Abstract
Background
Recent works have suggested a possible link between interleukin (IL)-33 and B-cell biology. We aimed to study the possible association between serum IL-33 detection and response to rituximab (RTX) in rheumatoid arthritis (RA) patients in different cohorts with an accurate enzyme-linked immunosorbent assay (ELISA).
Methods
Serum IL-33, rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP), and high serum immunoglobulin (Ig)G levels were assessed in 111 RA patients receiving a first course of 2 g RTX (cohort 1) in an observational study and in 74 RA patients treated with the same schedule in routine care (cohort 2). Univariate and multivariate analyses identified factors associated with a European League Against Rheumatism (EULAR) response at 24 weeks.
Results
At week 24, 84/111 (76%) and 54/74 (73%) patients reached EULAR response in cohorts 1 and 2, respectively. Serum IL-33 was detectable in only 33.5% of the patients. In the combined cohorts, the presence of RF or anti-CCP (odds ratio (OR) 3.27, 95% confidence interval (CI) 1.13–9.46; p = 0.03), high serum IgG (OR 2.32, 95% CI 1.01–5.33; p = 0.048), and detectable serum IL-33 (OR 2.40, 95% CI 1.01–5.72; p = 0.047) were all associated with RTX response in multivariate analysis. The combination of these three factors increased the likelihood of response to RTX. When serum IL-33 detection was added to seropositivity and serum IgG level, 100% of the patients with the three risk factors (corresponding to 9% of the population) responded to RTX (OR versus patients with none of the three risk factors 29.61, 95% CI 1.30–674.79; p = 0.034).
Conclusion
Detectable serum IL-33 may predict clinical response to RTX independently of, and synergistically with, auto-antibodies and serum IgG level.
Trial registration
NCT01126541; 18 May 2010.
Electronic supplementary material
The online version of this article (doi:10.1186/s13075-016-1190-z) contains supplementary material, which is available to authorized users.
Keywords: Rheumatoid arthritis, Interleukin 33, Rituximab, B-cell, Personalized medicine
Background
Interleukin (IL)-33 is one of the most recently discovered members of the IL-1 cytokine family mediating its biological effects via its binding to its receptor suppression of tumorigenicity (ST)2 [1]. IL-33 is upregulated in both resident cells and inflammatory infiltrating cells and is released in case of cell injury, thus acting as an alarmin [2, 3]. IL-33 induces production of Th2 cytokines and eosinophilia, and may activate mast cells that can in turn release several pro-inflammatory cytokines [4]. IL-33 investigations have been mainly devoted to asthma and allergy, with the development of a targeted IL-33/ST2 axis therapeutic strategy [5].
IL-33 may also be involved in rheumatoid arthritis (RA) pathogenesis. IL-33 administration exacerbates collagen-induced and K/BxN serum-mediated murine arthritis, and disease severity is reduced in mice treated with sST2-Fc fusion protein or anti-IL-33 monoclonal antibody [6–8]. Extracellular IL-33 is a critical enhancer of tumor necrosis factor (TNF)-induced RA synovial fibroblast activation [9] and could activate osteoclastogenesis [10, 11]. In patients with RA, biomarker studies have suggested that the serum level of IL-33 could reflect clinical activity [12] and disease severity, or predict carotid plaque progression [13]. However, the role of IL-33 could be paradoxical since, in K/BxN serum transfer-induced arthritis, ST2 but not IL-33 blockade may improve arthritis [14, 15]. Moreover, IL-33-stimulated mast cells could also suppress monocyte activation [16] and intracellular IL-33 also has anti-osteoclastogenic and anti-inflammatory properties [11].
Some recent works have suggested a possible link between IL-33 and B-cell biology [17]. In mice, IL-33 enhances immunoglobulin (Ig)M synthesis and markedly induces and activates B1 cells in an ST2-dependent manner [18]. Additionally, IL-33 could also induce regulatory B cells to produce IL-10, attenuating mucosal inflammation in the gut [19].
Using a transcriptomic approach, we have found that increased IL-33 mRNA expression in the whole blood of patients with RA was predictive of the response to rituximab (RTX), a targeted B cell-depleting agent [20]. We aimed to investigate, using an accurate and simple enzyme-linked immunosorbent assay (ELISA), the possible association between a detectable serum level of the IL-33 protein and a response to RTX in RA patients in different cohorts.
Methods
Patients
A total of 224 patients with RA for at least 6 months and fulfilling the American College of Rheumatology (ACR) 1987 criteria were included in the SMART study (NCT01126541). This study is a 2-year, national, multicenter, randomized open-label study evaluating the efficacy and tolerability of two doses of RTX for re-treatment after one initial course of RTX at a usual dose (1000 mg on days 1 and 15) described previously [21]. All patients had active disease, defined by a Disease Activity Score in 28 joints (DAS28) using C-reactive protein (CRP) (DAS28-CRP) >3.2, with ≥6/66 swollen and ≥6/68 tender joints, or a CRP ≥10 mg/L, or an erythrocyte sedimentation rate (ESR) ≥28 mm/h. Erosive status was based on the reading of hand and feet X-rays by the investigators in each center. Each patient received a stable dose of methotrexate (MTX) (≥10 mg/week for at least 4 weeks) and had experienced an inadequate response or intolerance to TNF inhibitors, or had contraindications to TNF inhibitors. All patients in the SMART study received one course of RTX (two 1000 mg infusions, given on days 1 and 15) with usual pre-medication (methylprednisolone, acetaminophen, and antihistamine). In this ancillary study, 111 patients from the 224 were included due to the availability of the serum samples for IL-33 assessment and were designated as cohort 1.
