Abstract
The Framingham Heart Study (FHS) has conducted seminal research defining cardiovascular disease (CVD) risk factors and fundamentally shaping public health guidelines for CVD prevention over the past five decades. The success of the Original Cohort, initiated in 1948, paved the way for further epidemiological research in preventive cardiology. Due to the keen observations suggesting the role of shared familial factors in the development of CVD, in 1971 the FHS began enroling the second generation cohort, comprising the children of the Original Cohort and the spouses of the children. In 2002, the third generation cohort, comprising the grandchildren of the Original Cohort, was initiated to additionally explore genetic contributions to CVD in greater depth. Additionally, because of the predominance of White individuals of European descent in the three generations of FHS participants noted above, the Heart Study enrolled the OMNI1 and OMNI2 cohorts in 1994 and 2003, respectively, aimed to reflect the current greater racial and ethnic diversity of the town of Framingham. All FHS cohorts have been examined approximately every 2–4 years since the initiation of the study. At these periodic Heart Study examinations, we obtain a medical history and perform a cardiovascular-focused physical examination, 12-lead electrocardiography, blood and urine samples testing and other cardiovascular imaging studies reflecting subclinical disease burden.
The FHS has continually evolved along the cutting edge of cardiovascular science and epidemiological research since its inception. Participant studies now additionally include study of cardiovascular imaging, serum and urine biomarkers, genetics/genomics, proteomics, metabolomics and social networks. Numerous ancillary studies have been established, expanding the phenotypes to encompass multiple organ systems including the lungs, brain, bone and fat depots, among others. Whereas the FHS was originally conceived and designed to study the epidemiology of cardiovascular disease, it has evolved over the years with staggering expanded breadth and depth that have far greater implications in the study of the epidemiology of a wide spectrum of human diseases. The FHS welcomes research collaborations using existing or new collection of data. Detailed information regarding the procedures for research application submission and review are available at [http://www.framinghamheartstudy.org/researchers/index.php].
Study rationale
By the middle of the past century, the rise in the prevalence of CVD in the USA necessitated a systematic investigation into its aetiological factors and its prevention and treatment. Given that CVD has a prolonged subclinical phase of development lasting years, a prospective observational cohort study was considered ideal for the investigation of these conditions. In 1948, the National Heart Institute (later to become the National Heart, Lung and Blood Institute) chose the town of Framingham, Massachusetts, to conduct an epidemiological study, as it had responded favourably to a tuberculosis screening project.1 The primary goal was to identify determinants of CVD to guide public health prevention. Whereas the initial goal was to invite individuals rather than family members free of prevalent CVD, the latter strategy was employed at the request of the then FHS Executive Committee to maintain goodwill among the families in the community.2 Of note, nearly equal numbers of women and men were enrolled into the FHS at its very outset, thereby facilitating a scientific enquiry into the epidemiology of CVD in both sexes and contributing to our understanding of the sex-related differences in manifestations and prognosis of CVD. Studies from the Original Cohort, which identified risk factors and the natural history of specific cardiovascular diseases, defined and established the role for the emerging field of cardiovascular epidemiology.
Following the successful enrolment of the Original Cohort and the initial major scientific reports emanating from a careful longitudinal study of its participants, progression towards examination of another wave of participants was natural. Emerging evidence suggested aggregation of CVD traits, including blood pressure, within families. With enrolment of family members in the Original Cohort, subsequent enrolment of their children as part of the FHS Offspring Cohort was deemed advantageous for studies investigating the familial clustering of CVD phenotypes and the role of shared environmental factors versus genetic factors in contributing to such aggregation. The investigations of the Offspring Cohort have similarly led to substantial scientific productivity and have further provided newer insights into CVD risk factors and related familial and non-familial associations.
As the FHS evolved over several decades, a Third Generation cohort was recruited. By the 1980s, the heritability of many CVD traits was demonstrated, but the genetic basis for such inheritance was poorly understood. The completion of the Human Genome project provided additional impetus for studying the genetic bases of CVD. Thus, a primary goal for enrolment of a third generation into the FHS was to increase the number of family members in order to study inheritance patterns and genetic determinants of CVD, using novel, state of the art methods including genome-wide association studies. Additional goals for recruitment of a young Third Generation cohort were to study subclinical CVD earlier in adulthood using novel cardiovascular imaging and to evaluate temporal trends in CVD and its risk factors. The three-generational FHS structure is unique among CVD epidemiology studies and has provided greater statistical power in genome wide association studies.
During its long course, FHS has nearly continuously received funding from the National Institutes of Health (NIH, core contract) and is administered by Boston University staff and investigators. Additionally, its investigator-led ancillary studies are supported by multiple sources, including multiple institutes within the NIH, the American Heart Association, the American College of Cardiology and various other medical societies and foundations.
Description of the FHS
The FHS was the first longitudinally-followed large cohort to study CVD epidemiology in the USA, now including a multigenerational community-based cohort of free-living adults. In 1948, FHS investigators sent invitation letters based on a random sampling of two of every three families with members aged 30–59 years, living in the town of Framingham, Massachusetts. Of 6507 contacts, 4494 (69%) men and women agreed to participate and an additional group of volunteers (n = 715) also joined, for a total of 5209 (n = 2336 men and 2873 women) constituting the Original Cohort.3 As noted above, to further investigate the role of heritability of CVD and related risk factors, interest lay in study of the next generation of participants. In 1971, the 2656 children of the 1644 husband-wife pairs in the Original Cohort, a group of children of Original Cohort members with coronary disease (n = 899) and the spouses of these groups of children (n = 1212 and 368, respectively), were enrolled in the Offspring Cohort (total n = 5124).4 The Third Generation Cohort was then begun in 2002, with the objective of expanding the phenotypic and genotypic spectrum for the study of CVD.5 For this cohort, adults who were at least 20 years of age with at least one parent in the Offspring Cohort were invited to participate, with preference given to larger families. Of 6553 eligible individuals, 4095 participants were enrolled. To add to familial data, 103 parents of Third Generation participants who were not previously enrolled in the Offspring Cohort were enrolled as the New Offspring Spouses Cohort.
Finally, the town of Framingham and surrounding community have increased in ethnic and racial diversity over the several decades since enrolment of the Original Cohort. Thus, the OMNI cohort, including individuals of African American, Hispanic, Asian, Indian, Pacific Islander and Native American descent, was begun in 1994, enrolling 506 participants. In 2003, a second OMNI cohort was initiated, enrolling 410 ethnically and racially diverse adults, some of whom were family members of those in the first OMNI cohort. Figure 1 displays enrolment and follow-up of the cohorts. Table 1 shows the demographic characteristics of the cohorts, including the superb follow-up of nearly the entire sample. Additional details of age and sex distributions of each cohort at study entry are available at [http://www.framinghamheartstudy.org/participants/index.php].
Figure 1.
