Abstract
This study demonstrates that most cholera deaths in this region of Cameroon occur out of hospital. This is a region which is prone to cholera, and interventions are needed to improve access to emergency medical care, especially during cholera outbreaks. Cameroon has experienced 14 cholera epidemics during the last 20 years, and these have had high case fatality rates. This study attempted to assess the effect of delays in seeking care and the locations of care as possible risk factors for cholera mortality. The study used data from a community-based survey regarding the circumstances of 97 fatal cases and 197 control (nonfatal) cases following a cholera-like syndrome in villages with cholera-like diseases during cholera outbreaks in Cameroon during 2009–2011. Deaths occurred in one of four environments: the community, in a temporary community treatment center (TCTC), in transit to a treatment center, or in a hospital (39%, 32%, 5%, and 24%, respectively). Using a case–control analysis, factors associated with deaths included the nonuse of a cholera treatment center, receiving health care in a TCTC instead of a hospital, and greater than 4 hours delay between the onset of symptoms and the decision to go to a treatment center (odds ratios of 17.1 [confidence interval (CI): 7.0–41.8], 2.5 [CI: 1.2–5.0], and 2.2 [CI: 1.0–4.6], respectively). During cholera epidemics, a higher proportion of deaths are still occurring in communities. The nonuse and delays in deciding to go a treatment center, and treatment at TCTC rather than a hospital were risk factors for death among patients with cholera-like syndrome in Cameroon. Informing people on community management of cholera-like syndrome and improving care in all health facilities are needed to reduce deaths during cholera epidemics.
Introduction
Cholera is an acute diarrheal disease caused by the bacterium, Vibrio cholerae. About 10–20% of cholera infections are severe, and if not promptly and adequately treated, patients can die within hours due to loss of large quantities of fluid and electrolytes.1 This disease of poverty remains a major public health problem in sub-Saharan African countries where approximately 60% cases and 68% of fatalities occur globally.2
Between 2009 and 2011, Cameroon reported its worst outbreaks since its first cholera cases in 1971 with a case-fatality rate (CFR) of 6.1%.3 According to World Health Organization (WHO) appropriate cholera case management should keep CFR below 1%. If the CFR exceeds this rate, there is a clear need to improve access to high-quality care. Underlying factors such as low accessibility to cholera treatment centers, inconsistent case management, malnutrition, and biases (e.g., unstandardized case definition, underestimation of the number of cases, and inclusion of deaths from other causes) could explain, as well as confound, high CFRs.
This study was conducted in two health districts in the Far North Region of Cameroon to investigate the causes of the high CFR during cholera outbreaks between 2009 and 2011 and specifically to identify the locations and types of facilities where the deaths were occurring. It was hoped that understanding the proportions of deaths occurring in different settings would generate hypothesis on factors associated with these deaths, allowing for improved treatment.
Methods
Study design.
This was a community-based, case–control study, involving participants recruited by active case finding. Cases were patients who died of cholera-like syndromes and controls were those who survived in the same period following cholera-like syndromes. The main exposures that were queried included household case management, case management in temporary community treatment center (TCTC), and the time between the onset of disease and decision to seek for treatment at a health facility. The ones who were treated at home and did not seek care at a TCTC nor a hospital/health center were defined as “household case management.” Patients treated in a TCTC but who did not reach a hospital/health center were termed “case management in TCTC.”
TCTC were points of treatment of suspected cases of cholera, established during the cholera epidemic for early rehydration in communities where geographic access to health facilities was limited. They were supplied with medications and were supervised by local health authorities. In these points, trained community health workers or nurse auxiliaries provide oral rehydration solution, and antibiotics to patients and preventive advice to the population.
Study area and study population.
