Abstract
Objectives:
To examine the relationship between loneliness and cognitive function and to explore the mediating role of physical health on the loneliness–cognition relationship in Chinese older adults (OAs).
Method:
Data came from a nationally representative sample of 14,199 Chinese OAs (aged 65+) from 2002, 2005, 2008, and 2011 waves of the Chinese Longitudinal Healthy Longevity Survey. A latent variable cross-lagged panel model combined with mediation analysis was used to determine the relationship between loneliness and cognitive function and the mediating effect of increase in the number of chronic conditions (ΔNCCs) on the ascertained loneliness–cognition relationship.
Results:
Severe loneliness at prior assessment points was significantly associated with poorer cognitive function at subsequent assessments, and vice versa. The ΔNCCs partially mediated this prospective reciprocal relationships, accounting for 2.58% of the total effect of loneliness on cognition and 4.44% of the total effect of cognition on loneliness, respectively.
Discussion:
Loneliness may predict subsequent cognitive decline, and vice versa. This loneliness–cognition relationship is partially explained by their impact on physical health. Multidisciplinary interventions aimed at reducing loneliness and cognitive decline per se and their associated risk factors as well as improving chronic illness management would be beneficial for emotional well-being and cognitive health in OAs.
Key Words: Chronic condition, Cognitive function, Cross-lagged panel analysis, Loneliness, Mediation, Older adults
Background
China is a rapidly changing society that in recent decades has seen large increases in the older adult (OA) population; high population mobility, with internal migration of younger and middle-aged people from rural to urban areas; decreased family size; and changes in traditional values of filial piety. Community bonds have weakened, and social interactions have become less routine, resulting in increasing rates of loneliness among Chinese OAs (P. Cheng et al., 2015; Luo & Waite, 2014; Yan, Yang, Wang, Zhao, & Yu, 2014). Loneliness is “the unpleasant experience that occurs when a person’s network of social relations is deficient in some important way, either quantitatively or qualitatively” (Perlman & Peplau, 1981) and has been identified as a major risk factor for a number of serious physical and mental health outcomes. In Western countries, prospective studies have demonstrated that, in middle-aged and older adults, feelings of loneliness are associated with increased mortality (Luo, Hawkley, Waite, & Cacioppo, 2012), an increase in systolic blood pressure (Hawkley, Thisted, Masi, & Cacioppo, 2010), reduced physical activity (Hawkley, Thisted, & Cacioppo, 2009), daytime dysfunction (Hawkley, Preacher, & Cacioppo, 2010), and depression (Cacioppo, Hawkley, & Thisted, 2010). To understand the nature of the negative effects of loneliness, studies are also warranted from non-Western settings such as China, where findings may not be applicable due to differences in social and cultural contexts (Yan et al., 2014). Nevertheless, the health consequences of loneliness in Chinese OAs have received very little research attention (S. Chen, Conwell, & Chiu, 2014; Y. Chen, Hicks, & While, 2014; Luo & Waite, 2014).
Loneliness also adversely affects cognitive function and increases the risk of developing late-life dementia, although all current available explanations for the loneliness–cognition association are tentative (Boss, Kang, & Branson, 2015; Zhong, Chen, & Conwell, in press). At the cognitive level, experimental studies have suggested that social isolation impairs reversal learning in rats and perceived isolation diminishes executive function in humans by causing chronic activation of implicit hypervigilance for social threat (Cacioppo & Hawkley, 2009). Another plausible cognitive mechanism is that loneliness might lead to a lack of engagement in sensory and cognitively stimulating activities (e.g., playing games, visiting museums, and leisure activities; Luo & Waite, 2014), thereby making lonely individuals less able to compensate for age-related neuropathology (i.e., decreasing neural reserve). At the biological level, loneliness may cause chronic inflammation, impair immune function, and trigger prolonged activation of the hypothalamic–pituitary–adrenal (HPA) axis, which in turn result in reductions of dendritic arborization in the hippocampus and prefrontal cortex and the synthesis of brain-derived neurotrophic factor, leading to neurodegeneration changes associated with dementia (Cacioppo & Hawkley, 2009).
Loneliness may also influence cognition through other mechanisms. The role of chronic physical conditions, such as cardiovascular and metabolic diseases and infectious illnesses, as well as unhealthy behaviors, on the risk of cognitive impairment and dementia has been partially clarified (Yaffe, 2013). For example, hypertension and diabetes mellitus could affect cognition by causing atherosclerotic small vessel disease, leading to increases in cerebral amyloid plaques, neurofibrillary tangles, and microinfarcts, the most common pathological correlates of late-life dementia (Attems & Jellinger, 2014; G. Cheng, Huang, Deng, & Wang, 2012; Faraco & Iadecola, 2013; Pregelj, 2008; Sharp et al., 2011). Moreover, infectious burden, a measure of past exposure to common pathogens, has been associated with an increased risk of cognitive impairment via the mechanisms of inflammation and neuronal toxicity (Katan et al., 2013). On the other hand, loneliness has been linked to elevated systolic blood pressure through increased vascular resistance (Hawkley et al., 2010), metabolic syndrome through unhealthy behaviors (e.g., physical inactivity, smoking, and sleep problems; Kurina et al., 2011; Luo & Waite, 2014; Whisman, 2010), and susceptibility to various illnesses via altered immune function and HPA functioning (Cole et al., 2015; Meaney, Szyf, & Seckl, 2007). Given that physical health problems, either communicable or noncommunicable, are proximal risk factors for cognitive impairment, physical health consequences of loneliness may represent a main potential bridge between loneliness and cognitive decline.