We also studied 32 RA patients from Leeds (UK) and 42 from Clermont-Ferrand (France) treated in real life with a first course of RTX using the same schedule. In order to match the numbers of patients in cohort 1, these two groups of patients from Leeds and Clermont-Ferrand were merged and called cohort 2. There were no overlaps between the two cohorts.
For all patients, treatment efficacy was evaluated 24 weeks after the first RTX infusion according to European League Against Rheumatism (EULAR) response [22]. Patients were then classified as responders (good or moderate) or non-responders after this first course of RTX.
Assessment of serum IL-33, auto-antibodies, and serum IgG
We first used an ELISA IL-33 kit (DuoSet, R&D Systems) for protein assessment, and preliminary presented as an abstract an association between serum IL-33 level and RTX response in a single cohort [23]. However, this kit was not validated for human sera and additional experiments have confirmed the need for caution about the accuracy of this kit for sera measurements [24]. Recommendations from the manufacturer advise us to use another assay for human sera, named Quantikine and also provided by R&D Systems. We aimed to use this more accurate ELISA in order to investigate the possible association between a detectable serum level of IL-33 and a response to RTX in RA patients in the different cohorts.
Using a sample obtained prior to the initiation of RTX in the two cohorts, we measured the serum IL-33 level using the Quantikine kit, which is a solid-phase ELISA with a 6.25 pg/mL lower limit threshold according to the manufacturer’s instruction [24]. The assessment of rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, and serum IgG level were also performed. The upper limit of normal (ULN) for serum IgG was 12.7 g/L and high serum IgG level was a value above this cut-off, as described previously [25].
Statistical analysis
Continuous data are described as means and standard deviations (mean ± SD) or as medians and ranges (median (range)).
For all analyses, since serum IL-33 is not systematically detectable, we presented qualitative results as detectable serum IL-33 or undetectable serum IL-33. Among patients of the SMART cohort, we compared patients who were assessed for serum IL-33 level and those who were not due to the availability of the serum samples. Student and Wilcoxon tests were used to compare quantitative values and the Chi-squared test was used for qualitative values.
We analyzed by logistic regression the relationship between EULAR response at 24 weeks and the following four explanatory variables: 1) high disease activity defined as DAS28-CRP >5.1; 2) high serum IgG level; 3) auto-antibody status (i.e., the presence or absence of RF and/or anti-CCP antibodies), since all of them have been found previously as associated with subsequent RTX response [25, 26]; and 4) detectable serum IL-33. All these explanatory variables were entered in a stepwise multivariate model systematically adjusted on RF or anti-CCP positivy (entry level, p = 0.15; level for staying in the model, p = 0.10). Results are expressed as odds ratios (ORs) with 95% confidence intervals (CIs). A p value <0.05 was considered as significant. Statistical analysis was performed with SAS 9.4 software.
Results
Characteristics of the populations
The characteristics of patients from cohort 1 are presented in Table 1. There was no significant difference between the 111 patients that underwent IL-33 assessment and the others that participated in the main SMART trial (n = 113) who did not (Table 1). Available characteristics of patients from cohort 2 are presented in Additional file 1 (Table S1).
Table 1.
Baseline characteristics of RA patients included in the IL-33 ancillary study from the SMART trial and a comparison between the patients in the SMART cohort included in the IL-33 study (cohort 1, n = 111) and the rest of the cohort not assessed for serum IL-33 level (n = 113)
| Cohort 1 | Patients in the SMART cohort without IL-33 dosage | Whole SMART cohort | Inter-group comparison | |
|---|---|---|---|---|
| (n = 111) | (n = 113) | (n = 224) | ||
| Age (years) | 56 ± 11 | 56 ± 11 | 56 ± 11 | 0.99 |
| Female | 95 (86%) | 92 (81%) | 187 (84%) | 0.401 |
| Disease duration (years) | 11 (1–42) | 10 (0.8–45) | 11 (0.8–45) | 0.094 |
| DAS28-CRP | 5.8 ± 0.8 | 5.8 ± 0.9 | 5.8 ± 0.9 | 0.791 |
| HAQ-DI | 1.8 ± 0.6 | 1.8 ± 0.6 | 1.8 ± 0.6 | 0.753 |
| Prednisone treatment | 76 (68%) | 88 (78%) | 165 (74%) | 0.11 |
| Prednisone dosage (mg/day) | 8 (2–20) | 10 (2–15)* | 10 (2–20)* | 0.243 |
| MTX (mg/week) | 14 ± 4 | 14 ± 4 | 14 ± 4 | 0.351 |
