Abstract
Osteochondral lesions of the talus are common injuries that affect a wide variety of active patients. The majority of these lesions are associated with ankle sprains and fractures though several nontraumatic etiologies have also been recognized. Patients normally present with a history of prior ankle injury and/or instability. In addition to standard ankle radiographs, magnetic resonance imaging and computed tomography are used to characterize the extent of the lesion and involvement of the subchondral bone. Symptomatic nondisplaced lesions can often be treated conservatively within the pediatric population though this treatment is less successful in adults. Bone marrow stimulation techniques such as microfracture have yielded favorable results for the treatment of small (<15 mm) lesions. Osteochondral autograft can be harvested most commonly from the ipsilateral knee and carries the benefit of repairing defects with native hyaline cartilage. Osteochondral allograft transplant is reserved for large cystic lesions that lack subchondral bone integrity. Cell-based repair techniques such as autologous chondrocyte implantation and matrix-associated chondrocyte implantation have been increasingly used in an attempt to repair the lesion with hyaline cartilage though these techniques require adequate subchondral bone. Biological agents such as platelet-rich plasma and bone marrow aspirate have been more recently studied as an adjunct to operative treatment but their use remains theoretical. The present article reviews the current concepts in the evaluation and management of osteochondral lesions of the talus, with a focus on the available surgical treatment options.
Keywords: cartilage repair, repair, talus, ankle, joint involved, microfracture, procedures, autologous chondrocyte, grafts
Introduction
The understanding of osteochondral lesions of the talus has developed gradually over the past several centuries. Monro1 was the first to describe talar osteochondral injury when he removed loose fragments from an ankle in 1737. In 1888, König coined the term osteochondritis dissecans (OCD), referring to loose bodies within a knee joint that he believed to be secondary to avascular necrosis. It was not until 1922 when OCD was first described in the ankle by Kappis, and in 1924 Phemister proposed a traumatic etiology for such talar lesions, a hypothesis that was supported by Fairbank in 1933 and later in 1959 by Berndt and Harty.2
Our current definition of an osteochondral lesion (OCL) is any defect involving both the articular surface and the subchondral bone of the talus. This definition recognizes that there are a variety of etiologic pathways that result in similar lesions within the dome of the talus. Many of these lesions are associated with traumatic events and are prevalent within active populations.3 In fact, concomitant OCLs have been reported in approximately 50% to 73% of acute ankle injuries.4,5 Less frequent causes of OCLs include genetic predisposition, degenerative joint disease, joint malalignment, avascular necrosis, peripheral vascular disease, and endocrine or metabolic abnormalities.3 Treatment of osteochondral lesions of the talus has been traditionally difficult due to the limited healing potential of the talar articular surface and the massive forces transmitted through the ankle joint. However, during the past 10 to 15 years, significant advancements have been made in understanding the pathophysiology of osteochondral injury and modern surgical techniques have continued to evolve in an effort to provide a more durable and functional repair.
Anatomy and Pathophysiology
The talus has a unique anatomy in that the majority of its surface (approximately 60%) is covered with articular cartilage and it does not serve as a site of attachment for any muscle.6 The extensive articular surface limits access for incoming vascular supply and creates multiple watershed areas.7 This limited vascular supply has been implicated in the high risk of posttraumatic osteonecrosis and overall limited healing potential for osteochondral injuries of the talus.
The talus is divided into 3 distinct regions; the body, the neck, and the head. Classically, OCLs are described in the dome of the body of the talus. Elias et al.,8 designed an anatomic 9-zone grid on the articular surface of the talar dome to examine the specific location of osteochondral lesions. They found that most talar OCLs occurred in zone 4 (centromedial) and zone 6 (centrolateral). In a study of 500 patients with talar OCLs, Flick and Gould9 found that 98% of lateral lesions are associated with a traumatic event, most commonly ankle sprains. The proposed mechanism of injury is a shearing force on the dome when the ankle is forced into a dorsiflexed and inverted position. These traumatic lateral lesions tend to be shallower than their medial counterparts but present at a higher stage and have a higher risk for displacement. Alternatively, 70% of medial lesions are associated with an axial load while the ankle is forced into a plantarflexed and inverted position.
A number of etiologies have been proposed for the development of nontraumatic lesions and include vascular or synovial insult, soft-tissue impingement by an accessory anterior inferior tibiofibular ligament (Bassett’s ligament), microtrauma, and chronic ankle instability. König10 in his original description, hypothesized that nontraumatic lesions were the result of subchondral vascular occlusion leading to subsequent cystic changes eventually leading to fragmentation and displacement. Vascular disruption has also been proposed as a mechanism for the development of traumatic lesions. Whether the vascular insufficiency preexisted the injury or whether vascular disruption is caused by fragmentation is unclear. In either scenario, the vascular insufficiency is thought to limit the inherent potential for spontaneous healing.
Several systemic abnormalities have also been associated with the development of OCLs of the talus, including hypothyroidism, vitamin D deficiency, calcium and parathyroid abnormalities.3 In cases of nontraumatic lesions or in patients who have polyarticular disease, screening for endocrine abnormalities should be considered. Finally, systemic vasculopathy leading to localized avascular necrosis should always be considered in the differential diagnosis.
Clinical Presentation
Patients presenting with OCLs of the talus are often athletes or have a history of significant ankle trauma within 1 year of symptom onset. The majority of patients are 20 to 40 years old, with men being more commonly affected than women (1.6:1). Typically, patients will present with nonspecific ankle pain that may or may not correspond to the location of the lesion. Additionally, they will often complain of swelling and occasional joint instability. Mechanical symptoms of clicking and locking have been historically associated with osteochondral lesions of the talus; however, Loomer et al.11 reported that none of their cohort of 92 patients had mechanical symptoms as a presenting symptom indicating that mechanical complaints associated with talar OCLs are less common than previously thought.
Physical examination findings are often subtle, therefore it is important to compare the affected ankle to the contralateral side. Examination should begin with palpating the medial and lateral aspects of the talar dome when the ankle is maximally plantarflexed. Inversion and eversion with the ankle in both plantarflexion and dorsiflexion is necessary to elicit any clicking or catching that may be present.12 Local tenderness may not always be apparent and should not rule out the diagnosis. Minor limitations in range of motion of both the tibiotalar joint and the subtalar joint can be present. Patients with chronic OCLs may present with deep, intermittent pain in the ankle joint with weightbearing.13 While a thorough history and physical examination are necessary, the ambiguous nature of this clinical presentation makes plain radiographs, magnetic resonance imaging (MRI), and computed tomography (CT) scans critical components to making the appropriate diagnosis.
Diagnostic Imaging
The first-line imaging modality in the workup of talar OCLs are standard anteroposterior (AP), lateral, and mortise radiographs of the ankle joint. In the event that persistent effusion, delayed synovitis, locking or mechanical symptoms, and/or continued pain are still present 4 to 5 weeks after the initial injury, repeat radiographs are indicated. It may be useful to obtain an AP or mortise view with the foot in plantar flexion, as this allows for better visualization of the posterior talus. This technique is analogous to obtaining a tunnel view of the knee for an improved visualization of posterior condylar OCD lesions. A Canale view (15° pronation with the x-ray beam angled 75° cephalad), normally used to assess the talar neck, may also be useful to image the subchondral surfaces. The lack of identifiable lesion on x-ray does not exclude the diagnosis of talar OCL. Loomer et al.11 found that only 50% of lesions in their series could be seen on the original radiographs, while Hepple et al.14 reported that as many as 43% of talar OCLs identified on MRI were originally not visible on radiography.
