Abstract
Background
Adverse childhood experiences (ACE) including childhood abuse and trauma increase depressive symptoms. The role of resilience and how it interacts with both ACEs and the potential development of depressive symptoms, including how race and ethnicity moderate these effects, are much less studied. The aims of this study were to examine: 1) whether there is a dose-response relationship between trauma and depressive symptoms; 2) whether early trauma affected European Americans (EA) and African Americans (AA) in a similar fashion; and 3) whether resilience mitigates the effect of trauma.
Methods
The present study comprised a cross-sectional study of subjects from a longitudinal cohort. All subjects were 19 years or older with traumatic experiences prior to age 18. Subjects were assessed for depressive symptoms as well as resilience.
Results
In 413 subjects enrolled, ACEs were significantly associated with depression severity in a dose-response fashion (p<0.001). Notably, AAs had lower depression scores at low to moderate levels of ACEs than EAs, but reported comparable levels of depression with severe exposure to ACEs (pInteraction=0.05). In both EAs and AAs, young adults with high and medium levels of resilience showed less depressive symptoms compared to those with low resilience (p<0.05).
Limitations
to consider are the cross-sectional design, possibility of other confounders, and potential for recall bias of this study.
Conclusion
While ACEs were significantly associated with severity of depression in a dose-response fashion, higher resilience mitigated the impact of childhood adversities on depressive symptoms in young adults. The results are encouraging, and guides research for therapeutics to boost resilience.
Keywords: adverse childhood experiences, depressive symptoms, resilience, race/ethnicity
Introduction
Adverse childhood experiences (ACEs), characterized by childhood maltreatment and household dysfunction, have been associated with multiple physical health impairments in adulthood, including heart disease, obesity and type 2 diabetes. (Felitti et al., 1998) Trauma exposure during early life has also been related to mental health issues later in life, including depression (Schulz et al., 2014; Wingo et al., 2010; Youssef et al., 2013b) and suicidality (Youssef et al., 2013a). For example, Youssef et al. found that childhood trauma exposures were significantly associated with both depressive symptoms and suicidal ideation in 1488 military personnel and veterans while controlling for the effects of combat exposure and posttraumatic stress disorder (PTSD) (Youssef et al., 2013b). Resilience, defined as qualities that enable one to thrive in the face of adversity, (Connor and Davidson, 2003) has been negatively associated with depressive symptoms and suicidal ideation, suggesting a protective effect (Youssef et al., 2013a; Youssef et al., 2013b). However, the role of resilience and how it interacts with both ACEs and the potential development of depressive symptoms, including how race and ethnicity moderate these effects, are much less studied.
The aims of the present study were to examine the following: 1) whether there is a dose-response relationship between number of trauma exposure in early life and depressive symptoms in young adulthood; 2) whether early trauma affected European Americans (EA) and African Americans (AA) in a similar fashion; and 3) whether resilience mitigates the effect of early trauma on the development of depression.
Methods
Subjects
The present study comprised of subjects from a longitudinal cohort that was established in 1989 to study the development of cardiovascular risk factors. All the subjects were recruited from the southeastern United States, who met the following criteria: (1) aged 5 to 16 years at the onset of the study; (2) African or European ancestry; and (3) healthy based on parental report or the child's medical history. Participants were classified as AAs if both parents reported being of African heritage and they considered themselves and their child to be AA, black, or Afro-American. Participants were classified as EAs if both parents reported that they were of European ancestry and they considered themselves and their child to be EA, white, or Caucasian, and not of Hispanic, Native American, or Asian descent. The study design and selection criteria have been described previously (Su et al., 2015).
At visit 15 (initiated at 2008), all subjects were 19 years or older and their traumatic experiences prior to age 18 were assessed by using the ACE questionnaire. Of 432 who were enrolled at visit 15, 413 completed the ACE questionnaire, including 192 EAs (99 males and 93 females) and 221 AAs (93 males and 128 females). There were no demographics differences (including age, gender, and ethnicity) between subjects who were included in the analysis (N=413) and those excluded (N=19) due to missing values. The Institutional Review Board at the Medical College of Georgia had given approval for the study. Informed consent was provided by all subjects or by parents if subjects were <18 years.
