Abstract
AIM
To evaluate the effect of incision types for Artisan phakic intraocular lens (PIOL) implantation on ocular higher-order aberrations (HOAs).
METHODS
A retrospective review was conducted of the patients who had undergone Artisan PIOL implantation for the correction of myopia and followed up for at least 6mo. Patients are classified into 2 groups considering the incision type: cornea group with patients undergone clear corneal incision; sclera group with patients undergone sclera tunnel incision. All patients with postoperative astigmatism of under 1 diopter (D) were included to minimize the effect of residual astigmatism on postoperative HOAs. Visual acuity, special equivalents, astigmatism, predictability (±1 D from target refraction), HOAs (coma, trefoil, spherical aberration), and corneal endothelial counts were analyzed preoperatively and 6mo postoperatively.
RESULTS
At the postoperative 6mo, all patients of both groups achieved uncorrected visual acuity of 16/20 or better, and significantly decreased the spherical equivalents compared with preoperative values. The predictability of refractive correction was 96% in the former, and 94% in the latter. Unlike the sclera group, preoperative astigmatism decreased significantly in cornea group at postoperative 6mo. The HOAs increased significantly at postoperative 6mo compared to the preoperative values in both groups, and the root mean square (RMS) total and trefoil wavefront aberration of cornea group were significantly higher than those of sclera group.
CONCLUSION
Although corneal incision significantly reduces preexisting astigmatism, the postoperative 6mo of total RMS and trefoil aberration change may deteriorate the visual quality after Artisan PIOL implantation.
Keywords: Artisan, astigmatism, higher- order aberrations, incision, phakic intraocular lens
INTRODUCTION
Recently, correction of myopic refractive errors is reportedly associated with favorable outcomes in terms of safety, efficacy, and predictability[1]–[3]. Correction of high myopia through the implantation of a phakic intraocular lens (PIOL), including Artisan PIOL, is a safe and effective alternative to other types of refractive surgeries that involve ablating the corneal stroma[2]–[4]. Although, in some patients an increased level of higher-order aberrations (HOAs) is produced postoperatively, resulting in various forms of visual discomfort such as glare, halo, and starburst[2]–[3],[5]–[6].
PIOL implantation is performed by many techniques including corneal and sclera incision. There are many reports about corneal incisions taking less time to create, and also known to induce much less astigmatism compare to scleral incisions during cataract surgery[7]–[8]. In addition, Wang et al[9] reported that corneal incision provides a faster visual recovery and lower postoperative corneal astigmatism compared with the scleral incisions in the implantation of iris-fixated PIOLs.
Although, Chung et al[10] have mentioned Artisan PIOL implantation for the correction of myopia resulted in a small increase in total HOAs, there are no studies reporting the relationship between incision types of Artisan PIOL implantation and postoperative induced HOAs. This study is to consider the effect of Artisan PIOL implantation incision type, sclera tunnel incision or clear corneal incision, on ocular HOAs.
SUBJECTS AND METHODS
Patients
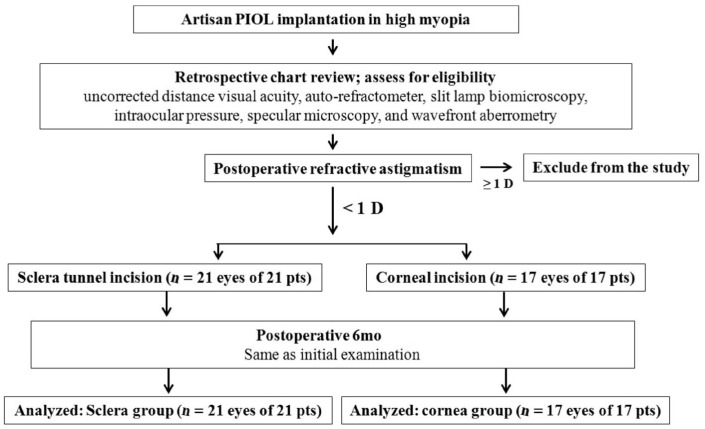
A retrospective review was conducted of the patients who had undergone Artisan PIOL implantation for the correction of myopia and followed up for at least 6mo. All patients provided informed written consent in accordance with the tenets of the Declaration of Helsinki, and an institutional review board (Pusan National University Hospital) approved the study. Only the patients with postoperative astigmatism of under 1 diopter (D) were included in this study to minimize the effect of residual astigmatism on postoperative HOAs (Figure 1). Patients with preoperative astigmatism of 3.00 D or greater were excluded as high natural astigmatism reduces the image quality obtainable from Hartmann-Shack wavefront sensing and is associated with higher levels of root mean square (RMS) higher-order wavefront aberration. Patients are classified into 2 groups considering the incision type during Artisan PIOL implantation: cornea group with patients undergone clear corneal incision; sclera group with patients undergone sclera tunnel incision. Patients with any pathologies or intra-operative or postoperative complications were further excluded from the study.