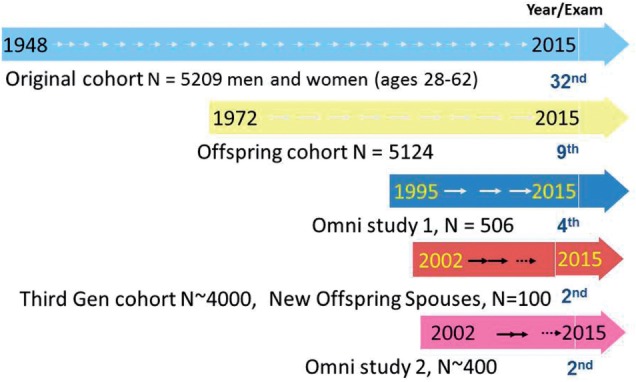
Time course of enrolment of the cohorts within the FHS. The FHS is a multigenerational longitudinally followed cohort spanning the spectrum of age. Numbers at arrows indicate most recent year of examination cycle (e.g. 32nd examination cycle for Original cohort). Figure from Benjamin I et al. Circulation 2015;131:100–12. Reprinted with copyright permission.
Table 1.
Characteristics of FHS cohorts
| Cohort | Total, n | DNA, n | Ancestry, % |
Year recruited | Age, years | Follow-up |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EA | AA | HA | AsA | Other | Examinations, n | Intervals, n | Duration, years | |||||
| Original | 5209 | 971 | 100 | 0 | 0 | 0 | 0 | 1948–53 | 28–74 | 32 | 2 | 65 |
| Offspring (and spouses) | 5124 | 3930 | 100 | 0 | 0 | 0 | 0 | 1971–75 | 5–70 | 9 | 4–8 | 43 |
| Third Generation | 4095 | 4077 | 100 | 0 | 0 | 0 | 0 | 2002–05 | 19–72 | 2 | 6 | ≈ 10 |
| Offspring Spouses | 103 | 101 | 100 | 0 | 0 | 0 | 0 | 2003–05 | 47–85 | 2 | 6 | ≈ 10 |
| Omni 1 Cohort | 507 | 493 | 0 | 28 | 42 | 24 | 6 | 1994–98 | 27–78 | 4 | 4–8 | ≈ 15–20 |
| Omni 2 Cohort | 410 | 407 | 0 | 28 | 42 | 24 | 6 | 2003–05 | 20–80 | 2 | 6 | ≈ 10 |
AA, African American; AsA, Asian American; EA, European American; HA, Hispanic American.
Table from Benjamin I et al. Circulation 2015;131:100–112.
Reprinted with copyright permission.
Cohort follow-up
Every 2–6 years, in-person examinations (referred to as exam cycles) are conducted for each FHS cohort (Table 1). Examination visits include: obtaining written informed consent; documentation of a detailed medical and family history, review of all medicines and supplements, and cardiovascular-targeted physical examination (all administered by a physician); measurement of anthropometric data, 12-lead electrocardiography, neurocognitive battery (including a ‘mini mental state’ examination questionnaire administered by staff), collection of blood and urine and participation in on-site ancillary studies, all within a 4-h window typically. For locally residing participants who are unable to return for an on-site examination (e.g. elderly, home- or nursing home-bound), staff members travel to the participants to administer the components of the cycle visit. FHS staff routinely contact all medical offices and hospitals to obtain primary results on participants regarding their medical diagnoses and testing (all authorized by the informed consent provided by the participants). Additionally, in between cycle examinations, interim questionnaires detailing updates of medical and family history are mailed, and information is obtained via regular phone calls, thereby maintaining continuous surveillance of the participants. Though originally recruited from the communities in and around Framingham, Massachusetts, FHS participants now reside worldwide. The 99% retention rate of participants regularly returning for scheduled examinations at FHS is a testament to the dedication of the participants to the study and contributes to the high quality of the study.
Phenotypes and outcomes measured
The FHS has collected a broad range of CVD phenotypes including biomarkers measured in blood (encompassing traditional CVD risk factors to novel biomarkers, genetics and ‘omics’) and urine, imaging tests, vascular function tests and adverse clinical outcomes. Extra-cardiovascular phenotypes span numerous organ systems, including the brain, lungs, bone, metabolic/fat and kidneys. Additionally, demographic and socioeconomic data are collected, and innovative integration of residence with pollution data allows for study of the impact of inhaled particles and pollutants on cardiovascular health.6 Tables 2 and 3 list phenotypic measures and outcomes assessed in each cohort. Specific details of measured phenotypes and the years of examination may be downloaded at [http://www.framinghamheartstudy.org/researchers/description-data/index.php]. The FHS has established standardized criteria for its outcomes, including coronary heart disease (myocardial infarction, angina), congestive heart failure, cardiovascular disease, atrial fibrillation, stroke, transient ischaemic attack, claudication, cardiovascular death and all-cause death. Adjudication of outcomes occurs weekly with a three-physician endpoints review committee, which reviews all medical records.
Table 2.
Phenotypic data collected in FHS
| Phenotype data | Examples |
|---|---|
| Clinical events (validated and adjudicated) |
|
| Subclinical disease (most measures repeated) |
|
| Pulmonary disease and sleep traits (pulmonary function test data available on multiple examinations) |
|
| Traditional risk factors (directly measured) |
|
| Anthropometry (directly measured) |
|
| Lifestyle |
|
| Measures of function |
|
| Medications |
|
| Medicare data |
|
| Bone health |
|
| Circulating and urine biomarkers | |
| Renal function |
|
| Inflammatory marker panel |
|
| Markers of haemostasis, thrombosis | Fibrinogen, factor VIIIc, von Willebrand factor, D-dimer, plasminogen activator inhibitor-1, platelet reactivity |
| Markers of myocardial injury | Troponin I, growth differentiation factor-15, ST-2, brain natriuretic peptide, N-terminal atrial natriuretic peptide |
| Adipokines |
|
| Growth factors |
|
| Molecules interacting with vessel wall and platelets |
|
| Markers of brain injury |
|
| Lipid subfractions |
|
| Hormones and vitamins |
|
Table from Benjamin I et al. Circulation 2015;131:100–12.
Reprinted with copyright permission.
Table 3.