Demographics Measurements
Demographic data were collected. Childhood socioeconomic status (SES) was assessed by Hollingshead Four Factor Social Status Index on the basis of parental education level and occupation. (Hollingshead, 1981). The Hollingshead scores ranged from 14 to 66, with a higher value indicating a higher SES.
Assessment of Adverse Childhood Experiences
The assessment of participants' exposure to ACEs covered the first 18 years of their lives. The ACE questionnaire consists of 28 items divided into 3 categories and 10 subscales, including childhood abuse (emotional, physical and sexual), neglect (emotional and physical), and growing up with household dysfunction (substance abuse, mental illness, domestic violence, criminal household member, and parental marital discord). The definition of ACEs has been described previously. (Su et al., 2015) The ACE score (the number of 10 ACE subscales reported) was used to assess the cumulative effect of multiple ACEs, by classifying respondents into four groups: no exposure (0 ACEs, n=126), mild (1-2 ACEs, n=157), moderate (3-4 ACEs, n=75) and severe (≥5 ACEs, n=55) exposure.
Assessment of Depressive Symptoms
The Beck Depression Inventory (BDI) was used to assess depressive symptoms, a standardized scale providing a continuous measure of depressive symptoms. (Beck et al., 1996) This self-report instrument includes 21 items. Participants rate the severity of each symptom from 0 to 3. It has been used extensively in community samples and has satisfactory test-retest and internal consistency reliability.
Assessment of Resilience
Resilience was assessed using the Connor Davidson Resilience Scale (CD-RISC), which is a 25-item self-reported instrument that measure the ability to cope with stress and adversity, such as self-confidence, self-efficacy, self-control, optimism and spirituality/autonomy. (Connor and Davidson, 2003) The items are scored on a five-point Likert scale, ranging from “not true at all” (scored 0) to “true nearly all the time” (scored 4). The scale rates participants over the past month with a total score of the CD-RISC varying from 0 to 100, with higher scores reflecting higher resilience.
Statistical Analysis
All analyses were done using STATA software. Sociodemographic variables were characterized with descriptive statistics (t-test for continuous traits and χ2-test for categorical traits). Multiple linear regression models were used to estimate the associations of ACE scores and resilience (CD-RISC scores) with depressive symptoms (BDI scores). Covariates included age, race, sex, BMI and childhood SES (Hollingshead index). The ethnicity and gender differences were further tested by including the interaction of ACE scores with race and sex, respectively. Statistical significance required a two-sided p-value of ≤0.05. We conducted a priori power calculation using the G*Power software. (Faul et al, 2009) At a two-tailed α level of 0.05, the required sample size was N=408 to achieve a sufficient power of 0.8 for identifying an effect size as small as 0.027 (Cohen f2). Therefore, the current study (N=413) should have sufficient power to identify small to medium effects.
Results
A total of 413 subjects were included in the present study. The mean age (±SD) was 28.3±3.1 (age range: 19.4 – 36.8). Table 1 presents the descriptive characteristics of the subjects by ethnicity and gender. African Americans (AA) had significantly greater BMI and lower childhood SES than European Americans (EA) (p≤0.001). Men had lower BMI than women (p=0.003). The mean score on the BDI (±SD) was 6.7±7.7, with a minimum of 0 and a maximum of 39. The mean score on the CD-RISC (±SD) was 75.5±13.9, with a minimum of 27 and a maximum of 100. No significant differences on the BDI score or CD-RISC score were found between AAs and EAs, or between men and women.
Table 1. Descriptive characteristics of study participants (total N=413).
| Characteristic | Men | Women | Pgender | EA | AA | Prace |
|---|---|---|---|---|---|---|
| N | 192 | 221 | 192 | 221 | ||
| Age, y | 28.2 (3.3) | 28.5 (2.9) | 0.45 | 28.0 (3.0) | 28.7 (3.1) | 0.025 |
| Body mass index, kg/m2 | 29.2 (6.6) | 31.5 (9.8) | 0.005 | 29.0 (7.8) | 31.7 (9.0) | 0.002 |
| Hollingshead index | 41.9 (13.9) | 40.6 (13.1) | 0.33 | 45.2 (12.3) | 37.7 (13.6) | <0.00 1 |
| Depression symptoms (BDI score) | 6.6 (7.8) | 6.8 (7.7) | 0.77 | 6.5 (7.4) | 6.9 (8.0) | 0.60 |
| Resilience (CD-RISC score) | 75.4 (14.6) | 75.7 (13.3) | 0.86 | 74.4 (13.4) | 76.5 (14.3) | 0.12 |
Means and standard deviations (SD) are shown.