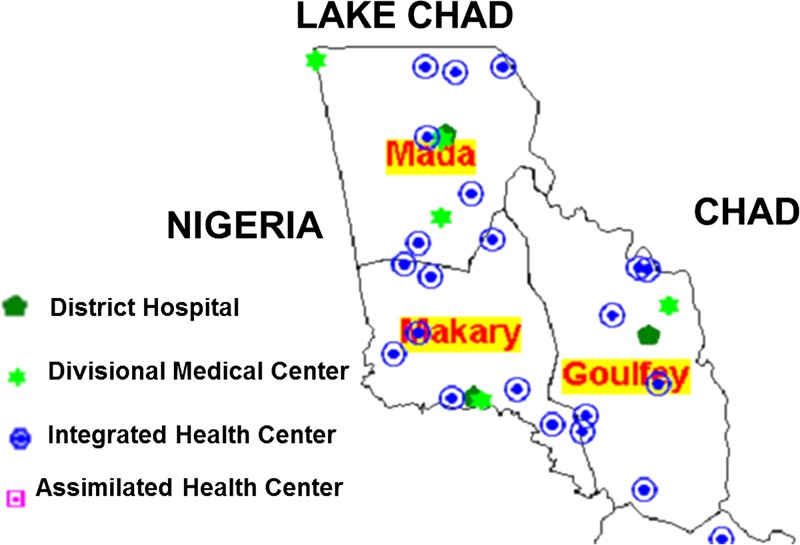
This study was conducted in Mada and Makary health districts. These are rural health districts located in the Logone and Chari Divisions of the Far North Region of Cameroon. These divisions share boundaries with Chad, Nigeria, Lake Chad, and the Goulfey health district (see Figure 1 ). The two health districts are served by 20 health facilities (six hospitals with at least one medical doctor in each one, and 14 health centers where care is provided by nurses). Mada and Makary health districts are divided into 10 and nine health areas, respectively. Access to improved water and sanitation in the study area is limited. During the 2009–2011 cholera epidemic outbreak, Mada and Makary health districts reported 1,015 cases of whom 67 died (CFR: 6.9%).
Figure 1.
Schema of Mada and Makary health districts. (Source: Ministry of Public Health).
The study population consists of people who developed a cholera-like syndrome and those who died of cholera-like syndrome during the 2009–2011 cholera epidemic. The definition of a cholera-like syndrome was adapted from the WHO case definition of a suspected case of cholera. According to WHO, a suspected case of cholera in an endemic area (such as in the present study site) is a patient aged 5 years or more who develops acute watery diarrhea with or without vomiting.4 Considering that cholera does occur in children < 5 years of age,5,6 our operational definition of patients with cholera-like syndrome was “A patient who develops acute watery diarrhea, with or without vomiting during a cholera epidemic.”
Sampling procedure.
A community-based sampling was used to identify fatal cases. All communities with at least one cholera death reported were included in the study. In the Cameroon health system, communities are defined as geographical areas referred to as villages or quarters where residents permanently live in a given number of households, generally not exceeding 500 households. Each health area has specified communities with a total population ranging from 5,000 to 30,000 inhabitants. A health district covers a predetermined number of health areas. Information from a line listing of patients diagnosed as having cholera during the epidemic was obtained from the District Heath Service. Taking into consideration the weakness of the district's information system in Cameroon, community health volunteers (members of the community who served as interfaces between the health system and their respective communities) were consulted to correct errors in the line lists. In these selected communities, all households with at least one death following a cholera-like syndrome registered during the epidemic were selected. From each of these households, all deaths due to a cholera-like syndrome were included in the study. For each fatal case, two controls were selected from the same household, neighboring households or from the same community. A control was defined as a person who had cholera-like syndrome and survived.
Data collection.
In each health area, one community health volunteer was selected and used as a translator. This person could speak both French and the local language. Each community within the health area had a corresponding community health volunteer and these persons assisted with obtaining the line listing of potential cases controls and also served as guides for the identification of their household. In each community, all persons identified by the community volunteer to have presented at least one episode of cholera-like syndrome were eligible. The household of each eligible participant was identified and visited. Permission was solicited from the head of household and consent from the participant followed by questionnaire administration. All those who died after suffering from the syndrome were cases and those who survived were controls.