Summary of measured phenotypes and outcomes in the FHS by cohort
| Phenotype measured | Cohort |
|||||
|---|---|---|---|---|---|---|
| Original | Offspring | New Offspring spouse | Third Gen. | OMNI 1 | OMNI 2 | |
| History | ||||||
| Medical history | x* | x* | x* | x* | x* | x* |
| Medicines | x* | x* | x* | x* | x* | x* |
| Social history | x* | x* | x* | x* | x* | x* |
| Family history | x* | x* | x* | x* | x* | x* |
| Symptoms | x* | x* | x* | x* | x* | x* |
| Questionnaires | ||||||
| Diet | x* | x* | x* | x* | x* | x* |
| Sleep habits | x* | x* | x* | x* | x* | x* |
| Physical activity | x* | x* | x* | x* | x* | x* |
| Menarche, menopause | x | |||||
| Physical examination | ||||||
| Anthropometric | x* | x* | x* | x* | x* | x* |
| Blood pressure | x* | x* | x* | x* | x* | x* |
| Eye examination | x* | x* | x* | x* | x* | x* |
| Hearing test | x* | x* | x* | x* | x* | x* |
| 12-lead ECG | x* | x* | x* | x* | x* | x* |
| Serum | ||||||
| Chemistries | x* | x* | x* | x* | x* | x* |
| Haemoglobin A1c | x* | x* | x* | x* | x* | x* |
| Complete blood count | x* | x* | x* | x* | x* | x* |
| Lipids | x* | x* | x* | x* | x* | x* |
| Lipid particles, characteristics | x | x | ||||
| Biomarkers: inflammatory, metabolic | x* | x* | x* | x* | ||
| Genetic | x | x* | x* | |||
| Metabolomics | x | x | ||||
| Proteomics | x | |||||
| Hormones: thyroid, sex, renal | x | x | x | |||
| Urine | ||||||
| Chemistries | x* | x* | x* | x* | x* | x* |
| Cardiovascular imaging | ||||||
| Chest X-ray | x* | |||||
| Echocardiography | x* | x* | x* | x* | x | x |
| Cardiac MRI | x | x | x | |||
| Cardiac CT | x* | x* | x* | |||
| Carotid ultrasound | x* | |||||
| Vascular | ||||||
| Applanation onometry | x | x* | x* | x* | ||
| Peripheral arterial tonometry | x | x* | x* | x | ||
| FMD | x* | x* | x | |||
| Chest and abdominal CT: fat | x* | x* | x* | |||
| Physical activity | ||||||
| Gait speed | x* | x* | x* | x* | x* | x* |
| Accelerometry | x | |||||
| Neurological | ||||||
| Mini mental status examination | x* | x* | ||||
| Neuropsychological battery | x* | x* | x* | x* | x* | x* |
| Brain MRI | x | x* | x* | |||
| Pulmonary | ||||||
| Pulmonary function tests | x | x* | x* | x* | x* | x* |
| Chest CT: lung measures | x* | x* | x* | x* | ||
| Musculoskeletal | ||||||
| Knee X-ray | x | x | ||||
| Bone mineral density | x | x* | ||||
| Whole-body and regional DXA | x | |||||
| Quantitative CT: volumetric bone density | x | x | ||||
| Muscle strength | x | x | ||||
| Sleep study | x* | |||||
| Autopsy | x | x | ||||
FMD: flow mediated dilation.
*Serial measures available.
Findings and contributions
Traditional risk factors in CVD
Over the past several decades, findings from the FHS have been pivotal in advancing our understanding of the epidemiology of CVD. In the initial 1957 study reporting 4-year follow up of Original Cohort participants, Dr Roy Dawber, one of the founding fathers of FHS, first identified the contributions of three key modifiable risk factors in CVD: blood pressure, overweight and cholesterol (Table 4).7 Subsequently, use of the term ‘risk factors’ spread following its use in one of the FHS seminal publications, ‘Factors of risk in the development of coronary heart disease’.8 This landmark report remains one of the most enduring studies in the field of cardiovascular epidemiology. Published in 1961 by Dr William Kannel, subsequent FHS director, this report first described the coronary heart disease risk associated with age, male sex, hypertension, elevated cholesterol, diabetes and electrocardiographic left ventricular hypertrophy.
Table 4.
Incidence of atherosclerotic heart disease in follow up of FHS males aged 45-62, by blood pressure, relative weight, and cholesterol levels
| Attributes |
Population at Risk |
|||||
|---|---|---|---|---|---|---|
| Blood pressure | Relative weight | Total cholesterol | No. | Percent | New disease | Rate/1000 |
| All persons* | 877 | 100 | 51 | 58 | ||
| High on two or more | 105 | 12 | 15 | 143 | ||
| High | High | High | 17 | 5 | ||
| High | High | Med. or low | 47 | 3 | ||
| High | Med. or low | High | 20 | 1 | ||
| Border. or normo. | High | High | 21 | 6 | ||
| High on one only | 290 | 33 | 23 | 79 | ||
| High | Med. or low | Med. or low | 91 | 9 | ||
| Border. or normo. | High | Med. or low | 87 | 5 | ||
| Border. or normo. | Med. or low | High | 112 | 9 | ||
| Border or medium on two or more | 186 | 21 | 7 | 38 | ||
| Borderline | Medium | Medium | 48 | 4 | ||
| Borderline | Medium | Low | 63 | – | ||
| Borderline | Low | Medium | 42 | 3 | ||
| Normotension | Medium | Medium | 33 | – | ||
| Border or medium on one only | 198 | 23 | 5 | 25 | ||
| Borderline | Low | Low | 89 | 2 | ||
| Normotension | Medium | Low | 54 | 1 | ||
| Normotension | Low | Medium | 55 | 2 | ||
| Normotension or low | 98 | 11 | 1 | 10 | ||
| Normotension | Low | Low | ||||
* Excludes 21 persons (one developing new disease) for whom measurements of one or more attributes were not available.
Table reproduced with copyright permission from Dawber TR et al, Am J Pub Health Nations Health 1957 Apr; 47(4 Pt 2): 4–24.
A major asset of FHS has been its serial examinations of participants, aiding the longitudinal tracking of many CVD risk factors prior to overt disease. The FHS characterized these key CVD risk factors in depth in subsequent publications. Early reports described changes in blood pressure with age,9 and established that hypertension was not benign or compensatory, as previously thought, nor was a rise in blood pressure with age a ‘normal’ phenomenon. Rather, hypertension was associated with numerous CVD outcomes, including coronary artery disease,10 stroke,11 congestive heart failure,12,13 peripheral arterial disease14 and atrial fibrillation.15 Additionally, the FHS elucidated that the primary morbidity related to hypertension was more strongly associated with systolic, rather than diastolic, blood pressure,16 that even borderline isolated systolic hypertension and high normal blood pressure were associated with significant morbidity17 and that blood pressure treatment was associated with a reduction in CVD mortality (demonstrated first in randomized clinical trials).18 Furthermore, the risk associated with a given blood pressure varied widely depending on the presence of other CVD risk factors,19 thereby introducing the concept of multivariable risk, a precursor of risk prediction algorithms.
As phenotyping at FHS advanced to include echocardiography, assessment of left ventricular mass—a more sensitive measure of left ventricular hypertrophy (LVH)—became possible. The FHS investigators reported that echocardiographic LVH was associated with greater age, blood pressure and obesity, among other CVD risk factors.20 Moreover, echocardiographic LVH predicted coronary disease, CVD death and all-cause mortality, beyond the risks conferred by standard CVD risk factors.21,22 LV remodelling occurs in response to long-term exposure to CVD risk factors and haemodynamic changes, and the FHS has also elucidated the prognostic importance of geometric patterns23 and change in these patterns,24 independently of CVD risk factors and LV mass.
