Abstract
Objective
To evaluate the use of the emergency department (ED) by elderly patients, their non-urgent visits and the prevalence of main disease for ED visits.
Methods
This cross-sectional study was conducted on patients aged 65 years and over who visited the ED of a tertiary care university hospital in Turkey between January 2015 and January 2016 retrospectively.
Results
A total of 36,369 elderly patients who visited the ED were included in the study. The rate of ED visits by elderly patients was higher than their representation within the general population (p < 0.001). While the rate of elderly patients visiting polyclinics was 15.8%, the rate of elderly patients visiting the ED was 24.3% (p < 0.001). For both genders, the rates of ED visits for patients between 65 and 74 years old was higher than for other elderly age groups (p < 0.001). The prevalence of upper respiratory tract infection (URTI) was the highest within the elderly population (17.5%, CI: 17.1–17.9). The proportion of ED visits for non-urgent conditions was 23.4%. Most of the ED visits were during the non-business hours (51.1%), and they were highest in the winter season (25.9%) and in January (10.2%). The hospitalization rate was 9.4%, and 37.9% of hospitalized patients were admitted to intensive care units.
Conclusion
The proportion of ED visits by elderly patients was higher than their representation within the general population. Elderly patients often visited the ED instead of a polyclinic. The rate of inappropriate ED use by elderly patients in this hospital was higher than in other countries.
Keywords: Non-urgent, Prevalence, Visit, Main disease, Elderly patient, Emergency department
1. Introduction
The World Health Organization (WHO) defines an elderly person as one who has a chronological age of 65 years or more.1 Life expectancy and the proportion of the elderly population are increasing worldwide. The population in Turkey is also aging rapidly. In fact, by 2050, it is expected that Turkey will have the highest percentage of elderly population in Europe.2 An emergency department (ED) provides a critically important service to elderly people, and accurately projecting the demographic characteristics of elderly patients who visit EDs is essential for planning ED health care. In the last few years, EDs have seen a dramatic increase in the number of visits from elderly patients. Although EDs are places of first intervention for emergency cases, patients frequently use EDs for non-urgent conditions, such as to obtain immediate tests and to receive medications to relieve symptoms. This may appear appropriate from the patient's perspective. However, these cases are better managed at polyclinics and primary health care institutions, and their treatment in EDs may compromise the treatment of true emergency cases.3 In the literature, research on elderly patients' inappropriate user of the ED is limited. To the best of our knowledge, this study is the first in Turkey to investigate elderly patients' inappropriate use of the ED.
The aim of this study was to evaluate elderly patients' demographic characteristics, their pattern of ED use, the rate of their non-urgent visits, and their main presenting diseases for ED visits.
2. Material and methods
2.1. Study design and settings
A retrospective, cross-sectional study was conducted on elderly patients who visited the ED between 1 January 2015 and 1 January 2016 at a 400-bed rural city hospital. The bed capacities of the hospital in the ED observational unit, intensive care unit, coronary care unit (CCU), internal intensive care unit, and surgical intensive care unit are 20, 15, 15, 15, and 21, respectively. This study was conducted according to principles of Helsinki Declaration. Due to retrospective nature, ethical committee approval for this study did not require.
2.2. Data sources
The data were collected from electronic hospital medical records and patient ED charts, including the patients' demographic characteristics (age, gender, and place of residence), presenting complaint and ED diagnosis, and outcome, including discharge and hospitalization rates and the date, season, and times of the ED visits.
2.3. Study population
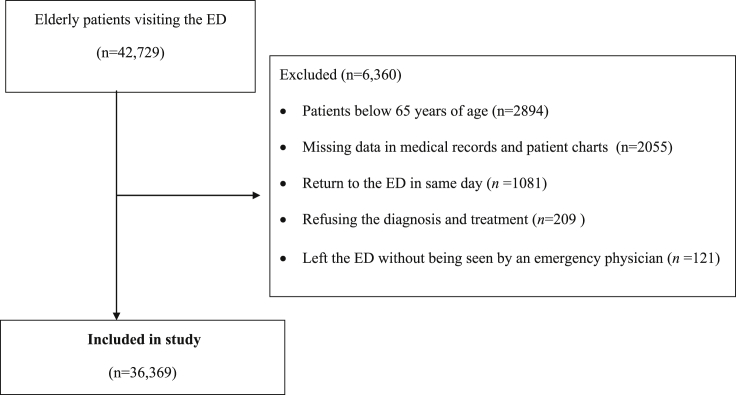
Elderly patients who visited the ED were eligible for inclusion in the study. Patients below 65 years of age, who returned to the ED in same day, whose medical records and patient charts were missing data, who left the ED without being seen by an emergency physician, or who refused the diagnosis and treatment were excluded from the study.
