Abstract
AIM
To assess the binocular visual function in bilateral cataract patients with unilateral astigmatism after combined implantations of Toric with multifocal intraocular lens (IOL), and to compare with that of Toric and monofocal IOL implantation.
METHODS
All the 30 patients with unilateral astigmatism suffered bilateral cataract were randomly divided into two groups: Toric plus multifocal IOL group and Toric plus monofocal IOL group. Uncorrected and corrected visual acuity at distance (5.0 m), intermediate distance (0.6 m), and near (0.33 m), contrast sensitivity, and stereopsis were assessed 6mo after surgery. Patients were also surveyed for visual disturbances and spectacle dependence.
RESULTS
Binocular uncorrected visual acuity (LogMAR) of Toric/multifocal IOL eyes at distance, intermediate, near were 0.05±0.05, 0.24±0.10, and 0.14±0.06 respectively. The values of Toric plus monofocal IOL eyes were 0.06±0.07, 0.26±0.08, and 0.37±0.10 respectively. These values did not indicate significant differences between two groups with exception of near visual acuity. In the photopic condition (with or without glare), the contrast sensitivity of multifocal IOL eyes was significant lower than the monofocal IOL eyes in 18 cpd. In the mesopic condition, the contrast sensitivity of multifocal group was significant lower than monofocal group in 12 cpd, and in mesopic glare condition, this significant difference was found both in 6 cpd and 12 cpd. The stereopsis of Toric/multifocal IOL eyes decreased slightly (100±80 seconds of arc, t=2.222, P=0.136). Mean near vision for patient satisfaction was statistically significantly higher in Toric/multifocal IOL group patients versus than that in Toric/monofocal IOL group (80% vs 25.5%, P=0.000). Visual disturbance was not noticed in either group.
CONCLUSION
Although the combination of Toric and multifocal IOL implantation results in compromising stereoacuity, it can still provide patients with high levels of spectacle freedom and good overall binocular visual acuity.
Keywords: Toric, multifocal, intraocular lens, binocular cataract, unilateral astigmatism
INTRODUCTION
With the advent of cataract refractive surgery, premium intraocular lenses (IOLs) such as Toric IOLs, multifocal IOLs and accommodative IOLs are used more and more widely. Better understanding of the optics of IOLs along with improved cataract surgical techniques and devices can result in greater refractive predictability. Multifocal IOLs provide good vision at a larger range of distances than standard IOLs, improving near and distance vision simultaneously[1]. They offered a new alternative to appropriately selected patients who aspire to a spectacle-free life after their cataract removal. Meanwhile, the second generation of multifocal IOL has led to renewed interest in their use to correct refractive errors, particularly in patients who require higher levels of refractive correction and are not good candidates for corneal refractive surgery. Following bilateral multifocal IOLs implantation, rates of spectacle freedom are reported to be significantly higher (76% to 92% of patients) than with monofocal IOLs (8% to 12% of patients)[2].
However, for cataract patients with astigmatism, multifocal IOL must be forbidden unless the astigmatism is corrected by other surgical procedure. Current options of dealing with preexisting corneal astigmatism are as followed: limbal relaxing incisions, opposite clear cornea incisions or simply the incision placement on the steep meridian. Other options include excimer laser treatment post cataract surgery or Toric IOL implantations[3]. Among all the options, astigmatism correction with Toric IOL does not affect the cornea and make the procedure easier, it has the advantage of higher predictability and reversibility over other procedures[4]–[5].
Although patients with unilateral astigmatism are suitable for Toric IOLs implantation in astigmatic eyes, there are still two options for their non-astigmatic eyes. One is monofocal IOLs implantation which will be a binocular monofocal consequence with a significant decrease in near vision, despite an increased distant visual acuity. Although the strategy is much more simple and easy to perform, spectacles are needed for these patients to compensate the lack of accommodation. The other is multifocal IOLs implantation, which is quite probably to bring potential benefits of compensation for pseudophakic presbyopia, binocular functional vision over a broad range of distances, and greater spectacle independence, even though it is more complicated and possible to lead to the declination of the stereopsis and contrast sensitivity.
