Abstract
Maternal depression, a non-psychotic depressive episode of mild to major severity, is one of the major contributors of pregnancy-related morbidity and mortality. Maternal depression (antepartum or post partum) has been linked to negative health-related behaviours and adverse outcomes, including psychological and developmental disturbances in infants, children, and adolescents. Despite its enormous burden, maternal depression in low-income and middle-income countries remains under-recognised and undertreated. In this Series paper, we systematically review studies that focus on the epidemiology of perinatal depression (ie, during antepartum and post-partum periods) among women residing in low-income and middle-income countries. We also summarise evidence for the association of perinatal depression with infant and childhood outcomes. This review is intended to summarise fi ndings from the existing literature, identify important knowledge gaps, and set the research agenda for creating new generalisable knowledge pertinent to increasing our understanding of the prevalence, determinants, and infant and childhood health outcomes associated with perinatal depression. This review is also intended to set the stage for subsequent work aimed at reinforcing and accelerating investments toward providing services to manage maternal depression in low-income and middle-income countries.
Keywords: antepartum depression, postpartum depression, LAMICS, maternal depression
Introduction
Perinatal depression is typically defined as a nonpsychotic depressive episode of mild to major severity that occurs during pregnancy or postnatally.1-3 Historically much greater emphasis has been placed on perinatal depression during the postpartum period, and relatively less attention has been paid to depression in the antepartum period.4,5 Pregnancy is a major life event that is inevitably accompanied by social, psychological and hormonal changes.6 These changes can trigger depressive episodes with serious implications for both maternal and infant outcomes.7-9 The prevalence of antepartum depression ranges from 7 to 15% in high-income countries2,10 and 19 to 25% in low-and middle-income countries (LAMICs).11 Notably, the prevalence of postpartum depression among women residing in high income countries is reported to be approximately 10%12 and 20% for women in LAMICs.3 The high prevalence of perinatal depression is influenced by a number of risk factors including increased somatic symptoms, 13 exposure to intimate partner violence, 14 lack of social support,15 unintended pregnancy16 and high rates of relapse of depression during the perinatal period.17 Antepartum depression has been linked to negative health-related behaviors and adverse outcomes, including poor nutrition, increased substance use, inadequate prenatal care, preeclampsia, low birth weight, preterm delivery, postpartum depression, and suicide.18-23 Women who experience antepartum depression often continue to experience depressive symptoms into the postpartum period, with more than 54% of those with postpartum depression reporting depressive episodes before or during pregnancy.5,24 Despite its enormous burden, antepartum depression in LAMICs remains under-recognized and under-treated,25 in part, because greater priority has been assigned to preventing deaths related to obstetric complications.3 Untreated antepartum depression is of concern because of its association with postpartum depression, and poor infant physical and neurocognitive developmental outcomes.4,26-30 A prior Lancet series on maternal mental health primarily focused on the effects of mood and anxiety disorders during the perinatal period, as well as other psychiatric disorders including bipolar disorder, psychoses, personality disorders, and eating disorders.31 With the exception of one study, all other studies included in the series focused on women residing in high-income countries. Therefore, the primary purpose of this report is to systematically review studies that focused on (1) the prevalence and risk factors of perinatal depression; and (2) the association of perinatal depression with infant and childhood outcomes among women residing in LAMICs. This review is intended to identify important knowledge gaps and to set the research agenda for creating new generalizable knowledge pertinent to increasing our understanding of the prevalence, determinants and infant health outcomes associated with perinatal depression.
Materials and methods
Meta-analysis
Published research papers were retrieved and included in this meta-analysis according to guidelines for Meta-Analysis of Observational Studies in Epidemiology (MOOSE).32 Given that the studies included in this review differed with regard to population samples and depression assessment tools, pooled estimates were calculated using the random effects model to take into account between study heterogeneity.33 We refer to the random effects estimate as the pooled prevalence estimate representing the weighted average of the prevalence estimates within the meta-analysis. The pooled prevalence estimate was consistent when the analysis was repeated using a fixed-effects model. A sensitivity analysis that allowed for omitting one study at a time and recalculating the pooled prevalence for the remainder of those studies in the meta-analysis showed that none of the studies substantially influenced the pooled estimates. Data analysis was performed using the metan procedure in STATA (version 14, STATA Corporation, College Station, TX, USA).
Results
Literature search for meta-analysis
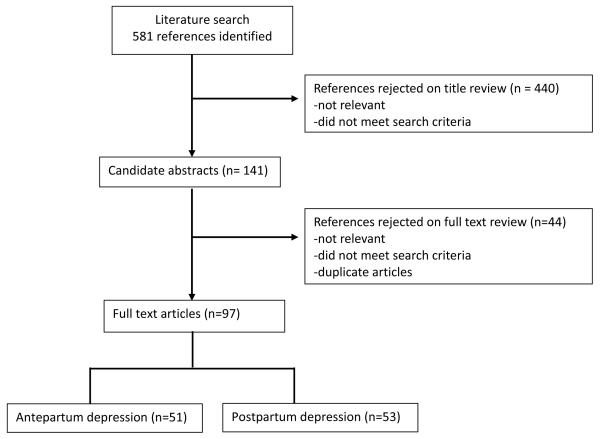
Figure 1 shows the study selection process and results from the literature search for the meta-analyses. The systematic search yielded 581 total articles. We excluded reviews, duplicates, studies conducted in high income countries and studies that did not report prevalence of antepartum or postpartum depression. We included a total of 51 full-length English language papers that reported on the prevalence of antepartum depression and 53 studies on the prevalence of postpartum depression.
Figure 1.
Flow chart of systematic literature review of articles in perinatal depression prevalence in low-income and middle-income countries. The search was done on April 5, 2016. *Seven studies assessed both antepartum and post-partum depression.
Literature search for perinatal depression with infant and childhood outcomes
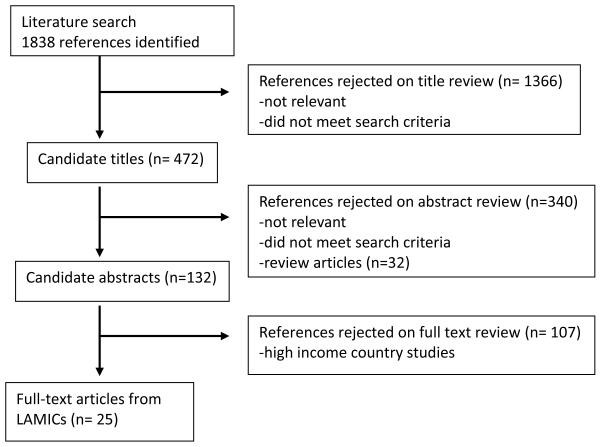
Figure 2 shows the study selection process and results from the literature search for articles examining the association of perinatal depression with infant and childhood outcomes. An initial search returned a total of 1,838 titles. We excluded reviews, duplicates, studies conducted in high income countries and studies that did not examine the relationship of perinatal depression with infant and childhood outcomes. We included a total 25 studies that reported on association of perinatal depression (antepartum or postpartum) and childhood outcomes (five assessing antepartum and 20 assessing postpartum depression).
Figure 2.
Flow chart of systematic literature review of articles assessing associations of perinatal depression with infant and childhood outcomes in low-income and middle-income countries
Prevalence of antepartum depression
A total of 51 studies were included in the meta-analysis which represented research conducted in 20 LAMICs with a total of 48,904 participants. Characteristics of populations considered in the selected studies are presented in Table 1. Of the 51 studies, 15 studies were from Brazil, six from Turkey, four from South Africa, three from China, three from Pakistan, and the rest (one or two studies) from other LAMICs (i.e., Bangladesh, Cote d'Ivoire, Ethiopia, Ghana, Jamaica, Jordan, Malawi, Malaysia, Mexico, Nepal, Papa New Guinea, Peru, Tanzania, Thailand, and Vietnam). Included studies were published between 1998 and 2015, with sample sizes that ranged from 29 in Brazil34 to 20,920 participants in Ghana.35 Antepartum depression was determined using Structured Clinical Interview for DSM-IV (SCID) in four studies, Edinburgh Postnatal Depression Scale (EPDS) in 22 studies, Patient Health Questionnaire-9 (PHQ-9) in four studies, Mini International Neuropsychiatric Interview (MINI) in four studies, Hamilton Depression Scale in four studies, Beck Depression Inventory (BDI) in three studies and other screening and diagnostic scales including Aga Khan University Anxiety and Depression Scale, Composite International Diagnostic Interview, Johns Hopkins Symptom Checklist, Primary Care Evaluation of Mental Disorders, Self-Rating Depression Scale, and Self-Reporting Questionnaire in other studies. As shown in Table 1, the pooled prevalence estimate of antepartum depression was 25.3% (95% CI 21.4-29.6%) across 51 studies. Significant heterogeneity was observed between studies (P-value <0.001). Visual inspection of the funnel plot showed some evidence of the presence of significant publication bias, and this was confirmed by the Egger’s test for publication bias (H0: intercept = 5.89; P-value = 0.0092). A sensitivity analysis was completed after excluding the study with the largest sample size35 from the summary analysis. In this sensitivity analysis, the pooled antepartum depression prevalence for the remaining studies was 25.8% (95% CI 22.8-29.0%).
Table 1.