| Previous biologic: None/mAb/Eta | 8 (7%)/66 (60%)/37(33%) | 7 (6%)/70(62%)/36(32%) | 15 (7%)/136 (61%)/73(33%) | 0.914 |
| Positive RF | 76 (69%) | 68 (61%) | 144 (65%) | 0.226 |
| Positive anti-CCP | 92 (83%) | 78 (70%) | 170 (76%) | 0.02 |
| Serum IgG level (g/L) | 11.8 (4.6–19.2) | 12 (5.4–23.3) | 12 (4.6–23.3) | 0.564 |
| CRP level (mg/L) | 12 (0.4–139) | 11 (0.3–102) | 11 (0.3–139) | 0.938 |
| Radiographic erosions | 100 (90%) | 98 (87%) | 198 (88%) | 0.432 |
| MTX duration (years) | 3.6 (0.1–20.8) | 3.2 (0.3–20.5) | 3.5 (0.1–20.8) | 0.856 |
| Time since last anti-TNF (months) | 2.7 (0.6–64.4) | 2.8 (1.2–73.6) | 2.7 (0.6–73.6) | 0.458 |
Values are shown as means and standard deviations (mean ± SD) or medians (range) for continuous data, and n (%) for qualitative data
*Some patients had a deviation protocol concerning the authorized prednisone dosage
anti-CCP anti-cyclic citrullinated peptide antibody, CRP C-reactive protein, DAS28 Disease Activity Score in 28 joints, Eta etanercept, HAQ-DI Health Assessment Questionnaire—Disease Index, IL interleukin, mAb monoclonal antibody, MTX methotrexate, RF rheumatoid factor, TNF tumor necrosis factor
Serum IL-33 levels
Using the validated Quantikine assay, most of the patients had undetectable serum IL-33: 84/111 (76%) and 39/74 (53%) in cohorts 1 and 2, respectively. In patients with detectable IL-33, mean serum levels were 63.39 ± 87.31 pg/mL and 45.35 ± 87.19 pg/mL in cohorts 1 and 2, respectively (Fig. 1).
Fig. 1.
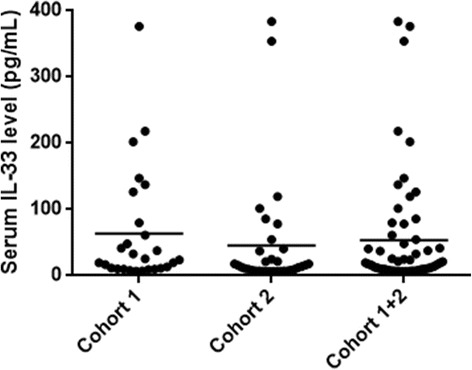
Serum IL-33 levels in patients from cohort 1, cohort 2, and the combined cohorts. Dosage performed with Quantikine ELISA IL-33 kit (R&D Systems). Each dot represents one patient; means are presented. IL interleukin
Factors associated with subsequent response to RTX at week 24 in cohort 1
Among the 111 patients, a total of 84 patients (76%) were classified as EULAR responders to RTX at week 24; 27 patients (24%) were non-responders. Detectable serum IL-33 was found in 27 (24.3%) patients. In univariate analysis, the three explanatory variables including DAS28-CRP >5.1, high serum IgG level, and auto-antibody status were associated with RTX response and were included in the multivariate model since they had a p value <0.15 for the association with EULAR response (Table 2).
Table 2.
Factors associated with rituximab response in cohorts 1 and 2
| Characteristic | EULAR non-responders | EULAR responders | Univariate | p value | Multivariate | p value | ||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||||||
| Cohort 1 (n = 111) | DAS28-CRP | 3.2–5.1 (Ref) | 12 (46.2%) | 14 (53.8%) | 4.0 (1.55–10.36) | 0.004 | 5.24 (1.85–14.85) | 0.002 |
| >5.1 | 15 (17.6%) | 70 (82.4%) | ||||||
| RF or anti-CCP | Negative (Ref) | 7 (41.2%) | 10 (58.8%) | 2.59 (0.88–7.67) | 0.08 | 3.48 (1.04–11.60) | 0.04 | |
| Positive | 20 (21.3%) | 74 (78.7%) | ||||||
| IgG > ULN (g/L) | No (Ref) | 21 (30.9%) | 47 (69.1%) | 2.76 (1.01–7.52) | 0.048 | 2.82 (0.97–8.14) | 0.056 | |
| Yes | 6 (14.0%) | 37 (86.0%) | ||||||
| Detectable IL-33 | No (Ref) | 23 (27.4%) | 61 (72.6%) | 2.17 (0.62–6.95) | 0.19 | – | – | |
| Yes | 4 (14.8%) | 23 (85.2%) | ||||||
| Cohort 2 (n = 74) | Disease activity DAS28-CRP | 3.2–5.1 (Ref) | 14 (36.8%) | 24 (63.2%) | 2.92 (0.97–8.73) | 0.056 | – | – |
| >5.1 | 6 (16.7%) | 30 (83.3%) | ||||||
| RF or anti-CCP | Negative (Ref) | 2 (100%) | 0 (0%) | 14.72 (0.34–629.71) | 0.16 | 32.76 (0.7–999) | 0.076 | |
| Positive | 18 (25.0%) | 54 (75%) | ||||||
| IgG > ULN (g/L) | No (Ref) | 15 (37.5%) | 25 (62.5%) | 2.10 (0.58–7.57) | 0.26 | – | – | |
| Yes | 4 (22.2%) | 14 (77.8%) | ||||||
| Detectable IL-33 | No (Ref) | 14 (35.9%) | 25 (64.1%) | 2.71 (0.91–8.10) | 0.07 | 3.73 (1.12–12.38) | 0.03 | |
| Yes | 6 (17.1%) | 29 (82.9%) | ||||||
Values are given as n (%) of responders or non-responders with a given characteristic
Rituximab response was evaluated at week 24 according to EULAR response
anti-CCP anti-cyclic citrullinated peptide antibody, CI confidence interval, DAS28-CRP Disease Activity Score in 28 joints by C-reactive peptide, EULAR European League Against Rheumatism, Ig immunoglobulin, OR odds ratio, Ref referent, RF rheumatoid factor, ULN upper limit of normal (i.e., 12.7 g/L)
The multivariate analysis indicated that high disease activity (OR 5.24, 95% CI 1.85–14.85) and auto-antibody status (OR 3.48, 95% CI 1.04–11.60) were independently associated with RTX response. A non-significant association between EULAR response and high serum IgG level was found (OR 2.82, 95% CI 0.97–8.14) (Table 2). There was no association with serum IL-33 detection in multivariate analysis in cohort 1.