The object of this study was to evaluate the safety and efficacy of combined implantation of multifocal and Toric monofocal IOLs in cataract patients with unilateral astigmatism.
SUBJETCTS AND METHODS
This was a prospective study composed of 60 eyes of 30 patients (17 women, 13 men, aged 60 to 82 years old), who had come to Tianjin Medical University Eye Hospital between August 2011 and April 2012 with bilateral cataract and unilateral astigmatism. Each patient had given informed consent to phacoemulsification and IOL implantation. The tenets of the Declaration of Helsinki were fully adhered during the study.
Inclusion criteria were as followed: cataract in both eyes classified by the Lens Opacity Classification System III, corneal astigmatism larger than 1.00 D in unilateral eye, potential acuity better than 0.20 logarithm of minimal angle of resolution (logMAR) units, IOL power between +15.00 D and +25.00 D, and capability of understanding and signing the informed consent. Exclusion criteria were irregular cornea astigmatism, recurrent or chronic uveitis, corneal disease potentially impairing IOL visualization, surgical complications contraindicating the use of a nonsutured posterior chamber IOLs, history of retina surgery, and associated ocular abnormalities (e.g. microphthalmos, coloboma, glaucoma) beside the cataract.
All the patients in the study were randomly divided into two groups, one was Toric (AcrySof Toric IOL, SN60AT, Alcon Laboratories, Inc., USA) plus multifocal (AcrySof ReSTOR IOL, SN6AD1, Alcon Laboratories, Inc., USA) IOLs implantation in astigmatic and fellow eye respectively, the other was Toric plus monofocal IOLs (AcrySof IQ, SN60WF, Alcon Laboratories, Inc., USA) implantation. Fifteen patients were recruited in each group. The target spherical refraction of Toric-monofocal group was -0.5-0 D for both eyes.
Surgical Technique
Cataract surgery was performed on all patients by the same experienced surgeon (Zhang H). Standard technique in all patients consisted of microcoexial phacoemulsification using Alcon Infinity Intrepid phacomachines, with clear cornea incisions up to 2.4 mm and 5.0-5.5 mm capsulorhexis, and using the Monarch III IOL injector. When implanting the Toric IOL, patients were firstly seated pre-operation, looked straight ahead and then their eyes were marked horizontally at the limbus using a special marker, during operation surgeons must mark the Toric axis and then adjust the IOL to the predetermined position.
The power used in this study ranged from +18.00 D to +23.50 D. The type and axis of Toric IOL was obtained from www.acrysoftoriccalculator.com. T3 and T4 Toric IOLs were used in this study. IQ ReSTOR IOL and IQ IOL were both produced from the same aspheric platform of Alcon, the former was a multifocal IOL, which combined the functions of an apodized diffractive region and a refractive region, offering near addition of +3.0 D at lens plane equivalent to +2.4 D at spectacle plane, the latter was an aspheric, monofocal IOL.
Outcome Measurements
Patients were scheduled for clinical evaluation preoperatively and one day, one week as well as one, three, and six months postoperatively. Standard comprehensive ophthalmic examination including manifest refraction, biomicroscopy, intraocular pressure measurement, and funduscopy was performed at each visit. Results for postoperative binocular visual acuity were obtained 6mo after implantation of the second IOL for each patient. The primary outcome measures were binocular, uncorrected distance (5.0 m) and intermediate visual acuities (60 cm) using the Snellen chart and uncorrected near visual acuity (33 to 40 cm) using the Jaeger chart. Patients were allowed to read the near and intermediate charts at the optimum distance within the specified limitations. The results obtained at other distances than those intended for the chart used were converted to reflect the change in apparent letter size. Through-focus binocular logMAR acuity was also measured 6mo after surgery. Patients observed a distance logMAR chart through pairs of negative lenses increasing from +2.00 D to -5.00 D in degrees of 0.50 D.
Patients were asked in a survey to grade associated visual symptoms, visual satisfaction, and spectacle independence. Stereopsis was determined using vectograph cards (Titmus Stereo test), which dissociate the eyes optically. The amount of threshold disparity incorporated into the target was then recorded. Contrast sensitivity was performed between the ReSTOR and IQ eyes.
