Abstract
Study Objectives:
This study aimed to determine the consequences of snoring independent of obstructive sleep apnea (OSA) and hypothesized that snoring sound intensity, as assessed by mean tracheal sound (TS) energy (Leq), is related to morning blood pressure (BP).
Methods:
A home-based TS monitoring study was performed for two nights on 191 workers in Japan using an IC recorder. Leq and the respiratory disturbance index (RDI) were calculated from the TS data. RDI was used as a marker of OSA severity. Systolic and diastolic BP measurements in the evening and morning (eSBP/eDBP and mSBP/mDBP, respectively) were done before and after TS recording. The data of the second night were analyzed.
Results:
Leq was significantly related to both mSBP and mDBP (r = 0.32, p < 0.0001; r = 0.34, p < 0.0001, respectively). Leq was also significantly related to morning BP after adjustment for age, sex, and body mass index. However, the relationship was no longer significant when both RDI and Leq were included in the multiple regression model. In non-apneic, non-obese subjects, Leq was significantly related to both mSBP and mDBP (r = 0.38, p < 0.0001; r = 0.33, p = 0.0004, respectively). In this group, Leq was associated with mSBP after adjusting for all confounding factors (n = 106, p = 0.022).
Conclusions:
The association between night TS intensity and morning BP suggests a pathological role of heavy snoring. To understand this association, a prospective cohort study in a general population is warranted.
Commentary:
A commentary on this article appears in this issue on page 1581.
Citation:
Furukawa T, Nakano H, Yoshihara K, Sudo N. The relationship between snoring sound intensity and morning blood pressure in workers. J Clin Sleep Med 2016;12(12):1601–1606.
Keywords: snoring, acoustics, morning blood pressure, sleep apnea
INTRODUCTION
Snoring is an acoustic phenomenon occurring during sleep caused by the vibration of the soft tissues of the upper airway. It is not only a nuisance to the bed partner but can also have a negative health consequence on the snorers.
Many epidemiological studies have shown that habitual snorers experience cardiovascular diseases.1–7 Obstructive sleep apnea (OSA), rather than snoring, was considered to contribute to the incidence of cardiovascular diseases because a considerable number of habitual snorers have OSA. However, according to some studies, snoring itself can lead to cardiovascular diseases through decreased baroreceptor sensitivity/ reactivity8,9 and mechanical injury to the carotid artery endothelium.10 These findings suggest that snoring has its own vascular risk. Recently, heavy snoring is shown to be associated with carotid atherosclerosis independent of apnea severity and other risk factors.11 However, several conflicting studies reported no association between snoring history and degree of carotid stenosis.12,13 Thus, whether or not snoring can lead to cardiovascular consequence remains to be clarified.
We have reported two studies supporting the cardiovascular effects of snoring. One study demonstrated that ambient snoring intensity is independently associated with daytime blood pressure (BP) in subjects with primary snoring or mild OSA.14 The other study demonstrated that the mean tracheal sound (TS) energy (Leq), which represents snoring sound intensity, is related to daytime BP in subjects suspected of OSA, independent of OSA severity.15 Because subjects in these studies consisted of a clinical population, those subjects were likely to have heavier snoring than those in a community population. To investigate the effects of snoring on BP according to severity, not only heavy but also mild snorers should be included as study subjects.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although many epidemiological studies have shown that snoring is associated with cardiovascular diseases, the snoring frequency obtained in those studies was questionnaire-based, and only a few studies have objectively measured snoring. Our previous study showed an association between objectively measured snoring and hypertension in clinic samples.
Study Impact: This population-based study showed the association between objectively measured snoring and hypertension. This study highlights the significance of snoring as well as sleep apnea in the pathophysiology of developing hypertension.
Our two previous studies tested the relationship between snoring and daytime BP measured in the office. It is possible that snoring contributes to increased BP in the morning rather than during daytime because snoring is a phenomenon occurring during sleep. We hypothesized that snoring sound intensity is related to morning BP, which was measured at home in a worker population.
METHODS
Subjects
The present study included 191 workers in two facilities. The subjects worked as public employees, mostly engaged in office work. This study was approved by the Institutional Review Board in Fukuoka National Hospital, and signed informed consent was obtained from all subjects.