Figure 1. Flow chart of this study.
Artisan Phakic Intraocular Lens Implantation
Preoperative exclusion criteria were unstable refraction during the previous 2y, preoperative best spectacle-corrected visual acuity 20/50 or less, anterior chamber depth (ACD) 3.0 mm or less (IOLMaster, Carl Zeiss Meditec AG), endothelial cell density of 2000 cells/mm2 or less (Pachy SP-9000, Noncon Robo, Konan Medical), abnormal pupil and iris configuration, history of glaucoma, preexisting corneal, lenticular, or retinal pathology likely to alter vision, history of chronic or recurrent uveitis, and use of medication that could affect contrast sensitivity, IOL decentration, IOL out of the capsular bag. The target refraction was within -1.0 D in all cases.
All surgery was performed by one surgeon (Choi BJ). As mentioned earlier, Artisan PIOL implantation was performed through a scleral tunnel or a clear corneal incision. In patients with preoperative vertical astigmatism over 2 D, clear corneal incision is used to reduce underlying astigmatism. The preoperative treatment included instillation of moxifloxacin 0.5% four times daily for 3d. The pupils were constricted preoperatively with pilocarpine 2%. Anesthesia was administered using 4% lidocaine hydrochloride eye drops followed by a sub-Tenon injection with approximately 1 mL of 2% lidocaine hydrochloride. Scleral tunnel frown incisions with a 6.2 mm cord length were made in the superior quadrant 1.0 mm behind the limbus. The tunnel was fashioned by splitting the sclera with a crescent blade before final penetration of the cornea with a 2.75 mm keratome at the anterior extent of the tunnel. The incision was enlarged with a 6.2 mm keratome for Artisan PIOL implantation. Three-step clear corneal incisions were made using a 2.75 mm keratome in the superior quadrant in the posterior cornea. The same keratome was used to enlarge the wound to 6.2 mm for PIOL implantation. Except for the location of the incision, the surgical procedure was identical in all patients. All Artisan PIOLs were implanted through incision using forceps. The anterior chamber was filled with viscoelastic material (sodium hyaluronate 1.4%, Healon GV; Abbott Medical Optics). After implantation of a phakic Artisan IOL with the use of implantation forceps (P1318B, Duckworth & Kent, Hertfordhire, England), the lens was fixed to the iris with an enclavation needle (model OD125, OPHTEC BV) in such a way that the optic was centered over the centering point in all cases. The corneoscleral wound was closed with interrupted 10-0 nylon sutures, and the viscoelastic agent was removed by manual irrigation. Balanced saline solution (BSS Plus; Alcon Japan, Tokyo, Japan) was used as the irrigation fluid. The patients instilled moxifloxacin 0.5% eye drops four times daily and the anti-inflammatory drug fluorometholone 0.1% four times daily for a maximum of 4wk postoperatively based on the degree of inflammation. The sutures were removed at 4-6wk postoperatively.
Refractive Data and Higher-order Aberrations Assessment
Each measurement of the total HOAs and refractive data were recorded preoperatively and 6mo postoperatively using the OPD Scan III (Nidek Co., Aichi, Japan). The coefficients of Zernike polynomials were determined up to the sixth order for 5-mm optical zones from the wavefront data. All measurements were performed under maximal mydriasis induced by eye drops containing 0.5% tropicamide and 0.5% phenylephrine hydrochloride (Mydrin-P; Santen Pharmaceutical Co.), the pupillary diameters during measurements exceeded 6-mm in all patients. The RMS of the total HOAs from the third- to sixth-order Zernike coefficients was calculated.
Statistical Analysis
SPSS version 12.0 (SPSS, Chicago, IL, USA) was used for statistical analyses. The Wilcoxon signed-rank test was used to determine significant changes following treatment. The Mann-Whitney U test was used to compare the results between the groups. P<0.05 were considered statistically significant.
