Abstract
Alzheimer's disease (AD) is a multifactorial, progressive neurodegenerative disorder with a poor prognosis, and thus, novel therapies for AD are certainly needed in a growing population of elderly patients or asymptomatic individuals, who are at risk for AD, worldwide. It has been established that some AD biomarkers such as amyloid-beta load in the brain, precede the onset of the disease, by approximately 20 years. Therefore, the therapy to prevent or effectively treat AD has to be initiated before the emergence of symptoms. A goal of this review is to present the results of recent clinical trials on monoclonal antibodies against amyloid beta, used for the treatment of AD and also to address some of the current challenges and emerging strategies to prevent AD. In recent trials, a monoclonal antibody, i.e. solanezumab has shown some beneficial cognitive effects among mild AD patients. Ongoing studies with gantenerumab and crenezumab will examine when exactly the AD treatment, aimed at modifying the disease course has to be started. This review was based on Medline database search for trials on passive anti-AD immunotherapy, for which the main timeframe was set from 2012 to 2015.
Key words: Alzheimer's disease, amyloid-beta, clinical trials, immunotherapy, monoclonal antibodies
Alzheimer's disease (AD) is a progressive neurodegenerative disorder, associated with dysregulation of several biologic pathways due to genetic, epigenetic, and environmental causes.[1] AD can exist in two variants, including the more common late-onset AD and an early-onset AD.[1] Present treatments available for AD are limited to symptomatic management that consist mostly of acetylcholinesterase inhibitors (including donepezil, galantamine, and rivastigmine) and the N-methyl-D-aspartate receptor antagonist - memantine). Prognosis in AD is poor, and thus, novel therapies for AD are certainly needed in a growing population of elderly patients or among asymptomatic individuals, who are at risk for AD, worldwide.[1] Current research studies are focused on exploring potential innovative therapies, to assess whether or not it is possible to modify the AD course. If the future treatments, designed to reduce the risk, postpone or even prevent the clinical onset of AD are going to be found, then the most accurate methodology to diagnose AD in the early stage, and to assess the safety and effectiveness of emerging AD treatments (including psychometric tests, biomarkers, procedures to expedite the initiation, and conduction of AD trials), as well as a large number of well-matched participants for these studies will be necessary.[2] Moreover, a recent knowledge about the AD pathology, and its specific genes and biomarkers can help stratify many asymptomatic individuals (often unaware of their AD risk) into groups with higher or lower risk of further cognitive deterioration, or full-blown dementia of AD or other types.[1,2]
At the present time, no effective disease-modifying therapies are available in clinical practice. This is related to the fact that the roots of AD are likely to go back decades before the afflicted individuals present with the first symptoms of the disease, and the traditional cognitive outcomes developed for clinical trials in AD are not well suited for the prevention AD trials.[1,2] Pathological processes in the brain of patients with AD start silently (approximately 10–20 years before any clinical manifestation), and so establishing an early diagnosis of AD, possibly in its prodromal stage, or among asymptomatic individuals, harboring AD-related genetic mutations, is extremely important. It is crucial to identify patients who have some risk factors for AD (e.g.: Diabetes mellitus, cardiovascular disease, arterial hypertension, and cerebrovascular events). Modification of these risk factors for AD and ongoing medication reviews (to simplify therapeutic regimens) can contribute to improvement of the mental and physical condition of such patients.[3]
The hallmarks of AD include senile plaques (a microtubule-associated amyloid beta protein, forming extracellular aggregates) and neurofibrillary tangles (NFTs) (filaments of hyperphosphorylated tau protein, creating intraneuronal protein clusters).[4] Amyloid-beta and tau protein, as a “signature” of AD, have inspired modern research to develop some immunotherapeutic strategies, in attempt to slow down or postpone the disease process.[1,5] Senile plaques consist of a proteinaceous core, composed of amyloid fibrils, surrounded by dystrophic neurons, astrocytes, and microglial cells. The amyloid precursor protein (APP) is cleared enzymatically by beta secretase and gamma secretase.[6] Products of this reaction include two forms of the amyloid beta peptide: (1) A chain containing 40 amino acids (the main form), and (2) a chain containing 42 amino acids (amyloid beta 1–42).[7] The amyloid beta 1–42 is more prone to aggregate into fibrils, which are the main components of cerebral neurotoxic senile plaques, characteristic for AD.[8] According to the “amyloid cascade hypothesis” that has been a cornerstone of the AD etiology for the last 20 years, the amyloid-beta deposition in the brain precipitates the formation of NFTs.[1,5,9] However, the precise way, in which the cerebral deposition of amyloid beta leads to the formation of NFTs still remains unclear. It is conceivable that the senile plaques and NFTs may develop independently, or can represent the products of neurodegeneration in AD, rather than the AD causes.[1,5,10] Since the senile plaque number is not well correlated with the severity of dementia,[11] in contrast to the soluble oligomeric forms of amyloid beta,[12] the amyloid cascade hypothesis has been reformulated, with a particular focus on soluble amyloid beta aggregates as the major neurotoxic structures that impair synaptic communication, leading to deterioration of cognition and memory, in patients with AD.[5,10,13] Among diverse amyloid beta species, the oligomeric amyloid beta, and amyloid beta-derived diffusible ligands (ADDLs) have been implicated in cognitive decline, according to recent evidence.[14] Moreover, some recent trials conducted in the patient population with familial[15] and sporadic AD[16] have revealed a long preclinical phase (approximately 20 years before the onset of dementia), during which the amyloid beta deposition process has been progressing very slowly. This suggests that in both asymptomatic genetic forms of AD, and in cognitively normal individuals prevention trials should be conducted, in search of safe and effective disease-modifying approaches to the AD treatment.[6] Anti-amyloid strategies for treating AD have appeared on the horizon over the last 10 years. These approaches are focused on reducing production (via gamma secretase and beta secretase inhibitors) or enhancing clearance (via monoclonal antibodies) of the neurotoxic amyloid beta. Monoclonal antibodies vary by immunoglobulin G (IgG) class, and some of them bind soluble amyloid beta, and the others bind the senile plaques. At present, immunotherapy represents one of the most innovative approaches to AD treatment and includes passive vaccinations (anti-amyloid-beta antibodies) and active vaccinations (amyloid beta antigens).[17,18] This review was based on Medline database search for trials on passive anti-AD immunotherapy, for which the main timeframe was set from 2010 to 2015. This search was supplemented with some information from cross references (cited in the bibliography of relevant articles). Publications focused on ongoing AD prevention clinical trials, investigating novel agents for passive immunization, as well as target populations (such as patients with prodromal, asymptomatic, or mild stages of AD), were analyzed and then included.
