Abstract
Background:
Subdural empyema is a rare form of intracranial infection. It is described as accumulation of purulent infective material between the inner layer of dura mater and outer layer of arachnoid membrane.
Case Description:
A 17-year-old girl was admitted to the emergency department with acute left hemiplegia and was diagnosed with interhemispheric subdural empyema that showed a three-fold increase in size within 12 hours. Complete recovery was achieved with emergency surgical evacuation and additional 3 weeks of antibiotic treatment.
Conclusion:
Subdural empyema should be diagnosed and managed early in time since it may progress very rapidly and can cause high morbidity and mortality. Complete recovery can be achieved if it is diagnosed early and treated in time.
Keywords: Increase in size, interhemispheric, rapidly progressing, subdural empyema
INTRODUCTION
Subdural empyema is an intracranial infection characterized by the accumulation of infective material between the inner layer of dura mater and outer layer of arachnoid membrane.[1,6] Subdural empyema accounts for 15–25% of all intracranial infections.[8,9] It may develop secondary to infections of the middle ear and paranasal sinuses. Subdural empyema may also occur as a complication of brain abscesses and cranial operations that involve paranasal sinuses.[3,4,12]
Timely diagnosis and treatment of subdural empyema is very essential since it can progress very rapidly and can cause severe neurological impairment. Full recovery can be achieved when it is diagnosed and treated in time.[4,5,13] Any delay in the diagnosis or management may result in considerable morbidity and mortality.[5] Here, we report the case of a 17-year-old girl admitted to the emergency department with acute hemiplegia who was diagnosed with interhemispheric subdural empyema that showed a three-fold increase in size within 12 hours of admission.
CASE REPORT
A 17-year-old girl was admitted to the emergency department with the complaint of rapidly progressing weakness of her left arm and leg. Her medical history was unremarkable other than a history of intermittent sessions of antibiotic treatment for sinusitis. Her physical examination revealed a temperature of 37.6°C, pulse of 96, respiratory rate of 14, blood pressure of 118/74 mmHg, and an oxygen saturation of 100% on room air. Her head and neck examination demonstrated no sign of meningeal irritation, but showed sinus tenderness. She had left hemiplegia with a Glasgow coma score of 15 and normal pupillary examination.
Laboratory examination revealed elevated erythrocyte sedimentation rate (80 mm/h), a high level of C-reactive protein (7.8 mg/L), with 16 × 109/L white blood cells and 84% neutrophils. Cranial computed tomography (CT) and cranial magnetic resonance imaging (MRI) scans of the patient revealed interhemispheric subdural empyema and accompanying frontal and paranasal sinusitis [Figure 1a–f]. At the 12th hour of admission, during observation in the inpatient clinic, she had a tonic-clonic seizure lasting for 2 minutes. She was taken to the intensive care unit, an anticonvulsive was started, and a new cranial CT scan was taken. This cranial CT scan revealed interhemispheric subdural empyema with a three-fold increase in size within 12 hours compared to the CT taken on admission [Figure 2].
Figure 1.
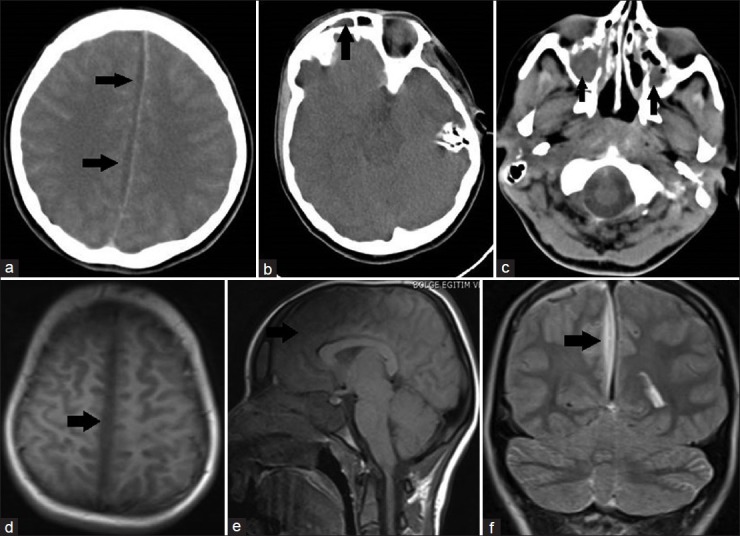
(a) Contrast-enhanced cranial axial computed tomography (CT) scan immediately taken on admission reveals interhemisferic subdural empyema indicated with black arrows. (b) On cranial axial CT scan immediately taken on admission, black arrow indicates frontal sinusitis. (c) On cranial axial CT scan immediately taken on admission, black arrows indicate bilateral paranasal sinusitis. (d) Cranial T-1 weighted axial magnetic resonance imaging (MRI) scan taken on admission reveals interhemisferic subdural empyema indicated with black arrow. (e) Cranial T-1 weighted sagittal MRI scan taken on admission reveals interhemisferic subdural empyema indicated with black arrow. (f) Cranial T-2 weighted coronal MRI scan taken on admission reveals interhemisferic subdural empyema indicated with black arrow
Figure 2.