Because cognitively impaired individuals may have difficulties in maintaining friendships, communicating with others, and participating in social and leisure activities (Brown, Devanand, Liu, Caccappolo, & Alzheimer’s Disease Neuroimaging Initiative, 2011), loneliness could also be regarded as a consequence of diminished cognition. Given that some specific cognitive domains (i.e., executive function, verbal fluency, and memory) were significantly correlated with loneliness (O’Luanaigh et al., 2012; Schnittger, Wherton, Prendergast, & Lawlor, 2012), it is more likely that loneliness and cognition have mutual effects on each other. Other indirect evidence includes the bidirectional relationships between cognitive function and depression (Yoon & Brown, 2014), and depression and loneliness (Luo et al., 2012), suggesting that cognition and loneliness may be linked by the mediator: depression. In addition, because cognitive impairment may result in difficulties in decision making for effective self-management of diseases and keeping healthy lifestyles (Mann, de Ridder, & Fujita, 2013; Yaffe, 2013), physical health can be exacerbated by impaired cognition via increasing the severity or incidence of physical conditions. Physical disabilities due to worsened health would further limit individuals’ ability to take part in social activities and in turn cause loneliness. Therefore, physical health may also mediate the bidirectional loneliness–cognition pathways. However, compared with the increasing number of studies on the simple one-way loneliness–cognition association, very few studies have explored their reciprocal relationship and mechanisms underlying such relationships. Supplementary Figure S1 summarizes the possible links between loneliness and cognition.
Dementia is among the most important contributors to disease burden in Chinese OAs (Yang et al., 2013), but its etiology remains only partially understood. Disentangling the complex relationship between loneliness and cognitive decline may help illuminate the processes involved in the pathogenesis of mental ill-being and cognitive impairment, potentially leading the way for effective preventive or therapeutic interventions. This study first examines the reciprocal relationship between loneliness and cognitive function using a national longitudinal survey of OAs in China. Then, given the potential important role of physical health in the pathogenesis of cognitive impairment, we further explore the mediating role of physical health on this relationship.
Method
Data and sample
Data were collected from the Chinese Longitudinal Health Longevity Study (CLHLS), a dynamic cohort study with first-wave data collected in 1998 and five follow-up surveys with replacement of deceased elders in 2000, 2002, 2005, 2008, and 2011. The CLHLS recruited a representative sample of Chinese OAs from about half of the counties and cities in 22 of the 31 provinces in China. The survey areas covered 1.16 billion people, accounting for 85% of the total population in China. In-person interviews were conducted by research assessors to obtain data on demographic characteristics, socioeconomic status, lifestyle, and health. More details about the study design, sampling, measures, and data quality of the CLHLS are available elsewhere (Zeng, Poston, Ashbaugh Vlosky, & Gu, 2008).
The current study used CLHLS’s last four waves of data from 2002 (hereafter referred to as “baseline” for this study) to 2011, each conducted at 3-year intervals. Our study focused on the 2002 cohort, excluding participants who were added to replace those who were deceased in the subsequent waves. At baseline, the cohort had 16,064 participants. Those whose self-reported ages were 106 or older were excluded due to lack of reliable information to verify their advanced age (Zeng et al., 2008). We further excluded respondents aged 60 to 64 and those who had missing values on baseline scores of loneliness and the modified Mini-Mental State Examination (mMMSE); the final sample for analyses, therefore, consisted of 14,199 respondents. Supplementary Figure S2 depicts the flow chart of study sample inclusion and follow-up.
Measures
Loneliness
A single question asking how often the interviewee feels lonely was administered to assess participants’ subjective feeling of loneliness. Response options for this item were 1 = never, 2 = seldom, 3 = sometimes, 4 = often, and 5 = always. A single-item self-report measure of loneliness has been widely used in previous studies and has been shown to be highly correlated with multi-item loneliness scales (Pinquart & Sorensen, 2001). Furthermore, a single item is preferable to reduce subjects’ response burden, particularly for the oldest old with decreased cognitive abilities.
Cognitive function
The cognitive function was assessed with a Chinese mMMSE. The original MMSE has 30 items and tests 7 domains of cognitive function (Folstein, Folstein, & McHugh, 1975). Considering that two thirds of Chinese OAs are illiterate, the CLHLS deleted 2 items of language (write a complete sentence and follow a written instruction to close eyes) from the original version. To make questions easily understandable and practically answerable by OAs, it further deleted 1 item of orientation to time and 4 items of orientation to place and culturally adapted the remaining 23 items (Lagona & Zhang, 2010). Each item of the Chinese mMMSE is scored 1 if the answer is correct and 0 for incorrect answer or “unable to answer,” so higher scores indicate better cognition. Our factor analyses revealed that a model with one single second-order factor and four first-order factors consistently fitted the four waves’ mMMSE data well. The four first-order factors were orientation (orientation to time and place), memory (registration and delayed recall), attention and calculation (calculation and copying intersecting polygons), and language (repeating phrase, three-step command, and naming), and the second-order construct represented cognition. Cronbach’s α coefficients of the mMMSE ranged from 0.88 to 0.91 for the four waves of the CLHLS.