Prevalence of antepartum depression from low and middle income countries
| Author, Year | Country | Depression Assessment |
Prevalence% (95%CI) |
Weight |
|---|---|---|---|---|
| Da-Silva, 1998 | Brazil | EPDS | 37.9 (22.4-56.4) | 0.10 |
| Chandran, 2002 | Thailand | CIS-R | 16.2 (12.7-20.4) | 0.69 |
| Lovisi, 2005 | Brazil | CIDI | 19.1 (14.5-24.7) | 0.50 |
| Azidah, 2006 | Malaysia | EPDS | 30.2 (26-34.8) | 1.26 |
| Gulseren, 2006 | Turkey | EPDS | 21.6 (15.2-29.7) | 0.30 |
| Limlomwongse 2006 | Thailand | EPDS | 20.5 (17.5-23.9) | 1.41 |
| Faisal-Cury, 2007 | Brazil | BDI | 19.6 (16.1-23.6) | 0.97 |
| Shakya 2008 | Nepal | HAM-d | 50.0 (35.6-64.4) | 0.16 |
| Karacam 2009 | Turkey | BDI | 27.9 (25.3-30.7) | 2.97 |
| Luna Matos, 2009 | Peru | EPDS | 40.1 (33.9-46.7) | 0.76 |
| Mitsuhiro, 2009 | Brazil | CIDI | 12.9 (11.0-15.1) | 1.59 |
| Qiao, 2009 | China | HADS | 4.8 (3.3-7.0) | 0.34 |
| Pottinger, 2009 | Jamaica | EPDS | 25.0 (21.2-29.2) | 1.20 |
| Soares, 2009 | Brazil | PRIME-MD | 27.8 (24.6-31.2) | 2.03 |
| Golbasi, 2010 | Turkey | EPDS | 27.5 (22.4-33.3) | 0.73 |
| Kaaya, 2010 | Tanzania | HSCL | 39.5 (36.1-43.0) | 2.67 |
| Kakirau-Hagali, 2010 | Papa New Guinea | HSRQ | 20.0 (11.1-33.3) | 0.11 |
| Manzolli, 2010 | Brazil | PRIME-MD | 27.8 (24.6-31.2) | 2.03 |
| Husain, 2011 | Pakistan | EPDS | 25.8 (23.5-28.2) | 3.69 |
| Mohammad, 2011 | Jordan | EPDS | 19.0 (15.2-23.4) | 0.77 |
| Narseen 2011 | Bangladesh | EPDS | 18.0 (15.4-21.0) | 1.51 |
| Rochat, 2011 | South Africa | SCID | 47.7 (38.5-57.0) | 0.39 |
| Senturk, 2011 | Turkey | EPDS | 33.1 (29.8-36.6) | 2.29 |
| Ali, 2012 | Pakistan | HADS | 16.8 (11.8-23.3) | 0.33 |
| da Silva, 2012 | Brazil | HADS | 23.6 (21.4-26.0) | 3.41 |
| Li, 2012 | China | EPDS | 39.0 (35.1-43.1) | 1.94 |
| Manikkam, 2012 | South Africa | EPDS | 38.5 (33.8-43.4) | 1.30 |
| Melo, 2012 | Brazil | EPDS | 24.3 (21.0-27.9) | 1.57 |
| Pinheiro, 2012 | Brazil | MINI | 17.8 (15.3-20.6) | 1.72 |
| Silva, 2012 | Brazil | EPDS | 20.5 (18.1-23.1) | 2.36 |
| Dibaba, 2013 | Ethiopia | EPDS | 19.9 (17.0-23.2) | 1.42 |
| Fadzil, 2013 | Malaysia | MINI | 8.6 (5.3-13.8) | 0.20 |
| Farias, 2013 | Brazil | MINI | 15.1 (11.1-20.2) | 0.43 |
| Fisher, 2013a | Vietnam | EPDS | 41.4 (37.1-45.8) | 1.70 |
| Fisher, 2013b | Vietnam | EPDS | 28.2 (24.1-32.7) | 1.20 |
| Mahenge, 2013 | Pakistan | HSCL | 55.9 (53.1-58.7) | 4.13 |
| Yanikkerem, 2013 | Turkey | BDI | 10.9 (8.7-13.5) | 0.90 |
| Abujilban, 2014 | Jordan | EPDS | 57.0 (50.3-63.4) | 0.76 |
| Akçal Aslan, 2014 | Turkey | SCID | 16.8 (13.7-20.5) | 0.92 |
| Guo, 2014a | Ghana | PHQ-9 | 26.5 (21.7-31.9) | 0.79 |
| Guo, 2014b | Cote d’Ivoire | PHQ-9 | 27.8 (23.5-32.6) | 1.05 |
| Stewart, 2014 | Malawi | SCID | 10.7 (8.4-13.5) | 0.79 |
| Tomlinson, 2014 | South Africa | EPDS | 37.0 (34.2-39.8) | 3.79 |
| Tsai, 2014a | South Africa | EPDS | 42.0 (39.2-44.9) | 3.95 |
| Tsai, 2014b | South Africa | EPDS | 46.0 (40.9-51.2) | 1.27 |
| Vaz, 2014 | Brazil | MINI | 17.0 (12.7-22.4) | 0.47 |
| Barrios, 2015 | Peru | PHQ-9 | 29.4 (27.2-31.8) | 4.43 |
| Biratu, 2015 | Ethiopia | EPDS | 24.9 (20.8-29.3) | 1.04 |
| Couto, 2015 | Brazil | EPDS | 17.3 (13.1-22.6) | 0.50 |
| Ferreira, 2015 | Brazil | CES-D | 73.5 (67.1-79.1) | 0.57 |
| Fonseca-Machado, 2015 | Brazil | EPDS | 28.2 (23.8-33.1) | 1.03 |
| Lara, 2015 | Mexico | SCID | 9.0 (5.8-13.7) | 0.24 |
| Weobong, 2015 | Ghana | PHQ-9 | 9.9 (9.5-10.3) | 26.48 |
| Zeng, 2015 | China | SDS | 28.5 (23.6-33.9) | 0.84 |
| Overall | 25.3 (21.4-29.6) | 100.00 |
Abbreviations: CIDI-Composite International Diagnostic Interview; CIS-R-Clinical Interview Schedule; EPDS- Edinburgh Postnatal Depression Scale; BDI-Beck depression inventory; HAM-d-Hamilton – Depression Scale; HADS-Hospital Anxiety and Depression Scale; HSCL-John Hopkins Symptoms Checklist; MINI- Mini-International Neuropsychiatric Interview; PHQ-9-Patient Health Questionnaire -9; PRIME-MD-Primary Care Evaluation of Mental Disorders; SCID- Structured Clinical Interview for DSM-IV Diagnoses; SDS-Self Rating Depression Scale; SRQ-Self Reporting Questionnaire.
Fisher 2013a and Fisher 2013b are from the same publication; Tsai, 2014a and Tsai, 2014b are from the same publication; Guo, 2014a and Guo, 2014b are from the same publication.
Prevalence of postpartum depression
A total of 53 studies were included in the meta-analysis which represented research conducted in 23 LAMICs representing 38,142 participants. The characteristics of study populations are presented in Table 2. Of the 53 studies, seven studies were from Brazil, six from Turkey, four from India, four from Thailand, four from China, three from Mexico, three from Nigeria, three from Iran and the rest (one or two studies) from other LAMICs (Armenia, Ghana, Jordan, Lebanon, Malaysia, Mongolia, Morocco, Nepal, Pakistan, Peru, South Africa, Tunisia, Uganda, Vietnam and Zimbabwe). Included studies were published between 1998 and 2015, with sample sizes that ranged from 41 in Thailand36 to 13,360 participants in Ghana.37 Among the studies, postpartum depression was predominantly determined using the EPDS. The EPDS was used in 38 studies, PHQ-9 in three studies, MINI in two studies, BDI in two studies and other screening and diagnostic scales in other studies including Aga Khan University Anxiety and Depression Scale, Center for Epidemiological Studies Depression Scale, Clinical Interview Schedule, Health Related Self Report Scale, Maternity Blues Scale, Self-Reporting Questionnaire, and Structured Clinical Interview for DSM-IV Diagnoses. As shown in Table 2, the pooled prevalence estimate of postpartum depression was 19.0% (15.5-23.0%) across 53 studies. Significant heterogeneity was observed between studies (P-value <0.001). Visual inspection of the funnel plot showed no evidence of a significant publication bias, confirmed by the Egger’s test for publication bias (H0: intercept =1.09; P-value = 0.656). A sensitivity analysis was performed after excluding the study with the largest sample size35 from the summary analysis. In this sensitivity analysis, the pooled postpartum depression prevalence for the remaining studies was 19.6% (16.8-22.6%). Furthermore, the prevalence of postpartum depression was re-calculated after removing a study conducted in teenage mothers.38 In this analysis postpartum depression prevalence for the remaining studies was 19.7% (16.9-22.8%).
Table 2.
Prevalence of postpartum depression from low and middle income countries
| Author, Year | Country | Depression Assessment |
Prevalence % (95%CI) |
Weight |
|---|---|---|---|---|
| Pyasil, 1998a | Thailand | DSM-Screener | 23.1 (16.0-32.2) | 0.44 |
| Pyasil, 1998b | Thailand | DSM-Screener | 11.9 (6.8-19.9) | 0.24 |
| Cooper, 1999 | South Africa | SCID | 34.7 (27.5-42.7) | 0.79 |
| Chaaya, 2002 | Lebanon | EPDS | 21.0 (17.3-25.3) | 1.56 |
| Chandran, 2002 | India | CIS—R | 19.8 (16.0-24.2) | 1.35 |
| Ekuklu, 2004 | Turkey | EPDS | 40.4 (33.4-47.8) | 1.02 |
| Faisal-Cury, 2004 | Brazil | BDI | 15.9 (11.2-22.1) | 0.55 |
| Fisher, 2004 | Viet Nam | EPDS | 32.9 (29.0-37.1) | 2.70 |
| Adewuya, 2005 | Nigeria | MBS | 31.3 (27.4-35.5) | 2.56 |
| Agoub, 2005 | Morocco | MINI | 18.7 (13.1-25.9) | 0.52 |
| Aydin, 2005 | Turkey | EPDS | 34.6 (31.2-38.1) | 3.91 |
| Adewuya, 2006 | Nigeria | EPDS | 20.9 (17.5-24.8) | 1.87 |
| Azidah, 2006 | Malaysia | EPDS | 22.8 (19.0-27.1) | 1.76 |
| Ho-Yen, 2006 | Nepal | EPDS | 4.9 (3.2-7.4) | 0.47 |
| Husain, 2006 | Pakistan | EPDS | 36.0 (28.7-44.0) | 0.81 |
| Limlomwongse, 2006 | Thailand | EPDS | 16.8 (14.0-20.0) | 2.03 |
| Pitanupong, 2007 | Thailand | EPDS | 11.0 (8.4-14.2) | 1.05 |
| Xie, 2007 | China | EPDS | 17.3 (13.8-21.5) | 1.26 |
| Ebeigbe, 2008 | Nigeria | EPDS | 27.2 (21.7-33.5) | 1.01 |
| Kara, 2008 | Turkey | BDI | 17.0 (12.0-23.6) | 0.55 |
| Tannous, 2008 | Brazil | EPDS | 20.7 (16.3-25.9) | 1.06 |
| Ali, 2009 | Pakistan | AKUADS | 28.8 (24.7-33.3) | 2.04 |
| Gomez-Beloz, 2009 | Peru | PHQ-9 | 41.3 (39.3-43.3) | 13.33 |
| Pollock, 2009 | Mongolia | SRQ | 9.1 (7.5-11.0) | 2.05 |
| Wan, 2009 | China | EPDS | 15.5 (12.3-19.4) | 1.23 |
| Chibanda, 2010 | Zimbabwe | EPDS | 33.0 (27.0-39.6) | 1.10 |
| Kirpinar, 2010 | Turkey | EPDS | 17.7 (14.5-21.4) | 1.66 |
| Dubey, 2011 | India | EPDS | 6.0 (4.2-8.4) | 0.68 |
| Lobato, 2011 | Brazil | EPDS | 24.3 (21.5-27.4) | 3.54 |
| Mohammad, 2011 | Jordan | EPDS | 19.0 (15.2-23.4) | 1.29 |
| Ozbasaran, 2011 | Turkey | EPDS | 28.3 (23.4-33.7) | 1.41 |
| Petrosyan, 2011 | Armenia | EPDS | 14.4 (11.0-18.6) | 0.98 |
| Pinheiro, 2011 | Brazil | EPDS | 22.7 (18.6-26.8) | 1.65 |
| Piyasil, 2011 | Thailand | HRSR | 22.0 (11.9-37.1) | 0.17 |
| da Rocha, 2012 | Brazil | EPDS | 26.4 (18.9-35.6) | 0.49 |
| Kakyo, 2012 | Uganda | EPDS | 43.0 (36.3-49.9) | 1.17 |
| Pio de Almeida, 2012 | Brazil | EPDS | 16.2 (11.9-21.6) | 0.72 |
| Silva, 2012 | Brazil | EPDS | 16.5 (14.4-18.8) | 3.62 |
| Tavares, 2012 | Brazil | MINI | 8.5 (6.9-10.5) | 1.70 |
| Zhang, 2012 | China | EPDS | 31.2 (25.4-37.7) | 1.09 |
| Dewing, 2013 | South Africa | EPDS | 31.7 (26.2-37.7) | 1.28 |
| Goshtasebi, 2013 | Iran | EPDS | 5.5 (3.4-8.9) | 0.35 |
| Abdollahi, 2014 | Iran | EPDS | 9.9 (8.7-11.3) | 4.13 |
| Masmoudi, 2014 | Tunisia | EPDS | 19.2 (15.1-24.0) | 1.11 |
| Sadat, 2014 | Iran | EPDS | 20.7 (16.5-25.7) | 1.17 |
| Wu, 2014 | China | EPDS | 9.4 (6.2-14) | 0.45 |
| Bodhare, 2015 | India | PHQ-9 | 4.7 (2.7-7.9) | 0.29 |
| de Castro, 2015 | Mexico | EPDS | 10.6 (8.4-13.3) | 1.36 |
| Giri, 2015 | Nepal | EPDS | 30.0 (25.4-35.0) | 1.72 |
| Lara, 2015 | Mexico | SCID | 13.8 (9.9-18.8) | 0.66 |
| Mohamad, 2015 | Malaysia | EPDS | 14.3 (12.9-15.9) | 6.02 |
| Patel, 2015 | India | EPDS | 48.5 (40.2-56.9) | 0.79 |
| Turkcapar, 2015 | Turkey | EPDS | 15.4 (12.6-18.7) | 1.67 |
| Weobong, 2015 | Ghana | PHQ-9 | 3.8 (3.5-4.1) | 11.59 |
| Overall | 19.0 (15.5-23.0) | 100.00 |
Abbreviations: AKUADS –Aga Khan University Anxiety and Depression Scale; BDI-Beck Depression Inventory; CES-D—Center for Epidemiological Studies Depression Scale; CIS-R-Clinical Interview Schedule; DSM-Screener—6 item Depression Screener Based on DSM IV; EPDS- Edinburgh Postnatal Depression Scale; HRSR—Health Related Self Report Scale; MBS—Maternity Blues Scale; MINI- Mini-International Neuropsychiatric Interview; PHQ-9-Patient Health Questionnaire -9; SCID- Structured Clinical Interview for DSM-IV Diagnoses; SRQ-Self Reporting Questionnaire
Pyasil, 1998a and Pyasil, 1998b are from the same publication.
