Abstract
Background:
The aims of this study were to determine among retirees: the associations of arthritis with limitations in physical functions, and whether these associations changed differently with age for those with arthritis versus without arthritis.
Methods:
We identified retirees from the Health and Retirement Study, a nationally representative longitudinal panel study of U.S. adults ≥51 years old. We calculated incidence density ratios (IDRs) using Poisson regression modeling with generalized estimating equations to estimate the associations between arthritis and limitations in four physical function measures (large muscle tasks, mobility, activities of daily living, and instrumental activities of daily living) adjusting for age, sex, race/ethnicity, marital status, education, total household income, depression, obesity, smoking, chronic conditions, physical activity, and cohort status. We examined interaction effects between arthritis and age to determine if the rate of change in physical function differed by arthritis status across age.
Results:
Over 8 years (2004–2012), significantly more retirees with arthritis had limitations with large muscle tasks (IDR 2.1: 95% confidence interval 1.6, 2.8), mobility (IDR 1.6: 1.2, 2.2), activities of daily living (IDR 2.2: 1.0, 4.7), and instrumental activities of daily living (IDR 3.7: 1.9, 7.4) than retirees without arthritis. Retirees with arthritis did not develop limitations in mobility, activities of daily living, and instrumental activities of daily living at a different rate as they aged compared to those without arthritis.
Conclusions:
Arthritis was associated with a greater prevalence of physical function limitations. Preventing limitations caused by arthritis is a key strategy to prevent disability in retirees.
Key Words: Arthritis, Functional performance, Epidemiology, Public health
Arthritis is one of the most common and disabling chronic health conditions. Doctor-diagnosed arthritis affects 52.5 million U.S. adults (22.7%) (1), and although often considered a disease of old age, most arthritis occurs in those younger than 65 years in the United States (1). Arthritis is also the most common cause of disability in U.S. adults (2). Although arthritis causes a significant amount of work disability, many people with arthritis remain in the labor force until retirement age. Participation in the labor force has positive effects on health; those who work generally report better mental and physical health than those who do not (3).
There is scant, conflicting research on the effects of retirement on health and function. Some research suggests that retirement improves mental health and feelings of well-being (4), whereas other research suggests that retirement is associated with decreases in physical function (4–6). In a 6-year follow-up study, retirement led to a 5%–14% increase in difficulties associated with mobility and activities of daily living (ADL) and a 6.9% decline in mental health (7). These declines in physical function are not simply the opposite of the “healthy worker effect” (ie, a greater proportion of workers retire because they are ill) (5,6) because these declines occur regardless of illness status.
People with chronic health conditions before retirement are consistently and more likely to retire early with poorer physical function after retirement (6,7). If retirement leads to declines in physical function, it should exacerbate declines in people with chronic conditions. While those who leave the work force due to a disability have poorer retirement outcomes, studies have not examined the effect of retiring with arthritis on physical function, and whether retirees with arthritis are more likely than those without arthritis to report an increased rate of limitations in physical function as they age.
The purposes of this study were to determine (i) the associations of arthritis with limitations in physical functions, hypothesizing that, after potential confounders were controlled, retirees with arthritis would be more likely to have limitations in physical functions than retirees without arthritis and (ii) whether these associations changed differently with age for those with versus without arthritis, hypothesizing that the development of these limitations with age would be significantly greater in retirees with arthritis.
Methods
Study Population
We analyzed data from the Health and Retirement Study (HRS), a multistage area probability sample longitudinal study of U.S. adults 51 years or older, representative of the national civilian, noninstitutionalized population. The HRS is a steady-state study and adds a new cohort of 51–56 year olds every 6 years (8). Respondents and their spouses are interviewed every 2 years. The HRS has been approved by the University of Michigan Health Sciences Human Subjects Committee. We excluded those who were still working, had never worked, or who had left the labor force due to disability to increase the homogeneity of the sample.
We examined physical function after retirement from 2004 until 2012 (five visits/8 years), using data from the RAND HRS Data File (v. N) (9,10). In 2004, HRS obtained data from 20,129 respondents (response rate of 88%) (11). Overall response rates from 2006 through 2012 ranged between 88% and 91%.