Measurements
The subjects recorded their TS for two nights at home using an IC recorder (ICR-PS285RM; Sanyo, Osaka, Japan) between February 2008 and February 2010. We used TS measurement for this study because it is immune to ambient noise and is suitable for home monitoring. TS was captured using an air-coupled microphone (MC-TP2; Sharp, Osaka, Japan) attached on the neck over the trachea. TS was digitized and recorded on the IC recorder as data with 44,100-Hz frequency and 16-bit resolution. The recording system of TS was calibrated by a reference sound pressure (94 dB). The subjects were instructed to switch their IC recorder and start TS recordings by themselves just before going to bed and to stop the TS recordings by themselves after getting up on the following morning. Subjects were asked to complete a questionnaire to identify their symptoms, sleep habits, alcohol consumption, cigarette smoking, and clinical history including medications. Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters. Their evening BP was measured just before starting the TS recording and going to bed, and their morning BP was measured after awakening and urination and before breakfast on the following morning. We used a digital home BP monitoring device (Omron HEM 762P; Omron, Kyoto, Japan) for the BP measurement. The average value of three measurements was recorded as the BP value. BP values measured in the evening and in the morning were designated as evening BP (eSBP/eDBP) and morning BP (mSBP/mDBP), respectively. Morning and evening hypertension was defined as mSBP/ eSBP ≥ 135 mm Hg or mDBP/eDBP ≥ 85 mm Hg. Morning and evening prehypertension was defined as 115 ≤ mSBP/ eSBP < 135 mm Hg or 75 ≤ mDBP/eDBP < 85 mm Hg.16
TS Analysis
The TSs were analyzed using a PC-based compressed sound spectrograph system that we developed to detect snoring.17 The details are described elsewhere. The system calculated several snoring variables, among which we used Leq (equivalent sound pressure level) as the primary snoring variable. Leq, expressed in decibels, was calculated as the average of the squared ratio of the instantaneous sound pressure and the reference signal (20 μPa). Leq represents the mean sound energy during total recording time. We calculated the respiratory disturbance index (RDI) using the method developed by Nakano et al.17 and used this as a marker of OSA severity.
Statistical Analysis
Thirty-five subjects were excluded from analysis because of insufficient data or because they were taking antihypertensive drugs. The remaining 156 subjects were included in subsequent analyses.
We analyzed the BP and snoring data from the second night of monitoring to avoid any effect that might be caused by the adjustment of the patient during the first night. The analysis was primarily performed for all subjects. Descriptive characteristics are summarized as the Leq tertiles (Table 1). Continuous variables are expressed as means and standard deviations for normally distributed variables; otherwise, as medians and interquartile ranges. Categorical variables are expressed as percentages. To detect differences among groups, one-way analysis of variance and the Kruskal-Wallis test were performed to compare parametric and nonparametric data, respectively. The χ2 test was performed to compare proportions among groups. A p value < 0.05 was considered to be statistically significant.
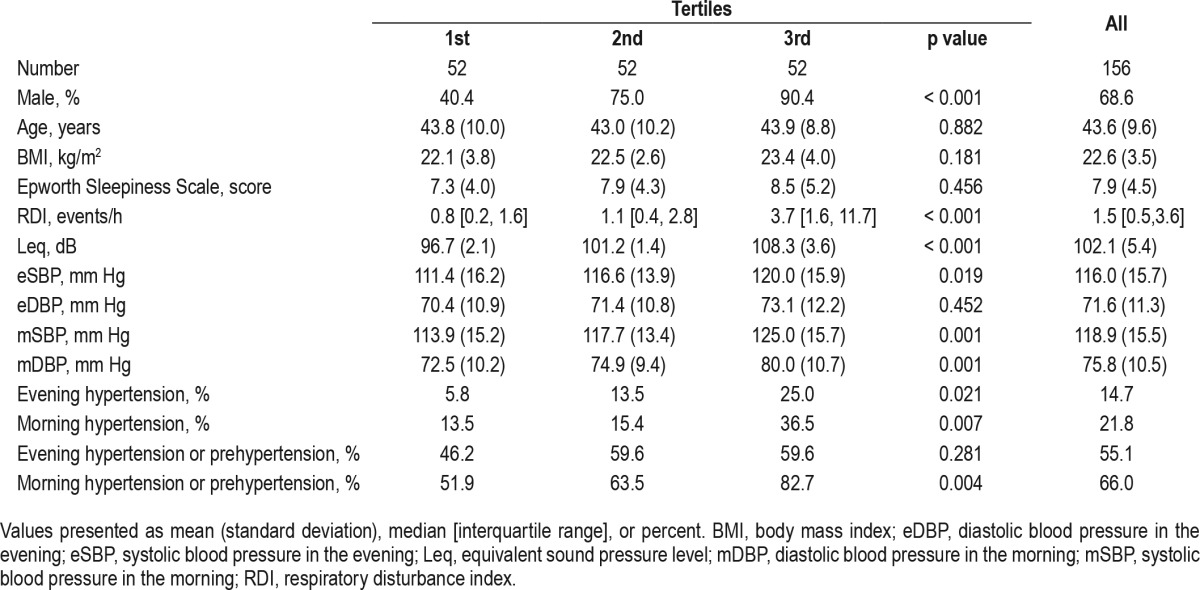
Table 1.