CT scans often provide a more detailed visualization of the lesion and may demonstrate that a given defect is larger than initially thought based on plain radiographs. A CT scan is particularly useful in determining bone stock availability and in the identification and characterization of lesion-associated cysts.15 CT scans remain a valuable imaging modality in the evaluation of talar OCLs, especially with respect to preoperative planning.16
Although not utilized at all institutions, a bone scan has been demonstrated to be a valuable tool in the workup of osteochondral lesions. Loomer and colleagues11 cited 99% sensitivity when using technetium 99m bone scans in the diagnosis of talar OCLs. According to their imaging algorithm, if radiographs were negative in the setting of persistent symptoms, or if the condition remained undiagnosed, a bone scan was obtained to evaluate localization to the talus. The addition of SPECT-CT scanning (single photon emission computed topography) may aid in the identification of asymptomatic lesions by assessing actual metabolic changes within the bone. Therefore, SPECT-CT may be a helpful adjunct when multiple areas of pathology are detected on MRI.17
MRI is a useful modality in the identification of bone bruises, loose bodies, soft tissue pathology, and correlates reasonably well with arthroscopic findings.18 Demonstration of loose fragments is particularly valuable, since identification of such bodies directly affects treatment decision making. Additionally, MRI is able to identify early stage lesions, which may not be visible on plain radiographs. T2-weighted MRI is the preferred modality due to increased sensitivity to cartilage tissue and demonstration of the depth of cartilage lesions. Of note, some authors have suggested that MRI may overstate the severity of lesions due to variability in signal changes that occur after any acute ankle injury.8
Classification
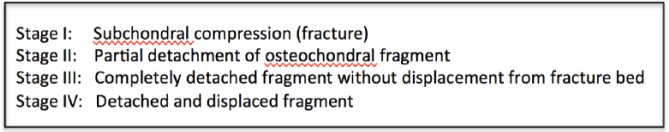
Many classification schemes for osteochondral lesions of the talus have been proposed with the Berndt and Harty2 classification being the earliest and most commonly used. It is a 4-stage classification that grades the lesion based on the appearance on plain radiographs and is focused on transchondral fractures ( Fig. 1 ). The main limitation of this classification is that, since its inception, advanced imaging techniques allow for detection of lesions that do not or are yet to have radiographic findings which makes them difficult to fit into the Berndt and Hardy classification system. This has prompted modern classifications based on CT, MRI, and arthroscopic characteristics.14,18-21 Several of these classification schemes have modified Berndt and Harty by adding a cystic subtype, which reflects the variation in etiologies that produce these lesions. Others have included evaluation of the articular surface as components of the classification.
Figure 1.
Berndt and Harty’s original classification of osteochondral lesions of the talus.
Several studies have attempted to correlate findings on imaging with arthroscopic evaluation of the articular surface. A study by Pritsch et al.21 demonstrated a poor correlation between plain radiographs and arthroscopic grading of the articular surface. Alternatively, a study by Mintz et al.20 found that MRI appearance corresponded well with evaluation of the articular surface during arthroscopy. However, when the evaluations did not coincide, the MRI tended to underestimate the severity of the lesion. Both of these studies underscore the importance of direct visualization of the lesion as a part of the algorithm determining the ultimate treatment of the lesion.
Management and Indications for Surgical Intervention
Nondisplaced OCLs are often initially treated with a nonoperative approach. Nonoperative treatment of OCLs includes activity modification, protected weightbearing, rehabilitation, bracing, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs).22,23 While this approach may lead to resolution in the pediatric population, this treatment is typically less successful in the adult population. This is mostly due to the inherent biologic properties of hyaline cartilage, namely its avascularity, which limit the healing potential of the articular surface. Clinically, a systematic review of OCLs of the talus by Verhagen et al.24 showed that among 201 patients in 14 studies, only 91 patients (45%) reported successful outcomes with nonoperative treatment.
Operative treatment is indicated in the acute setting when the lesion is displaced and in the more chronic setting when nonoperative treatment fails to improve patient symptoms and function. The specific operative techniques utilized vary based on clinical presentation, the location and characteristics of the lesion. With OCLs of the talus, surgical treatment generally involves repair or replacement of the damaged osteochondral unit. Bone marrow stimulation via drilling or microfracture is generally the primary treatment for smaller size lesions. Osteochondral grafting techniques (autograft or allograft) are often used for larger defects or in the case of failed prior curettage or drilling.22,25,26 More recently, cell-based repair techniques have been utilized in the management of talar OCLs, including autologous chondrocyte implantation and the use of juvenile chondrocytes.27-29 Biological agents such as bone marrow aspirate concentrate, platelet-rich plasma (PRP) therapy, and hyaluronic acid are increasingly being used to augment the repair process as well.30,31 While ample literature exists on many of these methods, indications and long-term results are still in question and will require further exploration as treatment options continue to evolve.
Bone Marrow Stimulation
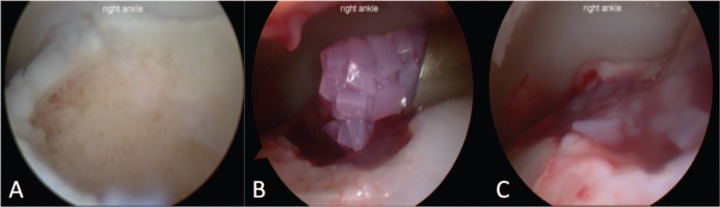
The principle behind bone marrow stimulation is to allow infiltration of mesenchymal stem cells at the site of the chondral defect. This can be done by microfracture or drilling. In microfracture, the subchondral plate is breached with a surgical awl in 3- to 4-mm intervals until the emergence of fatty droplets from the marrow is observed ( Fig. 2 ). Drilling induces the same process, using a surgical drill or wire. In both cases, a fibrin clot forms within the treated defect, initiating an inflammatory response and subsequent release of cytokines and growth factors to stimulate the healing process.32 As pluripotent marrow-derived mesenchymal stem cells migrate into the clot and begin to differentiate and proliferate, they form a fibrocartilaginous-type repair tissue with an extracellular matrix initially containing type II collagen (note that studies have shown an eventual transformation of this construct into scar tissue predominated by type I collagen with diminished levels of type II collagen).33 Bone marrow stimulation for the treatment of talar OCLs can be performed with minimally invasive techniques. It has a low complication rate, causes minimal postoperative pain, and may be less technically demanding than other techniques.32
Figure 2.
(A) Arthroscopic view of talar dome lesion after curettage. (B) The same lesion after bone marrow stimulation with microfracture.