This meta-analysis underscores the high prevalence of antepartum and postpartum depression among women residing in LAMICs; namely about one in four women were identified as having antepartum depression and one in five women having postpartum depression. Several risk factors, including financial and socio-environmental distress, increase susceptibility to perinatal depression.39 Some investigators have speculated that pregnancy related hormonal changes might increase vulnerability for the onset or return of depression.40,41 For example, blunted memory and diminished anxiety during pregnancy have been associated with progesterone and glucocorticoids.42,43 Taken together, these seminal observations combined with reviews by others3,15 and the results of our current meta-analysis indicate that antepartum and postpartum depression are common morbidities among women residing in LAMICs.
Risk factors for maternal antepartum and postpartum depression
In this section, we provide a brief summary of studies that have assessed risk factors of perinatal depression in LAMICs.
Early life abuse
Child maltreatment, a severe early life stressor, includes all forms of physical, sexual and psychological maltreatment that pose harm to a child’s health, development or dignity.44 Child abuse tends to co-occur with one or more types of childhood maltreatment such as child neglect, and emotional abuse.45,46 One of the most widely studied types of child maltreatment is childhood sexual abuse. To this end, during the period of 2007–2013, the Centers for Disease Control and Prevention (CDC) and United Nations Children's Emergency Fund (UNICEF), in partnership with host country governments, communities, and academic institutions developed and administered Violence Against Children Surveys (VACS) in seven LAMICs (Cambodia, Haiti, Kenya, Malawi, Swaziland, Tanzania, and Zimbabwe). The investigators found more than 25% of girls and more than 10% of boys reported experiencing childhood sexual violence.47 On balance available evidence shows that child maltreatment, particularly sexual abuse, is highly prevalent among individuals in LAMICs with potential long-term impact on onset and course of perinatal depression.
The adverse health sequelae of child abuse has been primarily studied in populations residing in higher income countries and very few have been conducted among populations in LAMICs.48,49 Pregnant women with a history of childhood abuse have increased risks of psychiatric disorders50, 51, sleep disturbances,51 health risk behaviors52 and adverse pregnancy outcomes.53 However, few studies have examined associations of child abuse with perinatal depression in LAMICS. These few studies have shown that women who experienced child abuse have increased risk of antepartum depression. For example, Lara et al., in their study of pregnant Mexican women, found that a history of sexual abuse in childhood was associated with a 2.49-fold increased odds of antepartum depression (OR=2.49; 95% CI: 1.86-4.61) even after adjusting for history of depression, poor partner relations, and low social support.54 Further, Barrios et al. recently reported that a history of sexual and physical abuse in childhood was associated with a 2.47-fold increased odds of antepartum depression (OR=2.47, 95% CI: 1.79-3.40) among Peruvian women.51 Biological mechanisms underlying reported associations of child abuse with perinatal depression are thought to be related to disruptions of neurobiological stress response systems including the sympathetic nervous system, the serotonin system, and the hypothalamic-pituitary-adrenal axis.55-57 Moreover, brain neuroimaging studies have shown alterations in brain structure and function and deficits in gray and white matter volumes among victims of early life abuse.58
Adult abuse
Intimate partner violence (IPV), encompassing physical, psychological and sexual abuse, is a common type of abuse experienced by women worldwide. 59 In the World Health Organization multi-country study on domestic violence conducted in nine LAMICs and Japan,60,61 the prevalence of physical IPV was reported to range from 10% to 52%.61 Physical IPV is often accompanied by psychological abuse, and between 33-50% the cases have experienced sexual abuse also.61,62 These figures were further confirmed in a recently aggregated global and regional prevalence estimates.63 Women who experience IPV are more likely to have a history of abuse in childhood. 51 A substantial literature indicates that young girls who survive abuse in childhood are more likely to experience further re-victimization in adulthood.51,64,65 Few studies have examined the relationship between adult abuse and depression in pregnancy. Lara et al. noted that pregnant women who experienced abuse were significantly more likely to develop antepartum depression.66 A study from Peru found that pregnant women who were victims of IPV had a 4.1-fold (95% CI 2.79-5.97) and 5.8-fold (95% CI 3.33-10.08) risk for moderately severe and severe depression, respectively.14 Similar findings were reported by other investigators. 67-69 The mechanisms that underlie the relationship between exposure to IPV and perinatal depression include social, emotional and physical isolation, separation, loss, and the unpredictability exerted by the abuser upon the abused woman.70 In sum, available evidence indicates that IPV is highly prevalent in LAMICs and is an important risk factor for perinatal depression. It is clear that programs aimed at addressing the burden of untreated antepartum and postpartum depression need to take into account ubiquitous stressors, such as IPV.
Other risk factors
In addition to childhood abuse and abuse by intimate partner, maternal low educational attainment,54,71 low socioeconomic status at the time of pregnancy,54,71,72 lack of social support73 and history of mental illness have been consistently identified as risk factors of antepartum and postpartum depression in the LAMICS.74 For instance, Melo et al. found that low educational attainment was associated with 2.38-fold increased odds of antepartum depression (OR=2.38; 95% CI: 1.38-4.12) among Brazilian women.75 Furthermore, Lara et al. found that low maternal educational attainment was associated with more than 5-fold increased odds of postpartum depression among Mexican women (OR=5.61; 95% CI: 1.87-16.80).54 Finally, few studies have reported culture-specific factors contributing to perinatal depression. In some Asian cultures, a gender bias exists where there is preference for a male first-born child.76 This gender-preference has been reported to be stressful experience for some women. Of note, mothers who give birth to a female child are often blamed for the birth with increased risk of depression compared to mother who give birth to a male child.71
Perinatal depression in relation to infant and childhood outcomes
In the next sections we discuss studies that assessed risks of adverse infant and child health outcomes associated with maternal antepartum and/or postpartum depression. A total of 21 studies from LAMICs have examined associations of perinatal depression with infant and childhood outcomes with details indicated in the following sections.
Infant weight, prematurity and child growth
Consistent with the fetal programming hypothesis (discussed in the accompanying review article of this Series by Herba et al77), some investigators78,79-83 have shown that women with untreated prenatal depressive disorders are more likely to have medical complications of pregnancy and to deliver low birth weight infants and have a preterm delivery as compared with their counterparts without such depressive disorders.78,79,84 Rahman et al., for example, in their study of Pakistani women, found that those with antepartum depression (assessed using Schedules for Clinical Assessment in Neuropsychiatry) were nearly twice as likely to deliver low birth weight infants (OR=1.90; 95% CI: 1.30-2.90) as compared with non-depressed women.79 Similarly, Wado et al. in their study of Ethiopian women, found that antepartum depression (assessed using EPDS) was associated with 1.87-fold increased risk of low birth weight (OR=1.87; 95% CI: 1.09-3.21).78 Sanchez et al. in their case-control study of Peruvian women, found that antepartum depression (determined using the PHQ-9 instrument) was statistically significantly associated with increased odds of preterm birth (OR=3.67; 95% CI 2.09-6.46).84 Notably, a recent meta-analysis of 11 LAMICs (conducted during the postpartum period) showed that children of mothers with depression or depressive symptoms were 1.5-times as likely to be underweight (OR=1.5; 95% CI: 1.2-1.8) or stunted (OR=1.4; 95% CI: 1.2-1.7) compared to children of non-depressed mothers.85
Antepartum and postpartum depression have also been implicated in impaired postnatal infant growth. For instance, Nasreen et al., in their prospective cohort study of Bangladeshi women, found that depression (assessed using EPDS during the third trimester, 2-3, and 6-8 months postpartum) was associated with infant stunting.80 Additionally, Uguz et al., in their study of 90 Turkish women assessed at postpartum period found that newborns of women with major depression (determined using Structured Clinical interview for the Diagnostic and Statistical Manual of Mental Disorders (SCID)) had significantly lower gestational age at delivery (1.44 weeks, P-value=0.015) and lower birth weight (343 g, P-value=0.021) compared with infants of mothers without major depressive disorder.81 In another study, Ndokera et al. reported that infants delivered of depressed Zambian mothers were 0.58 kg (95% CI: 0.09-1.08) lighter and 1.95 cm (95% CI: 0.49-3.50) shorter than infants of non-depressed mothers.82 A recent study by Bakare et al. of infants (mean age=3.56±3.21 months) attending immunization clinics in Nigeria found that the mean weight and length of infants of depressed mothers were significantly lower than infants of non-depressed mothers.83 However, Tomlinson et al. in South Africa found no evidence of association between postpartum depression (assessed using SCID) at 2 months with infant growth at 2 and 18 months of age although maternal nutritional status was not taken into account 86. In summary, available evidence supports the notion that impaired intrauterine growth is associated with antepartum depression. Additionally, infants delivered of depressed mothers also appear to have deficits in postnatal growth as compared with infant delivered of mothers without depression.
