Abstract
In the past, cockroach allergen exposure assessment mainly focused on settled dust in homes in low-income urban cities in the United States. That choice was not wrong; without measureable levels of cockroach allergen, it is difficult to show associations with any home characteristics much less with health outcomes (e.g., allergy, asthma). However, recent studies in other suburban areas, schools, and other countries have elucidated the importance of cockroach allergen in these environments too. In addition, characterizing the underlying factors that give rise to cockroach allergen exposure (or protect against it) can lead to more targeted public health interventions. This review discusses different approaches to sampling indoor environments, interprets recent asthma and allergy studies, compares cockroach allergen levels from past studies with those of recent studies, and describes strategies to decrease exposures.
Keywords: Cockroach allergen, exposure, Bla g 1, Bla g 2, environment, housing, schools, indoor air, house dust, allergy, asthma
Introduction
Since Arruda reviewed cockroach allergens in this journal [1], a few more allergens have been characterized, and the allergy nomenclature has been updated to include Per a 10, a serine protease from Periplaneta americana [2]. Also, there can be other components in cockroach exposure that are associated with allergy/asthma (e.g., chitin) [3, 4]. This review focuses on the measurement of Bla g 1 & 2 allergens, of which there have been the most exposure assessment studies for allergy and asthma.
Airborne cockroach allergen
Cockroach allergen has been thought to be carried mainly on larger particles ( > 10 microns) which are not easily airborne (i.e., without disturbing dust reservoirs), so that after 1990’s [5–7], few studies included air sampling of cockroach allergen in their exposure assessment protocols. Esposito et al.[8] reported that that not only could airborne cockroach allergen be detected in homes with cockroaches, but that it could be measured using a relatively simple technique that is often used for other particulate matter (PM) sampling. In this study, children with asthma living in low-income apartments in New York City (NYC) participated in an allergen avoidance study. Other inclusion criteria were 1) the child was skin prick test (SPT) positive to cockroach allergen and 2) the primary caregiver reported that the apartment had an ongoing cockroach infestation. The researchers aimed to collect at least 5 mg of dust on the air filters, so air was sampled for 7 consecutive days with pumps (flow rate = 10–15 lpm) that were placed in kitchens and bedrooms of each home (n= 16 homes). Each pump was equipped with a two polytetrafluoroethlyene (PTFE) filters in 37 mm cassettes; one filter cassette was placed at 0.3m (near the floor) and the other was at 1 m (a child’s breathing zone). Kitchen air at the 1-meter height had higher concentrations of Bla g 2 than those in the bedroom (geometric mean (GM)=4.0 pg/m3 and 2.5 pg/m3, respectively at p < 0.10), but the two locations were also highly correlated (r = 0.89, p < 0.001). In addition, the correlation between the Bla g 2 measurements at 0.3 and 1.0 meter were strong for both kitchen and bedroom locations (r = 0.92 and r = 0.98, respectively). The overall conclusion of the strong correlation between kitchen and bedrooms was that airborne cockroach allergen contains a substantial number of particles < 10 microns which could result in a chronic exposure because of normal domestic activity.
The importance of measurement locations within a home
For many years, the highest concentrations of cockroach allergen in homes have been found in the kitchen [9–11]. In addition, levels found elsewhere (e.g., bedroom, living room) are often too low to measure reliably [6]. So, the kitchen is where many investigators focused their cockroach allergen avoidance strategies and often their exposure assessment. Recent studies have challenged this approach. In a pooled analysis of nine US urban studies of allergy/asthma, bedroom levels of cockroach allergens were not only correlated with kitchen levels, but they were also affected by the presence of carpeting in the bedroom [12]. The studies were from several large urban areas including, Boston, New York, Cincinnati, Cleveland, Baltimore, and Seattle. Of the nine studies that contributed data to the pooled analysis, six were randomized controlled trials, two were non-randomized controlled studies, and one was a birth cohort study. For the analysis, only baseline or pre-intervention data were included because the aim was to identify housing characteristics prior to intervention that could serve as a screening tool to predict high allergen levels. One of the main findings of this pooled analysis was that bedrooms with carpet had lower levels than those without carpet. Presumably, carpet was protective because the children had an opportunity to wipe their feet (intentionally or not) before they got into bed. However, the lack of carpeting as a risk factor for cockroach allergen must be viewed in balance with prior studies that have found carpeting increases the risk of high dust mite allergen levels, given the right geography, climate, and housing type [13–16].
One study site in the pooled analysis, Baltimore, also had data that showed infrequently washing comforters (i.e., type of thick top-layer bedding) was protective against high Bla g 1 levels (odds ratio (OR)= 0.2 for levels ≥ 2 Units (U)/g and OR= 0.2 for levels ≥ 8 U/g) [16]. A possible explanation could be that in homes that had food/drink spills on the beds (i.e., a sign of eating in the bedroom which could lead to cockroach infestation) the residents had to wash their comforters often, whereas in homes without food/drink spills (i.e., no eating in the bedroom) the residents did not have to wash their comforters frequently. This finding was discussed in a manuscript about suburban room characteristics and indoor allergens, but it could easily apply to urban and rural homes too.