The study of lipids in the general population has been another key contribution of FHS. In 1965, the FHS laboratory began separating serum lipoproteins into fractions by ultracentrifugation. In 1971, the FHS published its earliest study relating circulating lipid fractions to the risk of developing coronary disease.25 Subsequent analyses revealed the prognostic implications of low-density lipoproteins (LDL), high-density lipoproteins (HDL) and the total cholesterol-to-HDL ratio, the latter of which would be a component of the Framingham Risk Score.26,27 Additionally, lipoprotein particles other than cholesterol, including lipoprotein(a), were found to be associated with CVD independently of LDL and HDL.28 Studies from FHS suggest the importance of serum cholesterol in the prediction of CHD incidence, and also occurrence of both CVD and all-cause mortality across the age spectrum.29,30 Leveraging use of repeated measures, FHS investigators also showed that time-averaged lipid measures were more associated with subclinical atherosclerosis measured by computed tomography than with single-point measures.31
During the first two decades of the study, evidence of the association between diabetes and coronary disease had accumulated. The FHS confirmed this association and extended these observations in several directions. Study of Original Cohort members with diabetes revealed greater risk for coronary heart disease, heart failure, stroke and peripheral arterial disease compared with individuals without diabetes.32 Notably, risks for CVD and morbidity/mortality following the onset of CVD were greater for women than men with diabetes.32,33 In participants without diabetes, the FHS also demonstrated the role of elevated blood glucose, measured by haemoglobin A1c, in mediating CVD risk,34 and an extension of the pattern of greater CVD risk in women in this group as well.35
Furthermore, FHS examinations include a comprehensive assessment of lifestyle factors, which allowed study of their implications for CVD risk. Indeed, cigarette smoking was shown to be associated with the risk of developing a myocardial infarction and of sudden death, with a significant reduction in the risk with smoking cessation.36,37 Additionally, the FHS has demonstrated the risk of CVD associated with poor physical activity and dietary factors.38,39 Connected with these lifestyle factors is the issue of overweight and obesity, whose associations with CVD were previously debated. FHS investigators demonstrated that excess body weight was associated with CVD risk factors and with CVD incidence independently of other CVD risk factors.40–42 These collective findings formed a critical and foundational knowledge base to guide public health efforts in CVD prevention. That the central tenets of risk factors reported decades ago in 1961 remain the main modifiable CVD risk factors today, is a testament to the foresight and discoveries of the original FHS investigators and the contributions of FHS participants.
Epidemiology of specific CVD entities
In addition to the contributions towards understanding CVD risk factors, the FHS has also been instrumental in establishing the epidemiology of specific CVD subtypes. The FHS demonstrated much of the characteristics and prognosis surrounding myocardial infarction (MI), including its frequent presentation as sudden cardiac death,43 and the high mortality associated with first MI, particularly in women.44 FHS investigators also introduced the important concept that MI frequently is clinically unrecognized, and that mortality rates in recognized (by 12-lead electrocardiography) and unrecognized MI are similar.43,45
Heart failure has been and is remains a growing epidemic, perhaps even more so in our modern era of improvements in treatment of coronary disease and survival after MI. The FHS was one of the first groups to describe the incidence, prevalence and grim natural history of heart failure in the community12,46,47 and also identified hypertension, valvular heart disease and coronary disease as key aetiologies for heart failure.13 The advent of echocardiography made it evident that individuals with heart failure may have normal left ventricular systolic function measured by ejection fraction. The FHS was one of the first population studies to shed light on the entity of heart failure with preserved ejection fraction, which represents up to half of all clinical heart failure. Importantly, this disorder is more common in women, and confers morbidity and mortality similar to that of heart failure with reduced ejection fraction, or classical systolic heart failure.48 Additionally, that asymptomatic individuals with greater left ventricular dimensions49 and even a mildly reduced ejection fraction50 are at greater CVD risk compared with those with a normal LV ejection fraction, was also described by FHS investigators.
The FHS has advanced our understanding of numerous related cardiovascular conditions as well, including peripheral arterial disease, stroke and disturbances in heart rhythm. Early FHS studies described the natural history of peripheral arterial disease manifesting as lower extremity claudication,51 and its predominant risk factor associations including diabetes52 and smoking.53 More recently, repeated 6-min walk testing has allowed examination of functional and haemodynamic response to exercise in relation to vascular disease.54,55 Additionally, the FHS was pivotal in clarifying the relation of blood pressure11 and smoking56 with risk of stroke. Similarly to the FHS CVD risk estimations, the FHS risk scores for peripheral arterial disease14 and stroke57 have pervasive, widespread, clinical impact. FHS investigations have also shed light on the epidemiology and prognosis of heart rhythm abnormalities, including the identification of atrial fibrillation as a powerful risk factor for stroke and all-cause mortality.58–60 This finding has significant public health implications, as atrial fibrillation is the most common chronic arrhythmia and likely to grow in prevalence with the ageing of the world population. FHS investigators established the epidemiology of the disorder, including its risk factors15,61 and associated morbidity and mortality.62 Furthermore, it is well-known that isolated electrocardiographic testing during routine examinations does not capture heart rhythm during regular activity. Ambulatory electrocardiographic monitoring has proved to be fruitful, linking the observations of reduced heart rate variability with incident CVD,63 and incidental asymptomatic ventricular arrhythmias with coronary disease and mortality.64
Expansion of phenotypes: imaging, novel biomarkers, and the ‘omics’ era
Despite the significant advances however, many aspects of CVD pathophysiology remain incompletely understood, and clearly risk remains despite evaluation and treatment of the traditional CVD risk factors. Thus, a holy grail is the use of non-invasive methods through which biomarkers of CVD risk may be identified and related biological mechanisms uncovered. Advanced non-invasive cardiovascular imaging has been one such promising area to fill these needs. Echocardiography, computed tomography and magnetic resonance imaging have enhanced our understanding of age- and CVD-related ventricular remodelling and prevalence and consequences of subclinical atherosclerosis in different vascular territories.24,65–67 Application of advanced techniques of imaging myocardial tissue mechanics in FHS68 may further add to understanding of the development and implications of subclinical ventricular dysfunction. Additionally, non-invasive assessment of central and peripheral vascular disease in FHS have demonstrated that carotid intimal medial thickness,69 ankle-brachial index,70,71 endothelial function (brachial artery flow-mediated dilation), conduit arterial stiffness (via applanation tonometry)72 and peripheral arterial tonometry are key correlates of CVD risk, and some of these measures are predictive of CVD risk and mortality and may improve CVD risk reclassification. Non-invasive imaging has also allowed investigation of cardiometabolic disease through evaluation of the quantity and characteristics (quality) of fat depots.73,74 Finally, recognizing the strong links between cardiovascular and cerebrovascular disease, the current team of FHS investigations have also included detailed assessment of subclinical neurological disease using state of the art brain magnetic resonance imaging and meticulous cognitive assessments to identify subclinical injury.75 Many of these imaging measures have been repeated in the same participants, allowing longitudinal tracking of these characteristics.