2.4. Outcome measures
The primary outcome measures were the prevalence of presenting diseases for elderly patients' ED visits. The secondary outcome measure was the demographic characteristics of the ED patients aged 65 years and over.
2.5. Definitions
The time of presentation was classified as business hours (07:00–16:59 h) (morning shift) and non-business hours (17:00–6:59 h) (evening and night shift). The main complaints and diseases were defined according to the International Classification of Disease-10 (ICD-10). The ICD-10 categories were classified into the following groups: diseases of the musculoskeletal system, respiratory system, genitourinary system, cardiovascular system, gastrointestinal system, neurological system, endocrine system, genitourinary system, and injury and trauma, psychiatric diseases, and poisoning and intoxication. According to WHO classification, patients were divided into three groups by age: 65–74 years, 75–84 years, and 85 years and older. Outpatient visits except the ED clinic were defined as polyclinic visits.
We determined the non-urgent illnesses retrospectively by medical record review of ED older patients. Non-urgent injuries or diseases were defined as the presence of non-urgent complaints and diseases which not require urgent investigation or treatment, not require remaining in observation. Inappropriate use of ED were classified as patients with non-urgent injuries or diseases that could be treated elsewhere.4
This study was verified according to the checklist for observational studies in Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). This study was recorded to clinicaltrials.gov (ID # NCT02734381).
2.6. Statistical analysis
The variables were presented as mean ± standard deviation (SD) or median (IRQ), where applicable. The Kolmogorov–Smirnov test was used to determine normality, and the Levene test was used to assess variance homogeneity. The differences in means between the groups were compared using the Student's t-test, and the Mann–Whitney U test was used to compare the medians. The categorical variables were analyzed by the chi-square test (χ2).
All of the hypotheses were constructed as two-tailed, and a 95% confidence interval (CI) was used to express the study variables. The study variables were analyzed by SPSS v17.0 and an online calculator (Evan's Awesome-http://www.evanmiller.org/ab-testing/chi-squared.html#). Values of p < 0.05 were considered statistically significant.
3. Results
A total of 42,729 elderly patients who visited the ED were evaluated, and 6360 (14.9%) were excluded for a variety of reasons, for a total of 36,369 included patients (Fig. 1). The demographic and clinical characteristics of the elderly patients who visited the ED are summarized in Table 1.
Fig. 1.
Patient flow diagram (n: number of patients, ED: emergency department).
Table 1.
The characteristics of elderly patients visiting the emergency department.
| Variables | n = 36,369 |
|---|---|
| Age (years), [mean ± SD (min–max)] | 74.87 ± 7.15 (65–115) |
| Gender, [n(%)] | |
| Female | 20,013 (55) |
| Male | 16,356 (45) |
| Place of residence, [n(%)] | |
| Inner-city | 29,221 (80.3) |
| Village | 3861 (10.6) |
| District | 1977 (5.4) |
| Unknown | 1209 (3.3) |
| Other city | 101 (0.3) |
| Time of presentation, [n(%)] | |
| Non-business hours (17:00–07:59) | 18,577 (51.1) |
| Business hours (08:00–16:59) | 17,792 (48.9) |
| Season, [n(%)] | |
| Winter | 9429 (25.9) |
| Spring | 9025 (24.9) |
| Summer | 9000 (24.7) |
| Autumn | 8915 (24.5) |
| Inappropriate use of ED | 8496 (23.4) |
SD: standard deviation, min: minimum, max: maximum, n: number of cases. ED: emergency department.
The total population of Adiyaman was 602,774 and the total elderly population was 42,958 (7.1%) in 2015 (see Table 2). During the study period, 149,928 general patients visited the ED, 36,369 (24.3%) of whom were elderly patients. The rate of ED visits by elderly patients was higher than representation within their the general population (p < 0.001). While rate of elderly patients visiting the polyclinics was 15.8%, the rate of elderly patients visiting the ED was 24.3%, and this difference was significant (p < 0.001, OR: 0.4, 95% CI: 0.39–0.45).
