Abstract
Objectives:
We study changes in average disability over nearly two decades for a large epidemiological cohort of older Americans. As some people exit by mortality, do average disability levels for the living cohort rise rapidly, rise gradually, stay steady, or decline?
Method:
Data are from the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD) cohort for 1993–2010. Cohort members are aged 70+ in 1993 (mean = 77.5 years), and the survivors are aged 87+ in 2010 (mean = 90.2 years). Personal care disability (activities of daily living), household management disability (instrumental activities of daily living), and physical limitations are studied. We study average disability for the living cohort over time and the disability histories for decedent and survivor groups.
Results:
Average disability rises gradually over time for the living cohort. Earlier decedent groups have higher average disability than later ones. Near death, disability rises sharply for all decedent groups. Longer surviving groups have less average disability, and slower disability increases, than shorter surviving groups. All results are repeated for younger cohort members (baseline age = 70–79 years), older ones (baseline age = 80+ years), women, and men.
Discussion:
As a cohort ages, average disability among living members increases gradually, signaling behavioral, psychological, and biological fitness in very old persons.
Key Words: Change, Cohort, Disability, Frailty, Older Ages
In recent decades, disability among older Americans has attracted an increasing amount of attention among health researchers and policymakers, gerontologists, health care planners, persons engaged in the Social Security debate, and advocates for older persons (Jacobsen, Kent, Lee, & Mather, 2011; Wiener & Tilly, 2002). This attention is well founded. The U.S. population is aging, and the proportion of older persons is rapidly increasing. Disability risk is generally higher for individuals as they age, and disability rates are highest in older populations (Brault, 2012; Erickson, Lee, & von Schrader, 2012; Federman et al., 2010; He & Larsen, 2014; Nikolova, Demers, Beland, & Giroux, 2011; van Houwelingen et al., 2014). The interplay of population aging and age-related disability drives concerns about high medical and rehabilitation needs of older Americans.
What we know about disability changes in older adults comes largely from research using two approaches. One approach focuses on repeated cross-sectional data, which yield trends in age-specific disability prevalence over time. The other approach analyzes longitudinal panel data for individuals, which yield typical trajectories of disability as people age. Our own approach focuses on an epidemiological cohort so as to study disability levels and changes in a specific population over time. We follow a closed population and describe average levels of disability over time for cohort members. The distinctive value of this approach is in showing how disability changes for a group of people as they reach advanced ages, taking decedents into account along the way.
The two standard approaches (repeated cross-section and longitudinal panel) characterize living persons and do not take selective mortality—the process whereby the most ill, frail, and disabled individuals in a cohort are likely to die sooner than others (Vaupel, Manton, & Stallard, 1979; Vaupel & Yashin, 1985)—into account. The surviving population has less disability than it would absent mortality (Keyfitz & Caswell, 2005; Zajacova & Burgard, 2013). In this analysis, we study both cohort members who survive and those who die. Another common, though not universal shortcoming of the two standard approaches is that they study only community dwellers. This biases disability estimates downward because nursing home residents have high disability levels, and a nontrivial share of the U.S. older population resides in nursing homes (Caffrey et al., 2012; Redfoot & Houser, 2010). This analysis includes nursing home residents.
We study disability from 1993 to 2010 for a single closed cohort of older persons. The cohort is a large, well-defined sample of U.S. persons born 1890–1923. We trace mean disability as they age in their late 70s, 80s, and 90s. This is an epidemiological cohort (a panel of persons studied over a long period of time), not a birth cohort (people born the same year). Our analysis takes selective mortality explicitly into account, and covers community-dwelling plus institutionalized persons.
The central questions are as follows: How does average disability change over time as cohort members acquire functional problems and some die? Do mean disability levels for the cohort rise rapidly, rise gradually, stay steady, or decline over time? How does disability for the people who die compare with disability for those who remain alive? Our analysis shows how an aging cohort changes as both disablement and mortality processes act upon it.
The study design is innovative, yet straightforward. It uses two views: cohort average and cohort history. Cohort average represents the levels of disability for the living cohort across time. The living cohort is those cohort members who are alive at a given interview wave. Cohort history brings mortality explicitly into the analysis, showing disability retrospectively for decedent groups and survivor groups. Decedent groups are cohort members who die in the intervals between interviews. For each decedent group, their disability history up to death is shown. Decedent groups are mutually exclusive; a deceased person can only be in one group. Survivor groups are cohort members who remain alive up to a given interview wave. For each survivor group, their disability history up to that wave is shown. Survivor groups are not mutually exclusive; survivors alive at the time of a later wave are also members of earlier survivor groups. Together, the cohort average and cohort history views reveal disability dynamics as a fixed group of people age.
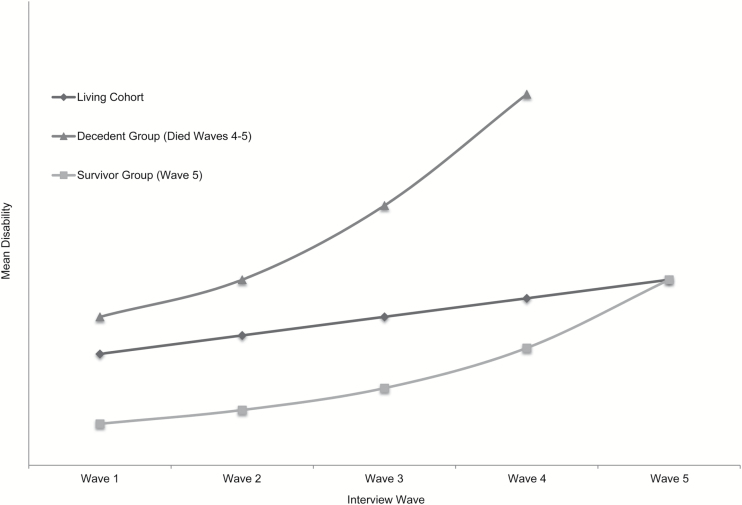
Figure 1 depicts the three groups (living cohort, decedent groups, and survivor groups). It is a hypothetical presentation for five interview waves. The black line represents disability levels for the living cohort at Waves 1–5. The dark gray line represents one decedent group—here, those who die between Waves 4 and 5. Their disability history up to Wave 4 is shown; they are deceased at Wave 5. The light gray line represents one survivor group—here, those who live up to Wave 5. Their disability history up to Wave 5 is shown. The survivor group is, in fact, the living cohort at Wave 5; the special feature is portraying their disability history prior to that.
Figure 1.
Hypothetical example of mean disability over time for living cohort, one decedent group, and one survivor group. The disability patterns shown in the figure are hypothetical. The purpose of the figure is to distinguish the cohort average (living cohort) and cohort history (decedents and survivors) views.
