Summary
Tumor-secreted extracellular vesicles (EVs) are critical mediators of intercellular communication between tumor cells and stromal cells in local and distant microenvironments. Accordingly, EVs play an essential role in both primary tumor growth and metastatic evolution. EVs orchestrate multiple systemic pathophysiological processes, such as coagulation, vascular leakiness, and reprogramming of stromal recipient cells to support pre-metastatic niche formation and subsequent metastasis. Clinically, EVs may be biomarkers and novel therapeutic targets for cancer progression, particularly for predicting and preventing future metastatic development.
Keywords: Exosomes, Extracellular vesicles, Microvesicles, Metastasis
Introduction
Tumor-secreted EVs are emerging as critical messengers in tumor progression and metastasis. In this review we summarize the metastatic role of various EVs: microvesicles, exosomes, ectosomes, oncosomes, cytoplast etc (Colombo et al., 2014; Di Vizio et al., 2012; Headley et al., 2016; Thery et al., 2009; van der Pol et al., 2012). Exosomes are EVs 30-150 nm in diameter derived from the multivesicular endosome pathway, but the term is used in many studies for small EVs recovered by various protocols which do not actually discriminate endosome-derived from plasma membrane-derived EVs. We will thus use the term as chosen by the authors of the articles described, not necessarily inferring an exclusively endosomal or plasma membrane origin of the EVs. EVs contain bioactive molecules, such as nucleic acids (DNA, mRNA, microRNA, and other non-coding RNAs), proteins (receptors, transcription factors, enzymes, extracellular matrix proteins), and lipids that can redirect the function of a recipient cell (Raposo and Stoorvogel, 2013). Cancer cell-derived EVs promote angiogenesis and coagulation, modulate the immune system, and remodel surrounding parenchymal tissue, which together support tumor progression (Ciardiello et al., 2016; Peinado et al., 2011; Ratajczak et al., 2006; van der Pol et al., 2012). Clinically, circulating exosomes and microvesicles isolated from cancer patients have been associated with metastasis or relapse, and therefore could serve as important diagnostic and prognostic markers as well as therapeutic targets (Lener et al., 2015).
Physiological role of EVs: from development onwards
In 1967, Peter Wolf first demonstrated a role for platelet-secreted vesicles during blood coagulation (Wolf, 1967). In 1980, Trams et al. uncovered the essential role that EVs play in intercellular transport of trophic substances or nutrients (Trams et al., 1981). In 1983, two groups described the role of secretory vesicles in reticulocyte maturation through recycling of transferrin and its receptor (Harding et al., 1983; Johnstone et al., 1987; Pan and Johnstone, 1983). Pioneering studies by Raposo et al. demonstrated the importance of EVs derived from B cells in antigen presentation and T cell stimulation (Raposo et al., 1996). Since then, many studies have further demonstrated that EVs derived from professional antigen presenting cells, such as DCs, express class I, class II MHC, adhesion, and co-stimulatory molecules that can directly activate CD4+ and CD8+ T cells (De Toro et al., 2015; Zitvogel et al., 1998).
Pregnancy is characterized by an immune tolerant microenvironment in order to protect the fetus, and secretion of vesicles with immunosuppressant activities is increased in pregnant women as compared with non-pregnant ones. Several proteins, such as human ligands of the activating NK cell receptor NKG2D, FAS-ligand and TRAIL, secreted in placental EVs seem to be responsible for the generation of an immune-privileged microenvironment (Hedlund et al., 2009; Pap et al., 2008; Stenqvist et al., 2013). EV-mediated bidirectional communication between the embryo and uterine endometrium is critical for successful implantation of the embryo. Characterization of these EVs revealed several key mRNAs related to pluripotency, such as Oct4, Sox2, Klf4, c-Myc and Nanog (Saadeldin et al., 2014). Additionally, it has been shown that trophoblast cells shed EVs, and extracellular matrix metalloproteinase inducer (EMMPRIN) released in EVs may regulate angiogenesis, tissue remodeling and growth of the placenta (Atay et al., 2011; Sidhu et al., 2004). Recent studies of EVs in Drosophila have also demonstrated that EVs may help establish the long range gradients of Wnt and Hedgehog required for proper anatomic axes and limb development (McGough & Vincent, 2016). To date, most of the studies published have been performed in vitro (Saadeldin et al., 2015), and more in vivo data are needed to understand the potential implications of EVs during embryonic development and how these EVs relate to the characterization and molecular pathways of tumor-derived EVs.
Role of EVs in promoting survival and growth of the primary tumor
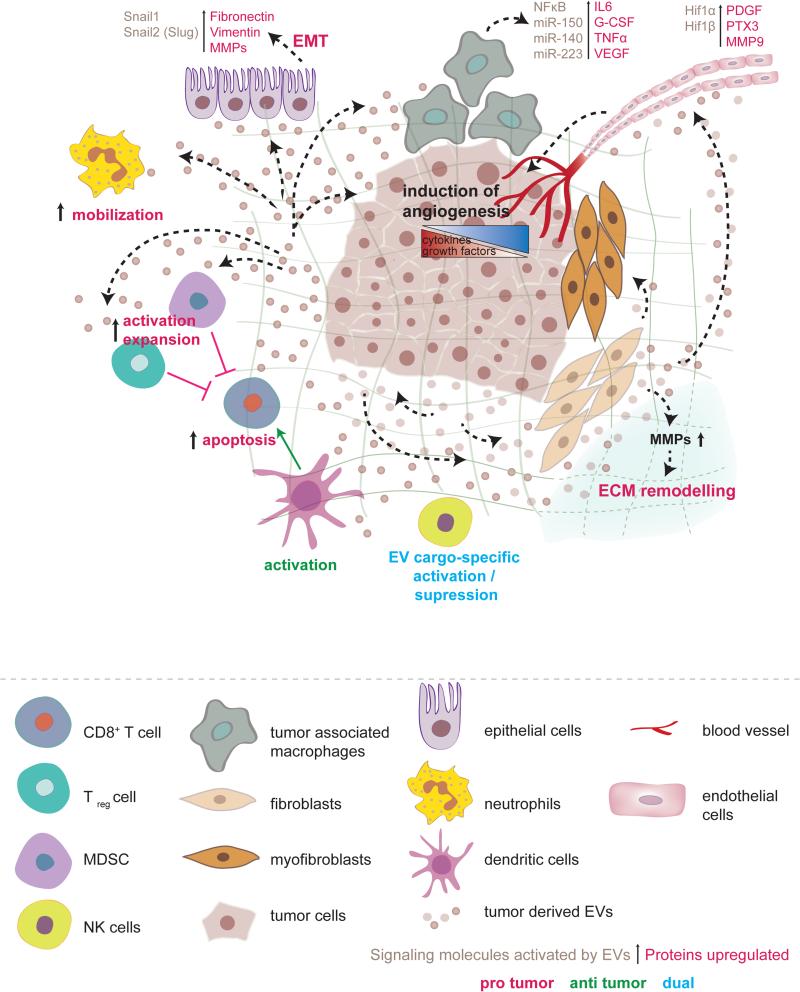
During primary tumor formation, tumor cells require active communication with neighboring cells and their local microenvironment. During the last decade, the critical role of EVs in cell-cell communication between tumor cells and surrounding cells in the primary tumor microenvironment has been highlighted (Figure 1). EVs are thought to participate in multiple steps during invasive processes and perhaps contribute to early steps involved in metastasis.
Figure 1. Role of tumor-derived EVs on the primary tumor microenvironment.