Factors associated with subsequent response to RTX at week 24 in cohort 2
In order to replicate these results in RA patients from routine care, we tested whether the DAS28-CRP >5.1, high serum IgG level, auto-antibody status, and detectable serum IL-33 were associated with response to RTX in cohort 2 in which there were 73% EULAR responders among 74 patients.
In univariate analysis, high disease activity and detectable serum IL-33 were associated with RTX response, but not auto-antibody status or high serum IgG (Table 2). In multivariate analysis, detectable serum IL-33 was the sole factor associated with RTX response (OR 3.73, 95% CI 1.12–12.38), with a non-significant association for auto-antibody status (OR 32.76 (0.7– 999). The presence of RF and anti-CCP auto-antibodies in 97% of the patients in cohort 2 might limit analysis on these markers.
Factors associated with subsequent response to RTX at week 24 in the combination of cohorts 1 and 2
Multivariate analyses indicated that four factors were independently and significantly associated with response to RTX: high disease activity (OR 4.10, 95% CI 1.90–8.85), auto-antibody status (OR 3.27, 95% CI 1.13–9.46), high IgG level (OR 2.32, 95% CI 1.01–5.33), and detectable serum IL-33 (OR 2.40, 95% CI 1.01–5.72) (Table 3 and Fig. 2). Since the presence of RF and/or anti-CCP antibodies and high serum IgG level have already been identified as predictive markers of subsequent EULAR response, we aimed to investigate whether the addition of detectable serum IL-33 increased the likelihood of response. While 55% of patients without these three factors responded to RTX, the presence of RF and/or anti-CCP antibodies and elevated serum IgG level further increased the likelihood of this response (77% responders; OR = 2.72, 95% CI 0.67–10.98; p = 0.16 versus patients without any of these three factors). When we added detectable serum IL-33 to these two factors, 100% of the patients with the three risk factors (corresponding to 9% of the combined population) responded to RTX (OR 29.61, 95% CI 1.30–674.79; p = 0.034 versus patients with none of the three risk factors) (Fig. 3).
Table 3.
Factors associated with rituximab response in the combination cohort (cohorts 1 and 2)
| Characteristics | EULAR non-responders (n = 47) | EULAR responders (n = 138) | Univariate OR (95% CI) | p value | Multivariate OR (95% CI) | p value | |
|---|---|---|---|---|---|---|---|
| DAS28-CRP | 3.2–5.1 (Ref) | 26 (40.6%) | 38 (59.4%) | 3.26 (1.64–6.47) | 0.0007 | 4.10 (1.90–8.85) | 0.0003 |
| >5.1 | 21 (17.4%) | 100 (82.6%) | |||||
| RF or anti-CCP | Negative (Ref) | 9 (47.4%) | 10 (52.6%) | 3.03 (1.15–8.001) | 0.025 | 3.27 (1.13–9.46) | 0.03 |
| Positive | 38 (22.9%) | 128 (77.1%) | |||||
| IgG > ULN (g/L) | No (Ref) | 36 (33.3%) | 72 (66.7%) | 2.55 (1.16–5.60) | 0.02 | 2.32 (1.01–5.33) | 0.048 |
| Yes | 10 (16.4%) | 51 (83.6%) | |||||
| Detectable IL-33 | No (Ref) | 37 (30.1%) | 86 (69.9%) | 2.24 (1.03–4.87) | 0.04 | 2.40(1.01–5.72) | 0.047 |
| Yes | 10 (16.1%) | 52 (83.9%) | |||||
Values are given as n (%) of responders or non-responders with a given characteristic
Rituximab response was evaluated at week 24 according to EULAR response
anti-CCP anti-cyclic citrullinated peptide antibody, CI confidence interval, DAS28-CRP Disease Activity Score in 28 joints by C-reactive peptide, EULAR European League Against Rheumatism, Ig immunoglobulin, OR odds ratio, Ref referent, RF rheumatoid factor, ULN upper limit of normal (i.e., 12.7 g/L)
Fig. 2.
