INTRODUCTION
Approximately 10% of UK blindness registrations are attributed to glaucoma[1]. The risk of glaucoma increases with age and it is estimated that the prevalence of chronic open angle glaucoma (COAG) is about 10% in white Europeans who are older than 70. There are an estimated 24.4 million people aged over 40 in England and around 489 000 people are currently affected by COAG. These numbers are likely to increase with increasing life expectancy[1]. With aging, there is an increase in prevalence of chronic diseases such as dementia, Alzheimer's disease and osteoarthritis, leading to severe frailty, disability and dependence for their basic needs and care[2]–[3].
The demographic profile of the South West of England shows it one third of it is population living in rural areas (31.3%) which is highest among all English regions. Also, the region's population is oldest with 4.4% people aged over 75, of whom 33% are older than 90. The life expectancy of men and women is also amongst the highest of all counties in the United Kingdom[4]. People diagnosed with COAG are managed by the hospital eye service and lifelong follow-up is normally needed so that any progression of glaucomatous damage can be detected and managed. Sight loss due to glaucoma cannot be restored, and therefore controlling the condition carefully is crucial to maintaining sight. People with severe physical and/or mental disability often reside in care homes and find journeys to hospital stressful, and in many cases not possible, even if appropriate transportation is available. Provisions of community hospitals and mobile clinic reviews has reduced the need to travel to main hospitals, however some patients are still not able to attend. To overcome this problem, a new care pathway called the glaucoma domiciliary service (GDS), managed by optometrists, a central coordinator and consultant glaucoma ophthalmologists was designed and commissioned at the Royal Devon and Exeter (RD&E) Foundation Trust. Glaucoma patients who are unable to attend normal follow-up clinics due to significant physical and/or mental disabilities are offered GDS at their residence. We present the service framework and outcome of our experience of GDS.
SUBJECTS AND METHODS
Optometrist Training
All eligible candidates have to complete two Masters of Science (MSc) glaucoma modules and separate training to gain independent prescribing rights. The optometrist then undergoes supervised sessions with a qualified glaucoma practitioner until all competencies are achieved.
Services Standards and Glaucoma Domiciliary Service Protocols
The protocols for the GDS were developed to adhere to the National Institute of Health and Care Excellence (NICE) guidelines for glaucoma (1). There was no example of GDS or a similar service found in the literature. A detailed framework is presented in Table 1.
Table 1. General service framework for glaucoma domiciliary service.
| 1. Referral of each patient to GDS should be made by a consultant glaucoma ophthalmologist | ||
| 2. GDS follow up and frequency of home visits planned according to the need and severity of glaucoma and decided by glaucoma specialist | ||
| 3. Target level for the IOP set by a consultant glaucoma ophthalmologist | ||
| 4. Ocular exam as detailed | ||
| Baseline examination |
Follow up examination |
|
| Ophthalmic and general history | Yes | Yes |
| Other problems | Yes | Yes |
| Ocular medication and side effect | Yes | Yes |
| Ocular examination | ||
| VA | Yes | Yes |
| Slit lamp exam | Yes | Yes (portable) |
| Gonioscopy | Yes | No |
| Pachymetry | Yes | No |
| IOP | Yes (applanation) | Yes (perkins) |
| Disc assessment and fundus exam 78 D/90 D lens (dilated) | Yes | Direct ophthalmoscope (dilated only if fundus details not seen clearly) |
| OCT disc | Yes | No |
| Visual field | Yes | No |
| Ocular drug administration and difficulties check |
No |
Yes |
| 5. Letter about the review should be sent to GP and consultant ophthalmologist | ||
| 6. If VA reduced, both carer and patient need to be informed | ||
| 7. Any concern, consultant ophthalmologist to be informed | ||
| 8. If IOP level high: (If >30 mm Hg than immediate consultation with consultant ophthalmologist) otherwise a. Compliance check b. Check technique of drop installation if patient manages own drops or to identify the responsible person c. Patients followed up within 2mo | ||
| 9. If IOP still high a. Consultant glaucoma ophthalmologist to feedback and decide whether to change treatment, revise the target pressure or request an attempt at further hospital clinic review b. Patient reviewed after changing treatment | ||
Study Subjects
Patients were identified via the database of the visiting optometry team over the period from January 2012 to February 2013. The GDS correspondence and hospital case notes were reviewed. Data collected and analysed included information on demographics, systemic morbidity and compliance against the set service framework (Table 1). Local ethics committee approval was granted for the study and it adhered to the principles outlined in the Declaration of Helsinki.
