Abstract
Objectives
Perceived burdensomeness is thought to contribute to suicide risk. However, suicidal behavior is clinically and psychologically heterogeneous. Does a high level of perceived burdensomeness differentiate medically serious suicidal acts, most closely resembling death by suicide, from less serious ones? How is perceived burdensomeness related to dysfunctional personality dimensions implicated in suicide? We sought to answer these questions in a cross-sectional, case control study of adults, aged 42 or older (N=165).
Methods
Participants were suicidal depressed with history of high- and low-lethality attempts, depressed with serious suicidal ideation, depressed non-suicidal and psychiatrically healthy controls. Following detailed clinical characterization, we assessed perceived burdensomeness, the Big Five, impulsivity, and anger-rumination.
Results
Low-lethality attempters reported highest levels of perceived burdensomeness, followed by ideators, high-lethality attempters, non-suicidal depressed and healthy controls. Group differences were robust to confounders, including demographics, severity of depression, and physical illness burden. In suicide attempters, perceived burdensomeness scaled positively with neuroticism, impulsivity, and anger; and negatively with extraversion, conscientiousness, and age.
Conclusions
Our findings suggest that perceived burdensomeness is most prominent in a subgroup of younger individuals with lower-lethality suicide attempts and a dysfunctional interpersonal style. Older adults with high-lethality attempts are surprisingly more resilient to the feelings of burdensomeness.
Keywords: suicide, perceived burdensomeness, attempt lethality
Suicidal risk is high in the second half of life and continues to increase with age (CDC, 2012), while suicide attempts become more serious (De Leo et al., 2001). Perceived burdensomeness (PB) is recognized as an important risk factor for suicide attempts (Joiner, 2005; Orden et al., 2005). The contribution of PB to suicidal behavior in later life has yet to be thoroughly examined. Older people may feel increasingly dependent on others due to physical illness, cognitive impairment, loss of prior sources of income, and a shrinking social network. Therefore, the focus of the present study is PB in middle-aged and elderly suicide attempters. While informed by the interpersonal theory of suicide (Van Orden et al., 2010), our study does not constitute a comprehensive test of its predictions. First, we investigated whether suicide attempts and ideation are associated with high levels of PB. An association of a factor with suicidal ideation and even attempts, however, does not reliably implicate it in death by suicide (Beautrais, 2001; Pagura et al., 2008) because of the heterogeneity of suicidal behavior (Dombrovski et al., 2011; Engström et al., 1996). Thus, we also tested whether PB was the highest in individuals who made medically serious attempts that could have resulted in death. Further, to understand the broader psychological context in which extreme feelings of burdensomeness may emerge, we examined its association with personality traits and interpersonal styles, which also play an important role in suicide diathesis (Mann et al., 1999).
Suicidal behavior in the second half of life provides an in vivo model of death by suicide. Older individuals who attempt suicide are demographically more similar to those who die by suicide than younger suicide attempters, and their suicide attempts tend to be more lethal (De Leo et al., 2001; Dombrovski et al., 2008). Several studies have reported associations between suicidal ideation in the elderly with physical illness and heightened concerns that this illness may burden loved ones (Akechi et al., 2004; Noor-Mahomed et al., 2003; Wilson et al., 2005). PB need not scale, however, with objective indicators such as physical health or personal income. Presently, PB independent of one’s physical health has been examined only once. A study of adults aged 55 and older found a positive association between PB and suicidal ideation (Cukrowicz et al., 2011). Importantly, because the sample did not include suicide attempters, the relationship with suicidal behavior remained unexamined and is the focus of the present inquiry.
Although PB is argued to represent a psychological determinant of suicidal behavior, it is unclear if the attempters experience greater burdensomeness than those who contemplate suicide but never attempt. Several studies have linked burdensomeness with increased suicidal ideation (Cukrowicz et al., 2011; Joiner et al., 2009; Van Orden et al., 2012, 2008, 2006). Only a subset of suicide ideators, however, goes on to attempt suicide. Of the three studies that have probed the relationship between PB and suicidal behavior, two reported a positive association with the number of attempts (Van Orden et al., 2008, 2006), but not with directly predicting a suicide attempt (Joiner et al., 2009). Most recently, Van Orden et al. (2015) have also shown in a case-control matched sample of 86 pairs of suicide victims and healthy controls that greater risk for burdensomeness (together with painful and provocative experiences) was associated with suicide (vs. controls). However, this study did not include suicide ideators or a psychiatric comparison group. If indeed feelings of burdensomeness increase the motivation for suicide, we would expect suicide attempters to report higher levels of these feelings than ideators.
Furthermore, suicide attempts range in severity from near fatal (“high-lethality”) to less medically serious (“low-lethality”). This heterogeneity is not explicitly addressed by the psychological theories of suicide, although Baumeister (1990) notes that a stronger motivation may be expected to result in suicidal acts of higher lethality. Indeed, one early study offered evidence that suicide notes of suicide victims – particularly those who used more lethal means – conveyed higher levels of burdensomeness (Joiner et al., 2002). To our knowledge the positive relationship between PB and the lethality of suicidal behavior has not been tested in vivo.