Indications for bone marrow stimulation remain somewhat undefined to date. Microfracture for small OCLs (<15 mm) have primarily yielded favorable results in the literature. Chuckpaiwong et al.34 performed microfracture on 105 ankles, defining successful treatment as meeting 3 of the 4 following criteria: (1) more than 50% improvement in visual analog scale (VAS) score for pain during daily activities, (2) more than 50% improvement in VAS score for pain during exercise, (3) an AOFAS (American Orthopaedic Foot and Ankle Society) score that was increased by at least 30 points, and (4) a Roles and Maudsley score of 1 or 2. Of the 105 ankles treated, all 73 lesions smaller than 15 mm met the criteria for successful outcome. However, only 1/32 lesions greater than 15 mm met the criteria for success, and none of the 24 lesions greater than 20 mm were successful.34 Choi et al.25 similarly found that lesion size predicted outcome following the microfracture procedure. In their analysis of 120 ankles undergoing microfracture they found that lesion size greater than 150 mm2 portended poor outcomes. While treated lesions smaller than this threshold value had a failure rate of 10.5%, 80% of lesions greater than 150 mm2 met criteria for treatment failure.25 Lee et al.35 reported on 35 ankles (all patients younger than 50 years) that underwent microfracture of isolated talar lesions <1.5 cm2 at a mean follow-up of 33 months. According to AOFAS scores, 89% reported good or excellent outcomes, while 11% were reported as fair, with a mean AOFAS score improvement of 27 points and a mean reduction of 5 points on VAS pain assessment.35
While good results have been shown in young patients with small, isolated talar lesions, other studies have reported on patients with more advanced lesions, concomitant injuries, and a history of prior ankle surgery. At a mean follow-up of 26 months after microfracture for Outerbridge grade 3 and 4 cartilage lesions, Clanton et al.36 reported mean Lysholm and total FADI (Foot and Ankle Disability Index) scores of 74 and 81 (FADI ADL [activities of daily living] 81 and FADI Sport 62), respectively and reported mean patient satisfaction of 8 out of 10. This was significantly better than that seen in patients who had undergone prior ankle surgery (FADI total 51) and patients with a longer time between injury and surgery. Despite this, patient satisfaction was still high.
Longer term follow-up has been less predictable. While it has also been shown that positive short-term results are maintained at a mean of 5.8 years after surgery for both pain and functional scores, Ferkel et al. showed deterioration in 35% of patients at 5-year second look arthroscopy.37,38 This is significant because microfracture of the knee has been shown to have deteriorating results as early as 18 to 36 months postoperatively.39 While functional scores remain high in the short term and mid-term after microfracture of talar OCLs, we know that repair tissue and subchondral bone remain far from normal. Some recent studies have used advanced MRI protocols and second-look arthroscopy in evaluating postmicrofracture cartilage tissue and subchondral bone quality. While they demonstrated similar T2 properties when comparing repair tissue to normal cartilage, the degree of defect filling, quality of repair tissue, integration with surrounding tissue and the quality of the subchondral bone was inconsistent at best.40,41 Second-look arthroscopy confirmed the discrepancy between clinical outcome and quality of cartilage healing. Lee et al.42 demonstrated that 12 months after microfracture only 60% of lesions healed in a normal or near-normal state according to ICRS (International Cartilage Repair Society) grade and only 30% of lesions were completely integrated with surrounding healthy cartilage, despite 90% of patients reporting good or excellent AOFAS scores.
Overall, short- and mid-term results of microfracture of isolated, talar OCLs less than 150 mm2 are generally good. A systematic review by Donnenwerth and Roukis43 supports microfracture as a primary treatment of OCLs of the talus, as they found a mean AOFAS hindfoot score of 86.8 when evaluating 299 ankles from various studies, which translates to good or excellent outcomes in 80% of patients undergoing this procedure.
Recently, there has been interest in comparing chondral lesions and osteochondral lesions independently, with the idea being more advanced injury may predict worse outcomes. Surprisingly, this has not been demonstrated. Several studies have compared chondral and osteochondral lesions treated with microfracture, but no differences were discovered between the 2 groups at mid-term follow-up (2-8 years).5,44,45
Recent studies have attempted to augment OCL healing and improve patient outcomes following microfracture by injecting hyaluronan or autogenous cell-based modalities at the time of the index surgery, including PRP and mesenchymal stem cells. Though the series are limited in scope and their overall numbers are low, intra-articular injection with either hyaluronan, PRP or mesenchymal stem cells during surgery or within the short-term postoperative period demonstrated significant functional improvement in the short term regardless of the functional scoring system used.46-48 Despite these promising results, these studies contained weaknesses that limit broader application of this type of treatment augmentation. With further evaluation in greater numbers, intra-articular injections as a treatment augmentation may have utility in the management of OCLs.
Both intra-articular and retrograde drilling techniques have been described. This decision can be made intraoperatively based on the arthroscopic examination. When the lesion’s articular surface is intact a retrograde drilling technique is generally preferred so as not to violate the articular surface. A 1-cm incision is used to expose the lateral talar process and protect the peroneal tendons then drilling is done under fluoroscopic guidance. An anterior cruciate ligament–type aiming device can be used for arthroscopic targeting of the lesion. Computer-guided techniques have also been described and shown to be at least as accurate as traditional 2-dimensional fluoroscopic techniques.49 Drilling or microfracture with an awl can be done with the foot plantar flexed. Transmalleolar drilling can be used for lesions that are not accessible. A single outside-in technique with a 1.25 wire can access a larger area if the talus is dorsi and plantar flexed to accommodate the wire for each successive hole in the talus. This technique can reduce the number of iatrogenic perforations in the tibial cartilage needed to access the lesion.
Osteochondral Grafting Techniques
In contrast to bone marrow stimulation, osteochondral grafting techniques are generally indicated for large primary OCLs. These grafts can either be autologous or come from a cadaveric donor and can be implanted as a single or as multiple plugs (mosaicplasty). The goal of autologous transplantation is to implant a graft that is similar in both mechanical and biological properties to that of the patient’s native hyaline cartilage.23 Autologous grafts are most commonly harvested from the ipsilateral knee, specifically from the lateral femoral condyle or the intercondylar notch.30 The primary concern with osteochondral autograft transfer is donor site morbidity, as reported by several studies.50-52
Several retrospective case series have demonstrated positive results with osteochondral autograft transfer. Imhoff et al.53 observed significant long-term improvements in mean AOFAS, VAS, and Tegner activity scores in 26 patients (all with ICRS type 4a or 4b OCLs, less than 3 cm2 in size). At a mean follow-up time of 7 years, 18 patients indicated they were very satisfied with the procedure, 4 satisfied, 3 neutral, and 1 moderately unsatisfied.53 Similar improvements in the short-term have been reported in other studies in the literature, with average lesion sizes of 1.5 cm2.30,54 Scranton et al.55 reported that 45 of 50 patients with cystic talar defects receiving autologous osteochondral grafts had good or excellent Karlsson-Peter ankle scores at a mean follow-up time of 36 months. Only 1 patient was treated for pain at the donor site, 12 weeks after surgery, and symptoms resolved after surgical debridement of scar tissue.55
In addition to assessing clinical outcomes, several studies have utilized second-look arthroscopy to evaluate graft condition and incorporation at follow-up. In 2003, Lee et al.56 reported 100% good or excellent outcomes in 18 Berndt and Harty type III and IV OCLs treated with osteochondral autograft mosaicplasty from the ipsilateral knee at a mean follow-up of 36 months. Second-look arthroscopy was performed in 16 of 18 patients, which demonstrated graft consistency and congruity in 14 of 16. Only 2 grafts demonstrated chondral softening or fissuring. These results may have been positively affected by the low mean patient age (22.7 years) and small mean lesion size (13.6 mm × 7.2 mm). Another study by Baltzer and Arnold57 presented outcomes with second-look arthroscopy in 43 patients with a mean age of 31.2 years with variable follow-up periods out to 2 years. Second-look arthroscopy at 6 to 9 months postprocedure revealed good integration in single-plug transplantation and incomplete filling defects in gaps between grafts in mosiacplasty at 1 year. In selected cases, needle biopsies were taken and demonstrated hyaline cartilage structure of the graft. Clinically, improvements in pain scores, range of motion, and functional outcome scores were reported. Young, athletic patients who underwent an anterior approach with a single graft were noted to have the best results in this series.