A factor that made the pooled analysis mentioned above difficult to conduct was the variety of sampling methods used in each of the studies. Differences in sampling methods could also be the reason some studies have not been able to show an association between cockroach allergen exposure and cockroach sensitization. In a recent study by Olmedo et al [17], levels of Bla g 2 in beds were significantly associated with cockroach-specific IgE among a case-control study of children living in low- and high-asthma prevalence neighborhoods in NYC (OR = 1.9 [1.4–2.6], p<0.001). The study enrolled children ages 7–8 through an insurance plan that serves mainly middle-income families. During the home visit, the upper half of the bed (near the breathing zone rather than the foot of the bed) and both sides of pillows were vacuumed for 3 minutes. The dust was analyzed with ELISA in the Columbia University researcher’s lab via the relatively new Universal Allergen Standard (Indoor Biotechnologies, Inc. Charlottesville, VA). The levels of Bla g 2 were higher in the beds of children living in the high-asthma prevalence neighborhoods (including the Bronx, Harlem, Washington Heights) compared with those living in neighborhoods with low-asthma prevalence (e.g., some neighborhoods in Queens and Brooklyn) (GM 22 ng/g vs. 37 ng/g, p=0.001). These findings confirm those of earlier inner-city asthma studies [18–22] and a recent rural childhood asthma study [23] that showed bedroom dust containing high levels of cockroach allergen is associated with allergic sensitization. The Inner-city Asthma Study (ICAS) found that bed and/or bedroom floor (i.e., the highest concentration from either bed or the bedroom floor sample) was associated with allergen sensitization [21]. Both the National Cooperative Inner-city Asthma Study (NCICAS) and the rural asthma study found that this association held for a combined sample from bed and bedroom floor [22, 23]. The relationship between dust samples containing bedroom floor dust and allergic sensitization could be difficult to replicate in some types of housing. The bedroom floor dust can contain many large particles (e.g., dirt, salt) that can inflate the denominator of the allergen concentration metric (i.e. micrograms per gram of dust collected) and lead to a highly-variable estimate of cockroach allergen. Bed dust is more homogeneous (e.g., skin flakes and allergenic particles) and not usually subjected to vacuuming, thus it probably has greater precision than floor dust as a measure of cockroach allergen concentrations in settled dust. This latter point notwithstanding, cockroach allergen concentrations in bed dust might be too low to show relationships with allergic sensitization, given certain household characteristics (e.g., wearing shoes inside the home, presence of carpeting in the home, floor cleaning method, proximity of kitchen to bedroom).
A different NYC study found that the association held for kitchen levels of Bla g 2 and allergic sensitization [20]; however, this constant exposure in the bed likely reflects a greater dose, given that children spend approximately 8 hours in bed each night (and more for younger children and infants who take frequent naps). It is not unreasonable to think that the actual time spent in the kitchen is much lower, unless, the family lives in a small studio apartment where the division between the kitchen area and the bedroom area is not well-defined. An earlier study in Baltimore also found that kitchen Bla g 1 was associated with sensitization [24]. For both NYC and Baltimore inner-city neighborhoods, apartment units are smaller, so this association might not hold for larger suburban homes. In fact, the Olmedo et al. study showed that sensitization to cockroach allergen was more common among children living in the high asthma prevalence neighborhoods compared with the low asthma prevalence neighborhoods (24% vs. 11%, p=0.01). The authors speculated that the main difference between the two types of neighborhoods was the building type. More multi-family apartment buildings were in the high asthma prevalence neighborhoods and more single-family homes were in the low asthma prevalence neighborhoods.
Housing and neighborhood factors
Income and building type
Exposure assessment strategies for cockroach allergen in suburban homes might vary from those in inner-city homes for reasons mentioned above. A recent study in Canada by Loo et al., [25] was conducted to assess the levels of indoor allergens and the predictive ability of questionnaire and inspection. A questionnaire about asthma and air pollution was administered to 5,559 parents of Grade 1 & 2 schoolchildren in Toronto, then a subset of 60 owner-occupied homes were inspected and sampled for dust allergens (in the main living area of the child other than the bedroom) during summer and fall months. Only one home reported current presence of cockroaches in the home. So, it was not surprising that Bla g 1 was below the limit of detection (0.04 U/G) for n=59 samples; one sample had insufficient amount of dust to conduct the ELISA. Income was categorized as lowest, lower middle, upper middle, and highest. Most (71%) of the homes in the home inspection subset were in the highest income category compared with the 2001 Canadian Census which found that 43.5% of Canadians were in the highest income category. Therefore, either the families that agreed to a home inspection/sampling visit did not have cockroaches in their homes (83% were single-family detached houses), or it could be that these families also had more resources to control cockroach infestations in their own home. The other possibility is that it was simply too cold to have a cockroach infestation in these homes.
Climate
In many cold-climate areas such as Sweden, Canada, upstate New York, and Minnesota, cockroach allergen is often low compared with those in warmer regions[25–28]. Yet, cockroach allergen can be found in urban areas that are cold. For example, a recent birth cohort study by Rosenfield et al [29] showed that Bla g 2 levels in the beds of NYC homes averaged 1.46 U/g (see section Allergen Concentration Conversion Factors for conversion to μg/g). Furthermore, 30% of the homes in the overall cohort had a measurement of Bla g 2 > 2 U/g which is not much lower than percentage of homes that contained Bla g 1 > 2 U/g in the Dallas study site of ICAS (47.7%) [21, 30].
