Abstract
Background
Insomnia is a robust correlate of suicidal ideation and behavior. Preliminary research has identified thwarted belongingness (c.f. social disconnection) as an explanatory link between insomnia and suicidal ideation.
Objectives
This study replicates and extends previous findings in four demographically diverse samples using both cross-sectional and longitudinal designs. Additionally, the specificity of thwarted belongingness was evaluated by testing anxiety as a rival mediator.
Method
Self-report measures of insomnia severity, thwarted belongingness, suicidal ideation and behavior, and anxiety were administered in four adult samples: 469 undergraduate students, 352 psychiatric outpatients, 858 firefighters, and 217 primary care patients.
Results
More severe insomnia was associated with more severe thwarted belongingness and suicidality. Thwarted belongingness significantly accounted for the association between insomnia and suicidality, cross-sectionally and longitudinally, beyond anxiety. Notably, findings supported the specificity of thwarted belongingness: anxiety did not significantly mediate the association between insomnia and suicidality, and insomnia did not mediate the relation between thwarted belongingness and suicidality.
Limitations
This study relied solely on self-report measures. Future studies incorporating objective sleep measurements are needed.
Conclusion
Findings underscore the utility of assessing and addressing sleep disturbances and social disconnection to reduce suicide risk.
Keywords: insomnia, sleep disturbance, thwarted belongingness, suicidal ideation, suicidal behavior, anxiety
To prevent the deaths by suicide of over 800,000 people globally (WHO, 2014), efforts have been made to understand suicide risk factors and the processes that contribute to risk. This approach is strategic as it informs the identification of at-risk individuals while also illuminating therapeutic targets for attenuating suicide risk.
A growing body of research indicates that insomnia is a potent contributor to suicidal thoughts and behaviors (Bernert & Joiner, 2007; Bernert et al., 2015). Strikingly, in a meta-analysis of 39 studies revealing a significant relationship between insomnia and suicidality, depression—of which insomnia and suicidal thoughts are key symptoms (APA, 2013)—did not moderate this association (Pigeon et al., 2012). This suggests that insomnia is a particularly robust suicide risk factor and that additional work is needed to understand the underlying mechanisms. Further, longitudinal studies with follow-up periods ranging from 1 week to 14 years have demonstrated a prospective association between insomnia and subsequent suicide ideation (McCall et al., 2010; Wong et al., 2011), suicide attempts (Wong & Brower, 2012), and suicide deaths (Bernert et al., 2014; Wong et al., 2011), beyond depression and hopelessness (Ribeiro et al., 2012).
Despite converging evidence that insomnia predict suicidality, there remains a relative lack of research investigating the factors underlying this relationship. Researchers have conjectured that emotion dysregulation (Bernert & Joiner, 2007; Bernert et al., 2014) or overarousal (Ribeiro et al., 2012) may explain this association; however, empirical evidence for these assertions is lacking. To better understand these variables, it may be useful to draw from theoretical suicide models.
One such model is the interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010). According to this theory, three key constructs interact to produce suicide risk: thwarted belongingness (i.e., social disconnection), perceived burdensomeness (i.e., feeling that others would be better off without them), and acquired capability (i.e., elevated physical pain tolerance and fearlessness about death). The theory posits that active suicidal desire emerges when individuals experience elevated levels of thwarted belongingness and perceived burdensomeness. Lethal or near-lethal suicidal behaviors are hypothesized to occur when individuals additionally possess elevated acquired capability.
From the perspective of the interpersonal theory of suicide, insomnia may confer suicide risk by increasing or exacerbating feelings of loneliness and thwarted belongingness. For example, the experience of being awake while most others are asleep is likely to be intrinsically isolating and lonely, and hallmark insomnia symptoms include difficulty falling or staying asleep, or waking up too early (APA, 2013). Furthermore, insomnia in particular has been consistently shown to impact daytime functioning (Sateia, Doghramji, Hauri, & Morin, 2000, for review), which may decrease motivation to engage with others or ability to do so effectively (Carskadon, 1990; Roberts et al., 2001). This may, in turn, increase feelings of social isolation and disconnection. Indeed, in an investigation across six unique samples, insomnia symptoms were both cross-sectionally and prospectively associated with greater perceptions of loneliness, despite controlling for related psychiatric symptoms, including anxiety (Hom et al., under review).
Several empirical studies offer further support for thwarted belongingness as an explanatory link in the relationship between insomnia and suicidality. For instance, in a study by Chu and colleagues (2016b) of 552 South Korean undergraduates, thwarted belongingness significantly mediated the cross-sectional relationship between insomnia and suicidal ideation. Importantly, these researchers also found that insomnia symptoms did not account for the relationship between thwarted belongingness and suicidal ideation, highlighting the specificity of the mediator and providing evidence for the proposed direction of the pathway between insomnia and suicidal ideation. Though not directly evaluating the mediating role of thwarted belongingness, Golding and colleagues (2015) found that among older adults, insomnia and suicide risk were not significantly related when controlling for all three interpersonal theory constructs, suggesting that they may help to explain the association. However, a two-sample investigation of undergraduates by Nadorff and colleagues (2014) produced mixed results. While the results of the first study were the same as those reported by Golding and colleagues (2015), in the second study, this association remained significant after controlling for these variables.
These equivocal results are based primarily on cross-sectional studies using undergraduate samples; thus, the generalizability and utility is limited. As a result, research is needed to replicate these findings in additional samples and studies employing prospective approaches. Delineation of this relationship has the potential to inform the development of targeted prevention and intervention strategies and enhance our understanding of the well-established relationships between sleep, social disconnection, and suicide risk.
This study examines thwarted belongingness as an explanatory link in the relationship between insomnia and suicidality across four distinct adult samples. Consistent with previous research, we hypothesized that: (1) insomnia would be significantly associated with thwarted belongingness and suicidal ideation both cross-sectionally (Studies 1,2,3) and prospectively (Study 4); and, (2) thwarted belongingness would be a significant mediator of the relations between insomnia and suicidality. Consistent with previous studies (Hom et al., under review; Kurina et al., 2011), we covaried anxiety, as anxiety and overarousal symptoms are frequently related to feelings of thwarted belongingness and may also confer risk for insomnia and suicidality (Chu et al., 2015a).
To strengthen findings, in all four samples, we evaluated the specificity of thwarted belongingness as a mediator in two ways. First, we examined whether insomnia severity (independent variable) and thwarted belongingness (mediator) were interchangeable in their roles. Specifically, we tested whether insomnia mediates the relationship between thwarted belongingness and suicidality. We predicted that insomnia and thwarted belongingness are not interchangeable as independent variable and mediator, respectively. Next, we tested our hypotheses against an alternative explanatory mechanism: anxiety, which has been linked to both sleep problems and suicidal symptoms (c.f.overarousal; Ribeiro et al., 2011). Specifically, we investigated whether anxiety is a rival mediator. We postulated that anxiety will not account for the relationship between these variables, which supports the robustness of thwarted belongingness as the mediator.
Study 1
First, we examined our hypotheses among U.S. undergraduate students in an effort to replicate previous findings among South Korean undergraduates (Chu et al., 2016b). Consistent with our study hypotheses, we predicted that thwarted belongingness would significantly account for the association between sleep problems and suicidality.
Method
Participants
Participants were 469 U.S. undergraduates (Table 1 for details).
Table 1.
