unclear about how these changes will affect stem cell behavior in vivo.247 Even the preparation methodology can significantly affect its composition and there is no standard protocol in literatures to obtain PRP gel or PRP for clinical application. These incongruences reduce the comparability and reproducibility of the various PRP studies.214 These challenges can be addressed by initiating systematic high throughput analyses.
Stem cells like MSCs, ASCs and MDSCs have shown great promise in the field of tissue and bone engineering for the regeneration of bone, periodontium and cartilage formation.248 However, one of the greatest challenge is obtaining a population with negligible heterogeneity, which can be overcome by cell sorting according to its characteristics, cell markers.249 However, large scale production of the stem cells may be inconvenient owing to the difficulty in obtaining a population of cells that are phenotypically and genetically similar. Moreover, the effectiveness of genetically modified MSCs has been reported in different disease models.250 However, the stability of the transfected cell lines may appear to be a challenge and potentiates further investigation.
Summary and perspective
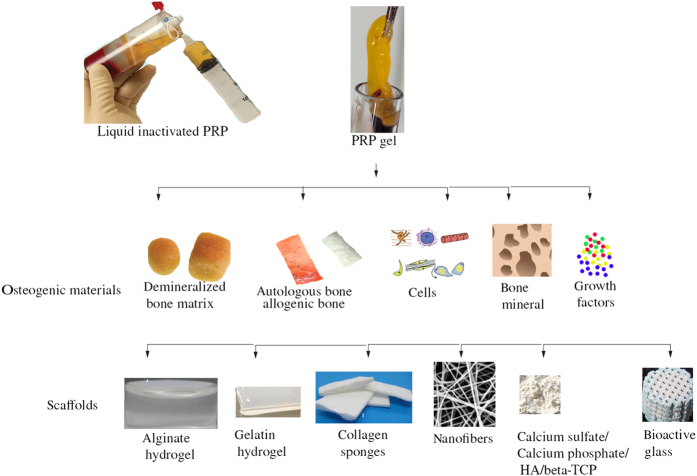
PRP consists of a cocktail of GFs which can promote osteogenic differentiation extensively and efficiently and yet appears to be inefficient as perceived from the findings in the clinical studies.125 The reason can be attributed to the fact that although, PRP is abundant in the bone GFs, these factors are released almost immediately when implanted into the body with the overall exhaustion of the factors occurring within twenty-four hours. The process of bone regeneration as previously described occurs over a span of 4-6 weeks. Hence, the effect of the PRP is almost negligible as far as bone healing is regarded. This makes it imperative to deliver the PRP in such a manner that the GFs may able to be sustained over the period of bone regeneration. Studies have employed the use of beads and capsules for the delivery of the PRP147 (Figure 2). Alginate capsules have however, demonstrated a consistent and greater concentration of GFs as compared to the beads, probably due to the chemical composition of the beads which allows the calcium ions to bind and integrate with the PRP, hence decreasing its ability to release the GFs efficiently.251 Moreover, the beads can be optimized to overcome this problem. The beads and capsules can also be allowed to incorporate a combination of PRP and GFs that may be able to increase the osteogenic differentiation of MSCs (unpublished data). As PRP is a good cell proliferator and BMPs are good osteogenic differentiators, it makes it feasible to administer them in conjunction with each other in order to increase the formation of bone in critical-sized defects.252 Furthermore, PRP with the GF beads can be double encapsulated with cements like Nano calcium sulfate. The slow degradation rate of Nano calcium sulfate would enable the PRP to be released at the peak of bone formation thus increasing its efficiency for bone formation greatly in clinical studies.253 As reviewed here, PRP and stem cells can be employed in conjunction for the regeneration of bone. However, since PRP leads to the cellular proliferation of pluripotent cells, it is important to incorporate a GF component as well, especially as bone Morphogenic protein since it can increase the osteogenic differentiation of bone. But, the fast degradation rate of the fibrin and the dissolution of PRP restricts its use to just in the early stages of bone healing and is negligible in the late stages of bone development. Hence, it is necessary to use and deliver the PRP via a carrier which can degrade slowly, so as to release the PRP GFs in a sustained manner. Future studies would have to be focused on developing a carrier for the delivery of GFs to increase its overall efficacy.
Figure 2.
Clinical delivery of PRP for bone regeneration.
Acknowledgments
We apologize to the many researchers whose work could not be cited due to space limitations. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and National Institute of Dental and Craniofacial Research under Award Numbers AR061052, AR066101 and DE023105 to S.Y. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare no conflict of interest.
References
- Moga G. Bone grafts. J Foot Surg 1976; 15: 125–127. [PubMed] [Google Scholar]
- Aichelmann-Reidy ME, Yukna RA. Bone replacement grafts. The bone substitutes. Dent Clin North Am 1998; 42: 491–503. [PubMed] [Google Scholar]
- Brunsvold MA, Mellonig JT. Bone grafts and periodontal regeneration. Periodontol 2000 1993; 1: 80–91. [PubMed] [Google Scholar]
- Delloye C. [Bone grafts using tissue engineering]. Bull Mem Acad R Med Belg 2001; 156: 418–425. [PubMed] [Google Scholar]
- Garrett S, Bogle G. Periodontal regeneration with bone grafts. Curr Opin Periodontol 1994: 168–177. [PubMed]
- Li W, Xiao L, Hu J. The use of enamel matrix derivative alone versus in combination with bone grafts to treat patients with periodontal intrabony defects: a meta-analysis. J Am Dent Assoc 2012; 143: e46–e56. [DOI] [PubMed] [Google Scholar]
- Yukna RA. Synthetic bone grafts in periodontics. Periodontol 2000 1993; 1: 92–99. [PubMed] [Google Scholar]
- Wiesmann HP, Nazer N, Klatt C et al. Bone tissue engineering by primary osteoblast-like cells in a monolayer system and 3-dimensional collagen gel. J Oral Maxillofac Surg 2003; 61: 1455–1462. [DOI] [PubMed] [Google Scholar]
- Boeckel DG, Shinkai RS, Grossi ML et al. Cell culture-based tissue engineering as an alternative to bone grafts in implant dentistry: a literature review. J Oral Implantol 2012; 38 Spec No: 538–545. [DOI] [PubMed] [Google Scholar]
- Andric T, Wright LD, Taylor BL et al. Fabrication and characterization of three-dimensional electrospun scaffolds for bone tissue engineering. J Biomed Mater Res A 2012; 100: 2097–2105. [DOI] [PubMed] [Google Scholar]
- Yamada Y, Hara K, Nakamura S et al. Minimally invasive approach with tissue engineering for severe alveolar bone atrophy case. Int J Oral Maxillofac Surg 2013; 42: 260–263. [DOI] [PubMed] [Google Scholar]
- Caplan AI, Sorrell JM. The MSC curtain that stops the immune system. Immunol Lett 2015; 168: 136–139. [DOI] [PubMed] [Google Scholar]
- Caplan AI, Correa D. The MSC: an injury drugstore. Cell Stem Cell 2011; 9: 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva Meirelles L, Sand TT, Harman RJ et al. MSC frequency correlates with blood vessel density in equine adipose tissue. Tissue Eng Part A 2009; 15: 221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmetz NJ, Aisenbrey EA, Westbrook KK et al. Mechanical loading regulates human MSC differentiation in a multi-layer hydrogel for osteochondral tissue engineering. Acta Biomater 2015; 21: 142–153. [DOI] [PubMed] [Google Scholar]