Tumor EVs cause fibroblasts to differentiate into myofibroblasts, which release MMPs and lead to extracellular matrix remodeling. The breakdown of ECM leads to the release of growth factors embedded in the ECM and promotes invasion through parenchymal cells. Tumor EVs activate tumor-associated macrophages to secrete G-CSF, VEGF, IL-6, and TNFα, which together promote angiogenesis and create an inflammatory niche. Tumor EVs affect immune system homeostasis mostly by triggering immunosuppressive changes that protect the tumor. Tumor EVs activate and expand Tregs and MDSCs, which inhibit CD8+ T-cell mediated targeting of the tumor. Furthermore, tumor EVs have been shown to express FasL and TRAIL on their membrane and directly induce apoptosis of CD8+ T-cells. Tumor EVs increase neutrophil mobilization and to be associated with increased tumor progression. Natural killer cells, which play an important role in antitumor immunity, can be either activated or suppressed by tumor EVs, depending on the tumor model studied and the EV cargo. Dendritic cells can be activated by the tumor-derived antigens delivered via tumor EVs and enforce a CD8+-mediated anti-tumor response. As the tumor grows, it develops metabolic demands that outgrow its blood supply and thus becomes increasingly hypoxic. In response to low oxygen concentrations, the tumor secrets angiogenic factors and EVs that promote blood vessel recruitment. EVs derived from the primary tumor can stimulate epithelial cells to release factors involved in EMT that trigger the loss of tumor cell adhesion (Fibronectin and Vimentin), ECM remodeling, and angiogenesis (MMPs), which together promote the release of tumor cells into the circulation and their spread to distant sites.
Primary tumor subpopulations can share oncogenic molecules through EVs
Tumor-secreted vesicles can transfer oncogenic molecules between tumor cells within the primary tumor. Al-Nedawi et al. demonstrated that glioma cells expressing epidermal growth factor receptor variant III (EGFRvIII) secrete microvesicles harboring EGFRvIII and transfer it to EGFRvIII-negative cancer cells in the same primary tumor. This mutation is seen in 25-64% of patients with glioblastoma and despite not binding any known ligand, EGFRvIII signals constitutively at low levels (Gan et al., 2013). Upon EV-mediated uptake by recipient cells, EGFRvIII activates the mitogen-activated protein kinase (MAPK) and protein kinase B (PKB/Akt) signaling pathways, thereby inducing morphological transformation and accelerating cancer growth (Al-Nedawi et al., 2008).
Tumor-secreted EVs communicate with neighboring non-tumor cells
Tumor EVs exert complex effects on neighboring stromal cells such as endothelial cells and fibroblasts. Glioblastoma-derived microvesicles containing mRNA, miRNA, and angiogenic proteins are taken up by recipient cells and promote primary tumor growth as well as endothelial cell proliferation (Skog et al., 2008). Pancreatic cancer-derived exosomes expressing tetraspanin 8 recruit proteins and mRNA cargo that activate angiogenesis-related gene expression in endothelial cells (Nazarenko et al., 2010). Tumor-derived exosomes containing TGF-β convert fibroblasts into myofibroblasts, contributing to vascularization, tumor growth and local invasion (De Wever et al., 2008; Webber et al., 2010). Breast cancer-derived exosomes also promote a myofibroblastic phenotype in adipose tissue-derived mesenchymal stem cells, resulting in increased expression of the tumor-promoting factors TGF-β, VEGF, SDF-1 and CCL5 (Cho et al., 2012).
Conversely, exosomes secreted by tumor stroma can also influence tumor progression. Breast cancer-associated fibroblasts (CAFs) secrete exosomes that have been shown to promote tumor motility, invasion, and dissemination of breast cancer cells through the Wnt-planar cell polarity (Wnt-PCP) signaling pathway (Luga et al., 2012). Therefore, exosomes mediate bi-directional communication between tumor cells and their environment and are central effectors of a feed-forward signaling loop that shapes the ever-evolving tumor microenvironment. However, the specific mechanisms through which healthy stromal cells are triggered to release exosomes that promote the malignant behavior of cancer cells remain to be determined.
In the past decade, much emphasis has been placed on the potential role of miRNAs packaged within EVs in regulating cell-cell interactions. Exosomes released by mast cells containing both mRNA and miRNA can be transferred to recipient cells and regulate gene expression (Valadi et al., 2007). Moreover, transfer of miRNAs specifically targeting PTEN expression from astrocyte-derived exosomes to invading tumor cells in the brain microenvironment promotes establishment of brain metastasis, although other autocrine and paracrine signaling may also cooperate during tumor progression (Zhang et al., 2015). However, the significance of this horizontal transfer of miRNAs for the global miRNA activity of a target cell remains unclear (Squadrito et al., 2014). Squadrito et al. detected transfer of miRNA activity via exosomes but the contribution to target gene repression was limited, suggesting exosomal miRNAs are degraded within recipient cell lysosomes (Squadrito et al., 2014). While these studies were performed in endothelial cells, other microenvironments, such as primary tumors, may facilitate increased miRNA transfer among cells (Baer et al., 2013). Recently, it was suggested that cancer exosomes, on average, contained only a single miRNA per exosome (Chevillet et al., 2014). However, stoichiometry of specific miRNAs may vary by tumor types and therefore the number and distribution of miRNAs secreted in other models may differ from these studies (Chevillet et al., 2014).
Interactions between metastatic cells and their microenvironment via miRNA-containing EVs have also been demonstrated (Zhang et al., 2015). Tumor-derived exosomes, but not those released by normal cells, contain key enzymes involved in miRNA biogenesis, which enabled cell-independent miRNA biogenesis within exosomes. Inhibition of target mRNA expression (e.g., PTEN and HOXD10) by transferred mature miRNAs can lead to cancer development in originally non-cancerous cells (Melo et al., 2014). Large oncosomes, atypically large EVs with diameter of 1-10 μM secreted by amoeboid tumor cells, from RWPE-2 prostate cancer cells are enriched in miR-1227 and may enhance the migration of fibroblasts (Morello et al., 2013). Similarly, comparing exosomes from prostate cancer stem cells with that of exosomes from the bulk tumor demonstrated a differential miRNA content that may contribute to local invasion and pre-metastatic niche formation through fibroblast migration (Sanchez et al., 2016). Highly abundant exosomal miRNAs, such as miR-100-5p, miR-21-5p and miR-139-5p, increased metalloproteinase (MMPs) −2, −9 and −13, RANKL expression and fibroblast migration upon transfection into prostate fibroblasts (Sanchez et al., 2016).
miRNAs within EVs from noncancerous cells within the tumor microenvironment have also demonstrated an ability to influence tumor growth and drug resistance. Metastatic breast cancer cells demonstrated a dormant phenotype when co-cultured with human bone marrow-derived mesenchymal stem cells (BM-MSCs) secreting exosomes containing miR-23b. In recipient breast cancer cells, miR-23b decreased expression of MARCKS, a cell cycle and motility regulator, suggesting that exosomal transfer of miRNAs from the bone marrow may promote tumor dormancy in a metastatic niche (Ono et al., 2014). Interestingly, exosomal miR-21 transfer from cancer-associated adipocytes and fibroblasts to ovarian cancer cells suppresses apoptosis and confers chemoresistance by binding to APAF1 (Au Yeung et al., 2016). Most of the studies regarding the relevance of miRNA in cancer biology are performed in vitro, limiting our interpretation of the data. However, these numerous studies support an active role for shuttling of miRNAs between tumor cells and their microenvironment during tumor progression and metastasis.
