Abstract
Objectives
Researchers have attempted to design various scoring systems to determine the severity and predict the outcome of critically ill patients. The present study aimed to evaluate the accuracy of SOFA score in predicting 1-month outcome of these patients in emergency department.
Methods
The present study is a prospective cross-sectional study of >18 year old non-trauma critically ill patients presented to EDs of 3 hospitals, Tehran, Iran, during October 2014 to October 2015. Baseline characteristics, SOFA score variables, and 1-month outcome of patients were recorded and screening performance characteristics of the score were calculated using STATA 11 software.
Results
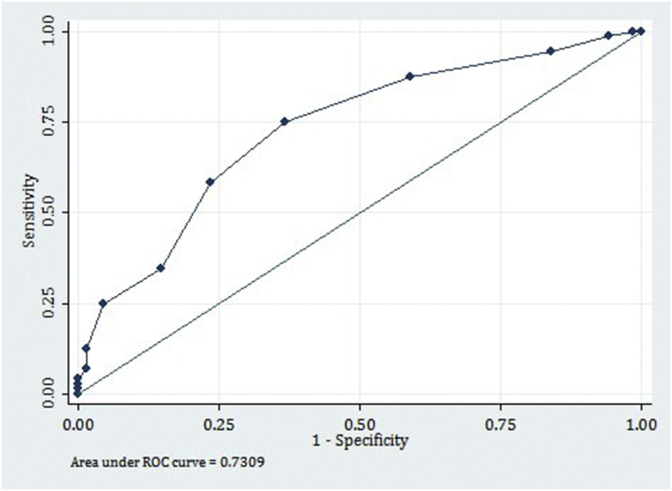
140 patients with the mean age of 68.36 ± 18.62 years (18–95) were included (53.5% male). The most common complaints were decrease in level of consciousness (76.43%) and sepsis (60.0%), were the most frequent final diagnoses. Mean SOFA score of the patients was 7.13 ± 2.36 (minimum 2 and maximum 16). 72 (51.43%) patients died during the following 30 days and 16 (11.43%) patients were affected with multiple organ failure. Area under the ROC curve of SOFA score in predicting mortality of studied patients was 0.73 (95%CI: 0.65–0.81) (Fig. 2). Table 2 depicts screening performance characteristics of this scale in prediction of 1-month mortality in the best cut-off point of ≥7. At this cut-off point, sensitivity and specificity of SOFA in predicting 1-month mortality were 75% and 63.23%, respectively.
Conclusion
Findings of the present study showed that SOFA scoring system has fair accuracy in predicting 1-month mortality of critically ill patients. However, until a more reliable scoring system is developed, SOFA might be useful for narrative prediction of patient outcome considering its acceptable likelihood ratios.
Keywords: Organ dysfunction scores, Prognosis, Patient outcome assessment, Critical illness, Emergency service, Hospital
1. Introduction
Emergency department (ED) is one of the most important hospital departments and the frontline of facing critically ill patients.1 Emergency physicians constantly have to choose the most accurate therapeutic plan for the patients based on the severity and prognosis of the disease and deal with the worries of the patients' relatives.2 Therefore, having a correct criteria for prioritizing patients is of great importance for providing special care for critically ill patients and help reducing health and financial burdens of diseases.3, 4 Since years ago, researchers have attempted to design various scoring systems to determine the severity of the disease and predict the outcome of patients.5, 6, 7 These systems have been successful in evaluating the efficacy of the diagnostic methods, pre and in-hospital triage, and finally improving the quality of therapeutic and preventive measures.8, 9 In addition, scoring systems are capable of converting the severity of patient's disease to a number, which leads to a common understanding between the physicians and making the same decision. Sequential Organ Failure Assessment (SOFA) is one of the scoring systems used for assessing the severity of disease in critically ill patients and predicting their outcome.10, 11 This system was introduced in 1996 and it performs based on evaluating the function of 6 vital organs of respiratory, coagulation, cardiovascular and circulatory, liver, central nervous system and renal. This tool is easy to use and evaluates the status of the mentioned organs systematically and continuously during hospitalization.12 Studies have shown that SOFA score is able to provide valuable prognostic data regarding in-hospital mortality of septic patients.10, 13 In addition, SOFA has been an acceptable and appropriate tool for classifying risk and predicting 14-day prognosis of cancer patients presented to ED.14 In Iran, due to shortage of intensive care unit (ICU) beds, a significant number of critically ill patients spend a portion of their hospitalization in ED. Responding to the patients' relatives regarding their outcome and choosing the best diagnostic and therapeutic plan for better outcome are common challenges of in charge emergency physicians. Therefore, taking the afore-mentioned points into account, the present study was designed aiming to evaluate the accuracy of SOFA scoring system in predicting 1-month outcome of non-trauma critically ill patients presented to ED.