- Arany PR, Huang GX, Gadish O et al. Multi-lineage MSC differentiation via engineered morphogen fields. J Dent Res 2014; 93: 1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory CA, Ylostalo J, Prockop DJ. Adult bone marrow stem/progenitor cells (MSCs) are preconditioned by microenvironmental "niches" in culture: a two-stage hypothesis for regulation of MSC fate. Scis STKE 2005; 2005: pe37. [DOI] [PubMed] [Google Scholar]
- Hamada H, Kobune M, Nakamura K et al. Mesenchymal stem cells (MSC) as therapeutic cytoreagents for gene therapy. Cancer Sci 2005; 96: 149–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathiasen AB, Qayyum AA, Jørgensen E et al. Bone marrow-derived mesenchymal stromal cell treatment in patients with severe ischaemic heart failure: a randomized placebo-controlled trial (MSC-HF trial). Eur Heart J 2015; 36: 1744–1753. [DOI] [PubMed] [Google Scholar]
- DeGowin RL, Gibson DP. Prostaglandin-mediated enhancement of erythroid colonies by marrow stromal cells (MSC). Exp Hematol 1981; 9: 274–280. [PubMed] [Google Scholar]
- Zhuang H, Zhang X, Zhu C et al. Molecular Mechanisms of PPAR-gamma Governing MSC Osteogenic and Adipogenic Differentiation. Curr Stem Cell Res Ther 2016; 11: 255–264. [DOI] [PubMed] [Google Scholar]
- Vogl M, Fischer J, Jäger M et al. Can thrombin-activated platelet releasate compensate the age-induced decrease in cell proliferation of MSC? J Orthop Res 2013; 31: 1786–1795. [DOI] [PubMed] [Google Scholar]
- Hao J, Zhang Y, Jing D et al. Mechanobiology of mesenchymal stem cells: Perspective into mechanical induction of MSC fate. Acta Biomater 2015; 20: 1–9. [DOI] [PubMed] [Google Scholar]
- Schwartz-Arad D, Levin L, Aba M. [The use of platelet rich plasma (PRP) and platelet rich fibrin (PRP) extracts in dental implantology and oral surgery]. Refuat Hapeh Vehashinayim (1993) 2007; 24: 51–55, 84. [PubMed] [Google Scholar]
- Mautner K, Malanga GA, Smith J et al. A call for a standard classification system for future biologic research: the rationale for new PRP nomenclature. PM R 2015; 7: S53–S59. [DOI] [PubMed] [Google Scholar]
- Marques LF, Stessuk T, Camargo IC et al. Platelet-rich plasma (PRP): methodological aspects and clinical applications. Platelets 2015; 26: 101–113. [DOI] [PubMed] [Google Scholar]
- Georgakopoulos I, Tsantis S, Georgakopoulos P et al. The impact of Platelet Rich Plasma (PRP) in osseointegration of oral implants in dental panoramic radiography: texture based evaluation. Clin Cases Miner Bone Metab 2014; 11: 59–66. [PMC free article] [PubMed] [Google Scholar]
- Roffi A, Filardo G, Kon E et al. Does PRP enhance bone integration with grafts, graft substitutes, or implants? A systematic review. BMC Musculoskelet Disord 2013; 14: 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 2001; 10: 225–228. [DOI] [PubMed] [Google Scholar]
- Pacifici L, Casella F, Maggiore C. [Platelet rich plasma (PRP): potentialities and techniques of extraction]. Minerva Stomatol 2002; 51: 341–350. [PubMed] [Google Scholar]
- Vanassche B, Defrancq J. [Use of PRP (Platelet Rich Plasma) in bone volume augmentation]. Rev Belge Med Dent (1984) 2001; 56: 125–133. [PubMed] [Google Scholar]
- Choi BH, Zhu SJ, Kim BY et al. Effect of platelet-rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells: an in vitro study. Int J Oral Maxillofac Surg 2005; 34: 420–424. [DOI] [PubMed] [Google Scholar]
- Shashikiran ND, Reddy VV, Yavagal CM et al. Applications of platelet-rich plasma (PRP) in contemporary pediatric dentistry. J Clin Pediatr Dent 2006; 30: 283–286. [DOI] [PubMed] [Google Scholar]
- Cancedda R, Mastrogiacomo M, Bianchi G et al. Bone marrow stromal cells and their use in regenerating bone. Novartis Found Symp 2003; 249: 133–143. [PubMed] [Google Scholar]
- Vaquero J, Zurita M. Bone marrow stromal cells for spinal cord repair: a challenge for contemporary neurobiology. Histol Histopathol 2009; 24: 107–116. [DOI] [PubMed] [Google Scholar]
- Derubeis AR, Cancedda R. Bone marrow stromal cells (BMSCs) in bone engineering: limitations and recent advances. Ann Biomed Eng 2004; 32: 160–165. [DOI] [PubMed] [Google Scholar]
- Fridenshteĭn Ala, Piatetskiĭ-Shapiro II, Petrakova KV. [Osteogenesis in transplants of bone marrow cells]. Arkh Anat Gistol Embriol 1969; 56: 3–11. [PubMed] [Google Scholar]
- Friedenstein AJ, Piatetzky S II, Petrakova KV. Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol 1966; 16: 381–390. [PubMed] [Google Scholar]
- Zhang LX, Yin YM, Zhang ZQ et al. Grafted bone marrow stromal cells: a contributor to glial repair after spinal cord injury. Neuroscientist 2015; 21: 277–289. [DOI] [PubMed] [Google Scholar]
- Dezawa M. Insights into autotransplantation: the unexpected discovery of specific induction systems in bone marrow stromal cells. Cell Mol Life Sci 2006; 63: 2764–2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komori T, Yagi H, Nomura S et al. Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell 1997; 89: 755–764. [DOI] [PubMed] [Google Scholar]
- Abdul Rahman R, Mohamad Sukri N, Md Nazir N et al. The potential of 3-dimensional construct engineered from poly(lactic-co-glycolic acid)/fibrin hybrid scaffold seeded with bone marrow mesenchymal stem cells for in vitro cartilage tissue engineering. Tissue Cell 2015; 47: 420–430. [DOI] [PubMed] [Google Scholar]
- Wang P, Liu X, Zhao L et al. Bone tissue engineering via human induced pluripotent, umbilical cord and bone marrow mesenchymal stem cells in rat cranium. Acta Biomater 2015; 18: 236–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohgushi H. Osteogenically differentiated mesenchymal stem cells and ceramics for bone tissue engineering. Expert Opin Biol Ther 2014; 14: 197–208. [DOI] [PubMed] [Google Scholar]
- Bertolo A, Mehr M, Janner-Jametti T et al. An in vitro expansion score for tissue-engineering applications with human bone marrow-derived mesenchymal stem cells. J Tissue Eng Regen Med 2016; 10: 149–161. [DOI] [PubMed] [Google Scholar]
- Mattioli-Belmonte M, Teti G, Salvatore V et al. Stem cell origin differently affects bone tissue engineering strategies. Front Physiol 2015; 6: 266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennerfeldt DA, Van Vliet KJ. Concise review: when colonies are not clones: evidence and implications of intracolony heterogeneity in mesenchymal stem cells. Stem Cells 2016; 34: 1135–1141. [DOI] [PubMed] [Google Scholar]
- Lee KD. Applications of mesenchymal stem cells: an updated review. Chang Gung Med J 2008; 31: 228–236. [PubMed] [Google Scholar]
- Heldring N, Mager I, Wood MJ et al. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum Gene Ther 2015; 26: 506–517. [DOI] [PubMed] [Google Scholar]
- Satija NK, Gurudutta GU, Sharma S et al. Mesenchymal stem cells: molecular targets for tissue engineering. Stem Cells Dev 2007; 16: 7–23. [DOI] [PubMed] [Google Scholar]
- Bruder SP, Jaiswal N, Ricalton NS et al. Mesenchymal stem cells in osteobiology and applied bone regeneration. Clin Orthop Relat Res 1998; 335 Suppl: S247–S256. [DOI] [PubMed] [Google Scholar]