Increase in number of chronic conditions (ΔNCCs)
At each wave, the CLHLS administered a chronic illness checklist asking the respondent to report whether he/she has a specific condition. Data were collected on 14 specific physical illnesses (e.g., hypertension, diabetes, heart disease, stroke and other cerebrovascular diseases, cancer, and arthritis) and dementia at each time point. After excluding dementia, the sum of NCCs, ranging from 0 to 14, was operationalized as an objective measure of physical health, with greater number indicating poorer physical health. The ΔNCCs was calculated as the count of conditions recorded at a later time point minus that recorded at a preceding time point. The accuracy of self-reported physical illness diagnosis by CLHLS respondents and/or their next of kin has been shown to be good (Zeng et al., 2008).
Control variables
To minimize the possibility that loneliness–cognition relationship is due to a third variable and to maximize the parsimony of our analytic model, only a limited number of covariates that were known to be associated with loneliness and cognition were controlled in our analysis. Age, gender, and education (0 = no schooling [0 year of education]; 1 = some schooling [≥1 year of education]) were included as basic demographic control variables. In addition, educational attainment was also regarded as a proxy measure of socioeconomic status, because this measure has at least two advantages when studying health and socioeconomic status (Montez, Hummer, & Hayward, 2012). First, education can be determined for all individuals, whereas not everyone has an income or an occupation. This is particularly important for OAs who have been retired. Second, a person’s education is most often unaffected by health impairment that emerged after age 25, whereas one’s income and occupation are, at least in part, affected by health problems.
Physical exercise and current smoking were included as lifestyle covariates. Subjects were asked whether they regularly participate in physical exercise (1 = yes; 2 = no) and whether they currently smoke (1 = yes; 2 = no). Social activity was assessed by a single question: “Do you take part in some social activities at present?” (1 = almost every day; 2 = not daily, but once for a week; 3 = not weekly, but at least once for a month; 4 = not monthly, but sometimes; 5 = never). Objective measures of social isolation included two variables: marital status (1 = never married, separated, divorced, or widowed; 0 = married) and living arrangement (1 = alone; 0 = with family members or in an institution).
Analytic strategies
Because measurement error in manifest variables can be addressed using latent variables with multiple indicators, the latent variable cross-lagged panel analysis (CLPA) was adopted to examine the direction and strength of association between loneliness and cognition (Kim, Noh, Park, & Kwon, 2014). Three domain-representative item parcels were created as the indicators of cognition (Coffman & MacCallum, 2005). We randomly selected 2 items from each mMMSE domain and summed the 8 items to create the first parcel. Using the same procedure, another 8 items were used to create the second parcel. The remaining 7 items were finally summed into the third parcel.
To correct for the effect of unreliability in loneliness scale scores, we created a single-indicator latent variable to represent the construct of loneliness at each wave, which was measured by its corresponding score and the residual variance of the scale score fixed to (1—Scale Reliability) × Scale Variance (Schumacker & Lomax, 2004). By applying the Stable Trait, Autoregressive Trait, State Model (Lucas & Donnellan, 2012) to the four-wave loneliness scores, we decomposed the total variance into three parts: stable trait, autoregressive trait, and state. A reliability of 0.595 was obtained by computing the ratio of the sum of the stable and autoregressive trait variance to total variance.
Longitudinal measurement invariance of cognition across measurement occasions is a prerequisite to modeling changes over time (Wang, Elhai, Dai, & Yao, 2012). Confirmatory factor analysis using measurement invariance testing found that our proposed construct of cognition was invariant over time on these parcels’ loadings and intercepts and thus satisfied the requirements for strong measurement invariance. The scalar invariance model of cognition allowed correlations between residual error variances of the same parcel and imposed invariance constraints on the factor loadings and intercepts across the four time points.
Our CLPA mainly involved the comparison of four nested models (Supplementary Table 1). The latent loneliness variables were added to the scalar invariance model of cognition to construct Model 1, which contained eight latent variables (i.e., cognition and loneliness at ~2002–2011), six autoregressive paths between two consecutive time points and four correlations within time points. Model 2 evaluated the stability in autoregressive paths of loneliness and cognition. Model 3 added cross-lagged paths of loneliness and cognition and tested the reciprocal relationships between them. Model 4 tested “stationarity” in cross-lagged paths. Nested models were compared with the corrected scaled χ2 difference test (Satorra & Bentler, 2001).
In temporal ordering, ΔNCCs was an intervening variable between time [t−3] (“t−3” represents “3 years earlier”) and time [t], thus ΔNCCs was hypothesized to medicate the reciprocal loneliness–cognition relationship ascertained in Model 4. The two indirect effects, [t−3] loneliness on [t] cognition via ΔNCCs and [t−3] cognition on [t] loneliness via ΔNCCs, were simultaneously tested in Model 5. The indirect effect of X predicting Y via M was the product of two direct effects in the path.
