Abstract
BACKGROUND
Endothelial dysfunction may represent an important link between chronic stress and cardiovascular disease (CVD) risk. However, few studies have examined the impact of chronic stress on endothelial dysfunction. The purpose of this study was to examine whether chronic stress was associated with flow-mediated dilation (FMD) and 2 biomarkers of endothelial dysfunction (intercellular adhesion molecule-1 (ICAM-1) and E-selectin) in a multiethnic sample of adults (ages 45–84 years).
METHODS
Data come from the baseline examination of Multi-Ethnic Study of Atherosclerosis participants. Chronic stress was assessed based on self-report of the presence and severity of ongoing problems in 5 domains. FMD was obtained using high-resolution ultrasound; biomarkers were assayed in different subsets of participants.
RESULTS
Higher chronic stress was associated with lower absolute FMD (mm FMD) in models adjusted for demographic and socioeconomic characteristics (0.169mm in high-stress participants vs. 0.178 and 0.179mm in medium and low-stress participants; P for trend = 0.04). This association remained unchanged with further adjustment for behavioral and biological CVD risk factors. Higher stress was related to higher ICAM-1 in models adjusted for sociodemographic characteristics and biological risk factors (P for trend = 0.005), but this association attenuated with adjustment for cigarette smoking (P for trend = 0.07). Chronic stress was not associated with E-selectin.
CONCLUSIONS
Our findings suggest chronic stress is related to endothelial dysfunction, possibly in part through other stress-associated CVD risk factors such as cigarette smoking.
Keywords: blood pressure, chronic stress, E-selectin, endothelial dysfunction, flow-mediated dilation, hypertension, ICAM-1.
Research suggests stress is a risk factor for cardiovascular disease (CVD),1–4 but the underlying mechanisms remain unclear. Mental stress activates the sympathetic nervous system,5 causing a constellation of adverse cardiovascular effects, including increased blood pressure, heart rate, and endothelial dysfunction.6 One potential pathway through which chronic exposure to psychosocial stressors are hypothesized to influence CVD risk is through injury to the endothelial lining of blood vessels due to sustained and repeated activation of the sympathetic nervous system.7 Endothelial dysfunction plays a critical role in the initiation and progression of atherosclerosis,8 and thus, may be a major pathway linking chronic stress and CVD.
Studies have shown that acute exposure to a mental stressor is significantly associated with prolonged endothelial dysfunction,6,9 but few studies have examined the impact of chronic stress and these studies have been in ethnically homogeneous populations. A national study of non-Hispanic Whites found that chronic exposure to discrimination predicted higher levels of circulating endothelial-leukocyte adhesion molecule-1 (E-selectin), an indicator of endothelial dysfunction, in men but not women.10 Two studies of caregivers (>80% non-Hispanic White) found that global stress and caregiver stress were each associated with lower brachial artery flow-mediated dilation (FMD).11,12
In this study, we examined associations of chronic stress with 3 markers of endothelial dysfunction in a multiethnic population of middle- and older-age adults. Brachial artery FMD is a noninvasive, commonly used method to assess endothelial function of the peripheral conduit artery. With this method, reduced artery dilation is suggestive of poorer endothelial function. We also included 2 serological biomarkers of endothelial dysfunction: intercellular adhesion molecule-1 (ICAM-1) and E-selectin. These cellular adhesion molecules are expressed on the surfaces of endothelial cells as part of the inflammatory response to endothelial damage. We hypothesized that higher chronic stress would be associated with lower FMD, higher ICAM-1, and higher E-selectin levels. Given previous heterogeneous findings by gender,10 and the dearth of studies in multiethnic populations, we also examined whether associations varied by race/ethnicity or gender.
METHODS
Study population
The Multi-Ethnic Study of Atherosclerosis is an observational cohort study designed to examine the determinants of subclinical CVD in adults aged 45–84 years. Participants free of clinical CVD at baseline were recruited from 6 field centers (New York, New York; Baltimore City and County, Maryland; Forsyth County, North Carolina; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles County, California) between 2000 and 2002. Random population samples were selected at each field center using lists of area residents. Additional details are provided elsewhere.13 Of the selected persons deemed eligible after screening, 59.8% participated in the study. Institutional review board’s approval was obtained at each site and all participants gave informed consent. Four additional examinations have been completed since baseline: exam 2 (2002–2004), exam 3 (2004–2005), exam 4 (2005–2007), and exam 5 (2010–2012).