Demographics for Studies 1, 2, 3, and 4.
| Variables | Study 1 (N=469) Undergraduates | Study 2 (N=352) Outpatients | Study 3 (N=858) Firefighters | Study 4 (N=217) Primary Care Patients |
|---|---|---|---|---|
| Age mean (SD) | 19.4 (2.0) years | 27.0 (10.4) years | 37.3 (10.8) years | 44.1 (12.4) years |
| Age Range | 18-42 years | 18-71 years | 18-76 years | 19-79 years |
| Female | 337, 71.9% | 216, 61.4% | 80, 9.3% | 136, 62.7% |
| Race/Ethnicity | ||||
| Hispanic/Latino | 70, 14.9% | n/a | 22, 2.6% | 6, 2.8% |
| Caucasian/White | 236, 70.1% | 264, 75.0% | 745, 86.8% | 189, 87.0% |
| African American/Black | 33, 7.0% | 31, 8.8% | 3, 0.3% | 15, 6.9% |
| Asian/Pacific Islander | 20, 4.3% | 7, 2.0% | 4, 0.5% | 1, 0.5% |
| American Indian/Alaskan Native | 1, 0.2% | 1, 0.3% | 73, 8.5% | 2, 0.9% |
| Biracial | 15, 3.2% | n/a | n/a | n/a |
| Other | 1, 0.2% | 6, 1.7% | 10, 1.2% | 3, 1.4% |
| Missing | n/a | 5, 1.4% | n/a | 2, 0.9% |
| Marital Status | ||||
| Single/Never Married | 454, 96.8% | 288, 81.8% | 166, 19.3% | 68, 31.5% |
| Married | 5, 1.1% | 32, 9.1% | 623, 72.6% | 48, 22.2% |
| Cohabitating/Not Married | 8, 1.7% | 26, 7.4% | n/a | n/a |
| Separated/Divorced | n/a | 5, 1.4% | 63, 7.4% | 87, 40.1% |
| Widowed | n/a | 1, 0.3% | 6, 0.7% | 13, 6.0% |
| Missing | 2, 0.4% | n/a | n/a | n/a |
| Suicide Attempt History | ||||
| None | 454, 96.8% | 267, 75.9% | 720, 83.9% | 176, 81.1% |
| At least 1 previous attempt | 15, 3.2% | 85, 24.1% | 138, 16.1% | 41, 18.9% |
| 1 previous attempt | 11, 2.3% | 58, 16.5% | n/a | n/a |
| 2+ previous attempts | 4, 0.9% | 27, 7.7% | n/a | n/a |
| Mental Health Treatment | ||||
| Outpatient | 115, 24.5% | 112, 31.8% | 366, 42.7% | 68, 56.2% |
| Inpatient | 7, 1.5% | 63, 17.9% | n/a | n/a |
Note. n/a = data were not available.
Procedure
Data for this study were obtained from a larger web-based investigation of the role of non-disclosure in suicidal symptom reporting. All participants provided informed consent prior to completing the self-report measures and were compensated with course credit. This study was approved by the university's Institutional Review Board (IRB).
Measures
Insomnia
The Insomnia Severity Index (ISI; Bastien et al., 2001) is a 7-item self-report measure that assesses the severity of insomnia symptoms, distress caused by the sleep disturbance, and its effect on functioning. Items are rated on a 5-point Likert scale. Bastien and colleagues (2001) demonstrated that the ISI has high internal consistency and concurrent validity. The ISI exhibited good internal consistency (α =0.84).
Thwarted belongingness
The Interpersonal Needs Questionnaire, Thwarted Belongingness Subscale (INQ-TB; Van Orden et al., 2012) is a 9-item measure of thwarted belongingness and a subscale of the 15-item INQ measure. Each item is rated on a 7-point Likert scale ranging from 1 to 7. The INQ-TB has sound psychometric properties and construct validity across samples, including outpatients, community members, and students (Van Orden et al., 2012). The INQ-TB exhibited excellent internal consistency (α =0.90).
Suicidal ideation
The Beck Scale for Suicide Ideation (BSS; Beck et al., 1979) is a 21-item measure of severity of suicidal ideation. Items are rated on a 3-point Likert scale ranging from 0 to 2. The first 19 items are used to compute the total score as items 20 and 21 assess prior suicidal behaviors. Internal consistency of the BSS was adequate (α =0.76).
Anxiety
The Depression and Anxiety Stress Scales (DASS; Lovibond & Lovibond, 1995) is a 21-item measure of depression, anxiety and stress over the past week. Each item is rated on a 4-point Likert scale ranging from 0 to 3. The 14-item DASS anxiety subscale was used. This subscale had poor internal consistency (α =0.51), a limitation which we discuss below and redress in subsequent studies.
Statistical Analyses
The bootstrap technique was used to test for the mediating effects of thwarted belongingness (INQ-TB) on the relationship between insomnia severity (ISI) and suicidal ideation (BSS), controlling for anxiety symptoms (DASS). In order to establish the specificity of the roles of the independent variable and the mediator, mediation analyses were conducted with the independent variable and the mediator reversed. Specifically, we tested the indirect effect of thwarted belongingness (independent variable) on suicidal ideation through insomnia severity (mediator). Next, we tested whether anxiety was a significant mediator of the relationship of between insomnia and suicidality, controlling for thwarted belongingness.
Mediation analyses were conducted using the PROCESS macro for SPSS Statistics 23, following procedures recommended by Hayes (2013). The indirect effect of insomnia on suicidal ideation through thwarted belongingness was evaluated using a bootstrapping resampling procedure: 10,000 bootstrapped samples were drawn, and bias-corrected 95% confidence intervals were used to estimate the indirect effects of each of the resampled datasets. Two measures of effect sizes are reported: R2 and kappa squared (κ2). Missing data, which were minimal (2.1%), were addressed using listwise deletion. With regard to power, previous research has indicated that a sample size of 53 is required for adequate power (0.80) to detect moderate effect sizes for the α path and large effect sizes for the β path using a bias-corrected bootstrap mediation approach (Fritz & MacKinnon, 2007). Thus, with our sample size of 469, we were adequately powered for analyses.
Results
Study 1 descriptive information is available in Table 2. For analyses examining the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness, the overall regression model explained a significant portion of the variance in suicidal ideation (R2=0.11, F[2,454]=27.19, p<0.001). Insomnia significantly predicted thwarted belongingness (b=0.66, SE= 0.09, p<0.001), and thwarted belongingness significantly predicted suicidal ideation (b=0.13, SE=0.02, p<0.001). The direct effect of insomnia on suicidal ideation was not significant after accounting for thwarted belongingness (b=0.04, SE=0.04, p=0.375), indicating mediation. The indirect effect of insomnia on suicidal ideation through thwarted belongingness was estimated to be between 0.0443 and 0.1489 (95%CI; effect=0.09, SE=0.03), indicating significance (R2=0.02, κ2=0.10; Figure 1). Further, insomnia was not a significant mediator of the relationship between thwarted belongingness and suicidal ideation (effect=0.01, SE=0.01, 95%CI:-0.0113, 0.0275), which supports the specificity of the roles of the independent variable (insomnia severity) and mediator (thwarted belongingness).
Table 2.
Means, Standard Deviations, and Correlations Between Studies 1,2,3 and 4 Variables.
