Abstract
Objectives
The relationship between the silence and voicing accumulations of primary school teachers and the teachers’ clinical status was examined. The goal was to determine whether more voicing accumulations and fewer silence accumulations were measured for the vocally unhealthy subjects than for the healthy subjects, which would imply more vocal loading and fewer short-term recovery moments.
Methods
26 Italian primary school teachers were allocated by clinicians to three groups: (1) with organic voice disorders, (2) with subjectively mild organic alteration and/or functional voice symptoms, and (3) normal voice quality and physiology. Continuous silence and voicing periods were measured with the APM3200 during the teachers’ 4-hour workdays. The accumulations were grouped into 7 time intervals, ranging from 0.03–0.9 s to 3.16–10 s, according to Italian prosody. The effects of group on silence and voicing accumulations were evaluated.
Results
Regarding silence accumulations, Group 1 accumulated higher values in intervals between 0.1 and 3.15 s than other groups, while Groups 2 and 3 did not differ from each other. Voicing accumulations between 0.17 and 3.15 s were higher for subjects with a structural disorder. A higher time dose was accumulated by these subjects (40.6%) than other subjects (Group 2, 31.9%; Group 3, 32.3%).
Conclusions
While previous research has suggested that a rest period of a few seconds may produce some vocal fatigue recovery, these results indicate that periods shorter than 3.16 s may not have an observable effect on recovery. The results provide insight into how vocal fatigue and vocal recovery may relate to voice disorders in occupational voice users.
Keywords: Silence and voicing accumulations, Occupational voice users, Teachers, Voice disorders, Vocal fatigue recovery
I. INTRODUCTION
Voice disorders can be defined as conditions involving a variety of pathological symptoms that range from a mild disturbance of voice quality to complete loss of the ability to produce a laryngeal voice.1 Such disorders are regularly experienced by occupational voice users because of the demands placed on the voice. Internationally, teachers comprise one of the occupational categories most affected by voice disorders.2–9 In Italy, Angelillo et al.7 found that 60.1% of 504 teachers reported suffering from voice problems, while, in Brazil and Spain, studies employing laryngoscopic examinations reported high rates of prevalence in teachers (9.7% and 13%, respectively).8–9 Despite the international prevalence of these problems, the occupational health and safety protocols for individuals in these professions are poorly developed.10
The overuse of the voice by professional voice users is known to cause physiological vocal fatigue.11–12 The vocal load of teachers,13–14 which can be quantified as the amount of voicing performed by speakers over time, has been characterized in the context of several time dose studies, where time dose (Dt) refers to the time the vocal folds spend vibrating. Masuda et al.15 measured a mean phonation time of 21.5% for elementary teachers and patients with vocal fold nodules over 8 h of work, while Bottalico and Astolfi16 found a mean voicing time percentage of 26% for primary school female teachers over a 4 h work period. With regard to recovery, Hunter and Titze12 characterized a complete long-term recovery time on the basis of perceptual ratings on a 12 to 18 h period after a 2 h oral reading. The minimum silence period for tissues to experience any degree of short-term recovery has not yet been established.
In their study of vocal load and recovery, Titze et al.17 investigated the distributions of silence and voicing periods in a typical teacher’s workday using an accelerometer that was placed at the base of the subject’s neck. From these data, the accumulation of each period was then obtained, in seconds, by multiplying the number of occurrences by the corresponding duration. The occurrences and the accumulations of silence and voicing periods were grouped into bin durations of half a decade of logarithmic time, according to English prosodic units and the results showed that the greatest accumulation of voicing periods at work occurred in the 0.316–1.0 s range, and the greatest accumulation of silence, in the 3.16–10 s range. In their study, the authors compared the vocal behavior of teachers at-work and not at–work and argued that at-work vocal fatigue might be related to the greatest accumulation of voicing periods, while the greatest accumulation of silence periods could be related to short-term vocal recovery.18–19
The question of how silence and voicing accumulations may differ between people with and without voice disorders is an open field of research. Many studies have supported the claim that respiratory behavior differs between people with and without voice disorders. Some of these studies have also investigated the differences in the speaking rate between subjects with normal and disordered voices but no definite conclusions have been drawn.
There is evidence that normal and disordered voices differ in glottal airflow and vibration patterns. According to Gordon et al.,20 glottal vibration pattern irregularities or incomplete closure of the glottis, which can lead to higher glottal airflow, are often present in subjects with voice disorders. Hyperfunctional voice production, in particular, has been characterized by disrupted inspiratory and expiratory cycles of tidal volume breathing and decreased phonation durations. Both women and children with vocal fold nodules have been observed to speak with higher glottal airflow than female and child talkers with normal voice production.21 Sapienza et al.22 found that alternating glottal airflow, defined as the amount of airflow from the maximum peak to the minimum valley of the glottal airflow waveform, was significantly higher for the disordered group than the normal voice group. In a subsequent study, Sapienza et al.23 demonstrated that both the glottal airflow and the volume of air expended per syllable and per utterance during reading tasks were greater for 10 female talkers with vocal nodules than for 10 age, weight and height matched controls. In both studies conducted by Sapienza and colleagues,22–23 it was hypothesized that the speech breathing patterns associated with disordered speakers reflected a compensatory strategy to maintain a constant subglottal pressure despite the loss of airflow during voicing.
Subjects with vocal fold nodules may have shorter periods of inhalation than healthy subjects. Iwarsson and Sundberg24 found that six female subjects with nodules had shorter durations of inhalations than 14 healthy controls.
There is some evidence for the claim that talkers with dysphonia have longer voicing periods than healthy subjects. Masuda et al.15 demonstrated than talkers with vocal fold nodules have longer phonation times. Watts and Awan25 measured vocalization time as the duration from vocal onset to vocal offset across two speech segments, each consisting of four syllables extracted from readings of CAPE-V sentences. They found that dysphonic speakers’ productions were associated with longer vocalization periods than non-dysphonic (normal) speakers.
In the present study, silence and voicing accumulations were measured in primary school teachers during the workday and were related to the clinicians’ evaluation of the subjects. The primary aim of the work is to identify and characterize the differences in the silence and voicing accumulations of teachers with and without structural voice disorders. The intention is to improve the understanding of the differences in speech behavior between unhealthy and healthy teachers, and in particular, the understanding of the distribution of unhealthy teachers’ silence periods, which relate to short-term recovery, and the understanding of what constitutes an unhealthy occupational dose of voicing. It was predicted in the present study that, during the workday, teachers with structural voice disorders would show (1) higher silence accumulations in shorter bins and lower silence accumulations in longer bins than teachers without such disorders, and (2) higher voicing accumulations than teachers without such disorders.
