Abstract
AIM
To investigate the etiology, diagnosis, management and outcome of epiphora referrals to an oculoplastic practice.
METHODS
Retrospective chart review of patients referred for epiphora to an oculoplastic clinic between 2005 and 2009. Patient demographics, past history, ophthalmic examination, treatment and outcome were analyzed.
RESULTS
There were 237 subjects with a primary complaint of epiphora. They included 130 (55%) females and 107 (45%) males with an average age of 55.9±25.9y. The most common cause of epiphora was lacrimal obstruction (46%); followed by multifactorial epiphora (22%), reflex tearing (22%) and eyelid malposition (11%). Differences in prevalence of etiology were noted in terms of age and gender distribution. Of the 182 (77%) patients who returned for follow up, 41 (23%) reported a complete resolution and 102 (56%) reported a significant improvement in their symptoms.
CONCLUSION
Epiphora is a common condition with many causes. A thorough history and examination are required to provide the appropriate treatment tailored to the underlying cause.
Keywords: epiphora, etiology, lacrimal disease, dry eye
INTRODUCTION
Epiphora or tearing is the presence of a watering eye, which is a common complaint for referrals to oculoplastics clinics for evaluation. The etiology of tearing can be divided into two categories: reflex tearing and reduced tear outflow[1]. Reflex tearing is usually secondary to dry eye, inflammation, allergy or other ocular surface disorders, whereas primary hypersecretion of the lacrimal glands is rare. Reduced tear outflow is due to eyelid malposition, tear pump dysfunction caused by eyelid laxity, or obstruction at any portion of the nasaolacrimal drainage system. Nasolacrimal duct obstruction (NLDO) may be congenital or acquired. Many cases evaluated for epiphora are found to have a combination of causes. In such cases, a multipronged treatment is necessary to address the patients' symptoms and assessment of treatment response may be needed to help confirm the working diagnosis.
Dry eye is a multifactorial inflammatory disease affecting the ocular surface. A recent investigation showed that dry eye comprised a significant proportion of patients (40%) referred for tearing[2]. Tearing improved in most cases after using topical lubricants. This highlights the role of dry eye in the etiology of tearing and demonstrates that tearing is not a simple surgical problem. Compensatory reflex hypersecretion due to evaporative loss is thought to be responsible for epiphora. In our practice, we found that many patients with dry eye symptoms referred for tearing did not have a tear volume deficiency but a significant number did have tear film instability. According to the Dry Eye Workshop report, tear film instability is one of the core underlying mechanisms of dry eye[3]. In a previous study[4], we found that 206 of 1000 (20.6%) patients with chronic epiphora had meibomitis and tear film instability as a main cause of tearing. Medical treatment for meibomitis improved tearing symptoms in a majority of those patients.
Few studies have investigated the prevalence of epiphora by etiology, and management with long-term outcome follow-up in an oculoplastic practice. The clinical characteristics of epiphora referrals, including age distribution and gender differences are still not well understood. We performed a retrospective chart analysis of patients evaluated for epiphora with the aim of reporting the clinical characteristics of patients with epiphora and evaluating their response to treatment.
SUBJECTS AND METHODS
Subjects
We performed a retrospective analysis of patients referred for epiphora to our oculoplastics clinic between January 2005 and December 2009. Additional data were obtained through 2011 to ensure adequate follow up time. Subjects were identified through an electronic patient database, using a key word search for “epiphora” or “tearing” for their initial clinic visit. Informed consent was obtained from all subjects and the study was conducted in accordance to the Declaration of Helsinki.
Methods
Demographics, medical and ocular history were collected for all subjects. Patients were questioned regarding the duration and frequency of tearing, symptoms related to dry eye (including burning, itching, scratchiness and blurry vision), and symptoms related to lacrimal obstruction (including epiphora, discharge and crusting). Slit-lamp examination findings included tear film appearance, lid margin telangiectasia, frothy discharge in the tear meniscus, pouting or plugging of meibomian orifices, expression of meibomian secretions, eyelid position, trichiasis, medial canthal anatomy, punctal position, and presence of dacryocystitis. Other tests included Schirmer test, tear break-up time (TBUT), and irrigation to assess lacrimal system patency. Patients with previous lacrimal or eyelid surgery, facial nerve palsy or who already received treatment for symptom-related conditions prior to referral were excluded from the study.
