Abstract
Background
Fatigue is a prevalent and functionally disabling symptom for individuals living with multiple sclerosis (MS) which is poorly understood and multifactorial in etiology. Bladder dysfunction is another common MS symptom which limits social engagement and quality of life. To manage bladder issues, individuals with MS tend to limit their fluid intake, which may contribute to a low-hydration (LoH) state and fatigue.
Objective
To evaluate the relationship between patient-reported MS fatigue, bladder dysfunction, and hydration status.
Methods
We performed a prospective cross-sectional study in 50 women with MS. Participants submitted a random urine sample and completed several fatigue-related surveys. Using a urine specific gravity (USG) threshold of 1.015, we classified MS subjects into two groups: high-hydration (HiH) and LoH states.
Results
LoH status was more common in MS subjects with bladder dysfunction. Statistically significant differences in self-reported Fatigue Performance Scale were observed between HiH and LoH subjects (p = 0.022). USG was significantly correlated with fatigue as measured by the MS Fatigue Severity Scale (FSS) score (r = 0.328, p = 0.020).
Conclusion
Hydration status correlates with self-reported fatigue, with lower fatigue scores found in those with HiH status (USG < 1.015).
Keywords: Multiple sclerosis, fatigue, dehydration, lifestyle, bladder control scale, modified fatigue impact scale, fatigue severity scale
Introduction
Multiple sclerosis (MS) is an inflammatory disease of the central nervous system (CNS) which results in neurologically diverse and debilitating symptoms. One of the most commonly reported yet elusive MS symptoms is fatigue, often defined as a sense of exhaustion, lack of energy, or tiredness.1 Fatigue is a multifactorial and primarily subjective symptom, often making it difficult to properly identify and treat. Researchers have identified multiple factors associated with or contributing to fatigue, including sleep disturbances, higher levels of cytokines, depression, pain, and overall baseline disability.2,3 Researchers and clinicians have tried to discern between “primary” MS fatigue and “secondary” fatigue (e.g. due to nocturnal awakenings and medications). Primary MS-related fatigue has been characterized as occurring later in the day, worsened by heat and exertion, and often variable from day to day.1,4,5
Bladder dysfunction is another common problem for individuals living with MS, often associated with urinary incontinence. Incontinence is usually secondary to a spastic bladder with increased sense of urgency and subsequent accidents, particularly in those who are less mobile and unable to reach a toilet facility with ease.6 To prevent embarrassment from accidents and avoid repeated bathroom trips, our clinical experience suggests that MS patients often self-restrict their fluid intake and thus exist in a chronic low or dehydrated state.
In 2012, a study of healthy young women in hydrated and dehydrated states found that several symptoms, including vigor, fatigue, perception of task difficulty, concentration, and headache, were adversely affected by small changes in hydration.7 It thus stands to reason that a similar effect could be found in MS, where hydration state would be impacted by regular restriction in fluid intake due to bladder concerns. Furthermore, in patients with MS with underlying CNS dysfunction, the effect of small changes in hydration may be more prominent due to underlying concurrent autonomic dysfunction. Indeed, fatigue has been clearly and repeatedly worsened by heat, a situation that would increase the impact of a low-hydration (LoH) state.
While serum osmolality is superior to urinary markers for assessing acute hydration status under controlled conditions,8 only urinary markers adequately measure chronic hydration status.9 Urine specific gravity (USG), osmolality, and color all differ between groups with different levels of water consumption, whereas serum osmolality does not;10,11 and several studies have confirmed the validity of USG as an indicator of chronic hydration status.12,13 Importantly, high levels of hydration have been associated with a USG of less than 1.015 in healthy young women.14 Guided by these data and our clinical experience with MS patients, we completed a cross-sectional study of self-reported fatigue and hydration status as measured by USG in 50 female MS patients.