II. EXPERIMENTAL METHOD
The case studies concern 26 teachers at 7 primary schools in Italy: 14 teachers in 4 schools in Turin, which were built at the end of the nineteenth century, and 12 teachers in 3 schools in Beinasco, which were built in the 1970s. The subjects voluntarily undertook both the monitoring during lessons and the medical examinations. All subjects were native Italian speakers and traditional teachers (who teach classes of 20 to 30 pupils), with a mean age of 44.7 years (range 31–59). Teachers were monitored over 1 or 2 workdays. In Italy a teacher‘s active teaching workday is 4 h long (continuous). The pupils’ ages ranged between 6 and 11 years. A total of 43 workday samples were collected and all samples were included in the analyses. Table I reports the gender and age of the teachers and the number of monitored workdays. Special aid teachers were excluded from the study because their vocal load per day is substantially different from traditional teachers.
Table I.
Characteristics of the investigated teachers, objective evaluation of the vocal folds and larynx by means of VLS and the subdivision into groups proposed by a team of speech pathologists and medical doctors.
| Subject | Gender | Age | Number of monitored workdays |
Subject taught |
Self-reported hearing condition |
VLS | Group |
|---|---|---|---|---|---|---|---|
| 1 | Female | 37 | 1 | Math | No | nodules | 1 |
| 2 | Female | 34 | 1 | Math | No | nodules | 1 |
| 3 | Female | 42 | 1 | Italian | - | nodules and cysts | 1 |
| 4 | Female | 54 | 1 | Italian | Yes | bilateral nodules | 1 |
| 5 | Female | 54 | 2 | Italian | No | normal physiology | 2 |
| 6 | Female | 49 | 1 | Italian | Yes | hypercontraction | 2 |
| 7 | Male | 59 | 2 | Italian | No | vocal fold hyperemia | 2 |
| 8 | Male | 43 | 2 | Math | No | normal physiology | 2 |
| 9 | Female | 58 | 2 | Italian | No | normal physiology | 2 |
| 10 | Female | 33 | 2 | Math | No | normal physiology | 2 |
| 11 | Female | 40 | 2 | Math | No | hypercontraction | 2 |
| 12 | Female | 47 | 1 | Italian | - | normal physiology | 2 |
| 13 | Female | 54 | 2 | Italian | Yes | vocal fold hyperemia | 2 |
| 14 | Female | 43 | 2 | Italian | No | hypotonia | 2 |
| 15 | Female | 58 | 1 | Math | No | normal physiology | 2 |
| 16 | Female | 34 | 2 | Math | No | normal physiology | 3 |
| 17 | Female | 55 | 2 | Math | No | normal physiology | 3 |
| 18 | Female | 52 | 2 | Math | No | normal physiology | 3 |
| 19 | Female | 38 | 2 | Math | No | normal physiology | 3 |
| 20 | Female | 56 | 2 | Italian | Yes | normal physiology | 3 |
| 21 | Female | 34 | 2 | Italian | - | normal physiology | 3 |
| 22 | Female | 39 | 2 | English | No | normal physiology | 3 |
| 23 | Female | 35 | 1 | Italian/ Math | No | hypercontraction | 3 |
| 24 | Female | 31 | 1 | Italian | No | normal physiology | 3 |
| 25 | Female | 40 | 2 | Italian | Yes | hypercontraction | 3 |
| 26 | Female | 38 | 2 | English | Yes | normal physiology | 3 |
Group 1 consists of subjects with structural voice disorders, Group 2, subjects with subjectively or functionally reported symptoms, and Group 3, with normal physiology.
Math = Mathematics.
The acoustic conditions in the classrooms covered a wide range of reverberation times; the average values of mid-frequency reverberation time ranged between 0.6 s to 1.5 s in occupied conditions. The average background noise level, which did not differ significantly among the classrooms, was 50.6 dB(A). Acoustic conditions in the classrooms during phonation are reported by Bottalico and Astolfi.16
A. Clinical examinations
The teachers underwent clinical examinations, which were performed by a team of logopedists and phoniatricians, as described by Astolfi et al.26 and Vallino.27 The examinations consisted of (1) a self-report of voice use, (2) a medical history (anamnesis), (3) an objective logopedic evaluation, and (4) a vocal health examination, which included instrumental examinations and videolaryngostroboscopy (VLS).
The self-evaluation survey used was the Voice Handicap Index; specifically the VHI-10. This is a validated instrument designed to assess patients’ self-perceived emotional, physical, and functional effects relative to their voice dysfunction. The medical history was obtained following the indication of Accordi and Tesserin.28 It consists of (1) anamnesis of family (genetic predisposition), (2) physiologic anamnesis (social and professional behavior related to the voice use), (3) past or remote pathologic anamnesis (allergies and inflammation of the airways, lung diseases, gastrointestinal diseases, a record of surgery with consequences for phonation, medicine consumption with collateral effects on phonation, neurological diseases), (4) recent pathological anamnesis including subjective sensations about phonation and recorder at vocal apparatus level. The objective logopedic evaluation was obtained following the indication of Vernero et al.29 It consists of (1) evaluation of the anatomical structures involved in resonance (nose, lips, tongue, tonsils, etc.), (2) evaluation of respiration (evaluation of diaphragmatic-abdominal breathing, costal-diaphragmatic breathing, sternocostal breathing and clavicular breathing), (3) muscles tone evaluation (face-neck and thorax-abdomen), (4) perceptual evaluation of the voice by means of the GIRBAS Scale.
After medical examination, the logopedists and phoniatricians, who had clinical expertise (particularly with respect to diagnosis), evaluated the severity of the disorder, or the likelihood of the subject developing a disorder. Subsequently, the team of clinicians assigned subjects to the following groups: (1) 4 subjects (15.4%) with organic voice disorders that were detected both subjectively and objectively, with indications for therapy and speech treatment; (2) 11 subjects (42.3%) with subjectively mild organic alteration and/or functional voice symptoms, with indications for the provision of vocal hygiene information and preventative speech treatment; and (3) 11 subjects (42.3%) with normal voice quality and physiology. Approximately 42% of the examined subjects showed no sign of voice disorders, while 58% presented with voice disorders. These proportions are similar to those reported by Angelillo et al.7
As far as the objective evaluation of the vocal folds and larynx by means of VLS was concerned, 15 subjects were normally functioning (“normal physiology”), 4 presented different types of muscle hypercontraction (detected during the VLS), 2 presented with hyperemia (inflammation), 1, hypotonia, and 4 subjects presented with nodules and/or cysts. Two of the subjects in the third group presented with a form of hypercontraction; however, it was a mild hypercontraction of extra laryngeal muscle. No other anomalies were detected during other parts of the examination (perceptual evaluation of the voice by means of the GIRBAS Scale, evaluation of the anatomical structures involved in the resonance, evaluation of the respiration, muscle tone evaluation, etc.). For this reason, the clinicians assigned these teachers to the third group. Subjects were asked to report whether they had a hearing disorder; however, no hearing tests were performed. Subjects were representative of the general teaching population, according to the percentage of Italian teachers suffering from voice problems.7
Some characteristics of the investigated teachers (gender, age, number of monitored workdays, subject taught, self-reported hearing status), objective evaluation of the vocal folds and larynx by means of VLS and the subdivision into groups proposed by the clinicians are reported per subject in Table I.