Characteristics of the subjects according to Leq tertiles.
We assessed a simple correlation between Leq and BP in the evening and the following morning. Thereafter, we performed multiple regression analysis to adjust for the confounding factors to identify the independent effect of Leq on BP. In our clinic-based study performed previously, we found that the relationship between Leq and high blood pressure is most prominent in non-obese and non-apneic subjects.15 As this finding was considered to be clinically important, we performed multiple regression analysis in non-obese, non-apneic subjects in the worker population. All statistical analyses were performed using the SPSS software package (version 17.0 for Windows; SPSS Inc., Chicago, Illinois, USA).
RESULTS
Subject Characteristics
The mean age of the subjects was 43.6 years, and the mean BMI was 22.6 kg/m2 (Table 1). Subjects were predominantly men (68.6%). There were 27 subjects (17.3 %) with an RDI ≥ 5 and 34 subjects (21.8%) and 23 subjects (14.7%) with morning and evening hypertension, respectively. Descriptive characteristics according to the Leq tertiles are summarized in Table 1. Subjects in the higher Leq tertiles tended to have higher BP than those in the lower Leq tertiles. BMI and RDI were also higher in subjects in the higher Leq tertiles compared with those in the lower Leq quintiles. Leq was modestly correlated with RDI (n = 156, r = 0.56, p < 0.001).
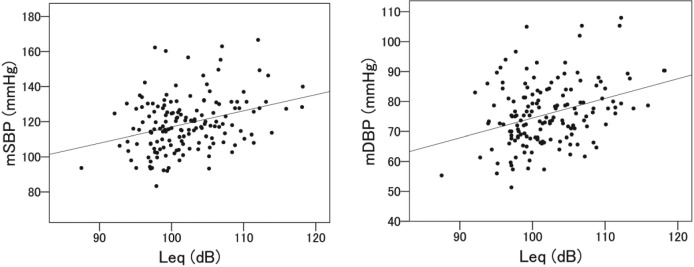
