Abstract
Sexual risk reduction interventions are often ineffective for women who drink alcohol. The present study examines whether an alcohol-related sexual risk reduction intervention successfully trains women to increase assertive communication behaviors and decrease aggressive communication behaviors. Women demonstrated their communication skills during interactive role-plays with male role-play partners. Young, unmarried, and nonpregnant African American women (N = 228, ages 18–24) reporting unprotected vaginal or anal sex and greater than three alcoholic drinks in the past 90 days were randomly assigned to a control, a sexual risk reduction, or a sexual and alcohol risk reduction (NLITEN) condition. Women in the NLITEN condition significantly increased assertive communication behavior compared to women in the control condition, yet use of aggressive communicative behaviors was unchanged. These data suggest assertive communication training is an efficacious component of a sexual and alcohol risk reduction intervention. Public health practitioners and health educators may benefit from group motivational enhancement therapy (GMET) training and adding a GMET module to existing sexual health risk reduction interventions. Future research should examine GMET’s efficacy in combination with other evidence-based interventions within other populations and examine talking over and interrupting one’s sexual partner as an assertive communication behavior within sexual health contexts.
Keywords: aggressive communication, alcohol risk reduction, assertive communication, health intervention, role-play, sexual risk reduction
Sexual risk reduction interventions are effective at increasing condom use and reducing incident sexually transmitted infections (STIs; Eaton et al., 2012; Johnson, Scott-Sheldon, Huedo-Medina, & Carey, 2011; Scott-Sheldon, Huedo-Medina, Warren, Johnson, & Carey, 2011; Wingood et al., 2013). Behavioral interventions focus on reducing exposure to human immunodeficiency virus (HIV)/STIs using training strategies focused on improving condom skills, healthy sexual choices, and assertive communication. Motivating sexual partners to negotiate safer sex (e.g., condom use) is vital to intervention success. In a meta-analysis of 34 studies examining sexual communication and condom use among adolescents (ages 12–23, M = 16.80 years), Widman, Noar, Choukas-Bradley, and Francis (2014) found a 0.24 effect size for the sexual communication–condom use relationship; the effect size was even larger when discussing condom use (r = .34). Thus, communication should be considered a primary predictor and mediator of condom use (Noar, Carlyle, & Cole, 2006; Widman et al., 2014). The specific aim of this study was to use a sexual health role-play assessment to investigate behavioral intervention efficacy at increasing assertive sexual communication.
Sexual risk reduction interventions teach assertive communication when negotiating condom use (Allen, Emmers-Sommer, & Crowell, 2002; Otto-Salaj et al., 2008). Assertive sexual communication uses firm and direct verbal and non-verbal communication to express a desire for safer sexual choices (e.g., condom use) without engaging in aggressive, hostile, or attacking communication toward a partner. More specifically, assertive communication reflects direct and appropriate expression of one’s feelings, beliefs, and opinions to a partner while protecting the self-concept of a partner (Rancer & Avtgis, 2006). Sexual assertiveness is linked to one’s insistence to engage in safe sex behaviors with a partner (Noar et al., 2006; Widman et al., 2014). Assertiveness also involves direct attempts to change partner behavior if it conflicts with one’s beliefs or attitudes. In contrast, aggression is demonstrated through communicating hostility, put-downs, threats, or manipulative statements (Malik & Lindahl, 2004).
Improving sexual communication skills is especially important among high-risk populations. Young, African American women who report a higher frequency of alcohol use have markedly higher rates of risky sexual behaviors than peers (Sales et al., 2014), yet there are no evidence-based STI/HIV interventions designed to be gender and culturally congruent for alcohol using African American women. HORIZONS, a CDC-defined evidence-based intervention, is a gender and culturally tailored intervention for young, African American women emphasizing HIV-related sexual communication, condom use, healthy relationships, and norms supportive of safer sex. The effects across biological, behavioral, and psychosocial outcomes demonstrate its efficacy (DiClemente et al., 2009). While HORIZONS was not designed to address alcohol use, alcohol consumption was a significant moderator adversely affecting intervention efficacy (Sales et al., 2014).
To address this gap, NLITEN, an alcohol-related sexual risk reduction intervention, was created that supplements HORIZONS with a motivational interviewing approach (Miller & Rollnick, 2013) called group motivational enhancement therapy (GMET; see Miller, 2000; Miller, Zweben, DiClemente, & Rychtarik, 1994). GMET has demonstrated promise in reducing alcohol use and alcohol-related risk-taking among the same age group of college students (LaChance, Feldstein Ewing, Bryan, & Hutchison, 2009) and in reducing HIV/STI risk among detained adolescents (Schmiege, Broaddus, Levin, & Bryan, 2009). NLITEN strengthens women’s communication skills efficacy and encourages assertive communication regarding sexual choices without engaging in aggressive behaviors.