| Study 1 N = 459-469 | 1 | 2 | 3 | 4 | Range | Mean | SD | Skew | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. ISI-Insomnia Severity | -- | 0-27 | 7.87 | 5.18 | 0.64 | |||||
| 2. INQ-Thwarted Belongingness | 0.337** | -- | 9-53 | 19.67 | 10.01 | 1.01 | ||||
| 3. BSS-Suicidal Ideation | 0.143* | 0.324** | -- | 5-39 | 5.87 | 4.20 | 1.17 | |||
| 4. DASS-Anxiety Symptoms | 0.457** | 0.379** | 0.241** | -- | 0-21 | 2.71 | 3.40 | 0.87 | ||
| Study 2 N = 352 | 1 | 2 | 3 | 4 | Range | Mean | SD | Skew | ||
| 1. ISI-Insomnia Severity | -- | 0-28 | 10.90 | 6.65 | 0.24 | |||||
| 2. INQ-Thwarted Belongingness | 0.271** | -- | 9-63 | 32.16 | 13.06 | -0.08 | ||||
| 3. BSS-Suicidal Ideation | 0.198** | 0.403** | -- | 0-31 | 2.66 | 5.35 | 1.56 | |||
| 4. BAI-Anxiety Symptoms | 0.439** | 0.305** | 0.265** | -- | 0-59 | 15.19 | 11.85 | 0.89 | ||
| Study 3 N = 837-858 | 1 | 2 | 3 | 4 | Range | Mean | SD | Skew | ||
| 1. ISI-Insomnia Severity | -- | 0-28 | 10.28 | 6.37 | -0.20 | |||||
| 2. INQ-Thwarted Belongingness | 0.524** | -- | 9-62 | 24.11 | 12.61 | 0.08 | ||||
| 3. DSI-Suicidal Ideation | 0.425** | 0.500** | -- | 0-12 | 2.24 | 2.41 | 1.02 | |||
| 4. History of Anxiety DX | 0.134** | 0.221** | 0.339** | -- | 0-1 | 0.06 | 0.23 | -0.20 | ||
| Study 4 N = 211-217 (T1), N = 96-99 (T2) | 1 | 2 | 3 | 4 | 5 | 6 | Range | Mean | SD | Skew |
| 1. PHQ-Sleep Disturbance (T1) | -- | 0-3 | 1.70 | 1.15 | -0.20 | |||||
| 2. INQ-Thwarted Belongingness (T1) | 0.466** | -- | 9-63 | 31.39 | 14.13 | 0.08 | ||||
| 3. SBQ-Suicide Ideation/Behavior (T1) | 0.352** | 0.533** | -- | 3-18 | 6.30 | 3.72 | 1.02 | |||
| 4. MOS-Sleep Disturbances (T2) | 0.515** | 0.329* | 0.291* | -- | 0-100 | 53.54 | 30.35 | -0.20 | ||
| 5. INQ-Thwarted Belongingness (T2) | 0.384** | 0.525** | 0.472** | 0.369** | -- | 9-57 | 27.24 | 13.39 | 0.42 | |
| 6. SBQ-Suicide Ideation/Behavior (T2) | 0.101 | <0.001 | 0.194 | 0.198* | 0.257* | -- | 3-18 | 6.01 | 3.58 | 1.26 |
| 7. History of Anxiety DX (T1) | 0.244** | 0.254** | 0.257** | 0.186 | 0.352** | 0.402** | 0-1 | 0.32 | 0.47 | 0.79 |
Note.
p < .01;
p < .001.
T1 = Time 1; T2 = Time 2. ISI = Insomnia Severity Index. PHQ = Patient Health Questionnaire-9 (item 3). MOS = Medication Outcomes Study Sleep Scale. INQ = Interpersonal Needs Questionnaire-15. BSS = Beck Scale for Suicide Ideation. DSI = Depressive Symptom Index-Suicidality Subscale. SBQ = Suicide Behavior Questionnaire – Revised. DASS = Depression and Anxiety Stress Scales-21. BAI = Beck Anxiety Inventory. History of Anxiety DX = self-reported history of anxiety disorder diagnoses (coded 0 = no, 1 = yes).
Figure 1.
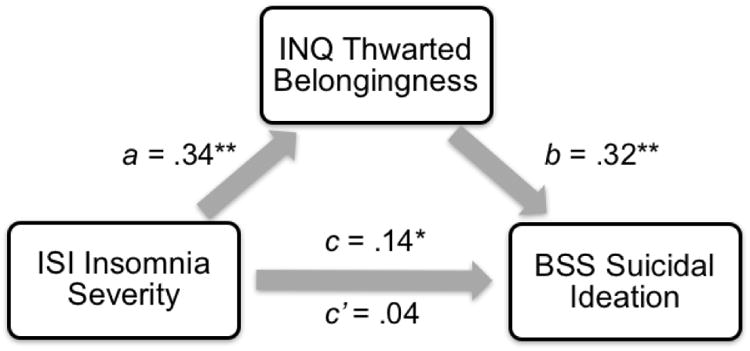
Standardized regression coefficients for the relationship between insomnia severity and suicidal ideation as mediated by thwarted belongingness in Study 1. Note. ** p < 0.001; * p < 0.01. ISI = Insomnia Severity Index. INQ = Interpersonal Needs Questionnaire-15. BSS = Beck Scale for Suicide Ideation.
The pattern of findings remained unchanged after controlling for anxiety symptoms. In particular, the direct effect of insomnia on suicidal ideation was not significant after accounting for thwarted belongingness and anxiety (b=0.35, SE=0.04, p=0.39). The indirect effect of insomnia on suicidal ideation through thwarted belongingness, controlling for anxiety symptoms, was estimated to be between 0.0209 and 0.0880 (95%CI; effect=0.05, SE=0.02), indicating significance. Contrary to expectations, anxiety significantly mediated the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness (effect=0.05, SE=0.03; 95%CI=0.0054, 0.1105; but see below).
Discussion
Study 1 results were consistent with our hypotheses and previous research indicating that severe insomnia is related to greater feelings of thwarted belongingness (Kurina et al., 2011) and suicidal ideation (Bernert et al., 2015), and that thwarted belongingness accounted for the relationship between insomnia and ideation (Chu et al., 2016b). Further, our findings indicated that the mediator and the independent variable were not interchangeable, which supports the specificity of our results. Notably, this finding remained significant even after accounting for anxiety. Prior research has shown that anxiety disorders are characterized by overarousal and withdrawal from social relationships (e.g., agoraphobia, social anxiety disorder) or from certain settings or situations (e.g., generalized anxiety disorder; APA, 2013) – both of which may contribute to sleep problems, loneliness, and suicidality. Therefore, that our findings remained significant even after controlling for anxiety highlights the robustness of thwarted belongingness. Contrary to our expectations, analyses with anxiety as the mediator indicated that anxiety also mediated the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness. This finding is not consistent with our hypotheses regarding the specificity of the mediator. However, given the low internal consistency of our measure of anxiety and these equivocal results, additional work is needed to verify these findings (which we provide in subsequent studies).
That our findings in a sample of U.S. undergraduates are consistent with previous research in a South Korean undergraduates (Chu et al., 2016b) is notable as it highlights the generalizability of this finding. Previously, Chu and colleagues (2016b) suggested that thwarted belongingness may be a particularly robust mediator of the relationship between insomnia and suicidal ideation among South Korean students given that collectivistic cultures place particular emphasis on social relationships and community. Thus, they postulated that young adults from collectivistic cultures who feel disconnected may be particularly vulnerable to suicide symptoms. However, our findings indicate that this pattern is not culturally bound, underscoring the importance of continued research in this area across diverse populations.
Although largely consistent with our hypotheses, findings are limited by the study's cross-sectional design, which precludes our ability to address the sequence of the relationship and thus to speak to causality. Furthermore, this study was limited by the low base rates of suicidality, which diminishes our ability to extend findings to populations with more severe suicidality.
Study 2
Given that Study 1 replicated previous findings (Chu et al., 2016b), we aimed to extend findings to an adult psychiatric outpatient sample with a greater prevalence and severity of suicidality. Similar to Study 2, we expected that thwarted belongingness would serve as the explanatory link.
Method
Participants
Participants were 352 adult mental health outpatients who sought and engaged in treatment from April 2010-December 2015. See Table 1 for details.
Procedure
Data from this study were collected from an outpatient, psychology training clinic affiliated with a large Southeastern U.S. university. After providing informed consent, participants completed an intake battery of questionnaires. This study was approved by the university's IRB.
Measures
Insomnia
Internal consistency of the ISI (Bastien et al., 2001) was good (α =0.88).
Thwarted Belongingness
Internal consistency of the INQ-TB (Van Orden et al., 2012) was excellent (α=0.90).
Suicidal ideation
Internal consistency of the BSS (Beck et al., 1979) total score (items 1-19) was excellent (α=0.94).
Anxiety
The Beck Anxiety Inventory (BAI; Beck & Steer, 1990) is a 21-item measure of anxiety symptoms experienced over the past month. Items are scored on a 4-point Likert scale ranging from 0 to 3 with total scores ranging from 0 to 63. Total scores of 22 and up indicate moderately severe anxiety symptoms. The BAI exhibited strong internal consistency (α =0.92).