To date, as reviewed by Hannon et al.23 there is only one known prospective randomized study involving osteochondral autograft transfer system (OATS). The study included 33 ankles with a mean follow-up time of 53 months. Eleven ankles were treated with chondroplasty, 10 with microfracture, and 12 with OATS. Pain and functional scores improved, but no significant differences in Ankle-Hindfoot Scale scores at 12 and 24 months or Subjective Assessment Numeric Evaluation (SANE) rating were observed between the treatment groups. Numeric Pain Intensity (NPI) 24 hours postoperatively was significantly lower for microfracture and chondroplasty than for OATS (P < 0.001), a factor that could be useful when advising patients about the early postoperative period.58
In addition to larger lesions, osteochondral autografts have been used as a salvage procedure after failed operative treatment of an OCL. Kreuz et al.59 evaluated autograft transplantation from the ipsilateral talus in a cohort of patients who failed operative management of an OCL. They found significant improvement in AOFAS scores in all 35 patients at a mean of 4 years postoperatively.59 This group also found significant differences in subgroups treated with no osteotomy, malleolar osteotomy or tibial wedge osteotomy (novel technique at the time), reporting scores of 94.1, 84.7, and 88.6 respectively. Postoperative MRI at 1 and 2 years demonstrated good graft integration and a congruent articular surface in all but 1 patient. They concluded that patients with well-integrated grafts, well-healed osteotomies, and good joint function can maintain good results over longer term follow-up. Therefore, monitoring of graft incorporation during the initial postoperative period is essential. They note that participation in weightbearing too early postoperatively may cause motion at the subchondral bed and is a potential cause for graft failure.
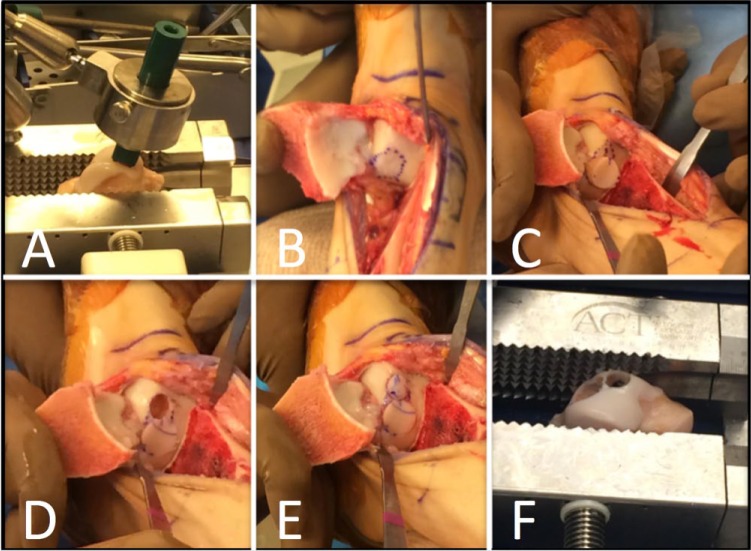
Allografts can also be used to treat larger OCLs ( Fig. 3 ), and they have several advantages to autografts. Use of an allograft allows the surgeon to avoid harvesting the graft from an asymptomatic site (such as the knee). A single dowel of cartilage and bone can often be used as opposed to multiple grafts with the OATS procedure, and the allograft can usually be manipulated to meet highly specific sizing requirements. Several types of graft exist and are characterized by their methods of storage. Frozen and fresh-frozen allograft has been used in the past, but has been shown to have a low chondrocyte viability rate (20%-30%) with an unacceptably high failure rate.60-62 Therefore, fresh allografts are now more commonly used. Typically grafts are harvested and stored in lactated ringers or culture medium and implanted within 7 days. Refrigerated grafts have been found to have 67% chondrocyte viability at 30 days.63 In addition, using an allograft can be very time consuming. Allograft use for implantation is a highly technical process and requires additional skill and time in the operating room. Using allograft is also a more expensive procedure than an autograft and there is a small risk of disease transmission.23
Figure 3.
Intraoperative photographs of a failed debridement and microfracture for a large talar dome lesion. (A) A size-matched cadaveric talus is secured within a transplant vice. (B) After medial malleolar osteotomy the lesion is circumscribed and sized for allograft. (C) The larger allograft plug is placed first and the remaining lesion is circumscribed for second plug using the “snowman” technique. (D) The talus is prepared for the second plug. (E) Both plugs have been press-fit into the defect. (F) The cadaveric talus after donation of both osteochondral plugs.
Gross et al.64 report good long-term results using allograft procedures on talar OCLs that are at least 1 cm in diameter. Nine patients with stage IV Berndt and Harty OCLs were followed for a mean of 12 years postoperatively. Three patients required ankle fusion following the initial allograft, so for the 6 patients remaining with the allograft in situ at the time of the study, all of them reported functional range of motion, no use of assistive devices, and minimal swelling. Only 1 of the 6 patients described mild pain, the other 5 reported no pain symptoms. Five patients reported full return to activities and 1 reported only mild restrictions in activities. All 6 indicated that they were satisfied with the results at a mean of 9 years after the procedure.64 Kwak et al.28 demonstrated similar improvement in their case series with the use of ACI for these lesions. However, their average follow-up was 70 months. Longer term study of ACI will be needed to truly compare the 2 procedures.