Table 2.
The distribution of polyclinic and the emergency department visits by age.
| Age | Polyclinic visits (n = 406,892) | ED visits (n = 149,928) | p-value | OR (95% CI) |
|---|---|---|---|---|
| ≥65 year, n (%) | 64,422 (15.8) | 36,369 (24.3) | <0.001 | 0.4 (0.39–0.45) |
| <65 year, n (%) | 342,470 (84.2) | 113,519 (75.7) |
ED: emergency department, OR: odds ratio, CI: confidence interval.
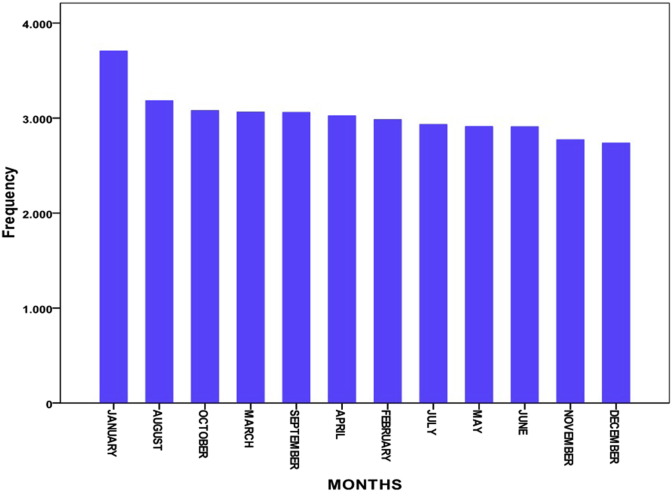
The mean age of elderly patients who visited the ED was 74.87 ± 7.15 years (65–115 years); they were 45% male (n = 16,356) and 55% female (n = 20,013), with a ratio of 1:1.2 (Table 1). Most of the elderly patients who visited the ED (n = 29,221, 80.3%) were living in the inner city. The number of ED visits during the night and evening (non-business hours) were higher than in the morning (business hours) (p < 0.001). The number of elderly patients' ED visits was higher in the winter (n = 9,429, 25.9%, p = 0.001) (Table 1) and the highest in January (n = 3,706, 10.2%, p < 0.001) (Fig. 2). The proportion of elderly patients to the total number of ED visits, according to gender and age, are shown in Table 3. The mean age was 74.9 ± 6.6 years for males and 74.8 ± 7.5 years for females. For both genders, the rates of ED visits for the 65–74 age group were higher than for other elderly age groups (p < 0.001).
Fig. 2.
The distribution of emergency department visits by month.
Table 3.
Proportional rates in emergency department visits of the elderly patients by age and gender group.
| Age groups | Visits by elderly patient to ED | Rates in age groups of total elderly female (n = 20, 013) and male (n = 16,356) % | Rates of the aged by age groups during study period by total ED visits (n = 149,928) % |
|---|---|---|---|
| Female | |||
| 65–74 | 11,172 | 55.8 | 7.5 |
| 75–84 | 6265 | 31.3 | 4.2 |
| ≥85 | 2576 | 12.9 | 1.7 |
| Total | 20,013 | 100 | 13.4 |
| Male | |||
| 65–74 | 8626 | 52.7 | 5.8 |
| 75–84 | 6443 | 39.4 | 4.3 |
| ≥85 | 1287 | 7.9 | 0.9 |
| Total | 16,356 | 100 | 11 |
ED: emergency department.
The most common presenting disease was upper respiratory tract infection (URTI) (n = 6,364, 17.5%, CI: 17.1–17.9), followed by chest pain (n = 5,282, 14.5%, CI: 14.2–14.9), injury (n = 4,264, 11.7%, CI: 11.4–12.1), myalgia (n = 3,232, 8.9%, CI: 8.6–9.2), and lower respiratory tract infection (LRTI) (n = 2,577, 7.1%, CI: 6.8–7.4). When disease prevalence was considered according to gender and age group, URTI was the most prevalent in the 65–74 age group for both genders and chest pain was the most prevalent for patients between 75 and 84 and ≥ 85 for both genders. The prevalence of the five most frequently seen diseases according to age group and gender is shown in Table 4.
Table 4.