The principal scientific contribution of this analysis is that it shows that disability rises gradually for an older cohort as it ages. That is counterintuitive to the common assumption that disability rises steeply in older populations, especially as people age into their 80s and 90s. The truth is quite different from an epidemiological cohort perspective.
Data Source
Our data source is the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD) (Soldo, Hurd, Rodgers, & Wallace, 1997). The AHEAD cohort was first interviewed in 1993. The initial sample was nationally representative of the U.S. community-dwelling population born before 1924 who thus were aged 70+ at initial interview. In a given household, if the sampled respondent and his/her spouse/partner were both aged 70+, they were both included in AHEAD. Since 1993, respondents have been interviewed biennially, whether they remained in the community or moved to a nursing home. In 1998, AHEAD was merged with the Health and Retirement Study (HRS; hrsonline.isr.umich.edu). AHEAD is an epidemiological cohort, that is, a large, well-defined sample of persons whose life experiences are studied from initial interview onward. The many analyses of AHEAD data are cited in the HRS bibliography (hrsonline.isr.umich.edu; Papers and Publications/Online Bibliography).
We study disability over 17 years, from 1993 to 2010. The observation period covers nine interview waves of AHEAD data (1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, and 2010). Data come from the RAND HRS file, a user-friendly version of HRS/AHEAD data prepared by the RAND Corporation (Chien et al., 2013; www.rand.org/labor/aging/dataprod.html).
The AHEAD cohort age span is broad, so we also conduct separate analyses for two age strata, persons aged 70–79 years at baseline (1993) and those aged 80+ at baseline. Analyses stratified by age group allow us to examine whether “younger” and “older” populations have similar patterns of average disability changes as they age. In addition, we conduct separate analyses for women and men. Although older women have more illness, higher disability, and lower mortality than older men (see Discussion), women and men could have similar patterns of disability changes.
This is a short article, with only a few of the analysis tables and figures. The others are available as Supplemental Material. We provide here a brief guide to all tables and figures, by topic. (i) Background: Sociodemographic characteristics, Supplementary Table S1; Sample sizes, Table 1 (total), Supplementary Table S2 (age strata, gender); Disability frequency distributions, Supplementary Table S3; Hypothetical example, Figure 1. (ii) Total: Living cohort, Table 2, Figure 2; Decedent groups, Supplementary Tables S4A–C, Figure 3 (combined), Supplementary Figures S1A–C (separate); Survivor groups, Supplementary Tables S5A–C, Figure 4 (combined), Supplementary Figures S2A–C (separate). (iii) Age strata: Living cohort, Table 2, Figure 5; Decedent groups, Supplementary Tables S4A–C, Supplementary Figures S3A–F; Survivor groups, Supplementary Tables S5A–C, Supplementary Figures S4A–F. (iv) Gender: Living cohort, Table 2, Figure 6; Decedent groups, Supplementary Tables S4A–C, Supplementary Figures S3G–L; Survivor groups, Supplementary Tables S5A–C, Supplementary Figures S4G–L.
Table 1.
AHEAD Analysis Cohort, 1993–2010
| Interview Wavea | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | Wave 7 | Wave 8 | Wave 9 | |
| Respondents (living cohort) | 7,227 | 6,096 | 5,114 | 4,250 | 3,404 | 2,721 | 2,111 | 1,612 | 1,065 |
| Community dwelling | 7,227 | 5,850 | 4,753 | 3,884 | 3,049 | 2,409 | 1,846 | 1,386 | 877 |
| Nursing home | 0 | 246 | 361 | 366 | 355 | 312 | 265 | 226 | 188 |
| Nonrespondents | |||||||||
| Died since last wave (decedent groups) | 0 | 794 | 1,006 | 896 | 870 | 713 | 642 | 547 | 577 |
| Died earlier | 0 | 0 | 794 | 1,800 | 2,696 | 3,566 | 4,279 | 4,921 | 5,468 |
| Other nonresponse | 0 | 337 | 313 | 281 | 257 | 227 | 195 | 147 | 117 |
| Total AHEAD cohort | 7,227 | 7,227 | 7,227 | 7,227 | 7,227 | 7,227 | 7,227 | 7,227 | 7,227 |
Notes. Source: RAND HRS Data File, Version M. Unweighted counts.
AHEAD = Study of Asset and Health Dynamics Among the Oldest Old; HRS = Health and Retirement Study.
aWaves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
Table 2.
Mean Disability of the AHEAD Living Cohort (total, baseline age, gender), 1993–2010
| Interview Wavea | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | Wave 7 | Wave 8 | Wave 9 | |
| Total | |||||||||
| ADL | 0.37 | 0.61 | 0.71 | 0.77 | 0.86 | 0.90 | 1.04 | 1.12 | 1.29 |
| IADL | 0.46 | 0.60 | 0.73 | 0.81 | 0.94 | 1.03 | 1.22 | 1.28 | 1.44 |
| PLIM | — | 2.38 | 2.63 | 2.73 | 3.00 | 3.10 | 3.45 | 3.50 | 3.82 |
| Aged 70–79 years | |||||||||
| ADL | 0.28 | 0.42 | 0.54 | 0.59 | 0.68 | 0.74 | 0.93 | 1.04 | 1.23 |
| IADL | 0.28 | 0.38 | 0.52 | 0.61 | 0.73 | 0.86 | 1.12 | 1.21 | 1.38 |
| PLIM | — | 2.09 | 2.35 | 2.48 | 2.79 | 2.92 | 3.32 | 3.38 | 3.77 |
| Aged 80 and older | |||||||||
| ADL | 0.55 | 1.02 | 1.23 | 1.37 | 1.68 | 1.84 | 1.96 | 2.03 | 2.50 |
| IADL | 0.83 | 1.10 | 1.34 | 1.52 | 1.84 | 2.05 | 2.11 | 2.20 | 2.64 |
| PLIM | — | 3.04 | 3.45 | 3.59 | 3.92 | 4.12 | 4.51 | 4.84 | 4.94 |
| Women | |||||||||
| ADL | 0.42 | 0.70 | 0.81 | 0.86 | 0.96 | 1.01 | 1.13 | 1.24 | 1.40 |
| IADL | 0.51 | 0.70 | 0.83 | 0.93 | 1.05 | 1.18 | 1.37 | 1.46 | 1.57 |
| PLIM | — | 2.73 | 2.93 | 3.01 | 3.29 | 3.35 | 3.72 | 3.81 | 4.11 |
| Men | |||||||||
| ADL | 0.30 | 0.48 | 0.54 | 0.61 | 0.67 | 0.70 | 0.87 | 0.85 | 1.03 |
| IADL | 0.39 | 0.46 | 0.56 | 0.60 | 0.73 | 0.75 | 0.93 | 0.92 | 1.14 |
| PLIM | — | 1.90 | 2.12 | 2.24 | 2.44 | 2.62 | 2.92 | 2.84 | 3.15 |
Notes. Source: RAND HRS Data File, Version M. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
aWeighted means. For each ADL item, disability is scored present for yes response, personal help, and cannot do. For each IADL item, disability is scored present for yes response, personal or equipment help, cannot do/don’t do for health reasons. Disability counts (RAND file RwADLA, RwIADLZA) are sums of present items; item missing data ignored. For PLIMs, we use same recode and sum procedures. Question wordings and detailed recode procedures are in RAND documentation (Chien et al., 2013).