A recent study of childhood asthma was conducted in Buffalo, NY by Lin et al. [27]. According to the national weather service [32], the average monthly temperature in Buffalo was < 10°C for December 2011-April 2012). Children ages 1–17 (n=193) were enrolled in this case-control study, and a subset of 99 was recruited for home environmental testing. Cockroach allergen was not detectable in most of the homes. Some homes had detectable Bla g 1 or Bla g 2, but the authors did not report the number of homes or the concentrations of those that were detectable. The possible reasons for low detection (beyond the cold climate of Buffalo) could be that similar to the Canadian study, very few homes (n=3) in the selected subset reported cockroaches in their homes (not that this is mutually exclusive with cold climate). Nonetheless, a high percentage of both the cases (42%) and controls (42%) were sensitized to cockroach allergen. Therefore, given climate change predictions, cockroach allergen exposure could occur in regions which heretofore have not experienced cockroach infestations [33].
Neighborhood-level factors
For a NYC birth cohort, newborns of Puerto Rican ethnicity with a maternal history of asthma and/or inhalant allergy were enrolled into the study [29]. A total of 274 mother/child pairs were recruited. Of those, 261 had address information that could be linked with the NYC Department of Buildings and NYC Dept. of Housing Preservation and Development databases that contained information about code violations at the building level, and by neighborhood. The number of housing code violations per 1000 rental units in a neighborhood was categorized. In adjusted regression models, living in a neighborhood with more housing code violations (per 1000 rental units) was associated with a greater odds of having Bla g 2 > 1 U/g in the mother’s bed. The authors stated: “Since one of our major findings was the importance of neighborhood-level housing code violations, it seemed important to adjust for building-level violations to see if this mediated any of the neighborhood level effect. It did not, and in fact, adjusting for building-level violations strengthened the neighborhood effect.” This study complements earlier studies in Boston (another cold- climate area) and Baltimore that showed families of lower SES had higher exposure to cockroach allergen, regardless of living in urban or suburban neighborhoods [18, 31].
Allergen concentration conversion factors
A recent article by Filep et al. [34] discussed conversion factors for allergen immunoassays that used different calibrations standards (i.e., those used in traditional ELISA on a 96-well microtiter plate vs. those used in the newer multiplex immunoassay with antibody-coated beads, MARIA® and also in the newer ELISA kits). Although internal validity for a given study conducted with these assays is not affected (as long as the same lot of standards were used), comparisons across studies using older vs. new calibration standards is problematic. In the Filep et al. study [34], individual purified allergen extracts (e.g., Bla g 2) and an allergen extract containing eight purified allergens: Bla g 2, Der f 1, Der p1, Der p 2, Fel d 1, Can f 1, Rat n 1, and Mus m 1 termed the universal allergen standard were assayed by ELISAs in 96-well microtiter plates. In addition, house dust extracts (n= 13–18) were analyzed by ELISA using both types of standards (the individual standard and the universal allergen standard). Two different methods were proposed for converting Bla g 2 allergen measurements from ELISAs using individual standards to those using the universal standard: 1) multiplying allergen measurements by 0.59 and 2) using a linear regression conversion equations (i.e., y = 0.67x + 22.59). In Table 1, the conversion factors for several studies from 1990s to present are shown. Different measures of central tendency were used in the studies, so in some cases, geometric means are reported; in other cases, median or arithmetic means were reported. Studies that could not be included in table 1 were those that only reported percentages above certain thresholds (e.g., percent of homes containing Bla g 2 > 2 U/g). In 1995, Bla g 2 Units were reported as equal to 40 ng of protein [35]. So this additional factor is used for converting allergen measurements of older studies reporting Bla g 2 U/g.
Table 1.
Comparison of Bla g 2 units in publications with conversion factors applied (from Units/g to μg/g).
