Abstract
Objective To test whether the number of reports of enjoyment of life over a four year period is quantitatively associated with all cause mortality, and with death from cardiovascular disease and from other causes.
Design and setting Longitudinal observational population study using the English Longitudinal Study of Ageing (ELSA), a nationally representative sample of older men and women living in England.
Participants 9365 men and women aged 50 years or older (mean 63, standard deviation 9.3) at recruitment.
Main outcome measures Time to death, based on mortality between the third phase of data collection (wave 3 in 2006) and March 2013 (up to seven years).
Results Subjective wellbeing with measures of enjoyment of life were assessed in 2002 (wave 1), 2004 (wave 2), and 2006 (wave 3). 2264 (24%) respondents reported no enjoyment of life on any assessment, with 1833 (20%) reporting high enjoyment on one report of high enjoyment of life, 2063 (22%) on two reports, and 3205 (34%) on all three occasions. 1310 deaths were recorded during follow-up. Mortality was inversely associated with the number of occasions on which participants reported high enjoyment of life. Compared with the no high enjoyment group, the hazard ratio for all cause mortality was 0.83 (95% confidence interval 0.70 to 0.99) for two reports of enjoyment of life, and 0.76 (0.64 to 0.89) for three reports, after adjustment for demographic factors, baseline health, mobility impairment, and depressive symptoms. The same association was observed after deaths occurring within two years of the third enjoyment measure were excluded (0.90 (0.85 to 0.95) for every additional report of enjoyment), and in the complete case analysis (0.90 (0.83 to 0.96)).
Conclusions This is an observational study, so causal conclusions cannot be drawn. Nonetheless, the results add a new dimension to understanding the significance of subjective wellbeing for health outcomes by documenting the importance of sustained wellbeing over time.
Introduction
There is growing evidence that subjective wellbeing is associated with reduced risk of all cause mortality and the incidence of specific conditions such as coronary heart disease (CHD).1 2 A meta-analysis of longitudinal observational studies published before 2008 indicated that greater wellbeing was associated with lower all cause mortality in initially healthy population cohorts (adjusted hazard ratio 0.82, 95% confidence interval 0.76 to 0.89), although there were indications of publication bias.3 Subsequently, several studies have documented protective associations between various measures of subjective wellbeing and mortality,4 5 6 7 8 9 10 albeit with some exceptions.11 In an earlier analysis of the English Longitudinal Study of Ageing (ELSA), we found that a one-off assessment of a four item measure of enjoyment of life was associated with reduced mortality over an average of 7.3 years. This association was independent of demographic factors, baseline illness, depressive symptoms, and health behaviours such as smoking and physical activity.12 Associations were maintained after the exclusion of people who died within two years of assessment, arguing against reverse causality, or terminal decline leading to reduced enjoyment of life and early mortality.
To date, studies have assessed subjective wellbeing on one occasion. But another aspect of exposure might be important, namely the duration of the experience. Evidence of time dependent exposure effects would increase confidence in a potential causal association. In the present analysis, we tested the notion that repeated reports over several years would have a stronger association with mortality than a single occurrence. We used measures of enjoyment of life taken three times at two year intervals between 2002 and 2006, and analysed associations with mortality up to 2013, predicting that a temporal dose-response association would be apparent. We adjusted statistically for a wide range of demographic, health, functional, emotional, and behavioural confounders; used multiple imputation to account for item non-response and attrition throughout the study; and tested associations with all cause mortality, deaths from cardiovascular disease (CVD), and deaths from other causes.
Methods
Participants
The English Longitudinal Study of Ageing (ELSA) is a panel study of men and women aged 50 and older living in England.13 The study began in 2002 (first phase of data collection referred to as wave 1) with 11 391 individuals who had previously taken part in the Health Survey for England. Comparisons of the sociodemographic characteristics of participants with national census data show that the sample is representative of the English population aged 50 and over. We excluded from the analysis proxy interviewees (n=330), those who did not provide a response to all items on the measure of enjoyment of life at wave 1 in 2002 (n=860), and those who had died between wave 1 and wave 3 of data collection in 2006 (n=836), resulting in an analytical sample of 9365. Participants were tracked for mortality from wave 3 of ELSA (2006) until March 2013, an average of 6.5 years (maximum follow-up seven years), during which there were 1310 deaths. For sensitivity analyses, we used wave 1 as the baseline, so the maximum follow-up was 11 years.
Measures
Enjoyment of life was indexed with four items from the CASP-19 quality of life instrument, as described previously.12 14 This was administered in waves 1 (2002), 2 (2004) and 3 (2006). Each item (“I enjoy the things that I do”; “I enjoy being in the company of others”; “On balance, I look back on my life with a sense of happiness”; “I feel full of energy these days”) was assessed on a four point scale, from 0 (“never”) to 3 (“often”), and was subsequently coded as 0 (“never or rarely”) and 1 (“sometimes and often”). The four binary items were summed to generate the number of items for which enjoyment was reported, with scores ranging from 0 to 4.
We then generated a variable for enjoyment, defining no enjoyment as scores from 0 to 2, and high enjoyment if scores were 3 or 4 (meaning that the individual reported enjoyment on 3 or 4 of the items). Socioeconomic status was indexed by total household wealth, including financial wealth (savings and investments), the value of any home and other property (less mortgage), the value of any business assets, and physical wealth such as artwork and jewellery, net of debt. Education was based on the highest qualification achieved and categorised into lower (no qualifications), intermediate (qualifications below college degree level), and higher (college degree or higher). We also included information on age, sex, ethnicity (white European v other ethnicity), marital status (cohabiting or not with a partner), and employment status (in paid employment or not in paid employment).