While sexual health interventions report increases in sexual communication skills after the intervention (DiClemente et al., 2004; DiClemente et al., 2009), these data are limited by self-report assessments of communication skills (for exceptions, see Jouriles, Simpson Rowe, McDonald, Platt, & Gomez, 2011; Kelly et al., 1994). In response to recent calls to evaluate intervention efficacy with alternatives to self-report measures (DiClemente et al., 2008; DiClemente, Milhausen, Sales, Salazar, & Crosby, 2005; Sales, Milhausen, & Diclemente, 2006), sexual communication role-play assessments are utilized to investigate intervention efficacy at increasing assertive and decreasing aggressive communication. This study tests whether women in the NLITEN condition act more assertively (Hypothesis 1) and less aggressively (Hypothesis 2) than women in either the control or HORIZONS-only conditions.
Method
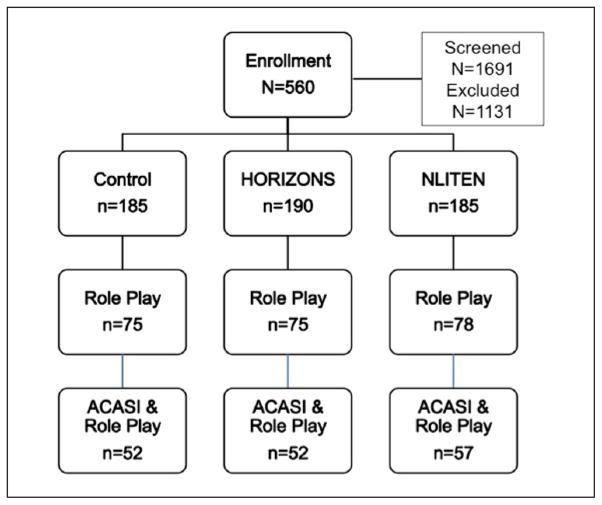
These data were collected as part of a comparative efficacy trial of an intervention to reduce alcohol-related sexual risk among young, African American women. A randomized sub-sample (40%) participated in role-play assessments (see Figure 1). Research protocols were approved by two university institutional review boards.
Figure 1.
Intervention enrollment, 40% randomized to role-play assessment, and complete audio computer assisted self-interview (ACASI) and role-play assessment data counts.
Participants
Recruitment and Eligibility
Participants (N = 228) were African American women, aged 18 to 24 years (M = 20.46, SD = 1.99) from a metropolitan city, recruited at various locations (e.g., malls, clubs, bars), work placement programs, and by referral from other participants beginning in January 2012. Enrollment began March 2012 through February 2014. Screening occurred onsite or by phone; eligible women were invited to participate if they met inclusion criteria: unmarried, unprotected vaginal or anal sex, and >3 alcoholic drinks in the past 90 days. Women were tested on site and excluded if currently pregnant. Participants received compensation up to $150 for completing all study activities.
Characteristics
At baseline, 31.5% (n = 72) of participants had some high school or less, 36.4% (n = 83) had graduated high school or earned their GED, and 26.3% (n = 60) had some college. The majority (82.5%, n = 188) received food stamps in the past 12 months and were unemployed (73.2%, n = 167). Furthermore, 35% (n = 80) had at least one STI.
Participant Flow
After determining eligibility, participants were given informed consent. Participants then completed an audio computer assisted self-interview (ACASI) survey assessing demographics, alcohol and drug use, personality, and sexual behavior; ACASI took 90 minutes on average. Next, participants were randomized (via a SAS macro) to one of three study conditions; 40% from each study condition were rerandomized to complete a baseline and postintervention communication role-play assessment (Figure 1). Of participants assigned to complete the role-play (n = 228), only those with complete ACASI and role-play assessment data at baseline and postintervention were included in the present study (71%, n = 161). Missing data occurred due to attrition, time constraints, participant refusal, and recording equipment failure.
Intervention Conditions
The intervention is a comparative trial with three arms: (1) standard of care control condition, (2) HORIZONS + GHP (general health promotion), and (3) NLITEN (HORIZONS + GMET module).
Control
The control condition was a 1-hour group session, implemented by an African American woman health educator, consisting of a culturally and gender appropriate STI/HIV prevention video, a question-and-answer session, and a group discussion.