This study uses data from the baseline exam. Data on the study outcomes were collected as part of different ancillary studies that included different subsets of the MESA population. Of the 2,622 participants with data on ICAM-1, 55 were excluded for missing data on the exposure and 44 were excluded for missing data on one or more of the other study covariates (n = 2,523). Among the 999 participants with data on E-selectin, 12 were excluded for missing data on the exposure and another 16 were excluded for missing data on other covariates (n = 971). Of the 3,027 participants with FMD data, 27 were excluded for missing data on the exposure and another 37 for missing data on other covariates (n = 2,963).
Chronic stress
Chronic stress was assessed using the Chronic Burden scale, measured at baseline.14 Participants were asked whether or not they had ongoing, financial, job, relationship, or health-related (both self and someone close to the participant) problems lasting over 6 months. In addition, they were asked to indicate how stressful the problems were on a scale ranging from 1 (not very stressful) to 3 (very stressful). Consistent with previous studies,15,16 chronic burden score was created by summing the number of domains in which moderate to severe stress was reported. Possible scores ranged from 0 to 5 and were modeled categorically in approximate tertiles as high (2 or more), medium (1), and low (0; referent).
Endothelial dysfunction
Brachial artery FMD was ascertained via ultrasound in MESA participants at baseline.17 Participants were required to fast for at least 6 hours prior to undergoing measurement, and they were examined in the supine position after 15 minutes of rest. An automated sphygmomanometer (Dinamap device) was used to monitor blood pressure and pulse in the left arm at 5-minute intervals throughout the examination. A standard blood pressure cuff was positioned around the right arm, 2 inches below the antecubital fossa, and the artery was imaged 5–9cm above the antecubital fossa. A linear-array multifrequency transducer operating at 9 MHz (GE Logiq 700 Device) was used to acquire images of the right brachial artery. After baseline images were obtained, the cuff was inflated to 50mm Hg above the participant’s systolic blood pressure for 5 minutes. Digitized images of the right brachial artery were captured continuously for 30 seconds before cuff inflation and for 2 minutes beginning immediately before cuff deflation to document the maximum vasodilator response.
Although FMD was measured in the majority of MESA participants (n = 6489), for cost reasons, only a subset had their ultrasound videotapes analyzed as part of a nested case–cohort study.17 This subset included a random sample of MESA participants who had not had a cardiovascular event and all participants who had an adjudicated cardiovascular event by 10 October 2005. All analyses were completed at the Wake Forest University Cardiology Image Processing Laboratory with the use of a previously validated semiautomated system. The semiautomated readings (media-adventitial interfaces to media-adventitial interfaces) of these digitized images generated the baseline and maximum diameters of the brachial artery. Change in FMD was calculated in 2 ways: absolute FMD (mm FMD), defined as maximum diameter—baseline diameter, and relative FMD (%FMD), calculated as ((maximum diameter − baseline diameter)/baseline diameter) × 100%. We chose to examine associations with mm FMD because it is not correlated with baseline diameter, as can be the case with %FMD.18 However, we also included %FMD because it is a commonly used measure that has been shown to predict cardiovascular events.17
Intrareader reproducibility for baseline diameter, maximum diameter, and %FMD was evaluated by comparing an original and a blinded quality control reread of ultrasounds from 40 MESA participants. The intraclass correlation coefficients were 0.99, 0.99, and 0.93, respectively. Intrasubject variability was evaluated by comparing results from repeated examinations of 19 subjects on 2 days a week apart. The intraclass correlation coefficients were 0.90 for baseline diameter, 0.90 for maximum diameter, and 0.54 for %FMD. Percent technical error of measurement was 1.39% for baseline diameter measurement, 1.47% for maximum diameter measurement, and 28.4% for %FMD measurement.