ADL = activity of daily living; AHEAD = Study of Asset and Health Dynamics Among the Oldest Old; HRS = Health and Retirement Study; IADL = instrumental activity of daily living; PLIM = physical limitation.
Figure 2.
Mean disability of the AHEAD living cohort (total), 1993–2010. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
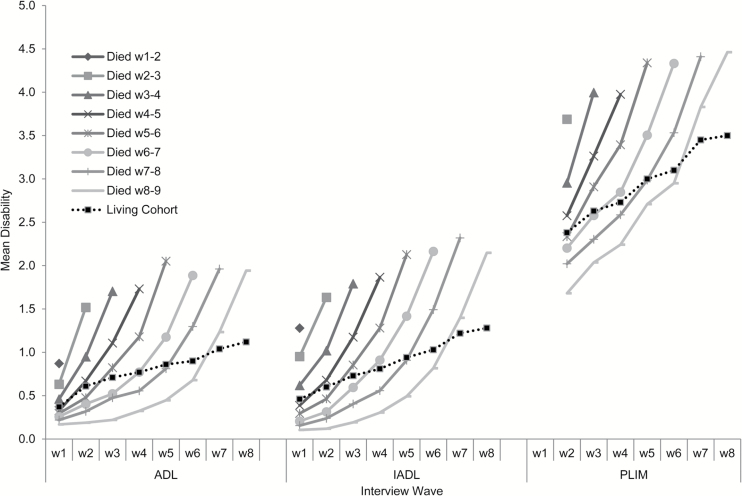
Figure 3.
Mean disability of AHEAD decedent groups (total), 1993–2010. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
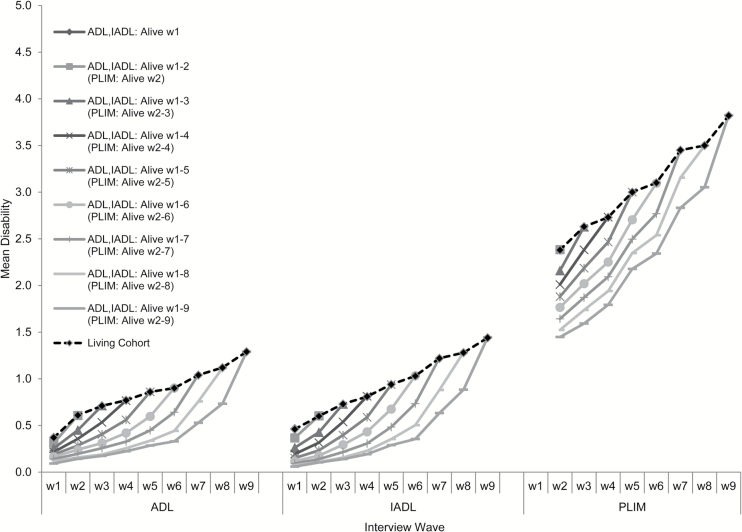
Figure 4.
Mean disability of AHEAD survivor groups (total), 1993–2010. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
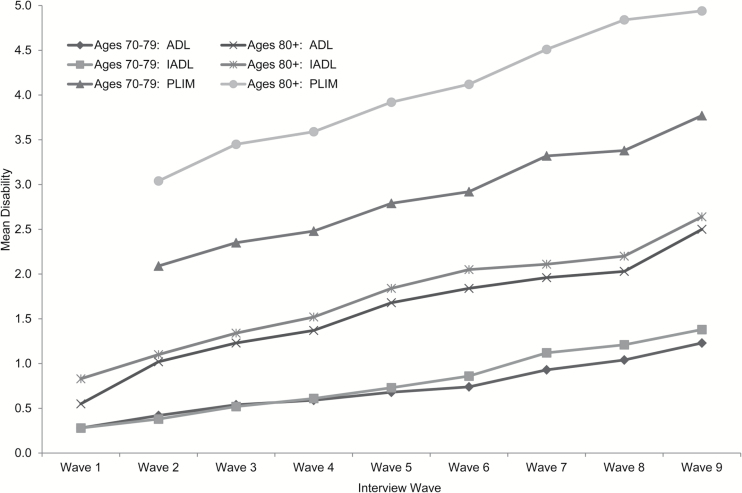
Figure 5.
Mean disability of the AHEAD living cohort by baseline age, 1993–2010. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
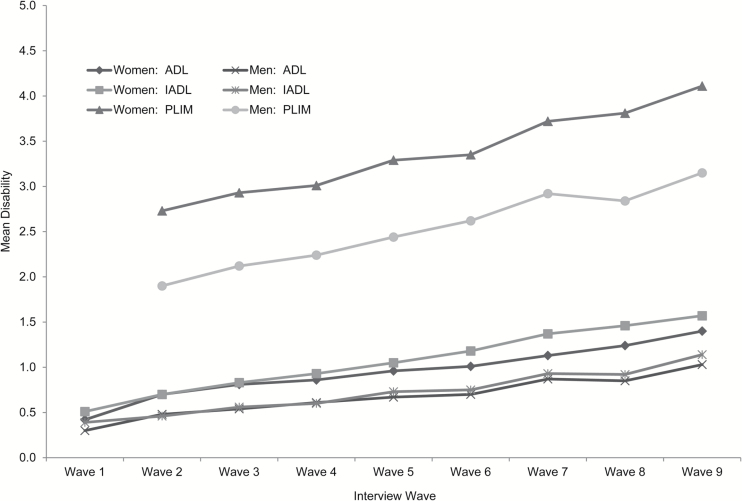
Figure 6.
Mean disability of the AHEAD living cohort by gender, 1993–2010. Waves 1–9 are years 1993, 1995, 1998, 2000, 2002, 2004, 2006, 2008, 2010.
Analysis Sample
At the 1993 AHEAD baseline, 7,442 age-eligible respondents were interviewed. Between 1993 and 2010, 215 people were permanently dropped from the sample for unstated administrative reasons. Our baseline analysis sample is thus of 7,227 persons.