On the basis of Models 4 and 5, Models 4i and 5i included all control variables as covariates predicting ~2002–2011 loneliness and cognition, respectively. In this final analysis, gender and education were treated as time-invariant variables, whereas all other covariates were time-varying variables. Paths from covariates to loneliness/cognition, correlations between variables at a given time, autoregressive paths of time-varying variables, and cross-lagged paths between time-varying variables were also added to Models 4i and 5i. Because CLPA routinely assumes that prospective relationships between variables are stable over time (Cacioppo et al., 2010), we applied equality constraints to the autoregressive and cross-lagged paths as well as paths from time-invariant covariates to loneliness/cognition. However, autoregressive coefficients in Model 2 were still allowed to be freely estimated, because we considered that the rate of cognitive decline over time was a gradually accelerating process, and these autoregressive paths cannot be stable during the 9-year follow-up period. Comparison results from the corrected scaled χ2 difference test for Models 1 and 2 also rejected the stability hypothesis in autoregressive paths (ΔS−B χ2 = 40.39, p < 0.001).
We did not impute the missing data; rather, available data of all the 14,199 respondents were used in this study. Full Information Maximum Likelihood (FIML) estimation was used to deal with missing data (Muthén & Muthén, 1998–2012).The highest absolute values of skewness and kurtosis for our observed variables were 1.402 (Parcel 3 in 2002) and 1.389 (Parcel 1 in 2008), therefore, the parameters were estimated with Robust Maximum Likelihood. We reported unstandardized regression coefficients (βs) and p values throughout.
The degree of model fit was assessed with Satorra–Bentler χ2 statistic (S−B χ2), root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker–Lewis index (TLI), however, we primarily depended on the results of RMSEA, CFI and TLI, because χ2 goodness-of-fit statistic is too sensitive for a very large sample such as is used in our study (Wang & Wang, 2012). An RMSEA value under 0.05 represents a good fit to the data, and values between 0.05 and 0.08 indicate reasonable fit. For the CFI/TLI, values greater than 0.90 are considered as an acceptable fit and 0.95 or more as a good fit (Hu & Bentler, 1999). All these analyses were conducted with Mplus, version 6.
Results
Descriptive statistics
Sample characteristics are shown in Table 1. At baseline, 67.0% of OAs “never” or “seldom” felt lonely, whereas 24.8% “sometimes” and 8.3% “often” or “always” felt lonely. Among the 2,456 survivors who were interviewed at each wave, the results of repeated-measures analysis of variance indicated that loneliness increased over time between 2002 and 2011 (F = 3.214, p = .022), whereas mean mMMSE scores decreased (F = 238.238, p < .001). The mean scores of the baseline cohort estimated using Mplus from 2002 to 2011 were 2.07, 2.14, 2.21, and 2.25 for loneliness,and 18.17, 16.42, 15.39, and 14.62 for mMMSE, respectively.
Table 1.
Descriptive Statistics
| Variables | 2002 (N = 14,199) | 2005 (N = 7,722) | 2008 (N = 4,055) | 2011 (N = 2,456) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (%) | SD | Mean (%) | SD | Mean (%) | SD | Mean (%) | SD | |
| Age (65–105 years) | 85.00 | 11.32 | 84.11 | 10.54 | 83.36 | 9.01 | 83.88 | 7.67 |
| Male | 44.26 | 46.11 | 47.03 | 47.37 | ||||
| No schooling | 60.10 | 56.59 | 54.43 | 53.16 | ||||
| Married | 33.95 | 37.05 | 38.50 | 39.78 | ||||
| Living alone | 13.91 | 13.80 | 16.20 | 15.90 | ||||
| Current smoker | 19.33 | 20.30 | 18.69 | 19.69 | ||||
| Regular physical exercise | 33.77 | 33.84 | 33.13 | 40.44 | ||||
| Frequency of social activity (1–5) | 4.70 | 0.83 | 4.66 | 0.90 | 4.72 | 0.83 | 4.66 | 0.90 |
| Loneliness (1–5) | 2.07 | 1.02 | 2.05 | 1.03 | 2,06 | 1.03 | 2.01 | 1.00 |
| Modified Mini-Mental State Examination (0–23) | 18.17 | 5.29 | 17.40 | 6.92 | 17.52 | 6.69 | 17.87 | 6.36 |
| Orientation domain (0–5) | 4.49 | 1.08 | 4.25 | 1.52 | 4.31 | 1.50 | 4.32 | 1.43 |
| Memory domain (0–6) | 4.47 | 1.91 | 4.42 | 2.13 | 4.37 | 2.15 | 4.42 | 2.08 |
| Attention and calculation domain (0–6) | 3.99 | 2.07 | 3.85 | 2.22 | 3.91 | 2.14 | 3.94 | 2.20 |
| Language domain (0–6) | 5.22 | 1.42 | 4.88 | 1.91 | 4.93 | 1.86 | 5.18 | 1.70 |
| Increase in number of chronic conditions | 0.10 | 1.30 | 0.10 | 1.36 | 0.21 | 1.45 | ||
Supplementary Table 2 presents the factor loadings of parcels in the measurement model of cognition, their standardized loadings ranged from 0.88 to 0.98.