EA: European American; AA: African American; BDI: Beck Depression Inventory; CD-RISC: Connor-Davidson Resilience Scale
Prevalence of ACEs
The prevalence of each individual ACE subscale and ACE scores are shown in Table 2, with the lowest prevalence of physical neglect (9.0%) and the highest prevalence of parental marital discord (38.7%). Compared to women, men reported much higher rate of experiencing physical neglect during childhood (15.1% vs. 3.6%). Significant racial differences are evident in some of the ACE subscales (Table 2). Approximately 1 in 3 EA respondents reported that they lived with a household member who was mentally ill or attempted suicide, a rate twice as high as the rate reported by AA respondents (35.4% vs. 17.2%). However, AA respondents reported higher rates of other ACE subscales than EA respondents. For example, 1 in 8 AA respondents reported experiencing physical neglect as a child, a rate 2 times higher than the rate reported by EA respondents (12.2% vs. 5.2%). AA respondents also reported higher rates of (a) witnessing domestic violence (24% vs. 17.2%), (b) a household member who went to prison (21.3% vs. 9.9%) and (c) parental marital discord (47.1% vs. 29.2). Overall, the prevalence of any ACE event is relatively higher in AAs than that in EAs (73.3% vs. 65.1%, p=0.07). In summary, 69.5% of respondents reported at least one exposure to ACEs, with mild (1-2 ACEs), moderate (3-4 ACEs), and severe (≥5 ACEs) exposure to ACEs representing 38.0%, 18.2% and 13.3%, respectively (Table 2). The prevalence of ACE scores was not significantly different between men and women, although men showed a higher rate of severe exposure to ACEs than women (16.6% vs. 10.4). AAs had a relatively higher prevalence of moderate and severe exposure to ACEs compared to EAs (21.3% vs. 14.6% and 14.9% vs. 11.4% respectively).
Table 2. Prevalence of adverse childhood experiences (ACEs) by race and gender.
| ACE | All (N=413) | Men (N=99) | Women (N=93) | Pgender | EA (N=93) | AA (N=128) | Prace |
|---|---|---|---|---|---|---|---|
| % | % | % | % | % | |||
| Abuse | |||||||
| Emotional | 13.6 | 14.7 | 12.7 | 0.54 | 11.1 | 15.8 | 0.16 |
| Physical | 17.8 | 21.1 | 14.9 | 0.11 | 15.3 | 19.9 | 0.22 |
| Sexual | 16.1 | 16.8 | 15.5 | 0.72 | 15.2 | 16.8 | 0.65 |
| Neglect | |||||||
| Emotional | 11.4 | 12.5 | 10.4 | 0.50 | 10.9 | 11.8 | 0.79 |
| Physical | 9.0 | 15.1 | 3.6 | <0.00 | 5.21 | 12.2 | 0.013 |
| Household Dysfunction | |||||||
| Substance abuse | 27.1 | 29.2 | 25.3 | 0.38 | 25.5 | 28.5 | 0.49 |
| Mental illness | 25.7 | 26.6 | 24.9 | 0.70 | 35.4 | 17.2 | <0.00 1 |
| Domestic violence | 20.8 | 21.4 | 20.4 | 0.80 | 17.2 | 24.0 | 0.09 |
| Criminal household member | 16.0 | 16.2 | 15.8 | 0.93 | 9.9 | 21.3 | 0.002 |
| Parental marital discord | 38.7 | 42.2 | 35.8 | 0.18 | 29.2 | 47.1 | <0.00 1 |
| Any ACE | 69.5 | 69.8 | 69.2 | 0.90 | 65.1 | 73.3 | 0.07 |
| ACE score | |||||||
| 0 | 30.5 | 30.2 | 30.8 | 0.90 | 34.9 | 26.7 | 0.07 |
| 1-2 | 38.0 | 36.5 | 39.4 | 0.54 | 39.1 | 37.1 | 0.68 |
| 3-4 | 18.2 | 16.7 | 19.4 | 0.46 | 14.6 | 21.3 | 0.08 |
| 5+ | 13.3 | 16.6 | 10.4 | 0.06 | 11.4 | 14.9 | 0.30 |
EA: European American; AA: African American
Effects of ACEs on depressive symptoms
The effects of each individual ACE on depressive symptoms are shown in Table 3 by gender and race. This table presents beta coefficients from regression models in which BDI score was regressed on one ACE, controlling for age, gender, race, BMI and childhood SES. Seven of ten ACEs were significantly associated with reports of higher depressive symptoms in both men and women, as well as in EAs and AAs. Women were more vulnerable to emotional neglect compared to men (beta coefficients: 8.0 vs. 2.5; interaction p=0.02), while men reported higher depressive symptoms than women if some household member went to prison (beta coefficients: 5.2 vs. 1.1; interaction P=0.03). The most frequently experienced ACE – parental marital discord – was not related to depressive symptoms in any gender or race group. The impacts of ACEs on depressive symptoms were generally stronger in EAs than in AAs for a given ACE, although they were not statistically different.