Prevalence of the most frequently seen diseases by age and gender.
| Diseases | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | N | URTI (n = 6364) n (%) | 95% CI | Chest Pain (n = 5282) n (%) | 95% CI | Injury (n = 4264) n (%) | 95% CI | Myalgia (n = 3232) n (%) | 95% CI | LRTI (n = 2577) n (%) | 95% CI |
| Male | |||||||||||
| 65–74 years | 5765 | 1662 (28.8) | 27.7–30.0 | 1080 (18.7) | 17.7–19.8 | 873 (15.1) | 14.2–16.0 | 805 (14.0) | 13.1–14.9 | 821 (14.2) | 13.4–15.2 |
| 75–84 years | 4292 | 1013 (23.6) | 22.4–24.9 | 1014 (23.6) | 22.4–24.9 | 808 (18.8) | 17.7–20.0 | 535 (12.5) | 11.5–15.5 | 527 (12.3) | 11.3–13.3 |
| ≥85 years | 834 | 140 (16.8) | 14.4–19.9 | 222 (26.6) | 23.7–29.7 | 155 (18.6) | 16.1–21.4 | 112 (13.4) | 11.3–15.9 | 155 (18.6) | 16.1–21.4 |
| Total | 10,891 | 2815 (25.9) | 25.0–26.7 | 2316 (21.3) | 20.5–22.0 | 1836 (16.9) | 16.2–17.6 | 1452 (13.3) | 12.7–14.0 | 1503 (13.8) | 13.2–14.5 |
| Female | |||||||||||
| 65–74 years | 7190 | 2177 (30.3) | 29.2–31.4 | 1459 (20.3) | 19.4–21.2 | 1214 (16.9) | 16–17.8 | 1011 (14.1) | 13.3–14.9 | 567 (7.9) | 7.3–8.5 |
| 75–84 years | 4187 | 1006 (24.0) | 22.8–25.3 | 1029 (24.6) | 23.3–25.9 | 874 (20.9) | 19.7–22.1 | 526 (12.6) | 11.6–13.6 | 357 (8.5) | 7.7–9.4 |
| ≥85 years | 1705 | 366 (21.5) | 19.6–23.5 | 478 (28.0) | 26.0–30.2 | 340 (19.9) | 18.1–21.9 | 243 (14.3) | 12.7–16.0 | 150 (8.8) | 7.5–10.2 |
| Total | 13,082 | 3549 (27.1) | 31.7–33.5 | 2966 (22.7) | 22.0–23.4 | 2428 (18.6) | 17.9–19.2 | 1780 (13.6) | 13.0–14.2 | 1074 (8.2) | 7.8–8.7 |
URTI: Upper respiratory tract infection, LRTI: Lower respiratory tract infection, CI: confidence interval.
Elderly patients' most common presenting complaints were throat pain (n = 6364), chest pain (n = 5282), extremity injuries (n = 4264), myalgia (n = 3232), abdominopelvic pain (n = 1348), hypertension (n = 964), diabetes mellitus (n = 921), food poisoning (n = 280), urinary tract infections (n = 381), and anxiety (n = 133). After the inappropriate use of the ED was classified according to whether a non-urgent disease or injury could be treated elsewhere, the rate of inappropriate ED visits was 23.4% (n = 8496).
Of the 36,369 elderly patients who visited the ED, 3416 (9.4%) were hospitalized, 23,130 (63.6%) were discharged without ED observation, 9218 (25.3%) were discharged after ED observation, 289 (0.8%) were transferred to another hospital, 46 (0.1%) died in the ED, and 270 (0.7%) died after admission to the hospital. Of the 3416 the elderly patients who were hospitalized, 2121 (62.1%) were admitted to service wards and 1295 (37.9%) were admitted to intensive care units. Just over half of admissions to intensive care units were to the coronary care unit (n = 704, 54.4%).
The proportion of elderly patients admitted to surgery service ward was 24.3% (n = 515), and the most common surgery service ward was orthopedics and traumatology (n = 209, 40.6%), followed by general surgery (n = 122, 23.7%), thoracic surgery (n = 54, 10.5%), and neurosurgery (n = 44, 8.5%). The proportion of elderly patients who were admitted to internal services was 75.7% (n = 1606), and the most common internal service was cardiology (n = 601, 37.4%), followed by neurology (n = 345, 21.5%), pulmonary disease (n = 343, 21.4%), and internal medicine (n = 149, 9.3%).