RESULTS
Thirty-eight eyes of 38 patients were included in study. There were 21 patients in the sclera group and 17 patients in the corneal group. Table 1 shows the patient characteristics and preoperative data by group. Only the preoperative cylinder values showed significant difference between the groups as all patients with preoperative vertical astigmatism over 2 D underwent clear corneal incision. There were no significant differences in the patient ages, spherical equivalents, intraocular pressure (IOP), corneal endothelial cell counts, or axial lengths, between the groups.
Table 1. Patient characteristics and preoperative data.
| Characteristics | Sclera group | Cornea group | P |
| No. of eyes | 21 | 17 | – |
| Age (a) | 30.2±5.1 | 32.6±6.2 | 0.66 |
| SE (D) | -9.05±1.90 | -10.26±1.20 | 0.39 |
| Spherical (D) | -8.57±1.8 | -9.12±1.2 | 0.45 |
| Cylinder (D) | -0.95±0.3 | -2.28±0.2 | 0.04 |
| CEC (cells/mm2) | 2875±54 | 2852±45 | 0.56 |
| IOP (mm Hg) | 14.6±2.1 | 14.3±2.3 | 0.77 |
| Axial length (mm) | 27.43±1.99 | 28.12±2.01 | 0.54 |
SE: Spherical equivalent of subjective refraction; D: Diopters; CEC: Corneal endothelial cell count; IOP: Intraocular pressure.
x±s
At the postoperative 6mo, all patients from both groups achieved uncorrected visual acuity (UCVA) of 16/20 or better. Eighteen patients (85.7%) from sclera group and 15 patients (88.2%) from cornea group had UCVA of 20/20 or better. Predictability within 1 D of target refraction was 96% in the former, and 94% in the letter. Spherical equivalents improved to -0.34±0.21 D in sclera group and to -0.40±0.18 D in cornea group at 6mo after surgery.
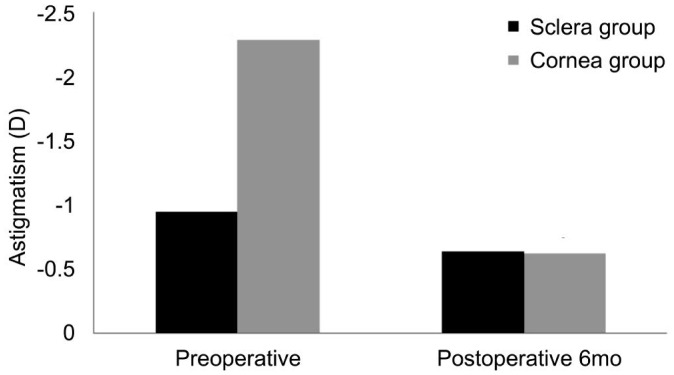
Unlike the sclera group, preoperative astigmatism decreased significantly in cornea group at postoperative 6mo. As a result of significant reduction in corneal group's preoperative astigmatism, postoperative astigmatism showed no difference between 2 groups (Figure 2).
Figure 2. Changes of astigmatism after Artisan PIOL implantation.
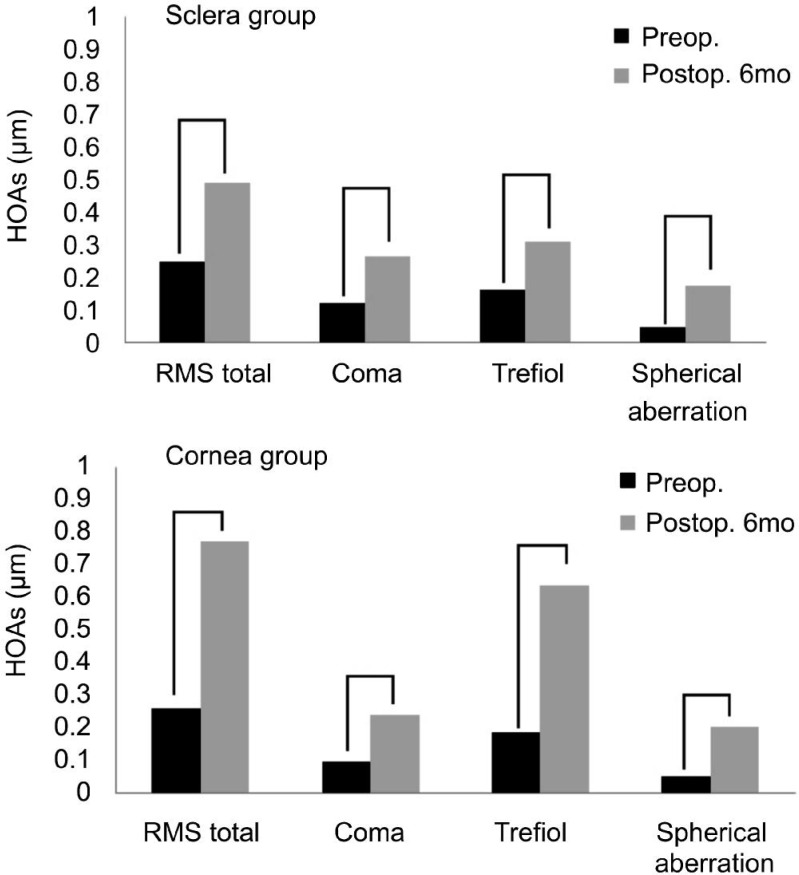
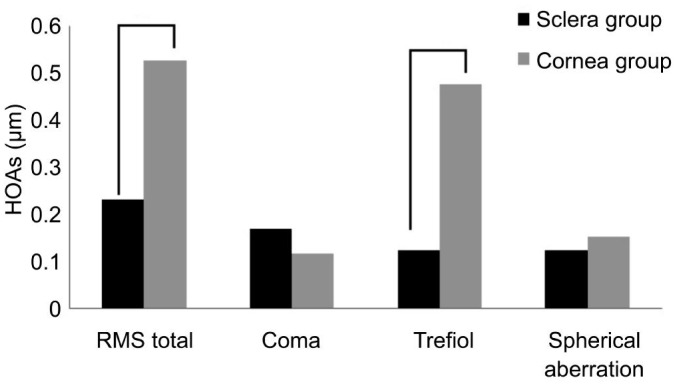
The HOAs increased significantly at postoperative 6mo compared to the preoperative values in both groups. The value of trefoil aberration was the highest among coma, trefoil, and spherical aberration in both groups at preoperative and postoperative 6mo (Figure 3). Postoperative induced HOAs, difference between preoperative and postoperative HOAs, showed various comparative results between 2 groups. Unlike induced spherical aberration showing insignificant differences between 2 groups, the induced RMS total and trefoil wavefront aberration at postoperative 6mo of cornea group were significantly higher than those of sclera group (Figure 4).