Blood was drawn after a 12-hour fast, and samples were stored at −70 °C. Lipids were measured at a central laboratory (Collaborative Studies Clinical Laboratory at Fairview University Medical Center, Minneapolis, MN). Plasma ICAM-1 was measured at baseline among 2,621 MESA participants using an ELISA assay (Parameter Human sICAM-1; R&D Systems, Minneapolis, MN). The coefficient of variation was 5.0%. Serum E-selectin was measured at baseline for 998 MESA participants (Parameter Human sE-selectin Immunoassay; R&D Systems; coefficient of variation 5.7–8.8%).
Covariates
We adjusted for several sociodemographic variables including age, sex, race or ethnicity (non-Hispanic White, non-Hispanic Black, Chinese, or Hispanic), education (categorized as less than high school, high school graduate, some college, and college or more completed), and income (broken into quartiles).
We also adjusted for several CVD risk factors explain associations of chronic stress with endothelial dysfunction, either as mediators or confounders. Waist circumference was measured at the umbilicus to the nearest 1cm. Seated, resting blood pressure was measured 3 times at 2-minute intervals using an automated oscillometric device with appropriate sized cuffs (Dinamap Monitor Pro 100, GE Healthcare). Systolic blood pressure and diastolic blood pressure were modeled continuously based on the average of the final 2 readings. Plasma high-density lipoprotein cholesterol and total cholesterol were measured by the cholesterol-oxidase method and modeled continuously. Use of blood pressure-lowering and any lipid-lowering medication were each self-reported. Cigarette smoking was based on self-report and categorized as current, former, and never. Physical activity was assessed using the MESA Typical Week Physical Activity Survey, adapted from the Cross-Cultural Activity Participation Study.19 Participants were asked to report the time and frequency spent in 28 different types of physical activities during a typical week in the previous month. Minutes of each activity were multiplied by the appropriate metabolic equivalent level and summed to obtain a composite score. Physical activity was modeled continuously.
Statistical analysis
Participant characteristics were generated for all study covariates separately for those with available data on FMD, ICAM-1, and E-selectin. Age- and sex-adjusted mean brachial artery FMD, ICAM-1, and E-selectin levels were estimated by chronic stress categories using linear regression.
Linear regression was used to estimate adjusted mean levels of each measure of endothelial dysfunction by category of chronic stress. Model 1 adjusted for age, race/ethnicity, sex, education, and income. Model 2 further adjusted for waist circumference, systolic blood pressure, diastolic blood pressure, antihypertensive medication use, total cholesterol, high-density lipoprotein cholesterol, and lipid-lowering medication use. Model 3 further adjusted for cigarette smoking and physical activity. Race/ethnicity * chronic stress and gender * chronic stress interaction terms were incorporated in separate models to test whether associations of chronic stress with endothelial dysfunction varied by these characteristics. Because the selection of participants for FMD readings was not completely random, the inverse of the probability of selection was used as weights to account for the sampling scheme in the analyses where FMD is the outcome. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Associations did not vary significantly by race/ethnicity (P for interaction > 0.3) or sex (P for interaction > 0.2), so pooled results are presented. Participant characteristics were similar among the study populations for the different markers of endothelial dysfunction (Table 1). Participants with FMD data were slightly older and more likely to be male than participants with ICAM-1 data. A larger percentage of FMD participants also had high chronic burden scores compared with ICAM-1 participants. FMD participants also had lower levels of socioeconomic attainment, and they were more likely to be racial/ethnic minorities. There were no notable differences across the populations in waist circumference, blood pressure, or cholesterol.
Table 1.
