Abstract
Kimura's disease is a rare, chronic inflammatory disorder of unknown cause. It is endemic in Asia, affecting more number of males than females, with a ratio of 3:1. The typical clinical manifestations include a triad of painless unilateral cervical lymphadenopathy or subcutaneous masses predominantly in the head and neck region, blood and tissue eosinophilia, and an elevated serum immunoglobulin E (IgE) levels. Variable conditions both benign and malignant may mimic Kimura's disease both clinically and on fine needle aspirates. The confirmatory diagnosis is established only by histopathological examination. We report a case of Kimura's disease in a patient who underwent multiple investigations in view of her past history and family history of pulmonary Koch's. Fine needle aspiration cytology (FNAC) was performed thrice with consistently similar result of reactive lymphadenitis with numerous histiocytes and eosinophilia. The final diagnosis of Kimura's disease could finally be established only on histopathological examination.
Keywords: Eosinophilia, fine needle aspiration cytology (FNAC), Kimura's disease, lymphadenopathy; postauricular, reactive lymphadenitis
Introduction
Kimura's disease is a benign, chronic inflammatory soft tissue disorder of unknown origin. It occurs predominantly in young adults with the age range of 27-40 years and the male to female ratio is 3:1.[1] It was first described in 1937 in Chinese medical literature by Kim and Szeto and later definitive histological description was published by Kimura et al. in 1948.[2] The clinical onset is insidious with enlarging soft tissue mass in the head and neck region, most frequently in infra- and retroauricular areas. Occasionally, an isolated lymphadenopathy is the only presentation.[3]
Cases have been reported with the involvement of the salivary gland, particularly the parotid, oral cavity, axilla, groin, and limbs.[4] Peripheral blood eosinophilia and elevated serum immunoglobulin E (IgE) levels are constant features of Kimura's disease.[5]
Case Report
A 44-year-old female of Asian origin presented with right postauricular swelling for the last 6 years, followed by left postauricular swelling for 1 year. It was associated with itching and has gradually progressed to the present size. There was a past history of pulmonary tuberculosis 17 years back and a positive family history of tuberculosis.
The present swelling was not associated with fever, weight loss, and chronic cough.
On examination, a globular matted nontender lymphadenopathy was seen extending from posterior auricular to posterior border of the mastoid measuring 4.5 cm × 4 cm. The left postauricular lymphadenopathy was small and superficial, measuring 2 cm × 1 cm. There were no organomegaly and other palpable lymph nodes.
Investigations revealed a hemoglobin level of 10.5 g/dL, a white blood cell count of 10.47 cells/L × 109 cells/L with 15% eosinophil, and a normal platelet count. Her blood urea and serum creatinine were within normal limits. The erythrocyte sedimentation rate was 22 mm/h. Sputum samples for tubercular bacilli were negative. The tests for hepatitis B surface antigen and anti-hepatitis C virus antibody were negative. A chest radiograph showed an old healed focus of tuberculosis.
Fine needle aspiration cytology (FNAC) was performed thrice from both the swelling at two different laboratories. FNAC reports had similar findings of reactive lymphadenitis, histiocytes with prominent nucleoli along with eosinophil and plasma cells [Figure 1]. In view of histiocytes with prominent nucleoli and eosinophil, and considering the past history of tuberculosis, an excision biopsy of the bilateral swelling was done and sent for histopathological examination.
Figure 1.