Methods
This study received approval from the University of Virginia (UVA) School of Medicine Institutional Review Board for Health Sciences Research. All subjects provided informed consent prior to participating in any study-related activities. Subjects were recruited from the UVA Department of Neurology outpatient clinics. All subjects were female, aged 18–64 years (inclusive), and had a confirmed diagnosis of MS. Exclusion criteria included the following: diagnosis of diabetes insipidus or renal disease (based on self-report and medical chart review), pregnancy, current symptoms of a gastrointestinal (GI) illness (vomiting or diarrhea), known urinary tract infection, use of diuretics, chronic indwelling bladder catheters, or administration of intravenous (IV) gadolinium or other medications in the prior 24 hours. Subjects were blinded to the study hypothesis to prevent behavior changes prior to urine sample collection. Urine specimens were processed in the clinical lab for routine analysis, including USG by standard colorimetric assay using Bayer urinalysis sticks. Estimated glomerular filtration rate (GFR) was obtained retrospectively from serum lab results within 6 months of study procedures. All surveys were completed by study subjects during the same visit as the urine collection.
Study packets included a general demographic form and several patient-reported outcomes to assess disability, bladder function, and fatigue. MS-related disability was ascertained using the Patient-Determined Disease Steps (PDDS).15 Bladder function was assessed by the Bladder & Bowel Performance Scale16 and the Bladder Control Scale (BLCS).17 We assessed fatigue using three MS-related fatigue scales: Fatigue Performance Scale (PSfatigue), Fatigue Severity Scale (FSS), and Modified Fatigue Impact Scale (MFIS). Fatigue Performance Scale is one subscale of the validated self-report tool that assess nine domains of MS-related disability, asking patients to rank their degree of disability from none (0) to total (5) disability from each domain.16 The Fatigue Severity Scale is a 9-item survey that asks subjects to rate the level of their fatigue from 1 to 7.18 The MFIS consists of 21 items that can be further reduced into subscales that focus on the physical, cognitive, and psychosocial components of fatigue.19 We also collected information regarding sleep and depression that may impact fatigue using the Pittsburgh Sleep Quality Index (PSQI)20 and the Beck Depression Inventory (BDI), respectively. Hydration status was classified by a USG threshold of 1.015, which is optimal to distinguish subjects with high-hydration (HiH) and LoH status.10,11,14
Study data were analyzed in SAS 9.4 unless otherwise noted. Demographic and survey data were compared between hydration groups using chi-square test, Mann–Whitney test, or t-test as appropriate for categorical, ordinal, and interval variables, respectively. Partial correlations between fatigue outcomes and clinical data were calculated via multiple linear regression in R 3.1.2. The clinical data were used as predictors for three different models, one for each fatigue outcome. In addition to the USG, clinical data used as predictors included the BDI fast screen, PDDS, PSQI, and number of nocturnal bathroom events. These specific variables were selected based on their previously reported relationship to MS-related fatigue. The partial correlation for each of these predictors is reported. To correct for multiple comparisons in our regression models (m = 21), only p values below 0.002 are reported as significant.
Results
In total, 50 MS subjects completed all study procedures. Of them, 18 subjects (36%) had USG < 1.015 and were classified as “HiH” state, while 32 subjects (64%) had USG ≥ 1.015 and were classified as “LoH” state. The two hydration state groups were similar in age, self-reported MS disability (PDDS), and other non-fatigue-related measures (Table 1). The timing of urine sample collection (morning vs afternoon) was also similar between groups (p = 1.00). Two subjects had an estimated GFR (eGFR) of less than 60 on chart review (eGFR = 59 and 48). Both were in the LoH group (USG = 1.025 and 1.017, respectively).
Table 1.