Selected characteristics for participants with data on FMD, ICAM-1, and E-selectin
| FMD (n = 2,963) | ICAM-1 (n = 2,523) | E-selectin (n = 971) | |
|---|---|---|---|
| Chronic burden, % | |||
| High | 21.7 | 25.2 | 23.5 |
| Medium | 27.9 | 27.9 | 29.3 |
| Low | 50.4 | 46.9 | 47.3 |
| Age, mean years (SD) | 61.8 (13.6) | 59.4 (9.7) | 59.3 (9.8) |
| Sex, % male | 47.0 | 44.0 | 42.7 |
| Education, % <HS | 17.9 | 16.6 | 16.7 |
| Family income, % <$15,999 | 18.1 | 15.7 | 14.1 |
| Race/ethnicity, % | |||
| Black | 23.0 | 18.1 | 20.8 |
| Chinese | 14.3 | 12.0 | 9.9 |
| Hispanic | 25.9 | 22.0 | 23.1 |
| White | 36.8 | 47.9 | 46.2 |
| Systolic BP, mean mm Hg (SD) | 125.2 (27.2) | 124.5 (21.0) | 123.8 (20.9) |
| Diastolic BP, mean mm Hg (SD) | 71.6 (13.8) | 71.8 (10.3) | 71.3 (10.2) |
| Waist circumference, mean cm (SD) | 97.8 (19.4) | 97.8 (14.8) | 97.9 (14.7) |
| Total cholesterol, mean mg/dl (SD) | 194.7 (48.7) | 196.7 (36.3) | 195.2 (35.0) |
| HDL cholesterol, mean mg/dl (SD) | 50.9 (19.9) | 51.8 (15.2) | 51.1 (14.5) |
| Cigarette smoking, % | |||
| Never | 51.4 | 50.6 | 50.5 |
| Former | 35.8 | 35.3 | 34.1 |
| Current | 12.8 | 14.1 | 15.5 |
| Physical activity, mean MET-hour/week (SD) | 25.4 (49.6) | 24.7 (36.4) | 25.8 (41.3) |
Abbreviations: BP, blood pressure; FMD, flow-mediated dilation; ICAM-1, intercellular adhesion molecule-1; HDL, high-density lipoprotein; HS, high school; MET, metabolic equivalent.
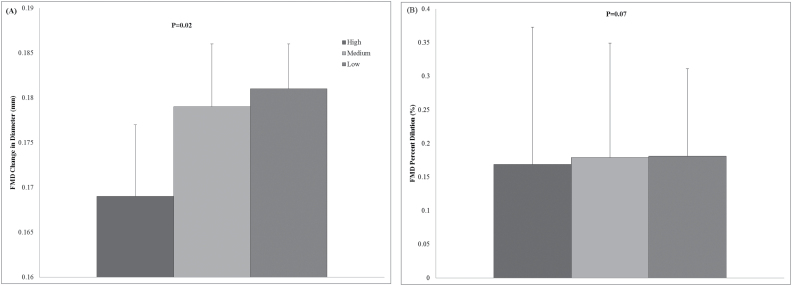
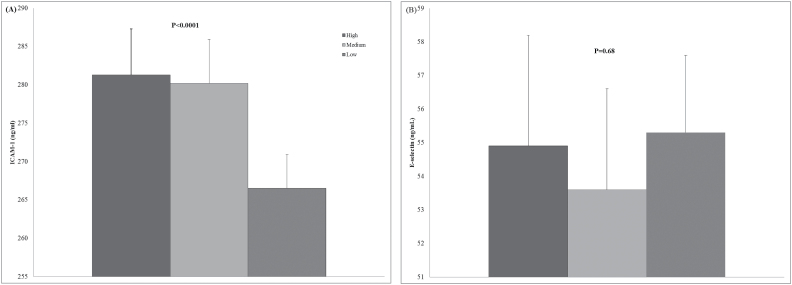
Participants in the high-stress category had lower age- and sex-adjusted mm FMD than those in the low-stress category (Figure 1a; 0.169mm vs. 0.181mm); findings were similar for %FMD (Figure 1b; 4.1% vs. 4.4%). Age- and sex-adjusted mean ICAM-1 levels were higher among participants in the high-stress category than in the low category (Figure 2a; 281.3ng/ml and 266.5ng/ml, respectively). There was no difference in E-selectin for those in the high- vs. low-stress category (Figure 2b; 54.9ng/ml and 55.3ng/ml).
Figure 1.
Age- and sex-adjusted mean levels of (a) FMD change in diameter and (b) FMD percent dilation by category of chronic stress. Abbreviation: FMD, flow-mediated dilation.
Figure 2.
Age- and sex-adjusted mean levels of (a) ICAM-1 and (b) E-selectin by category of chronic stress. Abbreviation: ICAM-1, intercellular adhesion molecule-1.