Baseline health was assessed with a combination of general and disease specific measures. Participants rated their health on a standard five point self-assessment scale from excellent to poor15; ratings of fair or poor were categorised as impaired self-rated health. We also asked if participants had any longstanding illnesses, and if the illnesses limited their daily activities; responses were combined to form a dichotomous variable, classifying participants as having a limiting longstanding illness or not. Participants were asked whether they had been given a doctor diagnosis of coronary heart disease, cancer, diabetes, stroke, arthritis, chronic lung disease (asthma, bronchitis, and chronic lung disease), and depression. Depressive symptoms were measured at baseline using the eight item Centre for Epidemiologic Studies Depression Scale (CES-D), and a score of at least 4 indicated elevated depressive symptoms.16 We considered mobility to be impaired if participants reported difficulties with one or more of 10 items concerning mobility or fine motor function (eg, climbing one flight of stairs without resting, picking up a small coin from a table), or impairment of one or more of six activities of daily living (eg, getting in or out of bed). Current smoking, vigorous or moderate activity at least once per week, and drinking alcohol at least daily at baseline were also recorded.
Mortality data were obtained from the National Health Service central data registry. We analysed data on all cause mortality until March 2013, together with deaths resulting from cardiovascular disease, as defined at chapter level by ICD-10 (international classification of diseases, 10th revision; myocardial infarction, coronary heart disease, cerebral infarction, and other cardiovascular diseases), and deaths from non-cardiovascular causes.
Statistical analysis
We generated a sustained enjoyment variable by summing the number of reports of high enjoyment of life between 2002 and 2006; scores could range from none to three reports for each individual. Having ascertained that the proportional hazards assumption had not been violated, Cox proportional hazards regression models were used to estimate hazard ratios of death and 95% confidence intervals in relation to number of reports of high enjoyment, with the reference group being those with no reports of high enjoyment on any occasion. Survival time was measured in months from date of interview (wave 3 in main analyses and wave 1 in sensitivity analysis 3) to date of death, or to follow-up in March 2013.
Five models were tested in the analyses of all cause mortality. Model 1 was adjusted for age (categorised as 50-59, 60-69, 70-79, and ≥80 years) and sex. Demographic factors (wealth, education, ethnicity, marital status, and employment status) were added in model 2, while model 3 added baseline health indicators (poor self-rated health, limiting longstanding illness, cancer, coronary heart disease, stroke, diabetes, arthritis, and chronic lung disease, impaired mobility, and impaired activities of daily living) to model 1. In model 4, depressive illness and depressive symptoms were added to model 1 to establish whether associations between enjoyment of life and mortality were independent of negative emotional states. The fully adjusted analysis in model 5 was adjusted for all the variables mentioned above. Separate regression analyses were carried out of non-cardiovascular deaths and deaths from cardiovascular disease. In addition, we modelled enjoyment of life as a continuous score (0, 1, 2, 3) where the hazard ratios represent (in the last column of each table) a one report increase of enjoyment of life.
Data on enjoyment of life and covariates at all waves were available for 5262 people. We imputed missing data due to attrition and item non-response using multiple imputation by chained equations, which included all variables (including the survival outcome) in the prediction model to generate 10 imputed datasets (each had a final n=9365). With imputations, all individuals in the initial sample had a measure of enjoyment at all three waves. In order to strengthen the missing at random assumption, we included in the imputation model two auxiliary variables known to be predictive of non-response (year of Health Survey for England interview, household size). Owing to the greater precision offered, we present the analyses from the imputed datasets in this paper.
We carried out four sensitivity analyses. Firstly, we ran our analysis on the complete case sample of 5262 participants without any missing data across all waves. Secondly, we examined all permutations of the timing of enjoyment ratings, to investigate different patterns in the high enjoyment reports (eg, one wave was wave 1 only, or wave 2 only or wave 3 only; two waves were waves 1 and 2, waves 2 and 3, or waves 1 and 3), and included deaths that occurred during the assessment of enjoyment of life (results available on request). Thirdly, we repeated the analyses excluding deaths that occurred within two years of the third assessment of enjoyment of life (deaths before 2008) as a check for reverse causality. Finally, to exclude the possibility of selection bias, we repeated the main analyses by including deaths that occurred between 2002 and 2006. All analyses were carried out with Stata version 14.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
We found that 2264 (24%) participants reported no high levels of enjoyment of life on any occasion, with 1833 (20%) having one, 2063 (22%) having two, and 3205 (34%) having three reports of high enjoyment. The number of reports of high enjoyment of life was greater in women, and in participants who were married or cohabiting, well educated, wealthier, younger, and currently employed (table 1). There was no association with white European ethnicity, although the proportion of non-white participants in ELSA is small. Baseline health profiles were more favourable in those who reported more sustained enjoyment of life, with better self-rated health; less limiting longstanding illness; fewer diagnoses of coronary heart disease, diabetes, arthritis, stroke, or chronic lung disease; and less impaired mobility and impaired activities of daily living. We also found associations with a history of depressive illness and current depressive symptoms.
Table 1.