Statistical Analyses
The statistical approach in Study 2 was the same as in Study 1.1 Missing data in the present study were also minimal (<1%) and power was adequate.
Results
See Table 2 for details on Study 2 variables. For analyses examining the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness, the overall regression model explained a significant amount of variance in suicidal ideation (R2=0.18, F[2,340]=36.63, p <0.001). Insomnia was significantly associated with thwarted belongingness (b=0.56, SE=0.10, p <0.001), and thwarted belongingness was significantly related to suicidal ideation (b=0.16, SE=0.02, p<0.001). The direct effect of insomnia on suicidal ideation was no longer significant after accounting for thwarted belongingness (b=0.07, SE=0.04, p=0.08). The indirect effect of insomnia on suicidal ideation through thwarted belongingness was estimated to be between 0.0507 and 0.1364 (95%CI; effect=0.09, SE=0.02), indicating significance (R2=0.03, κ2=0.11; Figure 2). Insomnia was not a significant mediator of the relationship between thwarted belongingness and suicidal ideation (effect=0.0102, SE=0.0067, 95%CI:-0.0004, 0.0268), supporting the specificity of our proposed mediation model.
Figure 2.
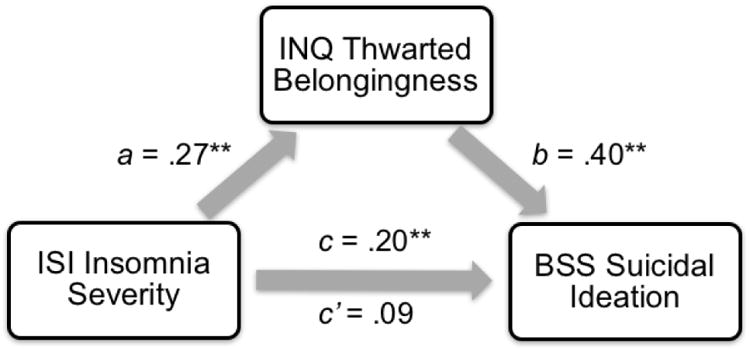
Standardized regression coefficients for the relationship between insomnia severity and suicidal ideation as mediated by thwarted belongingness in Study 2. Note. ** p < .001. ISI = Insomnia Severity Index. INQ = Interpersonal Needs Questionnaire-15. BSS = Beck Scale for Suicide Ideation.
After controlling for anxiety, the pattern of findings remained the same: the direct effect of insomnia on suicidal ideation was no longer significant after accounting for thwarted belongingness and anxiety (b=0.04, SE=0.05, p=0.45). The indirect effect of insomnia on suicidal ideation through thwarted belongingness, controlling for anxiety, was estimated to be between 0.0169 and 0.0932 (95%CI; effect=0.01, SE=0.003), indicating significance. Finally, anxiety was not a significant mediator of the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness (effect=0.04, SE=0.02; 95%CI=-0.0036, 0.0865).
Discussion
Again, consistent with our predictions and previous research, results indicated thwarted belongingness accounted for the relationship between insomnia and suicidal ideation, even when accounting for anxiety symptoms. As before, we found support for the specificity of the thwarted belongingness, as insomnia did not significantly mediate the relationship between thwarted belongingness and suicidal ideation and, in contrast to Study 1, anxiety did not significantly account for the relationship between insomnia and ideation. Importantly, the measure of anxiety symptoms used in this study exhibited excellent internal consistency, which bolsters these findings.
The present results are especially important because they highlight the role of thwarted belongingness in the relationship between insomnia and suicidal ideation in a sample with more severe psychiatric symptoms and suicide risk, for whom this research is particularly relevant and necessary. Findings underscore the importance of assessing and managing insomnia symptoms and feelings of thwarted belongingness in the outpatient treatment of suicidality.
Despite providing evidence for the clinical utility of this research, this is the first study to examine these hypotheses in a sample with more severe suicidality and as such, these findings have limited generalizability. Additional research among other high-risk groups is necessary to replicate and extend findings.
Study 3
Next, we sought to examine our hypotheses in another sample with elevated suicide risk. Specifically, given previous research revealing high rates of suicidality among firefighters and military service members (Ribeiro et al., 2012; Stanley et al., 2015), we investigated our hypotheses in a sample of firefighters, many of whom are currently serving or have previously served in the military. We hypothesized that thwarted belongingness would, again, emerge as a specific mediator.
Method
Participants
Participants were 858 current U.S. firefighters. The average length of service as a firefighter was 14.6 years (SD=10.2, range=0.5-60) with 27.1% reporting a history of military service (n=233). See Table 1.
Procedure
Data for Study 4 were obtained from a larger web-based study on mental health among U.S. firefighters (see Stanley et al., 2015 for details). Respondents completed an online consent form and battery of measures. All participants were provided with a debriefing form that included mental health resources and the option to receive a $10 gift card. The university's IRB approved study procedures.
Measures
Insomnia
Internal consistency of the ISI (Bastien et al., 2001) was excellent (α =0.91).
Thwarted belongingness
Internal consistency of the INQ-TB (Van Orden et al., 2012) was excellent (α =0.91).
Suicidal ideation
The Depressive Symptom Index – Suicidality Subscale (DSI-SS; Joiner, Pfaff, & Acres, 2009) is a 4-item measure of suicidal ideation. Items are rated on a 4-point Likert scale ranging from 0 to 3. Internal consistency of the DSI-SS was excellent (α =0.91).
Anxiety
In Study 3, participants reported any previous anxiety disorder diagnoses. A dichotomous variable representing the presence or absence of a previous anxiety disorder diagnosis was entered into analyses.
Statistical Analyses
The approach in Study 3 was similar to Studies 1 and 2. However, to accommodate a dichotomous mediator, Mplus 7 was used to evaluate the role of anxiety. Missing data were also minimal (<2.4%) and power was adequate.
Results
See Table 2 for information on Study 3 variables. For analyses examining the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness, the overall regression model explained a significant amount of variance in suicidal ideation (R2=0.29, F[2,834]=167.52, p <0.001). Insomnia was significantly related to thwarted belongingness (b=1.01, SE=0.06, p <0.001), and thwarted belongingness was significantly associated with suicidal ideation (b=0.07, SE=0.01, p <0.001). The direct effect of insomnia on suicidal ideation was no longer significant after accounting for thwarted belongingness (b=0.09, SE=0.01, p=0.06). The indirect effect of insomnia on suicidal ideation via thwarted belongingness was estimated to be between 0.0580 and 0.0912 (95%CI; effect=0.07, SE=0.01), indicating significance (R2=0.14, κ2=0.19; Figure 3). Insomnia was not a significant mediator of the relationship between thwarted belongingness and suicidal ideation (effect=0.02, SE=0.004, 95%CI:-0.0161, 0.0127), indicating specificity.
Figure 3.
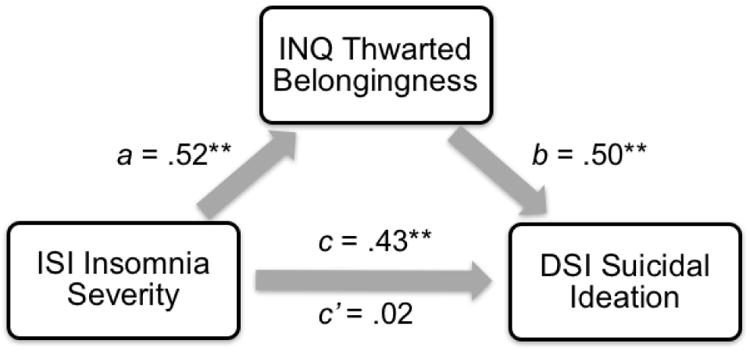
Standardized regression coefficients for the relationship between insomnia severity and suicidal ideation as mediated by thwarted belongingness in Study 3. Note. ** p < .001. ISI = Insomnia Severity Index. INQ = Interpersonal Needs Questionnaire-15. DSI = Depressive Symptom Index-Suicidality Subscale.