Finally, it is possible that feelings of burdensomeness occur in the context of a dysfunctional interpersonal style. Personality plays an important, if underspecified, role in suicidal behavior among older adults (Duberstein et al., 2000). From dimensional perspective, high neuroticism, low extraversion, and chronic interpersonal problems have been all associated with suicidal behavior (Duberstein et al., 2004, 2000; Harrison et al., 2010; Klonsky and May, 2010; Szanto et al., 2012). From the attachment theory perspective, the perception of being a burden is consistent with a high approach/high anxiety preoccupied attachment style seen in borderline, vulnerable narcissistic, and dependent personality (Meyer and Pilkonis, 2005). Similarly, one can draw a connection with the cognitive theory perspective on personality pathology (Pretzer and Beck, 2005). The early maladaptive schemas seen in borderline, avoidant and dependent personalities lead to negative self-related cognitions, such as “I am a burden to others”. Consequently, we predicted that individuals high on dysfunctional personality dimensions should report highest feelings of burdensomeness. An important related question is whether the association between suicidal behavior and PB is specific or whether it is subsumed by broader dispositional traits including neuroticism and extraversion. To rule out this account, we tested whether the relationship between PB and suicidal study groups was accounted for by the traits from the five-factor model of personality.
Thus, in the present study we investigate a dose-response relationship between PB and lethality (medical seriousness) of suicidal behavior. Five groups of participants were studied: 1) psychiatrically healthy controls with no lifetime history of suicidal behavior or suicidal ideation, 2) depressed participants with no lifetime history of suicidal behavior or ideation, 3) depressed participants with suicidal ideation but no history of suicidal behavior, 4) depressed low-lethality suicide attempters, and 5) depressed high-lethality suicide attempters.
Methods
Participants
One hundred and sixty-five participants aged 42 and older were recruited. All participants provided written informed consent. The University of Pittsburgh institutional review board approved the study. Their demographic, clinical and cognitive characteristics are described in Table 1. Major depression was diagnosed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (First et al., 1995) in 135 individuals. Depression severity was measured with the 17-item Hamilton Depression Rating Scale (HAM-D: Hamilton, 1960). All suicidal and non-suicidal depressed participants fulfilled DSM-IV criteria for major depression and had a Hamilton score that indicated at least mild to very severe depression (8 ≥ score ≥ 23).
Table 1.
Demographic, clinical, and cognitive characteristics
| Study Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Non-psychiatric Controls (n = 30) |
Non-suicidal Depressed (n = 37) |
Depressed Ideators (n = 34) |
Depressed Suicide Attempters, Low- Lethality (n = 32) |
Depressed Suicide Attempters, High- Lethality (n = 32) |
F, t, or χ2 |
p | Post-hoc Tukey HSD |
| Male sex, No. (%) | 12 (40) | 23 (62) | 21 (62) | 16 (50) | 18 (56) | 4.44 | .35 | |
| Age in years (SD) | 67.57 (11.7) | 66.68 (5.9) | 64.47 (10.1) | 61.25 (7.1) | 65.50 (11.0) | 2.21 | .07 | |
| White, No. (%) | 24 (80) | 30 (81) | 29 (85) | 25 (78) | 30 (94) | 3.64 | .46 | |
| Educational level, y | 15.30 (2.4) | 14.60 (2.4) | 14.71 (2.9) | 14.81 (3.1) | 13.47 (3.5) | 1.72 | .15 | |
| Mean income, ×1000 (n = 148) | 51.20 (2.4) | 33.34 (2.4) | 31.4 (2.7) | 31.11 (2.7) | 39.9 (3.2) | 2.83 | .03 | HC1 > I2, LL3 |
| Premorbid IQ, WTAR scaled (n = 155) | 110.27 (9.0) | 106.61 (15.3) | 108.79 (14.1) | 100.51 (16.1) | 101.14 (18.7) | 2.67 | .04 | —† |
| Dementia rating scale (n = 164) | 138.41 (3.2) | 134.95 (4.4) | 134.47 (7.1) | 134.84 (2.1) | 132.94 (6.6) | 4.27 | .00 | HC > I, LL, HL5 |
| Executive interview, EXIT | 6.83 (3.8) | 6.08 (3.6) | 7.15 (3.8) | 7.19 (3.3) | 8.19 (4.2) | 1.40 | .24 | |
| Physical illness burden (Miller et al., 1992) | 5.90 (3.3) | 10.46 (3.1) | 7.12 (4.2) | 8.25 (3.9) | 7.72 (4.7) | 6.42 | .00 | HC < D6; |
| D > I, HL | ||||||||
| Hamilton Rating Scale for Depression (w/o suicide item) |
2.17 (1.9) | 16.27 (3.7) | 22.35 (5.9) | 22.81 (6.8) | 21.72 (6.1) | 71.81 | .00 | HC < rest; D < I, LL |
| Beck Suicidal Ideation Scale (n = 163) |
0.03 (0.2) | 0.11 (0.5) | 15.85 (8.7) | 25.48 (8.1) | 25.47 (4.6) |
163.9 4 |
.00 | HC < D < I < LL, HL |
| Beck Suicide Intent Scale (SIS) total | NA | NA | NA | 17.47 (5.1) | 20.47 (4.4) | 2.52 | .01 | |
| Suicide intent planning subscale | NA | NA | NA | 7.41 (3.0) | 9.09 (3.0) | 2.25 | .03 | |
| Perceived burdensomeness | 0.27 (0.6) | 0.62 (0.8) | 3.62 (3.1) | 4.38 (3.0) | 2.41 (2.9) | 18.77 | .00 | HC, D < rest; LL > HL |
| Perceived social support (ISEL: (Cohen et al., 1985) (n = 161): | ||||||||
| Appraisal | 10.90 (1.5) | 8.56 (2.2) | 7.21 (3.5) | 7.26 (2.9) | 8.55 (2.7) | 9.76 | .00 | HC > rest |