- Charbord P. Bone marrow mesenchymal stem cells: historical overview and concepts. Hum Gene Ther 2010; 21: 1045–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuk PA. The adipose-derived stem cell: looking back and looking ahead. Mol Biol Cell 2010; 21: 1783–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuk PA, Zhu M, Mizuno H et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 2001; 7: 211–228. [DOI] [PubMed] [Google Scholar]
- Zuk P, Chou YF, Mussano F et al. Adipose-derived stem cells and BMP2: part 2. BMP2 may not influence the osteogenic fate of human adipose-derived stem cells. Connect Tissue Res 2011; 52: 119–132. [DOI] [PubMed] [Google Scholar]
- Chou YF, Zuk PA, Chang TL et al. Adipose-derived stem cells and BMP2: part 1. BMP2-treated adipose-derived stem cells do not improve repair of segmental femoral defects. Connect Tissue Res 2011; 52: 109–118. [DOI] [PubMed] [Google Scholar]
- Levi B, James AW, Nelson ER et al. Human adipose derived stromal cells heal critical size mouse calvarial defects. PloS one 2010; 5: e11177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu M, Liu L. [Application of adipose-derived mesenchymal stem cells in craniomaxillofacial restoration and reconstruction]. Hua Xi Kou Qiang Yi Xue Za Zhi 2013; 31: 644–647. [PubMed] [Google Scholar]
- Oedayrajsingh-Varma MJ, van Ham SM, Knippenberg M et al. Adipose tissue-derived mesenchymal stem cell yield and growth characteristics are affected by the tissue-harvesting procedure. Cytotherapy 2006; 8: 166–177. [DOI] [PubMed] [Google Scholar]
- Shi S, Gronthos S. Perivascular niche of postnatal mesenchymal stem cells in human bone marrow and dental pulp. J Bone Miner Res 2003; 18: 696–704. [DOI] [PubMed] [Google Scholar]
- Akiyama K, Chen C, Gronthos S et al. Lineage differentiation of mesenchymal stem cells from dental pulp, apical papilla, and periodontal ligament. Methods Mol Biol 2012; 887: 111–121. [DOI] [PubMed] [Google Scholar]
- Bao LY, Jin Y, Shi JN et al. [Tissue engineering of dentin-pulp complex-like structures by human dental mesenchymal cells]. Zhonghua Kou Qiang Yi Xue Za Zhi 2005; 40: 408–411. [PubMed] [Google Scholar]
- Moshaverinia A, Chen C, Xu X et al. Bone regeneration potential of stem cells derived from periodontal ligament or gingival tissue sources encapsulated in RGD-modified alginate scaffold. Tissue Eng Part A 2014; 20: 611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Walboomers XF, van Osch GJ et al. Hard tissue formation in a porous HA/TCP ceramic scaffold loaded with stromal cells derived from dental pulp and bone marrow. Tissue Eng Part A 2008; 14: 285–294. [DOI] [PubMed] [Google Scholar]
- Yang JW, Zhang YF, Sun ZY et al. Dental pulp tissue engineering with bFGF-incorporated silk fibroin scaffolds. J Biomater Appl 2015; 30: 221–229. [DOI] [PubMed] [Google Scholar]
- Giuliani A, Manescu A, Langer M et al. Three years after transplants in human mandibles, histological and in-line holotomography revealed that stem cells regenerated a compact rather than a spongy bone: biological and clinical implications. Stem Cells Transl Med 2013; 2: 316–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimond L. Blood Platelets in the Treatment of Disease. Br Med J 1914; 2: 828–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R, Glomset J, Kariya B et al. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci USA 1974; 71: 1207–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte LD, Kaplan KL, Nossel HL et al. Studies of the release from human platelets of the growth factor for cultured human arterial smooth muscle cells. Circ Res 1978; 42: 402–409. [DOI] [PubMed] [Google Scholar]
- Kaplan DR, Chao FC, Stiles CD et al. Platelet alpha granules contain a growth factor for fibroblasts. Blood 1979; 53: 1043–1052. [PubMed] [Google Scholar]
- Assoian RK, Komoriya A, Meyers CA et al. Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J Biol Chem 1983; 258: 7155–7160. [PubMed] [Google Scholar]
- Karey KP, Sirbasku DA. Human platelet-derived mitogens. II. Subcellular localization of insulinlike growth factor I to the alpha-granule and release in response to thrombin. Blood 1989; 74: 1093–1100. [PubMed] [Google Scholar]
- Banks RE, Forbes MA, Kinsey SE et al. Release of the angiogenic cytokine vascular endothelial growth factor (VEGF) from platelets: significance for VEGF measurements and cancer biology. Br J Cancer 1998; 77: 956–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari M, Zia S, Valbonesi M et al. A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Organs 1987; 10: 47–50. [PubMed] [Google Scholar]
- Gibble JW, Ness PM. Fibrin glue: the perfect operative sealant? Transfusion 1990; 30: 741–747. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Zeng B, Zhang C et al. [Effects of platelet-rich plasma on proliferation and osteogenetic activity of marrow mesenchymal stem cells in vitro]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2005; 19: 109–113. [PubMed] [Google Scholar]
- Yamada Y, Hata K, Ueda M. [Injectable bone]. Clin Calcium 2002; 12: 228–232. [PubMed] [Google Scholar]
- Elder BD, Holmes C, Goodwin CR et al. A systematic assessment of the use of platelet-rich plasma in spinal fusion. Ann Biomed Eng 2015; 43: 1057–1070. [DOI] [PubMed] [Google Scholar]
- Rodriguez IA, Growney Kalaf EA, Bowlin GL et al. Platelet-rich plasma in bone regeneration: engineering the delivery for improved clinical efficacy. Biomed Res Int 2014; 2014: 392398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zellner J, Taeger CD, Schaffer M et al. Are applied growth factors able to mimic the positive effects of mesenchymal stem cells on the regeneration of meniscus in the avascular zone? Biomed Res Int 2014; 2014: 537686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida K, Sumita Y, Marukawa E et al. Effect of platelet-rich plasma on bone engineering with an alloplastic substitute containing BMP2. Biomed Mater Eng 2013; 23: 163–172. [DOI] [PubMed] [Google Scholar]
- Huang S, Wang Z. Platelet-rich plasma-derived growth factors promote osteogenic differentiation of rat muscle satellite cells: in vitro and in vivo studies. Cell Biol Int 2012; 36: 1195–1205. [DOI] [PubMed] [Google Scholar]
- Evans CH. Advances in regenerative orthopedics. Mayo Clin Proc 2013; 88: 1323–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Backly RM, Zaky SH, Muraglia A et al. A platelet-rich plasma-based membrane as a periosteal substitute with enhanced osteogenic and angiogenic properties: a new concept for bone repair. Tissue Eng Part A 2013; 19: 152–165. [DOI] [PubMed] [Google Scholar]
- Chatterjea A, Yuan H, Fennema E et al. Engineering new bone via a minimally invasive route using human bone marrow-derived stromal cell aggregates, microceramic particles, and human platelet-rich plasma gel. Tissue Eng Part A 2013; 19: 340–349. [DOI] [PubMed] [Google Scholar]
- Dong Z, Li B, Liu B et al. Platelet-rich plasma promotes angiogenesis of prefabricated vascularized bone graft. J Oral Maxillofac Surg 2012; 70: 2191–2197. [DOI] [PubMed] [Google Scholar]
- Lei H, Xiao R, Tang XJ et al. Evaluation of the efficacy of platelet-rich plasma in delivering BMSCs into 3D porous scaffolds. J Biomed Mater Res B Appl Biomater 2009; 91: 679–691. [DOI] [PubMed] [Google Scholar]