The analysis includes nursing home residents. Analyses of HRS/AHEAD data often exclude them, although they are interviewed. The reason for this is usually technical, not substantive. Public data files provide nonzero respondent weights at each wave for community dwellers, but nursing home residents receive a weight of zero. Thus, they are automatically deleted in weighted analyses unless researchers prepare and assign nonzero weights. We think disability among the older U.S. population should be studied with nursing home residents included, so we developed appropriate weights for them (see Procedures).
Table 1 shows sample counts across the nine waves. After the initial interview (community-dwelling), some cohort members reside in nursing homes temporarily or permanently; the percentage of members residing in nursing homes rises from 4% (1995) to 18% (2010). Mortality reduces the cohort over time. Percentages of the living cohort who die between one wave and the next increase from 8% (1993 to 1995) to 36% (2008 to 2010). As of 2010, 84% of the initial cohort have died. Nonresponse for other reasons (presumed alive but no interview) is 2%–5% across the nine waves. Despite mortality and nonresponse, the number of cohort members interviewed in 2010 is still sizable (n = 1,065).
Sample counts for the living cohort, decedent groups, and survivor groups are as follows: The living cohort is cohort members alive and interviewed at a given wave (Table 1, top line). Average age for the living cohort rises over the observation period from 77.5 years in 1993 to 90.2 years in 2010 (Supplementary Table S1). Decedent groups are those who die between waves (Table 1, fourth line). For example, 794 people died between Waves 1 and 2, and 577 died between Waves 8 and 9. Average age for decedents rises over the observation period from 81.7 years for the first decedent group to 90.8 years for the last one. Survivor group numbers are the same as the living cohort (top line).
For age strata and gender, respondent counts in 1993 are 4,703 younger cohort members (baseline age = 70–79 years), 2,524 older ones (baseline age = 80+ years), 4,392 women, and 2,835 men. In 2010, their sample sizes are 999, 66, 727, and 318, respectively. Wave-by-wave sample sizes for age strata and gender are given in Supplementary Table S2.
Measures
Three types of disability are studied: personal care (activities of daily living [ADLs]), household management (instrumental activities of daily living [IADLs]), and physical limitations (PLIMs). Disability is defined as health-related difficulty in performing an activity for 3+ months. For ADL, five activities are used: walking across a room, dressing, bathing, eating, and getting in and out of bed. For IADL, five activities are used: using the phone, taking medications, managing money, shopping for groceries, and preparing meals. For PLIM, nine activities are used: walking one block, sitting for about 2 hours, getting up from a chair after sitting for long periods, climbing one flight of stairs without resting, lifting or carrying weights more than 10 pounds (such as a heavy bag of groceries), reaching arms above shoulder level, pushing or pulling large objects, picking up a dime from the table, and stooping, kneeling, or crouching. Conceptually, PLIMs are functional limitations rather than disability (Verbrugge & Jette, 1994), but we economize prose here and call all three outcomes disability. The analysis variables are number of activities with disability. ADL and IADL variables pertain to all years 1993–2010, but PLIM variables start in 1995 because the nine functional items are available only from that year forward. Means for disability variables at all waves are shown in Table 2, and frequency distributions for them are shown in Supplementary Table S3.
Procedures
The AHEAD sample design involves disproportionate weights and geographic clustering. Weighted analyses are necessary for unbiased estimates of population parameters. For community dwellers, we use respondent weights for each wave in the RAND data file. To obtain nonzero weights for nursing home residents, we followed recommendations in HRS sample design documentation and applied the “last valid weight” approach (Health and Retirement Study, 2011). The weight for a nursing home resident at Wave w equals the value of his/her weight the last (most recent) wave she/he resided in the community. To adjust for clustering, we use the svy suite of commands in Stata to compute complex variances (StataCorp, 2013).
We prepared tables and graphs of all results for the living cohort, decedent groups, and survivor groups. The figures in this article readily tell the story of cohort changes over time. They display wave-specific disability means (averages), and we observe changes in means over time.
It is easy to reify points and lines in the figures, but caution is warranted. There is individual variability around plotted means. Lines connecting means are just lines, not the actual path that cohort disability takes between waves. Further, all results are population-level, and interpretations are about groups of people as a whole. It is easy to slip into individual-level language, interpreting the results as usual paths of disability for individuals over time. In order to avoid this ecological fallacy, we routinely say “average disability” or “mean disability.” That can be tedious for readers, so we sometimes use “disability” when the context clearly implies average or mean.
Our goal is to get a clear picture of how the aging process unfolds over time for the cohort. Our analysis does not involve multivariate models that control for sociodemographic features of cohort members. Importantly, statistical controls for age would effectively remove aging from the cohort changes. To address the cohort’s large age span, we repeat the analysis for two narrower age strata. This allows us to assess whether disability patterns are robust among older persons regardless of specific age spans. To examine possible gender differences in disability patterns, we conduct separate analyses for men and women.
Results
Disability Over Time for the Living Cohort
For the living cohort, average disability of all types increases over 17 years (Figure 2). ADL disability means rise from 0.37 to 1.29 over the study period, IADL disability means from 0.46 to 1.44, and mean PLIMs from 2.38 to 3.82 (Table 2). PLIMs increase numerically more than ADL and IADL disabilities, but percentage increases are greater for ADL/IADLs. Regressions of disability by time show that the linear increases are statistically significant (p < .05). (The ADL/IADL disability increases from 1993 to 1995 contain some artifact of sample design. The 1993 sample is community dwellers, excluding nursing home residents, who are 10% of the population aged 70+ in the 1990 Census. As of 1995, respondents are interviewed wherever they live, whether in the community or in a nursing home.)
Disability Histories for Decedent Groups
Disability histories for decedent groups are shown in Figure 3. The disability values are shown in Supplementary Tables S4A–C. Supplementary Figures S1A–C show each disability separately and full-scale. There are eight decedent groups, starting with cohort members who died between 1993 and 1995 and ending with those who died between 2008 and 2010. Graphs show disability means for the decedent groups and connect each group’s history with a line. For example, the first decedent group had just one interview, and their one disability mean is plotted at the far left. The last decedent group had eight interviews, and their disability history is plotted from far left (Wave 1) to far right (Wave 8). As a reference for the decedent histories, the dashed line shows the living cohort means.