2. Material and methods
2.1. Study design and setting
The present study is a prospective cross-sectional study, evaluating the diagnostic accuracy of SOFA scoring system in prediction of 30-day outcome of non-trauma critically ill patients presented to EDs of … Hospitals, …during 1 year from October 2014 to October 2015. The protocol of the study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences. The patients were included in the study voluntarily and informed consent was obtained from them or their relatives. The researchers adhered to the principles of Helsinki Declaration throughout the study period.
2.2. Participants
Non-trauma critically ill patients over 18 years of age, who were willing to participate in the study were included, regardless of the cause. Patients referred from other hospitals or those whose clinical or laboratory data were not available were excluded.
2.3. Data gathering
Non-random convenience sampling was used. A checklist consisting of 3 parts: baseline characteristics (age, sex, chief complaint, symptoms on presentation, final diagnosis), data needed for calculation of SOFA score, and 1-month outcome of the patients was used for data gathering. Before data gathering, the senior emergency medicine resident performing the research was trained on filling the checklist and calculating SOFA score.
2.4. Calculation of SOFA score
The severity of the disorder in any of the 6 vital organs of respiratory, coagulation, cardiovascular and circulatory, liver, central nervous system and renal, were scored on a 0–4 scale based on definitions of SOFA scoring system. Calculation of the score for each organ has been summarized in Appendix 1.12 SOFA score was calculated based on data recorded in the initial 24 h of admission to ED.
2.5. Outcome
The final outcome of the patient included multiple organ failure or mortality, which were evaluated and recorded a month after hospitalization by calling patients or their relatives (in cases that were discharged) or visiting the department (in cases of remaining hospitalized). Finally, to calculate the predictive value of SOFA model for 1-month outcome of critically ill patients, the relationship between patients' SOFA score and final outcome was assessed.
2.6. Statistical analysis
Considering the 21% prevalence of mortality in critically ill patients10 and 95% confidence interval (CI) (α = 0.05), sample size needed for the present study was estimated to be 131 patients. Finally, data were analyzed using STATA 11.0. Quantitative data were reported as mean ± standard deviation (SD), and qualitative ones as frequency and percentage. To calculate the predictive value of SOFA scoring model in predicting 1-month outcome of critically ill patients, sensitivity, specificity, positive and negative predictive values, positive and negative likelihood ratios, and area under the receiver operating characteristic (ROC) curve were calculated with 95% CI.
3. Results
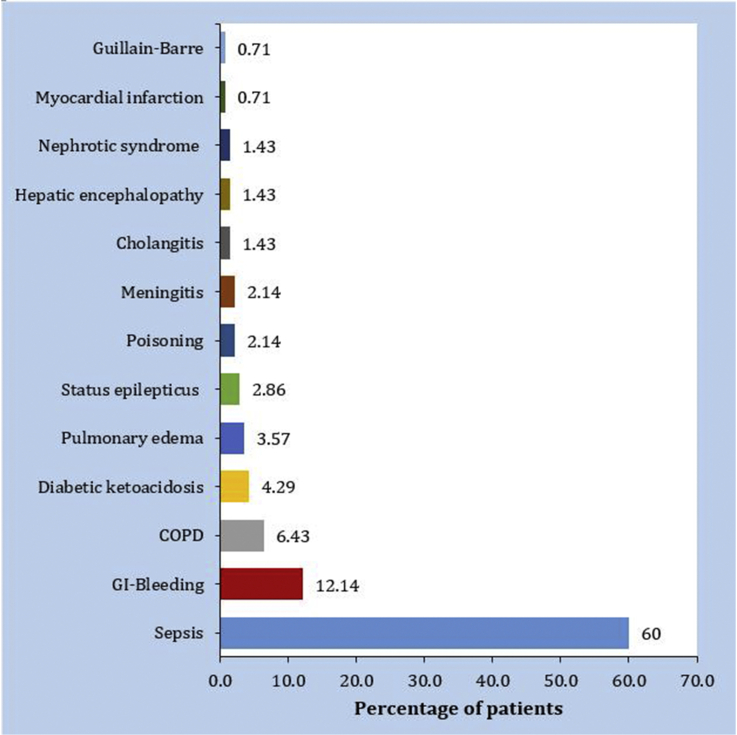