We classified the most common cause of tearing based on pathophysiology. Categories included the following: 1) eyelid malposition (e.g. entropion, ectropion and eyelid laxity); 2) congenital NLDO; 3) acquired upper lacrimal obstruction (e.g. punctal stenosis, canalicular obstruction); 4) acquired lower lacrimal obstruction (e.g. dacryocystitis, NLDO); 5) reflex tearing (e.g. dry eye, meibomitis, blepharitis); and 6) multifactorial epiphora: more than one causative factor (e.g. eyelid laxity and punctal stenosis).
A preliminary diagnosis was made at the initial evaluation but was confirmed at follow-up visits for many subjects. For example, “eyelid malposition” was confirmed as a cause of epiphora if symptoms improved after eyelid malposition surgery; “reflex tearing” was confirmed if symptoms improved after dry eye treatment; and “multifactorial” epiphora was suspected if only partial improvement of tearing resulted after eyelid surgery in a patient where lid malposition was the main working diagnosis and a secondary working diagnosis was determined after intervention or diagnosed initially but not directly treated before surgery.
Dry eye treatment included warm soaks, lid scrubs, artificial tears and flaxseed oil supplements four times daily. Patients diagnosed with lacrimal obstruction underwent surgery including balloon dacryoplasty, dacryocystorhinostomy (DCR), and conjunctivodacryocystorhinostomy (CDCR). Patients with eyelid malposition also underwent surgical correction of the underlying lid malposition (e.g. ectropion repair, medial spindle procedure for punctal ectropion).
Statistical Analysis
Statistical analysis was performed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics were presented as raw numbers and percentage for nominal variables and as mean±standard deviation for continuous data. Differences between groups were examined using Pearson's Chi-squared test for categorical factors. A P value <0.05 was considered statistically significant.
RESULTS
Demographics and Diagnoses
A total of 237 subjects with a primary complaint of epiphora were included. The mean age was 55.9±25.9y (range 1-93y), and 55% (n=130) were female. Among them, 49% (n=117) of cases had bilateral epiphora, and 51% (n=120) had unilateral epiphora. The number of patients aged 60 years or older was 131, accounting for 55% of patients. Demographics and clinical characteristics of the patients are presented in Table 1.
Table 1. Demographics and clinical characteristics of 237 patients.
| Etiology | No. | Age (a) | Sex |
Laterality |
Duration of epiphora (mo) | Follow-up (mo) | ||
| F | M | Unilateral | Bilateral | |||||
| Eyelid malposition | 26 (11) | 64.5±28.6 | 12 (46) | 14 (54) | 13 (50) | 13 (50) | 4.4±2.6 | 3.1±2.4 |
| Reflex tearing | 51 (22) | 61.2±19.2 | 28 (55) | 23 (45) | 10 (20) | 41 (80) | 6.8±6.2 | 7.4±8.3 |
| Lacrimal obstruction | 108 (46) | 45.2±28.1 | 70 (65) | 38 (35) | 81 (75) | 27 (25) | 17.9±18.5 | 9.5±13.0 |
| Congenital NLDO | 17 (7) | 3.5±3.9 | 6 (35) | 11 (65) | 12 (71) | 5 (29) | 14.9±15.2 | 3.9±3.1 |
| Upper obstruction | 26 (11) | 42.6±24.6 | 19 (73) | 7 (27) | 17 (63) | 9 (37) | 41.6±49.2 | 14.3±19.3 |
| Lower obstruction | 65 (27) | 57.1±21.8 | 45 (69) | 20 (31) | 52 (80) | 13 (20) | 18.9±18.5 | 8.5±9.6 |
| Multifactorial epiphora | 52 (22) | 69.0±14.1 | 20 (38) | 32 (62) | 16 (31) | 36 (69) | 21.2±19.4 | 3.7±3.0 |
| 2 causative factors | 40 (77) | 68.2±15.0 | 17 (43) | 23 (57) | 15 (38) | 25 (62) | 19.0±18.2 | 3.5±2.9 |
| 3 causative factors | 12 (23) | 71.5±10.3 | 3 (25) | 9 (75) | 1 (8) | 11 (92) | 24.3±21.8 | 4.4±3.6 |
| Total | 237 | 55.9±25.9 | 130 (55) | 107 (45) | 120 (51) | 117 (49) | 15.3±17.1 | 7.2±10.1 |
x±s; n (%)
The most common cause of epiphora was lacrimal obstruction, occurring in 108 of 237 (46%) patients (27% occurred in the lower lacrimal system, 11% in the upper lacrimal system, and 7% was congenital NLDO), followed by multifactorial epiphora (n=52, 22%), reflex tearing (n=51, 22%) and eyelid malposition (n=26, 11%). Although unilateral epiphora equally prevalent as bilateral epiphora in all cases of tearing (51% and 49%, respectively), unilateral epiphora was more common in cases with lacrimal obstruction than other causes, with a ratio of 3:1. Epiphora occurred bilaterally more often in cases with reflex tearing, with a ratio of 4:1 (χ2=53.51, P=0.000).