Factors associated with duration of enjoyment of life between 2002 and 2006, in the English Longitudinal Study of Ageing cohort. Data are No (%) of participants unless stated otherwise
| No of reports of high enjoyment of life between 2002 and 2006 per participant | P | ||||
|---|---|---|---|---|---|
| None (n=2264) | One (n=1833) |
Two (n=2063) |
Three (n=3205) |
||
| Sex: | |||||
| Men | 1089 (48.1) | 876 (47.8) | 906 (43.9) | 1314 (41.0) | <0.001 |
| Women | 1175 (51.9) | 957 (52.2) | 1157 (56.1) | 1891 (59.0) | |
| Age (years): | |||||
| 50-59 | 1071 (47.3) | 779 (42.5) | 838 (40.6) | 1449 (45.2) | <0.001 |
| 60-69 | 657 (29.0) | 557 (30.4) | 666 (32.3) | 1006 (31.4) | |
| 70-79 | 401 (17.7) | 365 (19.9) | 411 (19.9) | 574 (17.9) | |
| ≥80 | 136 (6.0) | 130 (7.1) | 149 (7.2) | 176 (5.5) | |
| Ethnicity: | |||||
| Non-white ethnicity | 68 (3.0) | 57 (3.1) | 39 (1.9) | 51 (1.6) | <0.001 |
| White European | 2196 (97.0) | 1776 (96.9) | 2024 (98.1) | 3154 (98.4) | |
| Cohabiting with a partner | 1426 (63.0) | 1290 (70.4) | 1525 (73.9) | 2497 (77.9) | <0.001 |
| Education: | |||||
| Lower | 457 (20.2) | 370 (20.2) | 450 (21.8) | 923 (28.8) | <0.001 |
| Intermediate | 799 (35.3) | 691(37.7) | 757 (36.7) | 1228 (38.3) | |
| Higher | 1010 (44.6) | 772 (42.1) | 858 (41.6) | 1054 (32.9) | |
| Wealth: | |||||
| Group 1 (richest) | 337 (14.9) | 328 (17.9) | 462 (22.4) | 926 (28.9) | <0.001 |
| Group 2 | 444 (19.6) | 367 (20.0) | 431 (20.9) | 763 (23.8) | |
| Group 3 | 446 (19.7) | 392 (21.4) | 458 (22.2) | 641 (20.0) | |
| Group 4 | 496 (21.9) | 370 (20.2) | 411 (19.9) | 538 (16.8) | |
| Group 5 (poorest) | 541 (23.9) | 378 (20.6) | 301 (14.6) | 337 (10.5) | |
| Employment: | |||||
| Paid employment | 722 (31.9) | 616 (33.6) | 706 (34.2) | 1231 (38.4) | <0.001 |
| Not in paid employment | 1544 (68.2) | 1219 (66.5) | 1360 (65.9) | 1974 (61.6) | |
| Self-rated health: fair or poor | 992 (43.8) | 599 (32.7) | 522 (25.3) | 497 (15.5) | <0.001 |
| Limiting longstanding illness | 1026 (45.3) | 669(36.5) | 625 (30.3) | 679 (21.2) | <0.001 |
| Coronary heart disease | 308 (13.6) | 229 (12.5) | 235 (11.4) | 266 (8.3) | <0.001 |
| Cancer | 125 (5.5) | 101 (5.5) | 113 (5.5) | 176 (5.5) | <0.980 |
| Diabetes | 192 (8.5) | 136 (7.4) | 138 (6.7) | 151 (4.7) | <0.001 |
| Arthritis | 781 (34.5) | 566 (30.9) | 569 (27.6) | 750 (23.4) | <0.001 |
| Stroke | 113 (5.0) | 64 (3.5) | 66 (3.2) | 64 (2.0) | <0.001 |
| Chronic lung disease | 324 (14.3) | 224 (12.2) | 227 (11.0) | 327 (10.2) | <0.001 |
| Impaired mobility | 1519 (67.1) | 1125 (61.4) | 1089 (52.8) | 1445 (45.1) | <0.001 |
| One or more impaired activities of daily living | 602 (26.6) | 401 (21.9) | 320 (15.5) | 359 (11.2) | <0.001 |
| History of depressive illness | 249 (11.0) | 114 (6.2) | 83 (4.0) | 80 (2.5) | <0.001 |
| Elevated depressive symptoms | 686 (30.3) | 326 (17.8) | 235 (11.4) | 160 (5.0) | <0.001 |
Results based on 10 imputed datasets.
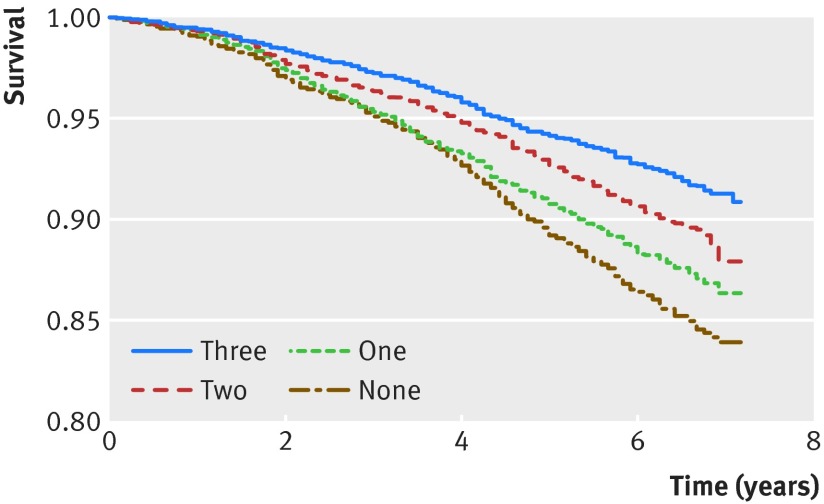
There were 1310 deaths over the average 6.5 year follow-up period, and the proportion people who died was 30% in those with no reports of high enjoyment of life, 23% in those with one report, 22% in those with two reports, and 25% in those with three reports. Cox regression confirmed that the number of reports of high enjoyment of life showed a graded inverse association with mortality (table 2). Compared with no reports of high enjoyment, the hazard ratio adjusted for age and sex was 0.87 (95% confidence interval 0.73 to 1.03) for one report, 0.73 (0.62 to 0.87) for two, and 0.60 (0.51 to 0.70) for three reports. The hazard ratio for every unit increase in reported enjoyment of life was 0.84 (0.80 to 0.89). These associations were somewhat attenuated with adjustment for covariates, particularly pre-existing health issues (model 3). Nevertheless, in the final model including all covariates, the adjusted hazard ratio was 0.83 (0.70 to 0.99) for two reports of enjoyment and 0.76 (0.64 to 0.89) for three reports, and the hazard ratio for every additional report of high enjoyment of life was 0.91 (0.86 to 0.96). Additional variables that were independently associated with all cause mortality in the fully adjusted model included older age, male sex, lower wealth, not being in paid employment, poorer self-rated health, a baseline diagnosis of coronary heart disease, cancer, chronic lung disease, and impaired activities of daily living. Figure 1 shows the Kaplan-Meier survival curves for all cause mortality.