140 patients with the mean age of 68.36 ± 18.62 years (18–95) were entered (53.5% male). Fig. 1 shows the final diagnosis of the patients. The most common complaints were drop in level of consciousness (76.43%), severe weakness (14.29%), and dyspnea (2.86%), respectively. Sepsis (60.0%), upper gastrointestinal bleeding (12.14%) and chronic obstructive pulmonary disease (6.43%) were the most frequent final diagnoses among patients, respectively. Mean and SD of the patients' SOFA score was 1.96 ± 1.0 for the respiratory system, 0.27 ± 0.64 for coagulation system, 1.01 ± 0.92 for cardiovascular system, 0.73 ± 0.86 for the hepatic system, 2.09 ± 0.84 for the central nervous system, and 1.07 ± 1.14 for renal system (Table 1). Mean overall SOFA score of the patients was 7.13 ± 2.36 (minimum 2 and maximum 16). 84.12% (117) of the patients had a score between 4 and 10. Finally, 72 (51.43%) patients died during 30 days and 16 (11.43%) patients were affected with multiple organ failure. These failures included 6 (4.29%) cases of renal failure, 1 (0.71%) case of cardiovascular failure and 9 (6.43%) cases of neurological impairment. Area under the ROC curve of SOFA score in predicting mortality of studied patients was 0.73 (95%CI: 0.65–0.81) (Fig. 2). Table 2 depicts screening performance characteristics of this scale in prediction of 1-month mortality in the best cut-off point of ≥7. As can be seen, at this cut-off point, sensitivity and specificity of SOFA in predicting 1-month mortality were 75% and 63.23%, respectively.
Fig. 1.
Final diagnosis of the studied patients.
Table 1.
The result of SOFA scoring system in various organs.
| Score (%) |
|||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Respiratory | 9.29 (13) | 19.29 (27) | 42.14 (59) | 25 (35) | 4.29 (6) |
| Coagulation | 80.71 (113) | 12.86 (18) | 5.71 (8) | 0 | 0.71 (1) |
| Cardiovascular | 31.43 (44) | 45.71 (64) | 15 (21) | 6.43 (9) | 1.43 (2) |
| Liver | 47.14 (66) | 37.86 (53) | 12.14 (17) | 0.71 (1) | 2.14 (3) |
| Nervous system | _ | 30.71 (43) | 30 (42) | 39.29 (55) | _ |
| Renal | 37.14 (52) | 35.71 (50) | 16.43 (23) | 4.29 (6) | 6.43 (9) |
Fig. 2.
Area under the receiver operating characteristic (ROC) curve of SOFA score in prediction of 1-month mortality in critically ill patients admitted to emergency department.
Table 2.
Screening performance characteristics of SOFA model in prediction of 1-month mortality of the studied patients on the cut-off point of ≥7.
| Variable | Measure (95% confidence interval) |
|---|---|
| Sensitivity | 75.0 (63.16–84.13) |
| Specificity | 63.23 (50.62–74.45) |
| Positive likelihood ratio | 2.04 (1.45–2.86) |
| Negative likelihood ratio | 0.40 (0.26–0.60) |
| Positive predictive value | 68.35 (56.80–78.11) |
| Negative predictive value | 70.49 (57.26–81.13) |
4. Discussion
The findings of the present study showed that SOFA scoring system has fair accuracy in predicting 1-month mortality of critically ill patients presenting to ED (area under the curve 0.73). On the best cut-off point, score ≥7, sensitivity and specificity of this scale in predicting 1-month mortality were 75% and 63.23%, respectively.
SOFA scoring scale was designed aiming to develop an objective tool to evaluate single and multiple organ failure.12 Functionality of this model for critically ill patients has been confirmed through cohort studies.15, 16 Of course, these studies have been carried out on patients admitted to ICU. This scale has various characteristics that makes it applicable in ED as it is easy to calculate and can be easily measured on patient's bedside. The components of this scale include clinical and laboratory data that is commonly available and measured in ED. However, few studies have attempted to evaluate the accuracy of this model in predicting patient mortality in ED.