Figure 3. Changes of HOAs after Artisan PIOL implantation.
Figure 4. HOAs changes (Δ) from the base line measured at postoperative 6mo.
Corneal endothelial cell count showed insignificant change at postoperative 6mo compared to the preoperative results, 2891 cells/mm2 (preoperative corneal endothelial cell count; 2874 cells/mm2, 0.6% increase compared to the preoperative result) in the sclera group and 2847 cells/mm2 (preoperative corneal endothelial cell count; 2853 cells/mm2, 0.2% decrease compared to the preoperative result) in the cornea group. There was also insignificant difference of IOP and axial length between the former and latter group at preoperative and postoperative 6mo.
None of the eyes in this study experienced postoperative complications which required surgical or medical managements.
DISCUSSION
An aberration is a distortion of an image of an object that is caused by irregularities of its refractive components including tear film, cornea, aqueous humor, crystalline lens and vitreous. Lower-order aberrations consist of nearsightedness and farsightedness, as well as astigmatism. HOAs are composed of spherical aberration, coma, and trefoil, which can produce visual discomfort such as halos, blurring, starburst or monocular diplopia. Spherical aberration is halos around point images which causes night myopia and is commonly increased after myopic LASIK and surface ablation[3]. Coma aberration is induced by imperfection of the optical system which results in off-axis point sources producing distorted light image appearing to have a tail. Trefoil aberration causes the point of light to look more like a Mercedez Benz symbol, and is known to induce less degradation in image quality compared with coma. The immediate postoperative astigmatism and HOAs are affected by factors such as the surgical incison technique, type of suture used, and experience of the surgeons[11]. The aim of this study was to evaluate changes in total HOA after Artisan PIOL implantation for the correction of myopia, undermining the incision type.
We found that the refractive errors of patients with high myopia were successfully corrected by Artisan PIOL implantation, in that 95% of the sclera group and 94% of the corneal group were within 1 D of the attempted correction. Also, all patients in both group showed UCVA of 20/20 or better. This result collaborates with the studies noting the efficacy and safety of Artisan PIOL implantation[4],[12]–[15].