Table 3. Individual effects of adverse childhood experiences (ACEs) on depressive symptoms by race and gender.
| ACE | Men | Women | EA | AA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Beta (SE) | Pmen | Beta (SE) | Pwomen | PInteraction | Beta (SE) | PEA | Beta (SE) | PAA | PInteraction | |
| Abuse | ||||||||||
| Emotional | 6.7(1. 6) | <0.0 01 | 8.3(1.4) | <0.0 01 | 0.37 | 9.8(1. 5) | <0.0 01 | 6.3(1.4) | <0.0 01 | 0.09 |
| Physical | 5.6(1. 4) | <0.0 01 | 6.1(1.4) | <0.0 01 | 0.73 | 7.6(1. 4) | <0.0 01 | 4.7(1.3) | <0.0 01 | 0.13 |
| Sexual | 4.8(1. 5) | 0.001 | 7.8(1. 3) | <0.001 | 0.15 | 7.8(1. 3) | 0.001 | 5.3(1. 4) | 0.002 | 0.15 |
| Neglect | ||||||||||
| Emotional | 2.5(1. 7) | 0.15 | 8.0(1.6) | <0.0 01 | 0.02 | 5.5(1. 7) | <0.0 01 | 5.2(1.7) | <0.0 01 | 0.87 |
| Physical | 9.4(1. 5) | <0.0 01 | 9.3(2.7) | 0.00 1 | 0.93 | 9.2(2. 3) | <0.0 01 | 9.1(1.6) | <0.0 01 | 0.77 |
| Household Dysfunction | ||||||||||
| Substance abuse | 5.0(1. 2) | <0.0 01 | 4.7(1.1) | <0.0 01 | 0.86 | 5.7(1. 1) | <0.0 01 | 4.0(1.2) | 0.00 1 | 0.24 |
| Mental illness | 4.7(1. 2) | <0.0 01 | 3.9(1.2) | 0.00 1 | 0.75 | 4.3(1. 0) | <0.0 01 | 4.6(1.4) | 0.00 1 | 0.90 |
| Domestic violence | 6.5(1. 4) | <0.0 01 | 4.7(1.2) | <0.0 01 | 0.42 | 3.4(1. 4) | 0.01 | 7.0(1.2) | <0.0 01 | 0.15 |
| Criminal household member | 5.2(1. 5) | 0.00 1 | 1.1(1.4) | 0.45 | 0.03 | 5.2(1. 7) | 0.00 3 | 2.3(1.3) | 0.09 | 0.10 |
| Parental marital discord | 1.0(1. 2) | 0.39 | 1.1(1.1) | 0.33 | 0.88 | 0.01(1.2) | 0.99 | 1.6(1.1) | 0.14 | 0.41 |
SE: standard error; EA: European American; AA: African American
Each model includes only one ACE subscale as predictor and controls for age, gender, race, BMI and childhood SES.