Observations of depression during the postpartum period and impaired postnatal growth associations have been attributed to differences in breastfeeding practices and insecure infant-mother attachments among depressed and non-depressed mothers. Investigators have reported that depressed mothers are more likely to stop breastfeeding earlier than non-depressed mothers87,88. Tomlinson et al. in South Africa found that postpartum depression (at 2 months) was associated with insecure infant attachments assessed at age 18 months.89 Notably, infants of depressed mothers are known to have more frequent episodes of diarrhea and other childhood illnesses as compared with infants of non-depressed mothers.87,88 For instance, in Pakistan90 children born to depressed mothers were 3-times as likely (OR=3.1; 95% CI: 1.8-5.6) to have 5 or more episodes of diarrhea per year as compared with children born to non-depressed mothers. Similarly, in a Nigerian study focused on infant growth during the first 9 months of life, Adewuya et al.87 reported a significant increase in the average number of episodes of diarrhea and other infectious illnesses in infants of depressed mothers as compared with infants of non-depressed mothers (mean (standard deviation: SD) 5.23 [2.37] vs. 3.70 [4.14]). Recently, in a birth cohort study of 654 mother/child dyads in Ghana and Cote d’Ivoire, Guo et al. found that children of depressed mothers were 32% more likely to experience febrile illness as compared with children of non-depressed mothers.91 On balance, available epidemiologic evidence documents increased risks of diarrheal and febrile illnesses and impaired growth among children of mothers with antepartum and/or postpartum depression.
Child obesity
Another childhood outcome that merits consideration is childhood obesity. Childhood obesity is a growing concern and serious public health challenge in many LAMICs. 92The literature examining the effects of maternal depression on childhood obesity largely comes from high-income countries and remains inconsistent.93 Some,94,95 though not all,96 investigators have found statistically significant associations between maternal depressive symptoms and child obesity.94 Inconsistencies across studies have been attributed to differences in population characteristics such as race/ethnicity, child sex, and family socioeconomic status.94 Research, particularly those involving women and children from LAMICS, is needed to clarify the relationship of impaired and excess infant somatic growth in relation to maternal mood disorders.
Child neurodevelopmental and behavioral outcomes
Although there is a well-established body of evidence from high-income countries,31 few investigators have assessed child neurodevelopmental outcomes in relation to perinatal depression in LAMICs settings. Furthermore, findings of these few studies have been inconsistent. Below, we provide a brief summary of selected available studies.
In their study of mother-infant dyads in Barbados, Galler et al., found that maternal depressive symptoms predicted lower infant social and performance scores at 3 months. The authors also observed that depression at 6 months postpartum was statistically significantly associated with lower scores in motor development at the same age (P-value<0.05).97 Similar findings were reported from studies conducted in India, Bangladesh, South Africa, Brazil and Pakistan. Briefly, Patel et al. reported that perinatal depression was significantly associated with reduced mental development quotient scores of infants in India.88 Further, in their study among 221 mother-infant dyads enrolled in a Bangladesh micronutrient supplementation trial, Black et al. found that maternal postpartum depressive symptoms were inversely associated with infant developmental scores.98 The authors noted that infants whose mothers reported depressive symptoms were more likely to have low scores on the Bayley Scales of Infant Development and more likely to have fewer cognitive, motor, and orientation/engagement skills at 6-12 months of age as compared with infants whose mother reported no depressive symptoms.98 In South Africa, postpartum depression was statistically significantly associated with child behavior problems at age 2 years.99 Further, Quevedro et al. in their study from Pelotas, Brazil, found that postpartum depression was associated with delayed language development in infants at 12 months of age.100 Another study from Pelotas, Brazil found that postpartum depression at 2 months was associated with sleep disturbances of infants at 12 months of age. 101 Using a community based cross-sectional survey conducted at 3-24 months, Hadley et al in Ethiopia found that children with mothers who had higher symptoms of depression and anxiety (assessed using Hopkins Symptoms checklist) were statistically significantly more likely to score low in all measures of development even after adjusting for nutritional stunting. 102 Maternal postpartum depression was noted to be associated with 6-fold increased odds of being delayed for emotional development (OR=5.9; 95% CI: 3.0-11.9), language development (OR=5.4; 95% CI: 2.3-12.4) and delayed gross motor development (OR=2.8; 95% CI: 1.2-6.6) in Pakistan.103 We are aware of one recent study which failed to document an association between maternal prenatal psychological distress and infant temperament.104 In summary, available studies indicate that perinatal depression, particularly postpartum depression, has significant clinical and developmental consequences for children. Causal inferences from available studies are hindered by small sample sizes, and incomplete control of confounding factors. Consequently, there is a clear need for rigorously designed longitudinal studies to improve our understanding of the relation between perinatal depression and child neurodevelopmental and behavioral outcomes, particularly among populations residing in LAMICs. There are several plausible biological mechanisms on how antepartum and postpartum depression may affect child development. These are fully discussed in the accompanying review article of this Series by Herba and colleagues. 77
Conclusions
The results of our meta-analyses show that antepartum and postpartum depression in LAMICs are highly prevalent affecting about one in four and one in five women, respectively. This is consistent with recent systematic reviews that reported common mental disorders including depression during the perinatal period are more prevalent3,15 compared with non-pregnancy periods.3 Recently the US Preventive Services Task Force (USPSTF) published a clinically influential report recommending screening US pregnant and postpartum women for depression particularly in the presence of additional treatment supports (e.g., treatment protocols, care management, and availability of specially trained depression care clinicians).105 No such evidence-based guideline exists for LAMICs. A broader guideline by the World Health Organization suggests integrating mental health services into primary care as the most viable way of closing treatment gap for mental health in the LAMICS.106,107 One of the main challenges for such integration in the LAMICS has been the low recognition rates of mental disorders by primary care health workers, in part, due to shortage of clinicians with specialized training in assessing and managing the treatment of patients with mental health disorders. Developing protocols for early identification, treatment and preventing the damaging effects of perinatal depression in LAMICs settings are needed. Another remaining challenge is lack of cross-culturally valid perinatal depression screening and diagnostic instruments particularly during the antepartum period. There is a clear need for researchers to develop, refine and rigorously evaluate the predictive validity and reliability of perinatal depression assessment tools in the LAMICS. Such research will allow for identifying perinatal depression, and also measure the efficacy of traditional and novel treatment strategies in reproductive health systems. Integrated antenatal care programs aimed at identifying and treating women with antepartum and postpartum depression are needed because for many women in LAMICS, antenatal care is typically the first and only time of interaction with the health care system. As such, antenatal care visits provide critically important opportunities for mental health interventions to occur. Moreover, the recent United Nations General Assembly Sustainable Development Goals (SDG) Agenda, for the first time, has included promotion of mental health and well-being..108 Accordingly, mental health policy is likely to become part of country development plans and of bilateral and multilateral development assistance. The mental health of mothers during pregnancy and after childbirth ought to be included in this agenda.
Supplementary Material
Search strategy and selection criteria.
We searched PubMed, Embase, CINAHL, and BIOSIS Online without language restrictions using the following medical subject heading (MeSH) terms and search terms : “antenatal”, “ante-natal”, “ante-partum”, “depressive disorder”[MeSH], “depression”[MeSH], “major depressive disorder“[MeSH], “pregnancy”, “prenatal”, ”antepartum”, “perinatal”, “postnatal”, “peripartum”, “postpartum”, “post-natal”, “post-partum”, with no date restrictions. The MeSH terms used to restrict to low-income and middle-income countries can be found in the appendix. To be included, studies had to: define depression as occurring sometime in pregnancy or during post-partum period using screening or diagnostic assessment; report prevalence of perinatal depression; be full-length papers (conference abstracts, case studies, grey literature, and editorials were excluded); be studies from low-income and middle-income countries as defined by the World Bank country income groups; and be in English or with sufficiently detailed English abstracts to allow comparison of methods and main findings with other studies. Figure 1 summarises the selection of studies reporting on the prevalence of perinatal depression.
We used all the aforementioned search terms and MeSH terms and key terms combined with all MeSH terms for child outcomes to look for studies of the associations of perinatal depression with infant and childhood outcomes. These terms included “child development” [MeSH], “pregnancy complications” [MeSH], “infant behaviour” [MeSH], and “mother child relations” [MeSH]. To be included, studies had to meet the above criteria and also report quantitative associations between perinatal depression and infant/childhood outcomes. Figure 2 summarises the selection of studies reporting the association between perinatal depression and infant or childhood outcomes. We focus on infant and child outcomes measured up through the age of 5 years. The final search was done on March 31, 2016.
Key messages.
Studies in low-income and middle-income countries are needed to determine the prevalence and risk factors of perinatal depression
Rigorously designed longitudinal studies are needed to investigate the association of perinatal depression with infant birthweight and growth, including childhood obesity, and to improve understanding of the relation between perinatal depression and child neurodevelopmental and behavioural outcomes, particularly in low-income and middle-income countries
Integrated care programmes aimed at identifying and treating women with perinatal depression in low-income and middle-income countries are urgently needed
Acknowledgments
This research was supported by the National Institutes of Health (R01-HD-059835 and T37-MD0001449). The NIH had no further role in study design, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The authors wish to thank Dr. Lauren E. Friedman for her technical assistance with this research.
Footnotes
Authors’ contribution
BG and MAW developed the outline of this review. BG performed the literature search and data analysis. All authors contributed to the writing and editing of the manuscript. All authors have read and approved the final manuscript.
Conflict of interest
The authors have no competing interests to declare.
Ethical committee approval
Not applicable.
References
- 1.Bowen A, Muhajarine N. Antenatal depression. Can Nurse. 2006;102(9):26–30. [PubMed] [Google Scholar]
- 2.Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323(7307):257–60. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher J, Cabral de Mello M, Patel V, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139G–49G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- 5.Stewart DE, Robertson E, Dennis C-L, Grace SL, Wallington T. Postpartum depression: Literature review of risk factors and interventions. 2003.