HORIZONS + GHP
The HORIZONS condition included HORIZONS (two 4-hour STI/HIV prevention sessions) and a GHP module time-equivalent to the GMET module. HORIZONS is based on social cognitive theory (Bandura, 1994), the theory of gender and power (Wingood & DiClemente, 2000), and previously published interventions for adolescent females seeking clinical services (DiClemente et al., 2004). HORIZONS strengthens women’s interpersonal power by supporting their sexual health choices and motivating women to assert the right to negotiate safer sex (Wingood, Hunter-Gamble, & DiClemente, 1993). Sessions are interactive, fostering cultural and gender pride, and emphasize factors contributing to STI/HIV risk, including individual factors (STI/HIV risk reduction knowledge, perceived peer norms supportive of condom use, condom use skills), relational factors (persuasive communication techniques), sociocultural factors (encouraged participants to reduce douching), and structural factors (e.g., partner access to STI testing and treatment). HORIZONS teaches assertive communication skills by first presenting components of assertive communication (e.g., eye contact, firm voice, listening skills) followed by participants role-playing assertive communication with sex partners about condom use, STI testing, and partner notification. To gain partner compliance to respect sexual health choices (e.g., condoms and/or abstinence), women are taught to recognize their own aggressive (e.g., blaming or insulting a partner) and passive communication behaviors (e.g., lack of eye contact) and ways to reduce ineffective communication behaviors.
NLITEN
The NLITEN condition included the two HORIZONS sessions and a GMET module. GMET was designed to increase intrinsic motivation to reduce alcohol-related sexual risk by promoting healthy alcohol consumption (e.g., reducing number of drinks, drinking less frequently) and positive sexual health choices (e.g., condom use, sexual abstinence). By design, GMET is less structured than traditional group-based workshops, being primarily discussion-based and participant driven. Specific activities include enhancing awareness of drinking levels, exploring alcohol use pros and cons, understanding alcohol’s effects on decision making, and developing goals and strategies to reduce alcohol-related sexual risk behavior. Women are encouraged to communicate these goals and use these strategies with sexual partners (Bryan, Schmiege, & Broaddus, 2009). Participants also watched a video depicting three African American young women who attended a house party, drank alcohol, and engaged in sex; each woman experienced a different scenario related to partner type (familiar/nonfamiliar) and condoms (condom use/nonuse). This video stimulated discussion about identifying strategies to make safer sexual decisions when alcohol is involved, setting clearly defined goals about sexual health choices, and enhancing efficacy to communicate with sex partners. With discussion facilitated by health educators (HEs) and content driven by participants, GMET content varied within the outlined structure.
Implementation
After participants completed ACASI and role-play assessment, they completed either the control condition or the first 4-hour STI/HIV prevention session. The following week, HORIZONS + GHP and NLITEN participants returned and completed the second 4-hour HORIZONS session and either the GHP or GMET module. After their sessions were complete, participants completed the postintervention role-play assessment.
Evaluation
Role-Play Communication Assessment and Procedures
Women engaged in a sexual communication role-play with a confederate role-play partner (RPP; N = 12). Having the ability to assertively communicate in a safe/low-stakes environment, such as a role-play, is a mechanism to assess how women communicate in actual sexual situations with partners. While other factors may influence sexual communication between partners, including partner type (e.g., Noar et al., 2012) and sex education (Troth & Peterson, 2000), if people cannot show assertive behavior and effectively manage the conversation in nonthreatening role-play enactments, they may not exhibit these skills in their normal lives (Somlai et al., 1998).
RPPs were African American men, aged 18 to 30 years, selected based on their interpersonal skills. RPPs attended 6 hours of training with 1-hour refresher trainings monthly for consistency in interpersonal skills to persuade a woman to engage in unsafe sex. There were no significant effects of RPP on the woman’s communication behaviors. Women were told the role-play was a conversation about sexual health with a male. Set-up was two chairs angled toward each other with video cameras opposing each chair. A research assistant (RA) introduced the role-play assessment and the RPP. Next, the RPP and woman were given 3 to 5 minutes to get acquainted. Next, the RA told the woman her goal was to convince the RPP to use a condom and presented a scenario. The woman and RPP were instructed to write down what each would say or do. When completed, the RA reread the scenario and instructed the participant to begin once the RA left. Role-plays lasted 5 to 7 minutes.
The RPPs consistently attempted to influence their partner to engage in sexual intercourse without a condom by engaging in three behaviors: (1) information seeking (e.g., “Why do you want to use a condom?”), (2) a seduction attempt (e.g., “I want to feel all of you”), and (3) a threat (e.g., “Don’t you trust me?”). Efforts were made so participants interacted with a different RPP at baseline and postintervention.
Three role-play scenarios utilized were pilot tested by the target population. The woman was asked to imagine herself drinking alcohol and expected to negotiate condom use with a regular partner (Scenario 1), new partner she had been dating (Scenario 2), or a new partner (Scenario 3). While Scenarios 1 and 2 specifically stated the couple has been intimate without sex, Scenario 3 asked women to negotiate condom use before foreplay or sexual activity. At baseline and postintervention, participants were randomly assigned without replacement to role-play one of three scenarios. There were no significant effects of role-play scenario on women’s communication behaviors.