Controlling for anxiety, the pattern of findings remained the same: the direct effect of insomnia on suicidal ideation was no longer significant after accounting for thwarted belongingness and anxiety symptoms (b=0.09, SE=0.01, p=0.09). The indirect effect of insomnia on suicidal ideation through thwarted belongingness, controlling for anxiety, was estimated to be between 0.0472 and 0.0780 (95%CI; effect=0.09, SE=0.01), indicating significance. Finally, mediation analyses with anxiety as the mediator of the relationship between insomnia and suicidal ideation, controlling for thwarted belongingness, indicated a non-significant indirect effect (effect=0.01, SE=0.02; 95%CI=-0.352, -0.236).
Discussion
Study 3 extended findings to a sample of current firefighters. As noted, past research has demonstrated markedly elevated rates of suicidal ideation among firefighters (Stanley et al., 2015), and a recent systematic review of the literature revealed that few studies exist examining correlates of risk for suicidality among this unique population (Stanley et al., 2016). Only one study of which we are aware has previously documented insomnia as a correlate of suicidal ideation among firefighters (de Barros et al., 2012); this study was limited to firefighters in Brazil, and did not examine mechanisms such as thwarted belongingness (cf. loneliness) that may account for this link. Our study finding that loneliness may account for the link between insomnia and suicidal ideation among firefighters speaks to the relevance of peer support programs in ameliorating suicide risk among this population (Chu et al., 2016a; Finney et al., 2015; Stanley et al., 2016). Further, given that the shiftwork inherent in the firefighter vocation may confer risk for sleep disturbances (Hom et al., 2016), it is important for firefighters to receive sleep hygiene services (e.g., CBT-I) as needed in order to thwart the trajectory towards increased suicide risk. As in the previous studies, a rival mediator—anxiety symptoms—did not demonstrate a mediating effect, which highlights the specificity of thwarted belongingness as the mediator.
There are several notable strengths of Study 3. Namely, this is the first study of which we are aware documenting a possible explanation for the link between insomnia and suicidality among firefighters. Additionally, a substantial proportion (27.1%) of this sample of firefighters also has previous or concurrent military experience. Findings, therefore, may extend to military samples as well; however, future studies are needed in this regard.
There are also several limitations to note. First, although the sample is large and includes a heterogeneous group of firefighters (i.e., those representing both volunteer and career departments), probability sampling strategies were not employed, and thus the sample may not be representative of the fire service at large. Additionally, these data are cross-sectional, and although statistical mediation was established, the data do not speak to the temporality between variables.
Study 4
Given the limitations of Studies 1, 2 and 3's cross-sectional designs, we sought to examine the predictive utility of our hypotheses in Study 4 in a primary care patient sample.
Method
Participants
Participants were 217 patients presenting for treatment at a Southeastern U.S. primary care clinic that serves low-income individuals (Table 1).
Procedure
These data originated from a larger study examining risk and protective factors for treatment adherence in primary care patients. All participants provided informed consent at baseline and follow-up. Most patients completed the follow-up assessment after a period of 6 months; however, due to difficulties contacting participants, the follow-up period ranged from 6 to 12 months (M=8). In this sample, 99 (45.6%) completed the follow-up assessment. Participants were monetarily compensated following completion. The study was approved by the university's IRB.
Measures
Insomnia
At Time 1, the 9-item Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001) is a subset of the full PHQ, which is used to screen for a broad range of mental health disorders. Items are rated on a 4-point rating scale, ranging from 0 to 3. In this study, PHQ-9 item 3, “Trouble falling or staying asleep, or sleeping too much” was used as proxy measure of insomnia; caution is warranted in interpretation given that this item also reflects broader sleep disturbances. Previous research has indicated high concurrent validity between the PHQ-9 item 3 and the ISI (r=0.75), which supports its utility as a proxy measure of insomnia (MacGregor et al., 2012).
Thwarted belongingness
Internal consistency of the INQ-TB (Van Orden et al., 2012) was excellent at Time 1 (α =0.90) and good at Time 2 (α =0.89), and were moderately correlated across time (r=0.53, Table 2).
Suicidality
The 4-item Suicide Behavior Questionnaire - Revised (SBQ-R; Osman et al., 2001) assesses lifetime and past-year suicidal ideation and behavior as well as disclosure of suicidal intent and likelihood of dying by suicide. Total scores range from 3 to 18 with a score of 7 indicating significant suicidal ideation and/or attempts in nonclinical, adult populations. Osman et al. (2001) adequate internal consistency for the SBQ-R in a sample of undergraduate students (α =0.76). Internal consistency of the SBQ-R was good at Times 1 and 2 (α =0.86, 0.84, respectively) and weakly correlated across time (r=0.19, Table 2).2
Anxiety
As in Study 3, participants indicated the presence or absence of an anxiety disorder diagnosis.
Statistical Analyses
The statistical approach was consistent with above. However, hypotheses were tested both cross-sectionally at Time 1, and longitudinally, across Times 1 and 2. Given that only two time points were available, we tested two models: first, we examined the effect of Time 1 insomnia on Time 2 suicidality through thwarted belongingness at Time 1 and subsequently, we examined the mediating role of thwarted belongingness at Time 2. As in Study 3, Mplus 7 was used to accommodate a dichotomous mediator. Missing data were also minimal (<3%) and power was sufficient for mediation analyses.
Results
Details on all Study 4 variables are presented in Table 2. At Time 1, cross-sectionally, for analyses examining the relationship between PHQ-9 insomnia and SBQ-R suicidality, controlling for INQ thwarted belongingness, the overall regression model explained a significant amount of variance in suicidality (R2=0.30, F[2,208]=44.66, p<0.001; Figure 4A). More severe insomnia was significantly associated with greater thwarted belongingness (b=5.67, SE=0.75, p<0.001), and greater thwarted belongingness was related to more severe suicidality (b=0.13, SE=0.02, p<0.001). The direct effects of insomnia on suicidality were no longer significant after accounting for thwarted belongingness (b=0.37, SE=0.21, p=0.08). The indirect effect of insomnia on suicidality through thwarted belongingness was estimated to be between 0.4847 and 1.0741 (95%CI; effect=0.72, SE=0.14), indicating significance (R2=0.11, κ2=0.22). Additionally, mediation analyses indicated that insomnia was not a significant mediator of the relationship between thwarted belongingness and suicidality (effect=0.01, SE=0.01, 95%CI:-0.0001, 0.0321).
Figure 4.
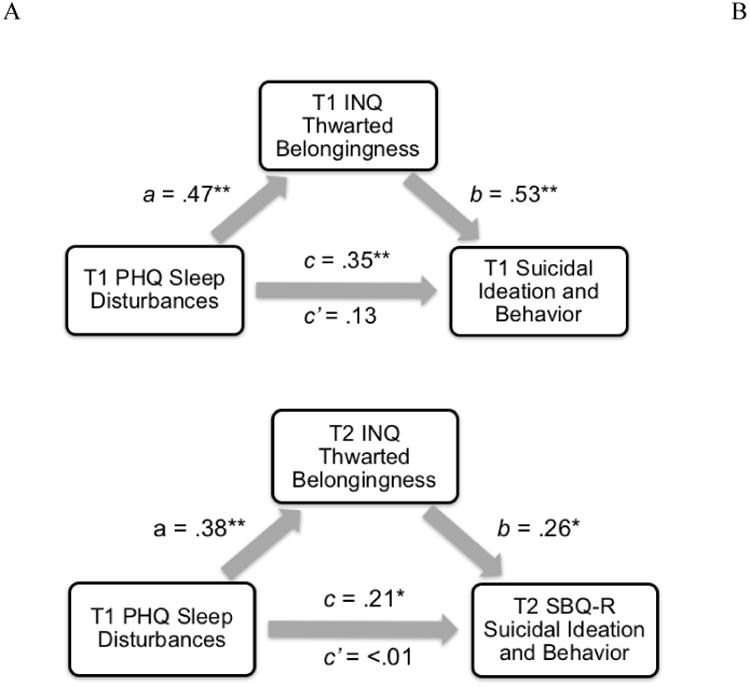
Standardized regression coefficients for the relationship between sleep disturbances and suicidal ideation and behavior as mediated by thwarted belongingness in Study 4 at Time 1 (Fig. 4A), and longitudinally, between Time 1 and 2 (Fig. 4B). Note. ** p ≤ .001; * p ≤ .05. T1 = Time 1. T2 = Time 2, 6 months follow-up. PHQ = Patient Health Questionnaire-9 (item 3). INQ = Interpersonal Needs Questionnaire-15. SBQ-R = Suicide Behavior Questionnaire-Revised.