The main results are (i) Earlier decedent groups (those who die sooner) have higher average baseline disabilities than later decedent groups (those who die at later waves). The relationship is monotonic (later death is associated with lower initial disability levels). This initial difference is maintained at all waves; groups who die sooner always have higher average disabilities in a given period than those who die later. (ii) Baseline disability levels for early decedent groups are above the living cohort average and below the average for later decedent groups. Soon-to-die groups push up the living cohort mean, whereas later-to-die groups are much better off. A few waves before death, decedent groups always cross above the living cohort average. That crossing occurs sooner for earlier decedents; their disability levels are already higher and keep going upward as they approach death. (iii) Disability rises over time for every decedent group. Earlier decedent groups have steeper rises than later decedents. For the later groups, initial rises in disability are gradual but accelerate near end of life. Thus, near death, all decedent groups have steep rises in mean disability levels. (iv) Mean disability levels near death are similar across all decedent groups. Later decedent groups catch up with earlier ones. (From a microperspective, later decedent groups have slightly higher average disability near death than earlier decedent groups, but that difference is small compared with their overarching similarity.) (v) These results occur for all disability outcomes (ADLs, IADLs, and PLIMs). The precise shapes of change vary slightly: ADL and IADL disabilities have gradual, then steeper (curvilinear) rises, whereas PLIMs have quite steady (linear) increases.
Disability Histories for Survivor Groups
Disability histories for survivor groups are shown in Figure 4. The disability values are shown in Supplementary Tables S5A–C. Supplementary Figures S2A–C show each disability separately and full-scale. There are nine survivor groups, starting with cohort members alive in 1993 and ending with those alive in 2010. For example, the first survivor group contains all respondents alive in 1993; they had just one interview by that point, and their one disability mean is the 1993 living cohort average. The last survivor group is everyone living in 2010; they had nine interviews by that point, and their disability history is plotted from far left (Wave 1) to far right (Wave 9). As a reference for the survivor histories, the dashed line shows the living cohort means.
The main results are (i) Earlier survivor groups (those with shorter histories) have more baseline disabilities than later survivor groups (those with longer histories). The relationship is monotonic (later survivorship is associated with lower initial disability levels). This initial difference is maintained at all waves; earlier survivor groups always have more average disability than later ones. This is because the earlier groups contain early decedents (high disability), who are gone at later waves. (ii) Disability rises over time for every survivor group. Earlier survivor groups (which contain some people near death) have steeper rises than later survivor groups (whose members remain alive for all or most of the observation period). Still, for longer survivor groups, increases in ADL/IADL disability steepen as time goes on. The survivors are older, and some members are now near death. (iii) These results occur for all disability outcomes (ADLs, IADLs, and PLIMs). Shapes of change vary slightly: ADLs and IADLs have gradual then steeper (curvilinear) increases, whereas PLIMs have steady (linear) increases.
Comparing Living Cohort, Decedent Groups, and Survivor Groups
Average disability rises over 17 years for all groups (living cohort, decedent groups, and survivor groups). The increases are smallest for the living cohort, in between for survivor groups, and largest for decedent groups.
Surprisingly, decedent groups and survivor groups have similar patterns of change, even though they are different subgroups of the total cohort. We think the similarity is driven by the soon-to-die people contained in survivor groups, whose proportions increase in later waves.
Disability Patterns Over Time for Younger and Older Age Strata
Younger cohort members are aged 70–79 years at first interview, and older ones are aged 80+. Figure 5 shows the living cohort results by age strata. The disability values for the figure are in Table 2. For decedent group results by age, see Supplementary Tables S4A–C and Supplementary Figures S3A–F. For survivor group results by age, see Supplementary Tables S5A–C and Supplementary Figures S4A–F.
The main results for the living cohort, decedent groups, and survivor groups are as follows: (i) For living cohorts, all three types of disability increase over 17 years for both younger and older groups (Figure 5). ADL disability means rise from 0.28 to 1.23 for the younger group, and from 0.55 to 2.50 for the older one (Table 2). IADL disability means rise from 0.28 to 1.38 for the younger group, and from 0.83 to 2.64 for the older one. PLIM means rise from 2.09 to 3.77 for the younger group, and from 3.04 to 4.94 for the older one. In absolute terms, PLIM means increase in absolute size more than mean disabilities for ADLs and IADLs within both age strata, but percentage increases are greater for ADL/IADL disabilities. For decedent and survivor groups, results we found for the total cohort are repeated for younger and older groups. (ii) Differences in average disability levels for the age strata hold no surprises. For living cohorts, the older group has higher average disability than the younger one at all time points. For decedent and survivor groups, the older group has higher average disability than the younger one at all waves in their histories.
Disability Patterns Over Time for Women and Men
Figure 6 shows the living cohort results by gender. The disability values for the figure are in Table 2. For decedent group results by gender, see Supplementary Tables S4A–C and Supplementary Figures S3G–L. For survivor group results by gender, see Supplementary Tables S5A–C and Supplementary Figures S4G–L.
The main results for the living cohort, decedent groups, and survivor groups are as follows: (i) For living cohorts, all three types of disability increase over 17 years for both women and men (Figure 6). ADL disability means rise from 0.42 to 1.40 for women, and from 0.30 to 1.03 for men (Table 2). IADL disability means rise from 0.51 to 1.57 for women, and from 0.39 to 1.14 for men. PLIM means rise from 2.73 to 4.11 for women, and from 1.90 to 3.15 for men. For both genders, PLIM means increase in absolute size more than disability means for ADL and IADL, but percentage increases are greater for ADL/IADL disabilities. For decedent and survivor groups, results we found for the total cohort are repeated for women and men. (ii) Gender differences in average disability levels concur with prior literature. For living cohorts, women have higher average disability than men at all time points. For decedent and survivor groups, women have higher average disability than men at all waves in their histories.
Discussion
In this analysis, we have described changes in average disability levels over time in a cohort of older persons born 1890–1923 as they age across their late 70s, 80s, and 90s. We used two views: cohort average and cohort history. Cohort average captures the average experience of the surviving (living) cohort as both disablement and selective mortality processes act on it and change it over time. Cohort history incorporates mortality explicitly into the analysis, separating the total sample by time to death (decedent groups) and length of survival (survivor groups), and showing mean disability changes over time for each. Together, the two views provide a window into disability dynamics at older ages in the U.S. population.
Living Cohort
Average disability rises over time in the living cohort. Thus, increasing incidence and severity of disability, and sustained health and functional problems, exceed functional improvements, and even the exit of ill/frail persons. Yet strikingly, the rise in mean disability for the living cohort is gradual, modest, and linear. Over nearly two decades, ADL disabilities increase by just 1 disability on average, IADL disabilities by 1, and PLIMs by 1½. Mean disability at very advanced ages (late 80s and older) increases at about the same pace as the cohort experienced 10–15 years earlier, when they were 10 or more years younger. This suggests some intrinsic fitness in those who stay alive.
