Abstract
Background
Disinfectant use among healthcare workers has been associated with respiratory disorders, especially asthma. We aimed to describe disinfectants used by U.S. nurses, and to investigate qualitative and quantitative differences according to workplace characteristics and region.
Methods
Disinfectant use was assessed by questionnaire in 8,851 nurses. Hospital characteristics were obtained from the American Hospital Association database.
Results
Working in a hospital was associated with higher disinfectant use (OR: 2.06 [95%CI: 1.89-2.24]), but lower spray use (0.74 [0.66-0.82]). Nurses working in smaller hospitals (<50 beds vs. ≥200 beds) were more likely to use disinfectants (1.69 [1.23-2.32]) and sprays (1.69 [1.20-2.38]). Spray use was lower in the West than in the Northeast (0.75 [0.58-0.97]).
Conclusion
Disinfectant use was more common among nurses working in smaller hospitals, possibly because they perform more diverse tasks. Variations in spray use by hospital size and region suggest additional targets for future efforts to prevent occupational asthma.
Keywords: healthcare workers, cleaning products, disinfectants, occupational asthma, hospital
Introduction
Healthcare workers experience high exposure levels to a wide range of cleaning and disinfecting products [Donnay et al., 2011; LeBouf et al., 2014; Saito et al., 2015]. While the frequency of disinfection tasks is increasing in hospitals to protect patients against healthcare-associated infections [Quinn et al., 2015], there is growing evidence that exposure to cleaning products and disinfectants increases risk of respiratory disorders, such as asthma [Siracusa et al., 2013; Dumas et al., 2014; Gonzalez et al., 2014; Vizcaya et al., 2015]. Although the specific causal agents are not well established [Siracusa et al., 2013; De Matteis & Cullinan, 2015], increased asthma risk has been associated with the use of bleach, quaternary ammonium compounds (quats), ammonia, products used to disinfect medical instruments and products in spray form [Delclos et al., 2007; Mirabelli et al., 2007; Arif & Delclos, 2012; Dumas et al., 2012; Gonzalez et al., 2014].
The U.S. has more than 3 million registered nurses, and nursing represents the largest healthcare profession [NSSRN, 2010; BLS, 2015]. Among healthcare workers, nurses have been identified as a subgroup with a higher risk for asthma [Kogevinas et al., 2007; Arif et al., 2009; Gonzalez et al., 2014]. Nurses perform many different tasks and are employed in various settings, but their work often involves disinfectant use [Arif et al., 2009; Gonzalez et al., 2014; Dumas et al., 2015; Saito et al., 2015].
To address health concerns related to cleaning products and disinfectant exposures in healthcare, a multidisciplinary group of experts have recently called for a more integrated approach in the development of infection control guidelines and work-related asthma prevention strategies, to ensure patients' security while minimizing adverse health effects among healthcare workers [Quinn et al., 2015]. For this purpose, a better knowledge of cleaning and disinfecting work practices in actual health care settings is warranted [Han et al., 2015; Quinn et al., 2015]. Indeed, many potentially hazardous chemicals are used for various disinfection tasks, but the workers' exposures and their determinants remain incompletely characterized. Results from a study conducted in three Veteran Affairs hospitals and two teaching hospitals in the U.S., including quantitative assessment of exposure to volatile organic compounds [LeBouf et al., 2014] and shift monitoring [Saito et al., 2015], were reported recently. The authors observed large variations in duration of exposures and chemicals used across healthcare occupations and activities. However, how exposures vary by workplace characteristics (e.g., hospital size, non-hospital settings) or geographic region is unknown. In addition, besides characterization of the chemical exposures (active ingredients), information regarding application procedures such as product spraying is of particular importance as changes in product application forms may offer opportunities for prevention [Le Moual et al., 2012; Vizcaya et al., 2015].
The Nurses' Health Study II (NHSII) is a large, ongoing, prospective study of U.S. female nurses. In the context of a study on asthma determinants within the NHSII, we collected detailed information regarding the participants' use of disinfectant and cleaning products at work. In the present paper, we describe the products used by U.S. nurses according to workplace characteristics and geographical region.
Material and methods
Population
The NHSII began in 1989 when 116,430 female registered nurses from 15 U.S. states, aged 25–44 years, completed a mailed questionnaire on their medical history and lifestyle characteristics [Camargo et al., 1999; Le Moual et al., 2013; Dumas et al., 2015]. Every 2 years, follow-up questionnaires have been sent to update information on potential risk factors and identify newly diagnosed diseases.