4. Discussion
To date, in Turkey, a study comparing the elderly patients' visits between the ED and polyclinic has not been conducted. This study suggested that the number of elderly patients visiting the ED was higher than the number of elderly patients visiting polyclinics. Additionally, the rate of ED visits by elderly patients was nearly three times higher than their representation within the general population. A reason for this may be that elderly patients prefer to use the ED rather than a polyclinic because laboratory and radiographic investigations are obtained more quickly, the fees are lower in EDs in Turkey, when compared to polyclinics, and all patients are investigated for diagnosis and treatment whether their admission is urgent or appropriate.
Earlier studies have shown the percentage of ED visits by elderly patients to be between 3.6 and 28.5%.5, 6, 7, 8, 9, 10 In the present study, elderly patients accounted for approximately one quarter of all ED visits (24.3%) and female elderly patients constituted an even higher proportion of the ED patient population. When was considered that estimated life expectancy for females is longer than for males,8 this rate the is an expected result.
The majority of elderly patients visited the ED during non-business hours (the evening and night), which was also found in the literature.8, 11, 12 One explanation for this is that relatives who take care of elderly patients are usually at work during business hours and can only care for elderly patients during the non-business hours.
The highest rate of ED visits was during the winter months. This is consistent with the results of previous studies.8, 12 For both genders, the rates of total ED visits was higher in the 65–74 age group years than in other age groups. This is an expected result, according to population registration system based to address of The Statistical Institute of Turkey, because this age group has the highest population of elderly people in city where this study was conducted.13 In the present study, and in line with Satar et al,14 the majority of elderly patients presenting to the ED came from the inner city, We assume that This situation may indicate that living in the inner city may help to facilitate ED utilization for elderly patients.
Many studies have been conducted on elderly patients' presenting diseases to EDs in different countries. In France, a study reported that the main reason for ED admission was cardiopulmonary diseases, in 31.6% of cases, followed by neuropsychiatric disorders, 28.2%, and falls, 8.3%.15 In the United States, a study found that the most common diagnoses in elderly patients were chest pain (24.0%), dehydration (11.7%), and syncope (6.5%).16 In Belgium, a study found that the most common complaints were general condition impairment (21.5%), dyspnea (15.0%), and falls and traumas (15.0%).17 In Turkey, a study by Keskinoglu et al12 reported that diseases related to the circulatory and the respiratory systems were the most common presenting conditions. Yet another study in Turkey found that the most frequent reasons for ED admission were hypertension, cardiac and pulmonary disorders, URTIs, and urinary tract infections.8
In Australia, a study by Ingarfield et al18 showed that elderly patients were more likely to be diagnosed with pneumonia/influenza (95% CI: 1.72–2.19), urinary tract infections (95% CI: 1.49–1.98), and hip fractures (95% CI: 1.03–1.32). Furthermore, in Singapore, a study conducted by Foo et al19 reported that falls were the most common complaint among elderly patients, which increased their odds of getting admitted compared to the control group (OR: 1.9; 95% CI: 1.4–2.6), and a similar report from the Italy revealed that older trauma patients have high odds (OR: 5.12, 95% CI: 3.34–7.85).20 In the present study, the most common diseases and complaints in elderly patients were URTI (17.5%, CI: 17.1–17.9), chest pain (14.5%, 95% CI: 14.2–14.9), injury (11.7%, 95% CI: 11.4–12.1), myalgia (8.9%, 95% CI: 8.6–9.2), and LRTI (7.1%, 95% CI: 6.8–7.4). The prevalence of chest pain was higher in the 75–84 and ≥ 85 age groups than in the 65–74 age group, whereas the prevalence of URTI was higher in the 65–74 age group. These differences among studies may result from the variations in hospital qualifications (university hospital, tertiary care hospital, or state hospital), the elderly patient profiles of the regions in which the studies were conducted, socio-cultural differences between cities and countries, the demographic and clinical characteristics of the population that the hospitals serve, and whether the hospital is a trauma center. Our hospital is not an advanced trauma center, and trauma patients are rarely referred to our hospital from other city hospitals.
According to a systematic review, the use of EDs for non-urgent conditions may lead to excessive health care spending, unnecessary testing and treatment, and ED crowding.21 There are few published studies on elderly patients' inappropriate ED use, and no data are available on elderly patients' inappropriate ED use in Turkey. Faulkner et al22 indicate that the increasing elderly population may lead to an increase in inappropriate ED use.