RESULTS
Patient Demographic
There were 102 patients who were managed under GDS during this period. Clinical records of 11 patients were not available and consequently not included in analysis. Of 91 patients, 63 were females and 28 males. The mean age of the patients was 89 (range: 56-101)y.
Type of Glaucoma
The majority of patients had primary open angle glaucoma (Figure 1). The severity of the disease was moderate to severe in 42.9%, with 31 (34.1%) patients having moderate and 8 (8.8%) severe glaucoma. The disease severity was defined according to the modified International Geographical and Epidemiologic Ophthalmology (IGEO) POAG criteria[5]. A total of 14 patients had previous glaucoma related intervention (7 trabeculectomy: 5 bilateral trabeculectomy, 2 unilateral trabeculectomy and 7 had peripheral iridotomy) and all patients were on pressure lowering medications.
Figure 1. Type of glaucoma in patients under glaucoma domiciliary service.
NTG: Normal tension glaucoma; NAG: Narrow angle glaucoma; OHT: Ocular hypertension; POAG: Primary open angle glaucoma; PXF: Pseudo-exfoliation.
Other Ocular Morbidities
Other ocular morbidities identified included cataract (n=7) and dry age related macular degeneration (n=4).
Residential Status and Systemic Morbidity
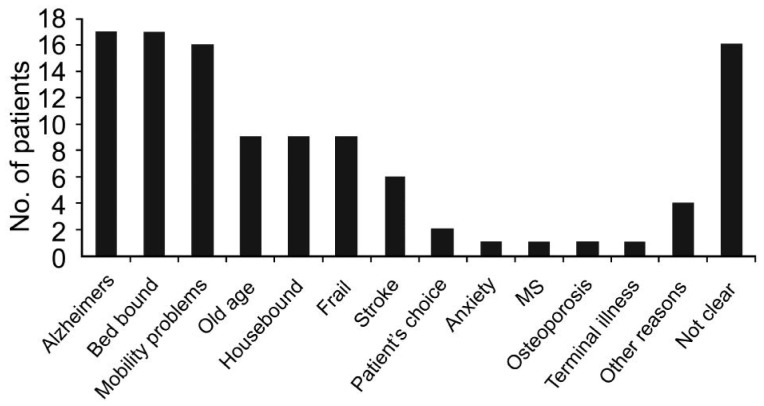
The majority of the patients under GDS lived in nursing or residential homes (60; 65.9%) whereas the others lived in their personal homes (31; 34.1%). In all cases, as per the guidelines, the referral to GDS was made by a consultant glaucoma ophthalmologist. The reasons for referral to GDS are highlighted in Figure 2.
Figure 2. Systemic morbidity in patients under glaucoma domiciliary service.
MS: Multiple sclerosis.
Study Compliance
In 98.9% (90/91) of cases the home visits were planned according to need and severity of disease. An intraocular pressure (IOP) target level was set by the consultant ophthalmologist in 96.7% (88/91). In those without a target IOP, which was noted in 3 patients in the initial GDS visits, this was subsequently set by consultant ophthalmologist. No risk to patient care was identified. For all patients on GDS, the visual acuity (VA), IOP, disc appearance and visual field were documented by a consultant ophthalmologist at the time of referral to GDS. All patients had a documented ophthalmic and general history. Changes in vision, medication and side effect records, general ocular examination, IOP, VA and optic disc examination was documented and performed. After each GDS visit, a letter summarising the findings was sent to the general practitioner (GP) and consultant ophthalmologist. Fourteen of 91 patients on GDS had IOP above the target at some point during their follow-up at home. For those 14 patients, the compliance with medication was checked and the patient was then followed up within 2mo. At follow-up, 6 patients still had high IOP and therefore the consultant ophthalmologist changed their management and revised the target IOP. These patients were subsequently followed-up by the GDS.