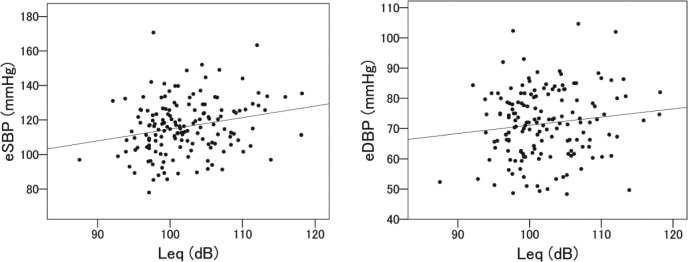
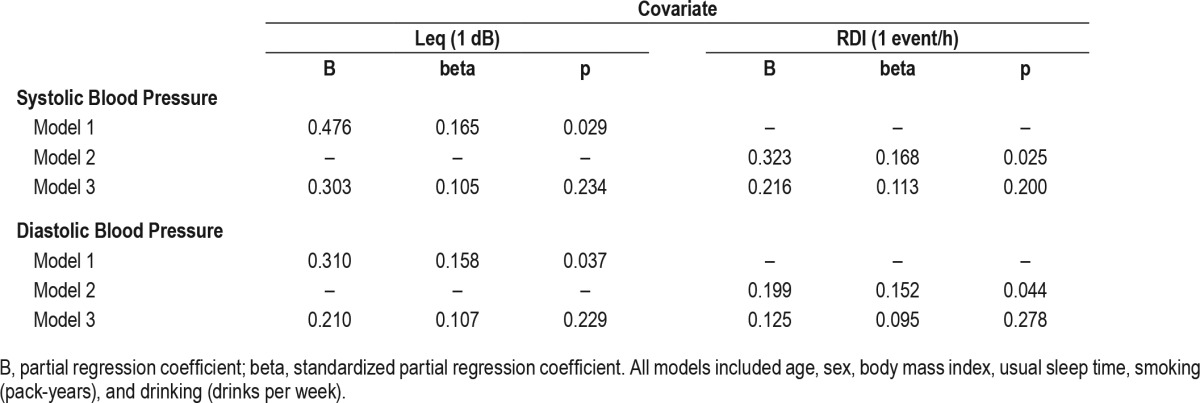
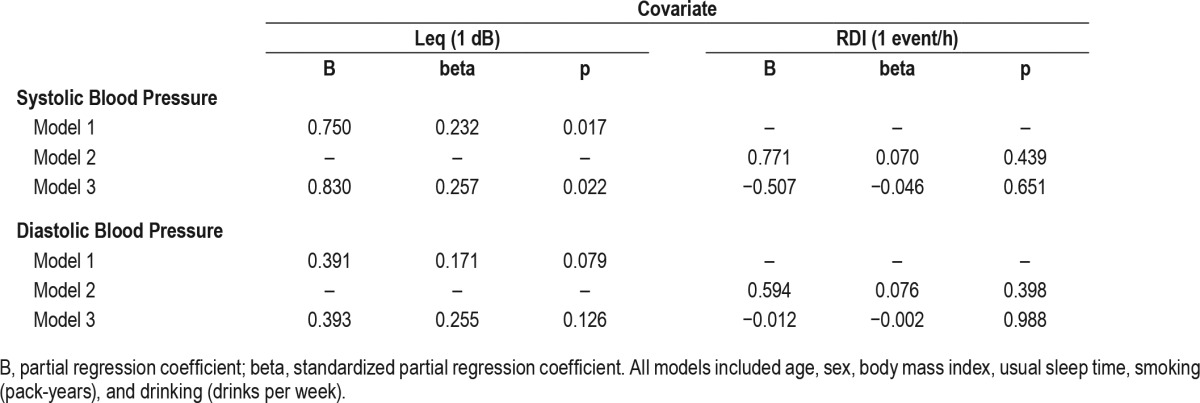
Relationship between Leq and Morning and Evening BP in All Subjects
In a simple correlation analysis, Leq was significantly related to mSBP and mDBP (r = 0.32, p < 0.001; r = 0.34, p < 0.001, respectively) (Figure 1) and to eSBP, but not to eDBP (r = 0.23, p = 0.004; r = 0.13, p = 0.11, respectively) (Figure 2). In a multiple regression analysis, if either variable of Leq or RDI was tested as an independent variable, it was significantly related to morning BP after adjustment for age, sex, and BMI (Table 2). However, the relationship was no longer significant when both RDI and Leq were included in the multiple regression model.
Figure 1. Relationship between tracheal sound intensity (Leq) and morning blood pressure.
mSBP, r = 0.32, p < 0.001; mDBP, r = 0.34, p < 0.001.
Figure 2. Relationship between tracheal sound intensity (Leq) and evening blood pressure.
eSBP, r = 0.23, p = 0.004; eDBP, r = 0.13, p = 0.11.
Table 2.
Multiple regression analysis for morning systolic blood pressure and morning diastolic blood pressure in all subjects.
Relationship between Leq and Morning and Evening BP in Non-Obese, Non-Apneic Subjects
We also reviewed the relationship between Leq and BP in non-obese, non-apneic subjects. The characteristics of this group are shown in Table 3.
Table 3.
Characteristics of the subjects according to RDI and BMI.