- Yokote K, Mori S. [Platelet derived growth factor (PDGF)]. Nihon Rinsho 2005; 63 Suppl 8: 103–106. [PubMed] [Google Scholar]
- Lawrence DA. Transforming growth factor-beta: a general review. Eur Cytokine Netw 1996; 7: 363–374. [PubMed] [Google Scholar]
- Jacobs CI. A review of the role of insulin-like growth factor 2 in malignancy and its potential as a modifier of radiation sensitivity. Clin Oncol (R Coll Radiol) 2008; 20: 345–352. [DOI] [PubMed] [Google Scholar]
- Przybylski M. A review of the current research on the role of bFGF and VEGF in angiogenesis. J Wound Care 2009; 18: 516–519. [DOI] [PubMed] [Google Scholar]
- Herbst RS. Review of epidermal growth factor receptor biology. Int J Radiat Oncol Biol Phys 2004; 59: 21–26. [DOI] [PubMed] [Google Scholar]
- Fei Y, Gronowicz G, Hurley MM. Fibroblast growth factor-2, bone homeostasis and fracture repair. Curr Pharm Des 2013; 19: 3354–3363. [DOI] [PubMed] [Google Scholar]
- Rubin JS, Bottaro DP, Chedid M et al. Keratinocyte growth factor. Cell Biol Int 1995; 19: 399–411. [DOI] [PubMed] [Google Scholar]
- Leask A, Abraham DJ. The role of connective tissue growth factor, a multifunctional matricellular protein, in fibroblast biology. Biochem Cell Biol 2003; 81: 355–363. [DOI] [PubMed] [Google Scholar]
- Hebert CA, Baker JB. Interleukin-8: a review. Cancer Invest 1993; 11: 743–750. [DOI] [PubMed] [Google Scholar]
- Mussano F, Genova T, Munaron L et al. Cytokine, chemokine, and growth factor profile of platelet-rich plasma. Platelets 2016; 27: 467–471. [DOI] [PubMed] [Google Scholar]
- Lavrova LA, Iakunin GA, Smolianitskii A. [Platelet factor 4. Properties and clinical significance of its determination (review of the literature)]. Lab Delo 1986; 2: 73–76. [PubMed] [Google Scholar]
- Casati L, Celotti F, Negri-Cesi P et al. Platelet derived growth factor (PDGF) contained in Platelet Rich Plasma (PRP) stimulates migration of osteoblasts by reorganizing actin cytoskeleton. Cell Adh Migr 2014; 8: 595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colciago A, Celotti F, Casati L et al. In Vitro Effects of PDGF Isoforms (AA, BB, AB and CC) on Migration and Proliferation of SaOS-2 Osteoblasts and on Migration of Human Osteoblasts. Int J Biomed Sci 2009; 5: 380–389. [PMC free article] [PubMed] [Google Scholar]
- Cenni E, Ciapetti G, Granchi D et al. Endothelial cells incubated with platelet-rich plasma express PDGF-B and ICAM-1 and induce bone marrow stromal cell migration. J Orthop Res 2009; 27: 1493–1498. [DOI] [PubMed] [Google Scholar]
- Hock JM, Canalis E. Platelet-derived growth factor enhances bone cell replication, but not differentiated function of osteoblasts. Endocrinology 1994; 134: 1423–1428. [DOI] [PubMed] [Google Scholar]
- Canalis E. Effect of platelet-derived growth factor on DNA and protein synthesis in cultured rat calvaria. Metabolism 1981; 30: 970–975. [DOI] [PubMed] [Google Scholar]
- Servold SA. Growth factor impact on wound healing. Clin Podiatr Med Surg 1991; 8: 937–953. [PubMed] [Google Scholar]
- Canalis E, Varghese S, McCarthy TL et al. Role of platelet derived growth factor in bone cell function. Growth Regul 1992; 2: 151–155. [PubMed] [Google Scholar]
- Wrana JL. TGF-beta receptors and signalling mechanisms. Miner Electrolyte Metab 1998; 24: 120–130. [DOI] [PubMed] [Google Scholar]
- Miyazono K. TGF-beta signaling by Smad proteins. Cytokine Growth Factor Rev 2000; 11: 15–22. [DOI] [PubMed] [Google Scholar]
- Rahman MS, Akhtar N, Jamil HM et al. TGF-beta/BMP signaling and other molecular events: regulation of osteoblastogenesis and bone formation. Bone Res 2015; 3: 15005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J, Li S, Chen D. TGF-beta signaling and the development of osteoarthritis. Bone Res 2014; 2: 14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane JL, Cao X. Bone marrow mesenchymal stem cells and TGF-beta signaling in bone remodeling. J Clin Invest 2014; 124: 466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy TL, Centrella M. Regulation of IGF activity in bone. Adv Exp Med Biol 1993; 343: 407–414. [DOI] [PubMed] [Google Scholar]
- McCarthy TL, Centrella M, Canalis E. Insulin-like growth factor (IGF) and bone. Connect Tissue Res 1989; 20: 277–282. [DOI] [PubMed] [Google Scholar]
- Minuto F, Palermo C, Arvigo M et al. The IGF system and bone. J Endocrinol Invest 2005; 28: 8–10. [PubMed] [Google Scholar]
- Ueland T. GH/IGF-I and bone resorption in vivo and in vitro. Eur J Endocrinol 2005; 152: 327–332. [DOI] [PubMed] [Google Scholar]
- Bikle DD, Tahimic C, Chang W et al. Role of IGF-I signaling in muscle bone interactions. Bone 2015; 80: 79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus R. Skeletal effects of growth hormone and IGF-I in adults. Endocrine 1997; 7: 53–55. [DOI] [PubMed] [Google Scholar]
- Mehta V. Platelet-rich plasma: a review of the science and possible clinical applications. Orthopedics 2010; 33: 111. [DOI] [PubMed] [Google Scholar]
- Arora NS, Ramanayake T, Ren YF et al. Platelet-rich plasma: a literature review. Implant Dent 2009; 18: 303–310. [DOI] [PubMed] [Google Scholar]
- Arora NS, Ramanayake T, Ren YF et al. Platelet-rich plasma in sinus augmentation procedures: a systematic literature review: Part II. Implant Dent 2010; 19: 145–157. [DOI] [PubMed] [Google Scholar]
- Everts PA, Knape JT, Weibrich G et al. Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol 2006; 38: 174–187. [PMC free article] [PubMed] [Google Scholar]
- Denfors I, Jacobsson S, Kutti J et al. The effect of centrifugation time and gravitational force on platelet yield and platelet volume distribution in platelet-rich plasma (PRP) obtained by differential centrifugation. Thromb Res 1991; 61: 463–468. [DOI] [PubMed] [Google Scholar]
- do Amaral RJ, da Silva NP, Haddad NF et al. Platelet-rich plasma obtained with different anticoagulants and their effect on platelet numbers and mesenchymal stromal cells behavior in vitro. Stem Cells Int 2016; 2016: 7414036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao F, Wang JX, Han Y. [Research advance on application of platelet-rich plasma in wound repair -- review]. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2009; 17: 840–843. [PubMed] [Google Scholar]
- Grageda E. Platelet-rich plasma and bone graft materials: a review and a standardized research protocol. Implant Dent 2004; 13: 301–309. [DOI] [PubMed] [Google Scholar]
- Griffin XL, Smith CM, Costa ML. The clinical use of platelet-rich plasma in the promotion of bone healing: a systematic review. Injury 2009; 40: 158–162. [DOI] [PubMed] [Google Scholar]
- Roh YH, Kim W, Park KU et al. Cytokine-release kinetics of platelet-rich plasma according to various activation protocols. Bone Joint Res 2016; 5: 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Textor JA, Tablin F. Activation of equine platelet-rich plasma: comparison of methods and characterization of equine autologous thrombin. Vet Surg 2012; 41: 784–794. [DOI] [PubMed] [Google Scholar]