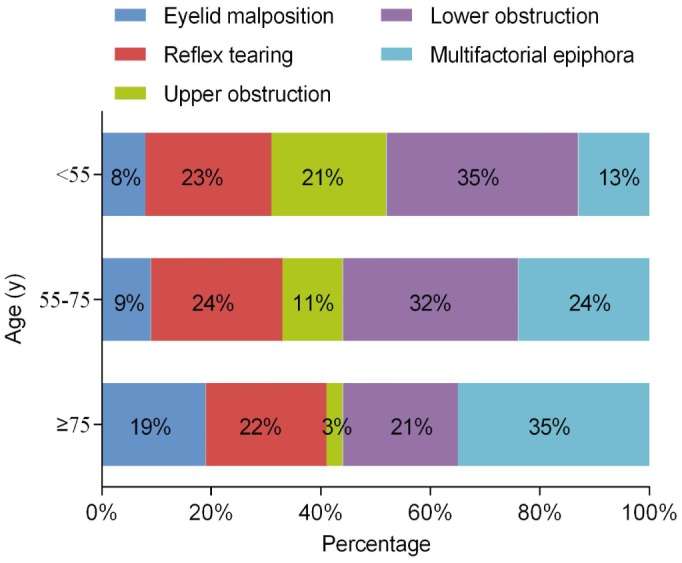
Subjects, excluding those with congenital NLDO, were divided into three groups by age distribution: <55y (n=75), 55-75y (n=75) and ≥75y (n=69). There were significant differences in etiologies of epiphora among the three age groups (χ2=23.88, P=0.002; Figure 1). Eyelid malposition was significantly more common in patients aged 75y or older compared with younger patients. The proportion of lacrimal obstruction decreased by age while that of multifactorial epiphora increased. The cases of reflex tearing did not significantly differ in different age groups.
Figure 1. Age distribution of the different etiologies of epiphora.
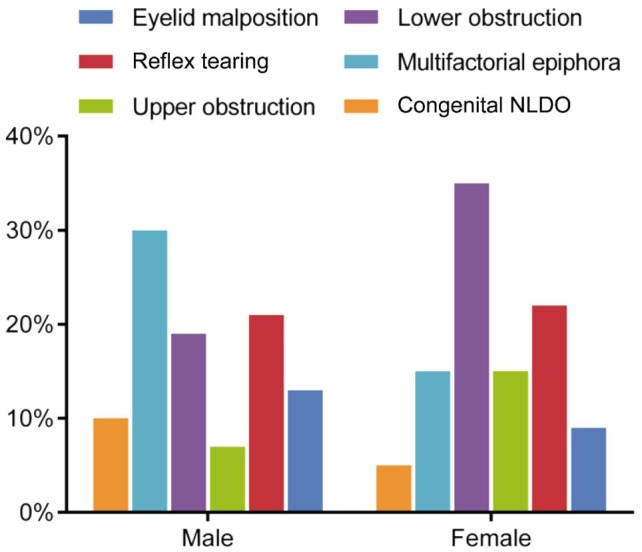
In comparing the different causes of epiphora by gender, there was a significant difference between females and males (χ2=17.98, P=0.003; Figure 2). The most common cause of epiphora was lower obstruction in females and multifactorial epiphora in males.
Figure 2. Gender distributions of the different etiologies of epiphora.
Treatment and Response
Of the 182 (77%) patients who returned for follow up, no treatment was necessary in 6 patients, whereas 52 patients required treatment for dry eye, 23 underwent eyelid surgery, 85 had lacrimal drainage system surgery, 10 underwent both eyelid and lacrimal drainage surgery, 4 required a combination of surgery and treatment of dry eye and 2 opted for observation in lieu of surgery. Forty-one patients had complete resolution of epiphora, 102 had significant improvement, 24 had slight improvement, 12 reported no change, and 3 experienced worse symptoms.
Three subjects developed dry eye after lacrimal surgery and 1 subject reported tearing due to tube irritation. In cases with Jones tube placement, 3 subjects reported that tubes were lost and 12 reported intermittent tube obstruction as a cause for tearing.
DISCUSSION
Epiphora is a common presenting complaint for almost every ophthalmologist and especially oculoplastic specialists. There is relatively little literature on the epidemiology and demographic characteristics of epiphora. This study presents new findings regarding patients with epiphora.