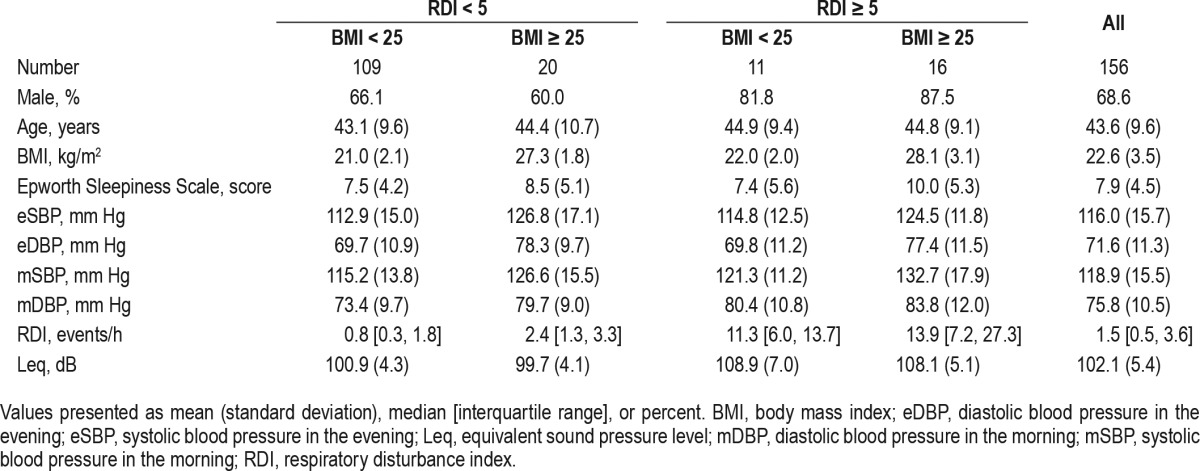
Leq was significantly related to both eSBP and eDBP (r = 0.33, p = 0.001; r = 0.23, p = 0.017, respectively). Leq was significantly related to both mSBP and mDBP (r = 0.38, p < 0.001; r = 0.33, p < 0.001, respectively).
We also performed a multiple regression analysis (Table 4). In this group, RDI had no effect on the relationship between Leq and BPs. The analysis showed a 5.0-mm Hg increase in mSBP associated with a 6-dB increase in Leq, which indicates a twofold increase in root mean square sound pressure.
Table 4.
Multiple regression analysis for morning systolic blood pressure and morning diastolic blood pressure in subjects with RDI of less than 5 and BMI of less than 25.
Secondary Analysis of Other Snoring Variables
We also examined the relationship of other snoring variables to morning BP in non-obese, non-apneic subjects. Variables related to snoring intensity were strongly related to morning BP after full adjustments for confounding factors. The top 1 percentile sound intensity (L1) and the percentage of time above 110 dB (% > 110 dB) were independently related to mSBP (β = 0.851, p = 0.008; β = 1.001, p = 0.010, respectively). Snoring time was not related to mSBP (p = 0.193).
DISCUSSION
We examined the relationship between Leq and morning BP in a worker population. We showed that Leq was independently related to morning systolic BP after adjusting for RDI and other confounding factors in non-obese, non-apneic subjects. This study suggests a possible independent effect of snoring on mSBP in non-apneic and non-obese subjects. Taking into account high prevalence of snoring, snoring can have very large population effects.
This study showed that Leq as well as RDI was related to BP after the adjustment for usual confounding factors. However, neither Leq nor RDI has significant association with BP if both RDI and Leq were added to the multiple regression model (Table 2). This result may be due to the co-dependence between Leq and RDI as well as the relatively small sample size. The co-dependence reflects well-known relationship between snoring sound intensity and OSA severity.18 In addition, the co-dependence might be enhanced by a methodological problem wherein both Leq and RDI were obtained from tracheal sound analysis. The subgroup analysis in non-apneic and non-obese subjects is free from the problem of co-dependence, and could show a statistically significant relationship between Leq and morning BP. Indeed, these findings are in line with our previous study in a relative large clinical population, which showed that the relationship between Leq and daytime BP was strongest in subjects without sleep apnea or obesity.15 The study using acoustical snoring analysis by Rich et al. also showed that objectively measured snoring has an independent association with all-cause mortality in subjects with apnea-hypopnea index (AHI) < 5 and BMI < 30.19 Accordingly, these results suggests that snoring has appreciable adverse effects on non-obese, non-apneic subjects.