Chronic stress was associated with mm FMD and %FMD in models adjusted for age, sex, race/ethnicity, education, and income (Table 2). Mean mm FMD was 0.169mm among high-stress participants compared with 0.179mm among participants in the low-stress category. This remained essentially unchanged with further adjustment for traditional CVD risk factors. Mean %FMD was 4.1% among those in the high-stress category compared with 4.4% in the low-stress category in sociodemographic-adjusted models. These estimates were similar with further adjustment for risk factors, but they were no longer statistically significant.
Table 2.
Adjusted mean FMD change in diameter (mm FMD) and FMD percent dilation (%FMD) and SE by category of chronic stress
| mm FMD | %FMD | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | Model 1a | Model 2b | Model 3c | |
| High | 0.169 (0.004) | 0.169 (0.004) | 0.169 (0.004) | 4.1 (0.1) | 4.1 (0.1) | 4.1 (0.1) |
| Medium | 0.178 (0.004) | 0.178 (0.004) | 0.179 (0.004) | 4.3 (0.09) | 4.3 (0.09) | 4.3 (0.09) |
| Low | 0.179 (0.003) | 0.180 (0.003) | 0.180 (0.003) | 4.4 (0.07) | 4.4 (0.07) | 4.4 (0.07) |
| P value for trend | 0.04 | 0.04 | 0.04 | 0.04 | 0.06 | 0.05 |
Abbreviations: FMD, flow-mediated dilation; HDL, high-density lipoprotein; mm FMD, absolute FMD; %FMD, relative FMD.
aAdjusted for age, sex, race/ethnicity, education, and income.
bAdjusted for age, sex, race/ethnicity, education, income, waist circumference, systolic blood pressure, diastolic blood pressure, total cholesterol, HDL cholesterol, antihypertensive medication use, and lipid-lowering medication use.
cAdjusted for model 2 covariates, physical activity, and cigarette smoking.
Participants in the high-stress category had an adjusted mean ICAM-1 level of 272.0 compared with 270.4 in the medium stress category, and 261.6 in the low-stress category (Table 3; P for trend = 0.003). Findings were similar for models further adjusted for waist circumference, blood pressure, and cholesterol but were attenuated with further adjustment for physical activity and cigarette smoking. Cigarette smoking was strongly associated with ICAM-1; adjustment for smoking attenuated the relationship between chronic stress and ICAM-1 even without physical activity in the model. Chronic stress was not associated with E-selectin.
Table 3.
Adjusted mean ICAM-1 (ng/ml) and E-selectin (ng/ml) and SE by category of chronic stress
| ICAM-1 | E-selectin | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | Model 1a | Model 2b | Model 3c | |
| High | 272.0 (3.2) | 271.5 (3.2) | 280.7 (3.2) | 56.7 (1.7) | 56.5 (1.7) | 57.9 (1.7) |
| Medium | 270.4 (3.1) | 270.8 (3.0) | 280.7 (3.0) | 56.9 (1.6) | 57.1 (1.6) | 58.6 (1.6) |
| Low | 261.6 (2.3) | 262.0 (2.3) | 273.1 (2.4) | 57.1 (1.2) | 57.9 (1.2) | 59.8 (1.3) |
| P value for trend | 0.003 | 0.005 | 0.08 | 0.83 | 0.46 | 0.30 |
Abbreviations: HDL, high-density lipoprotein; ICAM-1, intercellular adhesion molecule-1.
aAdjusted for age, sex, race/ethnicity, education, and income.
bAdjusted model 1 covariates, waist circumference, systolic blood pressure, diastolic blood pressure, total cholesterol, HDL cholesterol, antihypertensive medication use, and lipid-lowering medication use.
cAdjusted for model 2 covariates, physical activity, and cigarette smoking.
DISCUSSION
In this multiethnic study of middle- and older-age adults, we found evidence suggesting chronic stress is associated with poorer endothelial function. Chronic stress was associated with lower FMD independent of sociodemographic characteristics. Effect estimates were similar with further adjustment for blood pressure, waist circumference, and cholesterol, but associations were no longer statistically significant for %FMD. Chronic stress was associated with ICAM-1 but not E-selectin, and associations with ICAM-1 were explained by cigarette smoking status.