From each household, data were collected using pretested questionnaires administered by trained surveyors. The questionnaire captured data on sociodemographic characteristics of patients, patient's case management and their outcomes. For fatal cases, information was provided by their relatives, preferably those who were with them during their disease episode. For survivors who were < 15 years of age, information was provided by their parents or legal representative. Those who were ≥ 15 years of age responded to the questionnaire directly.
Data analysis.
For descriptive analyses, proportions and means were estimated. For univariate results, the χ2 test or the Fisher's exact were used. We used multiple logistic regression models to assess the relationships between all potential predictors, listed in the univariate analysis, and death cases. For the final model, significant predictors were selected using forward stepwise methods. Any variable with a P value < 0.20 in a univariate test was included in the multivariate analysis. P values < 0.05 were considered to be significant. All analyses were performed using Epi info software, version 3.5.3 (Centers for Disease Control and Prevention, Atlanta, GA).
Ethical considerations.
The study was approved by the National Ethics Committee. Administrative authorizations were obtained from the Mada and Makary health districts heads. Verbal consent was obtained from the traditional authorities in each community. Participants gave their verbal consent before inclusion in the study. For participants < 15 years of age, informed consent was obtained from their parents or legal representatives. To ensure confidentiality, questionnaires were anonymously codified.
Results
Participants.
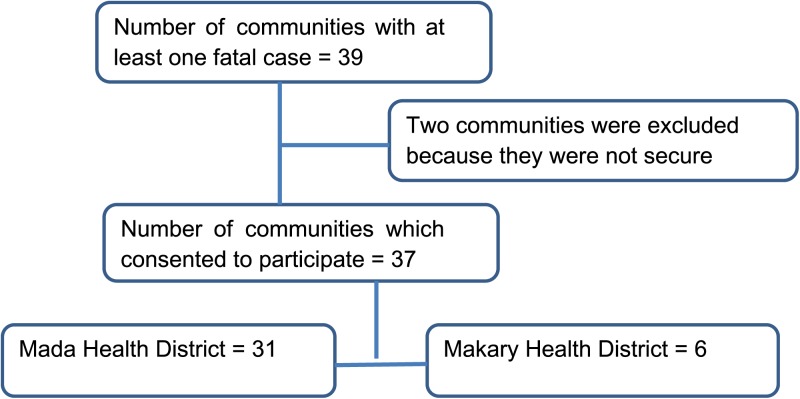
In the two health districts, 39 communities fulfilled the inclusion criteria. Of these, 37 (97.9%) were included in the study (31 from Mada health district and six from Makary health district). The remaining two were not included because of population migration and insecurity. Details on communities included in the study are presented in Figure 2 .
Figure 2.
Communities included in the study and their distribution in the Mada and the Makary health districts.
Descriptive analysis.
In these surveyed communities, 97 fatal cholera-like syndrome cases were identified. This number of deaths was 1.45 times higher than the number of death cases notified at the health district level. Eighty-four (86.6%) among these 97 death cases occurred in the Mada health district. The year 2010 registered the highest number of deaths, with 62 (63.9%) deaths.
As shown on Table 2, during this epidemic, 74 (76%) cases of deaths occurred outside a hospital/health center and the remainder, 23 (24%), occurred at a health facility. Among the deaths outside the hospital/health center, 38 (39%) occurred at home, 31 (32%) in the TCTC, and five (5%) on the way to a health facility.
Table 2.
Place of death for cholera-like syndrome patients in Mada and Makary health districts, 2009–2011
| Place of death | Frequencies n (%) |
|---|---|
| Households/communities | 38 (39.2) |
| Community treatment centers | 31 (32.0) |
| Health facilities | 23 (23.7) |
| Road to cholera treatment center | 5 (5.2) |
Case–control analysis.