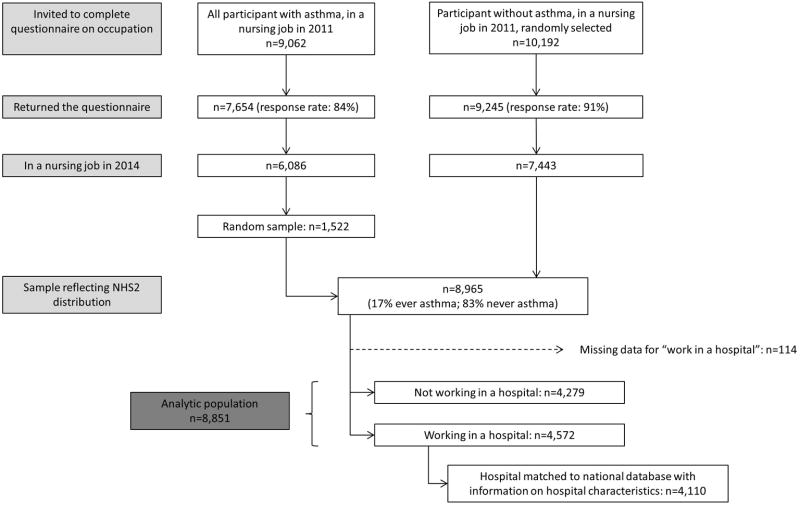
As a part of a larger project, we initiated a case-control study on asthma nested within the NHSII cohort in 2014. In this context, 9,062 nurses with asthma and a random sample of 10,192 nurses without asthma who were still in a nursing job at the most recent follow-up (2011) were invited to complete an occupational questionnaire (response rate: 84% and 91% for nurses with and without asthma, respectively; Figure 1). About 80% of the participants with asthma and 81% of the participants without asthma were still in a nursing job in 2014. For the present analysis that focuses on the use of cleaning products and disinfectants by U.S. nurses, we randomly selected a stratified sample of nurses according to asthma status (83% never asthma; 17% ever asthma), to reflect the distribution of all NHSII participants currently working in a nursing job.
Figure 1. Flow chart of study population.
This investigation was approved by the Institutional Review Board at the Brigham and Women's Hospital, Boston, Massachusetts, USA.
Tasks and products used for cleaning and disinfection
The occupational questionnaire collected information on the tasks performed and products used for cleaning and disinfection. Questions referred generally to cleaning (removal of soil using physical or chemical action) and/or disinfection (process of eliminating many or all pathogenic microorganisms) [Rutala et al., 2012; Quinn et al., 2015]. Questions were adapted to U.S. context from questionnaires used in European studies [Mirabelli et al., 2007; Donnay et al., 2011], with additions of relevant tasks based on results from a study of asthma among healthcare workers in Texas [Delclos et al., 2007]. Information on the frequency (never, <1 day/week, 1-3 days/week, 4-7 days/week) of cleaning and disinfecting tasks, and the use of specific cleaning products and disinfectants was collected. Two questions were included about general disinfection tasks: “Thinking about your current job and the use of disinfectants (such as ethylene oxide, hydrogen peroxide, ortho-phtalaldehyde, formaldehyde, glutaraldehyde and bleach): On how many days per week, on average, do you (a) clean medical instruments with disinfectants? (b) clean surfaces (like floors, tables) at work with disinfectants?”. Specific questions were asked about the use of sprays: “In your current job, on how many days per week, on average, do you use spray or aerosol products?”. Those who reported weekly use of sprays were asked to report tasks where they used sprays (patient care; instrument cleaning or disinfection; surface cleaning or disinfection; air-refreshing; other). Finally, questions were asked about the frequency of use of specific products: “On how many days per week do you use the following disinfectants at work?” with a list of 15 specific disinfectants or cleaning products (e.g., glutaraldehyde, bleach, quats; see Table II for complete list). Participants who did not know the active compound in the products they use could fill in the brand name instead (11% of the participants reported at least one brand name). We searched the safety data sheets of all provided brand names to determine the products' main active compounds and re-evaluated the nurses' exposure (for each ingredient) based on this additional information.
Table II. Disinfectant use among nurses according to type of workplace (n=8,851).
| Work in a hospital | ||||
|---|---|---|---|---|
|
| ||||
| No (n=4,279) | Yes (n=4,572) | OR | 95% CI | |
| Weekly use of disinfectants*, % | ||||
| To clean surfaces (n=4,352) | 40 | 58 | 2.06 | 1.89-2.24 |
| To clean instruments (n=1,669) | 15 | 23 | 1.70 | 1.53-1.90 |
| Weekly use of sprays*, % | ||||
| Any spray (n=1,668) | 21 | 17 | 0.74 | 0.66-0.82 |
| Spray for cleaning/disinfection† (n=1,169) | 16 | 12 | 0.72 | 0.63-0.81 |
| Weekly use of specific disinfectants / cleaning products‡, % | ||||
| Alcohol (n=3,235) | 35 | 41 | 1.31 | 1.20-1.43 |
| Hypochlorite bleach (n=1,571) | 17 | 24 | 1.61 | 1.45-1.79 |
| Quats (n=1,036) | 9 | 15 | 1.80 | 1.57-2.06 |
| Hydrogen peroxide (n=696) | 7 | 10 | 1.42 | 1.22-1.67 |
| Glutaraldehyde (n=555) | 6 | 7 | 1.26 | 1.06-1.50 |
| Formaldehyde (n=286) | 2 | 5 | 3.35 | 2.53-4.43 |
| Ortho-phtalaldehyde (n=353) | 3 | 5 | 1.59 | 1.28-1.98 |
| Enzymatic cleaners (n=284) | 3 | 4 | 1.47 | 1.16-1.88 |
| Phenolics (n=165) | 1 | 3 | 1.96 | 1.41-2.71 |
| “Green” products§ (n=375) | 6 | 4 | 0.60 | 0.48-0.74 |
| Peracetic acid (n=103) | 1 | 2 | 3.40 | 2.14-5.42 |
| Acetic acid (n=190) | 2 | 2 | 0.90 | 0.68-1.20 |
| Ammonia (n=99) | 1 | 1 | 1.20 | 0.81-1.79 |
| Ethylene oxide (n=33) | 0.3 | 0.5 | 1.91 | 0.93-3.95 |
| Chloramine T (n=17) | 0.1 | 0.3 | 1.77 | 0.65-4.78 |
Results in bold are statistically significant.