Local tumor invasion is promoted by EV-mediated ECM remodeling
During cancer progression, the cellular and molecular milieu of stromal cells, and their extracellular proteins and enzymes are dynamically changing due to the evolving influence of tumor-derived EVs. Extracellular matrix (ECM)-remodeling is generally thought to promote the invasive phenotype of tumors. Secreted tumor exosomes carrying the ECM molecule fibronectin promote nascent adhesion assembly and increase cell motility (Sung et al., 2015). Proteomic analysis of tumor EVs revealed that annexins, α3 integrin, and ADAM10 were enriched in exosomes compared to ectosomes, and correlated with local invasion and cell migration, (Keerthikumar et al., 2015). Large oncosomes also harbor abundant bioactive molecules involved in local invasion (e.g., ARF6, Cav-1, metalloproteinases MMP9, and MMP2) and their abundance also correlated with tumor progression (Di Vizio et al., 2012). Sidhu et al. reported that microvesicles shed by tumor cells deliver EMMPRIN to fibroblasts, triggering the production of MMPs and enabling tumor invasion and metastasis (Sidhu et al., 2004). Endothelial cells stimulated by VEGF and FGF-2 release EVs containing MMPs that initiate the proteolysis necessary for tumor invasion and uninhibited angiogenesis (Taraboletti et al., 2002). Moreover, Hendrix et al. demonstrated that, Rab27b-mediated exocytic release of HSP90 exosomes from metastatic breast cancer cells activates MMP2, leading to degradation of ECM components, release of growth factors, and promotion of cancer cell invasion (Hendrix et al., 2010).
Association between hypoxic microenvironment and pro-angiogenic tumor-EVs
Among the factors that shape the primary tumor microenvironment, hypoxia plays a central role by promoting survival and propagation of tumor cells through modulation of the stroma (Finger and Giaccia, 2010). During hypoxia, breast cancer cells exhibit an increase in exosome release that may be regulated by hypoxia-inducible factor 1-α (HIF1-α) (King et al., 2012). Exosomes derived from highly malignant glioblastoma multiforme (GBM) cells growing in hypoxic conditions induce angiogenesis by stimulating cytokine and growth factor secretion by endothelial cells, thereby promoting pericyte migration (Kucharzewska et al., 2013). In addition, GBM patient-derived exosomes are enriched in multiple hypoxia-regulated proteins involved in GBM pathogenesis. These observations suggest that the hypoxic microenvironment of the primary tumor may significantly impact exosome cargo and function, exerting local and systemic effects that warrant further investigation.
Tumor-secreted EVs may play a role in EMT
Tumor EVs also may participate in epithelial to mesenchymal transition (EMT). HRAS overexpression in Madin-Darby canine kidney epithelial cells promotes the packaging of mesenchymal markers (e.g., vimentin and MMPs) in exosomes, potentially inducing EMT in recipient cells (Tauro et al., 2013). Although not functionally validated, there is an association between exosomes derived from mesenchymal cells and induction of EMT in epithelial cells (Tauro et al., 2013). Similarly, EVs isolated from the metastatic breast cancer cell line MDA-MB-231 stimulated with linoleic acid induce an EMT-like process in epithelial MCF10A cells (Galindo-Hernandez et al., 2014). Elucidating the role of EVs in the regulation of cell polarity and the initiation of EMT in vivo requires intensive future investigation (Lakkaraju and Rodriguez-Boulan, 2008).
Tumor EVs path through the extracellular compartment
Tumor-shed EVs circulate and can be isolated from nearly all body fluids, including blood, saliva and urine (Boukouris and Mathivanan, 2015; Ciardiello et al., 2016). Accumulating evidence indicates that circulating EVs mediate the “reprogramming” of multiple cell types at distant sites and influence diverse processes, such as coagulation, the immune response, and the establishment of a pre-metastatic niche (PMN).
Sticky vesicles: Tumor EVs promote coagulation
It is generally accepted that development of metastasis correlates with the risk of thrombotic complications, a leading cause of mortality in cancer patients (Stein et al., 2006). Coagulation and platelet accumulation at cancer sites prevent recognition of cancer cells by the immune system and promote cancer cell migration and dissemination (Sierko and Wojtukiewicz, 2007). Microvesicles involved in coagulation can originate from platelets, inflammatory cells, and cancer cells (Rak, 2010). Elevated circulating levels of microvesicles containing tissue factor (TF) and other coagulation-promoting factors are observed in cancer patients and correlate with increased risk of thrombosis (Hron et al., 2007; Rak, 2010; Tilley et al., 2008). In vivo, TF-containing EVs released by monocytes bind to activated platelets and promote the generation of arterial thrombi (Falati et al., 2003). Interestingly, KRAS and p53 mutational status correlates with increased levels of TF in vesicles secreted by human colorectal carcinoma cells (Yu et al., 2005). Likewise, pancreatic cancer cell-derived microvesicles containing active TF and PSGL-1 were shown to accumulate at sites of injury, decreasing bleeding upon injection into living mice (Thomas et al., 2009). Together, these data suggest that tumor-secreted EVs have a potential pro-thrombotic effect (Thomas et al., 2009) and support the relevance of coagulation in cancer progression and metastasis (Yu et al., 2008).
Tumor EVs demonstrate a complex impact on the immune system
The involvement of EVs in immune regulation was first proposed in early studies showing that immune cell-derived exosomes carry major histocompatibility complex (MHC) class I, MHC class II, and T cell co-stimulatory molecules (Raposo et al., 1996; Zitvogel et al., 1998). Since then, the role of EVs in immune regulation has been intensively studied and several mechanisms have been proposed for the release of exosomes carrying immunomodulatory molecules by various immune cells upon infection, which can influence primary and secondary immune responses (Admyre et al., 2007; Bhatnagar et al., 2007).
In addition to EVs derived from lymphocytes (Raposo et al., 1996), macrophages (Bhatnagar et al., 2007) and DCs (Zitvogel et al., 1998), non-immune cell-derived EVs, such as those released by epithelial and tumor cells, also express MHC class I molecules and/or tumor antigens (e.g., Mart-1/MelanA) and can modulate immune responses (Wolfers et al., 2001). While tumor EVs appear to have mostly immunosuppressive effects that support tumor progression and metastasis, there is evidence of EVs promoting both pro-tumor and anti-tumor immunity, suggesting that the relationship between tumor EVs and the immune system is complex and may be largely dependent on cell type and EV cargo. The immune modulatory activity imposed by tumor exosomes can either involve direct signaling to immune cells or transfer of tumor antigens to DCs for antigen presentation to T cells to induce primary cytotoxic immune responses (Zitvogel et al., 1998). Chen et al. showed that under conditions of heat shock, mouse B cell lymphomas release exosomes carrying immunogenic molecules such as MHCs, CD40, CD86, RANTES and IL-1b. These tumor exosomes, in turn, induce the maturation of DCs leading to the activation of CD4+ and CD8+ T cell responses against the tumor (Chen et al., 2006).
Based on recent findings, several mechanisms have been proposed by which tumor-derived EVs mediate immunosuppression essential to tumor progression. For instance, breakdown of the subscapular sinus macrophage barrier in lymph nodes by chemotherapy and immunotherapy allows melanoma EVs to interact with B lymphocytes and initiate tumor-promoting humoral immunity (Pucci et al., 2016). The presence of Fas ligand or tumor necrosis factor–related apoptosis-inducing ligand (TRAIL) on tumor microvesicles induces apoptosis in Jurkat and CD8+ T cells (Abusamra et al., 2005; Kim et al., 2005). Similarly, tumor-secreted exosomes suppress the immunological activity of natural killer cells by inhibiting their proliferation and compromising their cytolytic activity (Liu et al., 2006).
Suppression of the immune system through an increase in myeloid-derived suppressor cells (MDSC) has been correlated with tumor progression and poor survival (Gabrilovich and Nagaraj, 2009). Although the mechanism by which tumor exosomes influence MDSC differentiation remains controversial, Chalmin et al. proposed that MDSC activation involves Hsp72 expressed on tumor exosomes that promotes the activation of signal transducer and activator of transcription 3 (STAT3) in a Toll-like receptor 2 (TLR2/MyD88)-dependent manner (Chalmin et al., 2010). Controversially, Xiang et al. proposed that only in vivo-derived tumor exosomes can mediate TLR2-dependent expansion of MDSCs, whereas in vitro-derived tumor exosomes regulate MDSC differentiation independently of TLR2 signaling (Xiang et al., 2010).