| Converted Bla g 2 (μg/g)
|
||||||
|---|---|---|---|---|---|---|
| First author (year) | Study description | Location of sampling | Measure reported | Bla g 2 concentration (as published) | Via a single conversion factor | Assessed by linear regression equation |
| Call et al (1992) | Children with asthma in Atlanta, GA (n=35) | Multiple areas in home | Median | 20–30 U/g | 0.472–0.708 | 0.559–0.827 |
| Gelber et al (1992) | ER patients (with/without asthma in Delaware (n=51, with visual evidence of cockroaches) | Kitchen | Median | 30 U/g | 0.708 | 0.827 |
| Sarpong et al (1996) | Children with asthma in Baltimore (urban=15)(suburban=7) | Child’s Bed and Bedroom floor | Arithmetic mean | 2.8U/g | 0.066 | 0.098 |
| 2.4 U/g | 0.057 | 0.087 | ||||
| de Blay et al. (1997) | Homes (with reports of cockroaches) in Strasbourg, France (n=9) | Bed | Geometric mean | 3 U/g | 0.071 | 0.103 |
| Kitchen | 497 U/g | 11.729 | 13.342 | |||
| Stelmach et al (2002) | Children with asthma in Poland | Child’s Bed and Bedroom floor (n=16) | Arithmetic mean | 9.37 U/g | 0.221 | 0.274 |
| Kitchen (n=27) | 75 U/g | 1.770 | 2.033 | |||
| Chew et al. (2003) | Birth cohort in inner-city NYC | Child’s Bed (n=124) | Geometric mean | 0.07 μg/g | 0.041x | 0.069 |
| Kitchen (n=121) | 0.3μg/g | 0.3μg/g | 0.043 | |||
| Brugge et al. (2003) | Children with asthma living in public housing in Boston (n=9) | Kitchen | Arithmetic mean | 2.5 U/g | 0.059 | 0.090 |
| Chew et al. (2006) | Residents living in public housing in NYC | Bed (n=269) | Median | 1.8 U/g | 0.042 | 0.071 |
| Kitchen (n=321) | 35.9 U/g | 0.847 | 0.985 | |||
| Peters et al (2007) | Children with asthma living in public housing (Boston, n=46) | Child’s Bed | Median | 1.99 U/g | 0.047 | 0.076 |
| Kitchen | 198 U/g | 4.673 | 5.329 | |||
| Rosenfeld et al. (2008) | Birth cohort in NYC ( n=221) | Mother’s Bed | Geometric mean | 1.46 U/g | 0.034 | 0.062 |
| Median | 0.5 U/g | 0.012 | 0.036 | |||
| Chew et al. (2008) | Children with asthma that attended Head Start daycare in inner-city NYC (n=330) | Child’s Bed | Geometric mean | 4.8 U/g | 0.113 | 0.151 |
| Kitchen | 15.3 U/g | 0.361 | 0.433 | |||
| Olmedo et al, (2011) | Children with same health insurance plan living in NYC | High asthma prevalence neighborhood, (n=120) | Geometric mean | 0.037 μg/g | n/a d | n/a d |
| Low asthma prevalence neighborhood, n=120) | 0.022 μg/g | |||||
| Lin et al. (2011) | Children in Buffalo, NY (n=99) | Bedroom | Median | BDa | n/a | n/a |
| Breysse et al. (2011) | Children with asthma living in Milwaukee, WI (n=121) | TV room | Median | BDb | n/a | n/a |
| Perry et al. (2012) | Asthmatic children living in Rural Arkansas (n=109) | Child’s Bedroom | Median | BDc | < 0.024 | < 0.049 |
| Permaul et al. 2012 | School study & Children with asthma in Boston | Schools (n=12) | Geometric mean | 0.200 μg/g | n/a d | n/a d |
| Homes (Child’s bed and bedroom floor) (n=118) | 0.200 μg/g | |||||
Below limit of detection (BD) value = not reported in manuscript
Below limit of detection (BD) value = 0.02 μg/g
Below limit of detection (BD) value = 1 U/g
This value was not applicable because the Universal Allergen Standard (UAS) was used in the MARIA (or ELISA) for estimation of Bla g 2 concentrations.
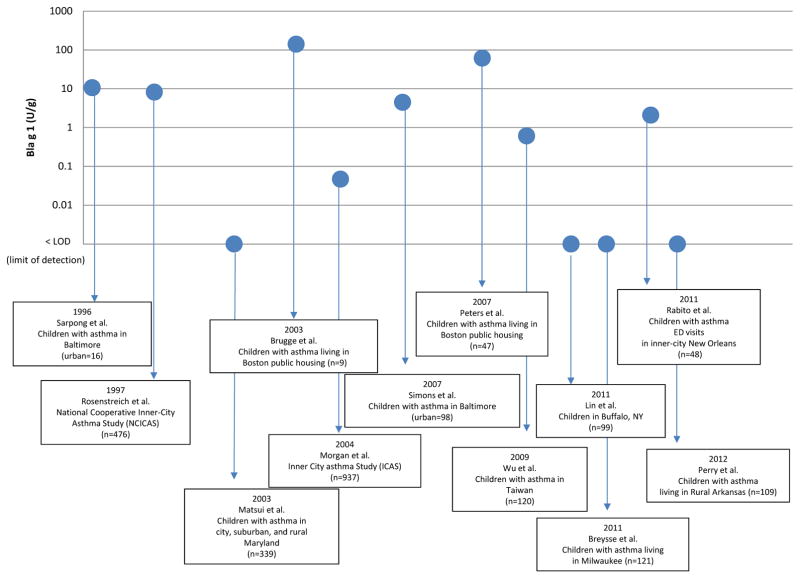
Even after adjusting for the conversion factors, it appears that there has been a drift toward decreasing cockroach allergen levels in studies of childhood asthma, primarily in urban areas. Bla g 1 was not affected by the conversion factor issue and has always been reported in Units/gram of settled dust. In Figure 1, more of the earlier studies of cockroach allergen in low-income urban environments seemed to have higher Bla g 1 central tendencies (e.g., median or geometric means, GM). Other studies were not included because they were birth cohorts, large national studies (based upon population-based sampling without regard to asthma status), interventions where a high level of cockroach allergen was an inclusion criterion (explicitly or implicitly), or because allergen levels were only reported as a percentage above certain cockroach allergen thresholds (i.e., 1 U/g, 2 U/ or 8 U/g). The Matsui et al. [24] study included suburban, urban and rural homes, and the median was reported across all locations, so it was not possible to plot the median just for the urban Baltimore population; this seems to be the one outlier for earlier studies of cockroach allergen levels being higher than the more recent studies. In addition, the later studies also occurred in more northern states and this could be another reason for lower cockroach allergen levels. Not that cockroaches cannot survive cold weather in homes, but rather, the type of housing that was sampled in these cities might have been more single-family detached houses. The recent Perry et al. [23] study of low-income children with asthma living in rural Arkansas also had a low central tendency measure of Bla g 1 (and also Bla g 2). Given that the public health message for the past one to two decades has been to decrease cockroach allergen exposure in urban environments in order to decrease a main trigger of children with asthma, it could be that this message is also reaching rural and suburban communities.