Missing for <1% of participants.
Use of spray for instrument or surface cleaning/disinfection
Range of missing values rates for specific disinfectants was 3% (quats) to 7% (“green” products).
“Green” products as evaluated by the participants (i.e. the questionnaire did not refer to specific green or environmentally preferable labels).
The outcomes of interest in the present study were: weekly use of disinfectant to clean surfaces or to clean medical instruments, weekly use of sprays (any spray or sprays for cleaning / disinfection tasks), and weekly use of specific disinfectants or cleaning products.
Workplace characteristics
In the occupational questionnaire, nurses were asked if they currently worked in a hospital, and if yes, to report the hospital's name, city and state. The hospital name and address were then matched to the corresponding hospital in the 2011 American Hospital Association (AHA) database, a national database of all U.S. hospitals, which provided information on various hospital characteristics [American Hospital Association (AHA)]. A vast majority (90%) of the hospitals where the NHSII nurses reported to work could be identified in the AHA database. Non-identified hospitals included facilities that were not actually a hospital, international hospitals, or hospitals opened too recently; otherwise, information provided by the nurses were insufficient to identify the hospital. Several NHSII nurses worked in the same hospitals (1 to 23 nurse(s) per identified hospital; average: 2.6).
AHA 2011 data provided information regarding the hospital size, as measured by the number of beds (<50, 50-199, ≥200). We evaluated the level of urbanization (urban, adjacent to urban, or rural) of the area where the hospital was located using the Urban Influence Code [USDA, 2013], a county-level indicator based on population size (metropolitan counties), or size of the largest city and proximity to metro and micropolitan areas (nonmetropolitan counties).
For nurses who reported not working in a hospital, no information regarding the workplace was collected. Non-hospital workplaces may include other types of healthcare facilities (eg, outpatient clinics, nursing homes), private practice, or work in non-healthcare settings (eg, public schools, research).
The predictors of interest were the type of workplace (hospital vs. non-hospital); and among nurses working in hospitals: the hospital size (number of beds), the U.S. region, and urbanization level of the area where the hospital was located.
Representativeness of NHSII nurses
NHSII participants were initially selected in 14 U.S. states, and as of the mid-1990s they resided in all 50 states and the District of Columbia. Nonetheless, NHSII participants may not be representative of all U.S. nurses. To address this question among nurses working in hospitals (n=4,572), we performed a weighted analysis among nurses working at each of the 1,594 unique hospitals, using a random selection of one nurse per hospital. Weights were computed in order to match the distribution of hospitals in the national AHA database, for geographic location, bed size, and urban influence. Distribution of disinfectant use in the weighted sample was compared to the crude distribution observed in all NHSII nurses working in hospitals. Results are presented in Supplemental Table SI. As no major difference in the distribution was observed, the main analyses were conducted using the unweighted original data.
Survey of hospital infection control departments
In order to obtain additional information regarding the disinfectants and cleaning products used in the hospitals where NHSII nurses worked, we addressed a 2-page survey to infection control departments of the 16 hospitals where ≥10 nurses worked. We received responses from 8 hospitals where a total of 177 NHSII nurses worked. Responses from infection control departments and nurses were compared qualitatively, in particular regarding the ingredients of the products used by nurses for cleaning/disinfection tasks.
Statistical analyses
Associations between type of workplace, hospital size, U.S. region and urbanization level on the one hand, and disinfectant/cleaning product use on the other hand were evaluated using logistic regression models. Results from unadjusted and multivariable adjusted models are presented. We took into account potential dependence between nurses working in the same hospital using generalized estimating equations (GEE). A two-sided P<0.05 was considered statistically significant. Most analyses were run using SAS V.9 (SAS Institute, Cary, North Carolina, USA). We corrected for multiple testing, using the false discovery rate approach (R package “p.adjust”; The R Project for Statistical Computing, www.r-project.org) for the analysis of variation in the use of the 15 specific disinfectants/cleaning products according to hospital characteristics.
Results
Of the 8,965 nurses selected in the stratified sample (Figure 1), we excluded 114 participants with missing values for the question “Are you working in a hospital”. This yielded an analytic population of 8,851 nurses. Participants were on average 59 years of age when they answered the occupational questionnaire, and 52% reported working in a hospital. Nurses commonly reported weekly use of disinfectants to clean surfaces (50%) and, to a lower extent, to clean instruments (19%) and weekly use of sprays (19%) (Table I). Among nurses reporting weekly use of spray, 66% used sprays for surface cleaning or disinfection, 21% for instrument cleaning or disinfection, 28% for patient care, 48% for air-refreshing and 4% for other use. The most common disinfectants used weekly by all nurses were alcohol (38%), hypochlorite bleach (21%), and quats (12%).