To assess the determinants of death in patients presenting with cholera-like syndromes, two controls were matched for each death case except for seven death cases for which only one control was found. Among all participants (cases and controls), 25% (69/284) were children less than 5 years of age. For most families where information was available, household heads (men) (92% [144/154]), were the ones responsible for taking decisions to seek treatment at a health facility.
Table 1 presents the comparisons of sociodemographic and clinical characteristics of the 97 death cases and their 187 controls. There was no difference with regard to sex, but age was associated with increased mortality (P = 0.01). Deaths were also more likely among those living in Makary health district (P < 0.01).
Table 1.
Sociodemographic and clinical characteristics of death cases and their controls during the 2009–2011 cholera epidemic in Mada and Makary health districts
| Characteristics | Death cases n (%) | Nonfatal controls n (%) | P value* |
|---|---|---|---|
| Sex of patients | |||
| Male | 52 (53.6) | 100 (53.5) | 0.983 |
| Female | 45 46.4) | 87 (46.5) | |
| Age | |||
| < 5 years | 34 (35.1) | 35 (18.7) | 0.002 |
| ≥ 5 years | 63 (64.9) | 152 (81.3) | |
| Years of epidemics | |||
| 2009 | 18 (18.6) | 46 (24.6) | 0.073 |
| 2010 | 62 (63.9) | 93 (49.7) | |
| 2011 | 17 (17.5) | 48 (25.7) | |
| Health district | |||
| Mada | 84 (86.6) | 179 (95.7) | 0.008† |
| Makary | 13 (13.4) | 8 (4.3) | |
| Symptoms | |||
| Diarrhea with vomiting | 85 (87.6) | 169 (90.4) | 0.027 |
| Diarrhea without vomiting | 12 (12.4) | 18 (9.6) | |
| Taking medicines at home | |||
| Yes | 13 (13.4) | 38 (20.3) | 0.113 |
| No | 44 (45.4) | 93 (49.7) | |
| Unknown | 40 (41.2) | 56 (29.9) | |
| Person taking decision to bring patient to a cholera treatment center (when known) | |||
| Head of household (men) | 30 (30.9) | 114 (61.0) | < 0.0001† |
| Others | 3 (3.1) | 10 (5.3) | |
χ2 test.
Fisher's exact test.
In unadjusted analysis (Table 3), household case management (odds ratio [OR]: 16.5, confidence interval [CI]: 7.0–39.0), management in TCTC (OR: 2.0, CI: 1.1–3.7), and a delay of > 4 hours between the onset symptoms and the decision to seek care at a health facility (OR: 2.1, CI: 1.0–4.3) were significantly associated with patients' deaths.
Table 3.
Ratio of determinants of death among cholera-like syndrome presenting patients in Mada and Makary health districts during the 2009–2011 epidemics, adjusted for sex, age, and health district
| Characteristics | Frequencies | Unadjusted analysis | Adjusted analysis | |||
|---|---|---|---|---|---|---|
| Case n (%) | Controls n (%) | OR (95% CI) | P value | AOR (95% CI) | P value | |
| Place were outcome occurred | ||||||
| Health facilities | 23 (17.4) | 109 (82.6) | 1 | – | 1 | – |
| Households/communities | 38 (84.4) | 7 (15.6) | 16.5 (7.0–39.0) | < 0.01 | 17.1 (7.0–41.8) | < 0.01 |
| Community treatment centers | 31 (30.4) | 71 (69.6) | 2.0 (1.0–3.7) | 0.01 | 2.5 (1.2–5.0) | < 0.01 |
| Delay indecision taking to use cholera treatment centers | ||||||
| < 4 hours | 20 (18.9) | 86 (81.1) | 1 | – | 1 | |
| ≥ 4 hours | 21 (33.3) | 42 (66.7) | 2.1 (1.0–4.3) | 0.01 | 2.2 (1.0–4.6) | 0.03 |
AOR = adjusted odds ratio; CI = confidence interval; OR = odds ratio.