- Yin W, Qi X, Zhang Y et al. Advantages of pure platelet-rich plasma compared with leukocyte- and platelet-rich plasma in promoting repair of bone defects. J Transl Med 2016; 14: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao HT, Marra KG, Rubin JP. Application of platelet-rich plasma and platelet-rich fibrin in fat grafting: basic science and literature review. Tissue Eng Part B Rev 2014; 20: 267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues SV, Acharya AB, Thakur SL. Platelet-rich plasma. A review. N Y State Dent J 2012; 78: 26–30. [PubMed] [Google Scholar]
- Alsousou J, Thompson M, Hulley P et al. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br 2009; 91: 987–996. [DOI] [PubMed] [Google Scholar]
- Nikolidakis D, Jansen JA. The biology of platelet-rich plasma and its application in oral surgery: literature review. Tissue Eng Part B Rev 2008; 14: 249–258. [DOI] [PubMed] [Google Scholar]
- Nikolidakis D, Meijer GJ, Jansen JA. Sinus floor elevation using platelet-rich plasma and beta-tricalcium phosphate: case report and histological evaluation. Dent Today 2008; 27: 66, 68, 70; quiz 71. [PubMed] [Google Scholar]
- Nikolidakis D, van den Dolder J, Wolke JG et al. The effect of platelet-rich plasma on the bone healing around calcium phosphate-coated and non-coated oral implants in trabecular bone. Tissue Eng 2006; 12: 2555–2563. [DOI] [PubMed] [Google Scholar]
- Yun JH, Han SH, Choi SH et al. Effects of bone marrow-derived mesenchymal stem cells and platelet-rich plasma on bone regeneration for osseointegration of dental implants: preliminary study in canine three-wall intrabony defects. J Biomed Mater Res Part B Appl Biomater 2014; 102: 1021–1030. [DOI] [PubMed] [Google Scholar]
- Chang SH, Hsu YM, Wang YJ et al. Fabrication of pre-determined shape of bone segment with collagen-hydroxyapatite scaffold and autogenous platelet-rich plasma. J Mater Sci Mater Med 2009; 20: 23–31. [DOI] [PubMed] [Google Scholar]
- Han B, Woodell-May J, Ponticiello M et al. The effect of thrombin activation of platelet-rich plasma on demineralized bone matrix osteoinductivity. J Bone Joint Surg Am 2009; 91: 1459–1470. [DOI] [PubMed] [Google Scholar]
- Kütük N, Baş B, Soylu E et al. Effect of platelet-rich plasma on fibrocartilage, cartilage, and bone repair in temporomandibular joint. J Oral Maxillofac Surg 2014; 72: 277–284. [DOI] [PubMed] [Google Scholar]
- Scala M, Mereu P, Spagnolo F et al. The use of platelet-rich plasma gel in patients with mixed tumour undergoing superficial parotidectomy: a randomized study. In Vivo 2014; 28: 121–124. [PubMed] [Google Scholar]
- Scala M, Gipponi M, Mereu P et al. Regeneration of mandibular osteoradionecrosis defect with platelet rich plasma gel. In Vivo 2010; 24: 889–893. [PubMed] [Google Scholar]
- Rupreht M, Vogrin M, Hussein M. MRI evaluation of tibial tunnel wall cortical bone formation after platelet-rich plasma applied during anterior cruciate ligament reconstruction. Radiol Oncol 2013; 47: 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupreht M, Jevtič V, Serša I et al. Evaluation of the tibial tunnel after intraoperatively administered platelet-rich plasma gel during anterior cruciate ligament reconstruction using diffusion weighted and dynamic contrast-enhanced MRI. J Magn Reson Imaging 2013; 37: 928–935. [DOI] [PubMed] [Google Scholar]
- Galasso O, Mariconda M, Romano G et al. Expandable intramedullary nailing and platelet rich plasma to treat long bone non-unions. J Orthop Traumatol 2008; 9: 129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smrke D, Gubina B, Domanovic D et al. Allogeneic platelet gel with autologous cancellous bone graft for the treatment of a large bone defect. Eur Surg Res 2007; 39: 170–174. [DOI] [PubMed] [Google Scholar]
- Kanthan SR, Kavitha G, Addi S et al. Platelet-rich plasma (PRP) enhances bone healing in non-united critical-sized defects: a preliminary study involving rabbit models. Injury 2011; 42: 782–789. [DOI] [PubMed] [Google Scholar]
- Lin SS, Landesberg R, Chin HS et al. Controlled release of PRP-derived growth factors promotes osteogenic differentiation of human mesenchymal stem cells. Conf Proc IEEE Eng Med Biol Soc 2006; 1: 4358–4361. [DOI] [PubMed] [Google Scholar]
- Lu HH, Vo JM, Chin HS et al. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. J Biomed Mater Res A 2008; 86: 1128–1136. [DOI] [PubMed] [Google Scholar]
- Huang S, Jia S, Liu G et al. Osteogenic differentiation of muscle satellite cells induced by platelet-rich plasma encapsulated in three-dimensional alginate scaffold. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114: S32–S40. [DOI] [PubMed] [Google Scholar]
- Hokugo A, Sawada Y, Hokugo R et al. Controlled release of platelet growth factors enhances bone regeneration at rabbit calvaria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 44–48. [DOI] [PubMed] [Google Scholar]
- Hokugo A, Ozeki M, Kawakami O et al. Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. Tissue Eng 2005; 11: 1224–1233. [DOI] [PubMed] [Google Scholar]
- Kim ES, Kim JJ, Park EJ. Angiogenic factor-enriched platelet-rich plasma enhances in vivo bone formation around alloplastic graft material. J Adv Prosthodont 2010; 2: 7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltfang J, Kloss FR, Kessler P et al. Effects of platelet-rich plasma on bone healing in combination with autogenous bone and bone substitutes in critical-size defects. An animal experiment. Clin Oral Implants Res 2004; 15: 187–193. [DOI] [PubMed] [Google Scholar]
- Taschieri S, Corbella S, Weinstein R et al. Maxillary sinus floor elevation using platelet-rich plasma combined with either biphasic calcium phosphate or deproteinized bovine bone. J Craniofac Surg 2016; 27: 702–707. [DOI] [PubMed] [Google Scholar]
- Berner A, Boerckel JD, Saifzadeh S et al. Biomimetic tubular nanofiber mesh and platelet rich plasma-mediated delivery of BMP-7 for large bone defect regeneration. Cell Tissue Res 2012; 347: 603–612. [DOI] [PubMed] [Google Scholar]
- Dutra CE, Pereira MM, Serakides R et al. In vivo evaluation of bioactive glass foams associated with platelet-rich plasma in bone defects. J Tissue Eng Regen Med 2008; 2: 221–227. [DOI] [PubMed] [Google Scholar]
- Wang SZ, Jin JY, Guo YD et al. Intervertebral disc regeneration using plateletrich plasmacontaining bone marrowderived mesenchymal stem cells: A preliminary investigation. Mol Med Rep 2016; 13: 3475–3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosselot G, Martínez J, Pablo Rodríguez J. [Cellular basis of bone tissue development]. Rev Med Chil 1996; 124: 15–20. [PubMed] [Google Scholar]
- Bruder SP, Caplan AI. Cellular and molecular events during embryonic bone development. Connect Tissue Res 1989; 20: 65–71. [DOI] [PubMed] [Google Scholar]
- Hall BK. Cellular interactions during cartilage and bone development. J Craniofac Genet Dev Biol 1991; 11: 238–250. [PubMed] [Google Scholar]
- Kale S, Biermann S, Edwards C et al. Three-dimensional cellular development is essential for ex vivo formation of human bone. Nat Biotechnol 2000; 18: 954–958. [DOI] [PubMed] [Google Scholar]