We considered respondents retired at baseline if they answered “completely retired” to the question “At this time do you consider yourself partly retired, completely retired, or not retired at all?” and also indicated their labor force status was “retired” in response to the question “Are you working now, temporarily laid off, unemployed and looking for work, disabled and unable to work, retired, a homemaker or what?”
We identified respondents with arthritis if they responded “yes” to the question “Have you ever had, or has a doctor ever told you that you have, arthritis or rheumatism.”
Limitations in physical function were assessed using four RAND summary indices: large muscle tasks (sitting for 2 hours, getting up from a chair, stooping/kneeling/crouching, or pushing or pulling large objects), mobility (walking one block, walking several blocks, walking across a room, climbing one flight of stairs, or climbing several flights of stairs), basic ADLs (bathing, dressing, eating, getting in/out of bed, or walking across a room), and instrumental activities of daily living (IADLs; using the phone, managing money, taking medications, shopping for groceries, or preparing hot meals). Respondents indicated if they had “any difficulty” with each subtask. The summary indices for each physical functional outcome were the total of “yes” responses for each subtask (12). We coded respondents as having limitations in physical function outcomes if they scored ≥1 for an index.
Covariates
Sociodemographic covariates included age, sex, race/ethnicity, and marital status (“married/partnered,” “not married/partnered”), education (“less than college degree,” “college and greater”), and income (household income score, categorized by thirds [$0–$19,999; $20,000–$39,999; $40,000 or greater]). Comorbidities included obesity (categorized using body mass index from self-reported height and weight: not obese [body mass index < 30kg/m2], obese [body mass index ≥ 30kg/m2] (13)), smoking (never, previous, current), the number of six chronic conditions (self-reports in response to “Has a doctor ever told you that you have...” high blood pressure, diabetes, cancer, lung disease, heart condition or stroke; categorized as 0, 1, or 2 or more), and depression (categorized as no depression or depression [cutoff of 4 or higher on the Center for Epidemiological Studies Depression Scale [CESD] (14)). Physical activity was based on responses to three questions concerning the frequency of (i) vigorous, (ii) moderately energetic, or (iii) mildly energetic physical activity. Responses for each magnitude were “more than once a week,” “once a week,” “one to three times a month,” or “hardly ever or never.” Many respondents volunteered “every day” as a frequency. We coded active if they replied “every day” or “more than once a week”; somewhat active if they replied “once a week” or “one to three times a month”; and inactive if they replied “hardly ever or never” to any magnitude of physical activity.
Statistical Analysis
All analyses incorporated strata and sampling units to account for HRS’s complex, multistage, sample design (15). HRS respondent–level sampling weights were applied to make estimates representative of the U.S. civilian, noninstitutionalized population aged 51 years and older (16). As HRS recommends (17), we used the base-year weights rather than the terminal year weights.
We calculated weighted proportions and 95% confidence intervals (CIs) using SAS survey procedures (v. 9.3; (18)) to describe the characteristics of respondents and to determine the distribution of the physical function indices of those with and without arthritis. We conservatively defined statistically significant differences in characteristics using nonoverlapping 95% CIs (19). To further describe our sample, we completed a subanalysis for each indices subtasks by calculating weighted proportions and 95% CIs.
We completed two types of analyses for the 8-year study period: a cross-sectional analysis (arthritis and function) for the first hypothesis and a longitudinal analysis (function change by arthritis status) for the second hypothesis. For the cross-sectional analysis, arthritis and function were measured together at five time points during the 8 years. For the longitudinal analysis, the same five time points were used up to 8 years of follow-up, but function change was measured with increasing age by arthritis status. We used modified Poisson regression with generalized estimating equations via the LOGLINK procedure in SUDAAN (v. 11; (20–23)) to estimate the effect of arthritis on physical function limitations controlling for covariates. Because the limitations in physical function are correlated within respondents over time, we assumed these correlations were equal or exchangeable. Taylor series linearization method was used for variance estimation to account for the study’s complex sample design. Respondents who died, refused, or were lost to follow-up were included in the study until their last follow-up (last interview date for the 8-year follow-up).
The modified Poisson regression models estimated incidence density ratios (IDRs) and 95% CIs. The IDRs represent the average association between the variable and the outcome measure. We completed secondary analyses of each subtask for physical function indices, to identify which type of tasks was more likely to be associated with arthritis.