| Belonging | 10.13 (1.9) | 8.03 (2.4) | 6.15 (3.6) | 5.39 (2.4) | 7.36 (2.8) | 14.25 | .00 | HC > rest; D > I, LL; LL < HL |
| Tangible | 10.43 (2.2) | 9.14 (2.1) | 7.24 (3.6) | 6.45 (3.1) | 7.51 (3.5) | 9.34 | .00 | HC > I, LL, HL; D > LL |
| Self-esteem | 9.30 (1.5) | 6.61 (2.5) | 4.58 (2.6) | 4.29 (2.6) | 4.81 (2.2) | 25.02 | .00 | HC > D > rest |
| Chronic Interpersonal Difficulties (IIP-15): | ||||||||
| Interpersonal Sensitivity | 3.00 (2.6) | 6.97 (4.0) | 9.09 (5.4) | 8.47 (4.1) | 8.32 (4.9) | 9.95 | .00 | HC < rest |
| Interpersonal Ambivalence | 2.87 (4.1) | 4.31 (3.2) | 5.36 (4.8) | 6.53 (5.3) | 6.53 (5.8) | 3.26 | .01 | HC < LL, HL |
| Aggression | 1.67 (2.0) | 4.97 (3.9) | 6.24 (4.6) | 5.09 (3.5) | 5.29 (5.1) | 5.89 | .00 | HC < rest |
| Anger Rumination Scale (n = 143) | 25.72 (4.1) | 34.45 (10.6) | 37.89 (10.0) | 39.77 (11.0) | 35.63 (11.7) | 8.87 | .00 | HC < rest |
| Barratt-nonplanning (n = 159) | 11.25 (6.6) | 16.43 (7.5) | 18.36 (7.7) | 20.56 (9.1) | 19.77 (8.7) | 6.35 | .00 | HC < rest |
| Lifetime substance use disorders (%) | NA | 31% | 42% | 47% | 34% | 2.35 | .50 | |
| Lifetime anxiety disorders (%) | NA | 41% | 47% | 47% | 31% | 2.40 | .50 | |
HC = healthy controls;
I = ideators;
LL = low-lethality suicide attempters;
HL = high-lethality suicide attempters;
D = depressed non-suicidal
A Kruskall-Wallis H Test verified that there was no significant difference between the IQof healthy vs. depressed groups.
Suicide attempters
Sixty-four attempters had a history of self-injurious acts completed with intent to die. Medical seriousness of attempts was assessed using the Beck Lethality Scale (BLS: Beck et al., 1975). For participants with multiple attempts, data for the highest-lethality attempt are presented. The suicidal intent of the suicide attempt was measured with Beck’s Suicide Intent Scale (SIS: Beck et al., 1974). The SIS-planning subscale (Mieczkowski et al., 1993) was used to assess the degree of planning of suicide attempts. A study psychiatrist (A.Y. D. or K. S.) verified a history of suicide attempts, based on the interview, medical records, information from family members and friends. We excluded participants with significant discrepancies between these sources.
Thirty-two of these individuals had high-lethality attempts (HL) which could have caused death without medical intervention due to unstable vital signs, penetrating wounds of abdomen or chest, third-degree burns, major bleeding, coma, or need for resuscitation, as defined by a score of ≥ 4 on the BLS. The rest were classified as low-lethality attempters (LL).
Suicidal ideators (I)
Thirty-four ideators had suicidal ideation with a plan, severe enough to require psychiatric hospitalization or outpatient treatment. None of the ideators had a suicide attempt. Suicidal ideation was assessed using Beck Scale for Suicide Ideation (SSI: Beck et al., 1979).
Non-suicidal depressed (D)
Thirty-seven non-suicidal depressed adults were included in the study as one of two benchmark groups to capture effects on PB scores beyond those of depression. These participants had no current or lifetime history of suicide attempts or suicidal ideation as established by clinical interview, review of medical records, SCID/DSMIV, and SSI.
Non-depressed controls (HC)
Thirty non-suicidal non-depressed adults served as another benchmark group. These participants did not have any lifetime history of psychiatric disorder as determined by SCID/DSMIV. Further, clinical interview, review of medical records, SCID/DSMIV, and SSI established no current or lifetime suicide ideation or attempts.
Measures
Interpersonal Needs Questionnaire
(Van Orden et al., 2012, 2006) assessed the degree to which one feels as a burden on loved ones (Table 2). In our sample, the internal consistency of this instrument was good, Cronbach’s alpha = 0.85. The maximum possible score (and maximum in our sample) is 12 and the minimum is 0.
Table 2.
Items used to assess perceived burden.
| For each of the following statements, please check off whether you think it is very true for you (2), somewhat true for you (1), or not at all true for you (0). |
|
|---|---|
| 1 | The people in my life would be better off if I were gone |
| 2 | The people in my life would be happier without me |
| 3 | My death would be a relief to the people in my life |
| 4 | The people in my life secretly wish they could be rid of me |
| 5 | I make things worse for the people in my life |
| 6 | I feel needed |
Dispositional measures
Personality dimensions were assessed using the NEO Five-Factor Inventory (NEO), which includes five scales (neuroticism, extraversion, openness, agreeableness and conscientiousness) (Costa and McCrae, 1989). Neuroticism reflects anxiety, hostility, depression, impulsiveness and vulnerability. Extraversion comprises warmth, excitement seeking, sociability. Openness incorporates fantasy, feelings, actions, and values. Agreeableness reflects trust, altruism and nurturance. Conscientiousness comprises organization, punctuality, planning, achievement and honesty.