Local interactions between tumors and innate immune cells ultimately determine whether the cancer can be contained locally or escape and invade both local and distant sites (Benito-Martin et al., 2015). Breast cancer cell-derived exosomes stimulate the activation of tumor-associated macrophages (TAMs), resulting in NF-κB activation and secretion of pro-inflammatory cytokines (Chow et al., 2014). Tumor EVs were shown to transfer miR-150 to TAMs and trigger key angiogenic factors, such as VEGF, leading to augmented tumorigenicity (Liu et al., 2013). Breast carcinoma cell-derived exosomes increased mobilization of neutrophils and tumor growth through an unclear mechanism (Bobrie et al., 2012). On the other hand, inhibition of TGF-β leads to the recruitment of CD11b+/Ly6G+ tumor-associated neutrophils (TAN) with potent cytotoxic effect on tumor cells (Fridlender et al., 2009). These data suggest the local interaction between tumor cells and the immune system is extremely dynamic and requires further investigation to understand the balance of pro-tumor and anti-tumor immune responses.
Tumor EV's promote vascular leakiness and facilitate circulating tumor cell arrival to distant sites
Vascular leakiness is considered a hallmark of PMN formation (Huang et al., 2009; Psaila and Lyden, 2009). Melanoma-secreted vesicles induce vascular leakiness, inflammation and recruitment of bone marrow progenitor cells through upregulation of factors such as S100a8, S100a9 and TNF-α (Peinado et al., 2012). Furthermore, human breast cancer-derived exosomes promote vascular leakiness in the lung by upregulating a subset of S100 proteins and activating Src kinase signaling (Hoshino et al., 2015). Metastatic breast cancer cells that secrete miR-105-containing exosomes cause the destruction of tight junction protein ZO1 in recipient endothelial cells thereby increasing vascular permeability and susceptibility for metastatic invasion (Zhou et al., 2014). Taken together these data suggest that tumor-secreted exosomes first permeabilize vessels by delivering specific cargo to endothelial cells and then diffuse through this compromised barrier to fuse directly with parenchymal cells within PMNs favoring metastatic colonization. However, more work is required to determine the exact mechanism by which EVs influence the integrity of the endothelial barrier as well as the specificity of this targeting within vasculature of different organs.
Tumor EVs create new sites hospitable for tumor growth: The PMN
The PMN is defined by the development of an environment distant from the primary tumor that is suitable for the survival and outgrowth of incoming circulating tumor cells. The concept of the PMN has developed from an early observation made by Stephen Paget in 1889 that different tumor types tend to metastasize to different organs, suggesting that the microenvironment plays a role in dictating metastatic invasion (Paget, 1989; Peinado et al., 2011).
The role of tumor-secreted factors and EVs in PMN initiation and evolution has recently gained greater recognition. In 2009, Jung et al. found that the combined effects of soluble factors and exosomes derived from CD44 variant isoform (CD44v)-positive pancreatic cancer cells mediate the formation of a PMN within the lymph node and lung (Jung et al., 2009). CD105-positive microvesicles released from human renal cancer stem cells promote angiogenesis and the formation of PMNs in the lungs through a defined a subset of pro-angiogenic mRNAs and microRNAs (Grange et al., 2011). Tumor exosomal miR-494 and miR-542p were transferred to lymph node stromal cells and lung fibroblasts, leading to cadherin-17 down-regulation and matrix metalloproteinase up-regulation (MMP2, MMP3, and MMP14) (Rana et al., 2013). Recently, the alteration of glucose metabolism by transfer of mir-122 from breast cancer-derived microvesicles to stromal cells has been shown to play an important role in the preparation of the PMN (Fong et al., 2015). By preventing glucose uptake in stromal cells via miR-122-mediated inhibition of pyruvate kinase, breast cancer cells create a PMN with greater glucose availability for their own utilization (Fong et al., 2015).
TLR3 activation in lung epithelial cells by tumor-exosomal non-coding snRNA enhances expression of S100A8, A100A9, MMP9, Bv8 and fibronectin which, in turn, contributes to lung PMN formation (Liu et al., 2016). Upregulation of TLR3 promotes secretion of chemokines that mobilize neutrophils (CD45+CD11b+Ly6G+Ly6Cint cKit+ VEGFR1+), as well as macrophages (F4/80+) and monocytes (VEGFR1+Ly6G−Ly6C+) that further support PMN formation (Liu et al., 2016). Interestingly, tumor-secreted exosomes have their own protein “zip-codes”, namely specific integrin profiles, that address them to specific target organs, thus determining metastatic organotropism (Hoshino et al., 2015). Tumor exosomes deliver messages which upregulate pro-inflammatory S100 molecules in resident cells of target organs and induce molecular and cellular changes that promote PMN development (Hoshino et al., 2015). Imaging of tumor-secreted EVs in metastatic organs has indeed demonstrated that the interactions of EVs with target cells are highly dynamic in PMNs and support their role in eliciting phenotypic alterations within stromal cells at future sites of metastasis (Suetsugu et al., 2013; Zomer et al., 2015).
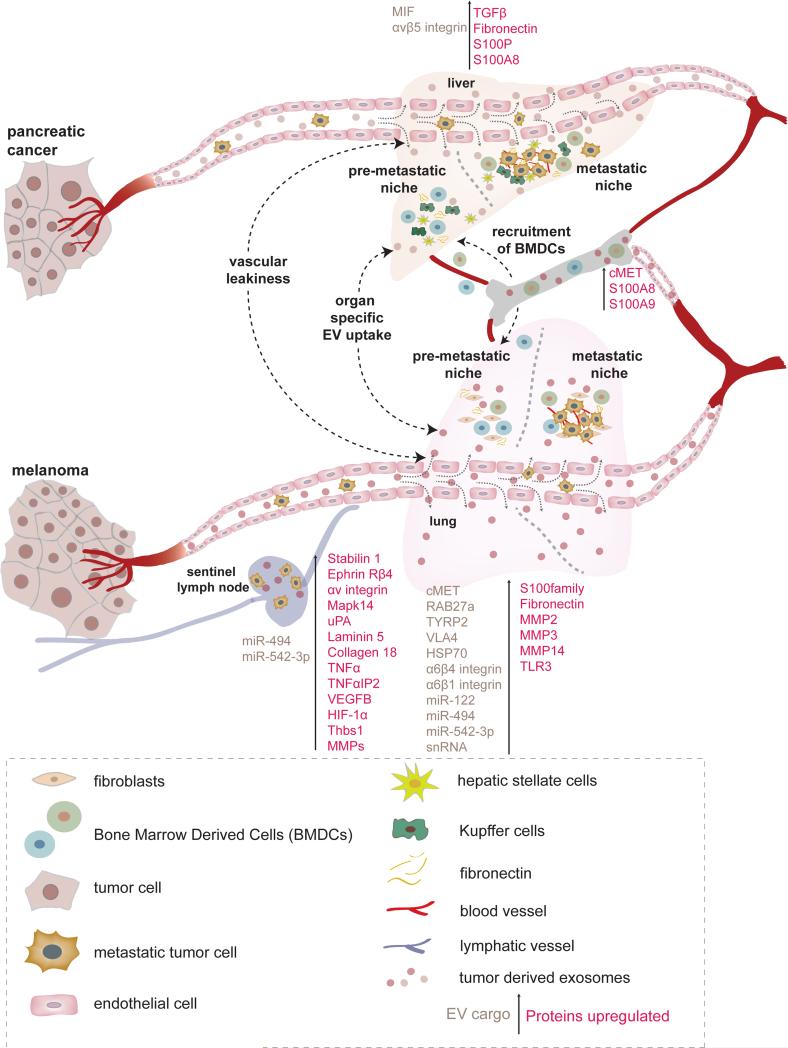
Recruitment of different cell types, such as fibroblasts, endothelial cells, macrophages and various populations of bone marrow-derived cells (BMDCs) to the PMN is promoted by tumor-secreted exosomes (Costa-Silva et al., 2015; Peinado et al., 2012). Exosomes secreted from pancreatic tumor cells execute the stepwise progression of PMN formation in the liver (Figure 2) (Costa-Silva et al., 2015). Specifically, Kupffer cells, the resident macrophages in the liver, are the primary cell type that is activated following uptake of exosomes derived from pancreatic cancer cells (Costa-Silva et al., 2015). Pancreatic tumor-derived exosomes loaded with macrophage inhibitory factor (MIF) promote TGF-β secretion in Kupffer cells, stimulating neighboring hepatic stellate cells to secrete fibronectin, ultimately leading to the recruitment of BMDCs which completes PMN formation (Costa-Silva et al., 2015). Melanoma-secreted exosomes foster PMN formation in lung via reprogramming of BMDCs leading to the recruitment and activation of cells in the lung (Peinado et al., 2012). Mechanistically, transfer of MET from melanoma exosomes to c-Kit+ Tie2+ bone marrow progenitor cells results in a pro-vasculogenic behavior (Peinado et al., 2012). More recently, exosome-secreted MET has been suggested to promote hepatocellular carcinoma progression promoting the mobilization of normal hepatocytes, which may facilitate the protrusive activity of HCC cells through liver parenchyma during tumor metastasis (He et al., 2015). Evidence has demonstrated that gastrointestinal stromal tumors (GIST) release exosomes containing the oncogenic protein tyrosine kinase KIT and triggers the conversion of progenitor smooth muscle cells to tumor-promoting cells that promote tumor invasion (Atay et al., 2014).