Table I. Description of the analytic population (n=8,851).
| Age, m (sd) | 58.7 (4.3) |
| Work in a hospital, n (%) | 4,572 (52) |
| Hospital bed size | |
| <50 beds | 241 (6) |
| 50-199 beds | 1,030 (25) |
| 200+ beds | 2,845 (69) |
| U.S. Region | |
| Northeast | 1,239 (30) |
| West | 695 (17) |
| Midwest | 1,364 (33) |
| South | 818 (20) |
| Urban-Rural Gradient | |
| Urban | 3,627 (88) |
| Adjacent urban | 316 (8) |
| Rural | 173 (4) |
| Weekly use of disinfectants*, n (%) | |
| To clean surfaces | 4,352 (50) |
| To clean instruments | 1,669 (19) |
| Weekly use of sprays*, n (%) | |
| Any spray | 1,668 (19) |
| Spray for cleaning/disinfection | 1,169 (14) |
| Weekly use of specific disinfectants†, n (%) | |
| Alcohol | 3,235 (38) |
| Hypochlorite bleach | 1,751 (21) |
| Quats | 1,036 (12) |
Missing for <1% of participants.
Missing for <5% of participants.
Working in a hospital was significantly associated with a higher use of disinfectants to clean surfaces (odds ratio: 2.06, 95% confidence interval: 1.89-2.24) and to clean instruments (1.70, 1.53-1.90), compared to other workplaces. However, the opposite was observed for spray use that was less often reported by nurses working in hospitals than those working in other facilities (any spray: 0.74, 0.66-0.82; sprays for cleaning/disinfection: 0.72, 0.63-0.81). Regarding specific disinfectants, the most commonly used products (eg, bleach, alcohol, quats) were used more often by nurses working in hospitals (Table II). Only the use of “green” products was reported significantly less often by nurses working in hospitals.
Results for the subgroup of nurses working in a hospital are presented in Tables III and IV. Nurses working in small (<50 beds, 6%) and medium size (50-199 beds, 25%) hospitals were more likely to use disinfectants to clean surfaces than those in large hospitals (≥200 beds, 69%), but no difference was observed regarding the use of disinfectants to clean instruments. In addition, no difference was observed across region and urbanization level for the general use of disinfectants (Table III). More variations were observed regarding the use of sprays according to the hospital characteristics studied, and differences remained significant after mutual adjustment (Table IV). The use of sprays was more common in nurses working in small hospitals. In addition, compared to nurses in the Northeast, nurses in the West had lower spray use, but nurses in the Midwest (any spray) or South (sprays for cleaning/disinfection) had a higher spray use. Finally, the use of sprays was more common in hospitals located in areas with intermediate urbanization level (adjacent to urban).
Table III. Disinfectant use among nurses working in hospitals, according to hospital characteristics (n=4,110).
| Weekly use of disinfectants to clean surfaces | Weekly use of disinfectants to clean instruments | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | % | OR | adjOR | 95% CI | % | OR | adjOR | (95% CI) | |
|
|
|
|
|||||||
| Bed size | |||||||||
| >=200 | 2840 | 56 | 1 | 1 | - | 23 | 1 | 1 | - |
| 50-199 | 1029 | 61 | 1.20 | 1.20 | 1.03-1.40 | 23 | 1.00 | 1.01 | 0.85-1.21 |
| <50 | 241 | 68 | 1.67 | 1.69 | 1.23-2.32 | 25 | 1.16 | 1.21 | 0.84-1.76 |
| U.S. Region | |||||||||
| Northeast | 1237 | 58 | 1 | 1 | - | 25 | 1 | 1 | - |
| West | 695 | 58 | 1.01 | 1.00 | 0.83-1.22 | 22 | 0.86 | 0.85 | 0.68-1.07 |
| Midwest | 1361 | 59 | 1.02 | 1.00 | 0.85-1.18 | 22 | 0.89 | 0.89 | 0.73-1.07 |
| South | 817 | 57 | 0.94 | 0.94 | 0.78-1.12 | 21 | 0.82 | 0.81 | 0.65-1.00 |
| Urban/Rural | |||||||||
| Urban | 3622 | 58 | 1 | 1 | - | 23 | 1 | 1 | - |
| Adjacent to urban | 315 | 66 | 1.45 | 1.18 | 0.90-1.55 | 24 | 1.06 | 0.99 | 0.72-1.38 |
| Rural | 173 | 51 | 0.77 | 0.66 | 0.48-0.90 | 21 | 0.89 | 0.86 | 0.56-1.31 |
Logistic regression with unadjusted odds ratios (OR) and mutually-adjusted odds ratios (adjOR) with GEE to take into account clustering among nurses working in the same hospital. Results in bold are statistically significant.