After controlling for anxiety, the pattern of findings remained the same at Time 1. The direct effect of insomnia on suicidality was no longer significant after accounting for thwarted belongingness and anxiety (b=0.31, SE=0.21, p=0.14), indicating mediation. The indirect effect of insomnia on suicidality through thwarted belongingness, controlling for anxiety, was estimated to be between 0.4097 and 0.9492 (95%CI; effect=0.64, SE=0.14). Mediation analyses with anxiety as the mediator of the relationship between insomnia and suicidality, controlling for thwarted belongingness at Time 1, indicated a non-significant indirect effect (effect=0.36, SE=0.26, 95%CI=-0.015, 0.355). Of note, the same pattern of results were obtained cross-sectionally at Time 2.3
In order to examine the longitudinal prediction of suicidality, we examined the relationship between Time 1 PHQ-9 insomnia and Time 2 SBQ-R suicidality through Time 1 INQ thwarted belongingness, controlling for SBQ-R suicidality. The overall regression model explained a significant portion of the variance in suicidality (R2=0.59, F[3,89]=42.88, p<0.001). Insomnia significantly predicted thwarted belongingness (b=6.65, SE=1.06, p<0.001), and thwarted belongingness significantly predicted suicidality (b=0.12, SE=0.03, p<0.001). The direct effect of insomnia on suicidality was no longer significant after accounting for thwarted belongingness (b=0.22, SE=0.62, p=0.54). The indirect effect of Time 1 insomnia on Time 2 suicidality through Time 2 thwarted belongingness, controlling for Time 1 suicidality, was estimated to be between 0.4167 and 1.2785 (95%CI; effect=0.79, SE=0.22), indicating significance. Finally, mediation analyses indicated that Time 1 insomnia was not a significant mediator of the relationship between Time 1 thwarted belongingness and Time 2 suicidality (effect=0.01, SE=0.02, 95%CI:-0.0183, 0.0404).
After controlling for anxiety, the pattern of findings remained the same such that the direct effect of Time 1 insomnia on Time 2 suicidality was no longer significant after accounting for Time 1 thwarted belongingness, Time 1 suicidality, and anxiety (b=-0.19, SE=0.37, p=0.62). The indirect effect of insomnia on suicidality through thwarted belongingness, controlling for Time 1 suicidality and anxiety, was estimated to be between 0.0483 and 0.6797 (95%CI; effect=0.32, SE=0.16), indicating significance. Mediation analyses with anxiety as the mediator of the relationship between Time 1 insomnia and Time 2 suicidality, controlling for Time 1 thwarted belongingness and Time 1 suicidality, indicated that the indirect effect was not significant (effect=0.11, SE=0.08, 95%CI=-0.0124, 0.3447).
Finally, we examined the relationship between Time 1 PHQ-9 insomnia and Time 2 SBQ-R suicidality (Figure 4B) through Time 2 INQ thwarted belongingness, controlling for Time 1 SBQ-R suicidality. The overall regression model explained a significant portion of the variance in suicidality (R2=0.134, F[3,91]=4.69, p=0.004). Insomnia significantly predicted thwarted belongingness (b=2.25, SE=1.18, p=0.049), and thwarted belongingness significantly predicted suicidality (b=0.24, SE=0.09, p=0.005). The direct effect of insomnia on suicidality was no longer significant after accounting for thwarted belongingness (b=-1.94, SE=0.99, p=0.06). The indirect effect of Time 1 insomnia on Time 2 suicidality through Time 2 thwarted belongingness, controlling for Time 1 suicidality, was estimated to be between 0.0485 and 2.6856 (95%CI; effect=0.55, SE=0.51), indicating significance. Finally, mediation analyses indicated that insomnia was not a significant mediator of the relationship between thwarted belongingness and suicidality (effect=0.002, SE=0.08, 95%CI:-0.1675, 0.1373).
After controlling for anxiety, the pattern of findings remained the same longitudinally. The direct effect of insomnia at Time 1 on suicidality at Time 2 was no longer significant after accounting for thwarted belongingness, Time 1 suicidality, and anxiety (b=-1.89, SE=1.00, p=0.06). The indirect effect of insomnia on suicidality through thwarted belongingness, controlling for Time 1 suicidality and anxiety, was estimated to be between 0.0199 and 2.1167 (95%CI; effect=0.46, SE=0.44), indicating significance. Mediation analyses with anxiety as the mediator of the relationship between Time 1 insomnia and Time 2 suicidality, controlling for Time 2 thwarted belongingness and Time 1 suicidality, indicated that the indirect effect was not significant (effect=0.01, SE=0.10, 95%CI=-0.009, 0.006).
Discussion
Results suggest that there exists a prospective relationship between sleep disturbances, including insomnia, and suicidal ideation and behavior. Importantly, the pattern of findings remained the same both cross-sectionally and longitudinally, supporting the predictive validity of our hypotheses. Findings remained even after accounting for baseline suicidal symptoms and anxiety, which highlights the strength of the prospective relationship as it suggests that this relationship is not fully accounted for by anxiety symptoms. As discussed previously, since anxiety disorders are often characterized by overarousal and withdrawal symptoms (APA, 2013), this finding is particularly noteworthy. As in Studies 1 and 2, our findings provided support for the specificity of the role of the mediator in our analyses. Most notably, across both time points, anxiety was not a significant mediator, which further underscores the specificity and strength of our findings.
Previous reviews have reported that 45% of individuals who die by suicide made contact with their primary care provider in the month prior to death with even higher rates in older adults (Luoma et al., 2002). Thus, our use of an adult primary care sample is also noteworthy as these settings represent key catchment areas for individuals at risk for suicide. However, limitations should be noted. For one, only two time points were available in this dataset. Although we showed that thwarted belongingness at both Times 1 and 2 significantly mediated the relationship between insomnia and suicidality, future studies using more than two time points and a variety of time frames will be necessary to further delineate this temporal relationship and to robustly establish the roles of the mediator and the predictor (Maric et al., 2012). Given that this was the first longitudinal test of these hypotheses, these prospective results may not generalize beyond primary care patients. Further, Study 4 was also limited by the use of one item to capture sleep disturbances broadly. Thus, further work in other samples using more robust measures of insomnia specifically is needed to replicate and extend findings.
General Discussion
This manuscript explored the cross-sectional and prospective associations between insomnia and suicidality in four distinct samples. Findings provided converging evidence that severe insomnia is associated with increased feelings of thwarted belongingness and severity of suicidality. Furthermore, our research indicates that thwarted belongingness may in part explain the robust link between insomnia and suicidality, and this relationship exists independent of anxiety symptoms. Overall, our findings contribute to the growing body of research revealing the psychosocial consequences of sleep problems. Thus, this research has significant empirical and clinical implications.