Table 2.
Sustained enjoyment of life and up to seven year mortality in the English Longitudinal Study of Ageing cohort (n=9365)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| All cause mortality (No (%) of participants) | 400 (31) | 298 (23) | 283 (22) | 329 (25) | — |
| Covariates (hazard ratio (95% CI): | |||||
| Model 1 (age, sex) | 1 (reference) | 0.87 (0.73 to 1.03) | 0.73 (0.62 to 0.87) | 0.60 (0.51 to 0.70) | 0.84 (0.80 to 0.89) |
| Model 1 plus baseline demographic factors* (model 2) | 1 (reference) | 0.88 (0.74 to 1.05) | 0.76 (0.64 to 0.90) | 0.64 (0.55 to 0.75) | 0.86 (0.82 to 0.91) |
| Model 1 plus baseline health indicators† (model 3) | 1 (reference) | 0.93 (0.78 to 1.11) | 0.83 (0.70 to 0.99) | 0.75 (0.64 to 0.87) | 0.91 (0.86 to 0.95) |
| Model 1 plus baseline depression‡ (model 4) | 1 (reference) | 0.89 (0.75 to 1.06) | 0.76 (0.64 to 0.91) | 0.63 (0.54 to 0.74) | 0.86 (0.82 to 0.90) |
| Fully adjusted (model 5) | 1 (reference) | 0.93 (0.78 to 1.12) | 0.83 (0.70 to 0.99) | 0.76 (0.64 to 0.89) | 0.91 (0.86 to 0.96) |
Results based on 10 imputed datasets.
*Wealth, education, ethnicity, marital status, and employment.
†Fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, and impaired mobility and activities of daily living.
‡Depressive illness and current symptoms of depression.
Fig 1 Kaplan-Meier survival curve for all cause mortality according to the number of reports (none to three) on which participants in the English Longitudinal Study of Ageing cohort reported higher enjoyment of life (n=9365). Horizontal axis=time in years from the final assessment of enjoyment in 2006
There were 410 deaths attributed to cardiovascular disease, and 905 non-cardiovascular deaths. The results for non-cardiovascular deaths were similar to those for all cause mortality (table 3), with a fully adjusted hazard ratio of 0.80 (95% confidence interval 0.74 to 0.86) for every additional report of high enjoyment of life. The pattern of results was weaker for cardiovascular deaths, possibly because of the reduced power in this analysis (table 4).
Table 3.
Sustained enjoyment of life and up to seven year mortality, excluding cardiovascular deaths in the English Longitudinal Study of Ageing cohort (n=9365)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| Excluding cardiovascular deaths (No (%)) | 277 (31) | 204 (23) | 196 (22) | 228 (25) | — |
| Covariates (hazard ratio (95% CI): | |||||
| Model 1 (age, sex) | 1 (reference) | 0.83 (0.67 to 1.02) | 0.71 (0.57 to 0.89) | 0.59 (0.49 to 0.72) | 0.84 (0.79 to 0.90) |
| Model 1 plus baseline demographic factors* (model 2) | 1 (reference) | 0.85 (0.69 to 1.05) | 0.74 (0.59 to 0.92) | 0.64 (0.53 to 0.77) | 0.86 (0.81 to 0.92) |
| Model 1 plus baseline health indicators† (model 3) | 1 (reference) | 0.87 (0.70 to 1.07) | 0.78 (0.62 to 0.98) | 0.70 (0.58 to 0.85) | 0.89 (0.83 to 0.95) |
| Model 1 plus baseline depression‡ (model 4) | 1 (reference) | 0.85 (0.68 to 1.05) | 0.74 (0.59 to 0.93) | 0.63 (0.52 to 0.76) | 0.86 (0.80 to 0.91) |
| Fully adjusted (model 5) | 1 (reference) | 0.88 (0.71 to 1.09) | 0.79 (0.63 to 1.00) | 0.72 (0.59 to 0.87) | 0.80 (0.74 to 0.86) |
Results based on 10 imputed datasets.
*Wealth, education, ethnicity, marital status, and employment.
†Fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, and impaired mobility and activities of daily living.
‡Depressive illness and current symptoms of depression.
Table 4.