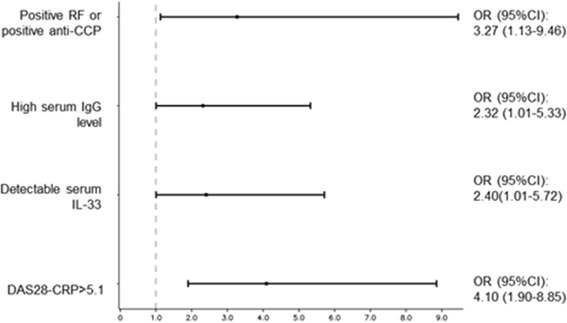
Association between the four explanatory variables and EULAR response at 24 weeks after the first rituximab infusion in the combination of cohorts 1 and 2. Results from the multivariate analysis are presented as odds ratios (OR) (95% confidence intervals (CI)) for each factor. anti-CCP anti-cyclic citrullinated peptide antibody, DAS28-CRP Disease Activity Score in 28 joints by C-reactive peptide, IL interleukin, RF rheumatoid factor
Fig. 3.
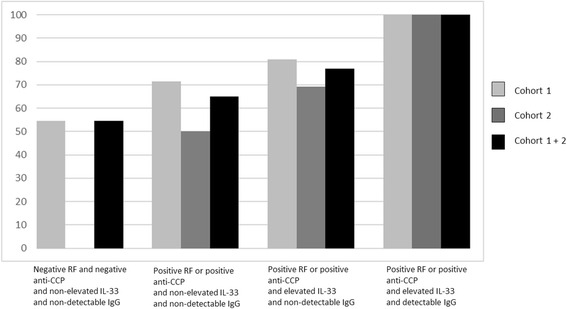
Frequency of EULAR response according to the presence of auto-antibodies, the detectability of serum IL-33, and a serum IgG above the upper limit of normal in cohort 1, cohort 2, and the combined cohorts. Results are presented for patients having auto-antibodies and/or elevated serum IL-33 level and/or elevated serum IgG level compared with patients having no auto-antibodies, a non-elevated serum IL-33 and a non-elevated IgG level (referent). anti-CCP anti-cyclic citrullinated peptide antibody, Ig immunoglobulin, IL interleukin, RF rheumatoid factor
If we restricted the analysis to seropositive patients from both cohorts (94/111 from cohort 1 and 72/74 from cohort 2), IL-33 detection was still highly predictive of EULAR response (OR 3.03, 95% CI 1.24–7.4; p = 0.015), confirming that this biomarker was independent of seropositivity.
Discussion
In this study, we have identified serum IL-33 detection as a novel biomarker associated with RTX response in RA, in addition to auto-antibody status, in real life patients.
This study was based on our previous observation of the upregulation of IL-33 mRNA expression in the whole blood that was associated with RTX response in a microarray study performed in patients randomly selected from the SMART trial [20]. Since the IL-33 protein may be easily quantified in the serum, we first assessed serum IL-33 levels in the same population using the DuoSet ELISA IL-33 kit (R&D System) and preliminary reported in an abstract that the serum IL-33 level was associated with the RTX response [23]. However, additional experiments in patients with Sjögren’s syndrome or RA have raised caution about the accuracy of this kit for sera measurements [24]. Consequently, we discarded these preliminary results and examined serum IL-33 again with an accurate ELISA kit (Quantikine) validated for sera, in two separate and then merged populations.
Here, we have found in univariate and multivariate analysis a significant association between serum IL-33 detection and EULAR response in cohort 2. Furthermore, when we combined the two cohorts, the association was significant with an odds ratio in the same range as high serum IgG level (i.e., approximately 2). We thus confirmed at the protein level the results found at the mRNA level, which demonstrates that transcriptomic analysis with non a-priori hypotheses might open the way to new pathogenic pathways.
This association was independent of strong predictive factors associated with RTX response, especially the presence of RF or anti-CCP antibodies, which strengthens the possible interest in serum IL-33 assessment. We previously reported that patients with a presence of auto-antibodies and high serum IgG level had a better response to RTX in comparison with patients having none of these characteristics [25]. If serum IL-33 detection is added to these two predictive factors, the likelihood of response to RTX reaches 29.6 (95% CI 1.3–675) in comparison with absence of these three factors. Indeed, 100% of patients displaying these three factors simultaneously were responsive to RTX in our combined cohort. However, these patients represented 9% of the study population.
Auto-antibody status was associated with RTX response in SMART, as previously reported [25], but also in the combination of cohorts. The absence of association in cohort 2 alone may be explained by the presence of these auto-antibodies in almost all the patients (97%) limiting analysis on these markers. Lastly, as in every trial, it is easier to have a response when the starting DAS28 is high and high disease activity was associated with a better response to RTX, as previously observed in SMART [25].