According to the National Hospital Ambulatory Medical Care Survey in the United States, 4.4% of ED visits made by elderly patients were non-urgent.23 A study by Yim et al24 found that the total proportion of non-urgent visits in three Hong Kong EDs was less than 5%. Another study by Salvi et al20 on older patients visiting the ED in Italy reported that the proportion of non-urgent visits was 3%. However, the present study found this rate to be much higher (23.4%). The organization of the health care system in Turkey is different than it is in those countries—in Turkey, all patients seeking medical care, whether an emergency case or not, can visit the ED without needing to visit a primary health care facility or being first examined by a family physician. Thus, the health care system in Turkey might exacerbate the high rate of inappropriate ED use.
In the present study, the proportion of elderly patients hospitalized after admission to ED was 9.4%. Of these patients, 37.9% were admitted to intensive care units. Previous studies have reported the percentage of the elderly patients hospitalized to be between 11.5 and 69.0%2, 6, 7, 8, 17 and the rate of admission intensive care units to account for 13.6–70.4% of hospitalized elderly patients.6, 7, 8, 14 In present study, the most common services for hospitalized elderly patients were, in decreasing order, orthopedics and traumatology, cardiology, general surgery, and neurology, which is consistent with the results of other studies.6, 14, 25
5. Limitations
This study is limited because it is a single-center study, which may not make it representative of all elderly patients in Turkey. However, this study gives a general idea about these patients' ED visits in Turkey. Because of retrospective nature of this study, the length of stay in the ED could not be evaluated. Additional multi-center, prospective studies are needed to gain more clarity about elderly patients' non-urgent visits in Turkey.
6. Conclusion
Emergency physicians' knowledge regarding the clinical characteristics of elderly patients is important for their ability to provide emergency care. The ED visits by elderly patients have increased, and they often visit EDs instead of polyclinics. These visits are more frequent during non-business hours. The inappropriate ED use by elderly patients is higher in this hospital, where study was conducted, than in other countries. We believe that this high rate may result from the current health care system in Turkey.
Most emergency physicians have not been thoroughly trained in approaches to geriatric care. This study may provide some guidance for emergency physicians on the correct diagnosis and approach to the emergency treatment of elderly patients in Turkey.
Conflict of interest disclosure
No conflict of interest was declared by the authors.
Funding disclosure
The authors declared that this study has received no financial support.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
Contributor Information
Umut Gulacti, Email: umutgulacti@gmail.com.
Ugur Lok, Email: ugurlok@hotmail.com.
Murat Celik, Email: mcelik@hotmail.com.
Nurettin Aktas, Email: nurettin-aktas@hotmail.com.
Haci Polat, Email: dr.polat@hotmail.com.
References
- 1.World Health Organization (WHO) Definition of an Older or Elderly Person. http://www.who.int/healthinfo/survey/ageingdefnolder/en/. Accessed 2 May 2016.
- 2.Özşaker E., Demir-Korkmaz F., Dölek M. Analyzing individual characteristics and admission causes of elderly patients to emergency departments. Turkish J Geriatr. 2011;14(2):128–134. [Google Scholar]
- 3.Carret M.L., Fassa A.C., Domingues M.R. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica. 2009;25(1):7–28. doi: 10.1590/s0102-311x2009000100002. [DOI] [PubMed] [Google Scholar]
- 4.Coleman P., Irons R., Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency? Emerg Med J. 2001;18:482–487. doi: 10.1136/emj.18.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saritas A., Kandis H., Baltaci D. Approach to geriatric patients in emergency services. JAEM. 2013;12:93–97. [Google Scholar]
- 6.Baz Ü., Satar S., Kozaci N., Açikalin A., Gülen M., Karakurt Ü. Geriatric patient admissions to the emergency service. JAEM. 2014;13:53–57. [Google Scholar]
- 7.Logoglu A., Ayrik C., Kose A. Analysis of non-traumatic elderly patient presentations to the emergency department. Turk J Emerg Med. 2013;13(4):171–180. [Google Scholar]
- 8.Unsal A., Ayranci U., Alper Cevik A., Metintas S., Arslantas D., Unluoglu I. Use of emergency departments by elderly patients in a city of Western Turkey. Eur J Emerg Med. 2007;14(3):125–129. doi: 10.1097/MEJ.0b013e3280111f99. [DOI] [PubMed] [Google Scholar]
- 9.Latham L.P., Ackroyd-Stolarz S. Emergency department utilization by older adults: a descriptive study. Can Geriatr J. 2014;17(4):118–125. doi: 10.5770/cgj.17.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang J.A., Weng R.H., Tsai W.C., Hu W.H., Yang D.Y. Analysis of emergency department utilization by elderly patients under National Health Insurance. Kaohsiung J Med Sci. 2003;19(3):113–120. doi: 10.1016/S1607-551X(09)70458-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pitts S.R., Niska R.W., Xu J., Burt C.W. National hospital ambulatory medical care Survey: 2006 emergency department summary. Natl Health Stat Rep. 2008;7:1–38. [PubMed] [Google Scholar]
- 12.Keskinoğlu P., Inan F. Analysis of emergency department visits by elderly patients in an urban public hospital in Turkey. J Clin Gerontol Geriatr. 2014;5(4):127–131. [Google Scholar]
- 13.Statistical Institute of Turkey. Population Registration System Based to Address. http://www.tuik.gov.tr/PreTablo.do?alt_id=1059. Accessed 2 May 2016.