Figure 2. Tumor-derived EVs promote pre-metastatic niche formation and metastasis.
EVs play a distinct role at multiple steps in PMN formation at distant sites of future metastasis. Depending on the cancer cell of origin, EVs can circulate through both blood and lymphatic vessels to reach their destination for PMN initiation. Through an unknown mechanism, tumor EVs can induce vascular leakiness and interact with the resident cells of distant organs. Depending on their membrane composition, such as specific exosomal integrin combinations (exosomal α6β4 and α6β1 integrins associated with lung metastasis / exosomal αvβ5 integrin with liver metastasis), EVs are targeted to particular resident cell types within a particular organ. Upon their uptake by the recipient cells, EVs can induce the expression of several inflammatory mediators (e.g. S100 family proteins, TGFβ, IL-6, IL-8 and TNFα), resulting in the activation and remodeling of stromal cells and the recruitment of BMDCs to the PMN, which are critical for tumor progression. In pancreatic cancer, migration inhibitory factor (MIF)-containing exosomes are taken up by Kupffer cells promoting TGFβ secretion. TGFβ, in turn, then induces fibronectin secretion by hepatic stellate cells. The increase in fibronectin ultimately leads to the recruitment of BMDC's, which are critical for establishment of the PMN. In melanoma, exosomes can educate BMDCs through the transfer of MET and help establish a PMN in the lung. Melanoma-derived exosomes can also prepare lymph node PMN formation, by promoting recruitment of melanoma cells, extracellular matrix deposition, and vascular proliferation in the lymph nodes.
Melanoma-derived exosomes promote cancer cell recruitment, extracellular matrix deposition, and vascular proliferation in the lymph nodes (Hood et al., 2011). Several genes related to cell recruitment (Stabilin 1, Ephrin receptor β4 and αv integrin), extracellular matrix (Mapk14, uPA, Laminin 5, Col 18α1, G-α13) and vascular growth factors (TNF-α, TNF-αip2, VEGF-B, HIF-1α, Thbs1) were upregulated by tumor-secreted exosomes in lymph nodes (Hood et al., 2011). Exosomes isolated from highly metastatic colorectal cancer promote metastasis by recruiting CXCR4-expressing stromal cells, establishing of a favorable metastatic microenvironment and reinforcing metastasis of low metastatic models (Wang et al., 2015).
Overall, these data support the role of tumor-derived EVs in both early and late PMN formation, and likely suggests their essential contribution to metastatic niche development upon the arrival of tumor cells as well as to the progression from micrometastatic to macrometastatic disease.
Clinical Potential of EVs as Biomarkers and Therapeutics
EVs as Biomarkers
Circulating tumor-derived EVs have emerged as promising biomarkers to monitor cancer progression and as novel targets for future anticancer therapies. Although many unanswered questions and methodological challenges remain, this rapidly advancing field will ultimately provide important insights into the relevance of EVs in the clinical setting.
Finding proteins unique to tumor-derived EVs has been the subject of intense research. One such tumor-derived EV biomarker is the epithelial cell adhesion molecule (EpCAM) (Runz et al., 2007). EpCAM positive exosomes increase during ovarian cancer progression and are significantly higher in patients with ovarian cancer than in women with benign ovarian disease and healthy control subjects (Taylor and Gercel-Taylor, 2008). Exosomal integrins (as opposed to tumor-expressed integrins) could serve as biomarkers to predict the likelihood of cancer as well as metastatic propensity for specific organ sites (Hoshino et al., 2015). Specific exosomal integrin combinations seem to dictate organ-specific metastasis. For instance, α6β4 and α6β1 exosomal integrins are associated with lung metastasis, αvβ5 exosomal integrin with liver metastasis, and αvβ3 exosomal integrin with brain metastasis models (Hoshino et al., 2015). Circulating exosomes from patients with Stage IV melanoma contain a protein signature consisting of the melanoma-specific protein tyrosinase-related protein-2 (TYRP2), very late antigen 4 (VLA-4), HSP70, and MET oncoprotein (Peinado et al., 2012). Furthermore, exosomes from plasma of melanoma patients are enriched in caveolin-1 compared to the healthy controls, rendering caveolin-1 positive exosomes as another potential melanoma biomarker (Logozzi et al., 2009). Serum-circulating exosomes from melanoma patients have been demonstrated to contain S100B and Melanoma Inhibitory Activity (MIA) (Alegre et al., 2016). High levels of exosomes carrying the melanoma marker Melan-A and characteristic miRNA signatures could be isolated from liver perfusates of patients with liver metastases from uveal melanoma (Eldh et al., 2014). Exosomal glypican-1 has also been proposed as a diagnostic and prognostic marker for pancreatic cancer disease (Melo et al., 2015). In patients with pancreatic ductal adenocarcinoma (PDAC), the quantity of the protein MIF within exosomes may serve as a prognostic marker for liver metastasis. Circulating exosomes from stage I PDAC patients who later developed liver metastasis exhibited enhanced levels of MIF compared to patients whose cancer did not progress and to healthy control subjects (Costa-Silva et al., 2015).
Exosomal genetic material also shows potential as a diagnostic marker of cancer and metastasis. Tumor specific mRNA isolated from microvesicles from serum and tissue of glioblastoma patients reflects the mutational status of EGFRvIII (Pelloski et al., 2007; Skog et al., 2008). Microvesicles also carry single-stranded DNA (ssDNA) that recapitulates genomic aberrations such as oncogene amplifications (i.e., c-Myc), in the primary tumor (Balaj et al., 2011). In the metastatic setting, a higher level of double-stranded DNA (dsDNA) in exosomes was found in aggressive melanoma as compared to melanoma with low metastatic potential or non-metastatic melanoma (Thakur et al., 2014). Importantly, exosomal dsDNA reflects the oncogenic mutational status of the respective parental cancer cell (Kahlert et al., 2014; Melo et al., 2015; Thakur et al., 2014), highlighting the utility of exosomal dsDNA as valuable biomarker for the detection of oncogenic mutations in the clinical setting.