Few studies have examined associations of chronic stress with markers of endothelial dysfunction, and findings are mixed. In contrast to our findings, a study of discrimination and E-selectin found men who experience 3 or more instances of major discrimination and more chronic exposure to everyday discrimination had higher E-selectin levels than men who experienced fewer or no instances of discrimination. However, they found no association in women.10 A study of work stress and endothelial function found no association between job strain and %FMD in adjusted models.20 Two studies have examined FMD in caregivers. Both showed those who had been caregivers longer had lower FMD,11,12 but those who reported feeling overloaded in their roles as caregivers only had significantly lower FMD in one of the studies.11 The diverse ways in which stress was measured across these studies make it difficult to compare their findings with ours, but the inconsistencies suggest the contributions of different sources of stress to endothelial dysfunction is in need of further study.
A major strength of our study is that we were able to include multiple markers of endothelial dysfunction. Our findings for ICAM-1 were consistent with our findings for FMD, but not for E-selectin. There are multiple potential explanations for the different findings by marker of endothelial dysfunction. The smaller sample size for E-selectin may have reduced our power to detect differences by chronic burden category. Alternatively, the different findings may be indicative of the way in which chronic stress impacts endothelial dysfunction. Although E-selectin and ICAM-1 are both cell adhesion molecules, E-selectin is uniquely expressed by endothelial cells, while ICAM-1 is expressed on multiple cell types. Thus, it is possible that our measure of chronic stress is more strongly associated with nonspecific endothelial damage that leads to dysfunction. Cigarette smoking was strongly associated with ICAM-1 and E-selectin, but unassociated with FMD, which may explain why adjusting for cigarette smoking attenuated the relationship between stress and ICAM-1 but not between stress and FMD.
This study has several strengths and limitations. The large sample size and well-measured exposure and outcome are the key strengths of this study. Chronic stress was assessed by not only asking about ongoing problems but also having participants appraise the extent to which those experiences were stressful. In addition, brachial artery FMD is a direct measure of endothelial dysfunction, and the assessment of both absolute and relative changes further strengthens our study. A key limitation of our study is the cross-sectional design, which precludes us from being able to establish causality or the temporal ordering of the relationship between stress and endothelial dysfunction. However, since FMD, ICAM-1, and E-selectin are all subclinical markers of endothelial dysfunction, it is less likely that levels of any of these markers would cause high levels of chronic stress. In addition, the dependency of %FMD on baseline artery diameter, along with the higher intraindividual variability of %FMD compared with baseline and maximum diameter described in the Methods section, may provide biased estimates of endothelial dysfunction.18 However, the general consistency in our findings for mm FMD and %FMD suggest this potential bias may be small in this case.
In summary, examining the relationship between chronic stress and endothelial dysfunction may provide important mechanistic insights into the role of stress in CVD risk. Our findings provide further evidence supporting physiologic wear-and-tear due to repeated activation of the sympathetic nervous system as a key contributor to stress-associated increased CVD risk. A better understanding of these pathways linking stress to CVD risk could help support the design of more effective interventions that target stress and stress coping behaviors in addition to more traditional approaches.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
This research was supported by contracts HHSN268201500003I, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-TR-001079 from NCRR. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
REFERENCES
- 1. Aboa-Eboulé C, Brisson C, Maunsell E, Mâsse B, Bourbonnais R, Vézina M, Milot A, Théroux P, Dagenais GR. Job strain and risk of acute recurrent coronary heart disease events. JAMA 2007; 298:1652–1660. [DOI] [PubMed] [Google Scholar]