In line with the findings of the present study, Jones et al. in their study evaluating the accuracy of SOFA score in sepsis patients revealed that area under the curve of SOFA scoring system for predicting in-hospital mortality was 0.75 on admission and 0.84 after 72 h. They concluded that SOFA scoring system provides valuable prognostic information regarding in-hospital mortality for the medical team.10 In addition, Mahjobipoor et al. aimed to use SOFA system in ICU for prediction of mortality and showed that there is a significant correlation between SOFA score at various times and mortality rate (p = 0.0001) and concluded that SOFA is an appropriate tool for predicting length of stay and mortality for ICU patients.13 In another study, SOFA score ≥4, history of chemotherapy, and change in mental status were predictive factors of 14-day mortality in cancer patients. These researchers expressed that SOFA score is an acceptable tool for classifying cancer patients visiting ED, regarding their risk and prognosis. This scoring system helps physicians in predicting 14-day mortality and choosing a proper therapeutic plan.14 Huang et al. believed that SOFA score has high efficiency for predicting in-hospital mortality of myocardial infarction (MI) patients. In fact, this scale can also efficiently predict 1-year and 3-year mortality. Area under the curve of this scale was 0.79 for predicting 30-day mortality in that study and SOFA score was identified as a valuable diagnostic tool for predicting short and long term clinical outcome of patients with acute MI.17 In another study in Germany, application of SOFA score for predicting 30-day morbidity and mortality of patients with heart transplantation revealed that from the first to the 7th day, SOFA score was significantly higher in patients who died eventually compared to those who survived. These researchers expressed that SOFA score can be an effective tool for classifying the severity of morbidity and predicting 30-day mortality in heart transplant patients.18 Anami et al. also showed that when SOFA score is higher, mortality increases. Area under the curve was reported to be 0.82 in this study. The researchers revealed that using SOFA score in critically ill patients efficiently describes the severity of organ failure and high SOFA score directly correlates with mortality.19
As can be seen, there is a high agreement between findings of this study with previous ones. Area under the curve reported in various studies ranges between 0.70 and 0.82, which has acceptable compatibility with the value reported in the present study (0.73).
Accuracy of other scoring models designed for ICU have also been evaluated for use in ED.10, 20 Findings of these studies are indicative of fair to excellent predictive values of these scoring models. However, calculation of some of these models is complex and requires software calculations, which has limited their use in ED. This limitation does not exist regarding SOFA model. This score can be calculated using vital signs and a number of routine evaluations in ED and does not require a final diagnosis. This might promote the use of this model instead of others for classifying critically ill patients regarding mortality risk.
4.1. Limitations
The sample size of this study is among its limitations. Although the sample size was calculated to be 131 patients, involving a higher number of patients in evaluating the accuracy of a scoring model increases the power of the study. Yet, the power of the present study was 83%, which is in the acceptable range. Among other limitations of the study is the single step evaluation of SOFA scale (in the first 24 h), while sequential evaluation of organs in this system is more accurate and efficient. Evaluation of the accuracy of the model based on the cause of illness might be helpful in increasing its accuracy, but due to the low number of patients in some causes sub-section analysis based on the cause of illness could not be performed.
It is suggested to evaluate the predictive value of SOFA scale with larger sample size, perform sequential evaluations and carry out sub-section analysis based on the cause of illness to obtain more accurate results.
5. Conclusion
Findings of the present study showed that SOFA scoring system has fair accuracy in predicting 1-month mortality of critically ill patients. However, until a more reliable scoring system is developed, SOFA might be useful for narrative prediction of patient outcome considering its acceptable likelihood ratios.
Funding and support
There is no source of funds or financial support in the present study.
Conflict of interest
None.
Acknowledgement
The authors wish to thank the staff of Emergency Departments of … Hospitals for their valuable contribution in data gathering.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
Appendix 1. Calculating the score of the 6 vital organs based on SOFA scoring system
| Organ System score | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Respiration | ||||
| PaO2/FiO2 (kPa) | 40–53.3 | 0–39.9 | 0–25.2 R) | 0–13.3 R) |
| Coagulation | ||||
| Platelets x103 (mm3/L) | 101–150 | 51–100 | 21–50 | 0–20 |
| Liver | ||||
| Bilirubin (mg/dL) | 1.2–1.9 | 2.0–5.9 | 6.0–11.9 | >12.0 |
| Nervous system | ||||
| Glasgow coma score | 13–14 | 10–12 | 6–9 | <6 |
| Cardiovascular | ||||
| Hypotension | MAP* 0–70 | Dopamine ≤ 5.0 or Dobutamine (any dose) |
Dopamine 5–14.9 or Epinephrine ≤ 0.1 or Norepinephrine ≤ 0.1 |
Dopamine ≥ 15 or Epinephrine ≤ 0.1 or Norepinephrine ≤ 0.1 |
| Renal | ||||
| Creatinine (mg/dL) | 1.2–1.9 | 2.0–3.4 | 3.5–4.9 | >5.0 |
MAP: mean arterial pressure (mmHg).
Adrenergic agents administered for at least 1 h.