In contrast to the Chung et al's[10] report, RMS total, coma, trefoil, and spherical aberration showed significant increase at 6mo after Artisan PIOL implantation in both the cornea and sclera group. Due to spherical optic design of the Artisan PIOL, both group showed significantly increased spherical aberration after the surgery. On contrary, amount of spherical aberration change from the baseline differed insignificantly between both groups at postoperative 6mo. As both group used the same IOL, similar amount of spherical aberration might have been induced.
The corneal group of our study showed significant increase in the RMS total and trefoil aberration compared to the sclera group, which suggests significant postoperative increase in trefoil aberration is presumably the main cause results in the changes of RMS total aberration in the corneal group. Factors believe to be associated with postoperative HOAs other than incision type are age over 40y, higher keratometry values, higher degrees of myopia, and increasing pupil size[16]. In our study, previously mentioned factors showed no significant difference between the groups, preoperatively. As both groups' postoperative astigmatism did not differ significantly, residual astigmatism also cannot explain the significant increase of HOAs in cornea group postoperatively. Internal optics, such as the crystalline lens, theoretically stayed unchanged by Artisan PIOL implantation, surgical incision might be solely responsible for the increase in HOAs. Our results supports the Buhren et al's[17] presumption that notable increase of trefoil aberration might be related to the distance between the limbus and incision after implantation of a phakic Artisan IOL. Previous studies of HOAs changes in cataract surgery also suggested that trefoil changes may be related to the surgical procedure, for example, the incision size and position[18]–[21]. It seems that due to the distance between the incision site and the corneal center, clear corneal incision contributes to the more increase in trefoil aberration compared to the sclera tunnel incision. Further analysis about the crystalline lens position and the thickness, corneal thickness, and retinal thickness measured by optical coherence tomography may help to clarify the findings.
Although the corneal incision might be helpful in terms of reducing preexisting astigmatism, the postoperative total RMS and trefoil aberration change may deteriorate the visual quality after Artisan PIOL implantation. Due to the retrospective design of our study, we were not able to evaluate the HOAs changes in the patients with small amount of preoperative astigmatism, astigmatism under 2 D, who had undergone clear corneal incision based Artisan PIOL implantation. Correlation analysis with more patients might be required to reveal the relationship between amount of the decreased preoperative astigmatism and the induced HOAs by clear corneal incision.
Acknowledgments
Conflicts of Interest: Park YM, None; Choi BJ, None; Lee JS, None.
REFERENCES
- 1.Alio JL, Muftuoglu O, Ortiz D, Perez-Santonja JJ, Artola A, Ayala MJ, Garcia MJ, de Luna GC. Ten-year follow-up of laser in situ keratomileusis for myopia of up to -10 diopters. Am J Ophthalmol. 2008;145(1):46–54. doi: 10.1016/j.ajo.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 2.Tuunanen TH, Tervo TT. Results of photorefractive keratectomy for low, moderate, and high myopia. J Refract Surg. 1998;14(4):437–446. doi: 10.3928/1081-597X-19980701-10. [DOI] [PubMed] [Google Scholar]
- 3.Vega-Estrada A, Alio JL, Arba Mosquera S, Moreno LJ. Corneal higher order aberrations after LASIK for high myopia with a fast repetition rate excimer laser, optimized ablation profile, and femtosecond laser-assisted flap. J Refract Surg. 2012;28(10):689–696. doi: 10.3928/1081597X-20120921-03. [DOI] [PubMed] [Google Scholar]
- 4.Maloney RK, Nguyen LH, John ME. Artisan phakic intraocular lens for myopia: short-term results of a prospective, multicenter study. Ophthalmology. 2002;109(9):1631–1641. doi: 10.1016/s0161-6420(02)01170-3. [DOI] [PubMed] [Google Scholar]