Sustained enjoyment of life and cardiovascular death in the English Longitudinal Study of Ageing cohort (n=9365)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| Cardiovascular deaths (No (%)) | 116 (28) | 98 (24) | 93 (23) | 103 (25) | — |
| Covariates (hazard ratio (95% CI)): | |||||
| Age, sex | 1 (reference) | 0.95 (0.69 to 1.29) | 0.80 (0.58 to 1.10) | 0.62 (0.46 to 0.84) | 0.86 (0.78 to 0.94) |
| Fully adjusted* | 1 (reference) | 1.02 (0.74 to 1.40) | 0.92 (0.76 to 1.30) | 0.83 (0.61 to 1.14) | 0.94 (0.85 to 1.04) |
Results based on 10 imputed datasets.
*Wealth, education, ethnicity, marital status, employment, fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, impaired mobility and activities of daily living, depressive illness, and current symptoms of depression.
The first sensitivity analysis limited the sample to participants with complete data (n=5262) instead of using the imputed datasets. The results led to similar conclusions as the main analysis, with a fully adjusted hazard ratio of 0.90 (95% confidence interval 0.83 to 0.96) for every additional report of high enjoyment (table 5). The second sensitivity analysis explored whether different patterns of enjoyment over time were important in relation to mortality. Hazard ratios were comparable whether high enjoyment was reported on consecutive waves (eg, waves 1 and 2, or waves 2 and 3) or non-consecutive waves (eg, waves 1 and 3), and whether a single report of high enjoyment occurred on waves 1, 2, or 3 (results available on request).
Table 5.
Sustained enjoyment of life and up to seven year mortality in the English Longitudinal Study of Ageing cohort (complete case, n=5262)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| All cause mortality (No (%)) | 179 (30) | 125 (21) | 127 (21) | 172 (29) | — |
| Covariates (hazard ratio (95% CI)): | |||||
| Model 1 (age, sex) | 1 (reference) | 0.83 (0.66 to 1.04) | 0.69 (0.55 to 0.87) | 0.57 (0.46 to 0.70) | 0.83 (0.78 to 0.89) |
| Model 1 plus baseline demographic factors* (model 2) | 1 (reference) | 0.84 (0.67 to 1.06) | 0.73 (0.58 to 0.91) | 0.61 (0.49 to 0.75) | 0.85 (0.79 to 0.91) |
| Model 1 plus baseline health indicators† (model 3) | 1 (reference) | 0.91 (0.72 to 1.14) | 0.79 (0.63 to 1.00) | 0.72 (0.58 to 0.90) | 0.90 (0.83 to 0.96) |
| Model 1 plus baseline depression‡ (model 4) | 1 (reference) | 0.84 (0.66 to 1.05) | 0.70 (0.56 to 0.88) | 0.58 (0.47 to 0.72) | 0.83 (0.78 to 0.89) |
| Fully adjusted (model 5) | 1 (reference) | 0.90 (0.71 to 1.14) | 0.80 (0.63 to 1.01) | 0.72 (0.58 to 0.90) | 0.90 (0.83 to 0.96) |
*Wealth, education, ethnicity, marital status, and employment.
†Fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, and impaired mobility and activities of daily living.
‡Depressive illness and current symptoms of depression.
Thirdly, we excluded deaths that occurred within two years of the third and final assessment of enjoyment in 2006, leaving 1179 deaths between 2008 and 2013. Compared with individuals who experienced no episodes of high enjoyment of life, the fully adjusted hazard ratio was 0.72 (95% confidence interval 0.61 to 0.86) among those experiencing three episodes, with a hazard of 0.90 (0.85 to 0.95) for every additional report of enjoyment (table 6). The final sensitivity analysis included 2146 deaths that occurred between 2002 and 2006 (table 7). The association with sustained enjoyment of life was stronger than in the main analyses, with a hazard ratio of 0.73 (95% confidence interval 0.70 to 0.76) for every additional report of high enjoyment.
Table 6.
Sustained enjoyment of life up to 2006 and mortality from 2008 to 2013 in the English Longitudinal Study of Ageing cohort (n=9234)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| All cause mortality (No (%)) | 355 (30%) | 279 (24%) | 262 (22%) | 283 (24%) | — |
| Covariates (hazard ratio (95% CI)): | |||||
| Age, sex | 1 (reference) | 0.87 (0.72 to 1.04) | 0.73 (0.62 to 0.88) | 0.58 (0.48 to 0.70) | 0.83 (0.78 to 0.88) |
| Fully adjusted1 | 1 (reference) | 0.94 (0.78 to 1.13) | 0.84 (0.70 to 1.01) | 0.72 (0.61 to 0.86) | 0.90 (0.85 to 0.95) |
Results based on 10 imputed datasets.
*Wealth, education, ethnicity, marital status, employment, fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, impaired mobility and activities of daily living, depressive illness, and current symptoms of depression.
Table 7.