In our study, the mean age of patients was 56 years and about half of patients were aged 60 years or older, which indicates that the elderly patients were more inclined to have a complaint of epiphora. Elderly patients presented more often with eyelid malposition and multifactorial epiphora, whereas younger patients presented more often with punctal stenosis, canaliculi obstruction or NLDO. This finding is consistent with previously reported age distribution of tearing according to etiology[5]–[7], which showed a relatively high prevalence of eyelid malposition in the elderly population. Eyelid abnormalities are often associated with significant ocular surface morbidity (e.g. dry eye)[6]–[7]. These findings can partially explain the age distribution of the different etiologies of epiphora in our study, especially with multiple etiologies in the elderly.
Causes of epiphora between female and male were significantly different in our study-lacrimal obstruction was more common in women than men. Consistent with our findings, Viso et al[8] reported that women had a higher prevalence of punctal stenosis than men and sex was an independent predictor. In another retrospective study of 2615 patients with NLDO, females were more frequently affected than males, with a rate of 65.6%[5]. Woog[9] also reported that females comprise 73% of patients with NLDO. It has been postulated that the smaller diameter, longer lacrimal canal and inferior bony lacrimal fossa leave females more vulnerable to chronic inflammation[10], which may contribute to this observation.
We found that 75% of cases with lacrimal obstruction were unilateral. Similar to our finding, Francisco et al[11] reported that the majority of their cases presented with unilateral obstruction, with a ratio of 5:1, whereas reflex tearing and eyelid malposition often occur bilaterally.
The prevalence of lacrimal obstruction in previous clinic-based surveys was reported to range from 31.8% to 48.7%[2],[12]–[14]. In our sample, lacrimal obstruction comprised 46% of the cases and it was the most common cause of epiphora. The prevalence of dry eye varies across different studies. Mainville and Jordan[2] reported a significant proportion of patients (40%) referred for tearing had dry eye. Sibley et al[12] reported 29.2% of patients referred for dry eye had epiphora. A Canadian study showed that dry eye contributed to 22% of the all cases of epiphora[13]. Similarly, we found that the proportion of dry eye in this study was 22%. The differences in prevalence may attribute to the complexity of multifactorial epiphora.
Dry eye is a common ocular surface disorder with a complicated etiology, which can be classified into 2 major subtypes: aqueous-deficient subtype (ADDE) resulting from a decrease in lacrimal gland secretion and evaporative subtype (EDE), in which there is excessive evaporative water loss[15]. Tear film instability, together with tear hyperosmolarity, represent the two core underlying mechanisms of dry eye[3]. Tear dynamics are maintained by a complicated arrangement of tear production by the lacrimal glands, distribution by blinking, evaporation from the ocular surface and drainage through the nasolacrimal duct. Disruption of the balance of any of these factors can result in tear film instability[16]–[17]. Tear film instability leads to an increase in evaporative loss and thus stimulates the neurosensory receptors in the cornea and conjunctiva. Reflex tearing secondary to dry eye is produced by neurosensory stimulation of the lacrimal gland in an attempt to reduce the tear film osmolarity. The Schirmer test without topical anesthesia has been used to measure reflex tearing. It has been suggested that the Schirmer test may be of diagnostic value for distinguishing ADDE and EDE subtypes[18]. In our study, we found that many dry eye patients with epiphora had normal Schirmer test values. Such observations have been noted in patients with meibomian gland dysfunction. The abnormal glandular lipids may lead to increased evaporation, hyperosmolarity and instability of the tear film, increased bacterial growth on the lid margin, ocular surface inflammation, and evaporative dry eye[19].
At follow up evaluation, 23% of subjects reported a complete resolution of and 56% reported a significant improvement in their symptoms. Sibley et al[12] reported a 52% rate of significant symptom improvement or resolution over a 2-year period, highlighting the complicated and inconsistent etiology of epiphora, such as the 3 cases developing dry eye after outflow surgery in our study. Therefore, the management of epiphora should be considered as a multifactorial issue.
Potential limitations of our study include its retrospective design. In addition, data of patients who did not follow-up were based only on the initial assessment, which may potentially reflect an inaccurate diagnosis of the cause of epiphora since would could not evaluate the effect of the recommended treatment.
In conclusion, our study reports the etiology, diagnosis, management and outcomes of epiphora referrals to an oculoplastic practice. The most common cause of epiphora was lacrimal obstruction; followed by multifactorial epiphora, reflex tearing and eyelid malposition. Differences in etiology prevalence are noted with respect to age and gender distribution.
Acknowledgments
Conflicts of Interest: Shen GL, None; Ng JD, None; Ma XP, None.