Coded Role-Play Measures
To code women’s nonverbal and verbal behavior, each role-play was edited to a 2-minute segment starting when a woman was focused on the topic/conversation. Primary and reliability coders (N = 7), unaware of the study hypotheses, received a minimum of three, 2-hour training sessions for each content type they coded, along with 1-hour refresher training every other month. A random 25% of the interactions were assessed for intercoder reliability. More general assessments (e.g., How assertive was the participant?) were coded using both audio and visual information.
Assertive Behavior
Assertiveness included using verbal and nonverbal symbols to exert control/achieve goal/defending position/avoid violation of own rights without attacking or insulting partner (Samp & Solomon, 2005). Measures for assertiveness were taken from Infante (1987) and Malik and Lindahl’s (2004) assessments. Coders assessed the woman’s behavior for overall assertiveness, confidence in making arguments, direct eye contact, communicating her opinions openly, directly addressing the partner’s arguments, responsiveness to his attempts to persuade, validating his perspective in the interaction, and the degree to which she allowed her partner to dictate the terms of the conversation.
Aggressive Behavior
Aggressive communication behavior included acting hostile and attacking the self-concept of RPP, instead of only his position on a particular topic. Aggression items were taken from Canary (2003), Malik and Lindahl (2004), and Coan and Gottman (2007). Coders assessed general (overall) aggression, defensiveness, frequency of threats and hostile verbal behavior (coded on occurrence of blaming, insults, put downs, negative mind reading, accusations, and denial, awkward silences, interruptions and talking over their partner). Finally, they coded for nonverbal indicators of disgust or hostility (coding on occurrence of these behaviors: rolling eyes, pointing or waiving finger at RPP, throwing hands up in the hair, lifting eye brows, shaking head, reactive attitude display).
As seen in Table 1, confirmatory factor analyses in Mplus using maximum likelihood estimation indicated best fit for a five-item assertiveness factor and a five-item aggressiveness factor. Also, a two-item talking over/interrupting (TO/I) partner factor was created.
Table 1.
Interitem and Interrater Reliability.
| Dimension | Interrater reliabilitya | Scale |
|---|---|---|
| Assertive behavior factor (α = .78; M = 1.84, SD = 0.54)b,c | ||
| General assertiveness level | .70 | 1 (Not at all assertive) to 5 (Highly assertive) |
| Communicated opinions openly | .72 | 1 (Strongly disagree) to 5 (Strongly agree) |
| Directly addressed arguments | .69 | 1 (Avoids) to 5 (Directly addresses) |
| Let RPP dictate conversation | .63 | 1 (Most of the time) to 5 (Hardly at all) |
| Validated RPP’s statements | .64 | Count on occurrence (range: 0–5) |
| Aggressive behavior factor (α = .77; M = 1.18, SD = 0.49)c | ||
| General verbal aggressiveness | .71 | 1 (Not at all) to 5 (Very verbally aggressive) |
| Hostile verbal behaviors | .84 | Count on occurrence (range: 0–17) |
| Used threat to convince RPP | .75 | 1 (Never), 2 (1–2 times), 3 (>2 times) |
| Nonverbal hostility or disgust | .71 | Count on occurrence (range: 0–37) |
| Defensive voice | .67 | 1 (Not often/not at all) to 5 (Consistently) |
| Talk over partner (α = .76, M = 1.95, SD = 0.74)c | ||
| Talked over RPP | .73 | 0 (Never), 1(A few times), 2 (3 or more) |
| Interrupted RPP | .69 | 1 (Never), 2 (A few times), 3 (3 or more) |
Note. RPP = role-play partner.
Intraclass correlation coefficient (Model: One-way random).
Cronbach’s alpha.
The factors were created by first multiplying each item by its respective factor loading and, second, summing the resulting five items creating an assertiveness factor and summing five items creating an aggression factor. Assertiveness was not related to aggression (r = −.002) and modestly related to the talking over factor (r = .18, p < .05). Aggression was also modestly correlated to the talking over factor (r = .34, p = .01).
Covariates
Three covariates were used in the analyses: age, proportion condom use, and alcohol use. Age was in years (M = 20.44, SD = 1.95). Proportion condom use was the total number of times the participant used a condom divided by the total number of times the participant engaged in vaginal sex in the past 3 months (M = 0.31, SD = 0.30). Alcohol use was assessed with 10 AUDIT items (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998). Following AUDIT scoring, items were assigned a point value and summed where higher numbers indicate higher consumption (M = 8.14, SD = 6.48, α = .84).
Data Analysis
Role-play assertive and aggressive communication data were analyzed using repeated-measures analysis of variance (ANOVA) with 2 (Time: baseline vs. postintervention) × 3 (Condition: Control, HORIZONS, and NLITEN) design. Dependent measures were assertive, aggressive, and talk over/interrupt factors. Covariates from baseline ACASI data were age, proportion condom use, and alcohol use.