References
- 1.Trzeciak S., Rivers E. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carstensen S., Nelson G.C., Hansen P.S. Field triage to primary angioplasty combined with emergency department bypass reduces treatment delays and is associated with improved outcome. Eur Heart J. 2007;28(19):2313–2319. doi: 10.1093/eurheartj/ehm306. [DOI] [PubMed] [Google Scholar]
- 3.Babl F.E., Lyttle M.D., Bressan S. A prospective observational study to assess the diagnostic accuracy of clinical decision rules for children presenting to emergency departments after head injuries (protocol): the Australasian Paediatric Head Injury Rules Study (APHIRST) BMC Pediatr. 2014;14(1):148. doi: 10.1186/1471-2431-14-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mommsen P., Zeckey C., Andruszkow H. Comparison of different thoracic trauma scoring systems in regards to prediction of post-traumatic complications and outcome in blunt chest trauma. J Surg Res. 2012;176(1):239–247. doi: 10.1016/j.jss.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Benzer A., Mitterschiffthaler G., Pühkringer F. Prediction of non-survival after trauma: innsbruck coma scale. Lancet. 1991;338(8773):977–978. doi: 10.1016/0140-6736(91)91840-q. [DOI] [PubMed] [Google Scholar]
- 6.Knaus W.A., Draper E.A., Wagner D.P., Zimmerman J.E. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 7.Staff T., Eken T., Wik L., Røislien J., Søvik S. Physiologic, demographic and mechanistic factors predicting New Injury Severity Score (NISS) in motor vehicle accident victims. Injury. 2014;45(1):9–15. doi: 10.1016/j.injury.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Chawda M., Hildebrand F., Pape H.C., Giannoudis P.V. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35(4):347–358. doi: 10.1016/S0020-1383(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 9.Nayduch D.A., Moylan J., Rutledge R. Comparison of the ability of adult and pediatric trauma scores to predict pediatric outcome following major trauma. J Trauma Acute Care Surg. 1991;31(4):452–458. doi: 10.1097/00005373-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Jones A.E., Trzeciak S., Kline J.A. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37(5):1649. doi: 10.1097/CCM.0b013e31819def97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen S.-J., Chao T.-F., Chiang M.-C. Prediction of patient outcome from Acinetobacter baumannii bacteremia with sequential organ failure assessment (SOFA) and acute physiology and chronic health evaluation (APACHE) II scores. Intern Med. 2011;50(8):871–877. doi: 10.2169/internalmedicine.50.4312. [DOI] [PubMed] [Google Scholar]
- 12.Vincent J.-L., Moreno R., Takala J. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 13.Mahjoubipour H., Mohammdi M., Salmani F., Saneei F. Survey of SOFA scoring system on predicting mortality rate and length stay in intensive care unit for patients of Al-Zahra hospital of Isfahan. Med Surg Nurs J. 2012;1(2):6–10. [Google Scholar]
- 14.Lee J.S., Kwon O.Y., Choi H.S., Hong H.P., Ko Y.G. Application of the Sequential Organ Failure Assessment (SOFA) score in patients with advanced cancer who present to the ED. Am J Emerg Med. 2012;30(2):362–366. doi: 10.1016/j.ajem.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira F.L., Bota D.P., Bross A., Melot C., Vincent J.L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. Jama. 2001;286(14):1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 16.Moreno R., Vincent J.L., Matos R. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis related Problems of the ESICM. Intensive Care Med. 1999;25(7):686–696. doi: 10.1007/s001340050931. [DOI] [PubMed] [Google Scholar]
- 17.Huang S.-S., Chen Y.-H., Lu T.-M., Chen L.-C., Chen J.-W., Lin S.-J. Application of the Sequential Organ Failure Assessment score for predicting mortality in patients with acute myocardial infarction. Resuscitation. 2012;83(5):591–595. doi: 10.1016/j.resuscitation.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 18.Qedra N., Yilmaz K., Gromann T., Lehmkuhl H., Knosalla C., Hetzer R. 498: prognostic value of the sequential organ failure assessment score (SOFA) for early postoperative monitoring of heart transplanted patients. J Heart Lung Transplant. 2009;28(2):S239. [Google Scholar]
- 19.Anami E.H., Grion C.M., Cardoso L.T. Serial evaluation of SOFA score in a Brazilian teaching hospital. Intensive Crit Care Nurs. 2010;26(2):75–82. doi: 10.1016/j.iccn.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen H.B., Banta J.E., Cho T.W. Mortality predictions using current physiologic scoring systems in patients meeting criteria for early goal-directed therapy and the severe sepsis resuscitation bundle. Shock (Augusta, Ga) 2008;30(1):23–28. doi: 10.1097/SHK.0b013e3181673826. [DOI] [PubMed] [Google Scholar]