- 2. Bairey Merz CN, Dwyer J, Nordstrom CK, Walton KG, Salerno JW, Schneider RH. Psychosocial stress and cardiovascular disease: pathophysiological links. Behav Med 2002; 27:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. De Bacquer D, Pelfrene E, Clays E, Mak R, Moreau M, de Smet P, Kornitzer M, De Backer G. Perceived job stress and incidence of coronary events: 3-year follow-up of the Belgian Job Stress Project cohort. Am J Epidemiol 2005; 161:434–441. [DOI] [PubMed] [Google Scholar]
- 4. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med 1998; 338:171–179. [DOI] [PubMed] [Google Scholar]
- 5. Hjemdahl P, Fagius J, Freyschuss U, Wallin BG, Daleskog M, Bohlin G, Perski A. Muscle sympathetic activity and norepinephrine release during mental challenge in humans. Am J Physiol 1989; 257:E654–E664. [DOI] [PubMed] [Google Scholar]
- 6. Ghiadoni L, Donald AE, Cropley M, Mullen MJ, Oakley G, Taylor M, O’Connor G, Betteridge J, Klein N, Steptoe A, Deanfield JE. Mental stress induces transient endothelial dysfunction in humans. Circulation 2000; 102:2473–2478. [DOI] [PubMed] [Google Scholar]
- 7. Bekkouche NS, Holmes S, Whittaker KS, Krantz DS. Stress and the heart: psychosocial stress and coronary heart disease. In Contrada R. and Baum A (eds), The Handbook of Stress Science: Biology, Psychology, and Health. Springer: New York, 2011, pp. 385–398. [Google Scholar]
- 8. Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993; 362:801–809. [DOI] [PubMed] [Google Scholar]
- 9. Spieker LE, Hürlimann D, Ruschitzka F, Corti R, Enseleit F, Shaw S, Hayoz D, Deanfield JE, Lüscher TF, Noll G. Mental stress induces prolonged endothelial dysfunction via endothelin-A receptors. Circulation 2002; 105:2817–2820. [DOI] [PubMed] [Google Scholar]
- 10. Friedman EM, Williams DR, Singer BH, Ryff CD. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: the MIDUS study. Brain Behav Immun 2009; 23:684–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mausbach BT, Chattillion E, Roepke SK, Ziegler MG, Milic M, von Känel R, Dimsdale JE, Mills PJ, Patterson TL, Allison MA, Ancoli-Israel S, Grant I. A longitudinal analysis of the relations among stress, depressive symptoms, leisure satisfaction, and endothelial function in caregivers. Health Psychol 2012; 31:433–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mausbach BT, Roepke SK, Ziegler MG, Milic M, von Känel R, Dimsdale JE, Mills PJ, Patterson TL, Allison MA, Ancoli-Israel S, Grant I. Association between chronic caregiving stress and impaired endothelial function in the elderly. J Am Coll Cardiol 2010; 55:2599–2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O’Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol 2002; 156:871–881. [DOI] [PubMed] [Google Scholar]
- 14. Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol 2003; 22:300–309. [DOI] [PubMed] [Google Scholar]
- 15. Everson-Rose SA, Roetker NS, Lutsey PL, Kershaw KN, Longstreth WT, Jr, Sacco RL, Diez Roux AV, Alonso A. Chronic stress, depressive symptoms, anger, hostility, and risk of stroke and transient ischemic attack in the Multi-Ethnic Study of Atherosclerosis. Stroke 2014; 45:2318–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kershaw KN, Diez Roux AV, Bertoni A, Carnethon MR, Everson-Rose SA, Liu K. Associations of chronic individual-level and neighbourhood-level stressors with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. J Epidemiol Community Health 2015; 69:136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the Multi-Ethnic Study of Atherosclerosis. Circulation 2009; 120:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Atkinson G, Batterham AM. The percentage flow-mediated dilation index: a large-sample investigation of its appropriateness, potential for bias and causal nexus in vascular medicine. Vasc Med 2013; 18:354–365. [DOI] [PubMed] [Google Scholar]
- 19. Ainsworth BE, Irwin ML, Addy CL, Whitt MC, Stolarczyk LM. Moderate physical activity patterns of minority women: the Cross-Cultural Activity Participation Study. J Womens Health Gend Based Med 1999; 8:805–813. [DOI] [PubMed] [Google Scholar]
- 20. Charles LE, Fekedulegn D, Landsbergis P, Burchfiel CM, Baron S, Kaufman JD, Stukovsky KH, Fujishiro K, Foy CG, Andrew ME, Diez Roux AV. Associations of work hours, job strain, and occupation with endothelial function: the Multi-Ethnic Study of Atherosclerosis (MESA). J Occup Environ Med 2014; 56:1153–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]