All models adjusted for all covariates and for HRS birth cohorts because research suggests that people in birth cohorts may experience unique environmental and life experiences that can shape health outcomes independent of age alone (24), but we do not report these results.
All the variables that could change with age (excluding sex, education, race/ethnicity, and birth cohort) were analyzed as age-dependent covariates. Interaction terms between age and these covariates were estimated. Significant interaction effects indicate that respondents at different ages developed physical function limitations at different rates.
Results
Of the 7,741 retirees, 5,212 (68.1%) had arthritis (Figure 1). A significantly greater proportion of retirees with arthritis than without arthritis were 75 years old or older, female, non-Hispanic black, married/partnered, less well educated, in the lowest income level, depressed, obese, previous smokers, inactive or only somewhat physically active, or had 2 or more chronic conditions (Supplementary Table 1).
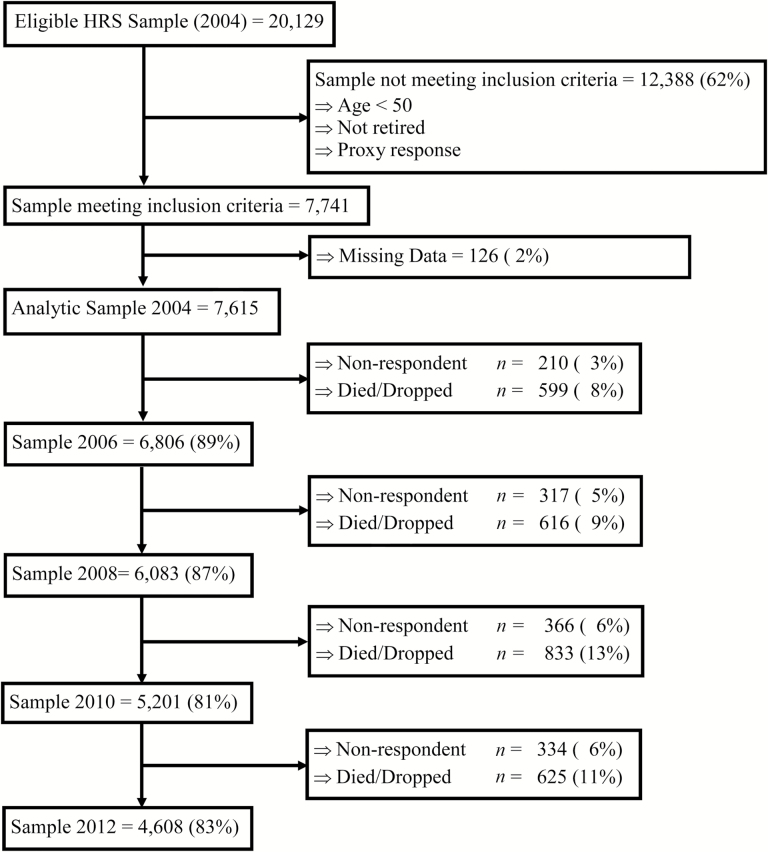
Figure 1.
Flow chart showing the creation of our analytic sample from the Health and Retirement Study [number (% of sample immediately above)].
Retirees with arthritis were significantly more likely than those without arthritis to report a limitation with one or more physical function (Table 1). A significantly greater proportion of retirees with arthritis had difficulty with every subtask of every indices (Supplementary Table 2).
Table 1.