We used the Anger Rumination Scale (Sukhodolsky et al., 2001) to measure the tendency to focus attention on angry affects, to recollect anger-provoking events and to think about their causes and consequences.
Chronic interpersonal difficulties were measured by the Inventory of Interpersonal Problems (IIP), specifically 15 items that aid in screening for personality disorders (Morse and Pilkonis, 2007). Interpersonal difficulties are characteristic of personality disorders and play a role in maintaining or exacerbating affective symptoms. Subscales on the IIP-15 include interpersonal sensitivity, interpersonal ambivalence, and aggression. Interpersonal sensitivity reflects strong affectivity and reactivity in interpersonal settings. Interpersonal ambivalence reflects inability to collaborate with others. Aggression reflects hostile interpersonal cognitions.
Trait impulsivity was assessed with the Nonplanning subscale of the Barratt Impulsiveness Scale (Barratt-nonplanning: Patton et al., 1995). High values on the BIS-nonplanning subscale correspond to acting without considering the consequences and with the focus on the immediate rather than long-term outcomes. This dimension of impulsivity, i.e., lack of premeditation, has been associated with suicide attempts in previous studies (Klonsky and May, 2010).
Statistical Analyses
We tested group differences using univariate analysis of variance and co-variance (ANOVA) for continuous variables and chi-square tests for categorical variables. Pairwise group comparisons were conducted with Tukey HSD post-hoc tests. To verify that the group differences were robust to possible confounders, we conducted sensitivity analyses using a general linear model that included both group and potential confounding variables (ANCOVA). Then we used a linear regression model to test association between the PB and group, adjusting for demographic variables (age and education), and for each of the dispositional measures separately (NEO, Barratt, ARS, IIP-15, and ISEL). The results of these latter analyses are presented in the Supplementary Materials. Finally, we used a multinominal logistic regression model to examine the extent to which PB predicted group membership, and whether this relationship was robust to effects of other dispositional measures.
While burdensomeness questionnaires were available for all participants, NEO data were missing for 38 of 165 participants (23%) because of the changes in the assessment battery over time. We used multiple imputation to recover accurate estimates of the association between personality traits and burden (Rubin, 2004). The imputation model included demographics (e.g., age, sex, race, education, income), clinical variables (e.g., levels of depression), cognitive characteristics (e.g., intelligence, executive functioning), and other dispositional measures (e.g., impulsivity and aggression scales). To avoid circularity, group membership was not used in the imputation procedure. Ten complete datasets were imputed using SPSS with 1000 burn-in Monte Carlo iterations to achieve 97.75% estimation efficiency (Rubin, 2004). Multiple group analysis indicated that the significance and the size of the effects did not differ across imputations (unless otherwise noted); hence, we report the mean, the minimum and the maximum of F-values and sizes of effects of interest. Finally, unless otherwise noted, the results were the same using non-missing data only.
Results
Group characteristics
Descriptive statistics and preliminary analyses are presented in Table 1. The composition of the five groups was approximately the same with respect to age, sex, race and education. Healthy controls reported higher income than ideators and low-lethality attempters. Physical illness burden differed across groups: non-suicidal depressed reported higher levels than healthy controls, ideators, and high-lethality attempters. Comorbid anxiety disorders and substance abuse/dependence were similarly prevalent in the depressed groups. Non-suicidal depressed had lower HAM-D scores than ideators and low-lethality suicide attempters. No demographic or clinical differences among suicidal depressed or suicide attempters were detected. Age at depression onset was similar between the depressed groups (F[3, 121] = 1.32, p = .27). Ideators reported lower levels of suicidal ideation than both low- and high-lethality suicide attempters (vs. LL: t[64] = 4.38, p < .01; vs. HL: t[64] = 4.74, p < .01) on the SSI, but no significant differences were detected between low- versus high-lethality suicide attempters (t[61] = 0.01, p = .99). SIS-planning scores for the most lethal attempt were predictably lower for low-lethality attempters than high-lethality attempters (t[62] = 2.25, p < .05).
Healthy controls reported having the most social support, least interpersonal difficulties, were the least impulsive and were least likely to engage in anger-rumination than other groups.
Perceived burdensomeness
PB differed significantly across groups, F(4, 160) = 18.77, p < .01, η2 = .32 (Figure 1). Low lethality suicide attempters reported the highest levels of PB relative to healthy controls (t[60] = 7.41, p < .01), depressed non-suicidal participants (t[67] = 7.35, p < .01) and high-lethality suicide attempters (t[62] = 2.66, p < .05). High lethality suicide attempters reported feeling more burdensome than healthy controls (t[60] = 3.90, p < .01) and non-suicidal depressed (t[67] = 3.53, p < .01). Neither group of suicide attempters was different from suicidal ideators.
Figure 1.