B. Measurements of silence and voicing accumulations
Each teacher was supplied with the Ambulatory Phonation Monitor (APM, model 3200, KayPENTAX®, Montvale, NJ). This device consists of an accelerometer, which was positioned below the talker’s glottis at the sternal notch, and an acquisition unit that processed the accelerometer signal. The APM 3200 provided a time-history with a frame length of 50 ms. This time-history comprised the fundamental frequency, fo, and an estimation of the sound pressure level, SPL, at a distance of 15 cm on-axis from the speaker’s mouth, obtained after a calibration. The calibration was carried out by means of a reference microphone in order to correlate the skin acceleration level with the SPL.
Of the information provided by the device, only the detection of the presence or absence of voice excitation is of interest for the present study. Voiced and unvoiced frames were discriminated by the APM. When the RMS level acquired by the transducer exceeded a preset threshold, the frame was designated as voiced, and for that frame, fo and SPL were determined.30 Otherwise, the output result was equal to 0. The level acquired by the transducer was not affected by environmental noise. Silence and voicing accumulations, as defined in Sec. I, were derived from the time-histories provided by the APM.
The occurrences of continuous silence and voicing periods from 0.05 s to 10 s with a step of 50 ms were obtained from APM time histories. Subsequently, the accumulations for each time step were calculated by multiplying the occurrences by the corresponding step duration and divided by the total time of the monitoring. In this way, the accumulation values are reported in seconds per hour, compensating for eventual differences in monitoring time among teachers.
The accumulation values were grouped into bins according to Italian prosodic units,31–32–33 as reported in Table II. Seven bins were used for the accumulations as follows: (Bin 1) 0.03–0.9 s long (silence and voicing periods below and up to the phonemic or segmental level); (Bin 2) 0.1–0.16 s long (at the level of unstressed syllables); (Bin 3) 0.17–0.33 s long (at the level of stressed syllables); (Bin 4) 0.34–0.66 s long (s at the word level); (Bin 5) 0.67–1.31 s long (at the non-terminal unit level); (Bin 6) 1.32 –3.15 s long (at the short tone unit level); (Bin 7) 3.16 – 10 s long (at the long tone unit level). Examples can be found elsewhere.33
Table II.
Bin subdivision according to Italian prosodic units.
| Bin 1 | Bin 2 | Bin 3 | Bin 4 | Bin 5 | Bin 6 | Bin 7 | |
|---|---|---|---|---|---|---|---|
| Time Interval [s] | 0.03–0.09 | 0.1–0.16 | 0.17–0.33 | 0.34–0.66 | 0.67–1.31 | 1.32 –3.15 | 3.16 –10 |
|
Voicing and Silence Period Correspondences |
below and up to the phonemic segmental level |
unstressed syllable level |
stressed syllable level |
word level | non- terminal unit level |
short tone unit level |
long tone unit level |
In addition, in order to better compare the results of the current study with Titze et al.,17 a secondary analysis of the data was conducted in which the silence and voicing accumulations were allocated to bins in agreement with the bin widths specified by Titze et al.17 Specifically, the 6 bins used were as follows: (1) silence and voicing periods below and up to the phonemic segmental level (0.0316–0.10) s; (2) silence and voicing periods at the phonemic and syllabic level (0.10–0.316) s; (3) silence and voicing periods at the word and sentence level (0.316–1.0) s; (4) all-voiced sentences and pauses between sentences (1.0–3.16) s; (5) sustained phonations and pauses between sentences (3.16–10) s; (6) rare long phonations and silences in a dialogue (10–31.6) s. The longest bins were not considered because there were no accumulations in those bins by the subjects of the present study.
C. Statistical procedures
Statistical analysis was conducted in R 3.1.2.34 For both types of accumulation, non-linear (polynomial) multiple regression models were fitted with Bins as the polynomial term and with subject as a random effect. For the silence accumulations, the model was fit with the response variable of silence accumulations and a 3rd order polynomial term for Bins. For the voicing accumulations, the model was fit with a 2nd order polynomial term, Bins, in an interaction with the term, Group, and the main effect, Group. Bins were treated as a continuous variable for the purposes of readily interpretable models. Before fitting the final models, the main effect of Group on silence or voicing accumulations was tested in univariate regression models. In the case of the silence accumulations, the main effect of Group was associated with a p value > 0.1, so was excluded from the final model. In the case of the voicing accumulations, the main effect of Group was associated with a p value < 0.1, so was included in the final model.
The final models were determined to be appropriate on the basis of parameter distribution estimations, data visualization, Likelihood Ratio Tests (LRTs) and the R-squared (an assessment of the goodness of fit). To evaluate the significance of a term (a predictor variable in this case), models were fit with and without the term, and a LRT was applied to the full and reduced models. The test is based on the likelihood ratio, which expresses how many times more likely the data are under one model than the other; if the difference is significant, the model with more terms is preferred over the model with fewer terms. In this paper, the reported output of the LRT comprises a Chi-square value, X2, and p values calculated from the X2 distribution with degrees of freedom (df) equal to the difference in the number of parameters in the models being compared.
The concept of Normalized Error35 was adopted for the analysis of compatibility between two sets of data, those reported in the present study, and those reported by Titze et al.,17 which were obtained in different conditions, where no value(s) could be taken as the reference value(s). This test is used to determine whether the difference in the compared models is due to an effective difference between the evaluated phenomena or to systematic effects, rather than to random effects. The Normalized Error, EN, is calculated as the ratio between the absolute value of the difference between the two samples mean and the relative expanded uncertainty of the difference,36 according to the following formula:
| (2) |
where m1 and m2 represent the average values of the two samples, s1 and s2 represent the standard deviations of the two samples and k is the coverage factor, calculated as the Student-t value for a conventional risk of error α of 5% and a number of degrees of freedom corresponding to n−2, where n is the number of samples used. This analysis can be considered a particular kind of hypothesis test. If the EN value is higher than unity, the difference between the two sample means, m1 and m2, is higher than its uncertainty. Therefore, the difference is not merely due to random effects and the two results can be considered incompatible. Alternatively, if EN is lower than unity, the difference could be due to random effects and there is no reason to reject the hypothesis of compatibility. Values lower than unity do not mean that real differences or systematic effects are not present, but rather that random effects cover their presence.