Correlations between latent variables of loneliness and cognition and a manifest variable of ΔNCCs are presented in Supplementary Table 3. At any given occasion, loneliness and cognition negatively and significantly correlated (p < .001). Loneliness was negatively correlated with later cognition (p ≤ .023) and cognition was negatively correlated with later loneliness (p ≤ .031). The ΔNCCs was positively correlated with loneliness and negatively correlated with cognition two both at a prior occasion and the same occasion (p ≤ .046).
Reciprocal Relationship Between Loneliness and Cognitive Function
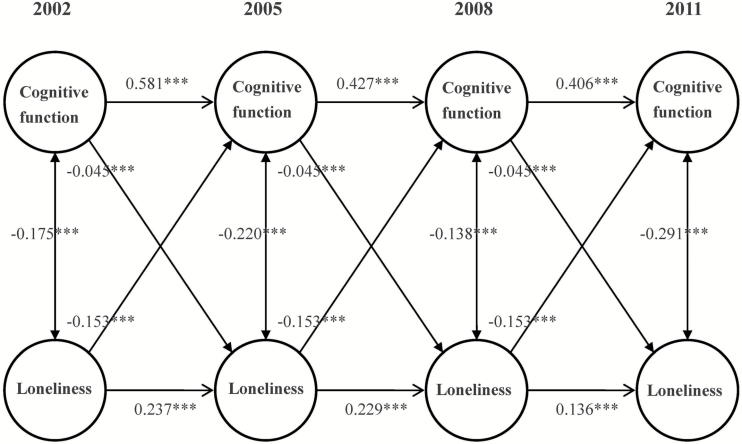
Figure 1 depicts Model 4i. After controlling for covariates, Model 4i fitted the data adequately (RMSEA = 0 .034, CFI = 0.949, TLI = 0.940; Supplementary Table 1), and the 3-year cross-lagged effects of prior loneliness on cognition (β = 0.153, p < .001) and cognition on subsequent loneliness (β = −0.045, p < .001−) were significant. In this final model, the 3-year lagged effect of social activity on cognition was significant (β = −0.12, p < .001), but its influence on loneliness was not significant (β = 0.006, p = .561). Independent of loneliness and other covariates, the cross-lagged effects of marital status and living arrangement on cognition (β = −0.30, p < .001; β = −0.16, p < .001) and loneliness (β = 0.34, p < 0.001; β = 0.37, p < 0.001) remained significant. With regard to other covariates, we found education was positively associated with cognition (β = 0.413, p < 0.001) and negatively associated with loneliness (β = −0.105, p < 0.001). We also found physical exercise predicted relative increases in cognition (β = 0.168, p < 0.001) and decreases in loneliness (β = −0.072, p < 0.001).
Figure 1.
Latent variable cross-lagged panel model of reciprocal relationship between loneliness and cognitive function. Parcels of cognitive function, overtime correlations between parcel-specific residuals, fixed residual variances of loneliness, and control variables are not shown to enhance clarity. Unstandardized regression coefficients are presented. ***p < .001.
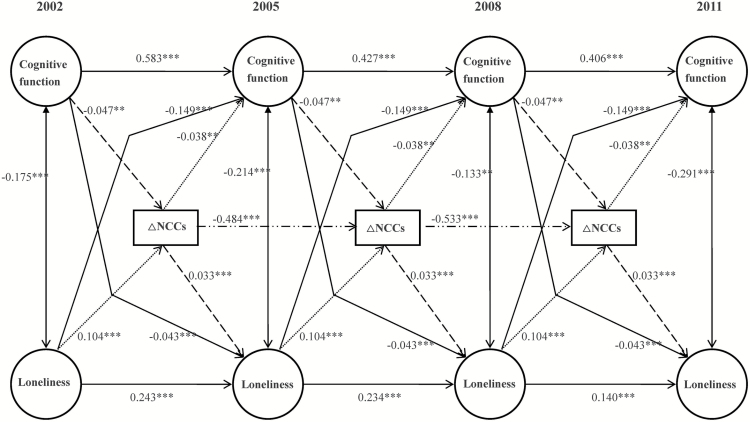
Mediating Effect of ΔNCCs
As Figure 2 presents, after adding two indirect paths that shared ΔNCCs as a potential mediator and adjustment for control variables, Model 5i still had a good fit to the data (RMSEA = 0.031, CFI = 0.949, TLI = 0.940; Supplementary Table 1), and the 3-year cross-lagged effects of loneliness on subsequent cognition (β = −0.149, p < .001) and prior cognition on subsequent loneliness (β = −0.043, p < .001) were significant but slightly reduced in size compared with those in Model 4i. The indirect effects of prior loneliness on cognition via ΔNCCs, as well as prior cognition on loneliness via ΔNCCs, were significant across the three time intervals (effect size = −0.004 and −0.002, −0.001), however, on average, the two indirect effects only accounted for 2.58% and 4.44% of their respective total effects demonstrated in Model 4i.
Figure 2.
Mediating effect of increase in the number of chronic conditions (ΔNCCs) on reciprocal relationship between loneliness and cognitive function. Parcels of cognitive function, overtime correlations between parcel-specific residuals, fixed residual variances of loneliness, and control variables are not shown to enhance clarity. Unstandardized regression coefficients are presented. ***p < .001 and **p < .01.