REFERENCES
- 1.Blackmore KJ, Ainsworth G, Robson AK. Epiphora: an evidence based approach to the 12 minute consultation. Clin Otolaryngol. 2010;35(3):210–214. doi: 10.1111/j.1749-4486.2010.02138.x. [DOI] [PubMed] [Google Scholar]
- 2.Mainville N, Jordan DR. Etiology of tearing: a retrospective analysis of referrals to a tertiary care oculoplastics practice. Ophthal Plast Reconstr Surg. 2011;27(3):155–157. doi: 10.1097/IOP.0b013e3181ef728d. [DOI] [PubMed] [Google Scholar]
- 3.The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5(2):75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 4.Ma XP, Ng JD. Chronic epiphora secondary to ocular meibomianitis. Guoji Yanke Zazhi (Int Eye Sci) 2014;14(3):386–389. [Google Scholar]
- 5.Nemet AY, Vinker S. Associated morbidity of nasolacrimal duct obstruction--a large community based case-control study. Graefes Arch Clin Exp Ophthalmol. 2014;252(1):125–130. doi: 10.1007/s00417-013-2484-3. [DOI] [PubMed] [Google Scholar]
- 6.Damasceno RW, Osaki MH, Dantas PE, Belfort R., Jr Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthal Plast Reconstr Surg. 2011;27(5):317–320. doi: 10.1097/IOP.0b013e3182115229. [DOI] [PubMed] [Google Scholar]
- 7.Ansari Z, Singh R, Alabiad C, Galor A. Prevalence, risk factors, and morbidity of eye lid laxity in a veteran population. Cornea. 2015;34(1):32–36. doi: 10.1097/ICO.0000000000000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viso E, Rodriguez-Ares MT, Gude F. Prevalence and associations of external punctal stenosis in a general population in Spain. Cornea. 2012;31(11):1240–1245. doi: 10.1097/ICO.0b013e31823f8eca. [DOI] [PubMed] [Google Scholar]
- 9.Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis) Trans Am Ophthalmol Soc. 2007;105:649–666. [PMC free article] [PubMed] [Google Scholar]
- 10.Groessl SA, Sires BS, Lemke BN. An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol. 1997;115(1):71–74. doi: 10.1001/archopht.1997.01100150073012. [DOI] [PubMed] [Google Scholar]
- 11.Francisco FC, Carvalho AC, Francisco VF, Francisco MC, Neto GT. Evaluation of 1000 lacrimal ducts by dacryocystography. Br J Ophthalmol. 2007;91(1):43–46. doi: 10.1136/bjo.2005.088187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sibley D, Norris JH, Malhotra R. Management and outcomes of patients with epiphora referred to a specialist ophthalmic plastic unit. Clin Experiment Ophthalmol. 2013;41(3):231–238. doi: 10.1111/j.1442-9071.2012.02866.x. [DOI] [PubMed] [Google Scholar]
- 13.Williams B, Johnson D, Hurst J, Kratky V. Patterns and causes of epiphora referrals to a tertiary oculoplastic practice. Can J Ophthalmol. 2014;49(2):180–182. doi: 10.1016/j.jcjo.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Nemet AY. The etiology of epiphora: a multifactorial issue. Semin Ophthalmol. 2016;31(3):275–279. doi: 10.3109/08820538.2014.962163. [DOI] [PubMed] [Google Scholar]
- 15.Bron AJ, Tomlinson A, Foulks GN, Pepose JS, Baudouin C, Geerling G, Nichols KK, Lemp MA. Rethinking dry eye disease: a perspective on clinical implications. Ocul Surf. 2014;12(2 Suppl):S1–S31. doi: 10.1016/j.jtos.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Tsubota K. Tear dynamics and dry eye. Prog Retin Eye Res. 1998;17(4):565–596. doi: 10.1016/s1350-9462(98)00004-4. [DOI] [PubMed] [Google Scholar]
- 17.Zhang X, Chen Q, Chen W, Cui L, Ma H, Lu F. Tear dynamics and corneal confocal microscopy of subjects with mild self-reported office dry eye. Ophthalmology. 2011;118(5):902–907. doi: 10.1016/j.ophtha.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472–478. doi: 10.1097/ICO.0b013e318225415a. [DOI] [PubMed] [Google Scholar]
- 19.Nichols KK. The international workshop on meibomian gland dysfunction: introduction. Invest Ophthalmol Vis Sci. 2011;52(4):1917–1921. doi: 10.1167/iovs.10-6997. [DOI] [PMC free article] [PubMed] [Google Scholar]