- Mistura DV, Messias AD, Duek EA et al. Development, characterization, and cellular adhesion of poly(L-lactic acid)/poly(caprolactone triol) membranes for potential application in bone tissue regeneration. Artif Organs 2013; 37: 978–984. [DOI] [PubMed] [Google Scholar]
- Rameis MT, Cei S, Bernardi J et al. Development of an in vitro model on cellular adhesion on granular natural bone mineral under dynamic seeding conditions--a pilot study. J Biomed Mater Res B Appl Biomater 2009; 91: 766–771. [DOI] [PubMed] [Google Scholar]
- Pneumaticos SG, Triantafyllopoulos GK, Basdra EK et al. Segmental bone defects: from cellular and molecular pathways to the development of novel biological treatments. J Cell Mol Med 2010; 14: 2561–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenk RK, Willenegger HR. [Histology of primary bone healing: modifications and limits of recovery of gaps in relation to extent of the defect (author's transl)]. Unfallheilkunde 1977; 80: 155–160. [PubMed] [Google Scholar]
- Church LE. Histology of bone and healing of fractures. J Oral Surg Anesth Hosp Dent Serv 1963; 21: 337–344. [PubMed] [Google Scholar]
- Schenk RK. [Histology of primary bone healing]. Fortschr Kiefer Gesichtschir 1975; 19: 8–12. [PubMed] [Google Scholar]
- Mann M, Quitta P, Drápela J et al. [Recent views of bone fracture healing with respect to age and fixation in rats. Mechanical tests, histology and electron microscopy (author's transl)]. Cas Lek Cesk 1981; 120: 561–566. [PubMed] [Google Scholar]
- Sakata R, Reddi AH. Platelet-rich plasma modulates actions on articular cartilage lubrication and regeneration. Tissue Eng Part B Rev 2016; 22: 408–419. [DOI] [PubMed] [Google Scholar]
- Martinez-Zapata MJ, Marti-Carvajal A, Sola I et al. Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration: a systematic review. Transfusion 2009; 49: 44–56. [DOI] [PubMed] [Google Scholar]
- Plachokova AS, Nikolidakis D, Mulder J et al. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res 2008; 19: 539–545. [DOI] [PubMed] [Google Scholar]
- Sampson S, Gerhardt M, Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med 2008; 1: 165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roubelakis MG, Trohatou O, Roubelakis A et al. Platelet-rich plasma (PRP) promotes fetal mesenchymal stem/stromal cell migration and wound healing process. Stem Cell Rev 2014; 10: 417–428. [DOI] [PubMed] [Google Scholar]
- Mishra A, Tummala P, King A et al. Buffered platelet-rich plasma enhances mesenchymal stem cell proliferation and chondrogenic differentiation. Tissue Eng Part C Methods 2009; 15: 431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X, Zhang C, Tuan RS. Biology of platelet-rich plasma and its clinical application in cartilage repair. Arthritis Res Ther 2014; 16: 204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Azpeitia E, Andia I. Partnership between platelet-rich plasma and mesenchymal stem cells: in vitro experience. Muscles Ligaments Tendons J 2014; 4: 52–62. [PMC free article] [PubMed] [Google Scholar]
- Zou J, Yuan C, Wu C et al. The effects of platelet-rich plasma on the osteogenic induction of bone marrow mesenchymal stem cells. Connect Tissue Res 2014; 55: 304–309. [DOI] [PubMed] [Google Scholar]
- Fernandes G, Wang C, Yuan X et al. Combination of controlled release platelet-rich plasma alginate beads and bone morphogenetic protein-2 genetically modified mesenchymal stem cells for bone regeneration. J Periodontol 2016; 87: 470–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang HC, Chen WC, Chiang CW et al. Differentiation effects of platelet-rich plasma concentrations on synovial fluid mesenchymal stem cells from pigs cultivated in alginate complex hydrogel. Int J Mol Sci 2015; 16: 18507–18521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza TF, Sakamoto SS, Ferreira GT et al. Osteogenic potential of mesenchymal cells derived from canine umbilical cord matrix co-cultured with platelet-rich plasma and demineralized bone matrix. J Vet Sci 2015; 16: 381–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busilacchi A, Gigante A, Mattioli-Belmonte M et al. Chitosan stabilizes platelet growth factors and modulates stem cell differentiation toward tissue regeneration. Carbohydr Polym 2013; 98: 665–676. [DOI] [PubMed] [Google Scholar]
- Zhao SN, Liu WF, Zhang ZT. [Effect of platelet-rich plasma on cell proliferation and osteogenic activity of pulp stem cells]. Zhonghua Kou Qiang Yi Xue Za Zhi 2013; 48: 177–182. [PubMed] [Google Scholar]
- Lee UL, Jeon SH, Park JY et al. Effect of platelet-rich plasma on dental stem cells derived from human impacted third molars. Regen Med 2011; 6: 67–79. [DOI] [PubMed] [Google Scholar]
- Li H, Liu D, Yu Y et al. [Experimental research of the promotion effect of autogeneic PRP on osteogenic differentiation of human adipose-derived stem cells in vitro]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2009; 23: 732–736. [PubMed] [Google Scholar]
- Kasten P, Vogel J, Beyen I et al. Effect of platelet-rich plasma on the in vitro proliferation and osteogenic differentiation of human mesenchymal stem cells on distinct calcium phosphate scaffolds: the specific surface area makes a difference. J Biomater Appl 2008; 23: 169–188. [DOI] [PubMed] [Google Scholar]
- Murphy MB, Blashki D, Buchanan RM et al. Adult and umbilical cord blood-derived platelet-rich plasma for mesenchymal stem cell proliferation, chemotaxis, and cryo-preservation. Biomaterials 2012; 33: 5308–5316. [DOI] [PubMed] [Google Scholar]
- Kocaoemer A, Kern S, Kluter H et al. Human AB serum and thrombin-activated platelet-rich plasma are suitable alternatives to fetal calf serum for the expansion of mesenchymal stem cells from adipose tissue. Stem Cells 2007; 25: 1270–1278. [DOI] [PubMed] [Google Scholar]
- Duan J, Kuang W, Tan J et al. Differential effects of platelet rich plasma and washed platelets on the proliferation of mouse MSC cells. Mol Biol Rep 2011; 38: 2485–2490. [DOI] [PubMed] [Google Scholar]
- Mifune Y, Matsumoto T, Takayama K et al. The effect of platelet-rich plasma on the regenerative therapy of muscle derived stem cells for articular cartilage repair. Osteoarthritis Cartilage 2013; 21: 175–185. [DOI] [PubMed] [Google Scholar]
- Drengk A, Zapf A, Sturmer EK et al. Influence of platelet-rich plasma on chondrogenic differentiation and proliferation of chondrocytes and mesenchymal stem cells. Cells Tissues Organs 2009; 189: 317–326. [DOI] [PubMed] [Google Scholar]
- Scioli MG, Bielli A, Gentile P et al. Combined treatment with platelet-rich plasma and insulin favours chondrogenic and osteogenic differentiation of human adipose-derived stem cells in three-dimensional collagen scaffolds. J Tissue Eng Regen Med 2016; doi: 10.1002/term.2139. [Epub ahead of print]. [DOI] [PubMed]
- Yamada Y, Ueda M, Naiki T et al. Autogenous injectable bone for regeneration with mesenchymal stem cells and platelet-rich plasma: tissue-engineered bone regeneration. Tissue Eng 2004; 10: 955–964. [DOI] [PubMed] [Google Scholar]
