Abstract
Background:
In this study, we investigated the effect of melatonin administration on four markers of endothelial cell function including intercellular adhesion molecule (ICAM), vascular cell adhesion molecule (VCAM), C-reactive protein (CRP), and nitric oxide (NO) on patients with three vessels coronary disease.
Materials and Methods:
This double-blind, randomized, controlled trial study was conducted on 39 patients (32 men and 7 women) with three vessels coronary disease. The case group included 20 patients who received 10 mg oral melatonin 1 h before sleeping for 1 month. The control group included 19 patients who received placebo 1 h before sleeping for 1 month. The serum levels of CRP, ICAM, VCAM, and NO were compared after 1 month treatment.
Results:
After 1 month of melatonin treatment, the mean level of ICAM, VCAM, and CRP showed a statistically significant decrease in the case group. On the other hand, the mean level of VCAM increased significantly in the control group. The mean levels of CRP and ICAM were also increased in the control group, but the difference did not reach the significant threshold. With respect to NO, there was a statistically significant increase in the case group, while there was a statistically significant decrease in serum NO in the control group.
Conclusions:
The results of this study suggested that melatonin may have beneficial effects on endothelial oxidative stress even in patient with severe and advanced atherosclerosis.
Keywords: Computer-aided design, endothelial dysfunction, intercellular adhesion molecule, melatonin, vascular cell adhesion molecule
INTRODUCTION
Cardio vascular diseases (CVDs) due to atherosclerosis are the leading cause of death worldwide.[1] In the recent years, growing bodies of evidence have demonstrated the influence of inflammatory cytokines and oxidized low-density lipoprotein on endothelial dysfunction (ED) and the development of atherosclerosis.[2] ED is associated with the expression of endothelial adhesion molecules and cytokines which causes recruitment and activation of circulating leukocytes. Leukocytes adhere to the endothelium via adhesion molecules including intercellular adhesion molecule (ICAM) and vascular cell adhesion molecule (VCAM) and subsequently lead to a cascade of events that contribute in ED and damage. It has been well-established that ED plays a key role in the pathogenesis vascular injury and the development of atherosclerosis.[3] Furthermore, a large body of evidence have documented that ED is associated with a slight increase in the secretion of vasoconstriction molecule and also a lower bioavailability of vasodilator molecules such as nitric oxide (NO).[4]
Melatonin, an endocrine product of the pineal gland, is a multifunctional indolamine that plays a significant role in the protection against free radical formation and the related biochemical damages on endothelial cells.[5,6] It has been suggested that the nocturnal melatonin secretion is significantly lower in patients with CVDs.[7,8,9] With respect to the protective role of melatonin against endothelial oxidative stresses, the administration of melatonin may have beneficial effects in patients with CVD and atherosclerosis.
Until date, no study has investigated the effects of melatonin on markers of endothelial cell damage in patients with coronary artery diseases. In this study, we investigated the effect of melatonin administration on four markers of endothelial function including ICAM, VCAM, C-reactive protein (CRP), and NO on patients with three vessels coronary disease.
MATERIALS AND METHODS
Study population and data source
This double-blind, randomized, controlled trial study was conducted between February and November 2010, on patients with the clinical features of coronary artery disease who had referred to Noor, Sina and Shahid Chamran Hospitals, Isfahan province of Iran, for elective diagnostic coronary angiography. These hospitals are the major referral centers for patients with coronary artery diseases in the province. The inclusion criterion for this study was having a documented diagnosis of three vessels coronary artery diseases by angiography. The exclusion criteria were: (i) Severe left ventricular dysfunction (left ventricular ejection fraction <30% or an end-diastolic pressure >16 mmHg); (ii) recent myocardial infarction (<6 weeks), (iii) having an underlying pulmonary, renal or hepatic dysfunction, (iv) having diabetes, (v) age >80 years, and (vi) weight >90 kg. Patients who were not willing or able to continue the study were also excluded.
After applying the inclusion and exclusion criteria, a total of 39 patients were included in the study. Eligible cases gave informed consent to participate in the study. The study protocol was approved by the Ethical Committee of Isfahan University of Medical Sciences.
The enrolled cases were divided into two groups using random-maker software “random allocation.” The case group included 20 patients who received 10 mg oral melatonin (melatonin, nature made, CA, USA) 1 h before sleeping for 1 month. The control group included 19 patients who received placebo (manufactured as the same as melatonin tablets, in faculty of pharmacy of Isfahan University) 1 h before sleeping for 1 month. Blinding and randomization were performed by two investigators who were not involved in the patients’ evaluations. To maintain blinding, patients, personnel, and outcome assessors were unaware of the treatment allocation.