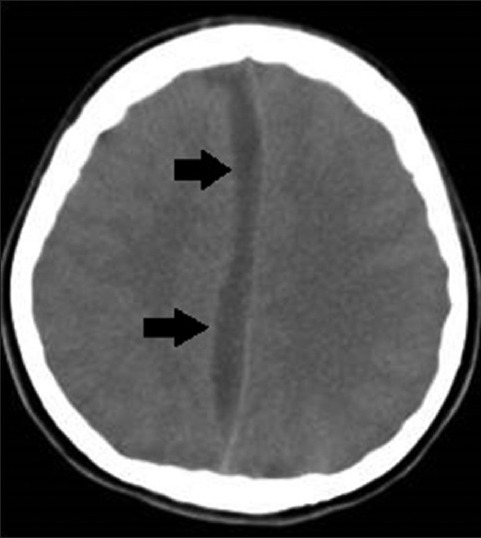
On cranial axial computed tomography scan taken following seizure, at the 12th hour of admission, reveals a 3-fold increase in the preexisting interhemisferic subdural empyema, indicated with black arrows
The patient was immediately taken to the operating theatre and subdural empyema was evacuated via parasagittal interhemispheric approach. Bone flap was not repositioned because it was seen to be contaminated with the infective material. Postoperative CT scan of the patient revealed that the empyema had been evacuated successfully [Figure 3]. Ceftriaxone (at a dose of 100 mg/kg/day), metronidazole (at a dose of 7.5 mg/kg every 6 hours), and vancomycin (at a dose of 15 mg/kg every 6 hours) were given empirically for 3 weeks. No microbial yield was detected in the culture of the material evacuated from interhemispheric subdural space. After 3 weeks of antibiotic treatment and close observation, clinical and laboratory examinations of the patient confirmed successful treatment of empyema, and the patient was discharged from the hospital with no neurological deficit.
Figure 3.

Postoperative cranial axial computed tomography scan reveals successful evacuation of interhemispheric subdural empyema. White arrow indicates the right parasagittal craniotomy defect
DISCUSSION
The most common causes of subdural empyema are meningitis in children and otolaryngeal infections in adults.[2,7,9] History of trauma and cranial operations involving sinuses are other causes of subdural empyema. Subdural empyema should be considered in patients who have a history of meningitis, otolaryngeal infections, trauma, and cranial operations because they are predisposing factors for the development of subdural empyema.[5,12,13] In case of prolonged fever, convulsion, focal neurological deficit, or altered consciousness in such patients, the likelihood of subdural empyema should be kept in mind. The history of untreated sinusitis was the most probable risk factor in the etiology of subdural empyema in our case.
CT and MRI are the diagnostic tools of choice in subdural empyema.[1,7] Even though subdural empyema can usually be diagnosed with CT, the diagnosis may be overlooked in mild cases. They may mimic subdural hematoma in the early periods when capsulation has not been completed yet.[5,8] MRI has high sensitivity in the detection of small subdural empyemas and high specificity in differentiating subdural empyema from subdural effusion.[1] In our case, the diagnosis was made with CT scan whereas MRI was utilized for excluding other possible etiologies and for establishing an accurate surgical plan.
The goal of the treatment is the complete evacuation of the empyema and successful treatment of infection.[4,5,7] Medical therapy alone may be effective in selected cases. However, an additional antibiotic treatment regime is usually required following the surgical evacuation of empyema. When infections of the paranasal sinuses are considered in the etiology, antibiotic treatment should be covering both gram negative and gram positive bacteria. A broad-spectrum antibiotic regime was administered to our patient following surgery.[2,6,7,10] Because there was no microbial yield in cultures of our case, ceftriaxone, vancomycin, and metronidazole were administered empirically to cover both aerobic and anaerobic pathogens.
Debate still exists regarding the ideal surgical technique. Though successful results with burr-hole drainage have been reported, surgical evacuation via craniotomy is still the most commonly preferred technique.[1,4,13] Craniotomy has the advantages of wide exposure, complete evacuation of purulent material, and chance of reaching intracranial spaces that are nonviable with burr-hole.[7,8] Gordon et al.[3] reported better results in cases operated via craniotomy than the cases operated via burr-hole drainage. Our case was a rapidly progressive subdural empyema reaching a large size in a relatively short time. For this reason, we evacuated subdural empyema via a parasagittal craniotomy and achieved successful evacuation of empyema.