Despite a number of strengths, and especially the use of a replication cohort, this study has several limitations. First, serum IL-33 assessment needs the use of an accurate assay such as the Quantikine kit, but the relatively low frequency of patients with detectable IL-33 level (33.5% in the merged population) justifies qualitative IL-33 detection rather than quantitative IL-33 values. Second, we have no data on the association between serum IL-33 detection and response to other biologic agents in RA, limiting our findings to RTX. Third, the association between serum IL-33 detection and response to RTX is statistically significant, but the usefulness of such a measurement for clinical practice needs to be further investigated. Finally, the presence of RF and anti-CCP auto-antibodies in 97% of the patients in cohort 2 might limit analysis on these markers, as well as the difference in terms of high disease activity (DAS 28-CRP >5.1) frequency between the two cohorts (cohort 1 = 77% versus cohort 2 = 49%).
Conclusions
In conclusion, serum IL-33 assessment with a robust assay may represent a novel, easy biomarker predicting RTX response in synergy with auto-antibody status and high serum IgG level. Such a finding concerning these three biomarkers being easy to monitor in clinical practice represents a further step towards the goal of personalized medicine to determine the best approach to the therapeutic management of RA [27].
Acknowledgements
We thank the other members of the scientific committee of the SMART study: Pr. J. Sibilia (Strasbourg, France), Pr. J. Tebib (Lyon, France), Pr. B. Combe (Montpellier, France), and Pr. X. Le Loët (Rouen, France).
We thank all the SMART investigators: Dr. I. Azais, Poitiers; Dr. J.C. Balblanc, Belfort; Dr. F. Berenbaum, Paris; Dr. P. Bertin, Limoges; Dr. M.-C. Boissier, Bobigny; Dr. P. Bourgeois, Paris; Dr. A. Cantagrel, Toulouse; Dr. P. Carli, Toulon; Dr. P.-Y. Chouc, Marseille; Dr. M. Couret, Valence; Dr. L. Euller-Ziegler, Nice; Dr. P. Fardellone, Amiens; Dr. P. Fauquert, Berck/Mer; Dr. R.-M. Flipo, Lille; Dr. P. Gaudin, Echirolles; Dr. J.-L. Grauer, Aix en Provences; Dr. A. Heraud, Libourne; Dr. P. Hilliquin, Corbeil; Dr. S. Hoang, Vannes; Dr. E. Houvenagel, Lomme; Dr. D. Keita, Paris; Dr. K. Lassoued, Cahors; Dr. L. Le Dantec, Lievin; Dr. J.-M. Le Parc, Boulogne; Dr. L. Lequen, Pau; Dr. F. Lioté, Paris; Dr. C. Marcelli, Caen; Dr. O. Meyer, Paris; Dr. J.-L. Pellegrin, Pessac; Dr. A. Perdriger, Rennes; Dr. G. Rajzbaum, Paris; Dr. S. Redeker, Abbeville; Dr. J.-M. Ristori, Clermont-Ferrand; Dr. A. Saraux, Brest; Dr. G. Tanguy, La Roche sur Yon; Dr. T. Thomas, Saint-Priest-en-Jarez; Dr. L. Zabraniecki, Toulouse, Dr. C. Zarnitski, Montivilliers, France.
We thank Dr. Pascale Boisseaux and François Gavini (Roche, France) for supporting this ancillary study.
The authors thank Laura Smales (BioMed Editing, Toronto, Canada) for editing the manuscript and Statitec (Toulouse, France) for independent statistical analysis.
Funding
This work was supported by Roche France, who sponsored the study but were not involved in the interpretation of the data or in the preparation of the manuscript.
Role of the study sponsor: Roche France designed the SMART study but did not participate in the design, data collection, or interpretation of the results of this ancillary study, which was proposed by an independent scientific committee. Roche France supported the measurement of serum biomarkers and the statistical analysis. Roche France was not involved in the writing of the manuscript. Their agreement to submit the manuscript for publication was not required, their approval of the content of the submitted manuscript was not required, and publication of the manuscript was not contingent upon their approval.
Availability of supporting data
Supporting data are available and authors had full access to all of the data in the study.
Authors’ contributions
JS: participated in conception and design of the study, participated in the statistical analysis and interpretation of the results, and wrote the manuscript. ER: performed acquisition of the data, participated in the statistical analysis and interpretation of the results, and wrote the manuscript. AC: participated in statistical analysis and interpretation of the data, and wrote the manuscript. MD: participated in conception and design of the study, acquisition and interpretation of the data, and manuscript preparation. XM: participated in conception and design of the study, statistical analysis and interpretation of the results, and wrote the manuscript. POR, BT, EV, PE, GF, MS, BL, HHC and YT: participated in acquisition and interpretation of the data, and manuscript preparation. All authors reviewed and approved the final manuscript.
Authors’ information
JS and XM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
JS and ER made equal contribution to this study.
Competing interests
XM and MD belonged to the scientific committee of the SMART study and received honoraria from Roche (less than $10,000 each) for this task. A research grant was provided from Roche for the IL-33 serum biomarkers measurements and for independent statistical analysis.
Consent for publication
We confirm that all authors approved the manuscript for submission.
Ethical approval and consent to participate
This study was approved by each local ethic committee: Groupe Hospitalier Pitié-Salpêtrière, Paris, France; Leeds West Research Ethics Committee; and Ethic Committee of Clermont-Ferrand. Consent has been obtained from all patients who participated in this study.