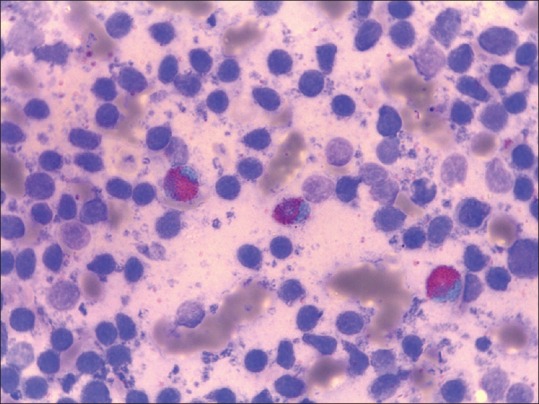
Cytology smear from the swelling showing eosinophil against a reactive background (MGG stain, ×100)
We received the excised mass; cut surface of both the masses were solid grey-brown. Histopathological examination of the excised tissue showed lymphoid hyperplasia with a well-maintained architecture. There were variable size germinal centers, with some showing occasional vascularization. The paracortical area showed marked infiltration by eosinophil and mast cells with postcapillary proliferations. At places, there were formations of eosinophilic microabscess [Figure 2]. The extranodal tissue showed eosinophilic infiltration as well. These features were consistent with Kimura's disease.
Figure 2.
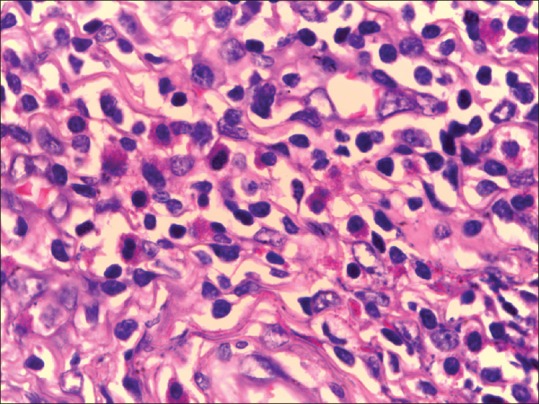
Histological section from the swelling showing eosinophilic micro abscess (H&E stain, ×400)
The diagnostic dilemma with clinical suspicion of tubercular lymphadenopathy and the cytological features of reactive lymphadenitis with eosinophilia in the current case came to the conclusion only through the histopathological examination. Thus, after multiple attempts through FNAC, a final diagnosis of Kimura's disease could only be established through histopathological examination.
Discussion
Kimura's disease is a rare form of chronic inflammatory disorder involving subcutaneous tissue and lymph nodes predominantly in the head and neck region. It occurs commonly in young adults with the age range of 27-40 years and the male to female ratio is 3:1. It is endemic in Asia, especially in China and Japan.[3] Peripheral blood eosinophilia and markedly elevated serum IgE levels is a constant feature of Kimura's disease. The present case of a 44-year-old lady of Asian origin presenting with bilateral swelling in the head and neck region falls within the typical age and clinical presentation of the disease. She had peripheral eosinophilia of 15%, which is as well a usual finding in such a disease. However, levels of IgE were not performed.
The etiology of this disease is still unknown, though many theories of an allergic reaction or an alteration of immune regulation and persistent antigenic stimulation following arthropod bites and parasitic or candidal infection have been proposed. The differential diagnosis includes both benign and malignant conditions such as angiolymphoid hyperplasia with eosinophilia, Hodgkin's disease, reactive lymphadenopathy, parasitic infections, and drug reactions. In our case, the clinical diagnosis considered was tuberculous lymphadenopathy that was supported by a strong positive family history of tuberculosis; with this, she underwent cytological examination.
Few of the studies have highlighted certain characteristic features in fine needle aspiration smears that are helpful in preoperative diagnosis of Kimura's disease;[6,7,8] these are, the presence of significant numbers of eosinophils in a background of lymphoid cells with occasional fragments of collagenous tissue and Warthin-Finkeldey polykaryocytes. The cytologic features of this disease have to be interpreted in the appropriate clinical setting in order to make a correct preoperative diagnosis. FNAC may be valuable in the diagnosis of recurrent lesions of Kimura's disease and may spare the patient from repeated biopsies. The present case showed the cytological features of reactive hyperplasia with increased eosinophils at three different settings. Thus, in the current case, the diagnosis could have been reviewed and the possibilities of Kimura's disease may have been suggested.