- 6.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 7.Field T, Diego M, Hernandez-Reif M. Prenatal depression effects on the fetus and newborn: a review. Infant Behav Dev. 2006;29(3):445–55. doi: 10.1016/j.infbeh.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938–46. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- 9.Hollins K. Consequences of antenatal mental health problems for child health and development. Curr Opin Obstet Gynecol. 2007;19(6):568–72. doi: 10.1097/GCO.0b013e3282f1bf28. [DOI] [PubMed] [Google Scholar]
- 10.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–24. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahman A, Iqbal Z, Harrington R. Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med. 2003;33(7):1161–7. doi: 10.1017/s0033291703008286. [DOI] [PubMed] [Google Scholar]
- 12.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–83. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 13.Senturk V, Hanlon C, Medhin G, et al. Impact of perinatal somatic and common mental disorder symptoms on functioning in Ethiopian women: the P-MaMiE population-based cohort study. J Affect Disord. 2012;136(3):340–9. doi: 10.1016/j.jad.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gomez-Beloz A, Williams MA, Sanchez SE, Lam N. Intimate partner violence and risk for depression among postpartum women in Lima, Peru. Violence Vict. 2009;24(3):380–98. doi: 10.1891/0886-6708.24.3.380. [DOI] [PubMed] [Google Scholar]
- 15.Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010;123(1-3):17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 16.Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reprod Health. 2015;12:99. doi: 10.1186/s12978-015-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499–507. doi: 10.1001/jama.295.5.499. [DOI] [PubMed] [Google Scholar]
- 18.Horrigan TJ, Schroeder AV, Schaffer RM. The triad of substance abuse, violence, and depression are interrelated in pregnancy. Journal of Substance Abuse Treatment. 2000;18(1):55–8. doi: 10.1016/s0740-5472(99)00058-6. [DOI] [PubMed] [Google Scholar]
- 19.Llewellyn AM, Stowe ZN, Nemeroff CB. Depression during pregnancy and the puerperium. Journal of Clinical Psychiatry. 1997;58(Suppl 15):26–32. [PubMed] [Google Scholar]
- 20.Barrio L, Burt V. Depression in pregnancy: Strategies for primary care management. Dealing with an underdiagnosed undertreated problem. Women's Health in Primary Care. 2000;3:490–8. [Google Scholar]
- 21.Hoffman S, Hatch MC. Depressive symptomatology during pregnancy: evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychology. 2000;19(6):535–43. [PubMed] [Google Scholar]
- 22.Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol. 2000;95(4):487–90. doi: 10.1016/s0029-7844(99)00602-x. [DOI] [PubMed] [Google Scholar]
- 23.Najman JM, Andersen MJ, Bor W, O'Callaghan MJ, Williams GM. Postnatal depression-myth and reality: maternal depression before and after the birth of a child. Social Psychiatry and Psychiatric Epidemiology. 2000;35(1):19–27. doi: 10.1007/s001270050004. [DOI] [PubMed] [Google Scholar]
- 24.Burt VK, Quezada V. Mood disorders in women: focus on reproductive psychiatry in the 21st century--Motherisk update 2008. Can J Clin Pharmacol. 2009;16(1):e6–e14. [PubMed] [Google Scholar]
- 25.Oates M. Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. Br Med Bull. 2003;67:219–29. doi: 10.1093/bmb/ldg011. [DOI] [PubMed] [Google Scholar]
- 26.Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med. 2001;63(5):830–4. doi: 10.1097/00006842-200109000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Lusskin SI, Pundiak TM, Habib SM. Perinatal depression: hiding in plain sight. Can J Psychiatry. 2007;52(8):479–88. doi: 10.1177/070674370705200802. [DOI] [PubMed] [Google Scholar]
- 28.Preti A, Cardascia L, Zen T, et al. Obstetric complications in patients with depression--a population-based case-control study. J Affect Disord. 2000;61(1-2):101–6. doi: 10.1016/s0165-0327(99)00185-8. [DOI] [PubMed] [Google Scholar]
- 29.Steer RA, Scholl TO, Hediger ML, Fischer RL. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093–9. doi: 10.1016/0895-4356(92)90149-h. [DOI] [PubMed] [Google Scholar]
- 30.Larsson C, Sydsjo G, Josefsson A. Health, sociodemographic data, and pregnancy outcome in women with antepartum depressive symptoms. Obstet Gynecol. 2004;104(3):459–66. doi: 10.1097/01.AOG.0000136087.46864.e4. [DOI] [PubMed] [Google Scholar]
- 31.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19. doi: 10.1016/S0140-6736(14)61277-0. [DOI] [PubMed] [Google Scholar]
- 32.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 33.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 34.Da-Silva VA, Moraes-Santos AR, Carvalho MS, Martins ML, Teixeira NA. Prenatal and postnatal depression among low income Brazilian women. Braz J Med Biol Res. 1998;31(6):799–804. doi: 10.1590/s0100-879x1998000600012. [DOI] [PubMed] [Google Scholar]
- 35.Weobong B, Soremekun S, Ten Asbroek AH, et al. Prevalence and determinants of antenatal depression among pregnant women in a predominantly rural population in Ghana: the DON population-based study. J Affect Disord. 2014;165:1–7. doi: 10.1016/j.jad.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 36.Piyasil V. Anxiety and depression in teenage mothers: a comparative study. Journal of the Medical Association of Thailand. 1998;81(2):125–9. [PubMed] [Google Scholar]
- 37.Weobong B, Ten Asbroek AH, Soremekun S, et al. Determinants of postnatal depression in rural ghana: findings from the don population based cohort study. Depress Anxiety. 2015;32(2):108–19. doi: 10.1002/da.22218. [DOI] [PubMed] [Google Scholar]
- 38.Lara MA, Berenzon S, Juarez Garcia F, et al. Population study of depressive symptoms and risk factors in pregnant and parenting Mexican adolescents. Rev Panam Salud Publica. 2012;31(2):102–8. [PubMed] [Google Scholar]
- 39.Kitamura T, Shima S, Sugawara M, Toda MA. Stress and puerperal psychosis. Br J Psychiatry. 1991;158:290–1. doi: 10.1192/bjp.158.2.290. [DOI] [PubMed] [Google Scholar]
- 40.O'Hara MW. Postpartum depression. In: Alloy LB, editor. Series in Psychopathology. Springer-Verlag; New York: 1995. pp. 1–27. [Google Scholar]
- 41.Burt VK, Stein K. Epidemiology of depression throughout the female life cycle. J Clin Psychiatry. 2002;63(Suppl 7):9–15. [PubMed] [Google Scholar]
- 42.Brett M, Baxendale S. Motherhood and memory: a review. Psychoneuroendocrinology. 2001;26(4):339–62. doi: 10.1016/s0306-4530(01)00003-8. [DOI] [PubMed] [Google Scholar]; 2002;27:299–302. correction. [Google Scholar]
- 43.Newcomer JW, Craft S, Hershey T, Askins K, Bardgett ME. Glucocorticoid-induced impairment in declarative memory performance in adult humans. J Neurosci. 1994;14(4):2047–53. doi: 10.1523/JNEUROSCI.14-04-02047.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization . Guidelines for medico-legal care for victims of sexual violence. World Health Organization; Geneva: 2003. [Google Scholar]
- 45.Andrews G, Corry J, Slade T, Issakidis C, Swanston H. Child sexual abuse. In: Ezzati M, Lopez A, Rodgers A, Murray C, editors. Comparative quantification of health risks : global and regional burden of disease atrributable to selected major risk factors. World Health Organization; Geneva: 2004. pp. 1851–940. [Google Scholar]
- 46.Ehlert U. Enduring psychobiological effects of childhood adversity. Psychoneuroendocrinology. 2013;38(9):1850–7. doi: 10.1016/j.psyneuen.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 47.Sumner SA, Mercy AA, Saul J, et al. Prevalence of sexual violence against children and use of social services - seven countries, 2007-2013. MMWR Morb Mortal Wkly Rep. 2015;64(21):565–9. [PMC free article] [PubMed] [Google Scholar]
- 48.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 49.Wosu AC, Gelaye B, Williams MA. History of childhood sexual abuse and risk of prenatal and postpartum depression or depressive symptoms: an epidemiologic review. Arch Womens Ment Health. 2015;18(5):659–71. doi: 10.1007/s00737-015-0533-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hornor G. Child sexual abuse: consequences and implications. J Pediatr Health Care. 2010;24(6):358–64. doi: 10.1016/j.pedhc.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 51.Barrios YV, Gelaye B, Zhong Q, et al. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among pregnant women. PLoS One. 2015;10(1):e0116609. doi: 10.1371/journal.pone.0116609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Frankenberger DJ, Clements-Nolle K, Yang W. The Association between Adverse Childhood Experiences and Alcohol Use during Pregnancy in a Representative Sample of Adult Women. Womens Health Issues. 2015;25(6):688–95. doi: 10.1016/j.whi.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Christiaens I, Hegadoren K, Olson DM. Adverse childhood experiences are associated with spontaneous preterm birth: a case-control study. BMC Med. 2015;13:124. doi: 10.1186/s12916-015-0353-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lara MA, Navarrete L, Nieto L, Le HN. Childhood abuse increases the risk of depressive and anxiety symptoms and history of suicidal behavior in Mexican pregnant women. Rev Bras Psiquiatr. 2015;37(3):203–10. doi: 10.1590/1516-4446-2014-1479. [DOI] [PubMed] [Google Scholar]
- 55.Teicher MH, Samson JA, Polcari A, McGreenery CE. Sticks, stones, and hurtful words: relative effects of various forms of childhood maltreatment. Am J Psychiatry. 2006;163(6):993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- 56.Hart C, de Vet R, Moran P, Hatch SL, Dean K. A UK population-based study of the relationship between mental disorder and victimisation. Soc Psychiatry Psychiatr Epidemiol. 2012;47(10):1581–90. doi: 10.1007/s00127-011-0464-7. [DOI] [PubMed] [Google Scholar]
- 57.Watts-English T, Fortson BL, Gibler N, Hooper SR, De Bellis MD. The Psychobiology of Maltreatment in Childhood. Journal of Social Issues. 2006;62(4):717–36. [Google Scholar]
- 58.Teicher MH, Samson JA. Annual Research Review: Enduring neurobiological effects of childhood abuse and neglect. J Child Psychol Psychiatry. 2016;57(3):241–66. doi: 10.1111/jcpp.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization-national intimate partner and sexual violence survey, United States, 2011. Am J Public Health. 2015;105(4):e11–2. [PMC free article] [PubMed] [Google Scholar]
- 60.Garcia-Moreno C, Jansen HA, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006;368(9543):1260–9. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 61.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–8. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 62.Watts C, Zimmerman C. Violence against women: global scope and magnitude. Lancet. 2002;359(9313):1232–7. doi: 10.1016/S0140-6736(02)08221-1. [DOI] [PubMed] [Google Scholar]
- 63.WHO. World Helath Organization Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and nonpartner sexual violence. 2013
- 64.McCauley J, Kern DE, Kolodner K, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277(17):1362–8. [PubMed] [Google Scholar]
- 65.Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl. 2003;27(11):1247–58. doi: 10.1016/j.chiabu.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 66.Lara MA, Natera-Rey G, Berenzon S, et al. Intimate partner violence and depressive symptoms in pregnant Mexican women: national survey results. Rev Invest Clin. 2014;66(5):431–8. [PubMed] [Google Scholar]
- 67.Ludermir AB, Lewis G, Valongueiro SA, de Araujo TV, Araya R. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet. 2010;376(9744):903–10. doi: 10.1016/S0140-6736(10)60887-2. [DOI] [PubMed] [Google Scholar]
- 68.Ludermir AB, Valongueiro S, Araujo TV. Common mental disorders and intimate partner violence in pregnancy. Rev Saude Publica. 2014;48(1):29–35. doi: 10.1590/S0034-8910.2014048004538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Intimate Partner Violence and Depression Symptom Severity among South African Women during Pregnancy and Postpartum: Population-Based Prospective Cohort Study. PLoS Med. 2016;13(1):e1001943. doi: 10.1371/journal.pmed.1001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Campbell JC, Lewandowski LA. Mental and physical health effects of intimate partner violence on women and children. Psychiatr Clin North Am. 1997;20(2):353–74. doi: 10.1016/s0193-953x(05)70317-8. [DOI] [PubMed] [Google Scholar]
- 71.Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159(1):43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 72.Abujilban SK, Abuidhail J, Al-Modallal H, Hamaideh S, Mosemli O. Predictors of antenatal depression among Jordanian pregnant women in their third trimester. Health Care Women Int. 2014;35(2):200–15. doi: 10.1080/07399332.2013.817411. [DOI] [PubMed] [Google Scholar]
- 73.Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregnancy Childbirth. 2013;13:135. doi: 10.1186/1471-2393-13-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Faisal-Cury A, Tedesco JJ, Kahhale S, Menezes PR, Zugaib M. Postpartum depression: in relation to life events and patterns of coping. Arch Womens Ment Health. 2004;7(2):123–31. doi: 10.1007/s00737-003-0038-0. [DOI] [PubMed] [Google Scholar]
- 75.Melo EF, Jr., Cecatti JG, Pacagnella RC, Leite DF, Vulcani DE, Makuch MY. The prevalence of perinatal depression and its associated factors in two different settings in Brazil. J Affect Disord. 2012;136(3):1204–8. doi: 10.1016/j.jad.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 76.Mithra A. [Accessed on: 5/15/2016];Son preference in India: implications. For gender development. 2016 Available at: http://www.socialeconomics.org/Papers/Mitra4A.pdf.