Distribution of Physical Function Outcomes in Retirees Aged 51 and Older Included in the 2004–2012 HRS Analytic Sample, by Arthritis Status
| Characteristics | Arthritis | No Arthritis | ||||
|---|---|---|---|---|---|---|
| n | N in 1,000s | % (95% CI) | n | N in 1,000s | % (95% CI) | |
| Total | 5,212 | 17,138 | 68.1 (66.9, 69.3) | 2,403 | 8,624 | 31.9 (30.7, 33.1) |
| Physical function outcomes | ||||||
| Large muscle tasks | ||||||
| No limitations | 1,181 | 4,122 | 22.4 (21.1, 23.7) | 1,315 | 4,780 | 55.4 (53.2, 57.7) |
| Limitations | 4,030 | 14,271 | 77.6 (76.3, 78.9) | 1,088 | 3,844 | 44.6 (42.3, 46.8) |
| Mobility | ||||||
| No limitations | 1,794 | 6,340 | 34.5 (33.0, 35.9) | 1,502 | 5,390 | 62.5 (60.3, 64.7) |
| Limitations | 3,416 | 12,052 | 65.5 (64.1, 67.0) | 901 | 3,234 | 37.5 (35.3, 39.7) |
| Basic activities of daily living | ||||||
| No limitations | 3,944 | 13,857 | 75.3 (74.0, 76.7) | 2,175 | 7,788 | 90.3 (88.9, 91.7) |
| Limitations | 1,268 | 4,539 | 24.7 (23.3, 26.0) | 228 | 836 | 9.7 (8.3, 11.1) |
| Instrumental activities of daily living | ||||||
| No limitations | 4,148 | 14,538 | 79.0 (77.7, 80.3) | 2,161 | 7,730 | 89.6 (88.2, 91.0) |
| Limitations | 1,064 | 3,857 | 21.0 (19.7, 22.3) | 242 | 894 | 10.4 (9.0, 11.8) |
Notes: CI = confidence interval; HRS = Health and Retirement Study.
Over 8 years and after adjustment for covariates, retirees with arthritis were 1.6–3.7 times more likely than retirees without arthritis to experience limitations (Table 2; IDRs [95% CIs]: large muscle tasks = 2.1 [1.6, 2.8], p < .001; mobility tasks = 1.6 [1.2, 2.2], p = .003; ADLs = 2.2 [1.0, 4.7], p = .001; IADLs = 3.7 [1.9, 7.4], p < .001). They were significantly more likely than those without arthritis to report limitations in “walk several blocks” and “climbing several flights” (mobility subtasks), “taking medication” and “shopping for groceries” (IADL subtasks), and in each of the activities of the large muscle subtasks. Arthritis was not significantly associated with individual ADL subtasks (Supplementary Table 2).
Table 2.
The Adjusted Incidence Density Ratios With 95% CI for Those With Arthritis (vs. No Arthritis) in Four Models Assessing Development of Limitations in Four Physical Functions (Large Muscle Tasks, Mobility, ADLs, and IADLs) by Selected Characteristics
| Large Muscle Tasks | Mobility | ADLs | IADLs | |||||
|---|---|---|---|---|---|---|---|---|
| IDR (95% CI) | p | IDR (95% CI) | p | IDR (95% CI) | p | IDR (95% CI) | p | |
| Arthritis (ref.: no arthritis) | ||||||||
| Yes | 2.1 (1.6, 2.8) | <.001 | 1.6 (1.2, 2.2) | .003 | 2.2 (1.0, 4.7) | .001 | 3.7 (1.9, 7.4) | <.001 |
| Demographic | ||||||||
| Age | 1.0 (1.00, 1.02) | — | 1.0 (1.00, 1.03) | — | 0.97 (0.94, 1.01) | — | 1.0 (0.96, 1.03) | — |