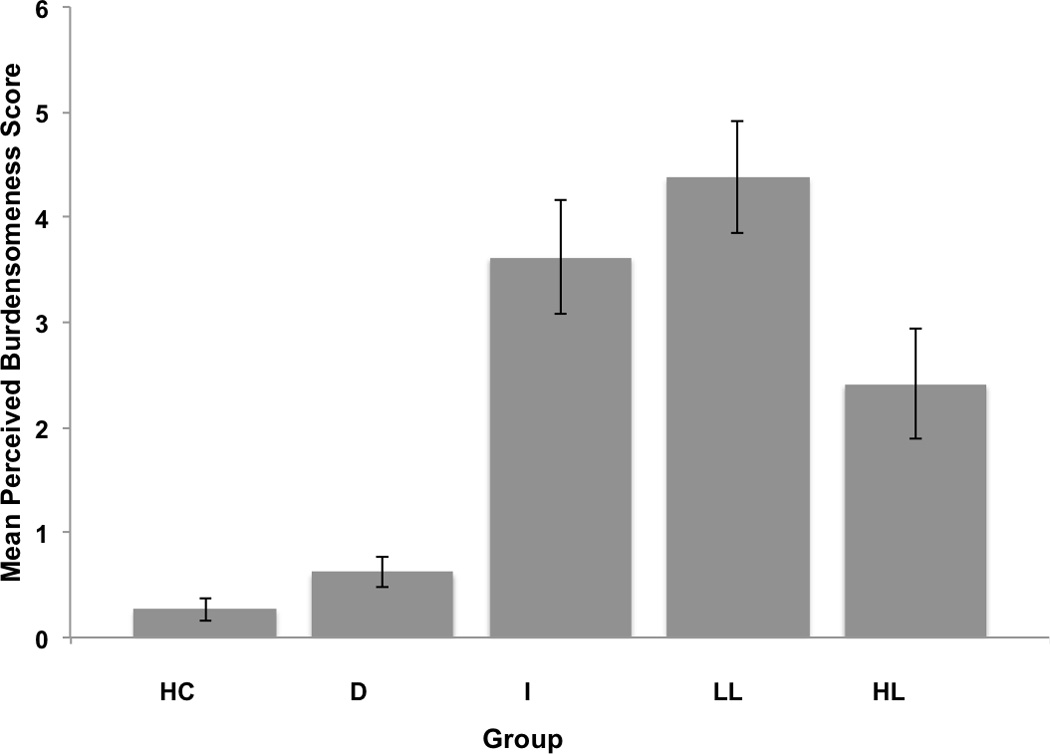
Mean perceived burdensomeness scores by group (HC = healthy controls; D = depressed non-suicidal; I = suicidal ideators; LL = low lethality attempters; HL = high lethality attempters). Pairwise comparisons indicate that all groups are different, except for HC vs. D, I vs. LL and I vs. HL.
We examined the extent to which feelings of burdensomeness were associated with potential objective markers of being a burden to others. In the whole sample, PB was weakly associated with mean income (r[146] = −.17, p < .05). This association did not hold within the subsample of suicidal individuals (I, LL, and HL: r[96] = − .14, p = .21). Interestingly, in the whole sample, PB was not associated with physical illness burden (CIRS-G), widowhood, or not-living independently (r[163] ≤ .10, p > .05).
Given the important role assigned to PB in the emergence of suicidal ideation, we also examined the association between these two variables. Level of PB was weakly and not significantly associated with the severity of suicidal ideation among all suicidal individuals (I, LL, and HL: r[95] = .19, p = .06; a Kendall’s tau-b correlation was also used to accommodate non-normally distributed suicide ideation scores: τb = .12, p = .09). Inspection of scatter plots, consistent with group differences reported above, suggested that a weak association may have been driven by the difference between LL and I. Nor was PB associated with suicidal ideation among suicide attempters (LL and HL: r[61] = .13, p = .30; τb = .11, p = .23). Further, there was a weak negative correlation of PB with suicide attempt planning (r[62] = −.22, p = .09; but non-parametric correlation τb = −.19, p < .05), suggesting that greater degree of suicide attempt planning may be associated with lower burdensomeness.
PB was associated, however, with low perceived social support, chronic interpersonal difficulties, high neuroticism, low extraversion, high impulsivity, and high anger-rumination (Table 3). These associations also held within the depressed groups. We observed similar patterns of associations in suicide attempters only (ISEL self-esteem: r[60] = −.36, p < .01; belonging: r[60] = −.24, p = .06; IIP-15 interpersonal sensitivity: r[61] = .39, p < .01; and aggression: r[61] = .25, p = .05; Barratt-nonplanning: r[61] = .24, p = .05; and ARS: r[55] = .32, p < .05).
Table 3.
Associations between perceived burdensomeness and personality measures in the entire sample.
| 1 | 2 | 3 | 4 | 5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | d | a | b | c | a | b | c | d | e | |||
| 1. Perceived burdensomeness | ||||||||||||||
| 2. Perceived social support (ISEL) |
||||||||||||||
| a. Appraisal | −.27** | |||||||||||||
| b. Belonging | −.40** | .75** | ||||||||||||
| c. Tangible | −.38** | .60** | .62** | |||||||||||
| d. Self-esteem | −.48** | .47** | .60** | .52** | ||||||||||
| 3. Chronic interpersonal difficulties (IIP-15) |
||||||||||||||
| a. Interpersonal Sensitivity | .45** | −.36** | −.36** | −.34** | −.52** | |||||||||
| b. Interpersonal Ambivalence | .27** | −.21** | −.26** | −.31** | −.32** | .37** | ||||||||
| c. Aggression | .28** | −.28** | −.33** | −.28** | −.49** | .76** | .45** | |||||||
| 4. NEO Five-Factor Inventory1 |
||||||||||||||
| a. Neuroticism | .52** | −.38** | −.41** | −.41** | −.62** | .60** | .25** | .48** | ||||||
| b. Extraversion | −.37** | .37** | .46** | .32** | .53** | −.40** | −.22* | −.40** | −.61** | |||||
| c. Openness | −.15 | .18* | .25** | .18* | .28** | −.14 | −.23** | −.24** | −.24** | .34** | ||||
| d. Agreeableness | −.13 | −.21* | .23** | .22* | .15 | −.21* | −.12 | −.32** | −.27** | .29** | .18* | |||
| e. Conscientiousness | −.26** | .22* | .31** | .30** | .47** | −.44** | −.29** | −.52** | −.60** | .60** | .20* | .42** | ||
| 5. Barratt-nonplanning | .35** | −.33** | −.36** | −.38** | −.46** | .33** | .36** | .40** | .37** | −.44** | −.37** | −.21* | −.58** | |
| 6. Anger Rumination Scale | .38** | −.32** | −.34** | −.34** | −.44** | .52** | .33** | .42** | .70** | −.51** | −.19* | −.27** | −.40** | .24** |
Intercorrelations reported in this Table are with non-imputed NEO scores (n = 127); same pattern of intercorrelations held across the imputed datasets.