Research shows that very old people often have strong adaptation abilities and psychological resilience that reduce disability onset, enhance disability recovery, and prolong life (Clarke & Smith, 2011; Higgins, Janelle, & Manini, 2014; Infurna, Ram, & Gerstorf, 2013; Mendes de Leon, Seeman, Baker, Richardson, & Tinetti, 1996). Research also suggests that very old people have distinctive biological or genetic features that enhance longevity (Garatachea, 2013; Montesanto, Dato, Bellizzi, Rose, & Passarino, 2012; Ruiz et al., 2012). This combination of behavioral, psychological, and biological fitness constitutes a “disability and death inhibition” package for very old people.
Selective Mortality
Illness, frailty, and disability are risk factors for earlier death (Fried et al., 1998; Nybo et al., 2003; Rockwood et al., 2004; Shamliyan, Talley, Ramakrishnan, & Kane, 2013; Simons, McCallum, Friedlander, & Simons, 1996; Song, MacKnight, Latta, Mitnitski, & Rockwood, 2007; Tiainen, Luukkaala, Hervonen, & Jylha, 2013). Our results show that decedent groups have much higher average disability than nondecedents (survivor groups), not only just before death but earlier in their histories as well. This result for an epidemiological cohort aligns with the large literature based on individual-level data.
Steep Rises in Disability Near Death
Retrospective studies of middle-aged and older people who die show that disability rises sharply in the months or year just prior to death (Chaudhry et al., 2013; Gill, Gahbauer, Han, & Allore, 2010; Smith, Walter, Miao, Boscardin, & Covinsky, 2013). Our results using population, not individual-level, data are consistent with the literature. Steep rises in average disability occur for all decedent groups near death. The acceleration is broad-based, occurring for young-old people, older-old people, women, and men.
Strikingly, average disability levels near death are similar across decedent groups. This means that later decedent groups (whose histories show lower levels of disability) catch up to earlier ones in their disability profiles near death. Later decedents are older at death (on average) than earlier decedents were. But the results suggest that when circumstances arise that overcome “disability and death inhibition,” disability typically accelerates. The fact that all decedent groups show this steep rise concurs with recent studies showing that chronological age often doesn’t matter for the “dying process” (Riffe, Chung, Spijker, & MacInnes, 2015; Wolf, Freedman, Ondrich, Seplaki, & Spillman, 2015).
Similarities for Type of Disability, Age Strata, and Gender
The patterns of average disability change reported earlier appear for all types of disability (ADLs, IADLs, and PLIMs). There is just one difference: mean ADL/IADL disabilities rise in a gradual, then steep (curvilinear) pattern, whereas mean PLIMs show steadier (linear) increases. ADL/IADL disabilities reflect inability to survive, either at all or on one’s own, due to health, and these abilities can erode at advanced ages. Also, ADL/IADL disabilities sometimes arrive in bundled, catastrophic manner from injury, stroke, heart attack, and the like (Ferrucci et al., 1996; Onder et al., 2005). In contrast, PLIMs tend to accumulate slowly but steadily for individuals as they age. These individual-level results underlie the patterns of average change that we see for ADL/IADL disabilities and PLIMs.
Younger cohort members(baseline age = 70–79 years) and older members (baseline age = 80 and older) have disability patterns over time similar to those for the total cohort. This suggests that the population-level disability changes over time found here are generalizable. Other samples of older persons, and varied age spans, will likely display similar patterns. The AHEAD cohort represents a population with a distinctive sociocultural history (Carlson, 2009), but we believe their (average) disability experience in late life will be repeated in other cohorts with their own sociocultural histories.
Older women have more illness, higher disability, and lower mortality levels than older men (Hardy, Allore, Guo, & Gill, 2008; Leveille, Penninx, Melzer, Izmirlian, & Guralnik, 2000; Read & Gorman, 2011; Verbrugge, 1985). Consistent with the ample literature, women in the AHEAD cohort have higher average disability levels than men at all time points. But our results point to a more important, and brand new, result. Disability patterns over time (namely, the shapes of average disability changes) are the same for women and men. That suggests that basic forces embedded in aging, illness, frailty, and disablement operate similarly for both genders. Levels of mean disability may differ for the two groups, but patterns of disability change do not.
The disability averages and histories studied here go to 2010 (latest available data when our analysis began). A sizable percentage (16%) of the AHEAD cohort are still alive in 2010. What happens to them as they become still older and eventually die? The patterns for living cohort, decedent groups, and survivor groups are so systematic that we expect them to continue for the cohort after 2010. This is a hypothesis for empirical verification. Some support comes from studies of centenarians. Most people aged 100 and older have long (prior) histories of steady low or gradually increasing disability (Ailshire, Beltrán-Sánchez, & Crimmins, 2015).
Comparison with Another Cohort Analysis
To our knowledge, only one other group—Christensen, McGue, Petersen, Jeune, and Vaupel (2008)—has used an approach similar to ours to study cohort disability over time. This group studied a Danish birth cohort (born 1905) who were aged 92 years at start of study, with four interviews over 7 years. Despite differences in national context, sample sizes, ages, and observation length, the AHEAD and Danish analyses produce highly similar results. Both studies find (i) small rises in disability for the living cohort over time, (ii) larger rises in disability for survivor groups and decedent/stop groups than for the living cohort (Danish “stop” groups are nonresponders due to death, refusal, noncontact, or other reason), (iii) monotonic differences across the subgroups at every wave, with higher disability among shorter survivor groups and earlier decedent/stop groups, and (iv) sharper rises in disability over time for shorter survivor groups than for longer ones, and for earlier decedent/stop groups than for later ones. Both studies reach the same conclusion: As a cohort ages and the most ill/frail persons exit by death, average disability rises only a little for living cohort members. Our AHEAD analysis is more elaborate and thorough-going, with extensive results for the living cohort, decedent groups, and survivor groups in the observation period. We prepared a full explication of the Danish study for a working paper, but other publication formats are prohibited by this journal, so readers are welcome to contact us for the explication.
Conclusion
The commonplace assumption that disability rises sharply with age may be true for individuals and the general population, but it is not true from an epidemiological cohort perspective. Mean disability levels increase only gradually as a cohort ages, even when cohort members are in their 80s and 90s.
This is the first analysis of disability changes in a large epidemiological cohort for the United States. The results join the large literatures on population trends in disability, individual-level transitions and trajectories of disability, and selective mortality. Our age strata and gender results are fundamentally the same as for the total cohort, thus implying that the disability changes observed here are general and will exist in other epidemiological cohorts. Only large societal perturbations in aging, disablement, and death processes, or in availability of health care and rehabilitation, would be able to alter these contemporary patterns.
Very old persons typically have some disability, but far less than if all the initial members of their cohort were still present. To be sure, the decedents don’t just drop away with typically high disability and no health care; they receive plenty of medical and rehabilitation effort before death. Still, those on the pathway to live for more time have much less disability. Remarkably, their average level of disability is only slightly higher than for cohort members a decade or so earlier. This situation makes for low health care and rehabilitation needs. Longevous people are a hardy lot, possessing some sort of intrinsic fitness—behavioral, psychological, or biological, or perhaps all of these.