III. RESULTS AND DISCUSSION
A. Silence and voicing accumulations during the workday
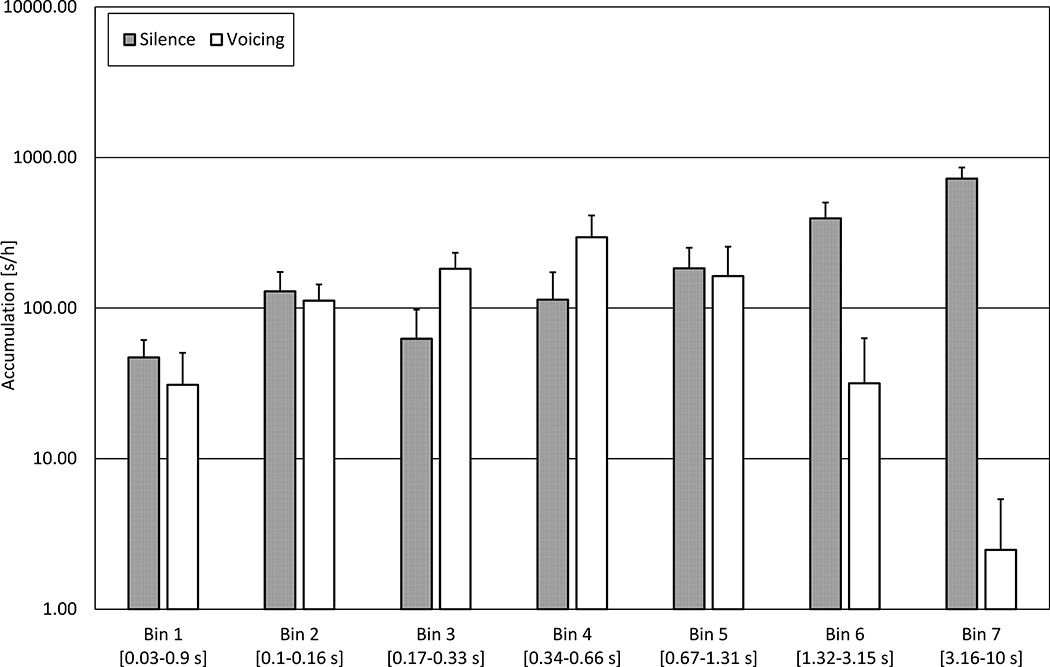
Figure 1 shows the average values of silence and voicing accumulations in seconds per hour (s/h) for each bin for the 26 subjects over the 43 workdays. Collectively, the data in Figure 1 represent 164.0 h of measurement. An average of 3.81 h per workday was measured, during which time the subjects were teaching pupils in a classroom. The average silence accumulation values were 47.0 s/h (Bin 1), 129.2 s/h (Bin 2), 62.5 s/h (Bin 3), 113.6 s/h (Bin 4), 184.0 s/h (Bin 5), 394.0 s/h (Bin 6) and 724.2 s/h (Bin 7). The peak of the silence distribution was in Bin 7 (3.16–10) s, which corresponds to silence periods at the long tone unit level. Average voicing accumulations were 30.9 s/h (Bin 1), 112.0 s/h (Bin 2), 182.4 s/h (Bin 3), 295.9 s/h (Bin 4), 162.9 s/h (Bin 5), 31.7 s/h (Bin 6) and 2.5 s/h (Bin 7). The greatest accumulation of voicing was found for Bin 4 (0.34–0.66) s, i.e., the word level.
FIG. 1.
Ensemble averages over 42 workdays of silence (in grey) and voicing (in white) accumulations per bin in seconds per hour with the standard error (SE) shown. The x-axis is bins corresponding to Italian prosodic units. The y-axis is accumulations in seconds per hour on a logarithmic scale.
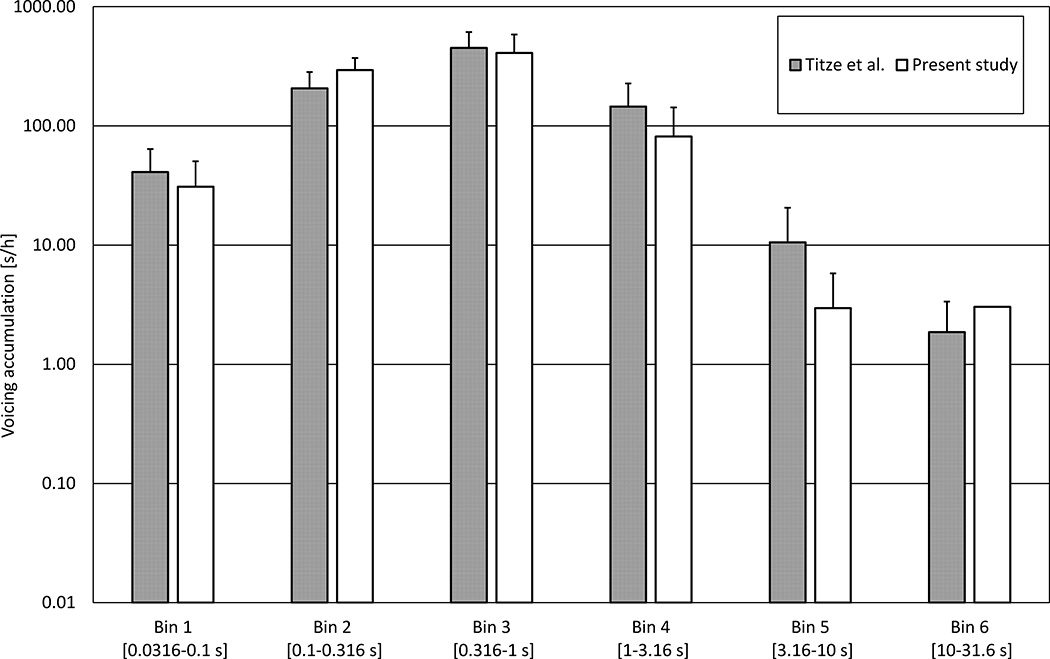
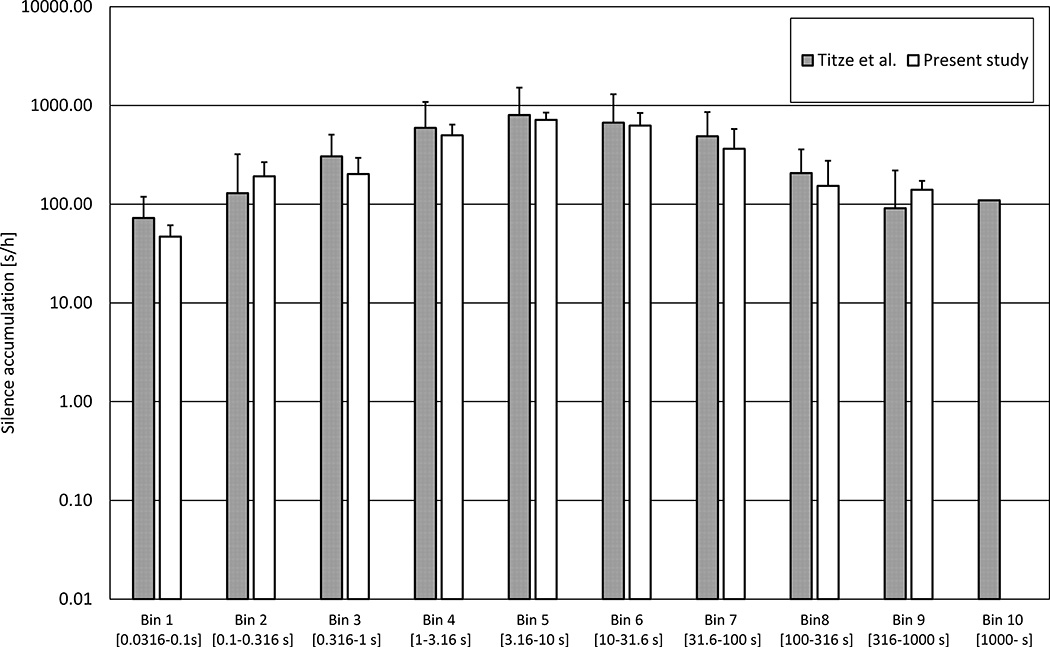
The results of the current study were compared to those of Titze et al.17 Figures 2 and 3 present a comparison of the silence and the voicing accumulation values obtained by Titze et al.17 and the results obtained in the present study. Titze et al.17 found that the peak of the silence distribution was in Bins 5–6. The 3.16–31.6 s silence periods in Bins 5 and 6, which are typical of dialogue turn taking, were associated the greatest amount of accumulated vocal rest. The greatest accumulation of voicing at work time (45 s/h) was found for the word and sentence level, i.e., Bin 3 (0.316–1.0) s. In Figures 2 and 3, the accumulations obtained in the current study are reported in seconds per hour on a logarithmic scale and the bin widths are identical to those of Titze et al.17 In order to test the compatibility between the two studies, the Normalized Error values pertaining to the silence and voicing accumulations per Bin were calculated. All values were lower than one. In other words, the difference could be due to random effects and there is no reason to reject the hypothesis of compatibility. In sum, although their subjects taught a wider range of grades (from K to 12th grade), which may involve different noise levels in the classroom, the results of Titze et al.17 are compatible with those of the present study.
FIG. 2.
Barplots comparing the silence accumulation results of the present study (in white) with those reported by Titze et al.17 (in grey). The x-axis is accumulations assigned to logarithmic bins widths as specified by Titze et al.17 The y-axis is silence accumulations in seconds per hour on a logarithmic scale, with SD shown by error bars.