p < .05.
p < .01
Although physical illness burden increased with age (r[163] = .24, p < .01), contrary to our hypothesis, older suicide attempters did not feel more burdensome, and the opposite was nearly true (age and PB in LL and HL: r[62] = −.24, p = .06).
Shown in Table 4, additional variance in PB was explained by depression severity (within the whole sample and the depressed groups), levels of perceived social support (self-esteem, belongingness, and tangible), levels of chronic interpersonal difficulties (sensitivity, ambivalence, and aggression), NEO neuroticism and extraversion, impulsivity (Barratt-nonplanning) and anger-rumination (ARS). Group differences in PB remained significant when these variables were included. Group differences were robust to the inclusion of age, sex, physical illness burden, education, mean income, intelligence, level of executive dysfunction, and global cognition.
Table 4.
Effect of group membership with other covariates
| Covariate | Group membership | |||||
|---|---|---|---|---|---|---|
| F | p | ηp2 | F | p | ηp2 | |
| Age | 3.30 | .07 | .02 | 16.58 | .01 | .29 |
| Sex | 0.22 | .64 | .00 | 18.80 | .01 | .33 |
| Educational level, y | 6.17 | .05 | .04 | 19.03 | .01 | .32 |
| Mean income, ×1000 | 1.18 | .28 | .01 | 15.40 | .01 | .30 |
| Premorbid IQ, WTAR scaled | 2.02 | .16 | .01 | 17.97 | .01 | .33 |
| Executive interview (EXIT) | 0.72 | .40 | .01 | 18.25 | .01 | .32 |
| Burden of physical illness | 4.32 | .05 | .03 | 19.65 | .01 | .33 |
| Dementia rating scale | 0.03 | .86 | .00 | 17.94 | .01 | .31 |
| Depression severity in the whole sample | 4.33 | .05 | .03 | 9.79 | .01 | .20 |
| Depression severity in the depressed groups | 4.54 | .05 | .03 | 8.60 | .01 | .17 |
| Perceived social support (ISEL): | ||||||
| Appraisal | 0.92 | .34 | .01 | 13.68 | .01 | .26 |
| Belonging | 5.57 | .05 | .04 | 10.02 | .01 | .21 |
| Tangible | 5.67 | .05 | .04 | 11.20 | .01 | .22 |
| Self-esteem | 12.01 | .01 | .07 | 7.63 | .01 | .17 |
| Chronic interpersonal difficulties (IIP-15) | ||||||
| Interpersonal Sensitivity | 20.79 | .01 | .12 | 12.32 | .01 | .24 |
| Interpersonal Ambivalence | 4.93 | .05 | .03 | 15.45 | .01 | .28 |
| Aggression | 5.77 | .05 | .04 | 15.46 | .01 | .28 |
| NEO Five-Factor Inventory1 | ||||||
| Neuroticism | 20.46 | .01 | .12 | 10.41 | .01 | .21 |
| Extraversion | 7.67 | .05 | .05 | 14.60 | .01 | .27 |
| Openness | 0.62 | .97 | .00 | 17.62 | .01 | .31 |
| Agreeableness | 0.69 | .88 | .00 | 18.51 | .01 | .32 |
| Conscientiousness | 6.05 | .05 | .04 | 17.47 | .01 | .31 |
| Barratt-nonplanning | 8.17 | .01 | .05 | 13.05 | .01 | .25 |
| Anger Rumination Scale | 7.29 | .01 | .05 | 9.85 | .01 | .22 |
For the co-variate and group effects, we report mean F, mean ηp2 and the maximum p-values of the analyses conducted on the ten imputed datasets.
These variables can only be assessed for the two groups of depressed participants, i.e., depressed non-suicidal and suicide attempters.
In addition, we examined the extent to which the group membership was predicted by PB, when demographic variables (age and education) and dispositional measures (IIP-15 subscales, ISEL subscales, NEO subscales, Barratt-nonplanning and ARS) were entered into the model. PB remained a robust predictor of group membership across all imputed datasets (χ2Mean[1, 4] = 26.71, all ps < .01; 23.96 ≤ χ2[1, 4] ≤ 29.57). A subset of personality measures also predicted the likelihood of being in particular group, however, the composition of personality measures in the subset was inconsistent across the imputed datasets (Supplementary materials).
Discussion
Unexpectedly, in our study, low-lethality (LL) suicide attempters reported the highest levels of PB, compared not only to the reference groups of healthy controls and depressed non-suicidal, but also to high-lethality (HL) attempters. This is surprising as LL attempters are thought to have a lower motivation to die (Baumeister, 1990). Suicide ideators reported intermediate levels of PB, not different from either LL or HL attempters. Perceptions of burdensomeness scaled positively with neuroticism, impulsivity, anger rumination, and chronic interpersonal problems. Nevertheless, PB remained a predictor of suicide attempts and ideation even after accounting for these dispositional measures.