In adjusted analysis (Table 3), age, sex, and patients' health district were included in a logistic regression models as potential confounders. After this adjustment, household case management (OR: 17.1, CI: 7.0–41.8), management in TCTC (OR: 2.5, CI: 1.2–5.0), and a delay > 4 hours between the first symptoms and the decision to seek treatment at a facility (OR: 2.2, CI: 1.0–4.6) remained significantly associated with a fatal outcome.
Discussion
During the 2009–2011 cholera epidemics in Mada and Makary health districts, the risk of death was significantly associated with failure to seek care at a treatment facility, receiving health care in a TCTC and a delay of > 4 hours from the onset of symptoms and the decision to seek care at a health facility. It appeared that because many patients live in very remote areas where health facilities are not easily reached, the delay in deciding to seek care was a key determinant of cholera mortality.
The study also found that the deaths reported to the health facilities underestimate the actual number of deaths in the population. By conducting this community-based study, more cholera deaths were detected suggesting that many deaths, especially those occurring in remote communities, are not always reported.
Cholera is a medical emergency, and its management therefore requires medical expertise. Although community-based interventions such as early household administration of oral rehydration solution7,8 are effective in reducing mortality, they do not exclude the need for adequate care in a proper cholera treatment center where intravenous fluids can be administered.1 This study has shown that the death following a cholera-like syndrome is strongly associated with the nonuse of health facilities and the use of TCTC for case management. Though not difficult, treatment of cholera patients need expert case management. Management of cases at home by patient's relatives and at the TCTC was not sufficient to prevent deaths in some cases and additional treatment was needed at the hospital/health center.
During cholera outbreaks, WHO recommends the establishment of TCTCs, generally referred to as oral rehydration treatment corners. Ideally, these decentralized cholera treatment units are able to manage patients with mild and moderate dehydration, but patients with severe dehydration should be transferred immediately to a health facility. Unfortunately, in the study area, access to health-care facilities was not always possible due to the remote area of the country. Thus, these TCTCs attempted to treat not only mild and moderate dehydration patients, but also severe cholera cases. In addition, cholera case management in the TCTC is generally performed by community volunteers (unqualified and untrained) due to the lack of more skilled health workers. These factors suggest that inadequate case management of severely dehydrated patients in TCTC increased the risk of death in the TCTCs.
Delay of case management is defined as the time lapse between the onset of disease symptoms and the effective beginning of case management. This lapse of time includes the time of decision-making to use health-care facilities, the travel time, and the waiting time in health facility. This concept is similar to the three-delay model used when assessing cause of death from maternity emergencies.9 The present study tried to determine the specific effect of decision-making time with respect to the use of a cholera treatment center on mortality outcomes. Since the questionnaires were administered many months after the deaths, the precise interval required to make the decision to seek treatment could not be determined, but it did appear that there was a delay, which increased the risk of death. In fact, if patients with severe symptoms are not promptly and adequately treated, the loss of such large amounts of fluid and salts can lead to severe dehydration and death within hours.1
Data collection for this study was carried out after the outbreak was already over when TCTCs were no longer functional; thus, it was not possible to assess the standard of care in these treatment centers to determine if the higher mortality in the TCTC was due to lack of supplies, or other deficiencies of care. However, our findings do suggest that appropriate drugs, supplies, training, and supervision are needed to improve case management in this setting.
Mada had fewer deaths than Makary. This difference was not explained by sociodemographic differences in the two populations since the two districts were inhabited by the same ethnic and religious groups with similar income and education levels. The difference was also not explained by a difference in health coverage since the Mada health district had eight health areas (thus eight integrated health centers and one district hospital) for a population of about 120,000 inhabitants while the Makary health district had 11 health areas (11 integrated health centers and one hospital district) for a population of about 150,000 inhabitants. However, one difference was access to a skilled health staff: Mada health district had three medical doctors but Makary had none.