Supplementary Material
Please visit the article online at http://psychsocgerontology.oxfordjournals.org/ to view supplementary material.
Funding
D. C. Brown received support for this research from NICHD Center Grant R24 HD041028 and NIA Training Grant T32 AG000221 awarded to the Population Studies Center, University of Michigan.
Supplementary Material
Acknowledgments
We thank Brady T. West (University of Michigan) for statistical advice, Jean-Marie Robine (French National Institute of Health and Medical Research [INSERM]) for pointing us toward the analysis design, Cindy Glovinsky for professional editing and copyediting, and the reviewers and editors for fair critques and fine suggestions. Results were presented at the Population Association of America meeting (May 2015, San Diego, CA), the TRENDS Network meeting (May 2015, Ann Arbor, MI), and the REVES International Network on Health Expectancy meeting (June 2015, Singapore).
Author Contributions: L. M. Verbrugge conceived the analysis purpose and initial design. The design was jointly revised and implemented by all three authors over the project course. D. C. Brown performed data management, computing, and preparation of tables and figures. All three authors worked together on manuscript writing and revisions.
References
- Ailshire J. A. Beltrán-Sánchez H., & Crimmins E. M (2015). Becoming centenarians: Disease and functioning trajectories of older US adults as they survive to 100. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 70, 193–201. doi:10.1093/gerona/glu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault M. W. (2012). Americans with disabilities, 2010 (Current Population Reports P70-131). Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. [Google Scholar]
- Caffrey C. Sengupta M. Park-Lee E. Moss A. Rosenoff E., & Harris-Kojetin L (2012). Residents living in residential care facilities: United States, 2010 (NCHS Data Brief No. 91). Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22617169 [PubMed] [Google Scholar]
- Carlson E. (2009). 20th-century U.S. generations. Population Bulletin, 64, 2–16. [Google Scholar]
- Chaudhry S. I. Murphy T. E. Gahbauer E. Sussman L. S. Allore H. G., & Gill T. M (2013). Restricting symptoms in the last year of life. A prospective cohort study. Journal of the American Medical Association: Internal Medicine, 173, 1534–1540. doi:10.1001/jamainternmed.2013.8732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien S. Campbell N. Hayden O. Hurd M. Main R. Mallett J., … St. Clair P (2013). RAND HRS Data Documentation, Version M. Santa Monica, CA: RAND Corporation, RAND Center for the Study of Aging; Retrieved from http://hrsonline.isr.umich.edu/modules/meta/rand/randhrsm/randhrsM.pdf [Google Scholar]
- Christensen K. McGue M. Petersen I. Jeune B., & Vaupel J. W (2008). Exceptional longevity does not result in excessive levels of disability. Proceedings of the National Academy of Sciences USA, 105, 13274–13279. doi:10.1073/pnas.0804931105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., & Smith J (2011). Aging in a cultural context: Cross-national differences in disability and the moderating role of personal control among older adults in the United States and England. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, 457–467. doi:10.1093/geronb/gbr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson W. Lee C., & von Schrader S (2012). 2011 Disability status report: United States. Ithaca, NY: Cornell University Employment and Disability Institute. [Google Scholar]
- Federman A. D. Penrod J. D. Livote E. Hébert P. Keyhani S. Doucette J., & Siu A. L (2010). Development of and recovery from difficulty with activities of daily living: An analysis of national data. Journal of Aging and Health, 22, 1081–1098. doi:10.1177/0898264310375986 [DOI] [PubMed] [Google Scholar]
- Ferrucci L., Guralnik J. M., Simonsick E., Salive M. E., Corti C., Langlois J. (1996). Progressive versus catastrophic disability: A longitudinal view of the disablement process. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 51, M123–M130. doi:10.1093/gerona/51A.3.M123 [DOI] [PubMed] [Google Scholar]
- Fried L. P. Kronmal R. A. Newman A. B. Bild D. E. Mittelmark M. B. Polak J. F., … Gardin J. M (1998). Risk factors for 5-year mortality in older adults. The Cardiovascular Health Study. Journal of the American Medical Association, 279, 585–592. doi:10.1001/jama.279.8.585 [DOI] [PubMed] [Google Scholar]
- Garatachea N. (2013). Genes, physical fitness and ageing. Ageing Research Reviews, 12, 90–102. doi:10.1016/j.arr.2012.09.003 [DOI] [PubMed] [Google Scholar]
- Gill T. M. Gahbauer E. A. Han L., & Allore H. G (2010). Trajectories of disability in the last year of life. New England Journal of Medicine, 362, 1173–1180. doi:10.1056/NEJMoa0909087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy S. E. Allore H. G. Guo Z. C., & Gill T. M (2008). Explaining the effect of gender on functional transitions in older persons. Gerontology, 54, 79–86. doi:10.1159/000115004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W. L., & Larsen L. M (2014). Older Americans with a disability, 2008–2012 (American Community Survey Reports No. ACS-29). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Health and Retirement Study (2011). Sampling weights revised for Tracker 2.0 and beyond. Ann Arbor, MI: Institute for Social Research, University of Michigan; Retrieved from http://hrsonline.isr.umich.edu/sitedocs/wghtdoc.pdf [Google Scholar]
- Higgins T. J. Janelle C. M., & Manini T. M (2014). Diving below the surface of progressive disability: Considering compensatory strategies as evidence of sub-clinical disability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69, 263–274. doi:10.1093/geronb/gbt110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna F. J. Ram N., & Gerstorf D (2013). Level and change in perceived control predict 19-Year mortality: Findings from the Americans’ Changing Lives Study. Developmental Psychology, 49, 1833–1847. doi:10.1037/a0031041 [DOI] [PubMed] [Google Scholar]
- Jacobsen L. A. Kent M. Lee M., & Mather M (2011). America’s aging population. Population Bulletin, 66, 2–16. [Google Scholar]
- Keyfitz N., & Caswell H (2005). Heterogeneity and selection in population analysis. In Keyfitz N., Caswell H. (Eds.), Applied mathematical demography (3rd ed, pp. 477–493). New York, NY: Springer. [Google Scholar]
- Leveille S. G., Penninx B. W., Melzer D., Izmirlian G., Guralnik J. M. (2000). Sex differences in the prevalence of mobility disability in old age: The dynamics of incidence, recovery, and mortality. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 55, S41–S50. doi:10.1093/geronb/55.1.S41 [DOI] [PubMed] [Google Scholar]