Demographics by hydration status.
| High hydration (HiH) (USG < 1.015) |
Low hydration (LoH) (USG ≥ 1.015) |
p value | |
|---|---|---|---|
| Subject number | 18 | 32 | |
| Age, mean ± SD (years) | 42.3 ± 9.5 | 42.5 ± 9.3 | 0.94 |
| Disease subtype | 0.16 | ||
| Relapsing-remitting MS | 16 | 32 | |
| Secondary-progressive MS | 1 | 0 | |
| Primary-progressive MS | 1 | 0 | |
| Years since diagnosis, mean ± SD | 6.9 ± 6.7 | 8.7 ± 5.4 | 0.36 |
| Years since symptom onset, mean ± SD | 9.7 ± 7.5 | 12.7 ± 8.8 | 0.22 |
| USG (dipstick), mean ± SD median (25th Q, 75th Q) | 1.010 ± 0.003 1.011 (1.009, 1.012) |
1.025 ± 0.005 1.025 (1.021, 1.029) |
NA* |
| Morning/afternoon urine sample, % AM | 55.6% | 59.4% | 1.00 |
| Serum osmolality,† mean ± SD | 288.7 ± 2.3 | 287.1 ± 5.0 | 0.14 |
| Serum sodium,† mean ± SD | 139.5 ± 1.0 | 138.1 ± 2.7 | 0.018 |
| Serum glucose,† mean ± SD | 89.3 ± 9.2 | 103.6 ± 54.7 | 0.17 |
| PDDS, median (25th Q, 75th Q) | 1.5 (0, 3) | 2 (0, 3) | 0.53 |
| BDI fast screen, mean ± SD, median (25th Q, 75th Q) | 3.6 ± 3.3, 3.5 (0, 6) | 3.1 ± 3.2, 2 (0, 5) | 0.54 |
| IADL score, mean ± SD, median (25th Q, 75th Q) | 1.6 ± 2.2, 0.5 (0, 3) | 2.1 ± 2.1, 1.5 (0, 4) | 0.32 |
| PSQI score, mean ± SD, median (25th Q, 75th Q) | 10 ± 5.6, 10.5 (5, 14) | 8.6 ± 4.0, 8 (6, 11) | 0.32 |
| BLCS, mean ± SD, median (25th Q, 75th Q) | 3.9 ± 6.0, 0 (0, 8) | 5.9 ± 5.3, 6 (0.5, 10) | 0.13 |
USG: urine specific gravity; PDDS: Patient-Determined Disease Steps; BDI: Beck Depression Inventory; IADL: Instrumental Activities of Daily Living; BLCS: Bladder Control Scale; SD: standard deviation; NA: not applicable; MS: multiple sclerosis.
Groups are based on a USG threshold, so USG is significantly different between them (p < 0.001).
From nearest metabolic panel within 6 months via chart review.
There was a non-significant difference in the number of nightly bathroom visits between groups, with a larger proportion of the LoH group reporting ≥3 bathroom trips per night (62.5% vs 50%). In contrast, a notable 11% reported no nocturnal bathroom breaks in the HiH group compared with only 3% in the LoH group (Supplemental Table 1). The BLCS also demonstrated that those with reduced bladder control were more likely to have LoH status (Table 1 and Figure 1), although this difference did not reach statistical significance (p = 0.13). This relationship was again demonstrated in the Bladder/Bowel Performance Scale results, where a smaller portion of the LoH group reported no dysfunction (39% HiH vs 25% LoH), while a larger portion reported bladder dysfunction, Performance Score >2 (39% HiH vs 50% LoH) (Supplemental Table 2).
Figure 1.
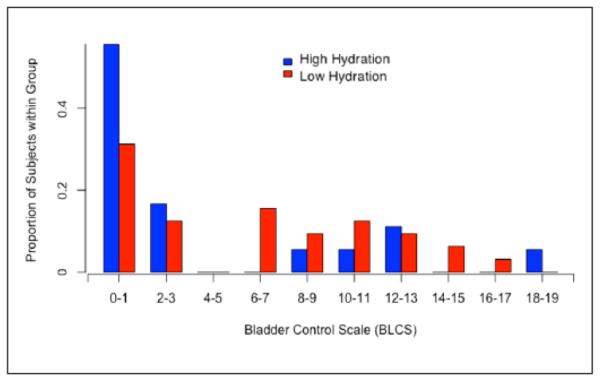
Histogram of Bladder Control Scale scores by hydration status group.