Bapineuzumab and Solanezumab - the first Anti-Amyloid Beta Monoclonal Antibodies
Passive immunization with the humanized monoclonal antibodies, bapineuzumab and solanezumab, has been evaluated in several, large-scale phase three clinical trials in AD patients.[19,20] However, many of these trials have failed to achieve their projected endpoints.[21] Bapineuzumab is the humanized monoclonal antibody, directed against the N-terminus of amyloid beta that recognizes the amyloid beta 1–5 region.[19,21] In a phase 2 clinical trial, the occurrence of amyloid-related imaging abnormalities (ARIA) detected by magnetic resonance imaging (MRI) of the brain,[22] in particular, vasogenic edema among bapineuzumab-treated mild to moderate AD patients (which was increased in apolipoprotein E epsilon 4 [APOE e4] carriers) was an important adverse effect of this therapeutic.[23] Simultaneously, in another phase 2 double-blind, placebo-controlled, ascending dose study conducted in mild-to-moderate AD patients, bapineuzumab was shown to lower the brain amyloid beta burden assessed by 11C Pittsburgh compound B positron emission tomography (PET) amyloid imaging (which is a marker of cortical fibrillar amyloid-beta load).[24] In post hoc analysis of two phase 2 trials on bapineuzumab, evaluating cerebrospinal fluid (CSF) biomarker (amyloid beta, and tau protein) levels in mild-to-moderate AD patients, the main study outcomes were slightly different for CSF tau protein (tau protein was lower in the treatment group). However, there was no difference in the CSF amyloid beta level between the treatment and placebo groups.[25] Similarly, no significant clinical benefits have been reported in two large phase three trials, leading in consequence to the discontinuation of all phase 3 clinical trials on bapineuzumab, in mild-to-moderate AD patients, in 2012.[25] In addition, it was reported that bapineuzumab failed to meet primary study endpoints, including changes in cognitive scores and functional performance, compared with placebo, in AD patients who were both APOE e4 carriers and noncarriers.[25] Although all phase 3 trials on bapineuzumab have ended, two phase 1 clinical trials in mild-to-moderate AD patients (ClinicalTrials.gov Identifiers: NCT01193608 and NCT01369225) are still ongoing [Table 1], to test the safety and tolerability of the re-engineered version of bapineuzumab (AAB-003), aimed at reducing the risk of ARIAs.[26]
Table 1.
Passive immunotherapy for Alzheimer's disease: Anti-amyloid beta monoclonal antibodies-novel medications and their current status, based on clinical trials
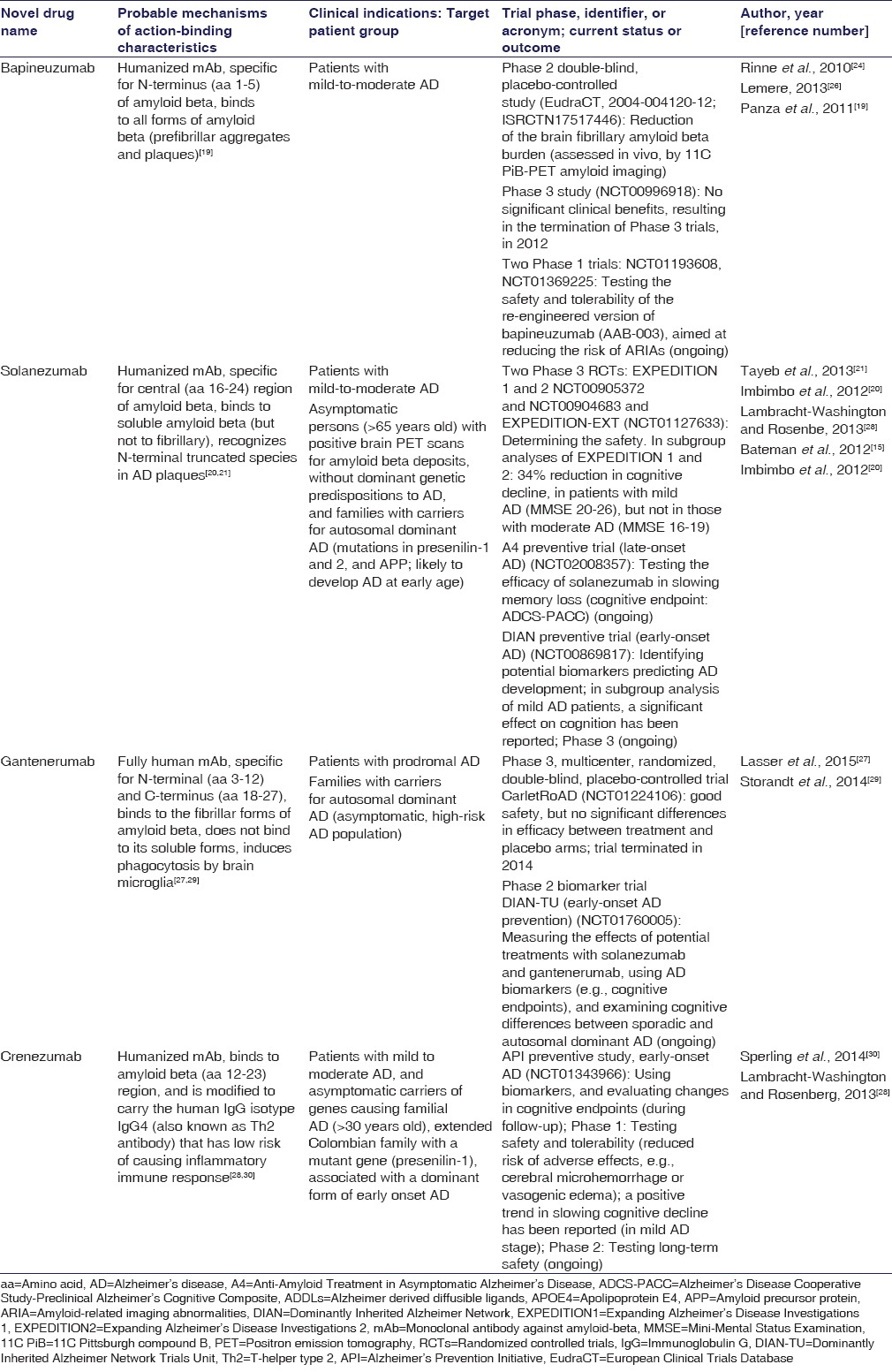