Discussion
To the best of our knowledge, this is the first large-scale 9-year cohort study in China that examined the prospective relationship between loneliness and cognition. Our findings not only add strength to the assertion that loneliness has an adverse impact on cognitive functioning, including in Chinese OAs, but also indicate that cognitive dysfunction may exacerbate loneliness, creating a “vicious cycle” that further damages cognition over time. Finally, although the indirect effects of loneliness/cognition on cognition/loneliness through ΔNCCs are small in size, their statistical significance still suggests a mechanism that loneliness and cognition mutually affect each other via their impact on physical health.
The bidirectional loneliness–cognition relationship over time remained significant after accounting for demographic, socioeconomic status, lifestyle, social activity, and objective isolation covariates, indicating that the reciprocal loneliness–cognition relationships are not explained by these variables. These findings are especially important because previous studies have shown that loneliness/cognition has significant associations with these risk factors (Y. Chen et al., 2014; Plassman, Williams, Burke, Holsinger, & Benjamin, 2010), in particular objective isolation (Wilson et al., 2007), but our analysis rules out the third-variable effects caused by these covariates. However, such results do not imply that these factors have no role in cognition and loneliness. In fact, we found actual isolation, as indicated by marital status and living arrangement, not only had a direct effect on later cognition, independent of loneliness and cognition at the same time point, but also had a significant lagged effect on loneliness at a later time point. Because the later loneliness has significant direct effect on its subsequent cognition, we may speculate that loneliness also additionally acts as a mediator that conveys the effect of isolation on cognition.
The significant direct effect of loneliness on cognition is in accordance with previous research in Western countries (Boss et al., 2015). However, the significant direct effect of cognition on loneliness is inconsistent with some previous studies reporting that discrete cognitive domains, not global cognitive function, predicted loneliness (O’Luanaigh et al., 2012; Schnittger et al., 2012) and that baseline cognition was not associated with later loneliness (Wilson et al., 2007). Besides less engagement in social activities due to diminished cognition, we also consider reduced social network size resulting from cognitive impairment as an alternative explanation for this reverse relationship (Alspach, 2013; Cacioppo, Fowler, & Christakis, 2009).
It is important to note that we only tested one possible mechanism and found that the mediating effect of physical health, although statistically significant, could only explain a very small portion of the direct effect. Consequently, we are not able to ascertain whether this reciprocal effect over time is mainly caused by loneliness and cognition per se (e.g., loneliness directly impairs cognition) by their effects on potential biological, cognitive, and clinical processes, such as worsened physical health, by a combination of these, or other mechanisms. We also are mindful that the process of reciprocal loneliness–cognition relationship might involve a “mediator chain” that includes many biological, cognitive, and clinical markers; the mediating effect of physical health identified in the present study may be only one of the many steps between loneliness and cognition. Further research is needed to address this issue.
Several limitations of this study should be noted. First, to make causal inferences in CLPA, a prerequisite is that the roles of all possible sources of spuriousness should be excluded. We had controlled a limited number of important covariates, but some unmeasured covariates, such as social support and social network size, have not been adjusted. In addition, our CLPA also violated the stability assumption in autoregressive paths, which implies that the loneliness–cognition relationship may be due to the universal life-course pattern. Therefore, in a strict sense, we should be cautious to interpret the reciprocal loneliness–cognition associations as causal relationships due to unavoidable omitted-variable bias. Second, loneliness might be underreported because this study only used a self-report question to assess loneliness. However, the item does avoid potential confounding that might arise from measures using indirect items, for example, some scales use social support to represent loneliness indirectly (Luo & Waite, 2014). In addition, we used a reliability correction technique to construct the measurement error of loneliness, but its reliability is estimated from the same sample in which our model is to be fit. This shortcoming may introduce sample dependencies limiting the generalizability of our results to other samples (Coffman & MacCallum, 2005). Third, NCCs was a crude measure of physical health in this study, because this indicator does not incorporate disease severity information. In addition, it is still possible that NCCs was underreported by the respondents due to self-report of or lack of awareness regarding their physical conditions. Considering worsened physical health’s associations with loneliness and cognitive impairment, the mediating effect of physical health might be underestimated.
In summary, 9-year cross-lagged longitudinal data from the CLHLS demonstrates in Chinese OAs that there may be a reciprocal relationship between loneliness and cognitive function, and the prospective loneliness–cognition relationship is partially mediated by physical health. Both loneliness and cognitive decline are major health challenges of contemporary Chinese OAs. Given their reciprocal relationships, multidisciplinary interventions that attempt to alleviate loneliness and maintain or delay the progression of cognitive decline, or their associated risk factors, may be helpful for the cognitive and mental health of OAs. More studies are needed to reveal the underlying pathways between loneliness and cognition. Targeting these pathways, including optimizing chronic disease management, interrupt the possible vicious cycle between loneliness and cognitive decline.
Supplementary Material
Please visit the article online at http://psychsocgerontology.oxfordjournals.org/ to view supplementary material.
Funding
This work was in part supported by the National Institutes of Health (NIH) Fogarty Center (NIH/FIC D43 TW009101; E. D. Caine, PI) and the University of Rochester Office for Aging Research and Health Services (Dr Conwell, Director)
Supplementary Material
Acknowledgments
B. L. Z. and Y. C. planned the study; B. L. Z. and Y. C. planned the study; B. L. Z. performed statistical analyses and wrote the manuscript; Y. C. contributed to revising the manuscript; and S. L. C. and X. T. provided comments to the manuscript.