| Sex (ref.: male) | ||||||||
| Female | 1.1 (0.9, 1.3) | .40 | 1.3 (1.0, 1.2) | .07 | 0.9 (0.5, 1.5) | .51 | 1.5 (0.9, 2.7) | .16 |
| Race (ref.: Non-Hispanic white) | ||||||||
| Non-Hispanic black | 1.4 (1.1, 1.7) | .001 | 1.7 (1.3, 2.3) | <.001 | 2.2 (1.2, 3.8) | .001 | 1.5 (0.8, 2.9) | .23 |
| Non-Hispanic other | 1.8 (1.1, 3.0) | .01 | 1.1 (0.6, 2.0) | .74 | 0.7 (0.1, 3.4) | .79 | 2.1 (0.4, 11.1) | .37 |
| Hispanic | 1.4 (1.0, 2.0) | .02 | 1.3 (0.8, 2.0) | .29 | 1.7 (0.7, 4.1) | .09 | 1.7 (0.7, 4.0) | .24 |
| Marital status (ref.: not married/partnered) | ||||||||
| Married/partnered | 1.1 (1.0, 1.4) | .16 | 1.1 (0.9, 1.4) | .56 | 1.2 (0.7, 2.0) | .67 | 1.1 (0.6, 1.9) | .80 |
| Socioeconomic | ||||||||
| Education (ref.: college or greater) | ||||||||
| Less than college | 1.3 (0.9, 1.8) | .15 | 1.6 (1.1, 2.4) | .01 | 1.4 (0.6, 3.4) | .51 | 1.4 (0.6, 3.6) | .45 |
| Income (ref.: $40,000+) | ||||||||
| $0–$19,999 | 1.4 (1.1, 1.9) | .01 | 1.2 (0.9, 1.7) | .26 | 2.2 (1.1, 4.7) | .02 | 2.2 (1.0, 4.7) | .04 |
| $20,000–$39,999 | 1.5 (1.2, 2.0) | .001 | 1.3 (1.0, 1.8) | .07 | 2.8 (1.3, 6.1) | .01 | 4.0 (1.8, 9.0) | <.001 |
| Comorbidities | ||||||||
| Depressed (ref.: not depressed) | ||||||||
| Depressed | 1.2 (1.1, 1.4) | .01 | 1.1 (1.0, 1.4) | .13 | 1.7 (1.2, 2.6) | 2.4 (1.5, 3.8) | <.001 | |
| Obesity (ref.: not obese) | ||||||||
| Obese | 1.2 (1.0, 1.5) | .02 | 1.5 (1.2, 1.9) | <.001 | 1.3 (0.8, 2.1) | .15 | 1.6 (0.9, 2.7) | .09 |
| Chronic conditions (ref.: 0 CC) | ||||||||
| 1 CC | 1.5 (1.1, 1.9) | <.001 | 1.7 (1.2, 2.4) | .001 | 1.8 (0.9, 3.7) | .03 | 1.4 (0.6, 3.5) | .43 |
| 2+ CC | 1.4 (1.1, 1.8) | <.001 | 2.1 (1.6, 3.0) | <.001 | 2.2 (1.0, 5.7) | <.001 | 2.1 (1.0, 4.6) | .07 |
| Smoking status (ref.: never smoked) | ||||||||
| Previous smoker | 1.0 (0.8, 1.2) | .86 | 1.1 (0.8, 1.4) | .87 | 1.0 (0.6, 1.7) | 1.4 (1.0, 2.7) | .37 | |
| Current smoker | 1.1 (0.8, 1.5) | .86 | 1.0 (0.7, 1.4) | .87 | 0.7 (0.3, 1.5) | .93 | 1.7 (0.7, 4.0) | .37 |
| Physical activity | ||||||||
| Physical activity (ref.: active) | ||||||||
| Inactive | 1.1 (1.0, 1.3) | .31 | 1.3 (1.1, 1.6) | .02 | 3.2 (1.9, 5.3) | <.001 | 4.6 (2.6, 8.1) | <.001 |
| Somewhat active | 1.0 (0.9, 1.2) | .31 | 1.3 (1.1, 1.6) | <.001 | 1.9 (1.2, 2.9) | .001 | 1.9 (1.1, 3.2) | <.001 |
Notes: ADL = activities of daily living; IADL = instrumental activities of daily living; CC = chronic conditions; CI = confidence interval; IDR = incidence density ratio; ref. = reference. This model is also adjusted for birth cohort (not presented). “—” indicates no p value calculated for age.
Non-Hispanic black, less than a college education, lower incomes, depression, and any chronic condition were associated with higher IDRs in all four outcome measures.