Solanezumab is an anti-amyloid beta monoclonal antibody, directed against the amyloid beta 13–28 region, and able to recognize various N-terminal truncated species (e.g., amyloid beta 3–42), which are often present in AD senile plaques.[20,21] Solanezumab has demonstrated preferential binding to soluble amyloid beta, but not to fibrillar amyloid beta.[21] Two large randomized, double-blind, controlled phase 3 trials of solanezumab: EXPEDITION1 (Expanding Alzheimer's Disease Investigations 1) and EXPEDITION2 (ClinicalTrials.gov Identifiers: NCT00905372 and NCT00904683) have involved over 2050 patients with mild-to-moderate AD, and as a follow-up of these trials, an open-label extension, EXPEDITION-EXIT trial (ClinicalTrials.gov Identifier: NCT01127633) has been conducted to determine the long-term safety of solanezumab [Table 1].[21] In 2012, it was reported that the cognitive and functional study outcomes were not met in either of the two EXPEDITION trials. In particular, the EXPEDITION1 trial did not meet primary cognitive and functional endpoints in the overall mild-to-moderate AD patient population. However, the prespecified secondary subgroup analyses of pooled data, across both studies (EXPEDITION1 and EXPEDITION2), showed a statistically significant 34% reduction in cognitive decline, in patients with mild AD (Mini-Mental Status Examination [MMSE] score of 20–26), but not in the ones with moderate AD (MMSE of 16–19).[21] Simultaneously, an independent analysis by the Alzheimer's Disease Cooperative Study (ADCS) confirmed these beneficial findings.[21] Furthermore, the biomarker analysis has shown an increase in plasma amyloid beta levels of AD patients suggesting that this toxic protein was removed from the brain. There were no significant changes in other AD biomarkers.[21] Adverse events that occurred more often in the solanezumab group than in the placebo group included lethargy, rash, and malaise in EXPEDITION1 and angina in EXPEDITION2. Two ongoing phase 3 trials on solanezumab: The open-label extension study EXPEDITION-EXT (ClinicalTrials.gov Identifier: NCT01127633) and the EXPEDITION3 (ClinicalTrials.gov Identifier: NCT01900665) in mild AD patients will hopefully provide new data, on cognitive performance in the early stage of AD.[21]
Preventive Clinical Trials Targeting the Presymptomatic Alzheimer's Disease Stage – focus on Solanezumab, Gantenerumab, and Crenezumab
Currently, new preventive trials (started in 2013, and projected for the next 3 years) on the anti-amyloid beta monoclonal antibodies: Solanezumab, gantenerumab, and crenezumab [Table 1] are going to investigate the research question: When exactly the early AD treatment should be initiated?[15,20,21,28] To target patients in the presymptomatic AD stage, there are now six large-scale AD prevention trials that represent the pioneering AD prevention-oriented therapeutic efforts. Four of them are now underway, and two will start shortly.