DISCUSSION
The RD&E Hospital provides a highly organised glaucoma service to house bound patients in East Devon via a fully equipped mobile van operated by trained glaucoma optometrist. The GDS has a central coordinator and a team of optometry practitioners who provide domiciliary optometric services under the supervision of glaucoma consultants.
The continuation of glaucoma monitoring in hospitals is very problematic in housebound patients. GDS is an extended concept of a shared care service which ensures disease monitoring for these patients continues.
Although a detailed cost analysis was not performed, shared care services are generally considered as cost effective[1]. The agreed tariff for an optometrist visit is £95, but this is reduced to £45 if they provide a NHS sight test simultaneously. The current tariff for an optometrist or nurse specialist follow-up in a hospital glaucoma clinic is £63. Thus it is an incentivised practise opportunity for optometrists. Potential cost saving is from the reduction in staff needed to accompany these vulnerable patients to hospital, administrative costs and the cost of transporting patients to hospital frequently. Nevertheless, many of these patients could not travel to hospital even if transport were provided.
We found that a majority of the GDS patients (42.9%) suffer from moderate to severe glaucoma, and the remaining have either mild or other form of the disease. This is in contrast to the usual glaucoma shared care service where the majority of patients would have mild stable glaucoma. This discrepancy is most likely due to the over-representation of older patients requiring domiciliary care. Most of the patients in the group are generally in poor health and are at risk of visual loss due to glaucoma (as evidenced by disease severity results) which can have a substantial impact on their quality of life (QOL)[5]. Through GDS, these patients remain under specialist supervision and also non-glaucomatous disease can be diagnosed early by the optometrist. Furthermore, issues such as treatment compliance can be addressed.
Serial visual field assessment, as stipulated by NICE guidelines, were not possible using the GDS, although it is debatable whether such tests would be possible in the hospital environment due to conditions such as dementia. This slightly limits the ability of the GDS to detect and monitor subtle disease progression. However, the presence of other checks within the framework (ONH assessment, VA decline) are hopefully effective at preventing or slowing visual loss.
In summary, GDS in East Devon is an effective and safe service providing care to over 100 housebound patients over this 2y period. It also met the vision statement as outlined by NICE. We are not aware of any other reported domiciliary glaucoma care service in the literature and hope this study will help increase the awareness of such management in the UK. Domiciliary care allows this vulnerable group of patients to remain under the care of the glaucoma team without the need for regular hospital visits. Future studies are planned to look at the longer term outcomes in this cohort of patients.
Acknowledgments
Conflicts of Interest: Gupta B, None; Faridi U, None; Gurmani N, None; Faverty J, None; Smith M, None; Byles D, None.
REFERENCES
- 1.National Institute for Health Care and Excellnce NICE clinical guideline 85 (Report) Glaucoma: diagnosis and management of chronic open angle glaucoma and ocular hypertension. 2009:1–39. [Google Scholar]
- 2.Boeckxstaens P, Peersman W, Goubin G, Ghali S, De Maeseneer J, Brusselle G, De Sutter A. A practice-based analysis of combinations of diseases in patients aged 65 or older in primary care. BMC Fam Pract. 2014;15:159. doi: 10.1186/1471-2296-15-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boeckxstaens P, Vaes B, Legrand D, Dalleur O, De Sutter A, Degryse JM. The relationship of multimorbidity with disability and frailty in the oldest patients: a cross-sectional analysis of three measures of multimorbidity in the BELFRAIL cohort. Eur J Gen Pract. 2014:1–6. doi: 10.3109/13814788.2014.914167. [DOI] [PubMed] [Google Scholar]
- 4.Office for National Statistics Report. UK population estimates 2013. 26-6-2014.
- 5.Mills T, Law SK, Walt J, Buchholz P, Hansen J. Quality of life in glaucoma and three other chronic diseases: a systematic literature review. Drugs Aging. 2009;26(11):933–950. doi: 10.2165/11316830-000000000-00000. [DOI] [PubMed] [Google Scholar]