Sustained enjoyment of life and up to 11 year mortality (between 2002 and 2013) in the English Longitudinal Study of Ageing cohort (n=10 196)
| No of reports of high enjoyment of life between 2002 and 2006 per participant | |||||
|---|---|---|---|---|---|
| None | One | Two | Three | Per one report increase | |
| All cause mortality (No (%)) | 852 (40%) | 597 (28%) | 373 (17%) | 324 (15%) | — |
| Covariates (hazard ratio (95% CI)): | |||||
| Model 1 (age, sex) | 1 (reference) | 0.89 (0.79 to 1.00) | 0.48 (0.42 to 0.55) | 0.31 (0.27 to 0.36) | 0.68 (0.65 to 0.71) |
| Model 1 plus baseline demographic factors* (model 2) | 1 (reference) | 0.90 (0.80 to 1.02) | 0.51 (0.44 to 0.58) | 0.34 (0.29 to 0.39) | 0.70 (0.67 to 0.73) |
| Model 1 plus baseline health indicators† (model 3) | 1 (reference) | 0.94 (0.84 to 1.07) | 0.54 (0.46 to 0.63) | 0.39 (0.34 to 0.44) | 0.73 (0.70 to 0.76) |
| Model 1 plus baseline depression‡ (model 4) | 1 (reference) | 0.90 (0.80 to 1.02) | 0.50 (0.45 to 0.61) | 0.32 (0.28 to 0.37) | 0.69 (0.66 to 0.72) |
| Fully adjusted (model 5) | 1 (reference) | 0.94 (0.83 to 1.06) | 0.54 (0.47 to 0.63) | 0.39 (0.34 to 0.45) | 0.73 (0.70 to 0.76) |
Results based on 10 imputed datasets.
*Wealth, education, ethnicity, marital status, and employment.
†Fair/poor self-rated health, limiting longstanding illness, coronary heart disease, cancer, stroke, chronic lung disease, diabetes, arthritis, and impaired mobility and activities of daily living.
‡Depressive illness and current symptoms of depression.
Discussion
Our results indicate that the maintenance of positive wellbeing over a four year period is systematically related to subsequent mortality. A graded effect was apparent, with progressively higher mortality among people with fewer reports of high enjoyment. In the fully adjusted model, the hazard was reduced by 17% among people giving two reports of high enjoyment of life, and by 24% in those giving three reports. Findings for all cause mortality were replicated in separate analyses of deaths from causes other than cardiovascular disease, after adjusting for multiple demographic, health, and emotional factors. Associations also persisted after deaths within two years of the last measure of enjoyment of life were excluded, arguing against reverse causality or the effect of terminal decline in wellbeing.17
Strengths and limitations
This study advances understanding of the role of subjective wellbeing in health in three ways. Firstly, it shows that duration of exposure to positive emotional states is important. Previous research has documented associations between intensity of positive wellbeing at a single measurement point and survival, but not how often wellbeing is experienced, and studies with repeated assessments of positive wellbeing are rare.18 Our observation that multiple reports of high enjoyment of life show stronger associations with mortality than a single episode adds to the plausibility that subjective wellbeing might causally influence health outcomes. Single reports of enjoyment of life could be affected by current circumstances or fleeting experiences, while persistent subjective wellbeing might influence longer term determinants of health.
Secondly, we took account of a wide range of potential confounders in these analyses. Previous studies have included controls for demographics and baseline prevalence of serious illness,3 4 10 19 but not disability or mobility impairment. Impaired mobility is an independent predictor of mortality,20 and is associated with reduced enjoyment of life.14 We also measured self-rated health and limiting longstanding illness as indicators of less tangible health problems that might confound associations between positive wellbeing and mortality, and assessments of depressive symptoms to account for the presence of negative affective states. An analysis of the Million Women Study showed no association between a simple four point rating of frequency of happiness and survival, due in large part to a substantial overlap of the happiness ratings with self-rated health.11 The number of reports of enjoyment was also associated with good self-rated health in the present study (table 1). Nevertheless, our observation that multiple reports of high enjoyment remained independent predictors of mortality when this and other factors had been included in the analytical models increases our confidence that associations are robust.
Thirdly, we have documented associations between sustained wellbeing and death from non-cardiovascular causes as well as all cause mortality. Previous work has documented links between lower subjective wellbeing and cardiovascular disease incidence and longer survival.4 21 22 However, cardiovascular disease accounted for only around a third of deaths in this study, limiting statistical power to detect associations. The findings for deaths from non-cardiovascular causes suggest that subjective wellbeing has a more general association with survival.
This was an observational study, so we are not able to interpret the associations between enjoyment of life and survival as causal. Although we controlled for a wide range of potential confounders, other unmeasured factors could be important. Our assessment of initial health was not complete, even though we included general measures such as self-rated health as well as serious diagnosed conditions. A substantial proportion of participants in ELSA did not complete all three assessments of enjoyment of life, either because they died during the four year measurement period or because they dropped out of the study temporarily or permanently. However, analyses of participants who completed all assessments showed results comparable to the multiply imputed datasets, indicating that attrition during the measurement period does not explain our findings.
Subjective wellbeing has many facets, including hedonic wellbeing (feelings of happiness and joy), evaluative wellbeing (life satisfaction), and eudemonic wellbeing (judgments about meaning and purpose in life).23 Our measure of enjoyment of life includes components of hedonic wellbeing, social engagement, and vitality, all of which might be important for sustained health.22 A limitation of this analysis was that we only assessed enjoyment of life every two years, and do not know whether it fluctuated between measurement points.18 We also do not know about the pattern of enjoyment of participants’ lives before they enrolled in the study. The proportion of ethnic minority participants in ELSA was very small, and our results might not generalise to other cultures. Baseline health status was measured by self-report, but this has been shown to be quite comparable with physician examination in studies of adults of comparable age.24 25 In defining covariates, we relied on baseline data rather than data from all three waves, because imputation of covariates at subsequent waves would increase uncertainty in multivariable adjusted effect estimates.
Mechanisms and implications
It is possible that the pattern of deaths results from reverse causality. Serious illness and terminal decline undoubtedly impair enjoyment of life, which could lead to an association between lack of enjoyment and mortality.26 We therefore carried out a sensitivity analysis restricted to deaths at least two years after the last measurement point, reasoning that if reverse causality was responsible, the mortality effect should be attenuated. The fact that the associations in this analysis were similar to the main findings argues against reverse causality as a primary explanation.