Although we excluded subjects with current use of antihypertensive drug, more than 80% of subjects in highest Leq tertile have hypertension or at least prehypertension in the morning. Recently, several meta-analyses have shown that prehypertension is a risk factor of cardiovascular disease.20 Therefore, it is desirable to intervene into the cause of prehypertension to prevent the development of CVD. This highlights the therapeutic significance of snoring as well as sleep apnea.
Our study has some strengths and limitations. The strengths of our study include the availability of BP monitoring at home. Although we adopted office BP in our previous study, it is suggested that hypertension is diagnosed more accurately by measuring BP out of the office with home monitoring.21,22 In addition, home BP monitoring better predicts cardiovascular event risk compared with clinic BP monitoring.23 Further, we measured BP values in the morning. A heightened morning BP surge measured by ambulatory BP monitoring is considered a risk factor for cardiovascular disease events occurring in the morning as mentioned above.24 This study was based on a worker population, not a clinic population. Therefore, we were able to examine the significance of snoring intensity in asymptomatic subjects. Unlike the results of a clinic-based study, the finding of this study might be extended to the general population.
Several limitations in this study should be addressed. First, this study design was cross-sectional, which does not allow for causal inferences. Thus, longitudinal studies concerning the relationship between snoring and incidence of hypertension are needed. In addition, it is possible that the relationship between snoring and BP was mediated by unadjusted confounding factors, including visceral fat distribution. Second, we did not perform full polysomnography, which yields AHI and sleep time. Instead, we used TS-RDI, which has been shown to be strongly related to AHI,17 and we excluded time periods with body movement noises by reviewing the spectrogram to minimize the effect of inclusion of wake time on the snoring variables. However, the fact that both Leq and RDI came from the same source may be a weak point because it could cause additional co-dependence of both variables. Third, as our measurements did not include nocturnal oximetry, we could not exclude the effect of hypoxia. Finally, the BP measurements were not continuous, but were performed at one point. A future study using 24-hour BP monitoring is desirable to further clarify the relationship between snoring and BP.
In conclusion, we showed that TS intensity, as assessed by Leq, was independently related to morning BP in workers without sleep apnea or obesity. This study suggests a cardiovascular consequence of snoring through elevated morning BP. Further study, including a cohort study, is needed to understand the effect of snoring on BP.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- BP
blood pressure
- eSBP/eDBP
systolic and diastolic blood pressure in the evening
- Leq
equivalent sound pressure level
- mSBP/mDBP
systolic and diastolic blood pressure in the morning
- OSA
obstructive sleep apnea
- RDI
respiratory disturbance index
- TS
tracheal sound
REFERENCES
- 1.Lugaresi E, Cirignotta F. Some epidemiological data on snoring and cardiocirculatory disturbances. Sleep. 1980;3:221–2. doi: 10.1093/sleep/3.3-4.221. [DOI] [PubMed] [Google Scholar]
- 2.Palomäki H. Snoring and the risk of ischemic brain infarction. Stroke. 1991;22:1021–55. doi: 10.1161/01.str.22.8.1021. [DOI] [PubMed] [Google Scholar]
- 3.Koskenvuo M, Kaprio J, Telakivi T, et al. Snoring as a risk factor for ischemic heart disease and stroke in men. BMJ. 1987;294:16–9. doi: 10.1136/bmj.294.6563.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leineweber C, Kecklund G, Janszky I, et al. Snoring and progression: the Stockholm female coronary angiography study. Sleep. 2004;27:1344–9. doi: 10.1093/sleep/27.7.1344. [DOI] [PubMed] [Google Scholar]
- 5.Bixler EO, Vgontzas AN, Lin HM, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med. 2000;160:2289–95. doi: 10.1001/archinte.160.15.2289. [DOI] [PubMed] [Google Scholar]