- Mendes de Leon C. F. Seeman T. E. Baker D. I. Richardson E. D., & Tinetti M. E (1996). Self-efficacy, physical decline, and change in functioning in community-living elders: A prospective study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51, S183–S190. doi:10.1093/geronb/51B.4.S183 [DOI] [PubMed] [Google Scholar]
- Montesanto A. Dato S. Bellizzi D. Rose G., & Passarino G (2012). Epidemiological, genetic and epigenetic aspects of the research on healthy ageing and longevity. Immunity & Ageing, 9, 1–12. doi:10.1186/1742-4933-9-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolova R. Demers L. Beland F., & Giroux F (2011). Transitions in the functional status of disabled community-living older adults over a 3-year follow-up period. Archives of Gerontology and Geriatrics, 52, 12–17. doi:10.1016/j.archger.2009.11.003 [DOI] [PubMed] [Google Scholar]
- Nybo H. Petersen H. C. Gaist D. Jeune B. Andersen K. McGue M. … Christensen K (2003). Predictors of mortality in 2,249 nonagenarians—The Danish 1905-Cohort Survey. Journal of the American Geriatrics Society, 51, 1365–1373. doi:10.1046/j.1532-5415.2003.51453.x [DOI] [PubMed] [Google Scholar]
- Onder G., Penninx B. W., Ferrucci L., Fried L. P., Guralnik J. M., Pahor M. (2005). Measures of physical performance and risk for progressive and catastrophic disability: Results from the Women’s Health and Aging Study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 60, 74–79. doi:10.1093/gerona/60.1.74 [DOI] [PubMed] [Google Scholar]
- Read J. G., & Gorman B. K (2011). Gender and health revisited. In Pescosolido B. A. Martin J. K. McLeod J. D., & Rogers A. (Eds.), Handbook of the sociology of health, illness, and healing: A blueprint for the 21st century (pp. 411–429). New York, NY: Springer. [Google Scholar]
- Redfoot D. L., & Houser A (2010). More older people with disabilities living in the community: Trends from the National Long-Term Care Survey, 1984–2004. Washington, DC: AARP Public Policy Institute; Retrieved from http://assets.aarp.org/rgcenter/ppi/ltc/2010-08-disability.pdf [Google Scholar]
- Riffe T. Chung P. H. Spijker J., & MacInnes J (2015). Time-to-death patterns in marker of age and dependency (MPIDR Working Paper WP 2015-003). Rostock, Germany: Max Planck Institute for Demographic Research; Retrieved from http://www.demogr.mpg.de [Google Scholar]
- Rockwood K. Howlett S. E. MacKnight C. Beattie B. L. Bergman H. Hébert R. … McDowell I (2004). Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: Report from the Canadian Study of Health and Aging. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 59, 1310–1317. doi:10.1093/gerona/59.12.1310 [DOI] [PubMed] [Google Scholar]
- Ruiz J. R. Fiuza-Luces C. Buxens A. Cano-Nieto A. Gomez-Gallego F. Santiago C., … Lucia A (2012). Are centenarians genetically predisposed to lower disease risk? Age, 34, 1269–1283. doi:10.1007/s11357-011-9296-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamliyan T. Talley K. M. C. Ramakrishnan R., & Kane R. L (2013). Association of frailty with survival: A systematic literature review. Ageing Research Reviews, 12, 719–736. doi:10.1016/j.arr.2012.03.001 [DOI] [PubMed] [Google Scholar]
- Simons L. A., McCallum J., Friedlander Y., Simons J. (1996). Predictors of mortality in the prospective Dubbo study of Australian elderly. Australian and New Zealand Journal of Medicine, 26, 40–48. doi:10.1111/j.1445-5994.1996.tb02905.x [DOI] [PubMed] [Google Scholar]
- Smith A. K. Walter L. C. Miao Y. H. Boscardin W. J., & Covinsky K. E (2013). Disability during the last two years of life. Journal of the American Medical Association, Internal Medicine, 173, 1506–1513. doi:10.1001/jamainternmed.2013.8738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldo B. J., Hurd M. D., Rodgers W. L., Wallace R. B. (1997). Asset and Health Dynamics Among the Oldest Old: An overview of the AHEAD Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 52, 1–20. doi:10.1093/geronb/52B.Special_Issue.1 [DOI] [PubMed] [Google Scholar]
- Song X., MacKnight C., Latta R., Mitnitski A. B., Rockwood K. (2007). Frailty and survival of rural and urban seniors: Results from the Canadian Study of Health and Aging. Aging Clinical and Experimental Research, 19, 145–153. doi:10.1007/BF03324681 [DOI] [PubMed] [Google Scholar]
- StataCorp (2013). Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. [Google Scholar]
- Tiainen K. Luukkaala T. Hervonen A., & Jylha M (2013). Predictors of mortality in men and women aged 90 and older: A nine-year follow-up study in the Vitality 90+ Study. Age and Ageing, 42, 468–475. doi:10.1093/ageing/aft030 [DOI] [PubMed] [Google Scholar]
- van Houwelingen A. H. Cameron I. D. Gussekloo J. Putter H. Kurrle S. de Craen A. J. M., … Blom J. W (2014). Disability transitions in the oldest old in the general population. The Leiden 85-Plus Study. Age, 36, 483–493. doi:10.1007/s11357-013-9574-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaupel J. W., Manton K. G., Stallard E. (1979). The impact of heterogeneity in individual frailty on the dynamics of mortality. Demography, 16, 439–454. doi:10.2307/2061224 [PubMed] [Google Scholar]
- Vaupel J. W., Yashin A. I. (1985). Heterogeneity’s ruses: Some surprising effects of selection on population dynamics. The American Statistician, 39, 176–185. doi:10.1080/00031305.1985.10479424 [PubMed] [Google Scholar]
- Verbrugge L. M. (1985). Gender and health: An update on hypotheses and evidence. Journal of Health and Social Behavior, 26, 156–182. doi:10.2307/2136750 [PubMed] [Google Scholar]
- Verbrugge L. M., Jette A. M. (1994). The disablement process. Social Science & Medicine (1982), 38, 1–14. doi:10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Wiener J. M., Tilly J. (2002). Population ageing in the United States of America: Implications for public programmes. International Journal of Epidemiology, 31, 776–781. doi:10.1093/ije/31.4.776 [DOI] [PubMed] [Google Scholar]
- Wolf D. A. Freedman V. A. Ondrich J. I. Seplaki C. L., & Spillman B. C (2015). Disability trajectories at the end of life: A ‘countdown’ model. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 745–752. doi:10.1093/geronb/bgu182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., & Burgard S. A (2013). Healthier, wealthier, and wiser: A demonstration of compositional changes in aging cohorts due to selective mortality. Population Research and Policy Review, 32, 311–324. doi:10.1007/s11113-013-9273-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.