Gantenerumab is a fully human monoclonal antibody that binds to the fibrillar forms of amyloid beta and induces their phagocytosis by brain microglia. In patients with prodromal AD, participating in Scarlet RoAD trial (NCT01224106) (a phase 3, multicenter, randomized, double-blind, placebo-controlled trial), gantenerumab was well tolerated. However, no significant differences in primary efficacy endpoints between treatment and placebo arms were observed. Subsequently, in December 2014, this trial was terminated.[27]
Crenezumab is the murine monoclonal antibody that binds to amyloid beta 12–23 and is modified to carry the human IgG isotype IgG4 (also known as Th2 antibody). The Th2 antibody is characterized by a low probability of causing inflammatory immune response. In phase 1 clinical study, patients with mild-to-moderate AD, treated with crenezumab, had a decreased risk of adverse effects such as cerebral microhemorrhage and vasogenic edema. In addition, a positive trend in slowing cognitive decline in patients with mild AD stage was observed. However, no effect on global functioning was noted.[28]
The A4 Study (The Anti-Amyloid Treatment in Asymptomatic Alzheimer's Disease)
The A4 study is exploring the impact of novel therapies on long-term neurodegenerative changes related to the amyloid beta [Table 1]. The A4 preventive study (late-onset AD), as a part of the Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) trials, is going to test the efficacy of solanezumab in slowing memory loss.[28] The primary cognitive endpoint of the A4 study is the rate of change on a cognitive composite (assessed with ADCS-Preclinical Alzheimer's Cognitive Composite), for 3 years, among 500 patients above 65 years of age, without a dominant genetic predisposition to AD, with positive brain PET scans for amyloid beta deposits but without clinical symptoms of AD.[28] In addition, some participant reported endpoints, as well as CogState (an assessment on AD Scale-cognitive subscale) and two episodic memory tests, will also be measured. It should be highlighted that the A4 study will examine both PET amyloid imaging and MRI (structural and functional) in all patients. In addition, in a subgroup of participants, CSF measures and Tau PET imaging (allowing to test the hypothesis that lowering the amyloid-beta load, if implemented in early AD stage, can prevent the spread of Tau protein into the neocortex) will be evaluated. It is expected that the comparison of the A4 placebo arm and the LEARN arm will provide important information on the individual risk of cognitive decline associated with the amyloid beta accumulation, and other factors that can impact cognitive impairment (without excessive amyloid beta deposits).[28]
The DIAN-TU study (the Dominantly Inherited Alzheimer Network Trials Unit) [Table 1] is measuring the effects of potential treatments with anti-amyloid beta monoclonal antibodies, using AD biomarkers (phase 2 biomarker trial). The DIAN trial[15,20] is going to analyze individuals, who are carriers of autosomal dominant genetic mutations in presenilin-1, presenilin-2, and APP mutations, which makes it very likely that they will develop AD at an early age. Two different treatment agents: Solanezumab and gantenerumab (DIAN-TU, ClinicalTrials.gov Identifier: NCT01760005) will be examined in this asymptomatic, high-risk AD population.[29] The DIAN trial that is focused on early-onset AD prevention is also planned to evaluate cognitive endpoints, and to examine cognitive differences between sporadic and autosomal dominant AD.[29]
The API study (the Alzheimer's Prevention Initiative)
The API study is focused on prevention (early-onset AD) [Table 1] with a particular attention to the healthy individuals, who (based on their genetic background and age) are at the highest risk for developing AD. The Alzheimer's Prevention Initiative (API) trial with crenezumab is being conducted among 300 asymptomatic individuals, 30 years of age and older, from a large Colombian family, with a mutant gene (presenilin-1 E280A), associated with a dominant form of early onset AD. This particular mutation leads to an early and increased cerebral amyloid beta 1–42 plaque deposition, at a young age.[30] Furthermore, around age 50, the presenilin-1E280A mutation is associated with a progressive decline in cognition and level of functioning. In these cases, clinical features of the early-onset AD are present decades earlier, comparing with the typical sporadic AD cases.[31] The API trial will utilize biomarker outcomes (in phase 1) and will evaluate changes in cognitive test scores (as endpoints) during follow-up.
Lessons Learned from the Past Unsuccessful Immunotherapy Trials
Many of the previous unsuccessful immunotherapy studies revealed that in patients with the mild-to-moderate AD (in whom most clinical progression trials had been conducted), it was too late in the disease process, to stop the progression in neurodegeneration since some irreversible damage to the brain might have already occurred. A decade ago, it was reported that passive immunotherapy, selectively directed at the oligomeric amyloid-beta, and at the ADDLs could produce beneficial learning and memory effects (in animals), without changing the monomeric amyloid beta.[32] Although in the past, several monoclonal antibodies failed to reach their primary clinical endpoints in humans, some recent trial data (phase 3) on solanezumab suggest that this antibody is superior to placebo, in mild AD patient population.[33] It should be noted that the therapeutic success of aducanumab may be related to including into this trial, the patients with AD diagnosed with the use of amyloid PET scans. It is possible that this particular improvement in the diagnostic accuracy contributed to meeting of the trial endpoints.[34] Moreover, PET scans used to detect amyloid beta plaques in AD were positive only in approximately 77% of cases that were categorized as AD.[34] This may also partially explain the reason why some previous studies failed to demonstrate the benefits of monoclonal antibodies. It is possible that if the monoclonal antibodies were used in patients with incorrect diagnosis of AD (without confirmed amyloid beta pathology by a PET scan), they could not target the amyloid beta plaque.[34] Furthermore, a study (phase 1b) with aducanumab has revealed a dose-related response in removing the amyloid beta deposits (measured by the Standard Uptake Value Ratio of florbetapir) and also has confirmed that this antibody not only achieves its molecular target but also contributes to some cognitive clinical benefits (such as reduced rate of cognitive decline, assessed by both the MMSE and Clinical Dementia Rating Scale - sum of boxes scores), raising some hope among AD patients.[35] Similarly, based on the data from the ADCS, solanezumab (that targets the monomeric amyloid beta and has a very good safety profile) has revealed a 34% reduction in the rate of cognitive decline, comparing to placebo, in patients with mild AD.[36]
New Hope for Rare Familial Cases of Alzheimer's Disease
The rare familial cases of AD consist of about 3% of all AD dementias.[1,2] However, when they occur in patients, who have the genetic mutation, the chance of getting AD is 100%, with a long lifespan.[37] For this particular group of patients (and their families or caregivers), it is optimistic and useful to know that there are ongoing clinical trials, investigating the use of monoclonal antibodies directed against the beta-amyloid-forming plaques in the brain.[37] In addition, there are ongoing trials conducted in persons, who are at a higher AD risk, due to genetic variations, including the APOE e4 genotype, and in individuals, who have biomarkers, suggestive of the amyloid beta presence in the brain, in whom the AD pathology may be developing.[37] Moreover, in these high-risk populations, new studies are in process, to investigate the monoclonal antibodies directed against amyloid-beta, or to explore active vaccines, and beta APP cleaving enzyme inhibitors, which block the transformation of the APP to neurotoxic forms of amyloid beta.[38] Furthermore, a randomized, double-blind, placebo-controlled, first-in-human study that examines the safety, tolerability, and antibody response of active amyloid-beta immunotherapy with CAD106, in patients with AD, has been conducted.[39] Currently, a few novel anti-amyloid beta monoclonal antibodies, with properties distinct from bapineuzumab and solanezumab, are being studied in various stages of clinical development. It is expected that the outcomes from the ongoing prevention trials will provide some evidence whether or not the passive or active anti-amyloid beta immunotherapy can prevent or delay the onset of AD in high-risk populations.