FIG. 3.
Barplots comparing the voicing accumulation results of the present study (in white) with those reported by Titze et al.17 (in grey). The x-axis is accumulations assigned to logarithmic bins widths as specified by Titze et al.17 The y-axis is silence accumulations in seconds per hour on a logarithmic scale, with SD shown by error bars.
B. Silence and voicing time percentages
On the basis of the accumulation distributions, the average percentage of the total monitoring time that the subjects spent in each bin was calculated for silence and voicing. With regard to silence periods, they spent 1.9% of the total time in Bin 1 (below and up to the phonemic segmental level), 5.2% in Bin 2 (unstressed syllable level), 2.5% in Bin 3 (stressed syllable level), 4.6% in Bin 4 (word level), 7.4% in Bin 5 (non-terminal unit level), 15.9% in Bin 6 (tone unit level) and 29.3% in Bin 7 (long tone unit level). With regard to voicing periods, they spent 1.2% of the total time in Bin 1, 4.5% in Bin 2, 7.4% in Bin 3, 12.0% in Bin 4, 6.6% in Bin 5, 1.3% in Bin 6 and 0.1% in Bin 7.
The trends in the accumulations are comparable with the findings for Swedish speakers of Löfqvist and Mandersson.37 They measured a silence percentage of 15% for unvoiced segments, which is almost identical to the 14.2% measured in the present study (considering the first 4 bins, up to the word level). Löfqvist and Mandersson37 found that in read monologues the voicing percentage was approximately 50%, and the silence percentage was 35% for boundary pauses. In the present analysis, the speech samples were not monologues but a mixture of monologue and dialogue. Consequently, the voicing percentage was lower (33.1%), with a higher percentage of boundary pauses (52.7%) due to the dialogue component. Boundary pauses were associated with Bins 5, 6 and 7, i.e., periods longer than the word level.
The voicing percentage reported in the present study (33.1%) is similar to those obtained by Hunter and Titze,38 in whose study 57 teachers were monitored over 2 weeks. The authors found that teachers vocalized for 29.9% of the occupational time, on average.
C. Effect of clinical status on accumulations
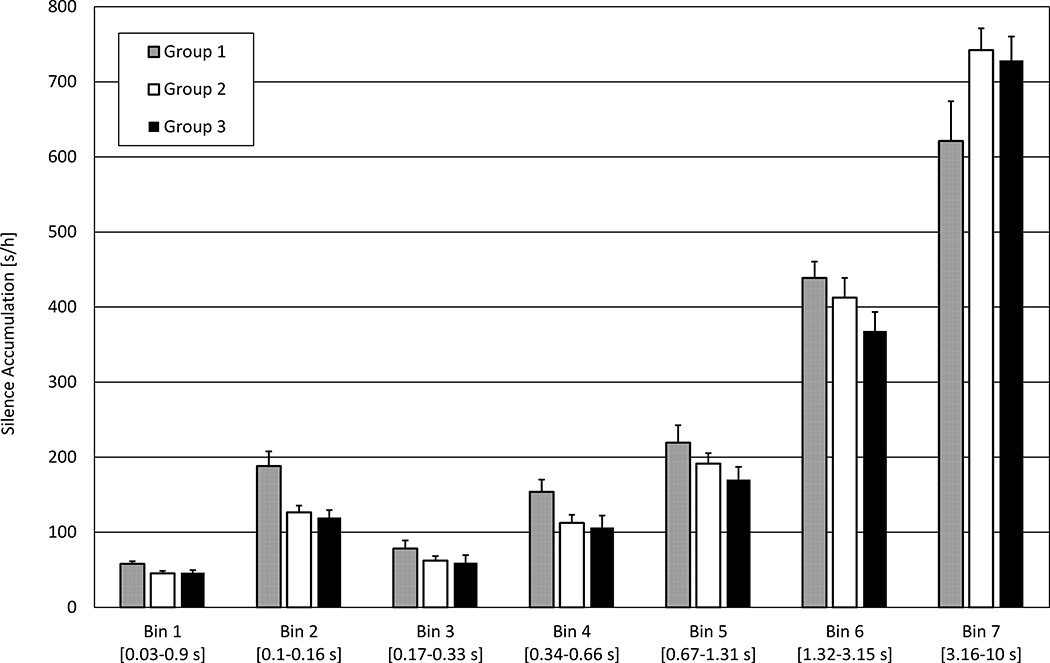
The effect of group on silence and voicing accumulations is shown in Figures 4 and 5, respectively. With regard to the polynomial regression model for silence accumulations, there was a significant interaction of Group and 3rd order polynomial term Bins (X2(9) = 716.17, p < 0.0001; when compared with the null model). The R-squared was equal to 0.93. Group 1 tended to be associated with higher values in all Bins except Bin 7. In the case of Bin 7 (involving periods of ≥ 3.16 s), there were lower values for Group 1 than for Groups 2 and 3.