El-Rashidy et al.65 used fresh osteochondral allografts in 42 ankles (38 patients with OCLs, average lesion size of 1.5 cm2) and evaluated AOFAS and VAS scores at a mean follow-up time of 37.7 months. Seven of 38 patients required secondary arthroscopic surgery following the procedure, and 4 of the 42 grafts failed. Mean VAS scores decreased from mean of 8.2 points preoperatively to 3.3 points at final follow-up (P < 0.001). Mean AOFAS scores significantly improved from 52.3 preoperatively to 78.8 postoperatively (P < 0.001). Overall, at final follow-up, patient satisfaction was reported excellent, very good, or good in 73% of patients, and fair or poor by only 27%. Postoperative MRI was reported in 15 of these patients at an average of 33 months after surgery. Of these 15 patients, graft incorporation was rated as fair or poor in 12, signs of graft instability were seen in 5, and graft subsidence was found in 1 patient. Ten of the 15 had good articular congruity with 4 having slightly irregular cartilage contact. It is unclear whether poorer MRI results portends a poorer clinical outcome.65
In a study by Görtz et al.66 involving OCLs treated with fresh allografts, only 2 of 12 grafts failed, with a mean follow-up time of 38 months. Of the 10 that did not, Olerud-Molander Ankle Scores increased from a mean of 28 points preoperatively to 71 points postoperatively. Five of 10 patients with nonfailed ankles reported good or excellent results at follow-up. Radiographic imaging (available for 5 of the total 12 ankles) demonstrated 25% joint space narrowing in only 1 ankle and preserved space in the remaining 4. Eighty percent of patients reported less pain and 60% reported improved function.66
While outcomes can be good for patients after allograft transplantation, it is still not a perfect solution to the problem. At an average follow-up time of 48 months for 13 patients, Hahn et al.67 showed increased AOFAS scores from a mean of 45 preoperatively to 81 postoperatively (average lesion size of 2.67 cm2). All patients were able to return to previous activities within 1 year of surgery, and all patients reported satisfaction with the surgery. However, in contrast to the study by Görtz et al., radiographs revealed the presence of osteophytes in all but 1 patient with additional mild arthritic changes in two patients. CT scanning revealed less than 50% healing in 2 of the patients, suggesting that on some level, allografts may just be delaying the inevitable.67 Similarly, in a study by Raikin et al.,68 AOFAS scores averaged 38 points before allograft surgery and increased to 83 points postoperatively (P < 0.05) at a mean follow-up of 54 months. Preoperative VAS scores averaged 8.5, and postoperatively 3.3 at final follow-up. Again, 10 of 15 ankles demonstrated bone resorption or collapse of the graft, and joint space narrowing was seen in 9 ankles. Two of the 15 had required an arthrodesis, but 11 patients reported excellent or good outcomes, and all 15 were glad they had the procedure and would repeat it.68
Allograft transplants for OCLs of the talus have proven to be clinically effective, and most patients seem to be pleased with the results. While they help restore joint function, alleviate pain, and allow patients to return to previous activities, it should be noted that they do not completely halt the development of degenerative arthritic changes.
Cell-Based Repair Techniques: Autologous Chondrocyte Implantation and Juvenile Chondrocyte Implantation
One of the great concerns with bone marrow stimulation and osteochondral grafts is the ability of these procedures to fully match the repair tissue to the original articular surface. Hyaline cartilage is composed primarily of water, type II collagen, and various glycosaminoglycans and proteoglycan. The repair tissue formed by microfracture or drilling is fibrocartilaginous in nature, containing more type I than type II collagen. Osteochondral grafts provide intact cartilage with preserved architecture, but achieving anatomic congruence, graft incorporation, and complete healing can be difficult. The principle behind cell-based treatment approaches is the ability of transplanted chondrocytes to generate a hyaline-like repair tissue with biochemical and biomechanical properties closer to the native articular tissue.
Autologous chondrocyte implantation (ACI) is a 2-stage procedure in which chondrocytes are harvested during the initial procedure, expanded in culture, and then reimplanted to the defect in a second procedure. There are several technical options for this procedure. At the initial procedure chondrocytes may be harvested from the knee, the ankle or, in some cases, a detached osteochondral fragment. During reimplantation, several coverage materials have been used. In the original description by Brittberg et al.,69 periosteum was used to cover the implanted cells. However, due to issues with graft hypertrophy, a collagen I/III membrane has been developed. In a study comparing the 2, Gooding et al.70 found similar clinical and arthroscopic results for the 2 types of covers. However, they found a significant difference in the complications. Twelve percent of patients required unplanned arthroscopy for graft hypertrophy, compared with 2.9% in the collagen group. Therefore, collagen has become the preferred method of covering the implanted chondrocytes. Also of note, biopsies were taken at second-look arthroscopy 1 year later in 13 patients with collagen covers. Of these 13 patients, 3 showed only hyaline cartilage, 6 showed both hyaline and fibrocartilage, and 4 showed fibrocartilage alone. Similar results were seen in the perisosteum covered group.
Clinically, studies have reported positive outcomes using this technique.71,72 At a mean follow-up of 26 months for 8 patients, Giannini et al.72 reported no complications after this procedure. Mean AOFAS scores improved from 32.1 points preoperatively to 80.6 at 6 months, 90 at 12 months, and 91 at 24 months (mean lesion size was 3.3 cm2). Gross examination showed a cartilage covering in the graft area in every ankle, and histological analysis revealed positive staining for type II collagen and proteoglycan in the extracellular matrix for all specimens.72 Battaglia et al.71 reported similar improvements in mean AOFAS scores for 20 patients, at a longer follow up time of 5 ± 1 years (mean lesion size 2.7 ± 1 cm2). In an effort to correlate clinical scores with MRI, they used T2 mapping and the MOCART (magnetic resonance observation of cartilage repair tissue) score to evaluate the repair constructs. While they found no statistically significant correlations between the 2 scores, they did note that 2 patients who had less defect filling had the lowest clinical scores.71
Matrix-associated chondrocyte implantation (MACI) involves culturing the harvested chondrocytes on collagen or hyaluronic acid–based matrices prior to implantation. Advantages of this method include a more even distribution of the chondrocytes at the implant, avoidance of dedifferentiation of chondrocytes, and the lack of need for a covering layer. Clinical and imaging studies have showed promising results after MACI for OCLs of the talus.73-75 Magnan et al.74 reported results for 30 ankles with a mean lesion size 2.36 cm2, treated with the MACI technique utilizing a collagen-based matrix. At an average follow-up time of 45 months, mean AOFAS scores had improved from 36.9 preoperatively to 83.9 postoperatively. Good to excellent results were reported by 28 of 30 patients, and postoperative MOCART scores revealed improved integration of the graft at the articular surface.74
Giannini et al.73 used a hyaluronic acid–based matrix for MACI in 46 patients with a mean lesion size of 1.6 cm2. Mean preoperative AOFAS scores were 57.2, improving to 86.8 at 12-month follow-up and 89.5 at 36-month follow-up (P < 0.0005). 82.5% of patients (38/46) reported excellent or good results at 36 months, with only 5% of patients reporting poor results. Twenty patients were able to resume their normal level of sports, and only 4 were forced to give up athletic activity. A significant negative correlation was found between age and AOFAS score at the 36-month follow-up, as well as in patients with a previous history of other surgical interventions to treat these lesions.73
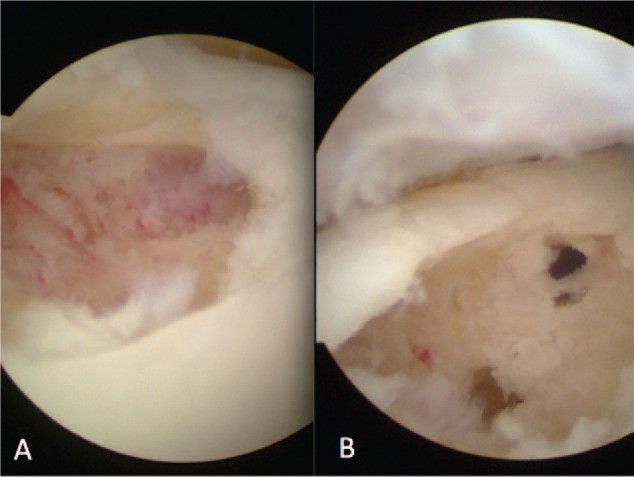
Minced or particulated articular cartilage obtained from juvenile allograft donors is an alternative source of chondrocytes used for implantation into OCLs. Juvenile grafts have shown increased density of chondrocytes and the ability to escape the extracellular matrix to form a new hyaline-like cartilage when compared with adult grafts. DeNovo NT is one type of graft utilizing this technique and has recently become a popularized technique for managing OCLs. The main benefit of this graft is that it provides an off-the-shelf product with the ability to manage the lesion in one procedure. Additionally, this graft only requires fibrin glue without the need for a biologic cover ( Fig. 4 ). One case study exists using DeNovo NT for 7 mm × 5 mm OCL lesion in the talus. At 2-year follow-up, the patient is reported to be pain free without limitation in activity. There currently are no published studies on DeNovo NT use in patients with symptomatic OCLs.76,77
Figure 4.