Challenges, Opportunities, and Emerging Strategies in Alzheimer's Disease Prevention Trials
In 2011, the Collaboration for Alzheimer's Prevention (CAP) that was created as a consensus - building and harmonizing initiative, designed to help advance AD prevention research.[2] CAP has integrated knowledge and experience of the scientific leaders in the field, to promote AD prevention.[2] CAP includes investigators from the Anti-Amyloid Treatment in Asymptomatic Alzheimer's Disease (A4) Study, the DIAN-TU, and the API, as well as representatives from the US Food and Drug Administration, the National Institute on Aging, the Alzheimer's Association, and the Fidelity Biosciences Research Initiative.[15,29,30]
The Impact of Collaboration for Alzheimer's Prevention on the Goals and Designs of Prevention Alzheimer's Disease Trials
It is expected that the scientific collaboration within CAP will allow to gain a potential insight into the earliest phases of cognitive deterioration in AD, through various strategies, to expand target population with elevated risk for AD (that can particularly benefit from the novel or emerging AD therapies).[2] Furthermore, CAP addresses some key issues relevant to the methodology of the recruitment of participants in clinical trials, initial testing procedures, and follow-up assessments over time, as well as selection of final outcome measures used for these prevention trials.[1,2,5] In these research endeavors, the Global Alzheimer's Association Interactive Network provides additional support by sharing comprehensive data sets, resources, and expertise (in reducing the risk or delaying the onset of AD).[2] To efficiently evaluate the range of some promising emerging therapies in AD, certain modern biomarkers including volumetric MRI, amyloid PET brain imaging, CSF analysis for amyloid beta, and tau protein levels, genetic tests focused on APOE e4 for homozygotes (and possibly heterozygotes), and presenilin 1 mutation (in carriers from the early-onset AD extended Colombian family), cognitive endpoints based on psychometric scales, and other parameters to monitor some of the earliest changes, related with the predisposition to AD, have currently been used.[1,5] To further explore this field and to establish the future treatment guidelines, the large-scale prevention trials are warranted, in patients with high AD risk.[5]
The Role of Genematch Program in Recruitment of Volunteers With Apolipoprotein E Epsilon 4 Genetic Status to Alzheimer's Disease Research Studies
One of the most potent risk factors for sporadic AD is carrier status of the epsilon 4 (e4) allele of the APOE gene. APOE e4 carriers show a differential response to many therapies, which are being investigated as AD treatments.[40] Understanding the reasons, behind differential treatment responses of the APOE e4 carriers, may help elucidate some neurodegenerative mechanisms in AD, and also, can partially explain why some treatments lead to positive or negative effects in various clinical trials. The GeneMatch program, which is designed to identify volunteers interested in participating in AD research, on the basis of their APOE e4 genetic status (and other risk factors for AD), is going to help with recruitment since it focuses on a precise inclusion criterion, allowing to match candidates with prevention studies. The APOE e4 gene is considered to be the major genetic risk factor for late-onset AD (among persons over 60 years of age). However, many individuals who have two copies of the e4 allele, very often, due to lack of symptoms, remain unaware of their impending AD risk.[40] Therefore, the APOE database, used in the GeneMatch program, will expedite recruitment of sufficiently large number of candidates in the early stages of AD. This, in turn, will help with the development of therapies that may slow down the progressive process of AD, at its earnest stages.[40] To spread awareness of early AD research, and to facilitate enrollment into AD clinical studies in the community, the Alzheimer's Prevention Registry was created, serving as a web-based recruitment program.[1] To further coordinate these actions, the patient-friendly website: www.endALZnow.org/GeneMatch (including instructional video and consent forms) has been created. Furthermore, the individuals, who intend to join the program, will be provided with a cheek swab kit, which needs to be returned to the laboratory, together with a patient's sample for APOE genetic testing.