- Vogel JP, Szalay K, Geiger F et al. Platelet-rich plasma improves expansion of human mesenchymal stem cells and retains differentiation capacity and in vivo bone formation in calcium phosphate ceramics. Platelets 2006; 17: 462–469. [DOI] [PubMed] [Google Scholar]
- Dohan Ehrenfest DM, Doglioli P, de Peppo GM et al. Choukroun's platelet-rich fibrin (PRF) stimulates in vitro proliferation and differentiation of human oral bone mesenchymal stem cell in a dose-dependent way. Arch Oral Biol 2010; 55: 185–194. [DOI] [PubMed] [Google Scholar]
- Gobbi A, Fishman M. Platelet-rich plasma and bone marrow-derived mesenchymal stem cells in sports medicine. Sports Med Arthrosc 2016; 24: 69–73. [DOI] [PubMed] [Google Scholar]
- Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am 1993; 75: 532–553. [DOI] [PubMed] [Google Scholar]
- Kruger JP, Hondke S, Endres M et al. Human platelet-rich plasma stimulates migration and chondrogenic differentiation of human subchondral progenitor cells. J Orthop Res 2012; 30: 845–852. [DOI] [PubMed] [Google Scholar]
- Hu ZM, Peel SA, Ho SK et al. Comparison of platelet-rich plasma, bovine BMP, and rhBMP-4 on bone matrix protein expression in vitro. Growth Factors 2009; 27: 280–288. [DOI] [PubMed] [Google Scholar]
- Chen JC, Ko CL, Shih CJ et al. Calcium phosphate bone cement with 10 wt% platelet-rich plasma in vitro and in vivo. J Dent 2012; 40: 114–122. [DOI] [PubMed] [Google Scholar]
- Jiang ZQ, Liu HY, Zhang LP et al. Repair of calvarial defects in rabbits with platelet-rich plasma as the scaffold for carrying bone marrow stromal cells. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 327–333. [DOI] [PubMed] [Google Scholar]
- Kreuz PC, Krüger JP, Metzlaff S et al. Platelet-rich plasma preparation types show impact on chondrogenic differentiation, migration, and proliferation of human subchondral mesenchymal progenitor cells. Arthroscopy 2015; 31: 1951–1961. [DOI] [PubMed] [Google Scholar]
- Muraglia A, Ottonello C, Spanò R et al. Biological activity of a standardized freeze-dried platelet derivative to be used as cell culture medium supplement. Platelets 2014; 25: 211–220. [DOI] [PubMed] [Google Scholar]
- Friedenstein AJ. Stromal mechanisms of bone marrow: cloning in vitro and retransplantation in vivo. Haematol Blood Transfus 1980; 25: 19–29. [DOI] [PubMed] [Google Scholar]
- Wright NA. Stem cell identification--in vivo lineage analysis versus in vitro isolation and clonal expansion. J Pathol 2012; 227: 255–266. [DOI] [PubMed] [Google Scholar]
- Janicki P, Boeuf S, Steck E et al. Prediction of in vivo bone forming potency of bone marrow-derived human mesenchymal stem cells. Eur Cell Mater 2011; 21: 488–507. [DOI] [PubMed] [Google Scholar]
- Cheng W, Jin D, Zhao Y. [Effect of platelet-rich plasma on proliferation and osteogenic differentiation of bone marrow stem cells in China goats]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2007; 21: 386–389. [PubMed] [Google Scholar]
- Castro FO, Torres A, Cabezas J et al. Combined use of platelet rich plasma and vitamin C positively affects differentiation in vitro to mesodermal lineage of adult adipose equine mesenchymal stem cells. Res Vet Sci 2014; 96: 95–101. [DOI] [PubMed] [Google Scholar]
- Qi Y, Niu L, Zhao T et al. Combining mesenchymal stem cell sheets with platelet-rich plasma gel/calcium phosphate particles: a novel strategy to promote bone regeneration. Stem Cell Res Ther 2015; 6: 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo JP, Kambayashi Y, Itho M et al. Effects of a synovial flap and gelatin/beta-tricalcium phosphate sponges loaded with mesenchymal stem cells, bone morphogenetic protein-2, and platelet rich plasma on equine osteochondral defects. Res Vet Sci 2015; 101: 140–143. [DOI] [PubMed] [Google Scholar]
- Cvetković VJ, Najdanović JG, Vukelić-Nikolić MĐ et al. Osteogenic potential of in vitro osteo-induced adipose-derived mesenchymal stem cells combined with platelet-rich plasma in an ectopic model. Int Orthop 2015; 39: 2173–2180. [DOI] [PubMed] [Google Scholar]
- Tajima S, Tobita M, Orbay H et al. Direct and indirect effects of a combination of adipose-derived stem cells and platelet-rich plasma on bone regeneration. Tissue Eng Part A 2015; 21: 895–905. [DOI] [PubMed] [Google Scholar]
- Xu Q, Li B, Yuan L et al. Combination of platelet-rich plasma within periodontal ligament stem cell sheets enhances cell differentiation and matrix production. J Tissue Eng Regen Med 2014; doi: 10.1002/term.1953. [Epub ahead of print]. [DOI] [PubMed]
- Ng MH, Duski S, Tan KK et al. Repair of segmental load-bearing bone defect by autologous mesenchymal stem cells and plasma-derived fibrin impregnated ceramic block results in early recovery of limb function. Biomed Res Int 2014; 2014: 345910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Y, Gu W, Cui J et al. Platelet-rich plasma enhanced umbilical cord mesenchymal stem cells-based bone tissue regeneration. Arch Oral Biol 2014; 59: 1146–1154. [DOI] [PubMed] [Google Scholar]
- Man Y, Wang P, Guo Y et al. Angiogenic and osteogenic potential of platelet-rich plasma and adipose-derived stem cell laden alginate microspheres. Biomaterials 2012; 33: 8802–8811. [DOI] [PubMed] [Google Scholar]
- Monteiro BS, Del Carlo RJ, Argôlo-Neto NM et al. Association of mesenchymal stem cells with platelet rich plasma on the repair of critical calvarial defects in mice. Acta Cir Bras 2012; 27: 201–209. [DOI] [PubMed] [Google Scholar]
- Ito K, Yamada Y, Nakamura S et al. Osteogenic potential of effective bone engineering using dental pulp stem cells, bone marrow stem cells, and periosteal cells for osseointegration of dental implants. Int J Oral Maxillofac Implants 2011; 26: 947–954. [PubMed] [Google Scholar]
- Liu X, Cao L, Jiang Y et al. [Repair of radial segmental bone defects by combined angiopoietin 1 gene transfected bone marrow mesenchymal stem cells and platelet-rich plasma tissue engineered bone in rabbits]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2011; 25: 1115–1119. [PubMed] [Google Scholar]
- Kohgo T, Yamada Y, Ito K et al. Bone regeneration with self-assembling peptide nanofiber scaffolds in tissue engineering for osseointegration of dental implants. Int J Periodontics Restorative Dent 2011; 31: e9–e16. [PubMed] [Google Scholar]
- Yamada Y, Ito K, Nakamura S et al. Promising cell-based therapy for bone regeneration using stem cells from deciduous teeth, dental pulp, and bone marrow. Cell Transplant 2011; 20: 1003–1013. [DOI] [PubMed] [Google Scholar]
- Kang J, Hur J, Kang JA et al. Activated platelet supernatant can augment the angiogenic potential of human peripheral blood stem cells mobilized from bone marrow by G-CSF. J Mol Cell Cardiol 2014; 75: 64–75. [DOI] [PubMed] [Google Scholar]
- Yoshimi R, Yamada Y, Ito K et al. Self-assembling peptide nanofiber scaffolds, platelet-rich plasma, and mesenchymal stem cells for injectable bone regeneration with tissue engineering. J Craniofac Surg 2009; 20: 1523–1530. [DOI] [PubMed] [Google Scholar]