Statistical Analysis
Both nonparametric and parametric methods were used in the statistical analysis. Mann-Whitney U tests were used to compare visual acuity of multifocal with monofocal IOL groups. Visual acuity analysis was performed using logMAR values. Tests for binocular functions and stereoacuity were compared using contingency tables and chi-square statistics. A P-value of <0.05 was considered statistically significant.
RESULTS
Of the 30 patients enrolled, 15 were in the Toric-monofocal group, and 15 were in the Toric-multifocal group. No eyes had posterior capsule rupture or outward vitreous flow intraoperatively.
Preoperative patient demographics, including age, gender, type of cataract, follow-up, dioptric power of implanted IOL (18-23.5 D), and best-corrected visual acuity, did not differ significantly between the two groups (Table 1).
Table 1. Patient demography.
| Groups | No. | Sex (n) |
Age | Acuity | Diopter of IOL | Type of Toric |
||
| M | F | T3 | T4 | |||||
| Toric/multifocal | 15 | 7 | 8 | 69.69±9.57 | 0.28±0.12 | 20.13±2.38 | 8 | 7 |
| Toric/monofocal | 15 | 6 | 9 | 71.41±10.20 | 0.26±0.12 | 21.03±2.90 | 8 | 7 |
x±s
Table 2 shows the monocular and binocular uncorrected, distance, intermediate and near visual acuities in two groups. For monocular acuity, there was no significant difference in distance vision among Toric eyes, multifocal eyes and aspheric monofocal eyes, but in near vision, multifocal eyes had much better results which were statistically significant. Upon comparison of binocular visual acuity, no significant difference was noted between the two groups for uncorrected distance and intermediate visual acuity, but there was still significant difference in near vision.
Table 2. Monocular visual acuities in Toric-multifocal group and binocular visual acuities of both groups 6mo post-operatively.
| Parameters | Distance vision | Intermediate vision | Near vision |
| Toric eyes | 0.05±0.05 | 0.25±0.10 | 0.40±0.10 |
| Aspheric multifocal eyes | 0.06±0.05 | 0.22±0.15 | 0.14±0.10 |
| t | -0.189 | -0.023 | 5.738 |
| P | 0.852 | 0.982 | 0.000 |
| Toric-multifocal group eyes | 0.05±0.05 | 0.24±0.10 | 0.14±0.06 |
| Toric-monofocal group eyes | 0.06±0.07 | 0.26±0.08 | 0.37±0.10 |
| t | -0.188 | -0.022 | 5.634 |
| P | 0.852 | 0.978 | 0.000 |
Visual acuity is recorded in the logMAR form.
n=15 each
Tables 3 and 4 showed the contrast sensitivity results. Apart from 18 cpd under photopic conditions and 12 cpd under mesopic conditions, few significant differences were observed between multifocal and monofocal eyes. Stereopsis was similar between the 2 groups, measuring 100±80 seconds of arc in patients with Toric-multifocal and 60±30 seconds of arc in patients with Toric-monofocal IOLs.
Table 3. Comparison of contrast sensitivity under photopic and photopic glare condition in monofocal and multifocal eyes.
| Parameters | 1.5 | 3 | 6 | 12 | 18 |
| Contrast sensitivity under photopic condition | |||||
| Monofocal eyes | 1.62±0.23 | 1.79±0.19 | 1.84±0.39 | 1.30±0.58 | 0.94±0.58 |
| Multifocal eyes | 1.67±0.23 | 1.67±0.27 | 1.64±0.31 | 0.94±0.61 | 0.30±0.37 |
| t | -0.549 | 1.151 | 1.485 | 1.519 | 3.476 |
| P | 0.587 | 0.259 | 0.148 | 0.140 | 0.001 |
| Contrast sensitivity under photopic glare condition | |||||
| Monofocal eyes | 1.67±0.21 | 1.79±0.21 | 1.82±0.41 | 1.12±0.68 | 0.88±0.52 |
| Multifocal eyes | 1.69±0.23 | 1.68±0.23 | 1.48±0.64 | 0.78±0.62 | 0.34±0.44 |
| t | -0.226 | 1.255 | 1.471 | 1.363 | 2.975 |
| P | 0.822 | 0.220 | 0.152 | 0.183 | 0.006 |
Table 4. Comparison of contrast sensitivity under mesopic and mesopic glare condition in monofocal and multifocal eye.