Table IV. Spray use among nurses working in hospitals-according to hospital characteristics (n=4,110).
| Weekly use of sprays | Weekly use of sprays for cleaning/disinfection | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | % | OR | adjOR | 95% CI | % | OR | adjOR | 95% CI | |
|
|
|
|
|||||||
| Bed size | |||||||||
| >=200 | 2840 | 16 | 1 | 1 | - | 11 | 1 | 1 | - |
| 50-199 | 1029 | 17 | 1.07 | 1.02 | 0.84-1.25 | 13 | 1.25 | 1.16 | 0.92-1.47 |
| <50 | 241 | 27 | 1.98 | 1.69 | 1.20-2.38 | 22 | 2.26 | 1.79 | 1.20-2.65 |
| U.S. Region | |||||||||
| Northeast | 1237 | 16 | 1 | 1 | - | 11 | 1 | 1 | - |
| West | 695 | 12 | 0.75 | 0.75 | 0.58-0.97 | 8 | 0.73 | 0.73 | 0.54-0.99 |
| Midwest | 1361 | 19 | 1.29 | 1.24 | 1.00-1.52 | 14 | 1.32 | 1.26 | 0.99-1.60 |
| South | 817 | 19 | 1.23 | 1.21 | 0.95-1.53 | 14 | 1.36 | 1.36 | 1.03-1.77 |
| Urban/Rural | |||||||||
| Urban | 3622 | 16 | 1 | 1 | - | 11 | 1 | 1 | - |
| Adjacent to urban | 315 | 25 | 1.76 | 1.43 | 1.05-1.95 | 21 | 2.08 | 1.63 | 1.16. 2.29 |
| Rural | 173 | 17 | 1.05 | 0.88 | 0.54-1.41 | 14 | 1.31 | 1.06 | 0.62-1.82 |
Logistic regression with unadjusted odds ratios (OR) and mutually-adjusted odds ratios (adjOR) with GEE to take into account clustering among nurses working in the same hospital. Results in bold are statistically significant.
Regarding specific disinfectants/cleaning products, after correction for multiple comparisons, we observed geographical variations. Compared to the Northeast, the use of quats and phenolics was more common in the Midwest, and the use of “green” products less common in the Midwest. The use of hydrogen peroxide was also more common in hospitals located in areas with intermediate urbanization level. Detailed results for the 15 specific products are shown in Supplemental Table SII.
Information regarding use of disinfectants and cleaning products obtained from the infection control departments survey, and qualitative comparison with NHSII nurses responses are presented in supplemental table SIII. When the two sources of information could be compared for specific tasks (surface/instrument cleaning, working in operating rooms), all products found in SDS from the 8 hospitals were also reported by the nurses working in these hospitals. The proportion of nurses reporting weekly exposure to these products varied according to products and tasks from 7% to 65%.
Discussion
In a large study of U.S. registered nurses, we found marked differences in the tasks performed and types of products used for cleaning and disinfection according to workplace characteristics. Nurses working in hospitals, especially small ones, performed general disinfection tasks more often. Notable variations in use of spray were observed by type of workplace and geographic location.
Our results complement and extend data recently reported regarding disinfectant use and chemical exposures among U.S. healthcare workers [LeBouf et al., 2014; Saito et al., 2015]. Based on shift-monitoring of workers in 14 different occupations in five U.S. hospitals, Saito et al. showed that many workers other than housekeepers performed tasks involving the use of cleaning products and disinfectants [Saito et al., 2015]. Registered nurses performed cleaning and disinfecting tasks in 66% of monitored shifts, and were found to use the widest variety of chemicals among patient-care occupations. Quantitative exposure assessment in the same five hospitals through personal- and area- sampling revealed moderate exposure to total volatile organic compounds (VOC) in registered nurses [LeBouf et al., 2014]. Higher VOC levels were observed in other nursing occupations (nursing assistants, licensed practical nurses) or other specific jobs such as medical equipment preparers. However, the results suggested that exposure levels were influenced by tasks performed and products used by workers possibly more than by their occupation per se. This finding is consistent with the heterogeneity we observed in disinfectant use among nurses in various workplaces all over the U.S. Although our study was restricted to registered nurses and used a questionnaire-based assessment of disinfectant use, it provides a broader picture of nurses' exposures in various healthcare facilities, and emphasizes important variations. It complements the more thorough exposure evaluation performed in smaller studies [Bessonneau et al., 2013; LeBouf et al., 2014; Saito et al., 2015].
Our finding of a higher use of disinfectants among nurses working in hospitals was expected given the higher need for disinfection in hospitals compared to other types of healthcare facilities or workplaces. We also found that disinfectant use was further increased among nurses working in smaller-size hospitals, in which up to 68% of the nurses reported using disinfectants for surfaces cleaning weekly. Nursing jobs involve many tasks besides patient care [Arif et al., 2009], but the amount of cleaning/disinfection activities performed by registered nurses varies across workplaces [Saito et al., 2015]. Because of organizational constraints, registered nurses in smaller hospitals may be responsible for more diverse tasks, including cleaning and disinfection.