Cost Considerations and Compliance Concerns With Injectable Immunotherapy for Alzheimer's Disease Prevention
Unquestionably, AD is a devastating illness with an enormous economic impact, both direct (e.g., medical long-term care expenses) and indirect (e.g., loss of professional employment, or income, among families members caring for disabled AD patients) on the health-care system and the society. Currently, about 35 million people worldwide live with AD, and this number is expected to reach 115 million by 2050.[41] At present, the AD-related expenses are projected to be close to 215 billion US dollars, and in the future (by 2040), they are estimated to increase to approximately 500 billion US dollars annually.[42] Of course, almost incalculable costs of caregiver burden including their physical, mental, emotional, and economic strain should also be added. However, to more accurately describe the AD progression, and its adverse consequences, a model called “dependence” (loss of autonomy, reliance on others for care, and basic needs) has been introduced.[43] This unifying model is helpful for more comprehensive appraisal of medical costs, resource utilization, and quality of life of AD patients or their families. Moreover, the dependence might be considered as one of the predictors of AD patient disability and caregiver burden.[43]
The staggering costs of long-term management of AD patients call for novel preventive, diagnostic, and therapeutic approaches. In fact, a multistep process of the discovery and development requires approximately 1.8 billion US dollars, and about 10–15 years, until a new investigational agent can be approved to the market.[44] Under these circumstances, passive amyloid-beta immunotherapy appears to be a reasonable option for the health-care budget. One of the challenges of anti-amyloid beta monoclonal antibodies is their injectable form of delivery. This might be viewed as inconvenient, by both patients and their caregivers, and as such, it could have a negative impact on compliance. However, despite this concern, there is a reasonable hope that the patients with early AD, as well as their families and caregivers, can be particularly motivated to adhere to this novel therapy, while “inconvenient” injections (e.g., monthly intravenous infusion for 3 years, as in case of solanezumab, in the A4 study, or subcutaneous injections every 2 weeks for 260 weeks of crenezumab, in the API study)[45] can be interpreted as a relatively “small price to pay,” considering an improved functioning. Since these agents are still investigated in clinical trials, a “real world” patient compliance to them is not known yet.[45] It can be expected that clear communication with regard to novel treatments for AD, possible beneficial effects, and safety issues, as well as the patient confidence in medical personnel and research investigators should enhance compliance with these new medicines.[46] Furthermore, patient and caregiver engagement in educational activities and support groups can be another motivating factor, and even small successes in slowing down cognitive decline should further reinforce adherence to novel anti-AD therapy. In addition to local resources, the Alzheimer's Disease Education and Referral Center represents one of the reliable sources of accurate information about AD (e.g., evidence-based new treatments or diagnostic tools).
Conclusion
Based on a growing body of knowledge of the genetics and molecular pathogenesis of AD, indicating that the pathophysiological brain alterations occur many years before the onset of cognitive decline; this review of therapeutic concepts focused on anti-amyloid beta monoclonal antibodies was undertaken. It should be highlighted that solanezumab has already shown some beneficial cognitive effects in mild AD patients, and prevention trial on crenezumab will examine when exactly the AD treatment should be started (e.g., in presymptomatic AD individuals, who harbor AD-related genetic mutations, or patients with prodromal AD stages) to yield beneficial outcomes. Furthermore, a spectrum of plaque-associated targets for AD therapies has broadened, and it appears that multimodal therapies targeting amyloid beta accumulation, tau protein malformation, or their combination can modify the AD course. Although a potential translation of promising research results into effective medications for AD has been very challenging, hopefully, in the near future, therapeutic advances in AD might stem the tide of this dreadful disease, robing the expanding number of patients, worldwide, from their mental and physical health, dignity, and independence.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Apter JT, Shastri K, Pizano K. Update on disease-modifying/preventive therapies in Alzheimer's disease. Curr Geriatr Rep. 2015;4:312–7. doi: 10.1007/s13670-015-0141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiman EM, Langbaum JB, Tariot PN, Lopera F, Bateman RJ, Morris JC, et al. CAP – Advancing the evaluation of preclinical Alzheimer disease treatments. Nat Rev Neurol. 2016;12:56–61. doi: 10.1038/nrneurol.2015.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller G. Alzheimer's research. Stopping Alzheimer's before it starts. Science. 2012;337:790–2. doi: 10.1126/science.337.6096.790. [DOI] [PubMed] [Google Scholar]