MiRNAs within circulating EVs have diagnostic and/or prognostic potential for many cancer types. In patient serum, exosomal miR-17-92a was correlated with increased colon cancer recurrence and exosomal miR-19a was associated with a poorer prognosis (Matsumura et al., 2015). Serum exosomal levels of seven miRNAs were found significantly higher in primary colorectal cancer patients compared to healthy controls. These miRNA levels decreased after surgical resection of tumor, suggesting their potential tumor origin (Ogata-Kawata et al., 2014). Several miRNAs are differentially expressed in circulating tumor exosomes from prostate cancer, compared to controls (Bryant et al., 2012; Li et al., 2016). Exosomal miR-141 and miR-375 have been associated with metastatic prostate cancer (Bryant et al., 2012; Li et al., 2016). Another study associated higher levels of miR-1290 and miR-375 within serum exosomes with decreased survival in patients with castration-resistant tumors (Huang et al., 2015). Exosomal miR-107 and miR-574-3p concentrations were higher in the urine of men with prostate cancer compared with controls, suggesting EV- miRNAs could serve as a biomarker in other fluids (Bryant et al., 2012). In melanoma, lower levels of miR-125b in serum circulating exosomes were observed in advanced melanoma (Alegre et al., 2014). When comparing exosomes from patients with metastatic sporadic melanoma to patients with familial melanoma patients or unaffected control subjects, miR-17, miR-19a, miR-21, miR-126, and miR-149 were found to be expressed at higher levels (Pfeffer et al., 2015). Exosomal miR-21 has been correlated with esophageal cancer recurrence and distant metastasis (Liao et al., 2016). One of the hurdles faced by analyzing both EV and non-EV derived miRNAs is that they could originate from either tumor or non-tumor cells and therefore their origin is unknown. Thus, translational studies will be crucial to determine the clinical utility of miRNAs-containing EVs as tumor biomarkers.
EVs for Therapy: Novel Mode of Drug Delivery and New Drug Targets
The properties of cancer exosomes in modulating the immune system and transforming healthy cells toward a malignant phenotype illustrate the clinical potential of exosomes in immunotherapy, therapeutic targeting and drug delivery. Activation of anti-tumor specific T cell responses by DC exosomes has been proposed to play a key role in suppression of established tumor growth (Zitvogel et al., 1998). The strategy of loading DC-derived exosomes with MHC/tumor antigen has been used for phase I clinical trials in patients with advanced melanoma (MAGE-A3, melanoma-associated antigen) (Escudier et al., 2005) and non-small cell lung carcinomas (MAGE-A3, -A4, and –A10) (Morse et al., 2005). These two studies showed the feasibility of DC exosome production and a tolerable safety profile for DC exosome therapy. In a subsequent phase II clinical trial in patients with advanced non-small cell lung carcinomas, interferon-γ-maturated DC exosome therapy failed to show a durable clinical response, but increased NK cell activity was observed in some patients with low initial NKp30 expression, correlating with longer progression-free survival (Besse et al., 2016).
EV biogenesis serves as a key strategy for EV targeting in cancer therapy (Azmi et al., 2013; Bobrie et al., 2012; Iero et al., 2008). Several Rab proteins have been shown to be involved in the selective packaging and production of exosomes in both normal cells and tumor cells (Ostrowski et al., 2010; Rak, 2010; Raposo and Stoorvogel, 2013). Rab27a knockdown in highly metastatic melanoma cells led to significant reduction in exosome production, primary tumor size, and metastasis (Peinado et al., 2012). Thus, determining the profile of Rab proteins responsible for exosome release in cancer cells may lead to unique therapeutic opportunities. In addition to targeting EV production, targeting their specific oncogenic cargo (i.e MIF, MET) and transmembrane integrins may result in reduced metastasis.
Recently, tumor microvesicles have been implicated in promoting resistance to chemotherapy. Transfer of miR-100, miR-222 and miR-30a miRNAs from the exosomes derived from adriamycin- and docetaxel-resistant MCF-7 breast cancer cells to drug sensitive MCF-7 cells increased the drug resistance of the previously sensitive cell line, although this requires further validation to rule out induction of miRNA expression in drug sensitive cells (Chen et al., 2014). Boelens and colleagues demonstrated that exosomal RNA from stromal cells can be transferred to breast cancer cells, activating NOTCH3 as well as STAT1-dependent antiviral signaling in these cancer cell resulting in the expansion of cancer cells resistant to chemotherapy and radiation (Boelens et al., 2014). In addition to transfer of chemoresistance-associated biomolecules to recipient cells, another mechanism associated with chemoresistance is EV-mediated expulsion/sequestration of chemotherapeutic agents from cancer cells. To this effect, enhanced release of exosomes has been associated with increased cisplatin resistance in melanoma (Federici et al., 2014) as well as ovarian carcinoma cells (Safaei et al., 2005).
Based on their surface protein composition, exosomes may be directed to specific tissues (Costa-Silva et al., 2015; Hoshino et al., 2015). These properties make them promising nanovehicles for the biodelivery of therapeutic RNAs, proteins, and other agents. In fact, an in vivo proof of principle study showed that neuron-targeted exosomes loaded with BACE1 siRNAs significantly reduced BACE mRNA (60%) and protein (62%), specifically in neurons (Alvarez-Erviti et al., 2011). Similarly, exosomes loaded with artificial siRNA against MAPK were able to efficiently knockdown the MAPK1 gene upon their delivery into monocytes and lymphocytes in vitro (Wahlgren et al., 2012). A significant reduction of the RAD51 transcript was observed in human embryonic kidney 293 cells (HEK293) and HCT116 colon cancer cell lines upon their incubation with exosomes carrying siRNA against RAD51 by electroporation (Shtam et al., 2013). These examples of cargo manipulation suggest that exosomes may prove beneficial as drug delivery vehicles.
Future directions
Currently, there are few markers (i.e., TSG101, syntenin, and simultaneous expression of three tetraspanins [CD9, CD63 and CD81]) to distinguish exosomes from other EVs, such as microvesicles or apoptotic bodies (Kowal et al., 2016). Furthermore, no reliable methods are available to characterize exosomes secreted by normal tissues. Most studies to date are based on heterogeneous populations of EVs which leaves open the question of whether different EV subpopulations play unique biological roles in cancer progression. Do these various sized particles have distinct tumor cell origins (i.e., tumor stem cells)? Do heterogeneous particles target specific cell types and help facilitate formation of the PMN and metastatic microenvironment through different yet complementary mechanisms?
Further analysis of molecules, such as integrins, that define EV subpopulations involved in exosome uptake in metastatic organs is needed. Tumor exosomes exert their systemic effects partly through transfer of exosome cargo, resulting in the ‘reprogramming’ of stromal cells, immune cells and BMDCs. Is the underlying mechanism of reprogramming a genetic or epigenetic process? Are the effects permanent or transient? Interestingly, multiple observations suggest that exosomes may lead to the transfer of complete phenotypic features, resulting in a phenocopy of the tumor (Balaj et al., 2011; Costa-Silva et al., 2015; Hoshino et al., 2015; Peinado et al., 2012; Zomer et al., 2015). Advances in biomedical engineering would advance our understanding of exosome biology by providing answers to questions related to categorization, nomenclature, and function of EVs.