Furthermore, the observed variations in spray use across type of workplace, hospital size and location are notable. Associations between the use of cleaning and disinfecting sprays and asthma have been observed in several studies, in the context of domestic cleaning [Zock et al., 2007; Le Moual et al., 2012; Bédard et al., 2014], but also in occupational settings among professional cleaners [Vizcaya et al., 2015] and healthcare workers [Dumas et al., 2012]. This relationship may be due to the high potential for inhalation exposure associated with product spraying [Bello et al., 2009]. In the current study, the use of sprays by nurses was more common in non-hospital workplaces, suggesting that sprays are used for cleaning and lower level disinfection [Quinn et al., 2015]. Alternatively, this result may indicate that some hospitals already have undertaken prevention measures limiting the use of products in spray form.
Among nurses working in hospitals, we observed some regional variations in the specific products used, even after controlling for bed size and urbanization level. Regional variations were observed for the use of quats and phenolics, two types of low-level disinfectants for use on environmental surfaces and non-critical medical devices [Rutala et al., 2008]. Phenols may also be added to glutaraldehyde-based formulations used for high-level disinfection [Rutala et al., 2008]. Cases of occupational asthma caused by quats have been reported [Purohit et al., 2000; Paris et al., 2012], and an association between quats exposures and asthma has been suggested in healthcare workers [Dumas et al., 2012; Gonzalez et al., 2014]. To our knowledge, a potential role of phenolic-based disinfectants in asthma has not been specifically investigated. Of particular interest was also the observed regional variation in the use of “green” products. There is no single standard definition for “green” cleaning products in the U.S. The absence of asthmagens or allergens is among the required criteria for only some of the green or environmentally preferable labels [Garza et al., 2015; Quinn et al., 2015]. Regional differences in the use of green products may thus be driven by differential environmental considerations or health concerns other than asthma. Overall, many factors could explain regional variations in use of disinfectants and cleaning products, among which specific state plans or regulations and potentially cultural differences. We also observed some variations in the use of cleaning products and disinfectants in hospitals according to urbanization level. Urban and rural hospitals may differ in many ways (e.g., financial and staff resources, facilities and services, clinical practices) [MacDowell et al., 2010; Muelleman et al., 2010; Sullivan et al., 2013; Kozhimannil et al., 2014] which could influence cleaning/disinfection practices. However, information regarding the specific hospital characteristics available in our study was too limited to further investigate this question.
In the present study, use of cleaning products and disinfectants was assessed through self-administered questionnaires. Despite the wide use of this method to evaluate exposure to cleaning products and disinfectants in large epidemiological studies [Mirabelli et al., 2007; Vizcaya et al., 2011; Arif & Delclos, 2012], relying on self-reported exposures only is not ideal. First, participants were asked to report their own use of disinfectants and cleaning products and this evaluation of exposure does not take into account use of products by other workers. Second, healthcare workers may under-estimate their own exposure, as suggested in a study of French hospital workers comparing self-reported exposure to an expert-assessment [Donnay et al., 2011]. This underestimation was observed when evaluating the use of specific chemicals (eg, quats, ammonia), probably because of a lack of knowledge regarding the active ingredients of the products used. To address this issue, our questionnaire allowed nurses to report the brand name of the product(s) they use and exposure estimates were re-evaluated based on the active ingredients found on the corresponding safety data sheets. We also contacted a few infection control departments from large hospitals to obtain additional information regarding the products used, and found similarities with the nurses' reports, although the comparability of the two sources of information was limited. Moreover, unlike specific chemicals, a good agreement between self-report and expert assessment was observed for spray use among French hospital workers [Donnay et al., 2011]. One may similarly expect that general disinfection tasks (the main outcome in our study) are reported with better accuracy than the use of specific chemicals. Finally, the current study did not focus on health outcomes, and misclassification of exposure is unlikely to be differential according to the studied variables (workplace characteristics, U.S. region).
Current knowledge regarding prevention of both healthcare-related infections in patients and work-related asthma in healthcare workers is advancing steadily but remains insufficient to establish effective prevention measures [Heederik, 2014; Quinn et al., 2015]. As reflected by the observed variations in the type of disinfectants used by nurses in U.S. hospitals, healthcare facilities select products from a relatively wide range of options effective for infection prevention [Han et al., 2015; Quinn et al., 2015] in accordance with existing infection control guidelines [EPA; Rutala et al., 2008], although choice may be more limited regarding disinfection of critical equipment. For work-related asthma prevention, elimination of hazardous substances and replacement with safer alternatives has been recommended over other types of measures, such as the use of personal protective equipment [Quinn et al., 2015]. Reducing the use of sprays may be relevant as part of a strategy for asthma prevention. Experts have also encouraged the investigation of green cleaning [Garza et al., 2015], and of emerging non-chemical technologies for disinfection (e.g., steam, ultraviolet light) as a potential alternative to chemical disinfection [Quinn et al., 2015].
In summary, in this large nationwide study of U.S. registered nurses, we observed important variations in the disinfection tasks as well as in the composition and presentation of disinfectants and cleaning products used in various workplaces. This heterogeneity supports a possibility for the development of infection control strategies in healthcare facilities that would integrate occupational health considerations in addition to ensuring patients' safety.