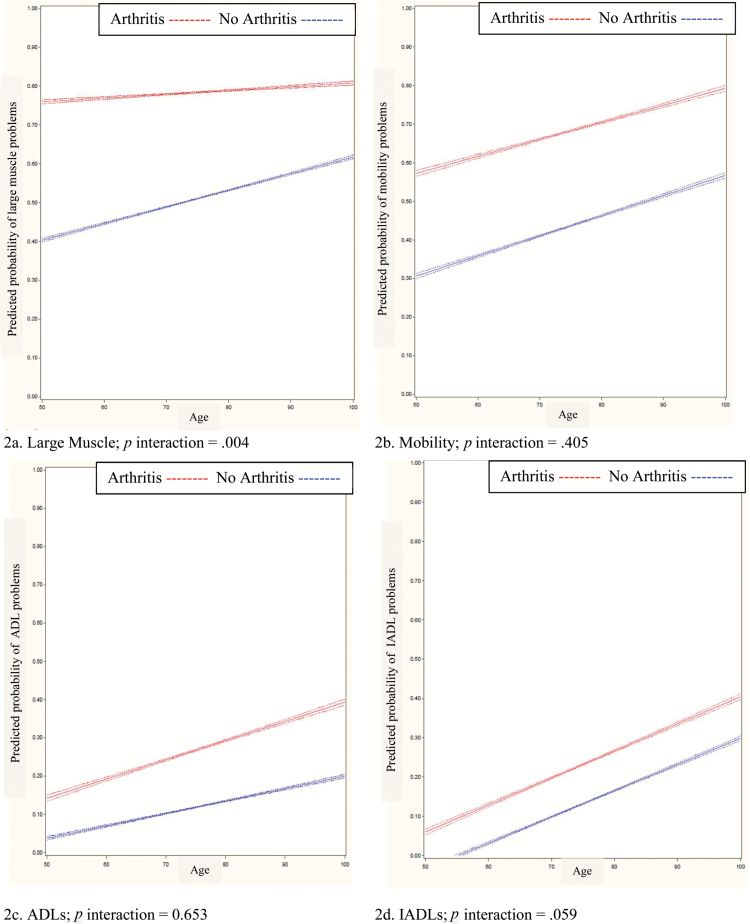
The only significant interaction effect between arthritis and age was large muscle tasks (Figure 2), indicating that as retirees with arthritis aged, their estimated rate of change to having limitations in large muscle tasks was slower than those without arthritis. There was a borderline significant (p = .059) association showing that those with arthritis developed IADL limitations at a greater rate. Significant subtask interactions were found for “getting up from a chair,” “pushing/pulling objects,” and “walking several blocks” suggesting that the number of retirees without arthritis who went from no difficulty to having difficulty for each item was greater as they aged then those with arthritis (Supplementary Table 2).
Figure 2.
Each line, flanked by its 95% confidence limit, represents the predicted probability of “any difficulty” for each of the four physical functions across age, by arthritis status. A significant p value indicates that these associations changed differently with age for those with arthritis versus without arthritis. Retirees without arthritis showed greater changes with increasing age in the prevalence of large muscle limitations (a). There were no significant associations for mobility (b), activities of daily living (ADLs) (c), or instrumental activities of daily living (IADLs) (d). The magnitude of these interaction effects was small (range 0.01–0.02/year of age).
Discussion
Overall, this study found that retirees with arthritis have lower physical function at an earlier age than those without arthritis, but the rate of decline in physical function as they age is no greater, and is in fact slower for the subtasks “getting up from a chair,” “pushing/pulling objects,” and “walking several blocks.” This study underscores how large the effect of arthritis is on physical function even in people healthy enough to work to retirement. After controlling for covariates that are associated with decreased physical function, such as socioeconomic factors, comorbidities, and physical function, arthritis remained as one of the strongest, independent factor associated with limitation in physical function, with IDRs ranging from 1.6 to 3.7.
The largest effect was seen for IADLs (IDR = 3.7), with taking medications (IDR = 6.4) and shopping for groceries (IDR = 3.3) as the subtasks most affected by arthritis status. Although retirees with arthritis were significantly more likely to have difficulty with ADLs, no one single subtask in ADL was significantly associated with some difficulty, which may be related to the sample size of people with ADL problems. Retirees with arthritis were more likely to report limitations in all subtasks of the large muscle indices, indicating that tasks that require high levels of lower and upper extremity strength (pushing/pulling large objects, getting up from a chair), awkward postures (stooping/kneeling/crouching), or endurance (sitting for 2 hours) are particularly difficult for retirees with arthritis. Mobility was least affected in our study (IDR = 1.6) in comparison to the other indices. The subtasks most affected were related to long distance mobility (walking several blocks, climbing several flights).
To our knowledge, this is the first study to examine whether limitations in physical function changed differently with age for retirees with arthritis. Retirees with arthritis did not have a significantly increased rate of development of limitations in mobility, ADLSs, and IADLs after controlling for other factors. These results suggest that although retirees with arthritis start with a greater level of limitations in physical function, the rate at which new retirees with arthritis develop limitation is similar to those without arthritis. Retirement, then, does not exacerbate physical function limitations in people with arthritis.