- 5.Seiler T, Kaemmerer M, Mierdel P, Krinke HE. Ocular optical aberrations after photorefractive keratectomy for myopia and myopic astigmatism. Arch Ophthalmol. 2000;118(1):17–21. doi: 10.1001/archopht.118.1.17. [DOI] [PubMed] [Google Scholar]
- 6.Yamane N, Miyata K, Samejima T, Hiraoka T, Kiuchi T, Okamoto F, Hirohara Y, Mihashi T, Oshika T. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45(11):3986–3990. doi: 10.1167/iovs.04-0629. [DOI] [PubMed] [Google Scholar]
- 7.Bar-Sela SM, Spierer A. Astigmatism outcomes of scleral tunnel and clear corneal incisions for congenital cataract surgery. Eye (Lond) 2006;20(9):1044–1048. doi: 10.1038/sj.eye.6702082. [DOI] [PubMed] [Google Scholar]
- 8.Olsen T, Dam-Johansen M, Bek T, Hjortdal JO. Corneal versus scleral tunnel incision in cataract surgery: a randomized study. J Cataract Refract Surg. 1997;23(3):337–341. doi: 10.1016/s0886-3350(97)80176-9. [DOI] [PubMed] [Google Scholar]
- 9.Wang KJ, Wang NL, Zhang FJ, Zhu SQ. Rigid iris-fixated phakic lens implantation for high myopia: novel trapezoidal corneal versus scleral incisions. Eur J Ophthalmol. 2012;22(Suppl. 7):S114–S119. doi: 10.5301/ejo.5000058. [DOI] [PubMed] [Google Scholar]
- 10.Chung SH, Lee SJ, Lee HK, Seo KY, Kim EK. Changes in higher order aberrations and contrast sensitivity after implantation of a phakic artisan intraocular lens. Ophthalmologica. 2007;221(3):167–172. doi: 10.1159/000099296. [DOI] [PubMed] [Google Scholar]
- 11.Gimbel HV, Sun R, DeBroff BM. Effects of wound architecture and suture technique on postoperative astigmatism. Ophthalmic Surg Lasers. 1995;26(6):524–528. [PubMed] [Google Scholar]
- 12.Landesz M, Worst JG, van Rij G. Long-term results of correction of high myopia with an iris claw phakic intraocular lens. J Refract Surg. 2000;16(3):310–316. doi: 10.3928/1081-597X-20000501-03. [DOI] [PubMed] [Google Scholar]
- 13.Teng H, Zhang H. Comparison of Artisan iris-claw intraocular lens implantation and posterior chamber intraocular lens sulcus fixation for aphakic eyes. Int J Ophthalmol. 2014;7(2):283–287. doi: 10.3980/j.issn.2222-3959.2014.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Güell JL, Verdaguer P, Elies D, Gris O, Manero F, Mateu-Figueras G, Morral M. Secondary iris-claw anterior chamber lens implantation in patients with aphakia without capsular support. Br J Ophthalmol. 2014;98(5):658–663. doi: 10.1136/bjophthalmol-2013-304035. [DOI] [PubMed] [Google Scholar]
- 15.Bamashmus MA, Mohamed AA, Alakhlee HA. A retrospective analysis of the first Yemeni experience on Artisan phakic intraocular lens for the treatment of moderate and high myopia. Oman J Ophthalmol. 2012;5(3):175–180. doi: 10.4103/0974-620X.106098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Castro LE, Sandoval HP, Bartholomew LR, Vroman DT, Solomon KD. High-order aberrations and preoperative associated factors. Acta Ophthalmol Scand. 2007;85(1):106–110. doi: 10.1111/j.1600-0420.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 17.Buhren J, Kasper T, Terzi E, Kohnen T. Higher order aberrations after implantation of an iris claw pIOL (Ophtec Artisan) in the phakic eye. Ophthalmologe. 2004;101(12):1194–1201. doi: 10.1007/s00347-004-1058-5. [DOI] [PubMed] [Google Scholar]
- 18.Guirao A, Tejedor J, Artal P. Corneal aberrations before and after small-incision cataract surgery. Invest Ophthalmol Vis Sci. 2004;45(12):4312–4319. doi: 10.1167/iovs.04-0693. [DOI] [PubMed] [Google Scholar]
- 19.Eliwa TF, Elsamkary MA, Hamza I. Effect of biaxial versus coaxial microincision cataract surgery on optical quality of the cornea. Indian J Ophthalmol. 2015;63(6):487–490. doi: 10.4103/0301-4738.162598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Serrao S, Lombardo G, Schiano-Lomoriello D, Rosati M, Lombardo M. Preliminary investigation of corneal wavefront aberration following femtosecond laser clear corneal incision for cataract surgery. Eur J Ophthalmol. 2014;24(6):842–849. doi: 10.5301/ejo.5000485. [DOI] [PubMed] [Google Scholar]
- 21.Kim SW, Yang H, Yoon G, Lee YJ, Kweon MN, Kim JK, Seo KY. Higher-order aberration changes after Implantable Collamer Lens implantation for myopia. Am J Ophthalmol. 2011;151(4):653–662. doi: 10.1016/j.ajo.2010.10.031. [DOI] [PubMed] [Google Scholar]