The results of this study are similar to findings from other areas. Studies from Guinea-Bissau10 and the Amazon11 showed that the nonuse of health-care facilities was significantly associated with increased risk of death among patients with cholera-like syndromes. The strengths of these associations (6.0 and 3.5, respectively) were however lower than recorded in the present study (17.1). This difference may be due to the source of the data used in the different studies. A community-based survey was used in the present study while the other studies used data from their routine surveillance systems. This hypothesis seems to be confirmed by a study done in Zimbabwe, using the same methodology as ours, where people with cholera who died were 17.2 times more likely to have received care at home.12 Another study from Rwanda showed an association between patients' death and case management in the TCTC.13
Our study has some limitations. Selection of participants was intended to cover all communities that registered at least one fatal case of cholera during the epidemic. Unfortunately, due to insecurity and constant population migration, two of the 39 eligible communities were not included in the study. However, we believed that the proportion of communities that were not surveyed (5.5%) was small and did not significantly influence our results. Second, data were collected at least 2 years after the onset of the most recent event, and this delay may have introduced recall biases. However, the fact that information on cases and controls covered the same period ensured an equal distribution of these potential biases in the two groups. Third, it was not possible to calculate the CFR for patients who come to health facilities compared with those who went to the TCTC. In this way, if many more people were treated in the TCTC, the CFR might have not been different from health center. But, with the information available, it appeared that more people went to a health center so, in fact, the CFR was higher in the TCTC.
In summary, during the 2009–2011 cholera epidemics in Mada and Makary health districts, the risk of patients' death was significantly associated with the nonuse of cholera treatment centers, receiving health care in TCTC and delays of more than 4 hours from the onset of symptoms to the decision to use a cholera treatment center. Targeted interventions must be implemented in these communities and in cholera treatment centers to reduce fatality rates during cholera epidemics. These interventions include education of populations on the necessity of immediate search for appropriate care following a cholera-like syndrome, increase in the quality of case managements in TCTC and health facilities. Further studies are needed to identify the reasons for the nonuse of cholera treatment centers by patients with cholera-like syndrome during cholera outbreaks in Cameroon.
Recommendations from these observations include the following. Before and during cholera outbreaks, there is a need to train staff and strengthen case management at TCTCs and insure adequate supplies for managing cholera patients. Second, there is a need to develop messages to villages and community health workers regarding the need to rapidly seek care for severe acute watery diarrhea, especially during cholera outbreaks. Given the limited geographical access of populations to health facilities, TCTC should remain part of strategies to limit CFR during cholera outbreak, but the health-care system must ensure that care offered in these sites comply with the recommended WHO standards.
Research is needed to identify factors associated with the nonuse of cholera treatment centers by patients with cholera-like syndromes as well as studies to assess the preparedness of health facilities before the onset of a cholera outbreak. Given the history of cholera in the Far North Region of Cameroon,3 outbreaks are certain to occur, even if the timing of the outbreaks is difficult to predict.
ACKNOWLEDGMENTS
We acknowledge the contribution of Francisco Javier Luquero Alcalde in reviewing the manuscript.
Disclaimer: This material is original, has not already been published, and has not and will not be submitted for publication elsewhere as long as it is under consideration by the AJTMH. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Financial support: This study was funded by the Delivering Oral Vaccine Effectively (DOVE) project, which is supported by the Bill & Melinda Gates Foundation (OPP1053556) and administered through the Johns Hopkins Bloomberg School of Public Health.
Authors' addresses: Fabrice N. Djouma, Epidemiology, Meilleur Accès aux Soins de Santé, Yaounde, Cameroon, E-mail: nembotfabrice2009@yahoo. Jerome Ateudjieu, Department of Biomedical Sciences, University of Dschang, Dschang, Cameroon, E-mail: jateudj@yahoo.fr. Malathi Ram, Amanda K. Debes, and David A. Sack, Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mails: mram1@jhu.edu, adebes1@jhu.edu, and dsack@jhsph.edu.