Biochemical evaluations
Clinical and laboratory data were collected after randomization and 1 month treatment period. A volume of 5 ml sample of venous blood was collected from each subject and centrifuged within 1 h of withdrawal at 4000 rpm for 10 min in a cold centrifuge. The plasma aliquots were stored at −80°C until analyses were performed. After 1 month administration of melatonin or placebo, another 5 ml blood samples were recollected from each subject. These samples were analyzed for serum NO2/NO3, CRP, ICAM, VCAM, and melatonin.
The methods of biochemical analyses
Melatonin assay
Plasma concentration of melatonin was measured in duplicate using Enzyme Linked Immunoassay (IBL International, Germany). The intra-assay coefficient of variation was 6.7%.
Intercellular adhesion molecule and vascular cell adhesion molecule assay
Plasma ICAM and VCAM levels were determined with an ELISA assay kit (Bender MedSystem, UK) according to manufacturer's instruction.
C-reactive protein assay
The serum levels of CRP were determined by ELISA kit according to manufacturers’ instruction (IBL, Hamburg, Germany). The sensitivity of the assay was <1 µg/ml.
Nitric oxide assay
The serum level of stable NO metabolites nitrite and nitrate were measured using a colorimetric assay (R and D Systems, Minneapolis, USA). For nitrite measurement, briefly, after serum addition into wells, sulfanilamide solution was added to all experimental samples, and after incubation, N-1-naphtylethylenediamine dihydrochloride solution was added. Then, absorbance was measured by a micro reader in 540 nm wavelength. For nitrate measurement, the enzymatic conversion of nitrate to nitrite by nitrate reductase was done. The reaction was followed by colorimetric detection of nitrite as an azo dye product of the Griess reaction. The nitrate concentration was calculated by subtracting the measured nitrite concentration from the total NO concentration.
Statistical analysis
Statistical analysis was performed using SPSS statistical software (version 11.0; SPSS, Chicago, IL, USA). Descriptive data are reported as mean ± standard deviation or number (%) as appropriate. The results were analyzed to verify the normality of distribution using test of Kolmogorov–Smirnov. To compare the studied variables between case and control groups, Student's t-test for quantitative data and Chi-square test for qualitative data were used. P < 0.05 was considered statistically significant.
RESULTS
This study included a total of 32 (82%) men and 7 (18%) women who were assigned to case and control groups, received treatments and followed for 1 month. The mean age of the patients was 59.3 ± 5.6 years (range, 41–73 years). All subjects completed the study successfully. The case group consisted of 17 (85%) men and 3 (15%) women, with a mean age of 60.1 ± 5.3 years (range, 49–73 years). The control group consisted of 15 (78%) men and 4 (22%) women, with a mean age of 58.6 ± 5.8 years (range, 41–73 years). No significant differences were noted between groups for sex, age, body mass index, ejection fraction, and the baseline levels of CRP, ICAM, VCAM, and NO (P ≥ 0.5). The baseline characteristics of patients between studied groups are presented in Table 1.
Table 1.
Baseline characteristics of 39 patients with coronary artery disease by group
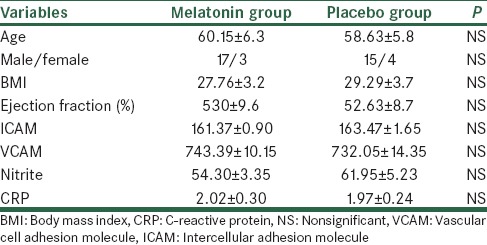
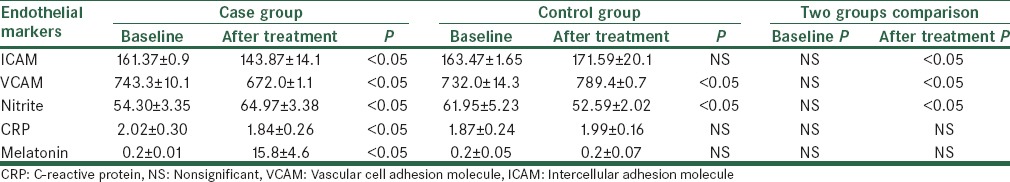
Table 2 shows the comparison of biochemical data after 1 month treatment between the case and control groups. As shown, after 1 month of melatonin treatment, the mean level of ICAM, VCAM, and CRP showed a statistically significant reduction in the case group. On the other hand, the mean level of VCAM increased significantly in the control group. The mean levels of CRP and ICAM were also increased in the control group, but the difference did not reach the significant threshold. With respect to the serum NO, there was a statistically significant increase in the case group, while there was a statistically significant decrease in serum NO in the control group. The serum level of melatonin was significantly increased in the case group, but it was not significantly changed in the control group.