References
- Alspach J. (2013). Loneliness and social isolation: Risk factors long overdue for surveillance. Critical Care Nurse, 33, 8–13. doi:10.4037/ccn2013377 [DOI] [PubMed] [Google Scholar]
- Attems J., & Jellinger K (2014). The overlap between vascular disease and Alzheimer’s disease—Lessons from pathology. BMC Medicine, 12, 206. doi:10.1186/s12916-014-0206-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boss L. Kang D., & Branson S (2015). Loneliness and cognitive function in the older adult: A systematic review. International Psychogeriatrics, 27, 541–553. doi:10.1017/s1041610214002749 [DOI] [PubMed] [Google Scholar]
- Brown P. Devanand D. Liu X. Caccappolo E., & Alzheimer’s Disease Neuroimaging Initiative. (2011). Functional impairment in elderly patients with mild cognitive impairment and mild Alzheimer disease. Archives of General Psychiatry, 68, 617–626. doi:10.1001/archgenpsychiatry.2011.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J., & Hawkley L (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13, 447–454. doi:10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J. Fowler J., & Christakis N (2009). Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of Personality and Social Psychology, 97, 977–991. doi:10.2139/ssrn.1319108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J. Hawkley L., & Thisted R (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25, 453–463. doi:10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S. Conwell Y., & Chiu H (2014). Loneliness and aging in China—A public health problem in need of solutions. International Psychogeriatrics, 26, 1771–1772. doi:10.1017/s104161021400177x [DOI] [PubMed] [Google Scholar]
- Chen Y. Hicks A., & While A (2014). Loneliness and social support of older people in China: A systematic literature review. Health & Social Care in the Community, 22, 113–123. doi:10.1111/hsc.12051 [DOI] [PubMed] [Google Scholar]
- Cheng G. Huang C. Deng H., & Wang H (2012). Diabetes as a risk factor for dementia and mild cognitive impairment: A meta-analysis of longitudinal studies. Internal Medicine Journal, 42, 484–491. doi:10.1111/j.1445-5994.2012.02758.x [DOI] [PubMed] [Google Scholar]
- Cheng P. Jin Y. Sun H. Tang Z. Zhang C. Chen Y., … Huang F (2015). Disparities in prevalence and risk indicators of loneliness between rural empty nest and non-empty nest older adults in Chizhou, China. Geriatrics & Gerontology International, 15, 356–364. doi:10.1111/ggi.12277 [DOI] [PubMed] [Google Scholar]
- Coffman D., & MacCallum R (2005). Using parcels to convert path analysis models into latent variable models. Multivariate Behavioral Research, 40, 235–259. doi:10.1207/s15327906mbr4002_4 [DOI] [PubMed] [Google Scholar]
- Cole S. Capitanio J. Chun K. Arevalo J. Ma J., & Cacioppo J (2015). Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proceedings of the National Academy of Sciences of the United States of America, 112, 15142–15147. doi:10.1073/pnas.1514249112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraco G., & Iadecola C (2013). Hypertension: A harbinger of stroke and dementia. Hypertension, 62, 810–817. doi:10.1161/hypertensionaha.113.01063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein M. Folstein S., & McHugh P (1975). “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. doi:10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Hawkley L. Preacher K., & Cacioppo J (2010). Loneliness impairs daytime functioning but not sleep duration. Health Psychology, 29, 124–129. doi:10.1037/a0018646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L. Thisted R., & Cacioppo J (2009). Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychology, 28, 354–363. doi:10.1037/a0014400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L. Thisted R. Masi C., & Cacioppo J (2010). Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging, 25, 132–141. doi:10.1037/a0017805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., & Bentler P (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. doi:10.1080/10705519909540118 [Google Scholar]
- Katan M. Moon Y. Paik M. Sacco R. Wright C., & Elkind M (2013). Infectious burden and cognitive function: The Northern Manhattan Study. Neurology, 80, 1209–1215. doi:10.1212/wnl.0b013e3182896e79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. Noh J. Park J., & Kwon Y (2014). Body mass index and depressive symptoms in older adults: A cross-lagged panel analysis. PLoS One, 9, e114891. doi:10.1371/journal.pone.0114891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurina L. Knutson K. Hawkley L. Cacioppo J. Lauderdale D., & Ober C (2011). Loneliness is associated with sleep fragmentation in a communal society. Sleep, 34, 1519–1526. doi:10.5665/sleep.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagona F., & Zhang Z (2010). A missing composite covariate in survival analysis: A case study of the Chinese Longitudinal Health and Longevity Survey. Statistics in Medicine, 29, 248–261. doi:10.1002/sim.3773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas R., & Donnellan M (2012). Estimating the reliability of single-item life satisfaction measures: Results from four national panel studies. Social Indicators Research, 105, 323–331. doi:10.1007/s11205-011-9783-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y. Hawkley L. Waite L., & Cacioppo J (2012). Loneliness, health, and mortality in old age: a national longitudinal study. Social Science & Medicine, 74, 907–914. doi:10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., & Waite L (2014). Loneliness and mortality among older adults in China. Journal of Gerontology: Social Sciences, 69, 633–645. doi:10.1093/geronb/gbu007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann T. de Ridder D., & Fujita K (2013). Self-regulation of health behavior: Social psychological approaches to goal setting and goal striving. Health Psychology, 32, 487–498. doi:10.1037/a0028533 [DOI] [PubMed] [Google Scholar]