- 14.Satar S., Sebe A., Avcı A., Karakuş A., İcme F. Emergency department and the elderly patient. Cukurova Universitesi Tıp Fakultesi Dergisi. 2004;29:43–50. [Google Scholar]
- 15.Onen F., Abidi H., Savoye L., Elchardus J.M., Legrain S., Courpron P.H. Emergency hospitalization in the elderly in a French university hospital: medical and social conditions and crisisfactors precipitating admissions and outcome at discharge. Aging (Milano) 2001;13(6):421–429. [PubMed] [Google Scholar]
- 16.Ross M.A., Compton S., Richardson D., Jones R., Nittis T., Wilson A. The use and effectiveness of an emergency department observation unit for elderly patients. Ann Emerg Med. 2003;41(5):668–677. doi: 10.1067/mem.2003.153. [DOI] [PubMed] [Google Scholar]
- 17.Vanpee D., Swine C., Vandenbossche P., Gillet J.B. Epidemiological profile of geriatric patients admitted to the emergency department of a university hospital localized in a rural area. Eur J Emerg Med. 2001;8(4):301–304. doi: 10.1097/00063110-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Ingarfield S.L., Finn J.C., Jacobs I.G. Use of emergency departments by older people from residential care: a population based study. Age Ageing. 2009;38(3):314–318. doi: 10.1093/ageing/afp022. Epub 2009 Mar 12. [DOI] [PubMed] [Google Scholar]
- 19.Foo C.L., Chan K.C., Goh H.K., Seow E. Profiling acute presenting symptoms of geriatric patients attending an urban hospital emergency department. Ann Acad Med Singap. 2009;38(6):515–516. [PubMed] [Google Scholar]
- 20.Salvi F., Mattioli A., Giannini E. Pattern of use and presenting complaints of older patients visiting an Emergency Department in Italy. Aging Clin Exp Res. 2013;25(5):583–590. doi: 10.1007/s40520-013-0112-z. Epub 2013 Aug 15. [DOI] [PubMed] [Google Scholar]
- 21.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. Deciding to visit the emergency department for non-urgent conditions: a systematic review of the literature. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 22.Faulkner D., Law J. The ‘unnecessary’ use of emergency departments by older people: findings from hospital data, hospital staff and older people. Aust Health Rev. 2015;39(5):544–551. doi: 10.1071/AH14185. [DOI] [PubMed] [Google Scholar]
- 23.Hing E., Hall M.J., Ashman J.J., Xu J. National hospital ambulatory medical care Survey: 2007 outpatient department summary. Natl Health Stat Rep. 2010;28:1–32. [PubMed] [Google Scholar]
- 24.Yim V.W., Graham C.A., Rainer T.H. A comparison of emergency department utilization by elderly and younger adult patients presenting to three hospitals in Hong Kong. Int J Emerg Med. 2009;2(1):19–24. doi: 10.1007/s12245-009-0087-x. Epub 2009 Feb 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kekeç Z., Filiz Koç F., Büyük S. Review of geriatric patients hospitalization in emergency department. Akademik Acil Tıp Dergisi. 2009;3:21–24. [Google Scholar]