FIG. 4.
Mean silence accumulations per group (Group 1 in grey, Group 2 in white, Group 3 in black) in seconds per hour with SD indicated by error bars. Group 1 consists of subjects with structural voice disorders, Group 2, subjects with subjectively or functionally reported symptoms, and Group 3, with normal physiology. The x-axis is bins corresponding to Italian prosodic units. The y-axis is silence accumulations in seconds per hour on a linear scale.
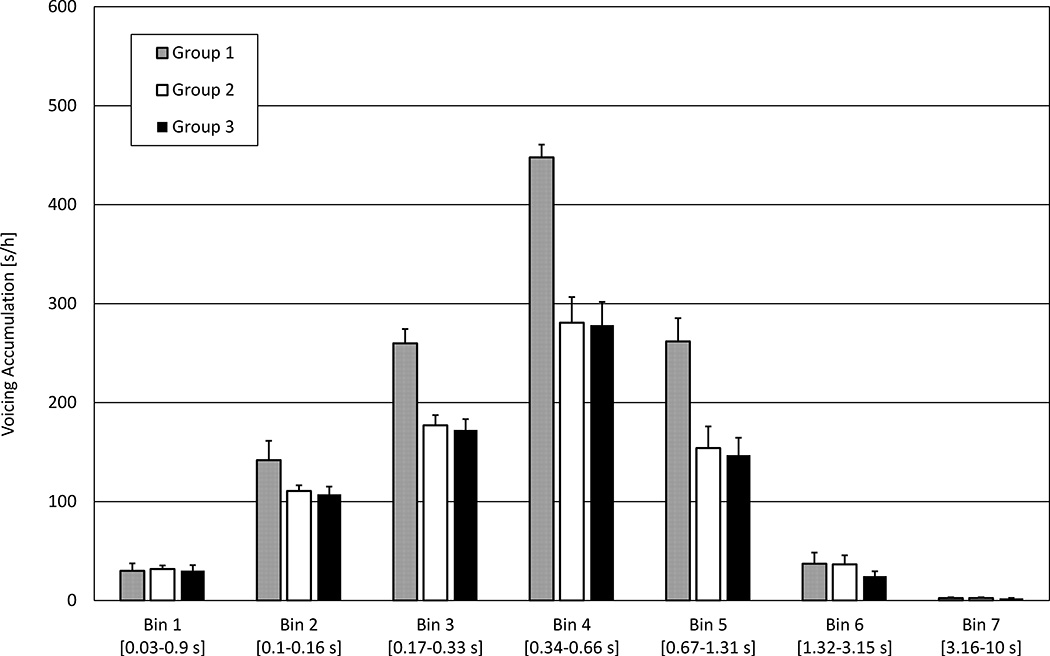
FIG. 5.
Mean voicing accumulations per group (Group 1 in grey, Group 2 in white, Group 3 in black) in seconds per hour with SD indicated by error bars. Group 1 is the group with structural voice disorders, group 2 comprises the subjects with reported symptoms, and group 3 is the group with normal physiology. The x-axis is bins corresponding to Italian prosodic units. The y-axis is voicing accumulations in seconds per hour on a linear scale.
With regard to the polynomial regression model for voicing accumulations, there was a significant interaction of 2nd order polynomial term Bins, and Group (X2(4) = 15.01, p < 0.01; when compared with the same model but without the interaction), and a main effect of Group (X2(2) = 10.01, p < 0.01; when compared with a model without Group as a main effect). The model indicated that Group 1 was associated with significantly higher values than Groups 2 and 3 (Groups 1:2, β̂ = −52.21, SE = 17.66, t = −3.0, p < 0.01; Groups 1:3, β̂ = −56.11, SE = 17.59, t = −3.19, p < 0.01). The R-squared was equal to 0.65. Group 1 was associated with higher values especially in Bins 3 to 6.
The finding of higher silence accumulations for the subjects with structural disorders in Group 1, with the exception of the longest bin, may relate to the respiratory and laryngeal functioning of such subjects. The respiratory behavior of these subjects can be considered from two points of view: (1) as a cause of pathology because a tendency towards shallow and quick breathing has been associated with vocal fold nodules,24 apnea and muscle tension, and, anecdotally, patients with voice disorders often complain of breathlessness,23 and (2) as an effect of pathology because dysfunction in vocal fold adduction due to nodules (incomplete closure) can result in higher glottal airflow during phonation.21–23
As mentioned, subjects with structural voice disorders (Group 1) were associated with higher voicing accumulations, especially in bins 3 to 6. The overall accumulation of Dt was higher in Group 1 than in other groups (Group 1, 40.2%; Group 2, 31.9%; Group 3, 32.3%). It can be argued on the basis of these results that teachers with structural voice disorders accumulate longer voicing periods than teachers without such disorders. This result is consistent with the findings of Watts and Awan25 for dysphonic vs. healthy speakers. Vocal abuse is generally regarded to be the main cause of vocal fold nodules. Hence, as discussed in Section I, the vocal behavior of persons with long phonation times could be considered a risk factor in vocal abuse.15
The present results indicate an increase of 54.9% in the voicing accumulations for Group 1 (subjects with organic voice disorders) relative to Group 3 (normal voice quality and physiology), and an increase of 4.1% for Group 2 (subjectively mild organic alteration and/or functional voice symptoms) relative to Group 3.
Titze et al.17 recognized that it is necessary to determine what rest period duration has a profound effect on vocal fatigue recovery. In the present study, as far as rest periods < 3.16 s were concerned, subjects with structural voice disorders tended to display higher overall silence accumulations than others. The silence accumulations reported in this paper represent the accumulation of vocal rest during the workday. Hence, the results of this study indicate that rest periods shorter than 3.16 s may not have an observable effect on vocal fatigue recovery. With regard to rest periods ≥ 3.16 s, subjects with structural voice disorders showed lower silence accumulations than subjects without such disorders. In this case, lower silence accumulations could indicate an inadequate redistribution of fluids in the vocal fold tissue.19 It is feasible that this result may indicate an inadequate recovery time, which could lead to pathology.