The FHS also has a large biorepository of participant data, including blood, urine and other biological samples, from which cutting-edge biomarker, genetic and ‘omics’ tools (transcriptomics, metabolomics, proteomics) have been harnessed. Numerous biomarkers have been evaluated in FHS participants (Table 2), and multiple biomarkers are related to CVD, including but not limited to metabolic disease,76 cardiac structure and function,77 heart failure 78 and mortality.79 FHS ‘omics’ measures include DNA methylation, transcriptomics (describing whole-blood mRNA and microRNA expression), metabolites and protein biomarkers. Such efforts have identified potential targets in the pathophysiology of CVD,80 including metabolic risk and diabetes81,82 and coronary disease.83
The three-generation family structure and the selection of large pedigrees in FHS families are its major strengths, allowing substantial investigations of cardiovascular genetics. Smaller observational studies had suggested that CVD clustered in families, and FHS was one of the earlier studies to demonstrate the heritability of blood pressure,84 lipids,85 diabetes86 and coronary disease.87 In the 1990s and 2000s, FHS investigators collected DNA samples in the Original, the Offspring (including Offspring Spouses) and the Third Generation cohort members from whole blood. Immortalized lymphoblastoid cell lines obtained in 8458 participants serve as a valuable replenishable source of DNA.
The FHS has been a vital contributor to international collaborative efforts to identify the non-genetic and genetic underpinnings of CVD traits. FHS participants have contributed data on lipids and inflammatory markers for investigation as part of the Emerging Risk Factors Collaboration.88 Additionally, the FHS has led efforts to identify variants in single-nucleotide polymorphisms (SNPs) associated with CVD. The FHS is part of the SNP Health Association Resource (SHARe)89 and Candidate Gene Association Resource (CARe)90 projects, through which ∼9300participants underwent genotyping of 550 000 SNPs using the Affymetrix platform (SHARe) and > 7500 participants had genotyping of 50 000 SNPs using the Illumina Cardiochip (CARe). Imputation to 40 million SNPs was achieved using the 1000 Genomes project. FHS efforts have enabled the identification of SNPs for traits including blood pressure,91–93 lipids,94,95 obesity,96 arterial stiffness97,98 and imaging measures of cardiovascular function including ventricular mass and dimensions,99,100 endothelial function,99 valvular calcification101 and carotid atherosclerosis.102 In addition, FHS has pursued investigation of the exome through genotyping of ∼ 200 000 exome variants using the Illumina V1.0 Exome Chip, and whole-exome sequencing in nearly 3000 participants from collaborations including the NHLVI’s Grand Opportunity Exome Sequence Project103 and CHARGE targeted Sequencing project.104 Among others, these investigations have identified rare variants associated with diabetes105 and lipids and coronary disease106–108. Furthermore, whole-genome sequencing is underway via the NHLBI TOPMed project,109,110 highlighting the importance of regulatory and non-protein coding regions, in addition to the protein coding regions that have been common targets for investigation. Whereas many biomarker and genetic associations have been found, the mechanisms behind these associations are often elusive. Using network analysis, FHS investigators have begun to integrate these separate pieces of the puzzles together for analysing the epidemiology of CVD.111–113
In the modern era, FHS has continued to move forward with cutting-edge research, taking advantage of the technology evolution. In addition to advanced network analysis to understand genetic and mechanistic associations, complex social network analyses have enabled study of important social determinants of cardiovascular epidemiology, including trends in obesity and smoking.114,115 The FHS is also applying mobile health technologies with evaluation of functional status with mobile, remote accelerometry monitoring,116 and has integrated participant-level public electronic health records (e.g. Centers for Medicare and Medicaid Services), thus providing a rich source of comprehensive data. A chronological list of FHS publications can be found at [http://www.framinghamheartstudy.org/fhs-bibliography/index.php].
Strengths and weaknesses
The strength of the FHS lies in the dedicated participants, its highly trained staff and its diverse body of scientific investigators over the years. The commitment of the participants to the study is reflected in the high retention rate, despite the fact that many participants live remotely. The FHS is also the only longitudinally followed cohort evaluating CVD risk across three generations of participants in whom extensive serial measurements have been obtained. The FHS has used standardized definitions to adjudicate CVD outcomes, including coronary heart disease and congestive heart failure, and these definitions have been applied consistently to the studies over the several-decade course of the study. The study has conducted meticulous phenotyping of participants (with a great emphasis on quality control issues including reproducibility), with numerous ancillary studies and measured phenotypes now spanning not only the cardiovascular system, but also including the brain, the lungs, the endocrine system, and the metabolic, gastrointestinal, renal and the musculoskeletal systems, to name a few. FHS participants are notably predominantly White individuals of Western European descent (with the exception of the OMNI cohorts). Thus, a more ethnically diverse group of individuals are reflected in the contemporary OMNI cohorts, and efforts to compare findings across ethnicities are being evaluated moving forward.
Conclusions
Whereas the FHS began as a study to identify aetiological factors for CHD and CVD and to improve the prevention of CVD, it has clearly evolved and expanded to encompass a ‘near whole-body’ study over several decades, the equivalent of a human phenome project. Application of novel technologies, integrative methods and multidisciplinary collaborations have fostered the expansion of FHS science over the years. Decades after its humble inception, the FHS remains at the forefront of not just cardiovascular, but also multisystem epidemiological research through the adult life course. With continued efforts, the FHS will continue to advance understanding of the human phenome for the next several decades to come.
Information and Data Access
The FHS website [www.framinghamheartstudy.org] contains further information for prospective investigators. Detailed information regarding the research application and review are available at [http://www.framinghamheartstudy.org/researchers/index.php]. The FHS welcomes research proposals using existing or new collection of data. In addition, phenotypes and genotypes generated in FHS are available publicly on dbGaP through the FHS link [http://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000007.v26.p10]. Individuals wishing to pursue research using FHS genetic data should apply for authorization through dbGaP [https://dbgap.ncbi.nlm.nih.gov/aa/wga.cgi?page=login]. The FHS is a non-profit research entity that has relied upon core contract and ancillary study funding from individual investigators for sustainment. The FHS Service Center handles the modest additional fees for provision of data and materials, and administrative support; further information of the fee structure is available at [http://www.framinghamheartstudy.org/researchers/service-center.php].
Acknowledgments
The authors are indebted to the participants, staff, and investigators of the FHS for their decades of service to the study. The FHS is funded by the National Heart, Lung and Blood Institute (HHSN268201500001I, NO1-HC-25195, HL076784, AG028321, HL070100, HL060040, HL080124, HL071039, HL077447, 6R01-NS-17950 and HL107385). C.W.T. is supported by the National Institutes of Health (1K23 HL118259).
Conflict of interest: None.