Supplementary Material
Acknowledgments
The Nurses' Health Study II is coordinated at the Channing Division of Network Medicine, Brigham and Women's Hospital, Boston, Massachusetts. We would like to thank the participants and staff of the Nurses' Health Study II for their valuable contributions. In particular, we would like to thank Charlotte Marsh, Lisa Abramovitz, Christina Staffiere, and Chidiogo Onwuakor for their help with data cleaning and management. We would like to thank Dr Abbas Virji for his help with designing the hospital survey questionnaire.
Funding: Grant sponsor: Centers for Disease Control and Prevention; Grant number R01 OH-10359.
Grant sponsor: National Institutes of Health; Grant number: UM1 CA176726.
Footnotes
- Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, USA
- INSERM, VIMA: Aging and chronic diseases. Epidemiological and public health approaches, U1168, F-94807, Villejuif, France
Authors' contributions: OD contributed to the study conception, the acquisition, analysis and interpretation of the data, and primary manuscript preparation. ASW and KMB were involved in the acquisition, analysis, interpretation of the data and critical revision of the manuscript. RV, JPZ and PKH were involved in the data interpretation and critical revision of the manuscript. FES contributed to the acquisition and interpretation of the data and critical revision of the manuscript. NLM contributed to the study conception, data interpretation and critical revision of the manuscript. CAC participated in the study conception, acquisition of the data, data interpretation and critical revision of the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Institution and Ethics approval and informed consent: The Nurses' Health Study II is coordinated at the Channing Division of Network Medicine, Brigham and Women's Hospital, Boston, Massachusetts. This investigation was approved by the Institutional Review Board at the Brigham and Women's Hospital, Boston, Massachusetts, USA. All participants gave written consent.
Disclosure statement: All the authors declare they have no conflict of interest.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- American Hospital Association (AHA) [Last accessed: March 29th, 2016];AHA Annual Survey Database. http://www.ahadataviewer.com/about/hospital-database/
- Arif AA, Delclos GL, Serra C. Occupational exposures and asthma among nursing professionals. Occup Environ Med. 2009;66:274–278. doi: 10.1136/oem.2008.042382. [DOI] [PubMed] [Google Scholar]
- Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Environ Med. 2012;69:35–40. doi: 10.1136/oem.2011.064865. [DOI] [PubMed] [Google Scholar]
- Bédard A, Varraso R, Sanchez M, et al. Cleaning sprays, household help and asthma among elderly women. Respiratory Medicine. 2014;108:171–180. doi: 10.1016/j.rmed.2013.10.018. [DOI] [PubMed] [Google Scholar]
- Bello A, Quinn MM, Perry MJ, Milton DK. Characterization of occupational exposures to cleaning products used for common cleaning tasks--a pilot study of hospital cleaners. Environ Health. 2009;8:11. doi: 10.1186/1476-069X-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessonneau V, Mosqueron L, Berrubé A, et al. VOC Contamination in Hospital, from Stationary Sampling of a Large Panel of Compounds, in View of Healthcare Workers and Patients Exposure Assessment. PLoS ONE. 2013;8:e55535. doi: 10.1371/journal.pone.0055535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLS. [Last accessed: March 29th, 2016];US Bureau of Labor Statistics. 2015 http://www.bls.gov/news.release/ocwage.nr0.htm.
- Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–2588. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- Delclos GL, Gimeno D, Arif AA, et al. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007;175:667–675. doi: 10.1164/rccm.200609-1331OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnay C, Denis MA, Magis R, et al. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Environ Med. 2011;68:611–617. doi: 10.1136/oem.2010.061671. [DOI] [PubMed] [Google Scholar]
- Dumas O, Donnay C, Heederik D, et al. Occupational exposure to cleaning products and asthma in hospital workers. Occup Environ Med. 2012;69:883–889. doi: 10.1136/oemed-2012-100826. [DOI] [PubMed] [Google Scholar]
- Dumas O, Siroux V, Luu F, et al. Cleaning and asthma characteristics in women. Am J Ind Med. 2014;57:303–11. doi: 10.1002/ajim.22244. [DOI] [PubMed] [Google Scholar]
- Dumas O, Varraso R, Zock JP, et al. Asthma history, job type and job changes among US nurses. Occup Environ Med. 2015;72:482–8. doi: 10.1136/oemed-2014-102547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA. U.S. EPA (U.S. Environmental Protection Agency) [Last accessed: March 29th, 2016];Selected EPA-registered Disinfectants. http://www.epa.gov/pesticide-registration/selected-epa-registered-disinfectants.