Scores on the Fatigue Performance Scale were significantly higher within the LoH population (p = 0.022), with 58% of LoH subjects rating their fatigue as moderate or higher versus only 39% of the HiH subjects (Table 2). Using the FSS, fatigue was significantly different between the hydration groups, with a mean score of 22.5 ± 12.06 in the HiH and 29.5 ± 9.65 in the LoH group (p = 0.029) (Table 2). Among individual FSS items, the USG was most strongly correlated with Item 6, “My fatigue prevents sustained physical functioning” (r = 0.328, p = 0.0213). In a partial correlation model controlling for depression, disability, sleep quality, and number of bathroom trips per night, USG was significantly correlated with FSS score (r = 0.488, p = 0.0002) (Table 3). FSS was most strongly correlated with USG, depression, and disability (Table 3).
Table 2.
Fatigue scales by hydration status.
| High hydration (HiH) (USG < 1.015) |
Low hydration (LoH) (USG ≥ 1.015) |
p value | ||
|---|---|---|---|---|
| Fatigue Performance Scale, count (%) |
0 (none) | 5 (27.78) | 0 (0.00) | 0.022 |
| 1 (minimal) | 1 (5.56) | 7 (22.58) | ||
| 2 (mild) | 5 (27.78) | 6 (19.35) | ||
| 3 (moderate) | 3 (16.67) | 8 (25.81) | ||
| 4 (severe) | 4 (22.22) | 7 (22.58) | ||
| 5 (totally) | 0 (0.00) | 3 (9.68) | ||
| Fatigue outcome measures, mean ± SD |
FSS total | 22.5 ± 12.1 | 29.5 ± 9.7 | 0.029 |
| MFIS total | 35.2 ± 22.4 | 41.2 ± 17.4 | 0.30 | |
| MFIS physical | 17.0 ± 10.7 | 20.1 ± 8.6 | 0.27 | |
| MFIS cognitive | 15.1 ± 10.3 | 17.9 ± 9.3 | 0.32 | |
| MFIS psychosocial | 3.1 ± 2.1 | 3.2 ± 2.1 | 0.86 |
USG: urine specific gravity; FSS: Fatigue Severity Scale; MFIS: Modified Fatigue Impact Scale; SD: standard deviation.
Bold indicates statistically significant values.
Table 3.
Partial correlations to fatigue outcomes.
| R | p value | |
|---|---|---|
| Fatigue Severity Scale | ||
| Urine specific gravity | 0.488 | 0.0002 |
| BDI fast screen | 0.520 | 0.0001 |
| PDDS | 0.547 | 0.0002 |
| PSQI | 0.169 | 0.2659 |
| Nocturnal bathroom events | 0.260 | 0.0804 |
| Modified Fatigue Impact Scale Total | ||
| Urine specific gravity | 0.248 | 0.0965 |
| BDI fast screen | 0.608 | <0.0001 |
| PDDS | 0.355 | 0.0137 |
| PSQI | 0.292 | 0.0478 |
| Nocturnal bathroom events | 0.374 | 0.0089 |
| Modified Fatigue Impact Scale: Physical and Cognitive composite subscale | ||
| Urine specific gravity | 0.263 | 0.0750 |
| BDI fast screen | 0.574 | <0.0001 |
| PDDS | 0.294 | 0.0460 |
| PSQI | 0.297 | 0.0472 |
| Nocturnal bathroom events | 0.378 | 0.0086 |
PDDS: Patient-Determined Disease Steps; BDI: Beck Depression Inventory; IADL: Instrumental Activities of Daily Living; FSS: Fatigue Severity Scale; MFIS: Modified Fatigue Impact Scale; PSQI: Pittsburgh Sleep Quality Index.
Bold indicates statistically significant values.