Figure 1.
A timeline of cockroach allergen measurements (Bla g 1) in childhood asthma studies
Strategies to decrease cockroach allergen exposure
The only way to systematically check this decrease in cockroach allergen levels is through population-based studies. In the recently-published Healthy People 2020 goals [36], decreases in health disparities (including asthma) are listed as an overall objective and evaluation is based upon nationwide surveys such as the American Healthy Homes Survey (AHHS) which was an offshoot of the National Survey of Lead and Allergens in Housing (NSLAH) and is scheduled to be continued again within this decade. In both of these surveys, home visits were conducted based upon a population–based clustering approach. For the 2005/6 AHHS, over 1,131 households were enrolled and a subset was randomly selected for allergen measurements in their homes. In the justification for the specific objective related to cockroach allergen, levels from the 2006 AHHS were set as the baseline level and by the year 2020, at least a 10% decrease in cockroach allergen levels should be achieved by public health efforts at federal, state, and local levels. According to the 2006 AHHS, the 90th percentile of cockroach allergen was 0.51 Bla g 1 Units/g in house dust samples. The 90the percentile was chosen because targets are difficult to base upon measures of central tendency (e.g., median, geometric mean) when a large percentage of non-detect values exist in the AHHS database. Targeting reductions in the concentrations at higher percentiles is significant from a public health perspective because these exposures represent a worst case scenario for adverse health effects (i.e., asthma and allergies). The strategies to get to those targets are discussed below.
Public health practitioners strongly recommend the use of integrated pest management (IPM) to control cockroaches in both homes and schools [37–39]. Two recent studies, one in schools and the other in homes, incorporated IPM principles as part of an allergen avoidance strategy. In an IPM study in North Carolina schools, Nalyanya et al. [40]compared cockroach trap counts and cockroach allergen levels (Bla g 1) in 13 schools (6 which used conventional pesticide application and 7 which used IPM) [40]. During a single academic year, cockroach populations were monitored (using sticky traps) and dust was collected in classrooms where teachers had seen cockroaches or where the investigators’ identified evidence of cockroaches. Monitoring and dust collection also occurred in food service areas and faculty/staff areas. Like the Boston school study, cockroach allergen levels were lower in the classrooms than in food service areas even though the North Carolina classrooms were selected based upon report of cockroaches. While cockroach trap counts were significantly different between IPM and conventional pesticide treatment schools (0 vs. 83 cockroaches per trap per week, P < 0.001), there was no significant difference in classroom concentrations of Bla g 1 between IPM-treated and conventionally-treated schools; the medians were the same (i.e., below limit of detection).
This is not to say that IPM did not work. Rather, the ability to detect differences in cockroach allergen in classrooms with regard to type of pest control strategy or repeated measures [41] is difficult. The classrooms of schools are often swept frequently and access to difficult-to-reach areas (e.g., behind bookcases, under radiators, and inside crowded cabinets) often limits vacuuming to only smooth floor surfaces that are devoid of cockroach allergen. Permaul et al. [42] recently showed that Boston schools contained Bla g 2 (GM = 0.2 μg/g). Dust and air samples were collected from 12 inner-city schools and dust was also collected from bedrooms of students with asthma (n=118) that attended these schools. The levels of Bla g 2 in dust from homes and schools were not significantly different; both were low (GM = 0.2 μg/g for both locations). Also, air concentrations of Bla g 2 were not reported, most likely because there were few positive samples. Possible explanations for why the levels of cockroach allergens were low in the school could be the cold climate (although this must be balanced with the earlier discussion above) or that pest management was effective in the schools.
Persky et al., [43] recruited and randomized pregnant women into the study from 1998–2004. Study participants from health clinics were eligible if the unborn baby had a family history of atopy and the mother lived in the west side of Chicago (a primarily Latino and African American population). The intervention consisted of three educational home visits by a community health educator during pregnancy in 2nd and 3rd trimesters and when the baby was 4 months old. IPM messages included identification of cockroach droppings, use of gel baits, and removal of harborage areas. In addition, the mothers were given mattress covers for their beds. A total of 328 homes had complete baseline and 1-yr follow-up measurements of Bla g 1 in vacuumed dust from the living room. Compared to mothers who received only basic health education, the intervention group reported a significant decrease in cockroach infestation. However, the decrease in the percent of homes with detectable Bla g 1 in the living room was not significantly different between the intervention group and the group receiving only basic health education (Intervention group: 50% at baseline and 47% at 1-year follow-up vs. Basic health education group: 45% at baseline and 37% at 1-year follow-up, p =0.64). The authors speculated that the basic education group modified their environment too, so this was a main the reason for no null findings for cockroach allergen. However, it is also possible that levels of cockroach allergen expressed in mass per unit area might have decreased and/or that levels in other areas of the home (e.g., bed, kitchen) might have decreased, or that merely using “percent of homes with detectable Bla g 1″ is too high of a target to be able to see a decrease.