Retirees with arthritis appeared to be less likely than retirees without arthritis to develop limitations in physical function in large muscle tasks as they aged. A ceiling effect may explain this unexpected result. Because 78% of retirees with arthritis at baseline reported limitations in large muscle function, there were fewer retirees with arthritis without such baseline limitations than those without arthritis available to develop these limitations during follow-up. Only three subtasks had significant differences in rates between those with and without arthritis, “getting up from a chair,” “pushing/pulling objects,” and “walking several blocks.” As with large muscle tasks, retirees without arthritis were more likely to develop limitations in these areas.
Our research emphasizes that preventing disability and limitations in physical function are important goals before and after retirement. People with arthritis start retirement with higher levels of disability, and continue to lose physical abilities at the same rate as those who do not have arthritis, leading to a much higher overall prevalence of physical function limitations at all ages. Addressing modifiable risk factors that affect physical function might help reduce the effects of arthritis on physical function limitations. For example, being inactive or only somewhat physically active was associated with greater limitations in ADLs and IADLs. Encouraging people with arthritis at all ages to participate in evidence-based programs that promote appropriate physical activity for people with arthritis, such as “Walk with Ease,” “Enhanced Fitness,” “Active Living Everyday,” or “Fit & Strong” (25), could help reduce existing limitations.
This study has several limitations. Arthritis status was from self-report. Although a similar definition of doctor-diagnosed arthritis has been shown to be a valid measure for surveillance purposes (26), different methods of case definition result in different prevalences of limitations (27). Additionally, we could not parse out subtypes of arthritis. Subtypes of arthritis, such as osteoarthritis or rheumatoid arthritis, will affect physical function differently. Physical functions were not validated by objective performance measures. Research has suggested that self-report is only moderately associated with actual performance and can be affected by many factors (28). We have controlled for many potentially confounding factors, but residual confounding is a component of all observational studies.
We could not assess the severity of arthritis, so we could not examine whether more severe arthritis was directly associated with worse physical functioning. Data on mediators of physical function limitations such as pain, disease-modifying treatments, and other interventions were not available in the data set, and therefore could not be considered in the analysis. Finally, the preferred method of base-year weighting does not correct for attrition (17).
This study also has several strengths. First, the complex, multiple stage sampling design helped ensure a nationally representative sample of civilian, noninstitutionalized people aged 51 years and older. This sampling enhances external validity and enables us to generalize our results. Second, the large sample size increased statistical power and allowed us to examine multiple associations. Third, the use of generalized estimating equations reduced the effects of missing data and provided a more accurate estimate of relationships (22,23). Fourth, we looked at the average change in physical function limitations by age.
In summary, 68% of retirees in our sample had arthritis, and those with arthritis were significantly more likely to have limitations in all types of physical functions than those without. This makes arthritis a significant public health hazard for older adults because it is common and is associated with greater physical function limitations at all ages. Providing interventions that reduce the effect of arthritis on physical function limitations (eg, interventions to increase physical activity, to learn self-management skills, and to achieve and maintain a healthy weight) has good potential to help those with arthritis maintain physical function.
Supplementary Material
Please visit the article online at http://biomedgerontology.oxfordjournals.org/ to view supplementary material.
Funding
This work was supported by funding for Dr. Nancy Baker under an appointment to the Research Participation program at the CDC, administered by the Oak Ridge Institute for Science and Education and as a Visiting Scholar through the Center for Rehabilitation Research using Large Datasets at the University of Texas Medical Branch (funded by the National Institutes of Health—National Center for Medical Rehabilitation Research in the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke [grant # R24-HD065702]). The Health and Retirement Study is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
Supplementary Material
Acknowledgments