(A) Arthroscopic view of talar dome osteochondral lesion after curettage. (B) Placement of particulated juvenile cartilage into defect. (C) The transplanted cartilage layer is coated in fibrin glue and adhered to bed of defect.
Biological Agents
Some authors have discussed the use of biologic agents such as bone marrow aspirate concentrate (BMAC), hyaluronic acid, and PRP to treat OCLs of the talus.30,31,78,79 Animal studies have demonstrated the efficacy of PRP80-82 and hyaluronic acid83,84 in chondrocyte growth and differentiation, but clinical studies are not as well represented in the literature as the previously discussed operative treatments.
Fortier et al.79 demonstrated improved healing of full thickness cartilage defects with the use of BMAC in conjunction with microfracture compared with microfracture alone in an equine model. Kennedy and Murawski30 treated 72 ankles using a combination of OATS and BMAC, and while clinical results were positive (improved Foot Ankle Outcome scores), the lack of a control group in this study makes it difficult to draw a meaningful conclusion about the impact of BMAC alone on the healing process.
In a randomized, controlled clinical trial by Doral et al.,46 weekly postoperative hyaluronic acid injections following microfracture surgery were found to correlate with significantly higher AOFAS scores for patients at a 2-year follow-up than those just treated with microfracture. Furthermore, PRP may prove even more useful than hyaluronic acid, as Mei-Dan et al.31 showed significantly more improved VAS stiffness scores, VAS function scores, and Ankle-Hindfoot Scales in treatment of 33 OCLs of the talus by PRP instead of hyaluronic acid.
Allograft materials have also been utilized in combination with some of the previously mentioned biologics. In particular, a recent case report was published utilizing a micronized allograft cartilage matrix (biocartilage) combined with autologous blood solution and marrow stimulation. The patient was kept nonweightbearing for 6 weeks following the procedure and was noted to return to high-impact and full athletic activity by 3 months. The patient was reported at most recent follow-up of 15 months to be asymptomatic.85 A similar procedure has been utilized at our institution with the combination of PRP with biocartilage.
Conclusion
Treatment for osteochondral lesions of the talus continues to improve as studies have demonstrated increasing clinical efficacy. Nonoperative treatment is the ideal primary protocol, with the hope that patients will be able to regain function and shed painful symptoms in order to return to daily activities. However, the lackluster healing properties of articular cartilage have rendered non-operative treatment limited in its power at best, and operative treatment has become increasingly common. Microfracture, drilling, and other bone marrow stimulating techniques yield positive results for smaller lesions, and autologous and cadaveric bone grafts may be necessary for failed bone marrow stimulation procedures or larger lesions. Other methods remain in their early developmental stages. Cell-based repair strategies have sparked interest among scientists and clinicians, but clinical applications and substantial studies are still lacking. PRP and hyaluronate therapy have also shown promise as useful therapy down the road. With the large incidence of ankle trauma and an increasing demand for the proper treatment of OCLs, operative techniques are continuing to evolve in hopes of improving pain and function while effectively halting degenerative arthritic changes in the ankle.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Monro A. Part of the cartilage of the joint separated and ossified. Medical Essays and Observations. 2nd ed. Edinburgh, Scotland: Ruddimans; 1737. [Google Scholar]
- 2. Berndt A, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41:988-1020. [PubMed] [Google Scholar]
- 3. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38(2):392-404. [DOI] [PubMed] [Google Scholar]
- 4. Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg. 2009;91(2):333-9. [DOI] [PubMed] [Google Scholar]
- 5. Saxena A, Eakin C. Articular talar injuries in athletes results of microfracture and autogenous bone graft. Am J Sports Med. 2007;35(10):1680-7. [DOI] [PubMed] [Google Scholar]
- 6. Shakked R, Tejwani N. Surgical treatment of talus fractures. Orthop Clin North Am. 2007;44(4):521-8. [DOI] [PubMed] [Google Scholar]
- 7. Lomax A, Miller RJ, Fogg QA, Jane Madeley N, Senthil Kumar C. Quantitative assessment of the subchondral vascularity of the talar dome: a cadaveric study. Foot Ankle Surg. 2014;20(1):57-60. [DOI] [PubMed] [Google Scholar]
- 8. Elias I, Jung JW, Raikin SM, Schweitzer MW, Carrino JA, Morrison WB. Osteochondral lesions of the talus: change in MRI findings over time in talar lesions without operative intervention and implications for staging systems. Foot Ankle Int. 2006;27(3):157-66. [DOI] [PubMed] [Google Scholar]
- 9. Flick A, Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial done lesions. Foot Ankle Int. 1985;5(4):165-85. [DOI] [PubMed] [Google Scholar]
- 10. König F. On the presence of loose bodies in joints. Deutche Z Chir. 1888;27:90-109. [Google Scholar]
- 11. Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993;21(1):13-9. [DOI] [PubMed] [Google Scholar]
- 12. Scranton P. Osteochondral lesions of the talus. In Nunley JA, Pfeffer GB, Sanders RW, Trepman E, editors.Advanced reconstruction foot and ankle. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2004. p. 261-5. [Google Scholar]
- 13. Verhagen R, Maas M, Dijkgraaf MG, Tol JL, Krips R, van Dijk CN. Prospective study on diagnostic strategies in osteochondral lesions of the talus: is MRI superior to helical CT? J Bone Joint Surg Br. 2005;87(1):41-6. [PubMed] [Google Scholar]
- 14. Hepple S, Winson I, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999;20(12):789-93. [DOI] [PubMed] [Google Scholar]
- 15. Davies A, Cassar-Pullicino V. Demonstration of osteochondritis dissecans of the talus by coronoal computer tomographic arthrography. Br J Radiol. 1989;62(744):1050-5. [DOI] [PubMed] [Google Scholar]
- 16. Zinman C, Wolfson N, Reis N. Osteochondritis dissecans of the dome of the talus. Computed tomography scanning in diagnosis and follow-up. J Bone Joint Surg Am. 1988;70(7):1017-9. [PubMed] [Google Scholar]
- 17. Mohan H, Gnanasegaran G, Vijayanathan S, Fogelman I. SPECT/CT in imaging of foot and ankle pathology—the demise of other coregistration techniques. Semin Nucl Med. 2010;40(1):41-51. [DOI] [PubMed] [Google Scholar]
- 18. Dipaola J, Nelson D, Colville M. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7(1):101-4. [DOI] [PubMed] [Google Scholar]