Results
Repeated-measures ANOVA results are divided below by assertive communication, talking over/interrupting partner, and aggressive communication. For means and standard errors, see Table 2.
Table 2.
Communication Behavior Means and Standard Errors at Baseline and Postintervention.
| Communication behavior | Baseline
|
Postintervention
|
||
|---|---|---|---|---|
| M | SEM | M | SEM | |
| Assertive | ||||
| Control | 1.86 | 0.07 | 1.78 | 0.07 |
| HORIZONS | 1.85 | 0.08 | 1.93 | 0.08 |
| NLITEN | 1.81 | 0.07 | 2.04 | 0.07 |
| Talk over/interrupt | ||||
| Control | 1.98 | 0.10 | 2.04 | 0.10 |
| HORIZONS | 2.08 | 0.11 | 1.99 | 0.09 |
| NLITEN | 1.82 | 0.09 | 2.17 | 0.09 |
| Aggressive | ||||
| Control | 1.24 | 0.07 | 1.08 | 0.07 |
| HORIZONS | 1.19 | 0.06 | 1.11 | 0.06 |
| NLITEN | 1.10 | 0.07 | 1.11 | 0.07 |
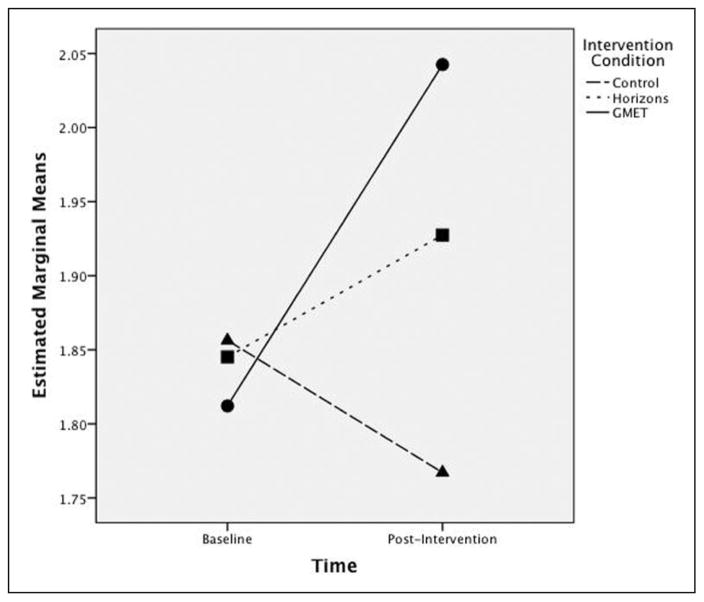
Assertive Communication
There was a significant time by intervention condition effect for assertive communication, Wilks’s Λ = .95, F(2, 152) = 4.28, p = .01, η2 = .05 (see Figure 2). At baseline, there was no significant difference as a function of intervention condition, F(2, 158) = 1.13, p = .33. However, postintervention there was a significant condition effect, F(2, 158) = 3.00, p = .05, such that participants in the NLITEN condition (M = 2.70, SD = 0.70) were significantly more assertive than those in the control condition (M = 2.37, SD = 0.68). However, neither the control nor NLITEN conditions were significantly different than the HORIZONS condition (M = 2.56, SD = 0.72). Finally, the NLITEN participants’ assertive communication significantly differed from baseline (M = 2.41, SD = 0.76) to postintervention, t(56) = −3.58, p < .05. Thus, participants in the NLITEN condition increased their use of assertive behavior from baseline to postintervention compared with the control condition.
Figure 2.
Assertive communication behavior at baseline and postintervention by intervention condition.
Note. GMET = group motivational enhancement therapy.
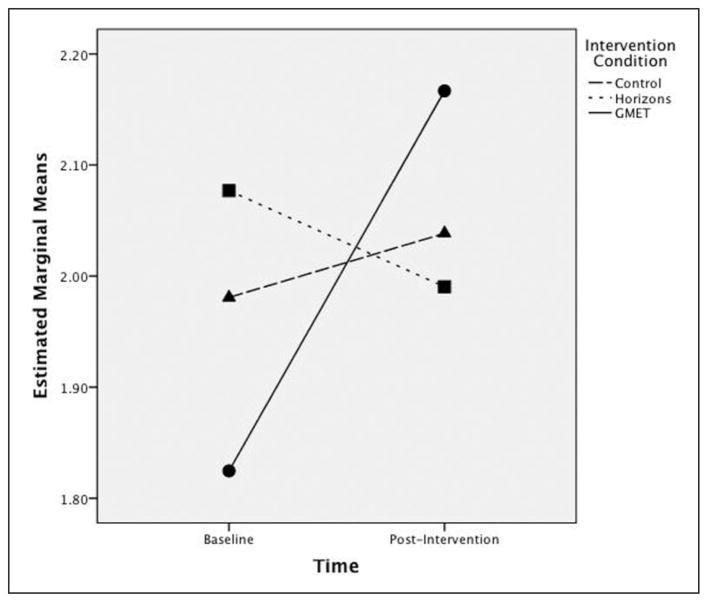
Talking Over and Interrupting Partner
There was also a significant time by intervention condition effect for how often a participant talked over or interrupted (TO/I) her partner, Wilks’s Λ = .94, F(2, 152) = 4.78, p = .01, η2 = .06 (see Figure 3). At baseline, there was no significant intervention condition differences, F(2, 158) = 1.64, ns. Using a one-way ANOVA, there were no significant effects of intervention condition on postintervention TO/I, F(2, 158) = 0.09, p = .91. However, as compared with participants in other conditions, NLITEN participants TO/I their role-play partner the least at baseline (M = 1.82, SD = 0.66) and TO/I the most postintervention, M = 2.17, SD = 0.73, t(56) = −3.55, p < .05.