Currently available studies are based on exosome injection or in vitro models, but it is essential to analyze the role of exosomes in vivo through the generation of genetic models in which exosome dynamics could be monitored over time. How is the rate of exosome secretion changing as the primary tumor grows? Are exosomes complementary or redundant to soluble factors? Recently, development of a biotinylated EV-Gaussia luciferase reporter enabled in vivo tracking of IV-administered EVs (Lai et al., 2014). Furthermore, in vivo imaging of fluorescent and bioluminescent EV membrane reporters revealed that both EV uptake and translation of EV-delivered mRNAs in cancer cells occurred at a rapid rate (Lai et al., 2015). Ridder et al. have developed a Cre-lox-based model of tracking EV-mediated RNA transfer from tumor to MDSCs in the tumor microenvironment in vivo and showed immunosuppressive phenotype and miRNA profiles in response to EV uptake (Ridder et al., 2015). Strikingly, Van Rheenen et al. have developed an intravital model to visualize spontaneous exosome transfer where highly metastatic cell-derived exosomes were received by less metastatic tumor cells and distant stromal cells (Zomer et al., 2015). Pittet and colleagues have developed additional in vivo labeling models for tracking tumor exosome dissemination via lymphatics (Pucci et al., 2016). In vivo models will serve to confirm the multiple roles of tumor exosomes during the metastatic process and potentially identify novel functions of exosomes in tumor biology.
By transferring content from tumor cells to non-cancerous cells, tumor EVs potently influence recipient cell behavior and promote the development of an environment hospitable toward cancer growth, invasion, and metastasis. Decoding how cancer-derived EVs mediate inter-cellular communication and harnessing these mechanisms for diagnostic and therapeutic purposes holds great promise to further understand cancer's widely systemic effects on the body and to improve the standard of care for cancer patients.
Acknowledgments
The authors gratefully acknowledge support from the following funding sources: the National Cancer Institute (CA169538 and CA169416 to D.L and H.P.), the Department of Defense (W81XWH-13-1-0427, W81XWH-13-1-0249 and W81XWH-14-1-0199 to D.L), the Hartwell Foundation, The Manning Foundation, The Sohn Foundation, The STARR Consortium, The POETIC Consortium, the Paduano Foundation, Alex's Lemonade Stand Foundation, the Champalimaud Foundation (all to D.L), and the Daedalus Fund (Weill Cornell Medicine, to D.L). H.P. is supported by grants from MINECO (SAF2014-54541-R), ATRES-MEDIA – AXA, Asociación Española Contra el Cáncer, WHRI Academy, and Worldwide Cancer Research. B.K.T. was supported by the Jose Carreras Leukaemia Foundation (DJCLS R12/06). H.S.K is supported by a Physician-Scientist Program from the Yonsei University College of Medicine. J.M.W. is supported by a Medical Scientist Training Program grant from the National Institute of General Medical Sciences of the National Institutes of Health (T32GM007739). The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions
A.B., B.K.T., J.M.W., H.S.K., and H.P. wrote the article. H.P. and D.L. supervised the article.
References
- Abusamra AJ, Zhong Z, Zheng X, Li M, Ichim TE, Chin JL, Min WP. Tumor exosomes expressing Fas ligand mediate CD8+ T-cell apoptosis. Blood cells, molecules & diseases. 2005;35:169–173. doi: 10.1016/j.bcmd.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Admyre C, Bohle B, Johansson SM, Focke-Tejkl M, Valenta R, Scheynius A, Gabrielsson S. B cell-derived exosomes can present allergen peptides and activate allergen-specific T cells to proliferate and produce TH2-like cytokines. J Allergy Clin Immunol. 2007;120:1418–1424. doi: 10.1016/j.jaci.2007.06.040. [DOI] [PubMed] [Google Scholar]
- Al-Nedawi K, Meehan B, Micallef J, Lhotak V, May L, Guha A, Rak J. Intercellular transfer of the oncogenic receptor EGFRvIII by microvesicles derived from tumour cells. Nature cell biology. 2008;10:619–624. doi: 10.1038/ncb1725. [DOI] [PubMed] [Google Scholar]
- Alegre E, Sanmamed MF, Rodriguez C, Carranza O, Martin-Algarra S, Gonzalez A. Study of circulating microRNA-125b levels in serum exosomes in advanced melanoma. Archives of pathology & laboratory medicine. 2014;138:828–832. doi: 10.5858/arpa.2013-0134-OA. [DOI] [PubMed] [Google Scholar]
- Alegre E, Zubiri L, Perez-Gracia JL, Gonzalez-Cao M, Soria L, Martin-Algarra S, Gonzalez A. Circulating melanoma exosomes as diagnostic and prognosis biomarkers. Clinica chimica acta; international journal of clinical chemistry. 2016;454:28–32. doi: 10.1016/j.cca.2015.12.031. [DOI] [PubMed] [Google Scholar]
- Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- Atay S, Banskota S, Crow J, Sethi G, Rink L, Godwin AK. Oncogenic KIT-containing exosomes increase gastrointestinal stromal tumor cell invasion. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:711–716. doi: 10.1073/pnas.1310501111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atay S, Gercel-Taylor C, Kesimer M, Taylor DD. Morphologic and proteomic characterization of exosomes released by cultured extravillous trophoblast cells. Experimental cell research. 2011;317:1192–1202. doi: 10.1016/j.yexcr.2011.01.014. [DOI] [PubMed] [Google Scholar]
- Au Yeung CL, Co NN, Tsuruga T, Yeung TL, Kwan SY, Leung CS, Li Y, Lu ES, Kwan K, Wong KK, et al. Exosomal transfer of stroma-derived miR21 confers paclitaxel resistance in ovarian cancer cells through targeting APAF1. Nature communications. 2016;7:11150. doi: 10.1038/ncomms11150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azmi AS, Bao B, Sarkar FH. Exosomes in cancer development, metastasis, and drug resistance: a comprehensive review. Cancer metastasis reviews. 2013;32:623–642. doi: 10.1007/s10555-013-9441-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer C, Squadrito ML, Iruela-Arispe ML, De Palma M. Reciprocal interactions between endothelial cells and macrophages in angiogenic vascular niches. Experimental cell research. 2013;319:1626–1634. doi: 10.1016/j.yexcr.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaj L, Lessard R, Dai L, Cho YJ, Pomeroy SL, Breakefield XO, Skog J. Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nature communications. 2011;2:180. doi: 10.1038/ncomms1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benito-Martin A, Di Giannatale A, Ceder S, Peinado H. The new deal: a potential role for secreted vesicles in innate immunity and tumor progression. Frontiers in immunology. 2015;6:66. doi: 10.3389/fimmu.2015.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besse B, Charrier M, Lapierre V, Dansin E, Lantz O, Planchard D, Le Chevalier T, Livartoski A, Barlesi F, Laplanche A, et al. Dendritic cell-derived exosomes as maintenance immunotherapy after first line chemotherapy in NSCLC. Oncoimmunology. 2016;5:e1071008. doi: 10.1080/2162402X.2015.1071008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar S, Shinagawa K, Castellino FJ, Schorey JS. Exosomes released from macrophages infected with intracellular pathogens stimulate a proinflammatory response in vitro and in vivo. Blood. 2007;110:3234–3244. doi: 10.1182/blood-2007-03-079152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobrie A, Krumeich S, Reyal F, Recchi C, Moita LF, Seabra MC, Ostrowski M, Thery C. Rab27a supports exosome-dependent and -independent mechanisms that modify the tumor microenvironment and can promote tumor progression. Cancer research. 2012;72:4920–4930. doi: 10.1158/0008-5472.CAN-12-0925. [DOI] [PubMed] [Google Scholar]