- 4.Newell KL, Hyman BT, Growdon JH, Hedley-Whyte ET. Application of the National Institute on Aging (NIA)-Reagan Institute criteria for the neuropathological diagnosis of Alzheimer disease. J Neuropathol Exp Neurol. 1999;58:1147–55. doi: 10.1097/00005072-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hampel H, Schneider LS, Giacobini E, Kivipelto M, Sindi S, Dubois B, et al. Advances in the therapy of Alzheimer's disease: Targeting amyloid beta and tau and perspectives for the future. Expert Rev Neurother. 2015;15:83–105. doi: 10.1586/14737175.2015.995637. [DOI] [PubMed] [Google Scholar]
- 6.Panza F, Solfrizzi V, Frisardi V, Capurso C, D’Introno A, Colacicco AM, et al. Disease-modifying approach to the treatment of Alzheimer's disease: From alpha-secretase activators to gamma-secretase inhibitors and modulators. Drugs Aging. 2009;26:537–55. doi: 10.2165/11315770-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Seubert P, Vigo-Pelfrey C, Esch F, Lee M, Dovey H, Davis D, et al. Isolation and quantification of soluble Alzheimer's beta-peptide from biological fluids. Nature. 1992;359:325–7. doi: 10.1038/359325a0. [DOI] [PubMed] [Google Scholar]
- 8.Iwatsubo T, Odaka A, Suzuki N, Mizusawa H, Nukina N, Ihara Y. Visualization of A beta 42(43) and A beta 40 in senile plaques with end-specific A beta monoclonals: Evidence that an initially deposited species is A beta 42(43) Neuron. 1994;13:45–53. doi: 10.1016/0896-6273(94)90458-8. [DOI] [PubMed] [Google Scholar]
- 9.Hardy J, Allsop D. Amyloid deposition as the central event in the aetiology of Alzheimer's disease. Trends Pharmacol Sci. 1991;12:383–8. doi: 10.1016/0165-6147(91)90609-v. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong RA. The pathogenesis of Alzheimer's disease: A reevaluation of the “amyloid cascade hypothesis”. Int J Alzheimers Dis. 2011;2011:630865. doi: 10.4061/2011/630865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terry RD. Alzheimer's disease and the aging brain. J Geriatr Psychiatry Neurol. 2006;19:125–8. doi: 10.1177/0891988706291079. [DOI] [PubMed] [Google Scholar]
- 12.Borutaite V, Morkuniene R, Valincius G. Beta-amyloid oligomers: Recent developments. Biomol Concepts. 2011;2:211–22. doi: 10.1515/bmc.2011.019. [DOI] [PubMed] [Google Scholar]
- 13.Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, et al. Amyloid-beta protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory. Nat Med. 2008;14:837–42. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koffie RM, Meyer-Luehmann M, Hashimoto T, Adams KW, Mielke ML, Garcia-Alloza M, et al. Oligomeric amyloid beta associates with postsynaptic densities and correlates with excitatory synapse loss near senile plaques. Proc Natl Acad Sci U S A. 2009;106:4012–7. doi: 10.1073/pnas.0811698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bateman RJ, Xiong C, Benzinger TL, Fagan AM, Goate A, Fox NC, et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N Engl J Med. 2012;367:795–804. doi: 10.1056/NEJMoa1202753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, et al. Australian Imaging Biomarkers and Lifestyle (AIBL) research group. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: A prospective cohort study. Lancet Neurol. 2013;12:357–67. doi: 10.1016/S1474-4422(13)70044-9. [DOI] [PubMed] [Google Scholar]
- 17.Panza F, Frisardi V, Solfrizzi V, Imbimbo BP, Logroscino G, Santamato A, et al. Immunotherapy for Alzheimer's disease: From anti-ß-amyloid to tau-based immunization strategies. Immunotherapy. 2012;4:213–38. doi: 10.2217/imt.11.170. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Liu Y, Wang Z, Jiang Y. Clinical trials of amyloid-based immunotherapy for Alzheimer's disease: End of beginning or beginning of end? Expert Opin Biol Ther. 2013;13:1515–22. doi: 10.1517/14712598.2013.838555. [DOI] [PubMed] [Google Scholar]
- 19.Panza F, Frisardi V, Imbimbo BP, Seripa D, Paris F, Santamato A, et al. Anti-ß-amyloid immunotherapy for Alzheimer's disease: Focus on bapineuzumab. Curr Alzheimer Res. 2011;8:808–17. doi: 10.2174/156720511798192718. [DOI] [PubMed] [Google Scholar]
- 20.Imbimbo BP, Ottonello S, Frisardi V, Solfrizzi V, Greco A, Seripa D, et al. Solanezumab for the treatment of mild-to-moderate Alzheimer's disease. Expert Rev Clin Immunol. 2012;8:135–49. doi: 10.1586/eci.11.93. [DOI] [PubMed] [Google Scholar]
- 21.Tayeb HO, Murray ED, Price BH, Tarazi FI. Bapineuzumab and solanezumab for Alzheimer's disease: Is the 'amyloid cascade hypothesis' still alive? Expert Opin Biol Ther. 2013;13:1075–84. doi: 10.1517/14712598.2013.789856. [DOI] [PubMed] [Google Scholar]
- 22.Sperling RA, Jack CR, Jr, Black SE, Frosch MP, Greenberg SM, Hyman BT, et al. Amyloid-related imaging abnormalities in amyloid-modifying therapeutic trials: Recommendations from the Alzheimer's Association Research Roundtable Workgroup. Alzheimers Dement. 2011;7:367–85. doi: 10.1016/j.jalz.2011.05.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salloway S, Sperling R, Gilman S, Fox NC, Blennow K, Raskind M, et al. A phase 2 multiple ascending dose trial of bapineuzumab in mild to moderate Alzheimer disease. Neurology. 2009;73:2061–70. doi: 10.1212/WNL.0b013e3181c67808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rinne JO, Brooks DJ, Rossor MN, Fox NC, Bullock R, Klunk WE, et al. 11C-PiB PET assessment of change in fibrillar amyloid-beta load in patients with Alzheimer's disease treated with bapineuzumab: A phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9:363–72. doi: 10.1016/S1474-4422(10)70043-0. [DOI] [PubMed] [Google Scholar]