Figure 3.
Talking over/interrupting partner at baseline and postintervention by intervention condition.
Note. GMET = group motivational enhancement therapy.
Aggressive Communication
Time by condition for aggression was not significant, Wilks’s Λ = 0.99, F(2, 152) = 1.14, ns. In all the above analyses, there was not a significant time by covariate effect (p >.10): alcohol use, Wilks’s Λ = 0.99, F(1, 152) < 1; age, Wilks’s Λ = 0.99, F(1, 152) < 1; proportion condom use, Wilks’s Λ = 0.99, F(1, 152) < 1. Thus, women in the NLITEN condition were more assertive and more likely to talk over their partners than were women in the control condition, supporting Hypothesis 1. Contrary to Hypothesis 2, women in the NLITEN were not less aggressive in their communication behavior than those in the other conditions.
Discussion
We demonstrated the efficacy of assertive communication skills training as part of a HIV/STI risk reduction intervention among young, African American women to increase assertive communication behavior. Using objective communication role-play assessments, within- and between-subjects effects were found. Specifically, NLITEN condition women expressed more assertive communication behaviors postintervention than at baseline and compared to control condition women. These data suggest the specialized HORIZONS + GMET module worked as intended and provided women with increased motivation to assert condom use during role-play. Furthermore, because NLITEN participants increased use of assertive communication while women in HORIZONS + GHP did not, this suggests NLITEN (HORIZONS + GMET) created an additive effect for assertive communication behavior.
Through discussion in the GMET modules, HEs and participants created a supportive environment where women were able to share past sexual choices and encourage each other to make healthier sexual choices (e.g., condom use). Furthermore, NLITEN women discussed the GMET video depictions of assertive communication that were introduced in HORIZONS and discussed assertive communication used during the past week. Thus, assertive behavior skills efficacy was reinforced through HE and peer encouragement, successful facilitation of the GMET video, and assertive communication use in relationships.
Results were not significant for aggressive communication. The intervention failed to reduce aggressive behavior possibly because the focus was on practicing assertive communication whereas there were fewer opportunities to demonstrate using less aggressive communication. Other research demonstrates aggressive communication behavior is problematic for relationships (Malik & Lindahl, 2004) and is positively associated to sexual risk (Coles et al., 2015). Thus, future research is needed to work on how to concomitantly increase assertive while decreasing aggressive communicative behaviors.
Additionally, NLITEN condition women did significantly increase the amount they talked over and interrupted (TO/I) their partner, which typically reflects communicative aggression (Malik & Lindahl, 2004). Yet such behavior may serve as a marker of increased motivation. Given women TO/I their partner more, yet were not more aggressive in other verbal aggression markers, suggests that TO/I might be more like an assertive behavior. Women feel more motivated to assert their wishes and to TO/I their partner when he behaved in ways not consistent with their wishes to use a condom. HORIZONS was designed to increase women’s interpersonal power or their belief they have a right to communicate about sexual health choices and this was further emphasized during GMET. Therefore, it may be that TO/I reflects this increased motivation, although more research is needed to fully understand this effect.
This study is limited in the use of role-play situations with confederates, which may not represent what women do in “real life.” Role-plays are advantageous, providing communication assessments beyond self-report. Other research consistently shows little relationship between self-report and observer-reported communication perceptions (Carrell & Clay Willmington, 1996; Jones, 1991; Rubin, Graham, & Mignerey, 1990). Indeed, most research supports Kelly’s (1995) claim that self-reports of behavioral skills often do not correlate highly with observation-based assessments of skill. Self-report may be a better marker of one’s anticipated self-efficacy for handling a problematic or anxiety-inducing situation rather than assessing what an individual’s behavioral repertoire is for such situations (Somlai et al., 1998). While role-play assessments are constrained they may more accurately reflect women’s communication skills negotiating safer sex than self-report measures.