First, it is important to highlight that our pattern of findings emerged across four samples, which were diverse not only with respect to their demographic qualities but also the severity of their clinical presentation. The replicability of this finding across a broad spectrum of individuals is notable as it suggests that insomnia not only negatively impact those who are vulnerable to psychological disorders, but also the general population. Despite robust evidence for the relationship between insomnia and suicide (e.g., Bernert et al., 2015), few studies to date have examined the underlying mechanisms. The current study adds to recent work indicating that thwarted belongingness may be one of these mechanisms, not only among young adults in East Asia (Chu et al., 2016b) but also in Western societies. It is important to note that these findings and those of Chu and colleagues (2016b) contrast those reported by Nadorff and colleagues' (2014), which indicated that insomnia remained associated with suicidal ideation even after controlling for interpersonal theory variables. It is possible that this difference in results was a result of alternate statistical approaches since Nadorff and colleagues (2014) did not employ mediation analyses to directly test thwarted belongingness as an explanatory link between insomnia and suicidal ideation. Thus, it is unclear whether thwarted belongingness may have partially mediated this relationship in their sample. This discrepancy also highlights the need for further replication using mediation models across diverse samples.
Second, it is notable that, conversely, insomnia did not significantly mediate the relationship between thwarted belongingness and suicidal ideation. This is an indicator of the specificity of our results and further strengthens our findings. This finding additionally bolsters the growing body of literature supporting the central role of thwarted belongingness as a mechanism for impacting suicidal desire (e.g., Chu et al., 2015a) and the conjectures of the interpersonal theory (Van Orden et al., 2010).
Given that anxiety symptoms have been shown to be associated with insomnia, thwarted belongingness, and suicidal ideation, it is also particularly notable that findings remained significant even after controlling for anxiety symptoms. Furthermore, anxiety symptoms did not significantly mediate the relationship between insomnia and suicide either in Studies 2, 3, and 4. As discussed previously, key features of anxiety disorders include insomnia and social withdrawal (APA, 2013). Thus, our findings not only highlight the robust association between insomnia and suicide, but they also suggest that this association is not merely a clustering of anxiety symptoms. In contrast, it should be noted that, in Study 1, anxiety symptoms did emerge as a significant mediator. However, due to the low internal consistency of the anxiety symptom measure, further investigation is needed to determine whether low internal consistency or other factors, such as demographic differences (e.g., young adult college students), drove these countervailing results. Nonetheless, our results largely indicated that our findings were not simply driven by the effects of anxiety and provide support for the independent role of thwarted belongingness.
In addition to replicating our findings cross-sectionally across samples, we also extended support for our hypotheses by incorporating a longitudinal study design in Study 4. Findings not only support the predictive validity of insomnia as an indicator of subsequent suicide-related symptoms, but also the mediating role of thwarted belongingness in this prediction. Specifically, our findings indicate that, over time, individuals who experience insomnia may be at increased risk for suicide after approximately 6 to 12 months, and that increased feelings of social disconnection may help explain this relationship. A follow-up period of approximately 6-12 months is also particularly advantageous with regard to understanding changes in suicide-related behaviors as prior research has indicated that risk for attempting suicide is highest within the 6 months to two years following a recent attempt (Christiansen & Jensen, 2007; Chu et al., 2015b). Thus, replication of these findings will be vital for understanding imminent suicide risk factors.
In Study 4, our measure of insomnia was nonspecific and also captured a broader range of sleep disturbances, including hypersomnia (i.e., sleeping too many hours). Previous studies examining these hypotheses have focused on insomnia symptoms (Chu et al., 2016b); however, hypersomnia may also have social consequences that lead to increased severity of suicide-related behaviors. For example, hypersomnia may increase daytime sleepiness and decrease opportunities for interpersonal interactions (Jennum et al., 2014), and thus, lead to loneliness. Preliminary findings from Study 4 shed light on potential areas for expanding on the present research.
Our research also has important clinical implications. For one, our findings underscore the importance of routinely assessing and addressing any sleep disturbances across health care settings, including university counseling, primary care, and outpatient psychological treatment clinics. Additionally, clinicians treating individuals who present with sleep difficulties or high levels of thwarted belongingness should regularly monitor and assess suicide risk using empirically informed suicide risk assessment approaches (e.g., Jobes, 2006; Joiner et al., 1999; Chu et al., 2015b). For patients experiencing sleep disturbances, monitoring of sleep habits and treatments targeting sleep, such as cognitive behavioral therapy for insomnia (CBT-I; Edinger & Means, 2005), may be indicated. CBT-I may also be delivered in a group format, which would be particularly useful for increasing feelings of belongingness and facilitating social connections. Furthermore, our results support the utility of monitoring and targeting feelings of thwarted belongingness in treatment. In particular, cognitive therapy approaches, which may involve identifying and restructuring distorted cognitions and beliefs about whether one belongs and one's relationships with others, may be effective (Joiner et al., 2009). Our findings are particularly relevant given the relatively low rates of help-seeking among those in need of treatment for suicidal symptoms (Hom et al., 2015) and that sleep disturbances are less stigmatized than suicidal thoughts. Therefore, treatments targeting difficulties in sleep and interpersonal functioning, which are deficits that are more socially accepted, may increase treatment seeking, adherence, and, ultimately, symptom remission.
Strengths, Limitations, and Future Directions
A significant strength of this multi-study investigation was the use of a robust analytic approach to examine the relationship between insomnia, loneliness, and suicidal ideation across three unique samples. Utilization of clinical outpatient and primary care samples also enhanced the generalizability of findings. Of note, Study 4, in particular, afforded us the unique opportunity to examine the prospective relationship between insomnia and suicidal ideation and to identify thwarted belongingness as an explanatory factor in this relationship. This represented an improvement upon a prior study conducted by Chu and colleagues (2016b) that was only able to examine the cross-sectional relationship between these variables in a sample of South Korean University students.
Despite these strengths, several limitations in these studies merit consideration. Although the samples included in this investigation were distinct from one another, they were restricted in sociodemographic and geographic diversity, which limits the generalizability of our findings. Consequently, additional research is indicated to examine whether this pattern of findings emerges across geographic regions (Chu et al., 2016b), clinical settings, and individuals from various socioeconomic backgrounds. As noted above, only cross-sectional data were available for Studies 1,2, and 3, and only two time points were available in Study 4; thus, the temporal relationship between insomnia and suicidality could not be determined definitively. Future studies incorporating more robust longitudinal designs will allow us to identify whether this pathway appears to more accurately capture short-term risk, long-term risk, or both, which would inform prevention efforts focused on thwarting the trajectory from sleep problems to suicide.
Furthermore, all three studies relied on self-report data. Future research in this domain may benefit both from the objective measurement of sleep disturbances (e.g., polysomnography, actigraphy) and implicit measurement of suicidal ideation (e.g., implicit association test; Nock et al., 2010), especially to circumvent stigma and other related concerns that may lead to inaccurate reporting or underreporting of symptoms. Relatedly, it is also possible that the INQ-TB may not fully capture the construct of loneliness that might arise from insomnia, especially since this measure was not designed with this intention. Therefore, it may be useful for studies aiming to replicate these findings to include a more direct measure of loneliness (e.g., UCLA Loneliness Scale; Russell et al., 1980). Relatedly, given that insomnia and hypersomnia can co-occur and are both correlated with suicidal behavior and increased severity of clinical presentation (Soehner et al., 2014), research that utilizes psychometrically sound measures of hypersomnia will be important for substantiating and furthering our findings.
In this manuscript, we presented evidence that more severe insomnia is associated with increased severity of suicidal ideation and behavior, and thwarted belongingness accounted for the relationship between insomnia and suicidality in four samples. Overall, our findings support the utility of encouraging social connections in suicide prevention and treatment efforts, particularly among individuals experiencing sleep problems.
Highlights.
Insomnia is a robust predictor of suicidality
We examine thwarted belongingness as an explanatory factor in four samples
Insomnia was significantly related to thwarted belongingness and suicidality
Thwarted belongingness accounted for relations between insomnia and suicidality
Anxiety did not significantly account for relations between insomnia and suicidality
Acknowledgments
This research was supported, in part, by a grant from the National Institute of Mental Health (T32 MH093311-04) and a grant from the National Fallen Firefighters Foundation. This work was also supported by the Military Suicide Research Consortium (MSRC) and the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-10-2-0181). Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense.