References
- 1.Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet. 2004;363:223–233. doi: 10.1016/s0140-6736(03)15328-7. [DOI] [PubMed] [Google Scholar]
- 2.Ali M, Nelson AR, Lopez AL, Sack DA. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis. 2015;9:e0003832. doi: 10.1371/journal.pntd.0003832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Djomassi LD, Gessner BD, Andze GO, Mballa GA. National surveillance data on the epidemiology of cholera in Cameroon. J Infect Dis. 2013;208((Suppl 1)):S92–S97. doi: 10.1093/infdis/jit197. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) Cholera Outbreak. Assessing the Outbreak Response and Improving Preparedness. Geneva, Switzerland: WHO; 2004. [Google Scholar]
- 5.Siddique AK, Ahmed S, Iqbal A, Sobhan A, Poddar G, Azim T, Sack DA, Rahman M, Sack RB. Epidemiology of rotavirus and cholera in children aged less than five years in rural Bangladesh. J Health Popul Nutr. 2011;29:1–8. doi: 10.3329/jhpn.v29i1.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clemens JD, Sack DA, Chakraborty J, Rao MR, Ahmed F, Harris JR, van Loon F, Khan MR, Yunis M, Huda S, Stanton BF, Kay BA, Svennerholm A-M, Holmgren J. Field trial of oral cholera vaccines in Bangladesh: evaluation of anti-bacterial and anti-toxic breast-milk immunity in response to ingestion of the vaccines. Vaccine. 1990;8:469–472. doi: 10.1016/0264-410x(90)90248-k. [DOI] [PubMed] [Google Scholar]
- 7.Sircar BK, Saha MR, Deb BC, Singh PK, Pal SC. Effectiveness of oral rehydration salt solution (ORS) in reduction of death during cholera epidemic. Indian J Public Health. 1990;34:68–70. [PubMed] [Google Scholar]
- 8.Mahalanabis D, Choudhuri AB, Bagchi NG, Bhattacharya AK, Simpson TW. Oral fluid therapy of cholera among Bangladesh refugees. Johns Hopkins Med J. 1973;132:197–205. [PubMed] [Google Scholar]
- 9.Maine D. The strategic model for the PMM Network. Int J Gynaecol Obstet. 1997;59((Suppl 2)):S23–S25. doi: 10.1016/s0020-7292(97)00144-6. [DOI] [PubMed] [Google Scholar]
- 10.Gunnlaugsson G, Angulo FJ, Einarsdottir J, Passa A, Tauxe RV. Epidemic cholera in Guinea-Bissau: the challenge of preventing deaths in rural west Africa. Int J Infect Dis. 2000;4:8–13. doi: 10.1016/s1201-9712(00)90059-6. [DOI] [PubMed] [Google Scholar]
- 11.Quick RE, Vargas R, Moreno D, Mujica O, Beingolea L, Palacios AM, Seminario L, Tauxe RV. Epidemic cholera in the Amazon: the challenge of preventing death. Am J Trop Med Hyg. 1993;48:597–602. doi: 10.4269/ajtmh.1993.48.597. [DOI] [PubMed] [Google Scholar]
- 12.Morof D, Cookson ST, Laver S, Chirundu D, Desai S, Mathenge P, Shambare D, Charimari L, Midzi S, Blanton C, Handzel T. Community mortality from cholera: urban and rural districts in Zimbabwe. Am J Trop Med Hyg. 2013;88:645–650. doi: 10.4269/ajtmh.11-0696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siddique AK. Failure of treatment centres to prevent cholera deaths in Goma. Lancet. 1995;346:379. doi: 10.1016/s0140-6736(95)92259-8. [DOI] [PubMed] [Google Scholar]