- 77.Herba C, Glover V, Ramchandani PG, Rondon M. Maternal depression and mental health in early childhood: An examination of underlying mechanisms in low and middle income countries. Lancet Psychiatry. 2016 doi: 10.1016/S2215-0366(16)30148-1. [DOI] [PubMed] [Google Scholar]
- 78.Wado YD, Afework MF, Hindin MJ. Effects of maternal pregnancy intention, depressive symptoms and social support on risk of low birth weight: a prospective study from southwestern Ethiopia. PLoS One. 2014;9(5):e96304. doi: 10.1371/journal.pone.0096304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatr Scand. 2007;115(6):481–6. doi: 10.1111/j.1600-0447.2006.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Impact of maternal depressive symptoms and infant temperament on early infant growth and motor development: results from a population based study in Bangladesh. J Affect Disord. 2013;146(2):254–61. doi: 10.1016/j.jad.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 81.Uguz F, Sahingoz M, Sonmez EO, et al. The effects of maternal major depression, generalized anxiety disorder, and panic disorder on birth weight and gestational age: a comparative study. J Psychosom Res. 2013;75(1):87–9. doi: 10.1016/j.jpsychores.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 82.Ndokera R, MacArthur C. The relationship between maternal depression and adverse infant health outcomes in Zambia: a cross-sectional feasibility study. Child Care Health Dev. 2011;37(1):74–81. doi: 10.1111/j.1365-2214.2010.01129.x. [DOI] [PubMed] [Google Scholar]
- 83.Bakare MO, Okoye JO, Obindo JT. Introducing depression and developmental screenings into the national programme on immunization (NPI) in southeast Nigeria: an experimental cross-sectional assessment. Gen Hosp Psychiatry. 2014;36(1):105–12. doi: 10.1016/j.genhosppsych.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 84.Sanchez SE, Puente GC, Atencio G, et al. Risk of spontaneous preterm birth in relation to maternal depressive, anxiety, and stress symptoms. J Reprod Med. 2013;58(1-2):25–33. [PMC free article] [PubMed] [Google Scholar]
- 85.Surkan PJ, Kennedy CE, Hurley KM, Black MM. Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bull World Health Organ. 2011;89(8):608–15. doi: 10.2471/BLT.11.088187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tomlinson M, Cooper PJ, Stein A, Swartz L, Molteno C. Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev. 2006;32(1):81–6. doi: 10.1111/j.1365-2214.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- 87.Adewuya AO, Ola BO, Aloba OO, Mapayi BM, Okeniyi JA. Impact of postnatal depression on infants' growth in Nigeria. J Affect Disord. 2008;108(1-2):191–3. doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 88.Patel V, DeSouza N, Rodrigues M. Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Arch Dis Child. 2003;88(1):34–7. doi: 10.1136/adc.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tomlinson M, Cooper P, Murray L. The mother-infant relationship and infant attachment in a South African peri-urban settlement. Child Dev. 2005;76(5):1044–54. doi: 10.1111/j.1467-8624.2005.00896.x. [DOI] [PubMed] [Google Scholar]
- 90.Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrhoeal illness: --a cohort study. Arch Dis Child. 2007;92(1):24–8. doi: 10.1136/adc.2005.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Guo N, Bindt C, Te Bonle M, et al. Association of antepartum and postpartum depression in Ghanaian and Ivorian women with febrile illness in their offspring: a prospective birth cohort study. Am J Epidemiol. 2013;178(9):1394–402. doi: 10.1093/aje/kwt142. [DOI] [PubMed] [Google Scholar]
- 92.Poskitt EM. Childhood obesity in low- and middle-income countries. Paediatr Int Child Health. 2014;34(4):239–49. doi: 10.1179/2046905514Y.0000000147. [DOI] [PubMed] [Google Scholar]
- 93.Benton PM, Skouteris H, Hayden M. Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review. Appetite. 2015;87:259–82. doi: 10.1016/j.appet.2014.12.227. [DOI] [PubMed] [Google Scholar]
- 94.McConley RL, Mrug S, Gilliland MJ, et al. Mediators of maternal depression and family structure on child BMI: parenting quality and risk factors for child overweight. Obesity (Silver Spring) 2011;19(2):345–52. doi: 10.1038/oby.2010.177. [DOI] [PubMed] [Google Scholar]
- 95.Gross RS, Velazco NK, Briggs RD, Racine AD. Maternal depressive symptoms and child obesity in low-income urban families. Acad Pediatr. 2013;13(4):356–63. doi: 10.1016/j.acap.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 96.Gibson LY, Byrne SM, Davis EA, Blair E, Jacoby P, Zubrick SR. The role of family and maternal factors in childhood obesity. Med J Aust. 2007;186(11):591–5. doi: 10.5694/j.1326-5377.2007.tb01061.x. [DOI] [PubMed] [Google Scholar]
- 97.Galler JR, Harrison RH, Ramsey F, Forde V, Butler SC. Maternal depressive symptoms affect infant cognitive development in Barbados. J Child Psychol Psychiatry. 2000;41(6):747–57. [PubMed] [Google Scholar]
- 98.Black MM, Baqui AH, Zaman K, et al. Depressive symptoms among rural Bangladeshi mothers: implications for infant development. J Child Psychol Psychiatry. 2007;48(8):764–72. doi: 10.1111/j.1469-7610.2007.01752.x. [DOI] [PubMed] [Google Scholar]
- 99.Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A. Maternal postnatal depression and children's growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child. 2010;95(9):690–5. doi: 10.1136/adc.2009.164848. [DOI] [PubMed] [Google Scholar]
- 100.Quevedo LA, Silva RA, Godoy R, et al. The impact of maternal post-partum depression on the language development of children at 12 months. Child Care Health Dev. 2012;38(3):420–4. doi: 10.1111/j.1365-2214.2011.01251.x. [DOI] [PubMed] [Google Scholar]
- 101.Pinheiro KA, Pinheiro RT, Silva RA, et al. Chronicity and severity of maternal postpartum depression and infant sleep disorders: a population-based cohort study in southern Brazil. Infant Behav Dev. 2011;34(2):371–3. doi: 10.1016/j.infbeh.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 102.Hadley C, Tegegn A, Tessema F, Asefa M, Galea S. Parental symptoms of common mental disorders and children's social, motor, and language development in sub-Saharan Africa. Ann Hum Biol. 2008;35(3):259–75. doi: 10.1080/03014460802043624. [DOI] [PubMed] [Google Scholar]
- 103.Ali NS, Mahmud S, Khan A, Ali BS. Impact of postpartum anxiety and depression on child's mental development from two peri-urban communities of Karachi, Pakistan: a quasi-experimental study. BMC Psychiatry. 2013;13:274. doi: 10.1186/1471-244X-13-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bhat A, Chowdayya R, Selvam S, Khan A, Kolts R, Srinivasan K. Maternal prenatal psychological distress and temperament in 1-4 month old infants - A study in a non-western population. Infant Behav Dev. 2015;39:35–41. doi: 10.1016/j.infbeh.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 105.O'Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary Care Screening for and Treatment of Depression in Pregnant and Postpartum Women: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;315(4):388–406. doi: 10.1001/jama.2015.18948. [DOI] [PubMed] [Google Scholar]
- 106.Eaton J, McCay L, Semrau M, et al. Scale up of services for mental health in low-income and middle-income countries. Lancet. 2011;378(9802):1592–603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- 107.WHO. World Health Organization [Accessed on: August 31,2013];Integrating mental health into primary care: A global perspective. 2008 Available at: http://whqlibdoc.who.int/publications/2008/9789241563680_eng.pdf.