IV. CONCLUSIONS
The primary aim of this study was to identify and characterize the differences among the distributions of silence and voicing periods during the workday for 26 primary school teachers with and without structural voice disorders. Durations of continuous voicing and silence periods were calculated in 50 ms frames and assigned to bins grouped according to Italian prosodic units. Silence and voicing accumulations were calculated as a product of the occurrence (statistical frequency) and these periods. The teachers underwent a thorough clinical examination and were assigned to three groups: (1) subjects with organic voice disorders that were detected both subjectively and objectively; (2) with subjectively mild organic alteration and/or functional voice symptoms; and (3) subjects with normal voice quality and physiology. The effect of group on the silence and voicing accumulations was evaluated.
The highest peak of voicing occurred at 0.316 – 1 s (word and phrase boundary level, on the analysis of Titze et al., 2007) and of silence, at 3 – 10 s (pause between sentences, again, on the analysis of Titze et al., 2007). Subjects with moderate voice disorders were associated with higher silence accumulations in the central bins, and lower silence accumulations in the longest bin, and higher voicing accumulations, especially in the central bins, than subjects without such disorders, consistent with the predictions discussed in Section I. While previous research has suggested that a rest period of a few seconds may cause some recovery from vocal fatigue, these results indicate that periods shorter than 3.16 s may not have an observable effect on recovery time, which phenomenon could lead to pathology.
A relationship was observed between clinical status and Dt. Higher Dt was accumulated by subjects with moderate voice disorders (40.6%) than other subjects (Group 2, 31.9%; Group 3, 32.3%).
The limitations of this paper include an imbalance in the sample sizes for the three groups, which was due to the voluntary nature of participation in the study and the fact that the clinical examination was conducted after subject selection and monitoring. Nevertheless, the proportions of subjects in the three groups in this study are likely to be representative of the proportions in the population.7–8–9 In future work, clinical evaluation will be conducted prior to subject selection.
Acknowledgments
The kind cooperation of the teachers, children and school administrators has made this work possible. Thanks are due to L. Pavese for assistance in the initial stages of the analysis and to L. Hunter for editing assistance, and to T. Nesci, C. Marello, A. Romano and M. Moneglia for their scholarship in the area of Italian prosody. We are also grateful to have had the opportunity to collaborate with Clinic 1 ORL, Department of Surgical Sciences, University of Turin. Thanks are due especially to Doctors C. Giordano, A. Accornero, M. Garzaro, J. Nadalin, G. Pecorari, M. Garzaro, and L. Raimondo. In addition, the authors express their gratitude to those who provided comments and suggestions on an early version of this work, which was presented at the Fall 2014 meeting of the Acoustical Society of America. Analysis reported in this publication was partially supported by the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health under Award Number R01DC012315. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hillman R. Improving the assessment and treatment of voice disorders: Emerging technologies. Proceedings of From Sound to Sense. 2004 [Google Scholar]
- 2.Titze I, Lemke J, Montequin D. Populations in the U.S. Workforce Who Rely on Voice as a Primary Tool of Trade: A Preliminary Report. Journal of Voice. 1997;11(3):254–259. doi: 10.1016/s0892-1997(97)80002-1. [DOI] [PubMed] [Google Scholar]
- 3.Comins D. Survey of UK voice clinics 2001/2. Voice Care Network UK. 2002 [Google Scholar]
- 4.Roy N, Merrill RM, Thibeault S, Parsa RA, Gray SD, Smith EM. Prevalence of voice disorders in teachers and the general population. J. Speech Lang. Hear. Res. 2004;47(2):281–293. doi: 10.1044/1092-4388(2004/023). [DOI] [PubMed] [Google Scholar]
- 5.Kooijman PG, De Jong FI, Thomas G, Huinck W, Donders R, Graamans K, Schutte HK. Risk factors for voice problems in teachers. Folia Phoniatr. Logop. 2006;58(3):159–174. doi: 10.1159/000091730. [DOI] [PubMed] [Google Scholar]
- 6.Sliwinska-Kowalska M, Niebudek-Bogusz E, Fiszer M, Los-Spychalska T, Kotylo P, Sznurowska-Przygocka B, Modrzewska M. The prevalence and risk factors for occupational voice disorders in teachers. Folia Phoniatr. Logop. 2006;58(2):85–101. doi: 10.1159/000089610. [DOI] [PubMed] [Google Scholar]
- 7.Angelillo M, Di Maio G, Costa G, Angelillo N, Barillari U. Prevalence of occupational voice disorders in teachers. J. Prev. Med. Hyg. 2009;50:26–32. [PubMed] [Google Scholar]
- 8.Filho M, Gomez FG, Macedo C. Proceedings of First World Congress of Voice. Oporto, Portugal: 1995. Videolaryngostroboscopy for pre-admissional examination of school teachers. [Google Scholar]
- 9.Urrutikoetxea A, Ispizua A, Mantellanes F, Aurrekoetxea J. Proc. First World Congress Voice. Oporto, Portugal: 1995. Prevalence of vocal nodules in teachers. [Google Scholar]
- 10.Villkman E. Voice problems at work: A challenge for occupational safety and health arrangement. Folia Phoniatr. Logop. 2000;52(1–3):120–125. doi: 10.1159/000021519. [DOI] [PubMed] [Google Scholar]
- 11.Welham NV, Maclagan MA. Vocal Fatigue: Current Knowledge and Future Directions. J. Voice. 2003;17(1):21–30. doi: 10.1016/s0892-1997(03)00033-x. [DOI] [PubMed] [Google Scholar]
- 12.Hunter EJ, Titze IR. Quantifying vocal fatigue recovery: dynamic vocal recovery trajectories after a vocal loading exercise. The Annals of otology, rhinology, and laryngology. 2009;118(6):449. doi: 10.1177/000348940911800608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buekers R, Bierens E, Kingma H, Marres EHMA. Vocal load as measured by the voice accumulator. Folia Phoniatrica et Logopaedica. 1995;47(5):252–261. doi: 10.1159/000266359. [DOI] [PubMed] [Google Scholar]