- 19. Ferkel RD, Sgaglione N. Arthroscopic treatment of osteochondral lesions of the talus: long-term results. Orthop Trans. 1994;17:1011. [DOI] [PubMed] [Google Scholar]
- 20. Mintz D, Tashjian GS, Connell DA, Deland JT, O’Malley M, Potter HG. Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy. 2003;19(4):353-9. [DOI] [PubMed] [Google Scholar]
- 21. Pritsch M, Horoshovski H, Farine I. Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1986;68(6):862-5. [PubMed] [Google Scholar]
- 22. Amendola A, Panarella L. Osteochondral lesions: medial versus lateral, persistent pain, cartilage restoration options and indications. Foot Ankle Clin. 2009;14(2):215-27. [DOI] [PubMed] [Google Scholar]
- 23. Hannon C, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014;96(2):164-71. [DOI] [PubMed] [Google Scholar]
- 24. Verhagen RA, Struijs PA, Bossuyt PM, van Dijk CN. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003;8(2):233-42. [DOI] [PubMed] [Google Scholar]
- 25. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974-80. [DOI] [PubMed] [Google Scholar]
- 26. Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):238-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giza E, Delman C, Coetzee JC, Schon LC. Arthroscopic treatment of talus osteochondral lesions with particulated juvenile allograft cartilage. Foot Ankle Int. 2014;35:1087-94. [DOI] [PubMed] [Google Scholar]
- 28. Kwak S, Kern BS, Ferkel RD, Chan KW, Kasraeian S, Applegate GR. Autologous chondrocyte implantation of the ankle: 2- to 10-year results. Am J Sports Med. 2014;42(9):2156-64. [DOI] [PubMed] [Google Scholar]
- 29. Nam EK, Ferkel RD, Applegate GR. Autologous chondrocyte implantation of the ankle: a 2- to 5-year follow-up. Am J Sports Med. 2009;37(2):274-84. [DOI] [PubMed] [Google Scholar]
- 30. Kennedy JG, Murawski CD. The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate surgical technique. Cartilage. 2011;2(4):327-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, Nyska M. Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med. 2012;40(3):534-41. [DOI] [PubMed] [Google Scholar]
- 32. Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013;95(11):1045-54. [DOI] [PubMed] [Google Scholar]
- 33. Bae DK, Yoon KH, Song SJ. Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy. 2006;22(4):367-74. [DOI] [PubMed] [Google Scholar]
- 34. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24(1):106-12. [DOI] [PubMed] [Google Scholar]
- 35. Lee KB, Bai LB, Chung JY, Seon JK. Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):247-53. [DOI] [PubMed] [Google Scholar]
- 36. Clanton TO, Johnson NS, Matheny LM. Outcomes following microfracture in grade 3 and 4 articular cartilage lesions of the ankle. Foot Ankle Int. 2014;35(8):764-70. [DOI] [PubMed] [Google Scholar]
- 37. Becher C, Driessen A, Hess T, Longo UG, Maffulli N, Thermann H. Microfracture for chondral defects of the talus: maintenance of early results at midterm follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):656-63. [DOI] [PubMed] [Google Scholar]
- 38. Ferkel RD, Zanotti RM, Komenda GA, Sgaglione NA, Cheng MS, Applegate GR, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750-62. [DOI] [PubMed] [Google Scholar]
- 39. Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14(11):1119-25. [DOI] [PubMed] [Google Scholar]
- 40. Becher C, Zühlke D, Plaas C, Ewig M, Calliess T, Stukenborg-Colsman C, et al. T2-mapping at 3 T after microfracture in the treatment of osteochondral defects of the talus at an average follow-up of 8 years. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2406-12. [DOI] [PubMed] [Google Scholar]
- 41. Kuni B, Schmitt H, Chloridis D, Ludwig K. Clinical and MRI results after microfracture of osteochondral lesions of the talus. Arch Orthop Trauma Surg, 2012. 132(12): p. 1765-71. [DOI] [PubMed] [Google Scholar]
- 42. Lee KB, Bai LB, Yoon TR, Jung ST, Seon JK. Second-look arthroscopic findings and clinical outcomes after microfracture for osteochondral lesions of the talus. Am J Sports Med. 2009;37(suppl 1):63S-70S. [DOI] [PubMed] [Google Scholar]
- 43. Donnenwerth MP, Roukis TS. Outcome of arthroscopic debridement and microfracture as the primary treatment for osteochondral lesions of the talar dome. Arthroscopy. 2012;28(12):1902-7. [DOI] [PubMed] [Google Scholar]
- 44. Jung HG, Carag JA, Park JY, Kim TH, Moon SG. Role of arthroscopic microfracture for cystic type osteochondral lesions of the talus with radiographic enhanced MRI support. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):858-62. [DOI] [PubMed] [Google Scholar]
- 45. Park HW, Lee KB. Comparison of chondral versus osteochondral lesions of the talus after arthroscopic microfracture. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):860-7. [DOI] [PubMed] [Google Scholar]
- 46. Doral M, Bilge O, Batmaz G, Donmez G, Turhan E, Demirel M, et al. Treatment of osteochondral lesions of the talus with microfracture technique and postoperative hyaluronan injection. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1398-403. [DOI] [PubMed] [Google Scholar]
- 47. Guney A, Akar M, Karaman I, Oner M, Guney B. Clinical outcomes of platelet rich plasma (PRP) as an adjunct to microfracture surgery in osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2384-9. [DOI] [PubMed] [Google Scholar]
- 48. Kim YS, Park EH, Kim YC, Koh YG. Clinical outcomes of mesenchymal stem cell injection with arthroscopic treatment in older patients with osteochondral lesions of the talus. Am J Sports Med. 2013;41(5):1090-9. [DOI] [PubMed] [Google Scholar]
- 49. Hoffmann M, Schroeder M, Rueger J. A novel computer navigation system for retrograde drilling of osteochondral lesions. Sports Med Arthrosc. 2014;22(4):215-8. [DOI] [PubMed] [Google Scholar]
- 50. Hangody L, Vásárhelyi G, Hangody LR, Sükösd Z, Tibay G, Bartha L, et al. Autologous osteochondral grafting—technique and long-term results. Injury. 2008;39(1):32-9. [DOI] [PubMed] [Google Scholar]
- 51. LaPrade RF, Botker JC. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20(7):e69-73. [DOI] [PubMed] [Google Scholar]
- 52. Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35(1):80-5. [DOI] [PubMed] [Google Scholar]
- 53. Imhoff AB, Paul J, Ottinger B, Wörtler K, Lämmle L, Spang J, et al. Osteochondral transplantation of the talus long-term clinical and magnetic resonance imaging evaluation. Am J Sports Med. 2011;39(7):1487-93. [DOI] [PubMed] [Google Scholar]
- 54. Kim YS, Park EH, Kim YC, Koh YG, Lee JW. Factors associated with the clinical outcomes of the osteochondral autograft transfer system in osteochondral lesions of the talus second-look arthroscopic evaluation. Am J Sports Med. 2012;40(12):2709-19. [DOI] [PubMed] [Google Scholar]
- 55. Scranton P, Frey C, Feder K. Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br. 2006;88(5):614-9. [DOI] [PubMed] [Google Scholar]