Public health practitioners, particularly HEs, may benefit from training and using the GMET approach for sexual health risk reduction education in conjunction with an evidence-based intervention. GMET is promising as it allows the participant to express her individual motivation(s) for changing her behavior. The HE and peers can build motivation through focused discussions to encourage change. These data suggest the combination of an evidence-based intervention and GMET are especially powerful to improve assertive communication skills among young, African American women. Future research should consider the additive effects of GMET and test within other populations beyond our single metropolitan sample. Future research should examine how TO/I a partner may be a marker of assertive communication within sexual health conversations.
In summary, NLITEN, an alcohol-related sexual risk reduction intervention, was efficacious at increasing African American women’s assertive communication behavior compared with women who did not receive the intervention. NLITEN intervention participants were also more likely to talk over and interrupt their partner during a sexual negotiation role-play.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Grant Number R01AA018096 from NIH/NIAAA.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allen M, Emmers-Sommer TM, Crowell TL. Couples negotiating safer sex behaviors: A meta-analysis of the impact of conversation and gender. In: Allen M, Preiss RW, Gayle BM, Burrell NA, editors. Interpersonal communication research: Advances through meta-analysis. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 263–279. [Google Scholar]
- Bandura A. A social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, Peterson J, editors. Preventing AIDS theories and methods of behavioral interventions. New York, NY: Plenum; 1994. pp. 25–59. [Google Scholar]
- Bryan AD, Schmiege SJ, Broaddus MR. HIV risk reduction among detained adolescents: A randomized, controlled trial. Pediatrics. 2009;124:e1180–e1188. doi: 10.1542/peds.2009-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Canary DJ. Nonverbal communication skills. In: Greene JO, Burleson BR, editors. Handbook of communication and social interaction skills. Mahwah, NJ: Lawrence Erlbaum; 2003. pp. 515–549. [Google Scholar]
- Carrell LJ, Clay Willmington S. A comparison of self-report and performance data in assessing speaking and listening competence. Communication Reports. 1996;9:185–191. [Google Scholar]
- Coan JA, Gottman JM. The Specific Affective Coding System (SPAFF) In: Coan JA, Allen JJB, editors. Handbook of emotion elicitation and assessment. New York, NY: Oxford University Press; 2007. pp. 267–285. [Google Scholar]
- Coles VB, Monahan JL, Bradley ELP, Mercer Kollar LM, Samp JA, Davis TL, … DiClemente RJ. Are all forms of insistence equally effective? Sexual assertiveness, aggression, and biological sexual risk markers. Paper presented at the 2015 International Communication Association Annual Conference, Interpersonal Communication Division; San Juan, Puerto Rico. 2015. [Google Scholar]
- DiClemente RJ, Crittenden CP, Rose E, Sales JM, Wingood GM, Crosby RA, Salazar LF. Psychosocial predictors of HIV-associated sexual behaviors and the efficacy of prevention interventions in adolescents at-risk for HIV infection: What works and what doesn’t work? Psychosomatic Medicine. 2008;70:598–605. doi: 10.1097/PSY.0b013e3181775edb. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Milhausen R, Sales JM, Salazar LF, Crosby RA. A programmatic and methodologic review and synthesis of clinic-based risk-reduction interventions for sexually transmitted infections: Research and practice implications. Seminars in Pediatric Infectious Diseases. 2005;16:199–218. doi: 10.1053/j.spid.2005.04.009. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW., III Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of the American Medical Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, … Crosby RA. Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2009;163:1112–1121. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- Eaton LA, Huedo-Medina TB, Kalichman SC, Pellowski JA, Sagherian MJ, Warren M, … Johnson BT. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: Implications for bundling prevention packages. American Journal of Public Health. 2012;102:e34–e44. doi: 10.2105/AJPH.2012.300968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infante DA. Aggressiveness. In: McCroskey JC, Daly JA, editors. Personality and interpersonal communication. Newbury Park, CA: Sage; 1987. pp. 157–192. [Google Scholar]
- Johnson BT, Scott-Sheldon LA, Huedo-Medina TB, Carey MP. Interventions to reduce sexual risk for human immunodeficiency virus in adolescents: A meta-analysis of trials, 1985–2008. Archives of Pediatrics & Adolescent Medicine. 2011;165:77–84. doi: 10.1001/archpediatrics.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S. Problems of validity in questionnaire studies on nonverbal behavior: Jourard’s Tactile Body-Accessibility Scale. Southern Communication Journal. 1991;56:83–95. [Google Scholar]
- Jouriles EN, Simpson Rowe L, McDonald R, Platt CG, Gomez GS. Assessing women’s responses to sexual threat: Validity of a virtual role-play procedure. Behavior Therapy. 2011;42:475–484. doi: 10.1016/j.beth.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Kelly JA. Changing HIV risk behavior: Practical strategies. New York, NY: Guilford Press; 1995. [Google Scholar]