| Groups | Contrast sensitivity under mesopic condition |
Contrast sensitivity under mesopic glare condition |
||||||
| 1.5 | 3 | 6 | 12 | 1.5 | 3 | 6 | 12 | |
| Monofocal eyes | 1.41±0.60 | 1.48±0.60 | 1.04±0.81 | 0.50±0.61 | 1.36±0.57 | 1.41±0.61 | 0.94±0.09 | 0.59±0.75 |
| Multifocal eyes | 1.30±0.50 | 1.08±0.60 | 0.34±0.67 | 0.05±0.22 | 1.24±0.50 | 0.91±0.70 | 0.34±0.66 | 0.05±0.22 |
| t | 0.514 | 1.689 | 2.484 | 3.057 | 0.579 | 1.876 | 2.047 | 3.154 |
| P | 0.611 | 0.102 | 0.019 | 0.005 | 0.567 | 0.071 | 0.050 | 0.004 |
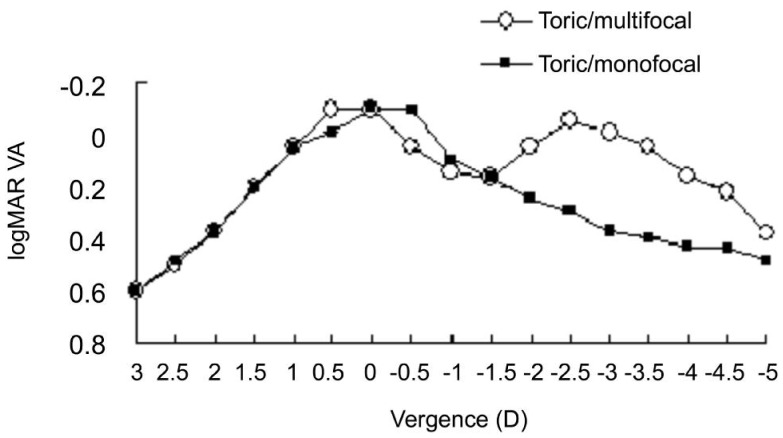
Figure 1 shows the postoperative through-focus best corrected binocular logMAR visual acuity in the 2 groups. The visual acuity shows 2 peaks at the expected far focus and near focus in the Toric-multifocal group (corresponding nominally to 0 D and -2.50 D respectively) while only 1 peak at 0 D in the Toric-monofocal group. Intergroup comparison from -2 D to -4.5 D shows better results in the Toric-multifocal group.
Figure 1. Mean high-contrast binocular visual acuity (logMAR) with best correction for distance as a function of the chart vergence for the Toric/multifocal group in this study, and the Toric/monofocal group.
The y-axis on the left shows the logMAR visual acuity and the x-axis on the bottom shows the distance equivalent of the chart vergence.
On the survey, 80% patients of the 2 groups did not need spectacles for distance activities. For the near activities, 73% of Toric-multifocal group and 25.5% of Toric-monofocal group did not need spectacles respectively, the difference of spectacle independence was statistically significant (χ2=56.00, P=0.000).
Two patients of Toric-multifocal group complained of dark vision in the multifocal eye 1wk after operation, but recovered 1mo later. The survey showed statistically significant difference between groups only in satisfaction with near vision (χ2=56.00, P=0.000).
DISCUSSION
As for the choice of premium IOLs in cataract patient, corneal astigmatism is looked upon as the standard. For the eye without astigmatism, multifocal or accommodative IOL could be implanted, otherwise Toric IOL with or without multifocal component will be chosen[6]. It has been suggested that the same type of IOLs implantation bilaterally could yield good results. However, it is perhaps hard to make a choice for bilateral cataract patient with unilateral corneal astigmatism when the contralateral eye would like to receive multifocal or accommodative IOL implantation. Compared the clinical results of different combination for these patients, the spectacle independence and patient satisfaction in multifocal plus Toric group are much better than that in monofocal plus Toric group.