- Garza JL, Cavallari JM, Wakai S, et al. Traditional and environmentally preferable cleaning product exposure and health symptoms in custodians. Am J Ind Med. 2015;58:988–995. doi: 10.1002/ajim.22484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez M, Jégu J, Kopferschmitt MC, et al. Asthma among workers in healthcare settings: role of disinfection with quaternary ammonium compounds. Clin Exp Allergy. 2014;44:393–406. doi: 10.1111/cea.12215. [DOI] [PubMed] [Google Scholar]
- Han JH, Sullivan N, Leas BF, et al. Cleaning hospital room surfaces to prevent health care-associated infections: A technical brief. Annals of Internal Medicine. 2015;163:598–607. doi: 10.7326/M15-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heederik D. Cleaning agents and disinfectants: moving from recognition to action and prevention. Clin Exp Allergy. 2014;44:472–4. doi: 10.1111/cea.12286. [DOI] [PubMed] [Google Scholar]
- Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II) Lancet. 2007;370:336–341. doi: 10.1016/S0140-6736(07)61164-7. [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, Hung P, Prasad S, Casey M, Moscovice I. Rural-urban differences in obstetric care, 2002-2010, and implications for the future. Med Care. 2014;52:4–9. doi: 10.1097/MLR.0000000000000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBouf RF, Virji MA, Saito R, et al. Exposure to volatile organic compounds in healthcare settings. Occup Environ Med. 2014;71:642–50. doi: 10.1136/oemed-2014-102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural Remote Health. 2010;10:1531. [PMC free article] [PubMed] [Google Scholar]
- De Matteis S, Cullinan P. Occupational asthma in cleaners: a challenging black box. Occup Environ Med. 2015;72:755–756. doi: 10.1136/oemed-2015-102985. [DOI] [PubMed] [Google Scholar]
- Mirabelli MC, Zock JP, Plana E, et al. Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup Environ Med. 2007;64:474–479. doi: 10.1136/oem.2006.031203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Moual N, Varraso R, Siroux V, et al. Domestic use of cleaning sprays and asthma activity in females. Eur Respir J. 2012;40:1381–1389. doi: 10.1183/09031936.00197611. [DOI] [PubMed] [Google Scholar]
- Le Moual N, Varraso R, Zock JP, et al. Are operating room nurses at higher risk of severe persistent asthma? The Nurses' Health Study. J Occup Environ Med. 2013;55:973–7. doi: 10.1097/JOM.0b013e318297325b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muelleman RL, Sullivan AF, Espinola JA, et al. Distribution of emergency departments according to annual visit volume and urban-rural status: Implications for access and staffing. Acad Emerg Med. 2010;17:1390–1397. doi: 10.1111/j.1553-2712.2010.00924.x. [DOI] [PubMed] [Google Scholar]
- NSSRN. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. U.S Department of Health and Human Services, Health Resources and Services Administration; 2010. [Google Scholar]
- Paris C, Ngatchou-Wandji J, Luc A, et al. Work-related asthma in France: recent trends for the period 2001-2009. Occup Environ Med. 2012;69:391–397. doi: 10.1136/oemed-2011-100487. [DOI] [PubMed] [Google Scholar]
- Purohit A, Kopferschmitt-Kubler MC, Moreau C, et al. Quaternary ammonium compounds and occupational asthma. Int Arch Occup Environ Health. 2000;73:423–427. doi: 10.1007/s004200000162. [DOI] [PubMed] [Google Scholar]
- Quinn MM, Henneberger PK, Braun B, et al. Cleaning and disinfecting environmental surfaces in health care: Toward an integrated framework for infection and occupational illness prevention. American Journal of Infection Control. 2015;43:424–434. doi: 10.1016/j.ajic.2015.01.029. [DOI] [PubMed] [Google Scholar]
- Rutala WA, Gergen MF, Weber DJ. Efficacy of different cleaning and disinfection methods against Clostridium difficile spores: importance of physical removal versus sporicidal inactivation. Infection control and hospital epidemiology. 2012;33:1255–8. doi: 10.1086/668434. [DOI] [PubMed] [Google Scholar]
- Rutala WA, Weber DJ HICPAC. Guideline for Disinfection and Sterilization in Healthcare Facilities. CDC Center for Disease Control; 2008. [Google Scholar]
- Saito R, Virji MA, Henneberger PK, et al. Characterization of Cleaning and Disinfecting Tasks and Product Use Among Hospital Occupations. Am J Ind Med. 2015;58:101–111. doi: 10.1002/ajim.22393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siracusa A, De Blay F, Folletti I, et al. Asthma and exposure to cleaning products - a European Academy of Allergy and Clinical Immunology task force consensus statement. Allergy. 2013;68:1532–1545. doi: 10.1111/all.12279. [DOI] [PubMed] [Google Scholar]
- Sullivan AF, Rudders SA, Gonsalves AL, et al. National survey of pediatric services available in US emergency departments. Int J Emerg Med. 2013;6:13. doi: 10.1186/1865-1380-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDA. Urban Influence Codes. United States Department of Agriculture; 2013. [Last accessed: March 29th, 2016]. http://www.ers.usda.gov/data-products/urban-influence-codes.aspx. [Google Scholar]
- Vizcaya D, Mirabelli MC, Antó JM, et al. A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup Environ Med. 2011;68:914–919. doi: 10.1136/oem.2010.063271. [DOI] [PubMed] [Google Scholar]
- Vizcaya D, Mirabelli MC, Gimeno D, et al. Cleaning products and short-term respiratory effects among female cleaners with asthma. Occup Environ Med. 2015;72:757–63. doi: 10.1136/oemed-2013-102046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zock JP, Plana E, Jarvis D, et al. The use of household cleaning sprays and adult asthma: an international longitudinal study. Am J Respir Crit Care Med. 2007;176:735–741. doi: 10.1164/rccm.200612-1793OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.