If the findings do reflect causal processes, two broad sets of factors might be involved. Firstly, enjoyment of life might exert an influence through associations with healthy lifestyle. Physical activity, not smoking, and healthy diet have been related to positive wellbeing,27 28 29 while healthcare and self-care behaviours (such as screening uptake, appropriate help seeking, and adherence to medical advice) might also be relevant.30 Sustained enjoyment of life over many years could be linked with healthier behavioural choices, promoting longevity.
Secondly, there could be direct biological correlates of positive wellbeing modulated through corticolimbic pathways that contribute to protective associations. Subjective wellbeing has been correlated with low concentrations of cortisol in everyday life,31 with low levels of inflammatory markers in some studies,32 and with changes in expression of genes regulating inflammation and antibody synthesis.33 Aspects of subjective wellbeing has been associated with reduced incident hypertension and cardiometabolic disease,34 35 slower decline in physical functional capacity,14 and better sleep,36 all of which might reduce risk of life threatening illness if sustained over time. These processes might contribute to a broad range of health outcomes.
Conclusions
These results add a new dimension to understanding the significance of subjective wellbeing for physical health outcomes by documenting a dose-response association with sustained wellbeing. This complements previous findings on wellbeing intensity, and demonstrating significant effects after controlling for a wide range of potential confounders. The findings highlight the need to study biological and behavioural mediators in order to establish the mechanisms through which subjective wellbeing is associated with health outcomes.
What is already known on this topic
Subjective wellbeing (feelings of enjoyment and satisfaction with life) has been associated with greater longevity in longitudinal population studies
Previous studies have measured wellbeing on a single occasion, and the importance of sustained wellbeing is not known
What this study adds
In the present study, a dose-response association was seen between sustained positive wellbeing over several years and all cause mortality
These effects remained significant after adjusting statistically not only for demographic and health status, but also adjusting for physical functional impairment and depressive symptoms
JW died before the publication of this paper.
Contributors: PZ and AS undertook the statistical analysis, and AS and JW wrote the first draft of the paper. All authors made substantial contributions to design, analysis, and interpretation of data, and contributed to drafting the article and revising it critically for important intellectual content and approved the final manuscript. AS is the guarantor.
Funding: The English Longitudinal Study of Ageing was developed by a team of researchers based at the University College London, NatCen Social Research, the Institute for Fiscal Studies, and the University of Manchester. The data were collected by NatCen Social Research. The funding is provided by the National Institute of Aging in the USA, and a consortium of UK government departments coordinated by the Economic and Social Research Council. The developers and funders of the English Longitudinal Study of Ageing and the UK Data Archive do not bear any responsibility for the analyses or interpretations presented here. AS was funded by the British Heart Foundation chair and JW by Cancer Research UK.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: support from the US National Institute for Aging and a consortium of UK government departments coordinated by the Economic and Social Research Council for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: ELSA was approved by the London Multicentre Research Ethics Committee (MREC/01/2/91), and informed consent was obtained from all participants.
Data sharing: Users registered with the Economic and Social Data Service (ESDS) have access to the ELSA datasets via www.esds.ac.uk.
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1.Boehm JK, Kubzansky LD. The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol Bull 2012;138:655-91. 10.1037/a0027448 pmid:22506752. [DOI] [PubMed] [Google Scholar]
- 2.Diener E, Chan MY. Happy people live longer: subjective well-being contributes to health and longevity. Appl Psychol Health Well-Being 2011;3:1-43 10.1111/j.1758-0854.2010.01045.x. [DOI] [Google Scholar]
- 3.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med 2008;70:741-56. 10.1097/PSY.0b013e31818105ba pmid:18725425. [DOI] [PubMed] [Google Scholar]
- 4.Boehm JK, Peterson C, Kivimaki M, Kubzansky LD. Heart health when life is satisfying: evidence from the Whitehall II cohort study. Eur Heart J 2011;32:2672-7. 10.1093/eurheartj/ehr203 pmid:21727096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shirai K, Iso H, Ohira T, et al. Japan Public Health Center-Based Study Group. Perceived level of life enjoyment and risks of cardiovascular disease incidence and mortality: the Japan public health center-based study. Circulation 2009;120:956-63. 10.1161/CIRCULATIONAHA.108.834176 pmid:19720937. [DOI] [PubMed] [Google Scholar]
- 6.Gana K, Broc G, Saada Y, Amieva H, Quintard B. Subjective wellbeing and longevity: Findings from a 22-year cohort study. J Psychosom Res 2016;85:28-34. 10.1016/j.jpsychores.2016.04.004 pmid:27212667. [DOI] [PubMed] [Google Scholar]
- 7.Krijthe BP, Walter S, Newson RS, Hofman A, Hunink MG, Tiemeier H. Is positive affect associated with survival? A population-based study of elderly persons. Am J Epidemiol 2011;173:1298-307. 10.1093/aje/kwr012 pmid:21454828. [DOI] [PubMed] [Google Scholar]