Table 2.
Comparison of intercellular adhesion molecule, vascular cell adhesion molecule, nitrite, C-reactive protein concentration between case and control groups
No serious side-effects were reported in patients in both groups. Nausea was reported in two of cases and one of the controls. Mild weakness was reported in three of cases and three of controls.
DISCUSSION
In this study, we investigated the effects of melatonin administration on markers of ED among patients with three vessels coronary artery diseases. The markers used in this study included ICAM, VCAM, CRP, and NO, which are generally accepted as the markers of endothelium function.
The results of this study suggested that melatonin may have beneficial effects on ED even in a patient with severe and advanced atherosclerotic plaques. In our study, the mean levels of ICAM, VCAM, and CRP were significantly reduced after 1 month of melatonin treatment. Furthermore, melatonin treatment was associated with an increased level of serum NO among the cases.
The findings of this study are inconsistent with recently published studies. Investigations in animal models have shown that melatonin improves the NO pathway, and can have protective effects against endothelial damage, vasoconstriction, platelet aggregation, and leukocyte infiltration.[10] Other studies have showed a reduced level of melatonin in patients with type 2 diabetes[11] and hypertension.[12] It has been also demonstrated that blood melatonin level correlates with the severity of the disease in CVD patients.[13] It is unclear whether low melatonin levels in these patients are the result of melatonin “consumption” caused by scavenging of the elevated free radical production, or represent lower melatonin production, and hence less protection against oxidative stress.[10,11,14]
In addition to scavenging free radicals, and antioxidant defense enzymes activation, melatonin has robust protective effects through lowering lipid and blood pressure and increasing NO bioavailability.[12] Furthermore, it is demonstrated that suppressing the nocturnal melatonin surge is associated with increased expression of adhesion molecules in the endothelial cells.[14] Studies on mice have shown that melatonin can also inhibit atherogenic lipoprotein oxidation in these animals.[15]
It has been suggested that melatonin can reduce the expression of the adhesion molecules, including P-selectin and ICAM,[5] and suppress NFκB translocation into the nucleus.[6] These mechanisms are suggested to be associated with reduction on cardiac cell injury.
It should be noted that there are a number of studies in the literature that demonstrated adverse effects of melatonin on endothelial cells. Tailleux et al.[16] demonstrated that feeding of hypercholesterolemic mice with melatonin supplementation may increases the surface of atherosclerotic lesions in the proximal aorta. They have suggested that caution should be taken as regards high melatonin dosage in hypercholesterolemic patients. However, until date, there is no report on the adverse effects of melatonin on endothelial cells in the human subjects.
The main limitation of our study is the relatively small sample size and short follow-up period. However, this was the first report on the effects of melatonin on endothelial markers in patients with three vessels coronary artery disease. More studies are needed to shed light on the beneficial effects of melatonin on endothelial functions in patients with coronary artery diseases.
CONCLUSIONS
Our study suggests that that melatonin can decrease the markers of endothelia cell injury and elevate the vasodilator cytokines. These features can be helpful in preventing ED and atherosclerosis in patients with CVD. Additional studies are needed to establish the utility of melatonin as a novel anti-inflammatory therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Miss Moavenian and Miss Mosayebi for their invaluable helps.