- 6.Thomas GN, Jiang CQ, Lao XQ, et al. Snoring and vascular risk factor and disease in a low-risk population: the Guangzhou Biobank Cohort Study. Sleep. 2006;29:896–900. doi: 10.1093/sleep/29.7.896. [DOI] [PubMed] [Google Scholar]
- 7.Zamarrón C, Gude F, Otero Otero Y, et al. Snoring and myocardial infarction: a 4-year follow-up study. Respir Med. 1999;93:108–12. doi: 10.1016/s0954-6111(99)90299-8. [DOI] [PubMed] [Google Scholar]
- 8.Mateika JH, Kavey NB, Mitru G. Spontaneous baroreflex analysis in nonapneic snoring individuals during NREM sleep. Sleep. 1999;22:461–8. doi: 10.1093/sleep/22.4.461. [DOI] [PubMed] [Google Scholar]
- 9.Schöbel C, Fietze I, Glos M, et al. Nocturnal snoring decreases daytime baroreceptor sensitivity. Respir Med. 2014;108:1049–55. doi: 10.1016/j.rmed.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Cho JG, Witting PK, Verma M, et al. Tissue vibration induces carotid artery endothelial dysfunction: a mechanism linking snoring and carotid atherosclerosis? Sleep. 2011;34:751–7. doi: 10.5665/SLEEP.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Liu J, Wang W, et al. Association of self-reported snoring with carotid artery intima media thickness and plaque. J Sleep Res. 2012;21:87–93. doi: 10.1111/j.1365-2869.2011.00936.x. [DOI] [PubMed] [Google Scholar]
- 12.Mason RH, Mehta Z, Fonseca AC, et al. Snoring and severity of symptomatic and asymptomatic carotid stenosis: a population-based study. Sleep. 2012;35:1147–51. doi: 10.5665/sleep.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim J, Pack A, Maislin G, et al. Prospective observation on the association of snoring with subclinical changes in carotid atherosclerosis over four years. Sleep Med. 2014;15:769–75. doi: 10.1016/j.sleep.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Furukawa T, Nakano H, Hirayama K, et al. Relationship between snoring sound intensity and daytime blood pressure. Sleep Biol Rhythms. 2010;8:245–53. [Google Scholar]
- 15.Nakano H, Hirayama K, Sadamitsu Y, et al. Mean tracheal sound energy during sleep is related to daytime blood pressure. Sleep. 2013;36:1361–7. doi: 10.5665/sleep.2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asayama K, Ohkubo T, Kikuya M, et al. Prediction of stroke by self-measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the joint national committee 7 classification: the Ohasama study. Stroke. 2004;35:2356–61. doi: 10.1161/01.STR.0000141679.42349.9f. [DOI] [PubMed] [Google Scholar]
- 17.Nakano H, Hayshi M, Ohshima E, et al. Validation of a new system of tracheal sound analysis for the diagnosis of sleep apnea-hypopnea syndrome. Sleep. 2004;27:951–7. doi: 10.1093/sleep/27.5.951. [DOI] [PubMed] [Google Scholar]
- 18.Maimon N, Hanly PJ. Does snoring intensity correlate with the severity of obstructive sleep apnea? J Clin Sleep Med. 2010;6:475–8. [PMC free article] [PubMed] [Google Scholar]
- 19.Rich J, Raviv A, Raviv N, et al. An epidemiologic study of snoring and all-cause mortality. Otolaryngol Head Neck Surg. 2011;145:341–6. doi: 10.1177/0194599811402475. [DOI] [PubMed] [Google Scholar]
- 20.Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:17. doi: 10.1186/1741-7015-11-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mancia G, De Backer G, Dominiczak A, et al. Management of arterial hypertension of the European Society of Hypertension; European Society of Cardiology. 2007 Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and of the European Society of Cardiology. J Hypertens. 2007;25:1105–87. doi: 10.1097/HJH.0b013e3281fc975a. [DOI] [PubMed] [Google Scholar]
- 22.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–48. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Stergiou GS, Siontis KC, Ioannidis JP. Home blood pressure as a cardiovascular outcome predictor: it's time to take this method seriously. Hypertension. 2010;55:1301–3. doi: 10.1161/HYPERTENSIONAHA.110.150771. [DOI] [PubMed] [Google Scholar]
- 24.Kario K. Morning surge in blood pressure and cardiovascular risk evidence and perspectives. Hypertension. 2010;56:765–73. doi: 10.1161/HYPERTENSIONAHA.110.157149. [DOI] [PubMed] [Google Scholar]