Key Messages
Main scientific findings in cardiovascular epidemiology:
identification of key risk factors, including lifestyle, biochemical and genetic risk factors for atherosclerotic CVD and its subtypes including stroke;
combination of multivariable risk factors to generate a composite risk score that can be used in prediction algorithms;
description of the epidemiology of specific CVD entities and cardiovascular remodelling across the age spectrum;
identification of novel mechanisms of CVD, including but not limited to novel biomarkers and genetic factors and a systems biology approach towards the pathogenesis of CVD.
References
- 1.Framingham Community Health and Tuberculosis Demonstration. National Tuberculosis Association, Final Summary Report. Framingham, MA, USA; National Tuberculosis Association, 1924. [Google Scholar]
- 2.Oppenheimer GM. Becoming the Framingham Study 1947-1950. Am J Public Health 2005;95:602–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health 1951;41:279–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kannel WB, Feinleib M, McNamara PM, et al. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol 1979;110:281–90. [DOI] [PubMed] [Google Scholar]
- 5.Splansky GL, Corey D, Yang Q, et al. The Third Generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 2007;165:1328–35. [DOI] [PubMed] [Google Scholar]
- 6.Wilker EH, Ljungman PL, Rice MB, et al. Relation of long-term exposure to air pollution to brachial artery flow-mediated dilation and reactive hyperemia. Am J Cardiol 2014;113:2057–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawber TR, Moore FE, Mann GV. Coronary heart disease in the Framingham study. Am J Public Health Nations Health 1957;47:4–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kannel WB, Dawber TR, Kagan A, et al. Factors of risk in the development of coronary heart disease – six year follow-up experience. The Framingham Study. Ann Intern Med 1961;55:33–50. [DOI] [PubMed] [Google Scholar]
- 9.Kannel WB, Gordon T. Evaluation of cardiovascular risk in the elderly: the Framingham study. Bull N Y Acad Med 1978;54:573–91. [PMC free article] [PubMed] [Google Scholar]
- 10.Kagan AGT, Kannel WB, Dawber TR. Blood pressure and its relation to coronary heart disease in the Framingham study. Hypertension 1959;7:53–81. [Google Scholar]
- 11.Kannel WB, Wolf PA, Verter J, et al. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA 1970;214:301–10. [PubMed] [Google Scholar]
- 12.Kannel WB, Castelli WP, McNamara PM, et al. Role of blood pressure in the development of congestive heart failure. The Framingham study. N Engl J Med 1972;287:781–87. [DOI] [PubMed] [Google Scholar]
- 13.Levy D, Larson MG, Vasan RS, et al. The progression from hypertension to congestive heart failure. JAMA 1996;275:1557–62. [PubMed] [Google Scholar]
- 14.Murabito JM, D'Agostino RB, Silbershatz H, et al. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation 1997;96:44–49. [DOI] [PubMed] [Google Scholar]
- 15.Benjamin EJ, Levy D, Vaziri SM, et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840–44. [PubMed] [Google Scholar]
- 16.Kannel WB, Gordon T, Schwartz MJ. Systolic versus diastolic blood pressure and risk of coronary heart disease. The Framingham study. Am J Cardiol 1971;27:335–46. [DOI] [PubMed] [Google Scholar]
- 17.Sagie A, Larson MG, Levy D. The natural history of borderline isolated systolic hypertension. N Engl J Med 1993;329:1912–17. [DOI] [PubMed] [Google Scholar]
- 18.Sytkowski PA, D'Agostino RB, Belanger AJ, et al. Secular trends in long-term sustained hypertension, long-term treatment, and cardiovascular mortality. The Framingham Heart Study 1950 to 1990. Circulation 1996;93:697–703. [DOI] [PubMed] [Google Scholar]
- 19.Kannel WB. Hypertension. Relationship with other risk factors. Drugs 1986;31(Suppl 1):1–11. [DOI] [PubMed] [Google Scholar]
- 20.Levy D, Anderson KM, Savage DD, et al. Echocardiographically detected left ventricular hypertrophy: prevalence and risk factors. The Framingham Heart Study. Ann Intern Med 1988;108:7–13. [DOI] [PubMed] [Google Scholar]
- 21.Levy D, Garrison RJ, Savage DD, et al. Left ventricular mass and incidence of coronary heart disease in an elderly cohort. The Framingham Heart Study. Ann Intern Med 1989;110:101–07. [DOI] [PubMed] [Google Scholar]
- 22.Levy D, Garrison RJ, Savage DD, et al. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990;322:1561–66. [DOI] [PubMed] [Google Scholar]
- 23.Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham Heart Study. J Am Coll Cardiol 1995;25:879–84. [DOI] [PubMed] [Google Scholar]
- 24.Lieb W, Gona P, Larson MG, et al. The natural history of left ventricular geometry in the community: clinical correlates and prognostic significance of change in LV geometric pattern. JACC Cardiovasc Imaging 2014;7:870–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kannel WB, Castelli WP, Gordon T, et al. Serum cholesterol, lipoproteins, and the risk of coronary heart disease. The Framingham study. Ann Intern Med 1971;74:1–12. [DOI] [PubMed] [Google Scholar]
- 26.Gordon T, Castelli WP, Hjortland MC, et al. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med 1977;62:707–14. [DOI] [PubMed] [Google Scholar]
- 27.Castelli WP, Abbott RD, McNamara PM. Summary estimates of cholesterol used to predict coronary heart disease. Circulation 1983;67:730–34. [DOI] [PubMed] [Google Scholar]
- 28.Bostom AG, Cupples LA, Jenner JL, et al. Elevated plasma lipoprotein(a) and coronary heart disease in men aged 55 years and younger. A prospective study. JAMA 1996;276:544–48. [DOI] [PubMed] [Google Scholar]
- 29.Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA 1987;257:2176–80. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd-Jones DM, Wilson PW, Larson MG, et al. Lifetime risk of coronary heart disease by cholesterol levels at selected ages. Arch Intern Med 2003;163:1966–72. [DOI] [PubMed] [Google Scholar]
- 31.Tsao CW, Preis SR, Peloso GM, et al. Relations of long-term and contemporary lipid levels and lipid genetic risk scores with coronary artery calcium in the Framingham Heart Study. J Am Coll Cardiol 2012;60:2364–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA 1979;241:2035–38. [DOI] [PubMed] [Google Scholar]
- 33.Abbott RD, Donahue RP, Kannel WB, et al. The impact of diabetes on survival following myocardial infarction in men vs women. The Framingham Study. JAMA 1988;260:3456–60. [PubMed] [Google Scholar]
- 34.Singer DE, Nathan DM, Anderson KM, et al. Association of HbA1c with prevalent cardiovascular disease in the original cohort of the Framingham Heart Study. Diabetes 1992;41:202–08. [DOI] [PubMed] [Google Scholar]
- 35.Wilson PW, Cupples LA, Kannel WB. Is hyperglycemia associated with cardiovascular disease? The Framingham Study. Am Heart J 1991;121:586–90. [DOI] [PubMed] [Google Scholar]
- 36.Kannel WB. New perspectives on cardiovascular risk factors. Am Heart J 1987;114:213–19. [DOI] [PubMed] [Google Scholar]
- 37.Doyle JT, Dawber TR, Kannel WB, et al. Cigarette smoking and coronary heart disease. Combined experience of the Albany and Framingham studies. N Engl J Med 1962;266:796–801. [DOI] [PubMed] [Google Scholar]
- 38.Kannel WB, Sorlie P. Some health benefits of physical activity. The Framingham Study. Arch Intern Med 1979;139:857–61. [PubMed] [Google Scholar]