Other factors associated with cockroach exposure that are relevant to allergy and asthma
The final issue to discuss is whether cockroach allergen measurements alone are enough for characterizing the biologically-relevant exposures to cockroaches. Rabito et al. [44] enrolled 86 children (ages 4–17 years) with allergic asthma from allergy clinics that serve mainly low-income patients in New Orleans, LA. Cockroach allergy was assessed by allergen specific IgE, and dust samples were collected from the kitchen floors in the children’s homes in order to asses Bla g 1 concentrations. One of the main findings of this study was that cockroach exposure (Bla g 1 > 2 U/g) was associated with asthma-related hospitalizations, adjusting for cockroach sensitization (OR=5.41, 95%CI, 1.14–25.62). In other words, cockroach allergen exposure was associated with asthma-related hospitalizations even for children who were not sensitized to German cockroach extract. The authors speculated that cockroach exposure in the kitchen (Bla g 1 > 2 U/g) could be a proxy for some other social (e.g., stress) or environmental exposure. Specifically, they mentioned one environmental exposure could be proteases in the cockroach frass. Earlier research from investigators in New Orleans showed that cockroach extracts have protease activity [45] and interest in proteases and protease-activated receptors (PAR) has increased recently as described in detail by another article in this issue of Current Allergy and Asthma Reports [46]. Clearly, there remain many research questions about cockroach allergen exposure assessment.
Conclusion
The two basic research questions about cockroach allergen exposure assessment are: 1) how? and 2) where to sample? One of the studies in this review suggests that air sampling deserves another look. Longer sampling times and lower flow rates can lead to recovery of cockroach allergen in air [8]; however, this might only hold for those homes (and possibly schools) where there are high concentrations of cockroach allergen in reservoir dust. Only by examining where the biologically-relevant exposures to cockroach allergens occur, will allergen avoidance strategies achieve success. Ideally, personal sampling for allergens could help in this endeavor. When air sampling is not feasible, several locations in the home can be vacuumed to collect dust. The dust measurements often vary by type of dust. Bed dust usually has lower concentrations of cockroach allergen, but it is more homogenous in dust consistency. Kitchen dust can contain higher concentrations of cockroach allergen, but it is heterogeneous in consistency. Recent data show that bedroom allergen concentrations can be affected by carpeting and other factors that might be independent of cockroach infestations elsewhere in the home [12]. Other important factors to consider when assessing cockroach allergen exposure are neighborhood and climate. Living in a suburban or rural neighborhood in a colder climate without cockroach infestations could mean that a family could leave used dishes in the sink and food uncovered in the kitchen without worrying about cockroaches migrating from other attached homes. On the other hand, once these homes become infested, the cockroach allergen issues are similar to those in the urban environments [16, 23, 24, 47]. That said, there seems to be a decreasing trend in cockroach allergen in homes of children with asthma living in the low-income environments, namely inner-cities. This is merely an observation based upon published literature with Bla g 1 levels in childhood asthma studies, but it can be tested with national surveys. If the levels are decreasing, then perhaps public health messaging and clinical recommendations about cockroach exposure are working.
Abbreviations
- AHHS
American Healthy Homes Survey
- Bla g 1
Cockroach allergen found in Blatella germanica
- Bla g 2
Cockroach allergen found in Blatella germanica
- Can f 1
Dog allergen found in Canis familiaris
- Der f 1
Dust mite allergen found in Dermatophagoides farinae
- Der p 1
Dust mite allergen found in Dermatophagoides pteronyssinus
- ELISA
Enzyme-linked immunosorbent assay
- Fel d 1
Cat allergen found in Felis domesticus
- GM
Geometric mean
- ICAS
Inner-city asthma study
- IPM
Integrated pest management
- MARIA®
Multiplex array for indoor allergens
- Mus m 1
Mouse allergen found in Mus musculus
- NCICAS
National cooperative inner-city asthma study
- NSLAH
National survey of lead and allergens in housing
- NYC
New York City
- OR
Odds ratio
- PAR
Protease activated receptor
- Per a 10
Cockroach allergen found in Periplaneta americana
- PM
Particulate matter
- PTFE
polytetrafluoroethlyene
- Rat n 1
Rat allergen found in Rattus norvegicus
- SPT
Skin prick test
- U
Units
Footnotes
The findings and conclusions in this manuscript are those of the author and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
References
- 1.Arruda LK. Cockroach allergens. Curr Allergy Asthma Rep. 2005;5(5):411–6. doi: 10.1007/s11882-005-0015-y. [DOI] [PubMed] [Google Scholar]