Footnotes
Hom and colleagues (under review) also conducted analyses examining the direct effect of insomnia severity on loneliness (c.f thwarted belongingness) in a subset of the Study 2 data. Although the direct effects are similarly reported in this manuscript, this study extends previous findings as it incorporates recently collected data. In this sample, 23.6% (n = 83) of the cases were new. Additionally, the emphasis of this manuscript is on the mediating role of thwarted belongingness in the relationship between insomnia and suicidal ideation and behavior, whereas Hom et al. did not examine this issue. Furthermore, this paper also presents evidence for the specificity of thwarted belongingness as the mediator using two different approaches, which further distinguishes this manuscript from that of Hom and colleagues (under review). Of note, the pattern of findings remained the same when analyzing the new cases in isolation, which supports the significance of the present results.
Item level analysis did not indicate any anomalies in the SBQ-R items and accordingly, adequate internal consistencies were observed for the SBQ-R at both time points. The low test-retest reliability of the SBQ-R may be a reflection of the fluctuations in suicide risk over time (Bryan & Rudd, 2016).
These analyses were also conducted at Time 2, cross-sectionally, using the Medical Outcomes Study Sleep Scale, Sleep Disturbance subscale (Stewart, Ware, Brook, & Davies, 1978), as the measure of insomnia. Notably, the pattern of findings remained the same.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Association; Washington: 2013. [Google Scholar]
- Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psych. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. Psychological Corporation; San Antonio: 1990. [Google Scholar]
- Bernert RA, Joiner TE. Sleep disturbances and suicide risk: A review of the literature. Neuropsychiatr Dis Treat. 2007;3(6):735–743. doi: 10.2147/ndt.s1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatr Rep. 2015;17(3):1–9. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Turvey CL, Conwell Y, Joiner TE. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: A longitudinal, population-based study of late life. JAMA Psychiatr. 2014;71(10):1129–1137. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD. The importance of temporal dynamics in the transition from suicidal thought to behavior. Clin Psychol-Sci Pr. 2016;23(1):21–25. [Google Scholar]
- Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatr. 1990;17(1):5–12. [PubMed] [Google Scholar]
- Christiansen E, Frank Jensen B. Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. Australian and New Zealand J Psychiatr. 2007;41(3):257–265. doi: 10.1080/00048670601172749. [DOI] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Hom MA, Stanley IH, Joiner TE. A test of the interpersonal theory of suicide in a large sample of current firefighters. Psychiatr Res. 2016a;240:26–33. doi: 10.1016/j.psychres.2016.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Moberg FB, Joiner TE. Thwarted belongingness mediates the relationship between fear of negative evaluation and suicidal ideation. Cog Ther Res. 2015a:1–7. doi: 10.1007/s10608-015-9715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Hom MA, Rogers ML, Ringer FB, Hames JL, Suh S, Joiner TE. Is insomnia lonely? Exploring thwarted belongingness as an explanatory link between insomnia and suicidal ideation in a sample of South Korean university students. J Clin Sleep Med. 2016b doi: 10.5664/jcsm.5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Klein KM, Buchman‐Schmitt JM, Hom MA, Hagan CR, Joiner TE. Routinized assessment of suicide risk in clinical practice: An empirically informed update. J Clin Psychol. 2015b;71(12):1186–1200. doi: 10.1002/jclp.22210. [DOI] [PubMed] [Google Scholar]
- de Barros VV, Martins L, Saitz R, Bastos RR, Ronzani TM. Mental Health conditions, individual and job characteristics and sleep disturbances among firefighters. J Health Psych. 2012;18(3):350–358. doi: 10.1177/1359105312443402. [DOI] [PubMed] [Google Scholar]
- Edinger J, Means M. Cognitive–behavioral therapy for primary insomnia. Clin Psychol Rev. 2005;2i5:539–558. doi: 10.1016/j.cpr.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Finney EJ, Buser SJ, Schwartz J, Archibald L, Swanson R. Suicide prevention in fire service: The Houston Fire Department (HFD) model. Aggress Viol Behav. 2015;21:1–4. [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psych Sci. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding S, Nadorff MR, Winer ES, Ward KC. Unpacking Sleep and Suicide in Older Adults in a Combined Online Sample. J Clin Sleep Med. 2014;11(12):1385–1392. doi: 10.5664/jcsm.5270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York: 2013. [Google Scholar]
- Hom MA, Hames JL, Bodell LP, Buchman-Schmitt JM, Chu C, Chiurliza B, et al. Joiner TE. Insomnia is lonely under review. [Google Scholar]
- Hom MA, Stanley IH, Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: a review of the literature. Clin Psych Rev. 2015;40:28–39. doi: 10.1016/j.cpr.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Hom MA, Stanley IH, Rogers ML, Tzoneva M, Bernert RA, Joiner TE. The association between sleep disturbances and depression among firefighters: Emotion dysregulation as an explanatory factor. J Clin Sleep Med. 2016;12(02):235–245. doi: 10.5664/jcsm.5492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennum P, Ibsen R, Avlund K, Kjellberg J. Health, social and economic consequences of hypersomnia: a controlled national study from a national registry evaluating the societal effect on patients and their partners. Europ J Health Econ. 2014;15(3):303–311. doi: 10.1007/s10198-013-0491-2. [DOI] [PubMed] [Google Scholar]
- Jobes DA. Managing suicidal risk: A collaborative approach. The Guilford Press; New York: 2006. [Google Scholar]
- Joiner TE. Why People Die by Suicide. Harvard University Press; Cambridge: 2005. [Google Scholar]
- Joiner TE, Pfaff JJ, Acres JG. A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behav Res Ther. 2002;40(4):471–481. doi: 10.1016/s0005-7967(01)00017-1. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Van Orden KA, Witte TK, Rudd MD. The interpersonal theory of suicide: Guidance for working with suicidal clients. American Psychological Association; 2009. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, Ober C. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011;34(11):1519–26. doi: 10.5665/sleep.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatr. 2002;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGregor KL, Funderburk JS, Pigeon W, Maisto SA. Evaluation of the PHQ-9 Item 3 as a screen for sleep disturbance in primary care. J Gen Intern Med. 2012;27(3):339–344. doi: 10.1007/s11606-011-1884-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maric M, Wiers RW, Prins PJ. Ten ways to improve the use of statistical mediation analysis in the practice of child and adolescent treatment research. Clin Child Fam Psych Rev. 2012;15(3):177–191. doi: 10.1007/s10567-012-0114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Blocker JN, D'Agostino R, Kimball J, Boggs N, Lasater B, Rosenquist PB. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11(9):822–7. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadorff MR, Anestis MD, Nazem S, Harris HC, Winer ES. Sleep disorders and the interpersonal-psychological theory of suicide: Independent pathways to suicidality? J Affect Disord. 2014:152–154. 505–12. doi: 10.1016/j.jad.2013.10.011. [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind: Implicit cognition predicts suicidal behavior. Psychol Sci. 2010;21(4):511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assess. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatr. 2012;73(9):e1160–7. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE., Jr Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136(3):743–750. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Chen IG. Functioning of adolescents with symptoms of disturbed sleep. J Youth Adol. 2001;30(1):1–18. [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J Pers Soc Psych. 1980;39(3):472–80. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23(2):243–308. [PubMed] [Google Scholar]
- Soehner AM, Kaplan KA, Harvey AG. Prevalence and J Affect Disord. 2014;167:93–97. doi: 10.1016/j.jad.2014.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley IH, Hom MA, Hagan CR, Joiner TE. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J Affect Disord. 2015;187:163–171. doi: 10.1016/j.jad.2015.08.007. [DOI] [PubMed] [Google Scholar]
- Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psych Rev. 2016;44:25–44. doi: 10.1016/j.cpr.2015.12.002. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE., Jr Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24(1):197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46(7):953–959. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011;45(4):505–11. doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO] Preventing suicide: A global imperative. WHO Press; Geneva: 2014. [Google Scholar]