- 108.WHO. World Health Organization [Accessed on 05/12/2016];Mental health included in the UN Sustainable Development Goals. 2015 Available at: http://www.who.int/mental_health/SDGs/en/
- 109.Da-Silva VA, Moraes-Santos AR, Carvalho MS, Martins MLP, Teixeira NA. Prenatal and postnatal depression among low income Brazilian women. Brazilian Journal of Medical and Biological Research. 1998;31:799–804. doi: 10.1590/s0100-879x1998000600012. [DOI] [PubMed] [Google Scholar]
- 110.Chandran M, Tharyan P, Muliyil J, Abraham S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. British Journal of Psychiatry. 2002;181:499–504. doi: 10.1192/bjp.181.6.499. [DOI] [PubMed] [Google Scholar]
- 111.Lovisi GM, Lopez JR, Coutinho ES, Patel V. Poverty, violence and depression during pregnancy: a survey of mothers attending a public hospital in Brazil. Psychol Med. 2005;35(10):1485–92. doi: 10.1017/S0033291705005362. [DOI] [PubMed] [Google Scholar]
- 112.Azidah A, Shaiful B, Rusli N, Jamil M. Postnatal depression and socio-cultural practices among postnatal mothers in Kota Bahru, Kelantan, Malaysia. The Medical Journal of Malaysia. 2006;61(1):76–83. [PubMed] [Google Scholar]
- 113.Gulseren L, Erol A, Gulseren S, Kuey L, Kilic B, Ergor G. From antepartum to postpartum: a prospective study on the prevalence of peripartum depression in a semiurban Turkish community. The Journal of Reproductive Medicine. 2006;51(12):955–60. [PubMed] [Google Scholar]
- 114.Limlomwongse N, Liabsuetrakul T. Cohort study of depressive moods in Thai women during late pregnancy and 6-8 weeks of postpartum using the Edinburgh Postnatal Depression Scale (EPDS) Arch Womens Ment Health. 2006;9(3):131–8. doi: 10.1007/s00737-005-0115-7. [DOI] [PubMed] [Google Scholar]
- 115.Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health. 2007;10(1):25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- 116.Shakya R, Situala S, Shyangwa P. Depression during pregnancy in a tertiary care center of Eastern Nepal. J Nepal Med Assoc. 2008;47(171):128–31. [PubMed] [Google Scholar]
- 117.Karacam Z, Ancel G. Depression, anxiety and influencing factors in pregnancy: a study in a Turkish population. Midwifery. 2009;25(4):344–56. doi: 10.1016/j.midw.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 118.Matos ML, Piélago JS, Figueroa AL. Depresión mayor en embarazadas atendidas en el Instituto Nacional Materno Perinatal de Lima, Perú. Rev Panam Salud Publica. 2009;26(4):310–4. doi: 10.1590/s1020-49892009001000004. [DOI] [PubMed] [Google Scholar]
- 119.Mitsuhiro SS, Chalem E, Moraes Barros MC, Guinsburg R, Laranjeira R. Brief report: Prevalence of psychiatric disorders in pregnant teenagers. J Adolesc. 2009;32(3):747–52. doi: 10.1016/j.adolescence.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 120.Qiao YX, Wang J, Li J, Ablat A. The prevalence and related risk factors of anxiety and depression symptoms among Chinese pregnant women in Shanghai. Aust N Z J Obstet Gynaecol. 2009;49(2):185–90. doi: 10.1111/j.1479-828X.2009.00966.x. [DOI] [PubMed] [Google Scholar]
- 121.Pottinger AM, Trotman-Edwards H, Younger N. Detecting depression during pregnancy and associated lifestyle practices and concerns among women in a hospital-based obstetric clinic in Jamaica. Gen Hosp Psychiatry. 2009;31(3):254–61. doi: 10.1016/j.genhosppsych.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 122.Soares RM, Nunes MA, Schmidt MI, et al. Inappropriate eating behaviors during pregnancy: prevalence and associated factors among pregnant women attending primary care in southern Brazil. Int J Eat Disord. 2009;42(5):387–93. doi: 10.1002/eat.20643. [DOI] [PubMed] [Google Scholar]
- 123.Golbasi Z, Kelleci M, Kisacik G, Cetin A. Prevalence and correlates of depression in pregnancy among Turkish women. Matern Child Health J. 2010;14(4):485–91. doi: 10.1007/s10995-009-0459-0. [DOI] [PubMed] [Google Scholar]
- 124.Kaaya SF, Mbwambo JK, Kilonzo GP, et al. Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in Dar es Salaam, Tanzania. Tanzania Journal of Health Research. 2010;12(1) doi: 10.4314/thrb.v12i1.56276. [DOI] [PubMed] [Google Scholar]
- 125.Kakirau-Hagali M. Study of depression and anxiety in prenatal and postnatal women at Port Moresby General Hospital. PNG Medical Journal. 2010;53(1-2):30–6. [PubMed] [Google Scholar]
- 126.Manzolli P, Nunes MA, Schmidt MI, et al. Violence and depressive symptoms during pregnancy: a primary care study in Brazil. Soc Psychiatry Psychiatr Epidemiol. 2010;45(10):983–8. doi: 10.1007/s00127-009-0145-y. [DOI] [PubMed] [Google Scholar]
- 127.Husain N, Parveen A, Husain M, et al. Prevalence and psychosocial correlates of perinatal depression: a cohort study from urban Pakistan. Arch Womens Ment Health. 2011;14(5):395–403. doi: 10.1007/s00737-011-0233-3. [DOI] [PubMed] [Google Scholar]
- 128.Mohammad KI, Gamble J, Creedy DK. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery. 2011;27(6):e238–45. doi: 10.1016/j.midw.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 129.Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC Women's Health. 2011;11(22) doi: 10.1186/1472-6874-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rochat TJ, Tomlinson M, Barnighausen T, Newell ML, Stein A. The prevalence and clinical presentation of antenatal depression in rural South Africa. J Affect Disord. 2011;135(1-3):362–73. doi: 10.1016/j.jad.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Senturk V, Abas M, Berksun O, Stewart R. Social support and antenatal depression in extended and nuclear family environments in Turkey: a cross-sectional survey. BMC Psychiatry. 2011;11:48. doi: 10.1186/1471-244X-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ali NS, Azam IS, Ali BS, Tabbusum G, Moin SS. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. ScientificWorldJournal. 2012;2012:653098. doi: 10.1100/2012/653098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.da Silva RA, da Costa Ores L, Jansen K, et al. Suicidality and associated factors in pregnant women in Brazil. Community Ment Health J. 2012;48(3):392–5. doi: 10.1007/s10597-012-9495-0. [DOI] [PubMed] [Google Scholar]
- 134.Li J, Mao J, Du Y, Morris JL, Gong G, Xiong X. Health-related quality of life among pregnant women with and without depression in Hubei, China. Matern Child Health J. 2012;16(7):1355–63. doi: 10.1007/s10995-011-0900-z. [DOI] [PubMed] [Google Scholar]
- 135.Manikkam L, Burns JK. Antenatal depression and its risk factors: an urban prevalence study in KwaZulu-Natal. S Afr Med J. 2012;102(12):940–4. doi: 10.7196/samj.6009. [DOI] [PubMed] [Google Scholar]
- 136.Pinheiro RT, da Cunha Coelho FM, da Silva RA, et al. Suicidal behavior in pregnant teenagers in southern Brazil: social, obstetric and psychiatric correlates. Journal of Affective Disorders. 2012;136(3):520–5. doi: 10.1016/j.jad.2011.10.037. [DOI] [PubMed] [Google Scholar]
- 137.Silva R, Jansen K, Souza L, et al. Sociodemographic risk factors of perinatal depression: a cohort study in the public health care system. Revista Brasileira de Psiquiatria. 2012;34(2):143–8. doi: 10.1590/s1516-44462012000200005. [DOI] [PubMed] [Google Scholar]
- 138.Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregnancy and Childbirth. 2013;13(135) doi: 10.1186/1471-2393-13-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Fadzil A, Balakrishnan K, Razali R, et al. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia Pac Psychiatry. 2013;5(Suppl 1):7–13. doi: 10.1111/appy.12036. [DOI] [PubMed] [Google Scholar]
- 140.Farias DR, Pinto Tde J, Teofilo MM, et al. Prevalence of psychiatric disorders in the first trimester of pregnancy and factors associated with current suicide risk. Psychiatry Res. 2013;210(3):962–8. doi: 10.1016/j.psychres.2013.08.053. [DOI] [PubMed] [Google Scholar]
- 141.Fisher J, Tran TD, Biggs B, Dang TH, Nguyen TT, Tran T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. 2013;5(1):29–37. doi: 10.1093/inthealth/ihs012. [DOI] [PubMed] [Google Scholar]
- 142.Mahenge B, Likindikoki S, Stockl H, Mbwambo J. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in Tanzania: a cross-sectional study. BJOG. 2013;120(8):940–6. doi: 10.1111/1471-0528.12185. [DOI] [PubMed] [Google Scholar]
- 143.Yanikkerem E, Ay S, Mutlu S, Goker A. Antenatal depression: prevalence and risk factors in a hospital based Turkish sample. Journal of Pakistan Medical Association. 2013;63(4):472–7. [PubMed] [Google Scholar]
- 144.Akcali Aslan P, Aydin N, Yazici E, Aksoy AN, Kirkan TS, Daloglu GA. Prevalence of depressive disorders and related factors in women in the first trimester of their pregnancies in Erzurum, Turkey. Int J Soc Psychiatry. 2014;60(8):809–17. doi: 10.1177/0020764014524738. [DOI] [PubMed] [Google Scholar]
- 145.Guo N, Bindt C, Bonle MT, et al. Mental health related determinants of parenting stress among urban mothers of young children--results from a birth-cohort study in Ghana and Côte d'Ivoire. BMC Psychiatry. 2014;14(156) doi: 10.1186/1471-244X-14-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stewart RC, Umar E, Tomenson B, Creed F. A cross-sectional study of antenatal depression and associated factors in Malawi. Arch Womens Ment Health. 2014;17(2):145–54. doi: 10.1007/s00737-013-0387-2. [DOI] [PubMed] [Google Scholar]
- 147.Tomlinson M, O'Connor MJ, le Roux IM, et al. Multiple risk factors during pregnancy in South Africa: the need for a horizontal approach to perinatal care. Prev Sci. 2014;15(3):277–82. doi: 10.1007/s11121-013-0376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tsai AC, Tomlinson M, Dewing S, et al. Antenatal depression case finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health. 2014;17(5):423–31. doi: 10.1007/s00737-014-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Vaz JS, Kac G, Nardi AE, Hibbeln JR. Omega-6 fatty acids and greater likelihood of suicide risk and major depression in early pregnancy. J Affect Disord. 2014;152-154:76–82. doi: 10.1016/j.jad.2013.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Couto TCe, Brancaglion MM, Cardoso MN, et al. What is the best tool for screening antenatal depression? J Affect Disord. 2015;178:12–7. doi: 10.1016/j.jad.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 151.Ferreira CR, Orsini MC, Vieira CR, do Amarante Paffaro AM, Silva RR. Prevalence of anxiety symptoms and depression in the third gestational trimester. Arch Gynecol Obstet. 2015;291(5):999–1003. doi: 10.1007/s00404-014-3508-x. [DOI] [PubMed] [Google Scholar]
- 152.Fonseca-Machado Mde O, Alves LC, Monteiro JC, et al. Depressive disorder in pregnant Latin women: does intimate partner violence matter? J Clin Nurs. 2015;24(9-10):1289–99. doi: 10.1111/jocn.12728. [DOI] [PubMed] [Google Scholar]
- 153.Lara MA, Navarrete L, Nieto L, Martin JP, Navarro JL, Lara-Tapia H. Prevalence and incidence of perinatal depression and depressive symptoms among Mexican women. J Affect Disord. 2015;175:18–24. doi: 10.1016/j.jad.2014.12.035. [DOI] [PubMed] [Google Scholar]