However, the cumulative effects of ACEs on depressive symptoms were significantly different between EA and AA respondents (interaction p=0.05). As shown in Table 4, after controlling for age, gender, BMI and childhood SES, the EA participants who reported mild, moderate, and severe exposure to ACEs (1-2, 3-4, 5+) had an average increase of 2.1, 7.3 and 11.1 points on BDI scores compared to those with no exposure to ACEs (p=0.05, <0.001 and <0.001 respectively), while the AA participants at the same ACE exposure levels showed an average increase of 0.8, 3.3 and 12.6 points on BDI scores compared to their counterparts without ACEs (p=0.5, 0.02 and <0.001 respectively). There was no significant gender-by-ACE interaction, suggesting that the cumulative effect of ACEs on depressive symptoms was similar between men and women.
Table 4. Cumulative effects of adverse childhood experiences (ACEs) on depressive symptoms by race and gender.
| ACE Score | Men | Wome n | EA | AA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Beta (SE) | Pmen | Beta (SE) | Pwomen | PInteraction | Beta (SE) | PEA | Beta (SE) | PAA | PInteraction | |
| 0 | Reference | Reference | 0.59 | Reference | Reference | 0.05 | ||||
| 1-2 | 1.2(1.2) | 0.31 6 | 1.7(1.1) | 0.11 4 | 2.1(1.0) | 0.05 | 0.8(1.2) | 0.50 | ||
| 3-4 | 5.4(1.5) | 0.00 1 | 4.7(1.3) | <0.0 01 | 7.3(1.4) | <0.0 01 | 3.3(1.4) | 0.02 | ||
| ≥5 | 11.7(1.6) | <0.0 01 | 13.4(1.6) | <0.0 01 | 11.1(1.6) | <0.0 01 | 12.6(1.6) | <0.0 01 | ||
SE: standard error; EA: European American; AA: African American
Each model includes ACE score as a categorical variable and controls for age, gender, race, BMI and childhood SES.
Role of resilience
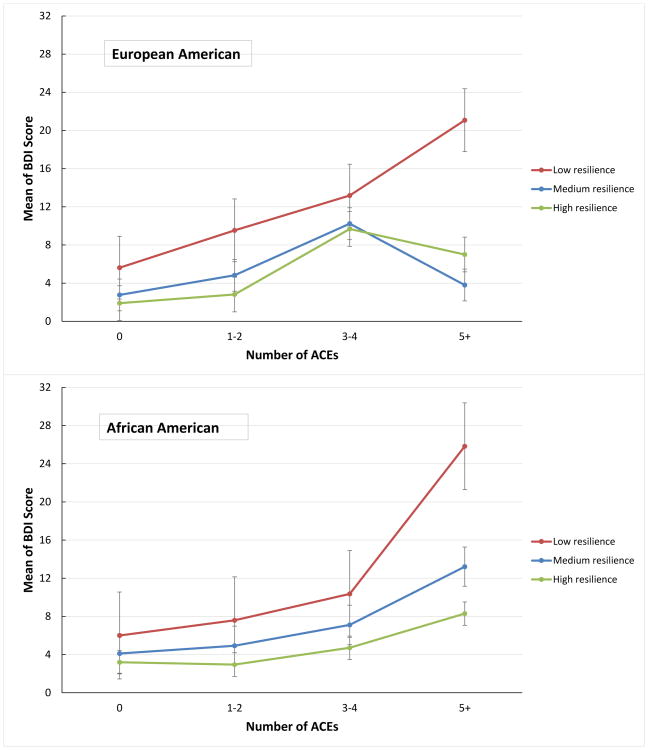
We next examined the role of resilience in the relationship between ACE exposure and depression. For a visual conceptualization of the interaction between childhood adversities and resilience, we divided resilience into 3 categories based on the percentile of the CD-RISC score: high resilience: CD-RISC score >75th percentile, medium resilience: CDRISC score >25th percentile and ≤75th percentile, and low resilience: CD-RISC score ≤25th percentile. We found a significant interaction between ACE scores and resilience on depressive symptoms (p<0.05). Given similar levels of childhood adversity exposure, in both EAs and AAs, the high and medium resilience group had lower BDI scores compared to the low resilience group (Figure 1), suggesting that resilience mitigates the tendency for developing depressive symptoms in young adults with a history of childhood adversities. There is no three-way interaction of race, ACE scores and CD-RISC scores on depressive symptoms, indicating that resilience is a protective factor in both EA and AA populations.