- Meaney M. Szyf M., & Seckl J (2007). Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends in Molecular Medicine, 13, 269–277. doi:10.1016/j.molmed.2007.05.003 [DOI] [PubMed] [Google Scholar]
- Montez J. Hummer R., & Hayward M (2012). Educational attainment and adult mortality in the United States: A systematic analysis of functional form. Demography, 49, 315–336. doi:10.1007/s13524-011-0082-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., & Muthén B (1998. –2012). Mplus User’s Guide. (7th ed.). Los Angeles, CA: Author. [Google Scholar]
- O’Luanaigh C. O’Connell H. Chin A. Hamilton F. Coen R. Walsh C., … Lawlor B (2012). Loneliness and cognition in older people: The Dublin Healthy Ageing study. Aging and Ment Health, 16, 347–352. doi:10.1080/13607863.2011.628977 [DOI] [PubMed] [Google Scholar]
- Perlman D., & Peplau L (1981). Toward a social psychology of loneliness. In Gilmour R., Duck S. (Eds.), Personal relationships, volume 3: Personal relationships in disorder. London, UK: Academic Press. [Google Scholar]
- Pinquart M., & Sorensen S (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23, 245–266. doi:10.1207/s15324834basp2304_2 [Google Scholar]
- Plassman B. Williams J. Burke J. Holsinger T., & Benjamin S (2010). Systematic review: Factors associated with risk for and possible prevention of cognitive decline in later life. Annals of Internal Medicine, 153, 182–193. doi:10.7326/0003-4819-153-3-201008030-00258 [DOI] [PubMed] [Google Scholar]
- Pregelj P. (2008). Involvement of cholesterol in the pathogenesis of Alzheimer’s disease: Role of statins. Psychiatria Danubina, 20, 162–167. doi:10.1345/aph.1d104 [PubMed] [Google Scholar]
- Satorra A., & Bentler P (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66, 507–514. doi:10.2139/ssrn.199064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittger R. Wherton J. Prendergast D., & Lawlor B (2012). Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging and Mental Health, 16, 335–346. doi:10.1080/13607863.2011.629092 [DOI] [PubMed] [Google Scholar]
- Schumacker R., & Lomax R (2004). A beginner’s guide to structural equation modeling. New Jersey,NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Sharp S. Aarsland D. Day S. Sønnesyn H., Alzheimer’s Society Vascular Dementia Systematic Review Group, & Ballard C (2011). Hypertension is a potential risk factor for vascular dementia: Systematic review. International Journal of Geriatric Psychiatry, 26, 661–669. doi:10.1002/gps.2572 [DOI] [PubMed] [Google Scholar]
- Wang J., & Wang X (2012). Structural equation modeling: Applications using Mplus. New York, NY: John Wiley. [Google Scholar]
- Wang M. Elhai J. Dai X., & Yao S (2012). Longitudinal invariance of posttraumatic stress disorder symptoms in adolescent earthquake survivors. Journal of Anxiety Disorders, 26, 263–270. doi:10.1016/j.janxdis.2011.12.009 [DOI] [PubMed] [Google Scholar]
- Whisman M. (2010). Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychology, 29, 550–554. doi:10.1037/a0020760 [DOI] [PubMed] [Google Scholar]
- Wilson R. Krueger K. Arnold S. Schneider J. Kelly J. Barnes L., … Bennett D (2007). Loneliness and risk of Alzheimer disease. Archives of General Psychiatry, 64, 234–240. doi:10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- Yaffe K. (2013). Chronic medical disease and cognitive aging: Toward a healthy body and brain. New York, NY: Oxford University Press. [Google Scholar]
- Yan Z. Yang X. Wang L. Zhao Y., & Yu L (2014). Social change and birth cohort increase in loneliness among Chinese older adults: A cross-temporal meta-analysis, 1995–2011. International Psychogeriatrics, 26, 1773–1781. doi:10.1017/s1041610214000921 [DOI] [PubMed] [Google Scholar]
- Yang G. Wang Y. Zeng Y. Gao G. Liang X. Zhou M., … Murray C (2013). Rapid health transition in China, 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet, 381, 1987–2015. doi:10.1016/s0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon J., & Brown R (2014). Causal inference in cross-lagged panel analysis: A reciprocal causal relationship between cognitive function and depressive symptoms. Research in Gerontological Nursing, 7, 152–158. doi:10.3928/19404921-20140310-01 [DOI] [PubMed] [Google Scholar]
- Zeng Y. Poston D. Ashbaugh Vlosky D., & Gu D (2008). Healthy longevity in China: Demographic, socioeconomic, and psychological dimensions. Dordrecht, The Netherlands: Springer Science & Business Media. [Google Scholar]
- Zhong B., Chen S., Conwell Y. (in press). Effects of transient versus chronic loneliness on cognitive function in older adults: Findings from the Chinese Longitudinal Healthy Longevity Survey. American Journal of Geriatric Psychiatry. Advance online publication. doi:10.1016/j.jagp.2015.12.009 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.