- 154.Zeng Y, Cui Y, Li J. Prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester: a cross-sectional survey. BMC Psychiatry. 2015;15:66. doi: 10.1186/s12888-015-0452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999;175:554–8. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- 156.Chaaya M, Campbell OM, El Kak F, Shaar D, Harb H, Kaddour A. Postpartum depression: prevalence and determinants in Lebanon. Arch Womens Ment Health. 2002;5(2):65–72. doi: 10.1007/s00737-002-0140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ekuklu G, Tokuc B, Eskiocak M, Berberoglu U, Saltik A. Prevalence of postpartum depression in Edirne, Turkey, and related factors. Journal of Reproductive Medicine. 2004;49(11):908–14. [PubMed] [Google Scholar]
- 158.Fisher JRW, Morrow MM, Nhu Ngoc NT, Hoang Anh LT. Prevalence, nature, severity and correlates of postpartum depressive symptoms in Vietnam. BJOG: An International Journal of Obstetrics and Gynaecology. 2004;111(12):1353–60. doi: 10.1111/j.1471-0528.2004.00394.x. [DOI] [PubMed] [Google Scholar]
- 159.Adewuya AO. The maternity blues in Western Nigerian women: prevalence and risk factors. Am J Obstet Gynecol. 2005;193(4):1522–5. doi: 10.1016/j.ajog.2005.02.085. [DOI] [PubMed] [Google Scholar]
- 160.Agoub M, Moussaoui D, Battas O. Prevalence of postpartum depression in a Moroccan sample. Arch Womens Ment Health. 2005;8(1):37–43. doi: 10.1007/s00737-005-0069-9. [DOI] [PubMed] [Google Scholar]
- 161.Aydin N, Inandi T, Karabulut N. Depression and associated factors among women within their first postnatal year in Erzurum province in eastern Turkey. Women & Health. 2005;41(2):1–12. doi: 10.1300/J013v41n02_01. [DOI] [PubMed] [Google Scholar]
- 162.Adewuya AO. Early postpartum mood as a risk factor for postnatal depression in Nigerian women. Am J Psychiatry. 2006;163(8):1435–7. doi: 10.1176/ajp.2006.163.8.1435. [DOI] [PubMed] [Google Scholar]
- 163.Ho-Yen SD, Bondevik GT, Eberhard-Gran M, Bjorvatn B. The prevalence of depressive symptoms in the postnatal period in Lalitpur district, Nepal. Acta Obstet Gynecol Scand. 2006;85(10):1186–92. doi: 10.1080/00016340600753158. [DOI] [PubMed] [Google Scholar]
- 164.Husain N, Bevc I, Husain M, Chaudhry IB, Atif N, Rahman A. Prevalence and social correlates of postnatal depression in a low income country. Arch Womens Ment Health. 2006;9(4):197–202. doi: 10.1007/s00737-006-0129-9. [DOI] [PubMed] [Google Scholar]
- 165.Pitanupong J, Liabsuetrakul T, Vittayanont A. Validation of the Thai Edinburgh Postnatal Depression Scale for screening postpartum depression. Psychiatry Res. 2007;149(1-3):253–9. doi: 10.1016/j.psychres.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 166.Xie RH, He G, Liu A, Bradwejn J, Walker M, Wen SW. Fetal gender and postpartum depression in a cohort of Chinese women. Soc Sci Med. 2007;65(4):680–4. doi: 10.1016/j.socscimed.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 167.Ebeigbe P, Akhigbe K. Incidence and associated risk factors of postpartum depression in a tertiary hospital in Nigeria. Nigerian Postgraduate Medical Journal. 2008;15(1):15–8. [PubMed] [Google Scholar]
- 168.Kara B, Unalan P, Cifcili S, Cebeci DS, Sarper N. Is there a role for the family and close community to help reduce the risk of postpartum depression in new mothers? A cross-sectional study of Turkish women. Matern Child Health J. 2008;12(2):155–61. doi: 10.1007/s10995-007-0232-1. [DOI] [PubMed] [Google Scholar]
- 169.Tannous L, Gigante LP, Fuchs SC, Busnello ED. Postnatal depression in Southern Brazil: prevalence and its demographic and socioeconomic determinants. BMC Psychiatry. 2008;8:1. doi: 10.1186/1471-244X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ali NS, Ali BS, Azam IS. Post partum anxiety and depression in peri-urban communities of Karachi, Pakistan: a quasi-experimental study. BMC Public Health. 2009;9:384. doi: 10.1186/1471-2458-9-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gomez-Beloz A, Williams MA, Sanchez SE, Lam N. Intimate Partner Violence and Risk for Depression Among Postpartum Women in Lima, Peru. Violence and Victims. 2009;24(3):380–98. doi: 10.1891/0886-6708.24.3.380. [DOI] [PubMed] [Google Scholar]
- 172.Pollock JI, Manaseki-Holland S, Patel V. Depression in Mongolian women over the first 2 months after childbirth: prevalence and risk factors. J Affect Disord. 2009;116(1-2):126–33. doi: 10.1016/j.jad.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 173.Wan EY, Moyer CA, Harlow SD, Fan Z, Jie Y, Yang H. Postpartum depression and traditional postpartum care in China: role of zuoyuezi. Int J Gynaecol Obstet. 2009;104(3):209–13. doi: 10.1016/j.ijgo.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 174.Chibanda D, Mangezi W, Tshimanga M, et al. Postnatal depression by HIV status among women in Zimbabwe. Journal of Womens Health. 2010;19(11):2071–7. doi: 10.1089/jwh.2010.2012. [DOI] [PubMed] [Google Scholar]
- 175.Kirpinar I, Gozum S, Pasinlioglu T. Prospective study of postpartum depression in eastern Turkey prevalence, socio-demographic and obstetric correlates, prenatal anxiety and early awareness. J Clin Nurs. 2010;19(3-4):422–31. doi: 10.1111/j.1365-2702.2009.03046.x. [DOI] [PubMed] [Google Scholar]
- 176.Dubey C, Gupta N, Bhasin S, Muthal RA, Arora R. Prevalence and associated risk factors for postpartum depression in women attending a tertiary hospital, Delhi, India. Int J Soc Psychiatry. 2012;58(6):577–80. doi: 10.1177/0020764011415210. [DOI] [PubMed] [Google Scholar]
- 177.Lobato G, Moraes CL, Dias AS, Reichenheim ME. Postpartum depression according to time frames and sub-groups: a survey in primary health care settings in Rio de Janeiro, Brazil. Arch Womens Ment Health. 2011;14(3):187–93. doi: 10.1007/s00737-011-0206-6. [DOI] [PubMed] [Google Scholar]
- 178.Ozbasaran F, Coban A, Kucuk M. Prevalence and risk factors concerning postpartum depression among women within early postnatal periods in Turkey. Arch Gynecol Obstet. 2011;283(3):483–90. doi: 10.1007/s00404-010-1402-8. [DOI] [PubMed] [Google Scholar]
- 179.Petrosyan D, Armenian HK, Arzoumanian K. Interaction of maternal age and mode of delivery in the development of postpartum depression in Yerevan, Armenia. J Affect Disord. 2011;135(1-3):77–81. doi: 10.1016/j.jad.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 180.Piyasil V, Pichaiyut P. Postpartum depression in the mothers of preterm infants at Queen Sirikit National Institute of Child Health. Journal of the Medical Association of Thailand. 2011;94(Supplement 3):S91–4. [PubMed] [Google Scholar]
- 181.da Rocha CM, Kac G. High dietary ratio of omega-6 to omega-3 polyunsaturated acids during pregnancy and prevalence of post-partum depression. Matern Child Nutr. 2012;8(1):36–48. doi: 10.1111/j.1740-8709.2010.00256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374–9. doi: 10.1016/j.midw.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 183.Pio de Almeida LS, Jansen K, Kohler CA, Pinheiro RT, da Silva RA, Bonini JS. Working and short-term memories are impaired in postpartum depression. J Affect Disord. 2012;136(3):1238–42. doi: 10.1016/j.jad.2011.09.031. [DOI] [PubMed] [Google Scholar]
- 184.Tavares D, Quevedo L, Jansen K, Souza L, Pinheiro R, Silva R. Prevalence of suicide risk and comorbidities in postpartum women in Pelotas. Rev Bras Psiquiatr. 2012;34(3):270–6. doi: 10.1016/j.rbp.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 185.Zhang Y, Zou S, Cao Y, Zhang Y. Relationship between domestic violence and postnatal depression among pregnant Chinese women. Int J Gynaecol Obstet. 2012;116(1):26–30. doi: 10.1016/j.ijgo.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 186.Dewing S, Tomlinson M, le Roux IM, Chopra M, Tsai AC. Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. J Affect Disord. 2013;150(2):460–5. doi: 10.1016/j.jad.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Goshtasebi A, Alizadeh M, Gandevani S. Association between maternal anaemia and postpartum depression in an urban sample of pregnant women in Iran. Journal of Health, Population, and Nutrition. 2013;31(3):398–402. doi: 10.3329/jhpn.v31i3.16832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Abdollahi F, Sazlina SG, Zain AM, Zarghami M, Asghari Jafarabadi M, Lye MS. Postpartum depression and psycho-socio-demographic predictors. Asia Pac Psychiatry. 2014;6(4):425–34. doi: 10.1111/appy.12152. [DOI] [PubMed] [Google Scholar]
- 189.Masmoudi J, Charfeddine F, Trabelsi S, et al. Postpartum depression: prevalence and risk factors. A prospective Study concerning 302 Tunisian parturients. Tunis Med. 2014;92(10):615–21. [PubMed] [Google Scholar]
- 190.Sadat Z, Kafaei Atrian M, Masoudi Alavi N, Abbaszadeh F, Karimian Z, Taherian A. Effect of mode of delivery on postpartum depression in Iranian women. J Obstet Gynaecol Res. 2014;40(1):172–7. doi: 10.1111/jog.12150. [DOI] [PubMed] [Google Scholar]
- 191.Wu M, Li X, Feng B, Wu H, Qiu C, Zhang W. Poor sleep quality of third-trimester pregnancy is a risk factor for postpartum depression. Med Sci Monit. 2014;20:2740–5. doi: 10.12659/MSM.891222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Bodhare T, Sethi P, Bele S, Gayatri D, Vivekanand A. Postnatal quality of life, depressive symptoms, and social support among women in southern India. Women & Health. 2015;55(3):353–65. doi: 10.1080/03630242.2014.996722. [DOI] [PubMed] [Google Scholar]
- 193.de Castro F, Place JM, Billings DL, Rivera L, Frongillo EA. Risk profiles associated with postnatal depressive symptoms among women in a public sector hospital in Mexico: the role of sociodemographic and psychosocial factors. Arch Womens Ment Health. 2015;18(3):463–71. doi: 10.1007/s00737-014-0472-1. [DOI] [PubMed] [Google Scholar]
- 194.Giri RK, Khatri RB, Mishra SR, Khanal V, Sharma VD, Gartoula RP. Prevalence and factors associated with depressive symptoms among post-partum mothers in Nepal. BMC Res Notes. 2015;8:111. doi: 10.1186/s13104-015-1074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Mohamad Yusuff AS, Tang L, Binns CW, Lee AH. Breastfeeding and Postnatal Depression: A Prospective Cohort Study in Sabah, Malaysia. J Hum Lact. 2016;32(2):277–81. doi: 10.1177/0890334415620788. [DOI] [PubMed] [Google Scholar]
- 196.Patel HL, Ganjiwale JD, Nimbalkar AS, Vani SN, Vasa R, Nimbalkar SM. Characteristics of Postpartum Depression in Anand District, Gujarat, India. J Trop Pediatr. 2015;61(5):364–9. doi: 10.1093/tropej/fmv046. [DOI] [PubMed] [Google Scholar]
- 197.Turkcapar AF, Kadioglu N, Aslan E, Tunc S, Zayifoglu M, Mollamahmutoglu L. Sociodemographic and clinical features of postpartum depression among Turkish women: a prospective study. BMC Pregnancy Childbirth. 2015;15:108. doi: 10.1186/s12884-015-0532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.