- 56. Lee CH, Chao KH, Huang GS, Wu SS. Osteochondral autografts for osteochondritis dissecans of the talus. Foot Ankle Int. 2003;24(11):815-22. [DOI] [PubMed] [Google Scholar]
- 57. Baltzer AW, Arnold JP. Bone-cartilage transplantation from the ipsilateral knee for chondral lesions of the talus. Arthroscopy. 2005;21(2):159-66. [DOI] [PubMed] [Google Scholar]
- 58. Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006;22(10):1085-92. [DOI] [PubMed] [Google Scholar]
- 59. Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Henle P, Niemeyer P. Mosaicplasty with autogenous talar autograft for osteochondral lesions of the talus after failed primary arthroscopic management: a prospective study with a 4-year follow-up. Am J Sports Med. 2006;34(1):55-63. [DOI] [PubMed] [Google Scholar]
- 60. Csönge L, Bravo D, Newman-Gage H, Rigley T, Conrad EU, Bakay A, et al. Banking of osteochondral allografts, part II. Preservation of chondrocyte viability during long-term storage. Cell Tissue Bank. 2002;3(3):161-8. [DOI] [PubMed] [Google Scholar]
- 61. Schachar N, McGann L. Investigations of low temperature storage of articular cartilage for transplantation. Clin Orthop Relat Res. 1986;(208):146-50. [PubMed] [Google Scholar]
- 62. Tomford WW, Duff GP, Mankin HJ. Experimental freeze-preservation of chondrocytes. Clin Orthop Relat Res. 1982;(197):11-4. [PubMed] [Google Scholar]
- 63. Pearsall AW, 4th, Tucker JA, Hester RB, Heitman RJ. Chondrocyte viability in refrigerated osteochondral allografts used for transplantation within the knee. Am J Sports Med. 2004;32(1):125-31. [DOI] [PubMed] [Google Scholar]
- 64. Gross AE, Agnidis Z, Hutchison CR. Osteochondral defects of the talus treated with fresh osteochondral allograft transplantation. Foot Ankle Int. 2001;22(5):385-91. [DOI] [PubMed] [Google Scholar]
- 65. El-Rashidy H, Villacis D, Omar I, Kelikian AS. Fresh osteochondral allograft for the treatment of cartilage defects of the talus: a retrospective review. J Bone Joint Surg Am. 2011;93(17):1634-40. [DOI] [PubMed] [Google Scholar]
- 66. Görtz S, De Young AJ, Bugbee WD. Fresh osteochondral allografting for osteochondral lesions of the talus. Foot Ankle Int. 2010;31(4):283-90. [DOI] [PubMed] [Google Scholar]
- 67. Hahn DB, Aanstoos ME, Wilkins RM. Osteochondral lesions of the talus treated with fresh talar allografts. Foot Ankle Int. 2010;31(4):277-82. [DOI] [PubMed] [Google Scholar]
- 68. Raikin SM. Fresh osteochondral allografts for large-volume cystic osteochondral defects of the talus. J Bone Joint Surg Am. 2009;91(12):2818-26. [DOI] [PubMed] [Google Scholar]
- 69. Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889-95. [DOI] [PubMed] [Google Scholar]
- 70. Gooding C, Bartlett W, Bentley G, Skinner JA, Carrington R, Flanagan A. A prospective, randomised study comparing two techniques of autologous chondrocyte implantation for osteochondral defects in the knee: periosteum covered versus type I/III collagen covered. Knee. 2006;13(3):203-10. [DOI] [PubMed] [Google Scholar]
- 71. Battaglia M, Vannini F, Buda R, Cavallo M, Ruffilli A, Monti C, et al. Arthroscopic autologous chondrocyte implantation in osteochondral lesions of the talus: mid-term T2-mapping MRI evaluation. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1376-84. [DOI] [PubMed] [Google Scholar]
- 72. Giannini S, Buda R, Grigolo B, Vannini F. Autologous chondrocyte transplantation in osteochondral lesions of the ankle joint. Foot Ankle Int. 2001;22(6):513-7. [DOI] [PubMed] [Google Scholar]
- 73. Giannini S, Buda R, Vannini F, Di Caprio F, Grigolo B. Arthroscopic autologous chondrocyte implantation in osteochondral lesions of the talus surgical technique and results. Am J Sports Med. 2008;36(5):873-80. [DOI] [PubMed] [Google Scholar]
- 74. Magnan B, Samaila E, Bondi M, Vecchini E, Micheloni GM, Bartolozzi P. Three-dimensional matrix-induced autologous chondrocytes implantation for osteochondral lesions of the talus: midterm results. Adv Orthop. 2012;2012:942174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Quirbach S, Trattnig S, Marlovits S, Zimmermann V, Domayer S, Dorotka R, et al. Initial results of in vivo high-resolution morphological and biochemical cartilage imaging of patients after matrix-associated autologous chondrocyte transplantation (MACT) of the ankle. Skeletal Radiol. 2009;38(8):751-60. [DOI] [PubMed] [Google Scholar]
- 76. Cerrato R. Particulated juvenile articular cartilage allograft transplantation for osteochondral lesions of the talus. Foot Ankle Clin. 2013;18(1):79-87. [DOI] [PubMed] [Google Scholar]
- 77. Kruse D, Ng A, Paden M, Stone PA. Arthroscopic DeNovo NT® juvenile allograft cartilage implantation in the talus: a case presentation. J Foot Ankle Surg. 2012;51(2):218-21. [DOI] [PubMed] [Google Scholar]
- 78. Doral MN, Bilge O, Batmaz G, Donmez G, Turhan E, Demirel M, et al. Treatment of osteochondral lesions of the talus with microfracture technique and postoperative hyaluronan injection. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1398-403. [DOI] [PubMed] [Google Scholar]
- 79. Fortier LA, Potter HG, Rickey EJ, Schnabel LV, Foo LF, Chong LR, et al. Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J Bone Joint Surg Am. 2010;92(10):1927-37. [DOI] [PubMed] [Google Scholar]
- 80. Akeda K, An HS, Okuma M, Attawia M, Miyamoto K, Thonar EJ, et al. Platelet-rich plasma stimulates porcine articular chondrocyte proliferation and matrix biosynthesis. Osteoarthritis Cartilage. 2006;14(12):1272-80. [DOI] [PubMed] [Google Scholar]
- 81. Sun Y, Feng Y, Zhang CQ, Chen SB, Cheng XG. The regenerative effect of platelet-rich plasma on healing in large osteochondral defects. Int Orthop. 2010;34(4):589-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Wu W, Chen F, Liu Y, Ma Q, Mao T. Autologous injectable tissue-engineered cartilage by using platelet-rich plasma: experimental study in a rabbit model. J Oral Maxillofac Surg. 2007;65(10):1951-7. [DOI] [PubMed] [Google Scholar]
- 83. Grigolo B, Roseti L, Fiorini M, Fini M, Giavaresi G, Aldini NN, et al. Transplantation of chondrocytes seeded on a hyaluronan derivative (Hyaff®-11) into cartilage defects in rabbits. Biomaterials. 2001;22(17):2417-24. [DOI] [PubMed] [Google Scholar]
- 84. Hegewald A, Ringe J, Bartel J, Krüger I, Notter M, Barnewitz D, et al. Hyaluronic acid and autologous synovial fluid induce chondrogenic differentiation of equine mesenchymal stem cells: a preliminary study. Tissue Cell. 2004;36(6):431-8. [DOI] [PubMed] [Google Scholar]
- 85. Desai S. Surgical treatment of a tibial osteochondral defect with debridement, marrow stimulation, and micronized allograft cartilage matrix: report of an all-arthroscopic technique. J Foot Ankle Surg. 2016;55(2):279-82. [DOI] [PubMed] [Google Scholar]