Multifocal IOLs can provide better distance, intermediate and near vision than monofocal IOLs in the patients with low level of astigmatism[7]–[8]. Bilateral multifocal IOL implantations are always favored. However, several studies approved the success of unilateral implantation[9]. Cionni et al[9] suggested that surgeons can use an AcrySof ReSTOR IOL to provide a unilateral multifocal-phakic patient with good functional vision at near, intermediate, and far distances regardless of whether the phakic fellow eye is myopic, hyperopic, or emmetropic. Multifocal - phakic patients may have a lower prevalence of halos than bilateral multifocal patients. It was also proved that a monofocal - multifocal IOL combination can produce good near UCVA (0.09 logMAR), better than that produced by bilateral monofocal IOLs (0.41 logMAR ) in Lehmann et al's[2] study. Besides of this Lehmann et al's[2] found 65% of the patients implanted with the combination of monofocal and ReSTOR IOLs achieved spectacle independence. This result was similar to our finding. In our study, the visual acuity of the Toric/ReSTOR group in the near and intermediate distances were both better than the Toric/monofocal group. What's more, the spectacle independence in Toric/ReSTOR IOLs group was 73%, which was much higher than that in the control. A small loss of contrast sensitivity was noted with the multifocal IOLs at 18 cpd under photopic condition and 12 cpd under mesopic conditions when compared with aspheric monofocal lenses, which was similar to the loss of contrast sensitivity reported by Hayashi et al[10]. Another study suggested that the contrast sensitivity could be increased in the multifocal IOLs implanted eyes[11]. The questionnaire of the present study also shows few visual differences in both eyes, so it could be hypothesized that patients can gradually adapt to the small loss.
To evaluate the stereoscopic perception of contours, we used the calibrated Titmus fly chart to quantitatively assess the fly's subjective height[12]. Up to 50% of both groups were equivalent to those in normal phakic, however, the Toric/multifocal patients got slightly lower scores. Goes et al[13] briefly reported results of Titmus, Lang, and Randot tests and found the stereopsis after bilateral implantation was better than that after unilateral multifocal IOLs implantation. However, in recent years, Cionni et al[9] demonstrated that multifocal-phakic eyes had a stereoacuity score of 7.9 which was comparable to that in bilateral multifocal IOLs implantation of 6.5. It is related to the add power of multifocal IOLs which perhaps results in different degree of anisometropia and therefore different stereoacuity.
Binocular visual function can be well presented by the binocular defocus curve. As expected, the defocus curve in Figure 1 showed 2 peaks at the expected near focus and far focus points in Toric/multifocal group, with a flat stage which suggested vision was better than 0.5 at intermediate distance. One the contrary, there was only 1 peak at the far focus in the Toric/monofocal group. Enlargement of focus depth made the eyes with Toric/multifocal implantation see much better at any distance, which resulted in higher satisfaction in the questionnaire.
Many studies on “mixing and matching” multifocal lenses had yielded positive visual outcomes and support the concept of better overall vision[13]–[14]. As for astigmatism correction in cataract patients, Toric IOLs implantation can realize much more precise, stable and satisfied results[5],[15]. The present study is mixing multifocal lenses and Toric lenses for unilateral astigmatic patients. Binocular summation in the bilateral monofocal group appeared to provide better stereoacuity and contrast sensitivity than the unilateral multifocal group.
Monovision is another option to achieve overall vision. Monovision was designed to allow presbyopes have clear distant and near vision, with one eye adjusted to distance vision and the other eye to near vision using glasses or contact lens[16]. Pseudophakic monovision is a type of monovision used in cataract surgery to correct postoperative presbyopia using monofocal IOLs[17]. In this approach, the distance vision spherical equivalent (SE) is -0.50 to +0.50 D, and the near vision SE is -3.75 D to -1.00 D. The anisometropia is 1.00 D or even greater[18]. However, it is hard to balance the excellent near vision and the acceptable anisometropia. The further study of the comparison of monovision and the monofocal-multifocal IOLs combination to correct presbyopia can be conducted in the future to evaluate the overall vision and vision disturbance in each approach.