The MFIS was not significantly different between hydration status groups, although there was an overall trend for lower total and subscale scores in the HiH group (Table 2 and Figure 2). MFIS question 21, “I have needed to rest more often and for longer periods of time,” strongly correlated to the USG (r = 0.260, p = 0.045). Although not statistically significant, the MFIS did trend toward correlation with hydration status in all areas: physical, cognitive, and psychosocial (Table 2). This trend strengthened when examining the physical and cognitive fatigue measures separately from the psychosocial (Table 2). The MFIS was strongly and significantly correlated with the BDI Fast Screen (r = 0.608, p < 0.0001) and moderately correlated with nocturnal bathroom events (r = 0.374, p = 0.0089) (Table 3).
Figure 2.
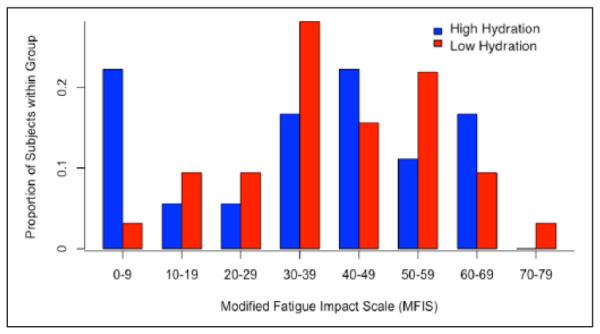
Histogram of Modified Fatigue Impact Scale scores by hydration status group.
Discussion
This study provides the first reported evidence that higher levels of hydration appear protective against some aspects of MS-related fatigue, specifically those measured by the FSS. There also is a suggested trend of reduced MS-related fatigue in the domains measured by the MFIS, although this relationship failed to reach statistical significance. As anticipated, subjects with LoH status had higher self-reported bladder dysfunction; in support of our hypothesis that bladder dysfunction drives fluid restriction in patients and in turn contributes to hydration status.
An association between fatigue and hydration status has been reported in other non-MS populations where fatigue is a prominent symptomatic issue. For example, Hurwitz et al. noted that compared to healthy controls, patients with severe chronic fatigue syndrome had lower overall cardiac volume levels. This finding did not appear to be related to cardiac contractility, and the investigators conjectured that it was instead linked to co-morbid hypovolemia.21 Focusing specifically on mental fatigue, a 2013 study targeted “brain fog,” which they described as forgetfulness, cloudy thinking, or difficultly focusing, in patients with Postural Orthostatic Tachycardia Syndrome (POTS).22 Postulated to be an autonomic derived chronic state of LoH/hypovolemia, the investigators recommended intervention with increased fluid intake along with salt tabs or IV saline. Caffeine, generally seen as having a positive effect on cognition and fatigue, had mixed results in patients with POTS, which was posited to be secondary to its diuretic effects exacerbating their LoH state. Another examination focusing on chronic pain found that patients with low hydration had increased pain sensitivity and intensity.23 Interestingly, this suggests another possible dimension to the relationship in MS patients, who often struggle with neuropathic pain.
The differential strength of the relationship between hydration status and individual fatigue outcome measures raises questions about the constructs assessed by each measure. What aspects of MS-associated fatigue does each outcome assess and how do they differ? In our study, the FSS correlates most significantly with hydration status and depression, while the MFIS largely correlated with depression and nighttime disruptions. The broad spectrum of the MS-related fatigue experience and underlying contributing etiologies suggest that hydration status is relevant, but only to some aspects of the multi-dimensional fatigue experienced by individuals living with MS. Differences in fatigue outcome measures’ performance have been reported previously; for example, a study of amantadine for MS-related fatigue found statistically significant treatment benefit with the MS-Specific Fatigue Scale, but not the FSS.24
Study limitations include the small sample size, which may have prevented associations between hydration status and the MFIS from reaching significance. Additional predictors such as age and disease duration were not included in the partial correlation model to avoid overfitting; however, future larger studies would permit further exploration of these variables. USG is among the best markers of habitual water consumption, but urine color and osmolality could be used in future studies confirm hydration status groups.9–12 More exhaustive assessment of hydration status could include 24-hour urine collection and measurement of serum osmolality, which have a specific value in settings of renal impairment or populations with concerns about urine concentrating capacity. The timing of urine sample collection (morning/afternoon) was similar between groups (p = 1.00), but collection timing should be standardized in future studies. Specifically, we recommend afternoon urine sample collection, which may be a more accurate measure of hydration status.25,26 Finally, assignment to hydration groups by USG could be confounded in the setting of renal dysfunction. Two of our subjects had no known history of renal disease, but did have a calculated eGFR < 60 (48 and 59, respectively). To confirm the findings of our study, we completed a sensitivity analysis eliminating these two subjects and found no change in our results. However, in future studies, we recommend using pre-study eGFR as an exclusion criterion to eliminate this potential confounder.