Because of improved diagnostic tools such as CT and MRI, early diagnosis and treatment has reduced the morbidity and mortality rates.[1,5,7] However, confirming the diagnosis may still be very difficult since the symptoms might be very mild at the beginning. Rapid diagnosis and management are very crucial in subdural empyema because timely diagnosis and management give the patient a chance of full recovery with little or no neurological impairment.[2,6] On the other hand, delayed establishment of the diagnosis may result in a dramatical outcome. In our case, the diagnosis was made early in time and rapid progression was detected on second cranial CT. Emergency evacuation of subdural empyema and additional antibiotic treatment resulted in the complete recovery of the patient.
CONCLUSION
It should be noted that subdural empyema may have a rapidly progressive course, reaching a relatively large size in a very short time. Nonetheless, subdural empyema can be treated with excellent results in case of early diagnosis and timely management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Mehmet O. Yüksel, Email: dr.onur_yksl@hotmail.com.
Mehmet S. Gürbüz, Email: mehmetsabrigurbuz@gmail.com.
Numan Karaarslan, Email: numikara@yahoo.com.
Tezcan Caliskan, Email: dtzcan_07@hotmail.com.
REFERENCES
- 1.Alvis Miranda H, Castellar-Leones SM, Elzain MA, Moscote-Salazar LR. Brain abscess: Current management. J Neurosci Rural Pract. 2013;4:67–81. doi: 10.4103/0976-3147.116472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bashir EF, Taha ZM. Challenges in the management of intracranial subdural empyema. Neurosurg Quart. 2003;13:198–206. [Google Scholar]
- 3.Gordon B, Bernard W, Smith S. Treatment of subdural empyema. J Neurosurg. 1991;55:82–8. doi: 10.3171/jns.1981.55.1.0082. [DOI] [PubMed] [Google Scholar]
- 4.Maniglia AJ, Goodwin WJ, Arnold JE, Ganz E. Intracranial abscesses secondary to nasal, sinus, and orbital infections in adults and children. Arch Otolaryngol Head Neck Surg. 1989;115:1424–9. doi: 10.1001/archotol.1989.01860360026011. [DOI] [PubMed] [Google Scholar]
- 5.Mauser HW, Van Houwelingen HC, Tulleken CA. Factors affecting the outcome in subdural empyema. J Neurol Neurosurg Psychiatry. 1987;50:1136–41. doi: 10.1136/jnnp.50.9.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menon S, Bharadwaj R, Chowdhary A, Kaundinya DV, Palande DA. Current epidemiology of intracranial abscesses: A prospective 5 year study. J Med Microbiol. 2008;57:1259–68. doi: 10.1099/jmm.0.47814-0. [DOI] [PubMed] [Google Scholar]
- 7.Nathoo N, Nadvi SS, Narotam PK, Van Dellen JR. Brain Abscess: Management and Outcome Analysis of a Computed Tomography Era Experience with 973 Patients. World Neurosurg. 2011;75:716–26. doi: 10.1016/j.wneu.2010.11.043. [DOI] [PubMed] [Google Scholar]
- 8.Tewari MK, Sharma RR, Shiv VK, Lad SD. Spectrum of intracranial subdural empyemas in a series of 45 patients: Current surgical options and outcome. Neurol India. 2004;52:346–9. [PubMed] [Google Scholar]
- 9.Tsai YD, Chang WN, Shen CC, Lin YC, Lu CH, Liliang PC, et al. Intracranial suppuration: A clinical comparison of subdural empyemas and epidural abscesses. Surg Neurol. 2003;59:191–6. doi: 10.1016/s0090-3019(02)01054-6. [DOI] [PubMed] [Google Scholar]
- 10.Tsou TP, Lee PI, Lu CY Chang LY, Huang LM, Chen JM, et al. Microbiology and epidemiology of brain abscess and subdural empyema in a medical center: A 10-year experience. J Microbiol Immunol Infect. 2009;42:405–12. [PubMed] [Google Scholar]
- 11.Tummala RP, Chu RM, Hall WA. Subdural empyema in children. Neurosurgery Quart. 2004;14:257–65. [Google Scholar]
- 12.Wu TJ, Chiu NC, Huang FY. Subdural empyema in children–20-year experience in a medical center. J Microbiol Immunol Infect. 2008;41:62–7. [PubMed] [Google Scholar]
- 13.Yilmaz N, Kiymaz N, Yilmaz C, Bay A, Yuca SA, Mumcu C, et al. Surgical treatment outcome of subdural empyema: A clinical study. Pediatr Neurosurg. 2006;42:293–8. doi: 10.1159/000094065. [DOI] [PubMed] [Google Scholar]