REFERENCES
- 1.Ruff CT, Braunwald E. The evolving epidemiology of acute coronary syndromes. Nat Rev Cardiol. 2011;8:140–7. doi: 10.1038/nrcardio.2010.199. [DOI] [PubMed] [Google Scholar]
- 2.Haghjooyjavanmard S, Nematbakhsh M, Monajemi A, Soleimani M. Von Willebrand factor, C-reactive protein, nitric oxide, and vascular endothelial growth factor in a dietary reversal model of hypercholesterolemia in rabbit. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2008;152:91–5. doi: 10.5507/bp.2008.014. [DOI] [PubMed] [Google Scholar]
- 3.Alian Z, Hashemipour M, Dehkordi EH, Hovsepian S, Amini M, Moadab MH, et al. The effects of folic acid on markers of endothelial function in patients with type 1 diabetes mellitus. Med Arh. 2012;66:12–5. doi: 10.5455/medarh.2012.66.12-15. [DOI] [PubMed] [Google Scholar]
- 4.Yang Z, Ming XF. Recent advances in understanding endothelial dysfunction in atherosclerosis. Clin Med Res. 2006;4:53–65. doi: 10.3121/cmr.4.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuzzocrea S, Mazzon E, Serraino I, Lepore V, Terranova ML, Ciccolo A, et al. Melatonin reduces dinitrobenzene sulfonic acid-induced colitis. J Pineal Res. 2001;30:1–12. doi: 10.1034/j.1600-079x.2001.300101.x. [DOI] [PubMed] [Google Scholar]
- 6.Beck WR, Botezelli JD, Pauli JR, Ropelle ER, Gobatto CA. Melatonin has an ergogenic effect but does not prevent inflammation and damage in exhaustive exercise. Sci Rep. 2015;5:18065. doi: 10.1038/srep18065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altun A, Yaprak M, Aktoz M, Vardar A, Betul UA, Ozbay G. Impaired nocturnal synthesis of melatonin in patients with cardiac syndrome X. Neurosci Lett. 2002;327:143–5. doi: 10.1016/s0304-3940(02)00368-3. [DOI] [PubMed] [Google Scholar]
- 8.Domínguez-Rodríguez A, Abreu-González P, García MJ, Sanchez J, Marrero F, de Armas-Trujillo D. Decreased nocturnal melatonin levels during acute myocardial infarction. J Pineal Res. 2002;33:248–52. doi: 10.1034/j.1600-079x.2002.02938.x. [DOI] [PubMed] [Google Scholar]
- 9.Yaprak M, Altun A, Vardar A, Aktoz M, Ciftci S, Ozbay G. Decreased nocturnal synthesis of melatonin in patients with coronary artery disease. Int J Cardiol. 2003;89:103–7. doi: 10.1016/s0167-5273(02)00461-8. [DOI] [PubMed] [Google Scholar]
- 10.Rodella LF, Favero G, Foglio E, Rossini C, Castrezzati S, Lonati C, et al. Vascular endothelial cells and dysfunctions: Role of melatonin. Front Biosci (Elite Ed) 2013;5:119–29. doi: 10.2741/e601. [DOI] [PubMed] [Google Scholar]
- 11.Tutuncu NB, Batur MK, Yildirir A, Tutuncu T, Deger A, Koray Z, et al. Melatonin levels decrease in type 2 diabetic patients with cardiac autonomic neuropathy. J Pineal Res. 2005;39:43–9. doi: 10.1111/j.1600-079X.2005.00213.x. [DOI] [PubMed] [Google Scholar]
- 12.Simko F, Paulis L. Melatonin as a potential antihypertensive treatment. J Pineal Res. 2007;42:319–22. doi: 10.1111/j.1600-079X.2007.00436.x. [DOI] [PubMed] [Google Scholar]
- 13.Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8. doi: 10.1253/circj.cj-08-1102. [DOI] [PubMed] [Google Scholar]
- 14.Marçola M, da Silveira Cruz-Machado S, Fernandes PA, Monteiro AW, Markus RP, Tamura EK. Endothelial cell adhesiveness is a function of environmental lighting and melatonin level. J Pineal Res. 2013;54:162–9. doi: 10.1111/j.1600-079X.2012.01025.x. [DOI] [PubMed] [Google Scholar]
- 15.Tailleux A, Gozzo A, Torpier G, Martin-Nizard F, Bonnefont-Rousselot D, Lemdani M, et al. Increased susceptibility of low-density lipoprotein to ex vivo oxidation in mice transgenic for human apolipoprotein B treated with 1 melatonin-related compound is not associated with atherosclerosis progression. J Cardiovasc Pharmacol. 2005;46:241–9. doi: 10.1097/01.fjc.0000175232.11079.7e. [DOI] [PubMed] [Google Scholar]
- 16.Tailleux A, Torpier G, Bonnefont-Rousselot D, Lestavel S, Lemdani M, Caudeville B, et al. Daily melatonin supplementation in mice increases atherosclerosis in proximal aorta. Biochem Biophys Res Commun. 2002;293:1114–23. doi: 10.1016/S0006-291X(02)00336-4. [DOI] [PubMed] [Google Scholar]