Our results were partially consistent with the predictions of Joiner’s interpersonal theory in that suicide attempters and ideators reported higher PB than comparison groups. The level of perceived burden was not different in ideators from suicide attempters and, more significantly, the highest levels of burdensomeness were associated with less lethal attempts and less attempt planning. As suggested by the theory, PB did not necessarily scale with putatively more objective indicators of burdensomeness such as low income and physical illness. In fact, although physical illness burden increased with age, it was younger and not older suicide attempters that felt more burdensome. Importantly, robust associations of PB with interpersonal problems and neuroticism, low extraversion, anger-rumination, and impulsivity, suggest that feeling like a burden may be part of an enduring pattern of interpersonal dysfunction. This constellation of burdensomeness and a maladaptive interpersonal style was seen mostly in younger, low-lethality suicide attempters. Thus, although PB may be high in this subgroup of suicide attempters, its value in terms of predicting the risk of more serious suicidal behavior appears limited. This is also consistent with recent findings of Van Orden, Wiktorsson and Duberstein (2015) which reported that only 13/101 older suicide attempters reported PB as the reason for their attempt. In that study, PB was not associated with the use of more lethal means for the suicide attempt and did not predict re-attempts.
Our findings underscore the psychological heterogeneity of suicidal behavior and align with other observations that support the existence of distinct pathways (Dombrovski et al., 2013, 2011). Several features of the putative pathway encompassing PB – interpersonal conflict, negative emotionality, impulsivity, and low-lethality suicide attempts – evoke borderline personality disorder (BPD). Our study unfortunately lacked a categorical BPD assessment, and future research will need to determine to what extent PB is predictive of suicidal behavior above and beyond BPD. A related question is whether, as a suicidogenic factor, PB is merely epiphenomenal to neuroticism and impulsivity. This does not seem to be the case: the unique association between PB and suicidal behavior was not entirely explained by effects of neuroticism or impulsivity. Thus, PB appears to be an aspect of maladaptive personality germane to emergence of suicidal behavior in a subgroup of individuals.
4.1. Limitations
The main limitation of our study is the cross-sectional case-control design. We do not know to what extent the perception of burdensomeness co-varies with depressive state. We used attempt lethality (medical seriousness) as a proxy for risk of death by suicide, thus, the extent to which the findings generalize to depressed older adults who die by suicide is also unknown. Another limitation is the lack of categorical assessments of dysfunctional personality, particularly borderline personality disorder. In addition, we cannot rule out that the difference between low- and high-lethality attempters in the level of PB may also be explained by the acquired capacity for self-harm. The negative association between age, physical illness and PB should be qualified by the study’s small sample size.
Conclusion
Our findings challenge the notion of rational suicide in old age, where illness and severe disability lead to feelings of burdensomeness. In contrast, PB in suicidal individuals emerges in the context of maladaptive personality, characterized by neuroticism, impulsivity, and interpersonal conflict. This constellation is associated with suicidal ideation and low-lethality suicide attempts.
Supplementary Material
KEYPOINTS.
1) Individuals with history of low-lethality attempts report greater feelings of being a burden (PB) to others than those with high-lethality attempts; 2) Higher PB is also associated with higher neuroticism, impulsivity and anger; 3) Among suicide attempters, older adults report lower feelings of burdensomeness; 4) These findings point to one putative pathway to suicide – interpersonal conflict, negative emotionality, impulsivity, and low-lethality suicide attempts – evoking borderline personality traits (BPD).
Acknowledgments
Swathi Gujral, BS, Laura Kenneally, BA, Julie Matz, BS, Erika Olsen, BS, Cori Shollenberger, BS, Natalie Truty, BS, assisted with recruitment and assessments. Joshua Feldmiller, BS, assisted with database coordination.
Funding/Support: Support for this research comes from K23MH086620, K23MH070471, R01MH100095, R01MH085651, P30MH90333, P60MD000207, UL1RR024153, and UL1TR000005 from the National Institute of Mental Health, John A. Hartford Foundation, American Foundation for Suicide Prevention, and the UPMC Endowment in Geriatric Psychiatry.