Figure 1. Depressive symptoms according to ACE scores by Conner-Davidson resilience scale (total score ≤25th percentile, >25th and <75th percentile, and ≥75th percentile) and race (European American or African American).
Discussion
This study has several findings that were expected, and some that were not. We found that exposure to ACEs was significantly associated with severity of depression in a dose-response fashion. Along the same lines, given similar levels of childhood trauma exposure, young adults with high and medium levels of resilience showed less depressive symptoms compared to those with low resilience, as previously reported in both active duty service members and veterans (Youssef et al., 2013b). Our results replicated and generalized previous findings to the civilian young adult population.
However, an interesting finding in this study is that depression was only markedly higher in AAs with severe ACEs but not in mild or moderate ACEs; showing a significant interaction by race (p=0.05). AAs in general have less depressive scores at low to moderate level of ACEs than EAs, except for the severe exposure to ACEs where both races where more comparable in the severity of depression.
Our results are consistent with previous literature in several ways. For example, in a community-based ethnically diverse cohort of young adults in South Florida, Turner and Lloyd observed that AA had generally experienced more adverse events than other ethnic groups but showed relatively lower prevalence of depressive disorder. (Turner and Lloyd, 2004) In a longitudinal survey in young adults, Schilling et al. found that when racial/ethnic differences exist, young EAs consistently exhibit greater vulnerability to ACEs. (Schilling et al., 2007) One possibility is the potential social or cultural differences in resilience between two ethnic groups. (Rutter, 1996)
However, the overall resilience scores are not different between two ethnic groups. Further adjustment for resilience scores didn't change the results, suggesting that this racial/ethnic difference may not be attributable to the social or cultural differences in resilience. Another possible explanation is that individuals from minority backgrounds may be less willing to disclose mental health symptoms, which are often stigmatized in AA communities. (2001) However, it is of note that AAs exhibited high depressive scores that were comparable to EAs as the number of stressful childhood events exceeds 5 or more, suggesting that high level of cumulative stress can have fairly equivalent negative effect on mental health for both AAs and EAs.
The protective role of resilience against stress and depression has been reported previously. For instance, a cross-sectional study of 792 predominantly African American men and women found that resilience moderated depressive symptom severity in individuals exposed to childhood abuse or other trauma (Wingo et al., 2010). Consistent with these findings, we also observed a significant interaction between ACE scores and resilience on depressive symptoms. In both EAs and AAs, young adults exposed to severe ACEs but with high levels of resilience showed less depressive symptoms compared to those with low resilience, suggesting that resilience mitigates the tendency for developing depressive symptoms in young adults with a history of childhood adversities.
There are several limitations to consider when interpreting the results of this study. First, given the cross-sectional design, the results cannot be interpreted in a cause-effect fashion, but only associations can be shown. Second, due to the observational design, the possibility of other potential confounding factors cannot be totally eliminated. Third, the potential effect of timing of traumatic experiences could not be examined, because information of the specific age of childhood trauma were not collected. Forth, the potential for recall bias of past childhood experiences is inevitable in this type of study. However, good test-retest reliability of recall of past childhood trauma, and stability over time has been shown (Dube et al., 2004). Examination against documented cases of childhood trauma showed that inconsistencies are likely to be due to under-reporting rather than over-reporting of the trauma (Della Femina et al., 1990; Dube et al., 2004; Hardt and Rutter, 2004).
Conclusion
While exposure to ACEs was significantly associated with depression severity, higher resilience mitigated the impact of childhood adversities on depressive symptoms in young adults. AAs exposed to low to moderate level of ACEs had less depressive symptoms than EAs while at high level of stress they exhibited similar severity of depression compared to EAs. This study provides useful information in the clinical assessment of patients with ACE and depression. The results of our study are encouraging, and guides further research for promising therapies to boost resilience and potentially decrease depressive symptoms.
Highlights.
ACEs are associated with depression severity.
AAs had lower depression at low to moderate levels of ACEs than EAs.
But AAs and EAs had comparable levels of depression with severe exposure to ACEs.
High and medium levels of resilience mitigated the impact of ACEs on depressive symptoms in young adults.
Acknowledgments
We thank Grant Zackary for his assistance in preparation of a subsection of this manuscript. We acknowledge the continued cooperation and participation of the members of the study and their families and thank the tireless staff at the Georgia Prevention Institute.