Abbreviations
- anti-CCP
Anti-cyclic citrullinated peptide
- CI
Confidence interval
- CRP
C-reactive protein
- DAS28
Disease Activity Score in 28 joints
- ELISA
Enzyme-linked immunosorbent assay
- ESR
Erythrocyte sedimentation rate
- EULAR
European League Against Rheumatism
- Ig
Immunoglobulin
- IL
Interleukin
- MTX
Methotrexate
- OR
Odds ratio
- RA
Rheumatoid arthritis
- RF
Rheumatoid factor
- RTX
Rituximab
- ST
Suppression of tumorigenicity
- TNF
Tumor necrosis factor
- ULN
Upper limit of normal
Additional file
Baseline characteristics of RA patients from Clermont and from Leeds. (DOC 33 kb)
Contributor Information
Jérémie Sellam, Phone: +33 1 49 28 25 20, Email: jeremie.sellam@aphp.fr.
Elodie Rivière, Email: elodie.riviere.fr@gmail.com.
Alice Courties, Email: acourties@yahoo.fr.
Paul-Olivier Rouzaire, Email: porouzaire@chu-clermontferrand.fr.
Barbara Tolusso, Email: barbara.tolusso@unicatt.it.
Edward M. Vital, Email: e.m.j.vittal@leeds.ac.uk
Paul Emery, Email: p.emery@leeds.ac.uk.
Gianfranco Ferraciolli, Email: gf.ferraccioli@rm.unicatt.it.
Martin Soubrier, Email: msoubrier@chru-clermontferrand.fr.
Bineta Ly, Email: bineta.oumouly@gmail.com.
Houria Hendel Chavez, Email: houria.chavez@aphp.fr.
Yassine Taoufik, Email: yassine.taoufik@bct.aphp.fr.
Maxime Dougados, Email: maxime.dougados@aphp.fr.
Xavier Mariette, Phone: +33 1 45 21 37 58, Email: xavier.mariette@aphp.fr.
References
- 1.Liew FY, Pitman NI, McInnes IB. Disease-associated functions of IL-33: the new kid in the IL-1 family. Nat Rev Immunol. 2010;10(2):103–10. doi: 10.1038/nri2692. [DOI] [PubMed] [Google Scholar]
- 2.Theoharides TC, Petra AI, Taracanova A, Panagiotidou S, Conti P. Targeting IL-33 in autoimmunity and inflammation. J Pharmacol Exp Ther. 2015;354(1):24–31. doi: 10.1124/jpet.114.222505. [DOI] [PubMed] [Google Scholar]
- 3.Millar NL, Murrell GAC, McInnes IB. Alarmins in tendinopathy: unravelling new mechanisms in a common disease. Rheumatol Oxf Engl. 2013;52(5):769–79. doi: 10.1093/rheumatology/kes409. [DOI] [PubMed] [Google Scholar]
- 4.Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23(5):479–90. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Stolarski B, Kurowska-Stolarska M, Kewin P, Xu D, Liew FY. IL-33 exacerbates eosinophil-mediated airway inflammation. J Immunol Baltim Md 1950. 2010;185(6):3472–80. doi: 10.4049/jimmunol.1000730. [DOI] [PubMed] [Google Scholar]
- 6.Xu D, Jiang H-R, Kewin P, Li Y, Mu R, Fraser AR, et al. IL-33 exacerbates antigen-induced arthritis by activating mast cells. Proc Natl Acad Sci U S A. 2008;105(31):10913–8. doi: 10.1073/pnas.0801898105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu D, Jiang H-R, Li Y, Pushparaj PN, Kurowska-Stolarska M, Leung BP, et al. IL-33 exacerbates autoantibody-induced arthritis. J Immunol. 2010;184(5):2620–6. doi: 10.4049/jimmunol.0902685. [DOI] [PubMed] [Google Scholar]
- 8.Athari SK, Poirier E, Biton J, Semerano L, Hervé R, Raffaillac A, et al. Collagen-induced arthritis and imiquimod-induced psoriasis develop independently of interleukin-33. Arthritis Res Ther. 2016;18(1):143. doi: 10.1186/s13075-016-1042-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kunisch E, Chakilam S, Gandesiri M, Kinne RW. IL-33 regulates TNF-α dependent effects in synovial fibroblasts. Int J Mol Med. 2012;29(4):530–40. doi: 10.3892/ijmm.2012.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malcolm J, Awang RA, Oliver-Bell J, Butcher JP, Campbell L, Adrados Planell A, et al. IL-33 exacerbates periodontal disease through induction of RANKL. J Dent Res. 2015;94(7):968–75. doi: 10.1177/0022034515577815. [DOI] [PubMed] [Google Scholar]
- 11.Lee E-J, So MW, Hong S, Kim Y-G, Yoo B, Lee C-K. Interleukin-33 acts as a transcriptional repressor and extracellular cytokine in fibroblast-like synoviocytes in patients with rheumatoid arthritis. Cytokine. 2016;77:35–43. doi: 10.1016/j.cyto.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Xiangyang Z, Lutian Y, Lin Z, Liping X, Hui S, Jing L. Increased levels of interleukin-33 associated with bone erosion and interstitial lung diseases in patients with rheumatoid arthritis. Cytokine. 2012;58(1):6–9. doi: 10.1016/j.cyto.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Shen J, Shang Q, Wong C-K, Li EK, Wang S, Li R-J, et al. IL-33 and soluble ST2 levels as novel predictors for remission and progression of carotid plaque in early rheumatoid arthritis: a prospective study. Semin Arthritis Rheum. 