- Pieri F, Lucarelli E, Corinaldesi G et al. Effect of mesenchymal stem cells and platelet-rich plasma on the healing of standardized bone defects in the alveolar ridge: a comparative histomorphometric study in minipigs. J Oral Maxillofac Surg 2009; 67: 265–272. [DOI] [PubMed] [Google Scholar]
- Ito K, Yamada Y, Naiki T et al. Simultaneous implant placement and bone regeneration around dental implants using tissue-engineered bone with fibrin glue, mesenchymal stem cells and platelet-rich plasma. Clin Oral Implants Res 2006; 17: 579–586. [DOI] [PubMed] [Google Scholar]
- Xie X, Wang Y, Zhao C et al. Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regeneration. Biomaterials 2012; 33: 7008–7018. [DOI] [PubMed] [Google Scholar]
- Ricco S, Renzi S, Del Bue M et al. Allogeneic adipose tissue-derived mesenchymal stem cells in combination with platelet rich plasma are safe and effective in the therapy of superficial digital flexor tendonitis in the horse. Int J Immunopathol Pharmacol 2013; 26: 61–68. [DOI] [PubMed] [Google Scholar]
- Betsch M, Schneppendahl J, Thuns S et al. Bone marrow aspiration concentrate and platelet rich plasma for osteochondral repair in a porcine osteochondral defect model. PLoS One 2013; 8: e71602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JC, Min HJ, Park HJ et al. Synovial membrane-derived mesenchymal stem cells supported by platelet-rich plasma can repair osteochondral defects in a rabbit model. Arthroscopy 2013; 29: 1034–1046. [DOI] [PubMed] [Google Scholar]
- Renzi S, Riccò S, Dotti S et al. Autologous bone marrow mesenchymal stromal cells for regeneration of injured equine ligaments and tendons: a clinical report. Res Vet Sci 2013; 95: 272–277. [DOI] [PubMed] [Google Scholar]
- Zhang ZY, Huang AW, Fan JJ et al. The potential use of allogeneic platelet-rich plasma for large bone defect treatment: immunogenicity and defect healing efficacy. Cell Transplant 2013; 22: 175–187. [DOI] [PubMed] [Google Scholar]
- Yuksel S, Gulec MA, Gultekin MZ et al. Comparison of the early period effects of bone marrow-derived mesenchymal stem cells and platelet-rich plasma on the Achilles tendon ruptures in rats. Connect Tissue Res 2016; 57: 360–373. [DOI] [PubMed] [Google Scholar]
- Koh YG, Choi YJ. Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee 2012; 19: 902–907. [DOI] [PubMed] [Google Scholar]
- Liebergall M, Schroeder J, Mosheiff R et al. Stem cell-based therapy for prevention of delayed fracture union: a randomized and prospective preliminary study. Mol Ther 2013; 21: 1631–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Z, Mi S, Fang G. [Clinical study on treatment of bone nonunion with MSCs derived from human umbilical cord]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2009; 23: 345–347. [PubMed] [Google Scholar]
- Ueda M, Yamada Y, Kagami H et al. Injectable bone applied for ridge augmentation and dental implant placement: human progress study. Implant Dent 2008; 17: 82–90. [DOI] [PubMed] [Google Scholar]
- Yamada Y, Nakamura S, Ueda M et al. Osteotome technique with injectable tissue-engineered bone and simultaneous implant placement by cell therapy. Clin Oral Implants Res 2013; 24: 468–474. [DOI] [PubMed] [Google Scholar]
- Yamada Y, Ueda M, Hibi H et al. A novel approach to periodontal tissue regeneration with mesenchymal stem cells and platelet-rich plasma using tissue engineering technology: a clinical case report. Int J Periodontics Restorative Dent 2006; 26: 363–369. [PubMed] [Google Scholar]
- Kanitkar M, Tailor HD, Khan WS. The use of growth factors and mesenchymal stem cells in orthopaedics. Open Orthop J 2011; 5 Suppl 2: 271–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filho Cerruti H, Kerkis I, Kerkis A et al. Allogenous bone grafts improved by bone marrow stem cells and platelet growth factors: clinical case reports. Artif Organs 2007; 31: 268–273. [DOI] [PubMed] [Google Scholar]
- Ueda M, Yamada Y, Ozawa R et al. Clinical case reports of injectable tissue-engineered bone for alveolar augmentation with simultaneous implant placement. Int J Periodontics Restorative Dent 2005; 25: 129–137. [PubMed] [Google Scholar]
- Kitoh H, Kitakoji T, Tsuchiya H et al. Distraction osteogenesis of the lower extremity in patients with achondroplasia/hypochondroplasia treated with transplantation of culture-expanded bone marrow cells and platelet-rich plasma. J Pediatr Orthop 2007; 27: 629–634. [DOI] [PubMed] [Google Scholar]
- Yu S, Wang Y, Dong Q. [Platelet-rich plasma and its applications in orthopedics field]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2008; 22: 880–883. [PubMed] [Google Scholar]
- Bianco P, Robey PG, Saggio I et al. "Mesenchymal" stem cells in human bone marrow (skeletal stem cells): a critical discussion of their nature, identity, and significance in incurable skeletal disease. Hum Gene Ther 2010; 21: 1057–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabali M, Mangano A, Lianos GD et al. Bone regeneration using mesenchymal stem cells: challenges and future perspectives in regenerative surgery. Regen Med 2015; 10: 543–547. [DOI] [PubMed] [Google Scholar]
- Jones E, Schäfer R. Where is the common ground between bone marrow mesenchymal stem/stromal cells from different donors and species? Stem Cell Res Ther 2015; 6: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhillon RS, Schwarz EM, Maloney MD. Platelet-rich plasma therapy - future or trend? Arthritis Res Ther 2012; 14: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell RP, Apostolakos J, Hirose T et al. Variability of platelet-rich plasma preparations. Sports Med Arthrosc 2013; 21: 186–190. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Yuan M, Meng HY et al. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarthritis Cartilage 2013; 21: 1627–1637. [DOI] [PubMed] [Google Scholar]
- Olivier V, Faucheux N, Hardouin P. Biomaterial challenges and approaches to stem cell use in bone reconstructive surgery. Drug Discov Today 2004; 9: 803–811. [DOI] [PubMed] [Google Scholar]
- Zhang L, Peng LP, Wu N et al. Development of bone marrow mesenchymal stem cell culture in vitro. Chinese Med J 2012; 125: 1650–1655. [PubMed] [Google Scholar]
- Sampson S, Botto-van Bemden A, Aufiero D. Stem cell therapies for treatment of cartilage and bone disorders: osteoarthritis, avascular necrosis, and non-union fractures. PM R 2015; 7: S26–S32. [DOI] [PubMed] [Google Scholar]
- Lin BN, Whu SW, Chen CH et al. Bone marrow mesenchymal stem cells, platelet-rich plasma and nanohydroxyapatite-type I collagen beads were integral parts of biomimetic bone substitutes for bone regeneration. J Tissue Eng Regen Med 2013; 7: 841–854. [DOI] [PubMed] [Google Scholar]
- Smith B, Goldstein T, Ekstein C. Biologic adjuvants and bone: current use in orthopedic surgery. Curr Rev Musculoskelet Med 2015; 8: 193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park EJ, Kim ES, Weber HP et al. Improved bone healing by angiogenic factor-enriched platelet-rich plasma and its synergistic enhancement by bone morphogenetic protein-2. Int J Oral Maxillofac Implants 2008; 23: 818–826. [PMC free article] [PubMed] [Google Scholar]