In summary, our study provides the first reported evidence that increased hydration may be helpful for individuals living with MS who are suffering from fatigue, particularly as measured by the FSS. Recommending increased oral hydration is low risk and could easily be incorporated with other interventions against fatigue. Additional attention and thought will be needed to assist patients in managing bladder-related issues that may be contributing to reduced hydration status. Larger, prospective, and interventional studies are needed to confirm our findings and further characterize the importance of fluid hydration status in MS fatigue.
Supplementary Material
Acknowledgments
Funding
The author(s) received the following financial support for the research, authorship, and/or publication of this article: Project funded by an unrestricted gift from the ziMS Foundation.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Goldman reports grants from National Institutes of Health-National Institute of Neurologic Disorders and Stroke (K23NS62898).
Contributor Information
Molly C Cincotta, Department of Internal Medicine, School of Medicine, University of Virginia, Charlottesville, VA, USA.
Matthew M Engelhard, Department of Systems and Information Engineering, University of Virginia, Charlottesville, VA, USA.
Makela Stankey, College of Arts and Sciences, University of Virginia, Charlottesville, VA, USA.
Myla D Goldman, Department of Neurology, School of Medicine, University of Virginia, Charlottesville, VA, USA.
References
- 1.Krupp L. Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult Scler. 2006;12(4):367–368. doi: 10.1191/135248506ms1373ed. [DOI] [PubMed] [Google Scholar]
- 2.Induruwa I, Constantinescu CS, Gran B. Fatigue in multiple sclerosis—A brief review. J Neurol Sci. 2012;323(1–2):9–15. doi: 10.1016/j.jns.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Lerdal A, Celius EG, Krupp L, et al. A prospective study of patterns of fatigue in multiple sclerosis. Eur J Neurol. 2007;14(12):1338–1348. doi: 10.1111/j.1468-1331.2007.01974.x. [DOI] [PubMed] [Google Scholar]
- 4.Krupp LP, Alvarez LA, LaRocca NG, et al. Fatigue in multiple sclerosis. Arch Neurol. 1988;45:435–437. doi: 10.1001/archneur.1988.00520280085020. [DOI] [PubMed] [Google Scholar]
- 5.Mills RJ, Young CA. A medical definition of fatigue in multiple sclerosis. Q J Med. 2007;101:49–60. doi: 10.1093/qjmed/hcm122. [DOI] [PubMed] [Google Scholar]
- 6.Williams D. Management of bladder dysfunction in patients with multiple sclerosis. Nurs Stand. 2012;13(23):39–46. doi: 10.7748/ns2012.02.26.25.39.c8951. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong LE, Ganio MS, Casa DJ, et al. Mild dehydration affects mood in healthy young women. J Nutr. 2012;142(2):382–388. doi: 10.3945/jn.111.142000. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong LE. Assessing hydration status: The elusive gold standard. J Am Coll Nutr. 2007;26(5 Suppl):575S–584S. doi: 10.1080/07315724.2007.10719661. [DOI] [PubMed] [Google Scholar]
- 9.Baron S, Courbebaisse M, Lepicard EM, et al. Assessment of hydration status in a large population. Br J Nutr. 2015;113(1):147–158. doi: 10.1017/S0007114514003213. [DOI] [PubMed] [Google Scholar]