- 39.Posner BM, Cupples LA, Gagnon D, et al. Healthy People 2000. The rationale and potential efficacy of preventive nutrition in heart disease: the Framingham Offspring-Spouse Study. Arch Intern Med 1993;153:1549–56. [DOI] [PubMed] [Google Scholar]
- 40.Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983;67:968–77. [DOI] [PubMed] [Google Scholar]
- 41.Garrison RJ, Feinleib M, Castelli WP, et al. Cigarette smoking as a confounder of the relationship between relative weight and long-term mortality. The Framingham Heart Study. JAMA 1983;249:2199–203. [PubMed] [Google Scholar]
- 42.Pencina MJ, D'Agostino RB, Sr, Larson MG, et al. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation 2009;119:3078–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gordon T, Kannel WB. Premature mortality from coronary heart disease. The Framingham study. JAMA 1971;215:1617–25. [PubMed] [Google Scholar]
- 44.Kannel WB, Sorlie P, McNamara PM. Prognosis after initial myocardial infarction: the Framingham study. Am J Cardiol 1979;44:53–59. [DOI] [PubMed] [Google Scholar]
- 45.Stokes J, 3rd, Dawber TR. The silent coronary: the frequency and clinical characteristics of unrecognized myocardial infarction in the Framingham study. Ann Intern Med 1959;50:1359–69. [DOI] [PubMed] [Google Scholar]
- 46.McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285:1441–46. [DOI] [PubMed] [Google Scholar]
- 47.Ho KK, Anderson KM, Kannel WB, et al. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation 1993;88:107–15. [DOI] [PubMed] [Google Scholar]
- 48.Vasan RS, Larson MG, Benjamin EJ, et al. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 1999;33:1948–55. [DOI] [PubMed] [Google Scholar]
- 49.Vasan RS, Larson MG, Benjamin EJ, et al. Left ventricular dilatation and the risk of congestive heart failure in people without myocardial infarction. N Engl J Med 1997;336:1350–55. [DOI] [PubMed] [Google Scholar]
- 50.Wang TJ, Evans JC, Benjamin EJ, et al. Natural history of asymptomatic left ventricular systolic dysfunction in the community. Circulation 2003;108:977–82. [DOI] [PubMed] [Google Scholar]
- 51.Kannel WB, Shurtleff D. The natural history of arteriosclerosis obliterans. Cardiovasc Clin 1971;3:37–52. [PubMed] [Google Scholar]
- 52.Brand FN, Abbott RD, Kannel WB. Diabetes, intermittent claudication, and risk of cardiovascular events. The Framingham Study. Diabetes 1989;38:504–09. [DOI] [PubMed] [Google Scholar]
- 53.Kannel WB, Shurtleff D. The Framingham Study. Cigarettes and the development of intermittent claudication. Geriatrics 1973;28:61–68. [PubMed] [Google Scholar]
- 54.Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension 2004;43:1239–45. [DOI] [PubMed] [Google Scholar]
- 55.Benjamin EJ, Larson MG, Keyes MJ, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation 2004;109:613–19. [DOI] [PubMed] [Google Scholar]
- 56.Wolf PA, D'Agostino RB, Kannel WB, et al. Cigarette smoking as a risk factor for stroke. The Framingham Study. JAMA 1988;259:1025–29. [PubMed] [Google Scholar]
- 57.Wolf PA, D'Agostino RB, Belanger AJ, et al. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991;22:312–18. [DOI] [PubMed] [Google Scholar]
- 58.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983–88. [DOI] [PubMed] [Google Scholar]
- 59.Wolf PA, Dawber TR, Thomas HE, Jr, et al. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology 1978;28:973–77. [DOI] [PubMed] [Google Scholar]
- 60.Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet 2015;386:154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kannel WB, Abbott RD, Savage DD, et al. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med 1982;306:1018–22. [DOI] [PubMed] [Google Scholar]
- 62.Benjamin EJ, Wolf PA, D'Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 1998;98:946–52. [DOI] [PubMed] [Google Scholar]
- 63.Tsuji H, Larson MG, Venditti FJ, Jr, et al. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation 1996;94:2850–55. [DOI] [PubMed] [Google Scholar]
- 64.Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham Heart Study. Ann Intern Med 1992;117:990–96. [DOI] [PubMed] [Google Scholar]
- 65.Lieb W, Xanthakis V, Sullivan LM, et al. Longitudinal tracking of left ventricular mass over the adult life course: clinical correlates of short- and long-term change in the Framingham Offspring Study. Circulation 2009;119:3085–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cheng S, Xanthakis V, Sullivan LM, et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation 2010;122:570–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Salton CJ, Chuang ML, O'Donnell CJ, et al. Gender differences and normal left ventricular anatomy in an adult population free of hypertension. A cardiovascular magnetic resonance study of the Framingham Heart Study Offspring cohort. J Am Coll Cardiol 2002;39:1055–60. [DOI] [PubMed] [Google Scholar]
- 68.Cheng S, Larson MG, McCabe EL, et al. Age- and sex-based reference limits and clinical correlates of myocardial strain and synchrony: the Framingham Heart Study. Circ Cardiovasc Imaging 2013;6:692–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Polak JF, Pencina MJ, Pencina KM, et al. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med 2011;365:213–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Murabito JM, Evans JC, Larson MG, et al. The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham Study. Arch Intern Med 2003;163:1939–42. [DOI] [PubMed] [Google Scholar]
- 71.Fowkes FG, Murray GD, Butcher I, et al. ; for the Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 2008;300:197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mitchell GF, Hwang SJ, Vasan RS, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010;121:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rosenquist KJ, Pedley A, Massaro JM, et al. Visceral and subcutaneous fat quality and cardiometabolic risk. JACC Cardiovasc Imaging 2013;6:762–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rosenquist KJ, Massaro JM, Pedley A, et al. Fat quality and incident cardiovascular disease, all-cause mortality, and cancer mortality. J Clin Endocrinol Metab 2015;100:227–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Das RR, Seshadri S, Beiser AS, et al. Prevalence and correlates of silent cerebral infarcts in the Framingham offspring study. Stroke 2008;39:2929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kaess BM, Enserro DM, McManus DD, et al. Cardiometabolic correlates and heritability of fetuin-A, retinol-binding protein 4, and fatty-acid binding protein 4 in the Framingham Heart Study. J Clin Endocrinol Metab 2012;97:E1943–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McManus DD, Lyass A, Ingelsson E, et al. Relations of circulating resistin and adiponectin and cardiac structure and function: the Framingham Offspring Study. Obesity (Silver Spring) 2012;20:1882–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ho JE, Liu C, Lyass A, et al. Galectin-3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J Am Coll Cardiol 2012;60:1249–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schnabel RB, Yin X, Larson MG, et al. Multiple inflammatory biomarkers in relation to cardiovascular events and mortality in the community. Arterioscler Thromb Vasc Biol 2013;33:1728–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wurtz P, Havulinna AS, Soininen P, et al. Metabolite profiling and cardiovascular event risk: a prospective study of 3 population-based cohorts. Circulation 2015;131:774–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cheng S, Rhee EP, Larson MG, et al. Metabolite profiling identifies pathways associated with metabolic risk in humans. Circulation 2012;125:2222–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang TJ, Larson MG, Vasan RS, et al. Metabolite profiles and the risk of developing diabetes. Nat Med 2011;17:448–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Joehanes R, Ying S, Huan T, et al. Gene expression signatures of coronary heart disease. Arterioscler Thromb Vasc Biol 2013;33:1418–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Havlik RJ, Garrison RJ, Feinleib M, et al. Blood pressure aggregation in families. Am J Epidemiol 1979;110:304–12. [DOI] [PubMed] [Google Scholar]