- 2.Sudha VT, Arora N, Singh BP. Serine protease activity of Per a 10 augments allergen-induced airway inflammation in a mouse model. Eur J Clin Invest. 2009;39(6):507–16. doi: 10.1111/j.1365-2362.2009.02112.x. [DOI] [PubMed] [Google Scholar]
- 3.Reese TA, et al. Chitin induces accumulation in tissue of innate immune cells associated with allergy. Nature. 2007;447(7140):92–6. doi: 10.1038/nature05746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elias JA, et al. Chitinases and chitinase-like proteins in T(H)2 inflammation and asthma. J Allergy Clin Immunol. 2005;116(3):497–500. doi: 10.1016/j.jaci.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 5.de Blay F, et al. Dust and airborne exposure to allergens derived from cockroach (Blatella germanica) in low-cost public housing in Strausbourg (France) J Allergy Clin Immunol. 1997;99:107–112. doi: 10.1016/s0091-6749(97)70307-5. [DOI] [PubMed] [Google Scholar]
- 6.Mollet JA, et al. Evaluation of German cockroach (Orthoptera: Blattellidae) allergen and seasonal variation in low-income housing. J Med Entomol. 1997;34(3):307–311. doi: 10.1093/jmedent/34.3.307. [DOI] [PubMed] [Google Scholar]
- 7.De Lucca SD, et al. Measurement and characterisation of cockroach allergens detected during normal domestic activity. J Allergy Clin Immunol. 1999;104(3):672–680. doi: 10.1016/s0091-6749(99)70341-6. [DOI] [PubMed] [Google Scholar]
- 8.Esposito WA, et al. Quantitative measurement of airborne cockroach allergen in New York City apartments. Indoor Air. 2011;21(6):512–20. doi: 10.1111/j.1600-0668.2011.00728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pollart SM, et al. Environmental exposure to cockroach allergens: Analysis with monoclonal antibody-based enzyme immunoassays. J Allergy Clin Immunol. 1991;87:505–510. doi: 10.1016/0091-6749(91)90009-d. [DOI] [PubMed] [Google Scholar]
- 10.Call RS, et al. Risk factors for asthma in inner city children. J Pediatr. 1992;121:862–866. doi: 10.1016/s0022-3476(05)80329-4. [DOI] [PubMed] [Google Scholar]
- 11.Gelber LE, et al. Sensitization and exposure to indoor allergens (dust mite, cat, and cockroach) as risk factors for asthma among patients presenting to hospital. Amer Rev Respir Dis. 1993;147:573–578. doi: 10.1164/ajrccm/147.3.573. [DOI] [PubMed] [Google Scholar]
- 12.Wilson J, et al. Housing and allergens: a pooled analysis of nine US studies. Environ Res. 2010;110(2):189–98. doi: 10.1016/j.envres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Arlian LG, et al. Prevalence of dust mites in the homes of people with asthma living in eight different geographic areas of the United States. J Allergy Clin Immunol. 1992;90:292–300. doi: 10.1016/s0091-6749(05)80006-5. [DOI] [PubMed] [Google Scholar]
- 14.Munir AK. Mite sensitization in the Scandinavian countries and factors influencing exposure levels. Allergy. 1998;53(48 Suppl):64–70. doi: 10.1111/j.1398-9995.1998.tb05001.x. [DOI] [PubMed] [Google Scholar]
- 15.van Strien RT, et al. Mite antigen in house dust: relationship with different housing characteristics in the Netherlands. Clin Exp Allergy. 1994;24:843–853. doi: 10.1111/j.1365-2222.1994.tb01807.x. [DOI] [PubMed] [Google Scholar]
- 16.Perry TT, et al. Room-specific characteristics of suburban homes as predictors of indoor allergen concentrations. Ann Allergy Asthma Immunol. 2006;97(5):628–35. doi: 10.1016/S1081-1206(10)61092-7. [DOI] [PubMed] [Google Scholar]
- 17.Olmedo O, et al. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat, and dog allergens in New York City. J Allergy Clin Immunol. 2011;128(2):284–292. e7. doi: 10.1016/j.jaci.2011.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarpong S, et al. Socioeconomic status and race as risk factors for cockroach allergen exposure and sensitization in children with asthma. J Allergy Clin Immunol. 1996;97:1393–1401. doi: 10.1016/s0091-6749(96)70209-9. [DOI] [PubMed] [Google Scholar]
- 19.Eggleston PA, et al. Relationship of indoor allergen exposure to skin test sensitivity in inner-city children with asthma. J Allergy Clin Immunol. 1998;102(4):563–570. doi: 10.1016/s0091-6749(98)70272-6. [DOI] [PubMed] [Google Scholar]
- 20.Chew GL, et al. Cockroach allergen levels and associations with cockroach-specific IgE. J Allergy Clin Immunol. 2008;121(1):240–5. doi: 10.1016/j.jaci.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Gruchalla RS, et al. Inner City Asthma Study: Relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol. 2005;115(3):478–485. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Rosenstreich DL, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 23.Perry TT, et al. Uncontrolled asthma and factors related to morbidity in an impoverished, rural environment. Ann Allergy Asthma Immunol. 2012;108(4):254–9. doi: 10.1016/j.anai.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 24.Matsui EC, et al. Cockroach allergen exposure and sensitization in suburban middle-class children with asthma. J Allergy Clin Immunol. 2003;112(1):87–92. doi: 10.1067/mai.2003.1588. [DOI] [PubMed] [Google Scholar]