We acknowledge Dr. Kristina Theis who was instrumental in developing conceptual elements for this article. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1. Barbour KE, Helmick CG, Theis K, Murphy LP, Hootman JM, Brady TJ. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2010–2012. MMWR. 2013;62:869–873. [PMC free article] [PubMed] [Google Scholar]
- 2. Brault MW, Hootman JM, Helmick CG, Theis KA, Armour BS. Prevalence and most common causes of disability among adults—United States, 2005. MMWR. 2009;58:412–426. [PubMed] [Google Scholar]
- 3. Waddell G, Burton AK. Is Work Good for Your Health and Well-being? London, UK: The Stationary Office (TSO); 2006. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/214326/hwwb-is-work-good-for-you.pdf. Accessed April 19, 2016. [Google Scholar]
- 4. Johnston DW, Lee W-S. Retiring to the good life? The short-term effects of retirement on health. Econ Lett. 2009;103:8–11. doi.org/10.1016/j.econlet.2009.01.015 [Google Scholar]
- 5. Dave D, Rashad I, Spasojevic J. The effects of retirement on physical and mental health outcomes. South Econ J. 2008;75:497–523. [Google Scholar]
- 6. Dwyer DS, Mitchell OS. Health problems as determinants of retirement: are self-rated measures endogenous? J Health Econ. 1999;18:173–193. [DOI] [PubMed] [Google Scholar]
- 7. Denton M, Plenderleith J, Chowhan J. Health and disability as determinants for involuntary retirement of people with disabilities. Can J Aging. 2013;32:159–172. doi:10.1017/S0714980813000202 [DOI] [PubMed] [Google Scholar]
- 8. Hauser RM, Willis RJ. Survey design and methodology in the Health and Retirement Study and the Wisconsin Longitudinal Study. Popul Dev Rev. 2004;30(suppl: Aging, Health, and Public Policy):209–235. [Google Scholar]
- 9. RAND HRS Data, Version N. Santa Monica, CA: RAND Center for the Study of Aging; 2014. [Google Scholar]
- 10. Moldoff M, Chien S, Campbell N, et al. RAND HRS Income and Wealth Imputations, Version N. Santa Monica, CA: RAND Center for the Study of Aging; 2014. [Google Scholar]
- 11. Health and Retirement Study. Sample Sizes and Response Rates 2011 http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf. Accessed April 19, 2016.
- 12. Fonda S, Herzog AR. Documentation of Physical Functioning Measured in the Heath and Retirement Study and the Asset and Health Dynamics Among the Oldest Old Study University: Survey Research Center; 2004 http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf. Accessed April 19, 2016.
- 13. Centers for Disease Control and Prevention. Recommended BMI-for-age Cutoffs 2014 http://www.cdc.gov/nccdphp/dnpao/growthcharts/training/bmiage/page4.html. Accessed April 19, 2016.
- 14. Steffick D, Wallace RB, Herzog AR, Ofstedal MB, Fonda S, Langa K. Documentation of Affective Functioning Measures in the Health and Retirement Study. Survey Research Center. Ann Arbor, MI: University of Michigan; 2000. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf. Accessed April 19, 2016. [Google Scholar]
- 15. Heeringa SG, Connor JH. Technical Description of the Health and Retirement Survey Sample Design. Ann Arbor, MI: University of Michigan; 1995. http://hrsonline.isr.umich.edu/index.php?p=userg&jumpfrom=HS. Accessed April 19, 2016. [Google Scholar]
- 16. Ofstedal MB, Weir DR, Chen K-T, Wagner J. Updates to HRS Sampling Weights (DR-013). Ann Arbor, MI: Survey Research Center; 2011. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-013.pdf. Accessed April 19, 2016. [Google Scholar]
- 17. Health and Retirement Study. Sampling Weights ND. http://hrsonline.isr.umich.edu/sitedocs/wghtdoc.pdf. Accessed April 19, 2016. [Google Scholar]
- 18. SAS Institute Inc. SAS/STAT 9.3 User’s Guide. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 19. Cumming G. Inference by eye: reading the overlap of independent confidence intervals. Stat Med. 2009;28:205–220. doi:10.1002/sim.3471 [DOI] [PubMed] [Google Scholar]
- 20. Research Triangle Institute. SUDAAN Language Manual. Vol. 1–2, Release 11. Research Triangle Park, NC: Research Triangle Institute; 2012. [Google Scholar]
- 21. Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 22. Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 23. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 24. Manton KG, Gu X, Lowrimore GR. Cohort changes in active life expectancy in the U.S. elderly population: experience from the 1982–2004 National Long-Term Care Survey. J Gerontol. 2008;63B:S269–S81. doi:10.1093/geronb/63.5.S269 [DOI] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention. Physical Activity 2015 http://www.cdc.gov/arthritis/interventions/physical-activity.html. Accessed April 19, 2016.
- 26. Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32:340–347. [PubMed] [Google Scholar]
- 27. Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80:945–949. doi:10.2105/ajph.80.8.945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cress ME, Schechtman KB, Mulrow CD, Fiatarone MA, Gerety MB, Buchner DM. Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc. 1995;43:93–101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.