- 8.Steptoe A, Wardle J. Positive affect measured using ecological momentary assessment and survival in older men and women. Proc Natl Acad Sci U S A 2011;108:18244-8. 10.1073/pnas.1110892108 pmid:22042845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawrence EM, Rogers RG, Wadsworth T. Happiness and longevity in the United States. Soc Sci Med 2015;145:115-9. 10.1016/j.socscimed.2015.09.020 pmid:26421947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tilvis RS, Laitala V, Routasalo P, Strandberg TE, Pitkala KH. Positive life orientation predicts good survival prognosis in old age. Arch Gerontol Geriatr 2012;55:133-7. 10.1016/j.archger.2011.06.030 pmid:21764146. [DOI] [PubMed] [Google Scholar]
- 11.Liu B, Floud S, Pirie K, Green J, Peto R, Beral V. Million Women Study Collaborators. Does happiness itself directly affect mortality? The prospective UK Million Women Study. Lancet 2016;387:874-81. 10.1016/S0140-6736(15)01087-9 pmid:26684609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steptoe A, Wardle J. Enjoying life and living longer. Arch Intern Med 2012;172:273-5. 10.1001/archinternmed.2011.1028 pmid:22332162. [DOI] [PubMed] [Google Scholar]
- 13.Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol 2013;42:1640-8. 10.1093/ije/dys168 pmid:23143611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steptoe A, de Oliveira C, Demakakos P, Zaninotto P. Enjoyment of life and declining physical function at older ages: a longitudinal cohort study. CMAJ 2014;186:E150-6. 10.1503/cmaj.131155 pmid:24446463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med 2006;21:267-75. 10.1111/j.1525-1497.2005.00291.x pmid:16336622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Demakakos P, Pierce MB, Hardy R. Depressive symptoms and risk of type 2 diabetes in a national sample of middle-aged and older adults: the English longitudinal study of aging. Diabetes Care 2010;33:792-7. 10.2337/dc09-1663 pmid:20086253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerstorf D, Ram N, Estabrook R, Schupp J, Wagner GG, Lindenberger U. Life satisfaction shows terminal decline in old age: longitudinal evidence from the German Socio-Economic Panel Study (SOEP). Dev Psychol 2008;44:1148-59. 10.1037/0012-1649.44.4.1148 pmid:18605841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boehm JK, Winning A, Segerstrom S, Kubzansky LD. Variability modifies life satisfaction’s association with mortality risk in older Adults. Psychol Sci 2015;26:1063-70. 10.1177/0956797615581491 pmid:26048888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koopmans TA, Geleijnse JM, Zitman FG, et al. Effects of happiness on all-cause mortality during 15 years of follow-up: The Arnhem Elderly Study. J Happiness Stud 2010;11:113-24 10.1007/s10902-008-9127-0. [DOI] [Google Scholar]
- 20.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011;305:50-8. 10.1001/jama.2010.1923 pmid:21205966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J 2010;31:1065-70. 10.1093/eurheartj/ehp603 pmid:20164244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry 2007;64:1393-401. 10.1001/archpsyc.64.12.1393 pmid:18056547. [DOI] [PubMed] [Google Scholar]
- 23.Stone AA, Mackie C, eds. Subjective well-being: measuring happiness, suffering, and other dimensions of experience.National Academies Press, 2013. [PubMed] [Google Scholar]
- 24.Baumeister H, Kriston L, Bengel J, Härter M. High agreement of self-report and physician-diagnosed somatic conditions yields limited bias in examining mental-physical comorbidity. J Clin Epidemiol 2010;63:558-65. 10.1016/j.jclinepi.2009.08.009 pmid:19959329. [DOI] [PubMed] [Google Scholar]
- 25.Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol 1996;49:1407-17. 10.1016/S0895-4356(96)00274-0 pmid:8970491. [DOI] [PubMed] [Google Scholar]
- 26.Gerstorf D, Ram N, Röcke C, Lindenberger U, Smith J. Decline in life satisfaction in old age: longitudinal evidence for links to distance-to-death. Psychol Aging 2008;23:154-68. 10.1037/0882-7974.23.1.154 pmid:18361663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mujcic R, J Oswald A. Evolution of well-being and happiness after increases in consumption of fruit and vegetables. Am J Public Health 2016;106:1504-10. 10.2105/AJPH.2016.303260 pmid:27400354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Black SV, Cooper R, Martin KR, Brage S, Kuh D, Stafford M. Physical activity and mental well-being in a cohort aged 60-64 years. Am J Prev Med 2015;49:172-80. 10.1016/j.amepre.2015.03.009 pmid:26070782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis [correction in: BMJ 2014;348:g2216]. BMJ 2014;348:g1151 10.1136/bmj.g1151 pmid:24524926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A 2014;111:16331-6. 10.1073/pnas.1414826111 pmid:25368165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc Natl Acad Sci U S A 2005;102:6508-12. 10.1073/pnas.0409174102 pmid:15840727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol 2007;26:305-13. 10.1037/0278-6133.26.3.305 pmid:17500617. [DOI] [PubMed] [Google Scholar]
- 33.Fredrickson BL, Grewen KM, Coffey KA, et al. A functional genomic perspective on human well-being. Proc Natl Acad Sci U S A 2013;110:13684-9. 10.1073/pnas.1305419110 pmid:23898182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boehm JK, Chen Y, Williams DR, Ryff CD, Kubzansky LD. Subjective well-being and cardiometabolic health: An 8-11year study of midlife adults. J Psychosom Res 2016;85:1-8. 10.1016/j.jpsychores.2016.03.018 pmid:27212662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trudel-Fitzgerald C, Boehm JK, Kivimaki M, Kubzansky LD. Taking the tension out of hypertension: a prospective study of psychological well being and hypertension. J Hypertens 2014;32:1222-8. 10.1097/HJH.0000000000000175 pmid:24786293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steptoe A, O’Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res 2008;64:409-15. 10.1016/j.jpsychores.2007.11.008 pmid:18374740. [DOI] [PubMed] [Google Scholar]