- 14.Gaskill CS, O’Brien SG, Tinter SR. The effect of voice amplification on occupational vocal dose in elementary school teachers. Journal of Voice. 2012;26(5):667.e19–667.e27. doi: 10.1016/j.jvoice.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Masuda T, Ikeda Y, Manako H, Komiyama S. Analysis of vocal abuse: fluctuations in phonation time and intensity in 4 groups of speakers. Acta Otolaryngol. 1993;113(4):547–552. doi: 10.3109/00016489309135861. [DOI] [PubMed] [Google Scholar]
- 16.Bottalico P, Arianna A. Investigations into vocal doses and parameters pertaining to primary school teachers in classrooms. J. Acoust. Soc. Am. 2012;131(4):2817–2827. doi: 10.1121/1.3689549. [DOI] [PubMed] [Google Scholar]
- 17.Titze IR, Hunter EJ, Švec JG. Voicing and silence periods in daily and weekly vocalizations of teachers. J. Acoust. Soc. Am. 2007;121(1):469–478. doi: 10.1121/1.2390676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Švec JG, Sram F. Proceedings of 25th World Congress Int. Assoc. Logoped. Phoniatr. Montreal, Canada: 2001. Violet-reddening of the vocal folds and the vocal fatigue. [Google Scholar]
- 19.Fisher KV, Telser A, Phillips JE, Yeates DB. Regulation of vocal fold transepithelial water fluxes. Journal of Applied Physiology. 2001;91(3):1401–1411. doi: 10.1152/jappl.2001.91.3.1401. [DOI] [PubMed] [Google Scholar]
- 20.Gordon MT, Morton FM, Simpson IC. Air flow measurements in diagnosis assessment and treatment of mechanical dysphonia. Folia Phoniatr. 1978;30(3):161–174. doi: 10.1159/000264123. Gordon et al. [DOI] [PubMed] [Google Scholar]
- 21.Sapienza CM, Stathopoulos ET. Respiratory and laryngeal measures of children and women with bilateral vocal fold nodules. J. Speech Lang. Hear. Res. 1994;37(6):1229–1243. doi: 10.1044/jshr.3706.1229. [DOI] [PubMed] [Google Scholar]
- 22.Sapienza CM, Stathopoulos ET. Speech task effects on acoustic and aerodynamic measures of women with vocal nodules. Journal of Voice. 1995;9(4):413–418. doi: 10.1016/s0892-1997(05)80203-6. [DOI] [PubMed] [Google Scholar]
- 23.Sapienza CM, Elaine TS, Brown WS. Speech breathing during reading in women with vocal nodules. Journal of Voice. 1997;11(2):195–201. doi: 10.1016/s0892-1997(97)80078-1. [DOI] [PubMed] [Google Scholar]
- 24.Iwarsson J, Sundberg J. Breathing behaviors during speech in healthy females and patients with vocal fold nodules. Log Phon Vocol. 1999;24:154–169. [Google Scholar]
- 25.Watts CR, Awan SA. An examination of variations in the cepstral spectral index of dysphonia across a single breath group in connected speech. Journal of Voice. 2015;29(1):26–34. doi: 10.1016/j.jvoice.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Astolfi A, Bottalico P, Accornero A, Garzaro M, Nadalin J, Giordano C. Proceedings of Euronoise. Prague, Czech Republic: 2012. Relationship between vocal doses and voice disorders on primary school teachers. [Google Scholar]
- 27.Vallino D. Thesis: Corso di Laurea in Logopedia, Facoltà di Medicina e Chirurgia, Università degli Studi di Torino. Torino, Italy: 2011. Clinical and acoustic analysis of vocal load of primary school teachers and speech therapy intervention. [Google Scholar]
- 28.Accordi M, Tesserin F. Proceedings of LXXXIX Congresso Nazionale della Società Italiana di Otorinolaringologia e Chirurgia Cervico-Facciale. Le disfonie: fisiopatologia, clinica ed aspetti medico-legali. San Benedetto del Tronto, Italy: SIOeChCF; 2002. L’anamnesi e l’esame obiettivo laringeo (Anamnesis and laryngeal objective examination) [Google Scholar]
- 29.Vernero I, Gambino M, Schindler A, Schindler O. La cartella logopedica - età adulta ed involutiva (Logopedic folder – Adulthood and Senescence) Omega Edizioni. 2002 [Google Scholar]
- 30.Cheyne HA, Hanson HM, Genereux RP, Stevens KN, Hillman RE. Development and testing of a portable vocal accumulator. Journal of Speech, Language, and Hearing Research. 2003;46(6):1457–1467. doi: 10.1044/1092-4388(2003/113). [DOI] [PubMed] [Google Scholar]
- 31.Giordano R. Note sulla fonetica del ritmo dell'italiano (Note on the Phonetics of rhythm in the Italian language) In: Savy R, Crocco C, editors. Procedings of Analisi prosodica: Teoria, Modelli e Sistemi di annotazione. Atti del II Convegno Nazionale Associazione Italiana di Scienze della Voce (AISV) Torriana: EDK Editore; 2006. [last viewed January 19 2015]. http://www.parlaritaliano.it/index.php/it/dati/450-note-sulla-fonetica-del-ritmodellitaliano. [Google Scholar]
- 32.Romano A. À propos de deux bases de données de parole publiées récemment: compterendu de ‘API - Archivio del Parlato Italiano’ et de ‘C-ORAL-ROM’ (On the matter of two recently published speech databases: a report on API and C-ORAL-ROM) Rivista di Linguistica. 2007;19(2):367–390. [Google Scholar]
- 33.Cresti E, Moneglia M, editors. C-ORAL-ROM: integrated reference corpora for spoken romance languages. Vol. 15. John Benjamins Publishing; 2005. [Google Scholar]
- 34.R Development Core Team. R Foundation for Statistical Computing. Vienna, Austria: 2011. [last viewed January 19, 2014]. R:A language and environment for statistical computing. http://www.R-project.org. [Google Scholar]
- 35.ISO, IEC. International Organization for Standardization. Vol. 13. Switzerland: 1997. ISO/IEC Guide 43-1 Proficiency Testing by Interlaboratory Comparisons–Part 1: Development and Operation of Proficiency Testing Scheme. [Google Scholar]
- 36.Joint Committee for Guides in Metrology. JCGM100 Evaluation of measurement dataguide to the expression of uncertainty in measurement. [last viewed August 25, 2015];Joint Committee for Guides in Metrology. 2008 http://www.bipm.org/en/publications/guides/gum.html. [Google Scholar]
- 37.Löfqvist A, Mandersson B. Long-time average spectrum of speech and voice analysis. Folia Phoniatrica et Logopaedica. 1987;39(5):221–229. doi: 10.1159/000265863. [DOI] [PubMed] [Google Scholar]
- 38.Hunter EJ, Titze IR. Variations in intensity, fundamental frequency, and voicing for teachers in occupational versus nonoccupational settings. J. Speech Lang. Hear. Res. 2010;53:862–875. doi: 10.1044/1092-4388(2009/09-0040). [DOI] [PMC free article] [PubMed] [Google Scholar]