References
- Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, Uchitomi Y. Suicidality in terminally ill Japanese patients with cancer. Cancer. 2004;100:183–191. doi: 10.1002/cncr.11890. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychol Rev. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. Am J Psychiatry. 1975;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Shuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HLP, Lettieri DJ, editors. The Prediction of Suicide. Bowie MD: Charles Press; 1974. pp. 45–56. [Google Scholar]
- CDC. National Suicide Statistics at a Glance. Centers for Disease Control and Prevention. 2012 [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social Support: Theory, Research and Applications. Springer Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- Costa PT, McCrae RR. The NEO-PI/NEO-FFI manual supplement. Odessa, FL: Psychological Assessment Resources; 1989. [Google Scholar]
- Cukrowicz KC, Cheavens JS, Van Orden KA, Ragain RM, Cook RL. Perceived burdensomeness and suicide ideation in older adults. Psychol Aging. 2011;26:331. doi: 10.1037/a0021836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leo D, Padoani W, Scocco P, et al. Attempted and completed suicide in older subjects: results from the WHO/EURO multicentre study of suicidal behavior. Int J Geriatr Psychiatry. 2001;16:300–310. doi: 10.1002/gps.337. [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Clark L, Reynolds CF, Siegle GJ. Reward signals, attempted suicide, and impulsivity in late-life depression. J Am Med Assoc Psychiatry. 2013;70:1020–1030. doi: 10.1001/jamapsychiatry.2013.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Duberstein PR, Conner KR, Houck PR, Conwell Y. Sex differences in correlates of suicide attempt lethality in late life. Am J Geriatr Psychiatry. 2008;16:905–913. doi: 10.1097/JGP.0b013e3181860034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, et al. Lethal forethought: Delayed reward discounting differentiated high- and low-lethality suicide attempts in old age. Biol Psychiatry. 2011;70:138–144. doi: 10.1016/j.biopsych.2010.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Seidlitz L, Denning DG, Cox C, Caine ED. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J Gerontol Psychol Sci. 2000;55B:18–26. doi: 10.1093/geronb/55.1.p18. [DOI] [PubMed] [Google Scholar]
- Engström G, Alsén M, Gustavsson P, Schalling D, Träskman-Bendz L. Classification of suicide attempters by cluster analysis: A study of the temperamental heterogeneity in suicidal patients. Personal Individ Differ. 1996;21:687–695. [Google Scholar]
- First MS, Gibbon M, Williams JBW. Version 2.0. Biometrics Research Department, New York State Psychiatric Institute; 1995. Structured clinical interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P) [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison KE, Dombrovski AY, Morse JQ, et al. Alone? Perceived social support and chronic interpersonal difficulties in suicidal elders. Int Psychogeriatr. 2010;22:445–454. doi: 10.1017/S1041610209991463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner. Why people die by suicide. Cambridge, MA, US: Harvard University Press; 2005. [Google Scholar]
- Joiner TE, Pettit JW, Walker RL, et al. Perceived burdensomeness and suicidality: Two studies on the suicide notes of those attempting and those completing suicide. J Soc Clin Psychol. 2002;21:531–545. [Google Scholar]
- Joiner TE, Van Orden KA, Witte TK. Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. J Abnorm Psychol. 2009;118:634. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide Life Threat Behav. 2010;40:612–619. doi: 10.1521/suli.2010.40.6.612. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Waterneaux C, Haas GL, Malone KM. Towards a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Meyer B, Pilkonis PA. An attachment model of personality disorders. In: Lenzenweger MF, Clark JF, editors. Major Theories of Personality Disorder. New York, NY: The Guilford Press; 2005. pp. 231–281. [Google Scholar]
- Mieczkowski TA, Sweeney JA, Haas GL, Junker BW, Brown RP, Mann JJ. Factor composition of the Suicide Intent Scale. Suicide Life Threat Behav. 1993;23:37–45. [PubMed] [Google Scholar]
- Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Morse JQ, Pilkonis PA. Screening for personality disorders. J Pers Disord. 2007;21:179–198. doi: 10.1521/pedi.2007.21.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor-Mahomed SB, Schlebusch L, Bosch BA. Suicidal behavior in patients diagnosed with cancer of the cervix. Crisis J Crisis Interv Suicide Prev. 2003;24:168–172. doi: 10.1027//0227-5910.24.4.168. [DOI] [PubMed] [Google Scholar]
- Orden V, Kimberly A, Merrill KA, Joiner TE. Interpersonal-Psychological Precursors to Suicidal Behavior: A Theory of Attempted and Completed Suicide. Curr Psychiatry Rev. 2005;1:187–196. [Google Scholar]
- Pagura J, Cox BJ, Sareen J, Enns MW. Factors associated with multiple versus single episode suicide attempts in the 1990–1992 and 2001–2003 United States national comorbidity surveys. J Nerv Ment Dis. 2008;196:806–813. doi: 10.1097/NMD.0b013e31818b6a77. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pretzer JL, Beck AT. A cognitive theory of personality disorders. In: Lenzenweger MF, Clarkin JF, editors. Major Theories of Personality Disorder. New York, NY: The Guilford Press; 2005. pp. 43–113. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; 2004. [Google Scholar]
- Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R. Self-mutilation and suicidal behavior in borderline personality disorder. J Personal Disord. 1994;8:257–267. doi: 10.1176/ajp.151.9.1316. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J Personal Disord. 2002;16:201–214. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky GD, Golub A, Cromwell EN. Development and validation of the anger rumination scale. Personal Individ Differ. 2001;31:689–700. [Google Scholar]
- Szanto K, Dombrovski AY, Sahakian BJ. Social emotion recognition, social functioning, and attempted suicide in late-life depression. Am J Geriatr Psychiatry. 2012;20:257–265. doi: 10.1097/JGP.0b013e31820eea0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE., Jr Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Lynam ME, Hollar D, Joiner TE., Jr Perceived burdensomeness as an indicator of suicidal symptoms. Cogn Ther Res. 2006;30:457–467. [Google Scholar]
- Van Orden KA, Smith PN, Chen T, Conwell Y. A case controlled examination of the Interpersonal Theory of Suicide in the second half of life. Arch Suicide Res. 2015 doi: 10.1080/13811118.2015.1025121. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Wiktorsson S, Duberstein P, Berg AI, Fässberg MM, Waern M. Reasons for Attempted Suicide in Later Life. Am J Geriatr Psychiatry. 2015;23:536–544. doi: 10.1016/j.jagp.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE., Jr Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Van Orden K, Witte TK, Cukrowicz KC. The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KG, Curran D, McPherson CJ. A burden to others: a common source of distress for the terminally ill. Cogn Behav Ther. 2005;34:115–123. doi: 10.1080/16506070510008461. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