- 85.Garrison RJ, Castelli WP, Feinleib M, et al. The association of total cholesterol, triglycerides and plasma lipoprotein cholesterol levels in first degree relatives and spouse pairs. Am J Epidemiol 1979;110:313–21. [DOI] [PubMed] [Google Scholar]
- 86.Meigs JB, Cupples LA, Wilson PW. Parental transmission of type 2 diabetes: the Framingham Offspring Study. Diabetes 2000;49:2201–07. [DOI] [PubMed] [Google Scholar]
- 87.Myers RH, Kiely DK, Cupples LA, et al. Parental history is an independent risk factor for coronary artery disease: the Framingham Study. Am Heart J 1990;120:963–69. [DOI] [PubMed] [Google Scholar]
- 88.Emerging Risk Factors C, Danesh J, Erqou S, et al. The Emerging Risk Factors Collaboration: analysis of individual data on lipid, inflammatory and other markers in over 1.1 million participants in 104 prospective studies of cardiovascular diseases. Eur J Epidemiol 2007;22:839–69. [DOI] [PubMed] [Google Scholar]
- 89.SHARe: SNP Health Association Resource. (22 August 2015, date last accessed).
- 90.Musunuru K, Lettre G, Young T, et al. Candidate gene association resource (CARe): design, methods, and proof of concept. Circ Cardiovasc Genet 2010;3:267–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.International Consortium for Blood Pressure Genome-Wide Association Studies; Ehret GB, Munroe PB, Rice KM, et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011;478:103–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wain LV, Verwoert GC, O'Reilly PF, et al. Genome-wide association study identifies six new loci influencing pulse pressure and mean arterial pressure. Nat Genet 2011;43:1005–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Levy D, Ehret GB, Rice K, et al. Genome-wide association study of blood pressure and hypertension. Nat Genet 2009;41:677–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Teslovich TM, Musunuru K, Smith AV, et al. Biological, clinical and population relevance of 95 loci for blood lipids. Nature 2010;466:707–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kathiresan S, Willer CJ, Peloso GM, et al. Common variants at 30 loci contribute to polygenic dyslipidemia. Nat Genet 2009;41:56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 2015;518:197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Levy D, Larson MG, Benjamin EJ, et al. Framingham Heart Study 100K Project: genome-wide associations for blood pressure and arterial stiffness. BMC Med Genet 2007;8(Suppl 1):S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mitchell GF, Verwoert GC, Tarasov KV, et al. Common genetic variation in the 3'-BCL11B gene desert is associated with carotid-femoral pulse wave velocity and excess cardiovascular disease risk: the AortaGen Consortium. Circ Cardiovasc Genet 2012;5:81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vasan RS, Larson MG, Aragam J, et al. Genome-wide association of echocardiographic dimensions, brachial artery endothelial function and treadmill exercise responses in the Framingham Heart Study. BMC Med Genet 2007;8(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Vasan RS, Glazer NL, Felix JF, et al. Genetic variants associated with cardiac structure and function: a meta-analysis and replication of genome-wide association data. JAMA 2009;302:168–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Thanassoulis G, Campbell CY, Owens DS, et al. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med 2013;368:503–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bis JC, Kavousi M, Franceschini N, et al. Meta-analysis of genome-wide association studies from the CHARGE consortium identifies common variants associated with carotid intima media thickness and plaque. Nat Genet 2011;43:940–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.NHLBI Grand Opportunity Exome Sequencing Project (ESP). (22 August 2015, date last accessed).
- 104.Boerwinkle E, Heckbert SR. Following-up genome-wide association study signals: lessons learned from Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Consortium Targeted Sequencing Study. Circ Cardiovasc Genet 2014;7:332–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wessel J, Chu AY, Willems SM, et al. Low-frequency and rare exome chip variants associate with fasting glucose and type 2 diabetes susceptibility. Nat Commun 2015;6:5897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lange LA, Hu Y, Zhang H, et al. Whole-exome sequencing identifies rare and low-frequency coding variants associated with LDL cholesterol. Am J Hum Genet 2014;94:233–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Peloso GM, Auer PL, Bis JC, et al. Association of low-frequency and rare coding-sequence variants with blood lipids and coronary heart disease in 56,000 whites and blacks. Am J Hum Genet 2014;94:223–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Do R, Stitziel NO, Won HH, et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature 2015;518:102–06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Morrison AC, Voorman A, Johnson AD, et al. Whole-genome sequence-based analysis of high-density lipoprotein cholesterol. Nat Genet 2013;45:899–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.NHLBI Whole Genome Sequencing Project. (22 August 2015, date last accessed).
- 111.Huan T, Meng Q, Saleh MA, et al. Integrative network analysis reveals molecular mechanisms of blood pressure regulation. Mol Syst Biol 2015;11:799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yao C, Chen BH, Joehanes R, et al. Integromic analysis of genetic variation and gene expression identifies networks for cardiovascular disease phenotypes. Circulation 2015;131:536–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Huan T, Zhang B, Wang Z, et al. A systems biology framework identifies molecular underpinnings of coronary heart disease. Arterioscler Thromb Vasc Biol 2013;33:1427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370–79. [DOI] [PubMed] [Google Scholar]
- 115.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med 2008;358:2249–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Andersson C, Lyass A, Larson MG, et al. Physical activity measured by accelerometry and its associations with cardiac structure and vascular function in young and middle-aged adults. J Am Heart Assoc 2015;4:e001528. [DOI] [PMC free article] [PubMed] [Google Scholar]