- 25.Blennow K, Zetterberg H, Rinne JO, Salloway S, Wei J, Black R, et al. Effect of immunotherapy with bapineuzumab on cerebrospinal fluid biomarker levels in patients with mild to moderate Alzheimer disease. Arch Neurol. 2012;69:1002–10. doi: 10.1001/archneurol.2012.90. [DOI] [PubMed] [Google Scholar]
- 26.Lemere CA. Immunotherapy for Alzheimer's disease: Hoops and hurdles. Mol Neurodegener. 2013;8:36. doi: 10.1186/1750-1326-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lasser R, Ostrowitzki S, Scheltens P, Boada M, Dubois B, Dorflinger E, et al. Efficacy and safety of gantenerumab in prodromal Alzheimer's disease: Results from scarlet road – A global, multicenter trial. Alzheimer's and Dementia: The Journal of the Alzheimer's Association. 2015;11(Suppl):331–2. [Google Scholar]
- 28.Lambracht-Washington D, Rosenberg RN. Advances in the development of vaccines for Alzheimer's disease. Discov Med. 2013;15:319–26. [PMC free article] [PubMed] [Google Scholar]
- 29.Storandt M, Balota DA, Aschenbrenner AJ, Morris JC. Clinical and psychological characteristics of the initial cohort of the Dominantly Inherited Alzheimer Network (DIAN) Neuropsychology. 2014;28:19–29. doi: 10.1037/neu0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sperling R, Mormino E, Johnson K. The evolution of preclinical Alzheimer's disease: Implications for prevention trials. Neuron. 2014;84:608–22. doi: 10.1016/j.neuron.2014.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lopera F, Ardilla A, Martínez A, Madrigal L, Arango-Viana JC, Lemere CA, et al. Clinical features of early-onset Alzheimer disease in a large kindred with an E280A presenilin-1 mutation. JAMA. 1997;277:793–9. [PubMed] [Google Scholar]
- 32.Lee EB, Leng LZ, Zhang B, Kwong L, Trojanowski JQ, Abel T, et al. Targeting amyloid-beta peptide (Abeta) oligomers by passive immunization with a conformation-selective monoclonal antibody improves learning and memory in Abeta precursor protein (APP) transgenic mice. J Biol Chem. 2006;281:4292–9. doi: 10.1074/jbc.M511018200. [DOI] [PubMed] [Google Scholar]
- 33.Siemers ER, Sundell KL, Carlson C, Case M, Sethuraman G, Liu-Seifert H, et al. Phase 3 solanezumab trials: Secondary outcomes in mild Alzheimer's disease patients. Alzheimers Dement. 2016;12:110–20. doi: 10.1016/j.jalz.2015.06.1893. [DOI] [PubMed] [Google Scholar]
- 34.Sabri O, Sabbagh MN, Seibyl J, Barthel H, Akatsu H, Ouchi Y, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer's disease: Phase 3 study. Alzheimers Dement. 2015;11:964–74. doi: 10.1016/j.jalz.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Patel KR. Biogen's aducanumab raises hope that Alzheimer's can be treated at its source. Manag Care. 2015;24:19. [PubMed] [Google Scholar]
- 36.Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, et al. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer's disease. N Engl J Med. 2014;370:311–21. doi: 10.1056/NEJMoa1312889. [DOI] [PubMed] [Google Scholar]
- 37.Yu JT, Tan L, Hardy J. Apolipoprotein E in Alzheimer's disease: An update. Annu Rev Neurosci. 2014;37:79–100. doi: 10.1146/annurev-neuro-071013-014300. [DOI] [PubMed] [Google Scholar]
- 38.Schneider LS, Mangialasche F, Andreasen N, Feldman H, Giacobini E, Jones R, et al. Clinical trials and late-stage drug development for Alzheimer's disease: An appraisal from 1984 to 2014. J Intern Med. 2014;275:251–83. doi: 10.1111/joim.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Winblad B, Andreasen N, Minthon L, Floesser A, Imbert G, Dumortier T, et al. Safety, tolerability, and antibody response of active Aß immunotherapy with CAD106 in patients with Alzheimer's disease: Randomised, double-blind, placebo-controlled, first-in-human study. Lancet Neurol. 2012;11:597–604. doi: 10.1016/S1474-4422(12)70140-0. [DOI] [PubMed] [Google Scholar]
- 40.Hanson AJ, Craft S, Banks WA. The APOE genotype: Modification of therapeutic responses in Alzheimer's disease. Curr Pharm Des. 2015;21:114–20. doi: 10.2174/1381612820666141020164222. [DOI] [PubMed] [Google Scholar]
- 41.Prince M, Prina M, Guerchet M, editors. World Alzheimer Report 2013. London, UK: Alzheimer's Disease International; 2013. Journey of caring: An analysis of long-term care for dementia; p. 92. [Google Scholar]
- 42.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368:1326–34. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McLaughlin T, Feldman H, Fillit H, Sano M, Schmitt F, Aisen P, et al. Dependence as a unifying construct in defining Alzheimer's disease severity. Alzheimers Dement. 2010;6:482–93. doi: 10.1016/j.jalz.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paul SM, Mytelka DS, Dunwiddie CT, Persinger CC, Munos BH, Lindborg SR, et al. How to improve R and D productivity: The pharmaceutical industry's grand challenge. Nat Rev Drug Discov. 2010;9:203–14. doi: 10.1038/nrd3078. [DOI] [PubMed] [Google Scholar]
- 45.Haberstroh J, Hampel H, Pantel J. Optimal management of Alzheimer's disease patients: Clinical guidelines and family advice. Neuropsychiatr Dis Treat. 2010;6:243–53. doi: 10.2147/ndt.s7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vellas B, Aisen PS, Sampaio C, Carrillo M, Scheltens P, Scherrer B, et al. Prevention trials in Alzheimer's disease: An EU-US task force report. Prog Neurobiol. 2011;95:594–600. doi: 10.1016/j.pneurobio.2011.08.014. [DOI] [PubMed] [Google Scholar]