2015;45(1):18–27. doi: 10.1016/j.semarthrit.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Martin P, Talabot-Ayer D, Seemayer CA, Vigne S, Lamacchia C, Rodriguez E, et al. Disease severity in K/BxN serum transfer-induced arthritis is not affected by IL-33 deficiency. Arthritis Res Ther. 2013;15(1):R13. doi: 10.1186/ar4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Talabot-Ayer D, Martin P, Seemayer CA, Vigne S, Lamacchia C, Finckh A, et al. Immune-mediated experimental arthritis in IL-33 deficient mice. Cytokine. 2014;69(1):68–74. doi: 10.1016/j.cyto.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Rivellese F, Suurmond J, Habets K, Dorjée AL, Ramamoorthi N, Townsend MJ, et al. Ability of interleukin-33- and immune complex-triggered activation of human mast cells to down-regulate monocyte-mediated immune responses. Arthritis Rheumatol Hoboken NJ. 2015;67(9):2343–53. doi: 10.1002/art.39192. [DOI] [PubMed] [Google Scholar]
- 17.Komai-Koma M, Gilchrist DS, McKenzie ANJ, Goodyear CS, Xu D, Liew FY. IL-33 activates B1 cells and exacerbates contact sensitivity. J Immunol Baltim Md 1950. 2011;186(4):2584–91. doi: 10.4049/jimmunol.1002103. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed A, Koma MK. Interleukin-33 triggers B1 cell expansion and its release of monocyte/macrophage chemoattractants and growth factors. Scand J Immunol. 2015;82(2):118–24. doi: 10.1111/sji.12312. [DOI] [PubMed] [Google Scholar]
- 19.Sattler S, Ling G-S, Xu D, Hussaarts L, Romaine A, Zhao H, et al. IL-10-producing regulatory B cells induced by IL-33 (Breg(IL-33)) effectively attenuate mucosal inflammatory responses in the gut. J Autoimmun. 2014;50:107–22. doi: 10.1016/j.jaut.2014.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sellam J, Marion-Thore S, Dumont F, Jacques S, Garchon H-J, Rouanet S, et al. Use of whole-blood transcriptomic profiling to highlight several pathophysiologic pathways associated with response to rituximab in patients with rheumatoid arthritis: data from a randomized, controlled, open-label trial. Arthritis Rheumatol Hoboken NJ. 2014;66(8):2015–25. doi: 10.1002/art.38671. [DOI] [PubMed] [Google Scholar]
- 21.Mariette X, Rouanet S, Sibilia J, Combe B, Le Loët X, Tebib J, et al. Evaluation of low-dose rituximab for the retreatment of patients with active rheumatoid arthritis: a non-inferiority randomised controlled trial. Ann Rheum Dis. 2014;73(8):1508–14. doi: 10.1136/annrheumdis-2013-203480. [DOI] [PubMed] [Google Scholar]
- 22.van Gestel AM, Anderson JJ, van Riel PL, Boers M, Haagsma CJ, Rich B, et al. ACR and EULAR improvement criteria have comparable validity in rheumatoid arthritis trials. American College of Rheumatology European League of Associations for Rheumatology. J Rheumatol. 1999;26(3):705–11. [PubMed] [Google Scholar]
- 23.Sellam J, Hendel-Chavez H, Rouanet S, Vernet N, Ly B, Marion-Thore S, et al. Serum IL-33 level is increased in rheumatoid arthritis and predicts response to rituximab in combination with high serum IgG level and autoantibody positivity: an open-label, prospective, multicentre biological trial. Arthritis Rheum. 2014;66(Suppl 10):S1279–80. [Google Scholar]
- 24.Rivière E, Ly B, Boudaoud S, Chavez H, Nocturne G, Chanson P, et al. Pitfalls for detecting interleukin-33 by ELISA in the serum of patients with primary Sjögren syndrome: comparison of different kits. Ann Rheum Dis. 2016;75(3):633–5. doi: 10.1136/annrheumdis-2015-208557. [DOI] [PubMed] [Google Scholar]
- 25.Sellam J, Hendel-Chavez H, Rouanet S, Abbed K, Combe B, Le Loët X, et al. B cell activation biomarkers as predictive factors for the response to rituximab in rheumatoid arthritis: a six-month, national, multicenter, open-label study. Arthritis Rheum. 2011;63(4):933–8. doi: 10.1002/art.30233. [DOI] [PubMed] [Google Scholar]
- 26.Couderc M, Mathieu S, Pereira B, Glace B, Soubrier M. Predictive factors of rituximab response in rheumatoid arthritis: results from a French university hospital. Arthritis Care Res. 2013;65(4):648–52. doi: 10.1002/acr.21865. [DOI] [PubMed] [Google Scholar]
- 27.van den Broek M, Visser K, Allaart CF, Huizinga TWJ. Personalized medicine: predicting responses to therapy in patients with RA. Curr Opin Pharmacol. 2013;13(3):463–9. doi: 10.1016/j.coph.2013.03.006. [DOI] [PubMed] [Google Scholar]