Funding: This research was supported in part by the National Institutes of Health Program Project Grant on Stress-Related Mechanisms of Hypertensive Risk (P01 HL69999 to FAT). Dr. Su is funded by the American Heart Association (09SDG2140117) and the NIH (HL106333-01A1 and HL125577-01). Dr. Youssef received research support from the Department of Veteran Affairs and The Augusta Biomedical Research Corporation.
Footnotes
Declaration of Interest: Dr. Youssef disclosure include Speaker CME honoraria from the Georgia Department of Behavioral Health and Developmental Disabilities (DHBDD).
Contributors: Nagy Youssef contributed to the conceptualization of the analysis and interpretation of the results and wrote the first draft of this manuscript and subsequent revisions. Shaoyong Su contributed to the performance of the statistical analysis and interpretation of the results and helped in writing the first draft of this manuscript and subsequent revisions. Daniel Belew, Guang Hao, Xiaoling Wang, Frank A. Treiber, Michael Stefanek, Mark Yassa, Elizabeth Boswell, W. Vaughn McCall helped in writing and editing this manuscript and contributed intellectually to this manuscript. All authors have approved the final article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nagy A. Youssef, Email: nyoussef@augusta.edu.
Shaoyong Su, Email: ssu@augusta.edu.
References
- 1.(US), O.o.t.S.G.U.C.f.M.H.S.U.N.I.o.M.H. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Substance Abuse and Mental Health Services Administration (US); Rockville (MD): 2001. [PubMed] [Google Scholar]
- 2.Beck AT, Steer RA, Brown G. Beck Depression Inventory–II. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- 3.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 4.Della Femina D, Yeager CA, Lewis DO. Child abuse: adolescent records vs. adult recall. Child Abuse Negl. 1990;14:227–231. doi: 10.1016/0145-2134(90)90033-p. [DOI] [PubMed] [Google Scholar]
- 5.Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28:729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 6.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 9.Hollingshead A. Four Factor Index of Social Status. Department of Sociology: New Haven, Conn; 1981. [Google Scholar]
- 10.Rutter M. Stress research: Accomplishments and tasks ahead. In: Haggerty RJ, Sherrod LR, Garmezy N, Rutter M, editors. Stress, risk, and resilience in children and adolescents: Processes, mechanisms, and interventions. Cambridge University Press; New York, NY, US: 1996. [Google Scholar]
- 11.Schilling EA, Aseltine RH, Jr, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7:30. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schulz A, Becker M, Van der Auwera S, Barnow S, Appel K, Mahler J, Schmidt CO, John U, Freyberger HJ, Grabe HJ. The impact of childhood trauma on depression: does resilience matter? Population-based results from the Study of Health in Pomerania. J Psychosom Res. 2014;77:97–103. doi: 10.1016/j.jpsychores.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Su S, Wang X, Pollock JS, Treiber FA, Xu X, Snieder H, McCall WV, Stefanek M, Harshfield GA. Adverse childhood experiences and blood pressure trajectories from childhood to young adulthood: the georgia stress and heart study. Circulation. 2015;131:1674–1681. doi: 10.1161/CIRCULATIONAHA.114.013104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner RJ, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults: racial and ethnic contrasts. Arch Gen Psychiatry. 2004;61:481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- 15.Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord. 2010;126:411–414. doi: 10.1016/j.jad.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Youssef NA, Green KT, Beckham JC, Elbogen EB. A 3-year longitudinal study examining the effect of resilience on suicidality in veterans. Ann Clin Psychiatry. 2013a;25:59–66. [PMC free article] [PubMed] [Google Scholar]
- 17.Youssef NA, Green KT, Dedert EA, Hertzberg JS, Calhoun PS, Dennis MF, Mid-Atlantic Mental Illness Research, E., Clinical Center, W. Beckham JC. Exploration of the influence of childhood trauma, combat exposure, and the resilience construct on depression and suicidal ideation among U.S. Iraq/Afghanistan era military personnel and veterans. Arch Suicide Res. 2013b;17:106–122. doi: 10.1080/13811118.2013.776445. [DOI] [PMC free article] [PubMed] [Google Scholar]