- Kelly JA, Murphy DA, Washington CD, Wilson TS, Koob JJ, Davis DR, … Davantes B. The effects of HIV/AIDS intervention groups for high-risk women in urban clinics. American Journal of Public Health. 1994;84:1918–1922. doi: 10.2105/ajph.84.12.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaChance H, Feldstein Ewing SW, Bryan AD, Hutchison KE. What makes group MET work? A randomized controlled trial of college student drinkers in mandated alcohol diversion. Psychology of Addictive Behaviors. 2009;23:598. doi: 10.1037/a0016633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik NM, Lindahl KM. System for coding interactions in dyads (SCID) In: Kerig PK, Baucom DH, editors. Couple observational coding systems. Mahwah, NJ: Lawrence Erlbaum; 2004. pp. 173–188. [Google Scholar]
- Miller WR. Motivational enhancement therapy: Description of counseling approach. In: Boren JJ, Onken LS, Carroll KM, editors. Approaches to drug abuse counseling. Bethesda, MD: National Institute on Drug Abuse; 2000. pp. 99–105. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping people change. 3. New York, NY: Guildford Press; 2013. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual. Washington, DC: National Institute on Alcohol Abuse and Alcoholism; 1994. Project MATCH Monograph Series. [Google Scholar]
- Noar SM, Carlyle K, Cole C. Why communication is crucial: Meta-analysis of the relationship between safer sexual communication and condom use. Journal of Health Communication. 2006;11:365–390. doi: 10.1080/10810730600671862. [DOI] [PubMed] [Google Scholar]
- Noar SM, Webb E, Van Stee S, Feist-Price S, Crosby R, Willoughby JF, Troutman A. Sexual partnerships, risk behaviors, and condom use among low-income heterosexual African Americans: A qualitative study. Archives of Sexual Behavior. 2012;41:327–345. doi: 10.1007/s10508-011-9890-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otto-Salaj L, Reed B, Brondino MJ, Gore-Felton C, Kelly JA, Stevenson LY. Condom use negotiation in heterosexual African American adults: responses to types of social power-based strategies. Journal of Sex Research. 2008;45:150–163. doi: 10.1080/00224490801987440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rancer AS, Avtgis TA. Argumentative and aggressive communication: Theory, research, and application. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Rubin R, Graham E, Mignerey J. A longitudinal study of college students’ communication competence. Communication Education. 1990;39:1–14. [Google Scholar]
- Sales JM, Milhausen RR, Diclemente RJ. A decade in review: Building on the experiences of past adolescent STI/HIV interventions to optimise future prevention efforts. Sexually Transmitted Infections. 2006;82:431–436. doi: 10.1136/sti.2005.018002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales JM, Monahan JL, Brooks C, DiClemente R, Rose E, Samp JA. Differences in sexual risk behaviors between lower and higher frequency alcohol-using African-American adolescent females. Current HIV Research. 2014;12:276–281. doi: 10.2174/1570162x12666140721122606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samp JA, Solomon DH. Toward a theoretical account of goals in message features. Communication Monographs. 2005;72:22–45. doi: 10.1080/0363775052000342517. [DOI] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STI risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology. 2009;77:38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Huedo-Medina TB, Warren MR, Johnson BT, Carey MP. Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: A meta-analysis, 1991 to 2010. Journal of Acquired Immune Deficiency Syndromes. 2011;58:489–498. doi: 10.1097/QAI.0b013e31823554d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somlai AM, Kelly JA, McAuliffe TL, Gudmundson JL, Murphy DA, Sikkema KJ, Hackl KL. Role-play assessments of sexual assertiveness skills: Relationships with HIV/AIDS sexual risk behavior practices. AIDS and Behavior. 1998;2:319–328. doi: 10.1023/a:1022622108917. [DOI] [Google Scholar]
- Troth A, Peterson CC. Factors predicting safe-sex talk and condom use in early sexual relationships. Health Communication. 2000;12:195–218. doi: 10.1207/s15327027hc1202_5. [DOI] [PubMed] [Google Scholar]
- Widman L, Noar SM, Choukas-Bradley S, Francis DB. Adolescent sexual health communication and condom use: A meta-analysis. Health Psychology. 2014;33:1113–1124. doi: 10.1037/hea0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior. 2000;27:539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Robinson-Simpson L, Lang DL, Caliendo A, Hardin JW. Efficacy of an HIV intervention in reducing high-risk HPV, non-viral STIs, and concurrency among African-American women: A randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes (1999) 2013;63:S36–S43. doi: 10.1097/QAI.0b013e3182920031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, Hunter-Gamble D, DiClemente RJ. A pilot study of sexual communication and negotiation among young African American women: Implications for HIV prevention. Journal of Black Psychology. 1993;19:190–203. doi:s10.1177/00957984930192008. [Google Scholar]