- 25.Loo CK, et al. Do questions reflecting indoor air pollutant exposure from a questionnaire predict direct measure of exposure in owner-occupied houses? Int J Environ Res Public Health. 2010;7(8):3270–97. doi: 10.3390/ijerph7083270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Munir AK, et al. Cat (Fel d I), dog (Can f I), and cockroach allergens in homes of asthmatic children from three climatic zones in Sweden. Allergy. 1994;49(7):508–16. doi: 10.1111/j.1398-9995.1994.tb01121.x. [DOI] [PubMed] [Google Scholar]
- 27.Lin S, et al. Childhood asthma and indoor allergen exposure and sensitization in Buffalo, New York. Int J Hyg Environ Health. 2012;215(3):297–305. doi: 10.1016/j.ijheh.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 28.Swanson M, Agarwal M, Reed C. An immunochemical approach to indoor aeroallergen quantification with a new volumetric air sampler: studies with mite, roach, cat, mouse, and guinea-pig antigens. J Allergy Clin Immunol. 1985;76:724–729. doi: 10.1016/0091-6749(85)90678-5. [DOI] [PubMed] [Google Scholar]
- 29.Rosenfeld L, et al. Are neighborhood-level characteristics associated with indoor allergens in the household? J Asthma. 2010;47(1):66–75. doi: 10.3109/02770900903362676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Acosta LM, et al. The New York City Puerto Rican asthma project: study design, methods, and baseline results. J Asthma. 2008;45(1):51–7. doi: 10.1080/02770900701815784. [DOI] [PubMed] [Google Scholar]
- 31.Kitch BT, et al. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. Environ Health Perspect. 2000 Apr;108(4):301–7. doi: 10.1289/ehp.00108301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NOAA (National Oceanic and Atmospheric Administration) Buffalo monthly temperature. 2012 [cited 2012 June 18]; Available from: http://www.erh.noaa.gov/buf/climate/buf_temp00s.php.
- 33.Institute of Medicine (IOM) Climate change, the indoor environment, and health. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 34.Filep S, et al. A multi-allergen standard for the calibration of immunoassays: CREATE principles applied to eight purified allergens. Allergy. 2012;67(2):235–41. doi: 10.1111/j.1398-9995.2011.02750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arruda LK, et al. Cloning of cockroach allergen, Bla g 4, identifies ligand binding proteins (or calycins) as a cause of IgE antibody responses. J Biol Chem. 1995;270(52):31196–201. doi: 10.1074/jbc.270.52.31196. [DOI] [PubMed] [Google Scholar]
- 36.HHS (US Department of Health and Human Services) Healthy People 2020 Topics and Objectives. 2012 [cited 2012 June 17]; Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=12.
- 37.Krieger J, et al. Housing interventions and control of asthma-related indoor biologic agents: a review of the evidence. J Public Health Manag Pract. 2010;16(5 Suppl):S11–20. doi: 10.1097/PHH.0b013e3181ddcbd9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crocker DD, et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2 Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 39.Everett Jones S, et al. School policies and practices that improve indoor air quality. J Sch Health. 2010;80(6):280–6. doi: 10.1111/j.1746-1561.2010.00502.x. quiz 321–3. [DOI] [PubMed] [Google Scholar]
- 40.Nalyanya G, et al. German cockroach allergen levels in North Carolina schools: comparison of integrated pest management and conventional cockroach control. J Med Entomol. 2009;46(3):420–7. doi: 10.1603/033.046.0302. [DOI] [PubMed] [Google Scholar]
- 41.Chew GL, Correa JC, Perzanowski MS. Mouse and cockroach allergens in the dust and air in northeastern United States inner-city high schools. Indoor Air. 2005;15:228–234. doi: 10.1111/j.1600-0668.2005.00363.x. [DOI] [PubMed] [Google Scholar]
- 42.Permaul P, et al. Allergens in urban schools and homes of children with asthma. Pediatr Allergy Immunol. 2012 doi: 10.1111/j.1399-3038.2012.01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Persky V, et al. The effect of low-cost modification of the home environment on the development of respiratory symptoms in the first year of life. Ann Allergy Asthma Immunol. 2009;103(6):480–7. doi: 10.1016/S1081-1206(10)60264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rabito FA, et al. Cockroach exposure independent of sensitization status and association with hospitalizations for asthma in inner-city children. Ann Allergy Asthma Immunol. 2011;106(2):103–9. doi: 10.1016/j.anai.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 45.Wongtim S, et al. Protease activity in cockroach and Basidiomycete allergen extracts. Allergy Proc. 1993;14(4):263–8. doi: 10.2500/108854193778811946. [DOI] [PubMed] [Google Scholar]
- 46.Page K. Role of Cockroach Proteases in Allergic Disease. Curr Allergy Asthma Rep. 2012 doi: 10.1007/s11882-012-0276-1. [DOI] [PubMed] [Google Scholar]
- 47.Simons E, et al. Indoor environmental differences between inner city and suburban homes of children with asthma. J Urban Health. 2007;84(4):577–90. doi: 10.1007/s11524-007-9205-3. [DOI] [PMC free article] [PubMed] [Google Scholar]