In our study, we did not consider the influence of the dominant eye for the following rationales. Several theories have been proposed for correcting the dominant eye, left eye or less myopic eye to maximize visual performance with less visual disturbance[18]. In the absence of rigorous clinical trials to support one method over the others, correcting the dominant eye for distance has become the common practice in many institutions. However, in the Jain et al's[18] study, crossed monovision (dominant eye corrected for near) in presbyopic correction can yield satisfactory results. In Kim et al's[16] study showed the similar results. He found that the clinical results of the crossed monovision (dominant eye corrected for near) were not significantly different from the results of conventional monovision (undominant eye corrected for near). Therefore, crossed monovision can also be a valuable option for correctin presbyopia in patients considering bilateral cataract surgery[16].
Multifocal toric IOLs can provide betterintermediate and near vision than monofocal Toric IOLs. It can improve UCVA and overall vision with spectacle independence by correcting corneal astigmatism and presbyopia at the same time[19]. However, we conducted this study of the combination of Toric IOL and ReSTOR IOL instead of the combination of Acrysof ReSTOR Toric IOL and ReSTOR IOL based on three considerations. First was the economic consideration. The cost of ART IOL is about twice of the Toric IOL. The combination of the monofocal and multifocal IOL will save a lot of money. This is an important factor in the developing country. Second was the correction range of astigmatism. The correction range of ART IOL is 0.5-2.5 D, while the Toric IOL can correct 0.5-4.0 D astigmatism[20]. In the patients with unilateral high astigmatism (>2.5 D), we can only refer to the combination of Toric and ReSTOR IOL to realize full range of vision. The last, if the patients had already been implanted with Toric IOL in one eye before the ART IOL was available, this study can provide the theoretical support to achieve full range of vision by the combination of Toric IOL and ReSTOR IOL[21]. This study provided a less expensive alternative to meet the patients' visual expectations in terms of all distances functional vision with spectacle independence. Satisfaction ratings and rates of spectacle freedom suggested that with proper counseling about realistic expectations, contralateral multifocal IOLs implantation for unilateral astigmatism yields satisfied patients with less cost.
Acknowledgments
Conflicts of Interest: Liang JL, None; Tian F, None; Zhang H, None; Teng H, None.
REFERENCES
- 1.Roensch MA, Charton JW, Blomquist PH, Aggarwal NK, McCulley JP. Resident experience with toric and multifocal intraocular lenses in a public county hospital system. J Cataract Refract Surg. 2012;38(5):793–798. doi: 10.1016/j.jcrs.2011.11.043. [DOI] [PubMed] [Google Scholar]
- 2.Lehmann R, Waycaster C, Hileman K. A comparison of patient reported outcomes from an apodized diffractive intraocular lens and a conventional monofocal intraocular lens. Curr Med Res Opin. 2006;22(12):2591–2602. doi: 10.1185/030079906X158039. [DOI] [PubMed] [Google Scholar]
- 3.Rubenstein JB, Raciti M. Approaches to corneal astigmatism in cataract surgery. Curr Opin Ophthalmol. 2013;24(1):30–34. doi: 10.1097/ICU.0b013e32835ac853. [DOI] [PubMed] [Google Scholar]
- 4.Freitas GO, Boteon JE, Carvalho MJ, Pinto RM. Treatment of astigmatism during phacoemulsification. Arq Bras Oftalmol. 2014;77(1):40–46. doi: 10.5935/0004-2749.20140011. [DOI] [PubMed] [Google Scholar]
- 5.Lam DK, Chow VW, Ye C, Nq PK, Wang Z, Jhanji V. Comparative evaluation of aspheric toric intraocular lens implantation and limbal relaxing incisions in eyes with cataracts and ≤3 dioptres of astigmatism. Br J Ophthalmol. 2016;100(2):258–262. doi: 10.1136/bjophthalmol-2014-306587. [DOI] [PubMed] [Google Scholar]