The definitive diagnosis is obtained by histological examination of the excised lesion. Histopathologically, the lesion is characterized by hyperplasia of lymphoid tissue with well-developed lymphoid follicles, marked infiltration of eosinophils, proliferation of thin-walled capillary venules, and varying degrees of fibrosis.[3,9]
Kimura's disease is a chronic disorder, with an indolent clinical course, frequently waxing and waning over time. Surgery is the mainstay of therapy, although regional or systemic corticosteroid therapy, cytotoxic therapy, and radiation have been used.
The present case is of a 44-year-old lady of Asian origin with bilateral swelling in the head and neck region. She had peripheral eosinophilia of 15%, which is a usual finding in such a disease. However, levels of IgE were not performed. The consistent similar cytological features of reactive hyperplasia with increased eosinophils at three different settings in the current case could have been reviewed and the possibilities of Kimura's disease may have been suggested. The diagnosis in our case was only through the histopathological examination of the excised tissue. Thus, the cytological features of reactive hyperplasia with the presence of eosinophils and giant cells should at least clinch the diagnosis of Kimura's disease at cytology in appropriate clinical settings. The awareness of the Kimura's disease being endemic in Asian population should be considered while dealing patients with such clinical scenario and cytological findings.
Our case is at regular follow-up and presented later after 6 months with recurrence. The recurrence was bilateral, associated with itching. She was started on steroids and is advised for close follow-up.
Conclusion
Kimura's disease is a benign, chronic inflammatory soft tissue disorder of unknown origin, occurring predominantly in young adults. It usually involves the subcutaneous tissue and lymph nodes of the head and neck region. A differential diagnosis of Kimura's disease should always be considered with cytological features of reactive lymphadenitis and eosinophilia in an endemic zone.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tseng CF, Lin HC, Huang SC, Su CY. Kimura's disease presenting as bilateral parotid masses. Eur Arch Otorhinolaryngol. 2005;262:8–10. doi: 10.1007/s00405-003-0677-9. [DOI] [PubMed] [Google Scholar]
- 2.Kimura T, Yoshimura S, Ishikawa E. On the unusual granulation combined with hyperplastic changes of lymphatic tissue. Trans Soc Pathol Jpn. 1948;37:179–80. [Google Scholar]
- 3.Kuo TT, Shih LY, Chan HL. Kimura's disease. Involvement of regional lymph nodes and distinction from angiolymphoid hyperplasia with eosinophilia. Am J Surg Pathol. 1998;12:843–54. [PubMed] [Google Scholar]
- 4.Hui PK, Chan JK, Ng CS, Kung IT, Gwi E. Lymphadenopathy of Kimura's disease. Am J Surg Pathol. 1989;13:177–86. doi: 10.1097/00000478-198903000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong WB, Allison G, Pena F, Kim JK. Kimura's disease: Two case reports and a literature review. Ann Otol Rhinol Laryngol. 1998;107:1066–71. doi: 10.1177/000348949810701212. [DOI] [PubMed] [Google Scholar]
- 6.Chow LT, Yuen RW, Tsui WM, Ma TK, Chow WH, Chan SK. Cytologic features of Kimura's disease in fine-needle aspirates. A study of eight cases. Am J Clin Pathol. 1994;102:316–21. doi: 10.1093/ajcp/102.3.316. [DOI] [PubMed] [Google Scholar]
- 7.Deshpande AH, Nayak S, Munshi MM, Bobhate SK. Kimura's disease. Diagnosis by aspiration cytology. Acta Cytol. 2002;46:357–63. doi: 10.1159/000326734. [DOI] [PubMed] [Google Scholar]
- 8.Jayaram G, Peh KB. Fine-needle aspiration cytology in Kimura's disease. Diagn Cytopathol. 1995;13:295–9. doi: 10.1002/dc.2840130404. [DOI] [PubMed] [Google Scholar]
- 9.Battaglione V, le Tourneau A, Soler C, Deville A, Michiels JF, Hofman P. Kimura's disease of the lymph node. Histology, immunohistochemistry, and differential diagnosis. Ann Pathol. 1998;18:492–6. [PubMed] [Google Scholar]