- 10.Perrier E, Vergne SS, Klein A, et al. Hydration biomarkers in free-living adults with different levels of habitual fluid consumption. Br J Nutr. 2013;109(9):1678–1687. doi: 10.1017/S0007114512003601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malisova O, Athanasatou A, Pepa A, et al. Water intake and hydration indices in healthy European adults: The European Hydration Research Study (EHRS) Nutrients. 2016;8(4):204. doi: 10.3390/nu8040204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armstrong LE, Maresh CM, Castellani JW, et al. Urinary indices of hydration status. Int J Sport Nutr. 1994;4(3):265–279. doi: 10.1123/ijsn.4.3.265. [DOI] [PubMed] [Google Scholar]
- 13.Oppliger RA, Magnes SA, Popowski LA, et al. Accuracy of urine specific gravity and osmolality as indicators of hydration status. Int J Sport Nutr Exe. 2005;15(3):236–251. doi: 10.1123/ijsnem.15.3.236. [DOI] [PubMed] [Google Scholar]
- 14.Armstrong LE, Johnson EC, Munoz CX, et al. Hydration biomarkers and dietary fluid consumption of women. J Acad Nutr Diet. 2012;112(7):1056–1061. doi: 10.1016/j.jand.2012.03.036. [DOI] [PubMed] [Google Scholar]
- 15.Hohol MJ, Orav EJ, Weiner HL. Disease steps in multiple sclerosis: A simple approach to evaluate disease progression. Neurology. 1995;45:251–255. doi: 10.1212/wnl.45.2.251. [DOI] [PubMed] [Google Scholar]
- 16.Marrie RA, Goldman M. Validity of performance scales for disability assessment in multiple sclerosis. Mult Scler. 2007;13:1176–1182. doi: 10.1177/1352458507078388. [DOI] [PubMed] [Google Scholar]
- 17.Turnbull GK, Hoare C, Ritvo PG, et al. Presented at department of medicine research symposium. Dalhousie University; Halifax, NS, Canada: May, 1993. The assessment of bowel and bladder dysfunction in clinic attending MS patients. [Google Scholar]
- 18.Krupp LB, LaRocca NG, Meir-Nash J, et al. The fatigue severity scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 19.Fisk JD, Pontefract A, Ritvo PG, et al. The impact of fatigue on patients with multiple sclerosis. Can J Neurol Sci. 1994;21:9–14. [PubMed] [Google Scholar]
- 20.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiat Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 21.Hurwitz BE, Coryell VT, Parker M, et al. Chronic fatigue syndrome: Illness severity, sedentary lifestyle, blood volume and evidence of diminished cardiac function. Clin Sci. 2009;118(2):125–135. doi: 10.1042/CS20090055. [DOI] [PubMed] [Google Scholar]
- 22.Ross AJ, Medow MS, Rowe PC, et al. What is brain fog? An evaluation of the symptom in postural tachycardia syndrome. Clin Auton Res. 2013;23(6):305–311. doi: 10.1007/s10286-013-0212-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bear T, Philipp M, Hill S, et al. A preliminary study on how hypohydration affects pain perception. Psychophysiology. 2016;53:605–610. doi: 10.1111/psyp.12610. [DOI] [PubMed] [Google Scholar]
- 24.Krupp LB, Coyle PK, Doscher C, et al. Fatigue therapy in multiple sclerosis: Results of a double-blind, randomized, parallel trial of amantadine, pemoline, and placebo. Neurology. 1995;45:1956–1961. doi: 10.1212/wnl.45.11.1956. [DOI] [PubMed] [Google Scholar]
- 25.Bottin JH, Lemetais G, Poupin M, et al. Equivalence of afternoon spot and 24-h urinary hydration biomarkers in free-living healthy adults. Eur J Clin Nutr. doi: 10.1038/ejcn.2015.217. Epub ahead of print 13 January 2016. DOI: 10.1038/ejcn.2015.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perrier E, Demazières A, Girard N, et al. Circadian variation and responsiveness of hydration biomarkers to changes in daily water intake. Eur J Appl Physiol. 2013;113(8):2143–2151. doi: 10.1007/s00421-013-2649-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