- 6.Marques EF, Ferreira TB, Simoes P. Visual performance and rotational stability of a multifocal toric intraocular lens. J Refract Surg. 2016;32(7):444–450. doi: 10.3928/1081597X-20160502-01. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi K, Masumoto M, Takimoto M. Comparison of visual and refractive outcomes after bilateral implantation of toric intraocular lenses with or without a multifocal component. J Cataract Refract Surg. 2015;41(1):73–83. doi: 10.1016/j.jcrs.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 8.Agresta B, Knorz MC, Kohnen T, Donatti C, Jackson D. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012;28(6):426–435. doi: 10.3928/1081597X-20120518-06. [DOI] [PubMed] [Google Scholar]
- 9.Cionni RJ, Osher RH, Snyder ME, Nordlund ML. Visual outcome comparison of unilateral versus bilateral implantation of apodized diffractive multifocal intraocular lenses after cataract extraction: prospective 6-month study. J Cataract Refract Surg. 2009;35(6):1033–1039. doi: 10.1016/j.jcrs.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Hayashi K, Manabe S, Hayashi H. Visual acuity from far to near and contrast sensitivity in eyes with a diffractive multifocal intraocular lens with a low addition power. J Cataract Refract Surg. 2009;35(12):2070–2076. doi: 10.1016/j.jcrs.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Mesci C, Erbil H, Ozdoker L, Karakurt Y, Bilqe AD. Visual acuity and contrast sensitivity function after accommodative and multifocal intraocular lens implantation. Eur J Ophthalmol. 2010;20(1):90–100. doi: 10.1177/112067211002000112. [DOI] [PubMed] [Google Scholar]
- 12.de Decker W, Dannheim E, Gockeln R. Fly test calibrated. In: Lennerstrand G, editor. Update on Strabismus and Pediatric Ophthalmology. Boca Raton: CRC Press; 1995. pp. 77–80. [Google Scholar]
- 13.Goes FJ. Visual results following implantation of a refractive multifocal IOL in one eye and a diffractive multifocal IOL in the contralateral eye. J Refract Surg. 2008;24(3):300–305. doi: 10.3928/1081597X-20080301-13. [DOI] [PubMed] [Google Scholar]
- 14.Gunenc U, Celik L. Long-term experience with mixing and matching refractive array and diffractive CeeOn multifocal intraocular lenses. J Refract Surg. 2008;24(3):233–242. doi: 10.3928/1081597X-20080301-04. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed II, Rocha G, Slomovic AR, Climenhaqa H, Gohill J, Greqoire A, Ma J, Canadian Toric Study Group Visual function and patient experience after bilateral implantation of Toric intraocular lenses. J Cataract Refract Surg. 2010;36(4):609–616. doi: 10.1016/j.jcrs.2009.10.044. [DOI] [PubMed] [Google Scholar]
- 16.Kim J, Shin HJ, Kim HC, Shin KC. Comparison of conventional versus crossed monovision in pseudophakia. Br J Ophthalmol. 2015;99(3):391–395. doi: 10.1136/bjophthalmol-2014-305449. [DOI] [PubMed] [Google Scholar]
- 17.Xiao J, Jiang C, Zhang M. Pseudophakic monovision is an important surgical approach to being spectacle-free. Indian J Ophthalmol. 2011;59(6):481–485. doi: 10.4103/0301-4738.86318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jain S, Ou R, Azar DT. Monovision outcomes in presbyopic individuals after refractive surgery. Ophthalmology. 2001;108(8):1430–1433. doi: 10.1016/s0161-6420(01)00647-9. [DOI] [PubMed] [Google Scholar]
- 19.Ganqwani V, Hirnschall N, Findl O, Maurino V. Multifocal toric intraocular lenses versus multifocal intraocular lenses combined with peripheral corneal relaxing incisions to correct moderate astigmatism. J Cataract Refract Surg. 2014;40(10):1625–1632. doi: 10.1016/j.jcrs.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 20.Kessel L, Andresen J, Tendal B, Ernqaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and Meta-analysis. Ophthalmology. 2016;123(2):275–286. doi: 10.1016/j.ophtha.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Farooqui JH, Koul A, Dutta R, Shroff NM. Management of moderate and severe corneal astigmatism with AcrySof® toric intraocular lens implantation-Our experience. Saudi J Ophthalmol. 2015;29(4):264–269. doi: 10.1016/j.sjopt.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]