- Boelens MC, Wu TJ, Nabet BY, Xu B, Qiu Y, Yoon T, Azzam DJ, Twyman-Saint Victor C, Wiemann BZ, Ishwaran H, et al. Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell. 2014;159:499–513. doi: 10.1016/j.cell.2014.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boukouris S, Mathivanan S. Exosomes in bodily fluids are a highly stable resource of disease biomarkers. Proteomics Clinical applications. 2015;9:358–367. doi: 10.1002/prca.201400114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RJ, Pawlowski T, Catto JW, Marsden G, Vessella RL, Rhees B, Kuslich C, Visakorpi T, Hamdy FC. Changes in circulating microRNA levels associated with prostate cancer. British journal of cancer. 2012;106:768–774. doi: 10.1038/bjc.2011.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmin F, Ladoire S, Mignot G, Vincent J, Bruchard M, Remy-Martin JP, Boireau W, Rouleau A, Simon B, Lanneau D, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. The Journal of clinical investigation. 2010;120:457–471. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Wang J, Shao C, Liu S, Yu Y, Wang Q, Cao X. Efficient induction of antitumor T cell immunity by exosomes derived from heat-shocked lymphoma cells. European journal of immunology. 2006;36:1598–1607. doi: 10.1002/eji.200535501. [DOI] [PubMed] [Google Scholar]
- Chen WX, Liu XM, Lv MM, Chen L, Zhao JH, Zhong SL, Ji MH, Hu Q, Luo Z, Wu JZ, Tang JH. Exosomes from drug-resistant breast cancer cells transmit chemoresistance by a horizontal transfer of microRNAs. PloS one. 2014;9:e95240. doi: 10.1371/journal.pone.0095240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevillet JR, Kang Q, Ruf IK, Briggs HA, Vojtech LN, Hughes SM, Cheng HH, Arroyo JD, Meredith EK, Gallichotte EN, et al. Quantitative and stoichiometric analysis of the microRNA content of exosomes. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:14888–14893. doi: 10.1073/pnas.1408301111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho JA, Park H, Lim EH, Lee KW. Exosomes from breast cancer cells can convert adipose tissue-derived mesenchymal stem cells into myofibroblast-like cells. International journal of oncology. 2012;40:130–138. doi: 10.3892/ijo.2011.1193. [DOI] [PubMed] [Google Scholar]
- Chow A, Zhou W, Liu L, Fong MY, Champer J, Van Haute D, Chin AR, Ren X, Gugiu BG, Meng Z, et al. Macrophage immunomodulation by breast cancer-derived exosomes requires Toll-like receptor 2-mediated activation of NF-kappaB. Scientific reports. 2014;4:5750. doi: 10.1038/srep05750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciardiello C, Cavallini L, Spinelli C, Yang J, Reis-Sobreiro M, de Candia P, Minciacchi VR, Di Vizio D. Focus on Extracellular Vesicles: New Frontiers of Cell-to-Cell Communication in Cancer. International journal of molecular sciences. 2016;17 doi: 10.3390/ijms17020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo M, Moita C, van Niel G, Kowal J, Vigneron J, Benaroch P, Manel N, Moita LF, Thery C, Raposo G. Analysis of ESCRT functions in exosome biogenesis, composition and secretion highlights the heterogeneity of extracellular vesicles. Journal of cell science. 2013;126:5553–5565. doi: 10.1242/jcs.128868. [DOI] [PubMed] [Google Scholar]
- Colombo M, Raposo G, Thery C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annual review of cell and developmental biology. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- Costa-Silva B, Aiello NM, Ocean AJ, Singh S, Zhang H, Thakur BK, Becker A, Hoshino A, Mark MT, Molina H, et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nature cell biology. 2015;17:816–826. doi: 10.1038/ncb3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Toro J, Herschlik L, Waldner C, Mongini C. Emerging roles of exosomes in normal and pathological conditions: new insights for diagnosis and therapeutic applications. Frontiers in immunology. 2015;6:203. doi: 10.3389/fimmu.2015.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wever O, Demetter P, Mareel M, Bracke M. Stromal myofibroblasts are drivers of invasive cancer growth. International journal of cancer Journal international du cancer. 2008;123:2229–2238. doi: 10.1002/ijc.23925. [DOI] [PubMed] [Google Scholar]
- Di Vizio D, Morello M, Dudley AC, Schow PW, Adam RM, Morley S, Mulholland D, Rotinen M, Hager MH, Insabato L, et al. Large oncosomes in human prostate cancer tissues and in the circulation of mice with metastatic disease. The American journal of pathology. 2012;181:1573–1584. doi: 10.1016/j.ajpath.2012.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldh M, Olofsson Bagge R, Lasser C, Svanvik J, Sjostrand M, Mattsson J, Lindner P, Choi DS, Gho YS, Lotvall J. MicroRNA in exosomes isolated directly from the liver circulation in patients with metastatic uveal melanoma. BMC cancer. 2014;14:962. doi: 10.1186/1471-2407-14-962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escudier B, Dorval T, Chaput N, Andre F, Caby MP, Novault S, Flament C, Leboulaire C, Borg C, Amigorena S, et al. Vaccination of metastatic melanoma patients with autologous dendritic cell (DC) derived-exosomes: results of thefirst phase I clinical trial. Journal of translational medicine. 2005;3:10. doi: 10.1186/1479-5876-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falati S, Liu Q, Gross P, Merrill-Skoloff G, Chou J, Vandendries E, Celi A, Croce K, Furie BC, Furie B. Accumulation of tissue factor into developing thrombi in vivo is dependent upon microparticle P-selectin glycoprotein ligand 1 and platelet P-selectin. The Journal of experimental medicine. 2003;197:1585–1598. doi: 10.1084/jem.20021868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federici C, Petrucci F, Caimi S, Cesolini A, Logozzi M, Borghi M, D'Ilio S, Lugini L, Violante N, Azzarito T, et al. Exosome release and low pH belong to a framework of resistance of human melanoma cells to cisplatin. PloS one. 2014;9:e88193. doi: 10.1371/journal.pone.0088193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fevrier B, Raposo G. Exosomes: endosomal-derived vesicles shipping extracellular messages. Current opinion in cell biology. 2004;16:415–421. doi: 10.1016/j.ceb.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Finger EC, Giaccia AJ. Hypoxia, inflammation, and the tumor microenvironment in metastatic disease. Cancer metastasis reviews. 2010;29:285–293. doi: 10.1007/s10555-010-9224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong MY, Zhou W, Liu L, Alontaga AY, Chandra M, Ashby J, Chow A, O'Connor ST, Li S, Chin AR, et al. Breast-cancer-secreted miR-122 reprograms glucose metabolism in premetastatic niche to promote metastasis. Nature cell biology. 2015;17:183–194. doi: 10.1038/ncb3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, Worthen GS, Albelda SM. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer cell. 2009;16:183–194. doi: 10.1016/j.ccr.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nature reviews Immunology. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galindo-Hernandez O, Serna-Marquez N, Castillo-Sanchez R, Salazar EP. Extracellular vesicles from MDA-MB-231 breast cancer cells stimulated with linoleic acid promote an EMT-like process in MCF10A cells. Prostaglandins, leukotrienes, and essential fatty acids. 2014;91:299–310. doi: 10.1016/j.plefa.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Gan HK, Cvrljevic AN, Johns TG. The epidermal growth factor receptor variant III (EGFRvIII): where wild things are altered. The FEBS journal. 2013;280:5350–5370. doi: 10.1111/febs.12393. [DOI] [PubMed] [Google Scholar]
- Grange C, Tapparo M, Collino F, Vitillo L, Damasco C, Deregibus MC, Tetta C, Bussolati B, Camussi G. Microvesicles released from human renal cancer stem cells stimulate angiogenesis and formation of lung premetastatic niche. Cancer research. 2011;71:5346–5356. doi: 10.1158/0008-5472.CAN-11-0241. [DOI] [PubMed] [Google Scholar]
- Guescini M, Genedani S, Stocchi V, Agnati LF. Astrocytes and Glioblastoma cells release exosomes carrying mtDNA. Journal of neural transmission. 2010;117:1–4. doi: 10.1007/s00702-009-0288-8. [DOI] [PubMed] [Google Scholar]
- Harding C, Heuser J, Stahl P. Receptor-mediated endocytosis of transferrin and recycling of the transferrin receptor in rat reticulocytes. The Journal of cell biology. 1983;97:329–339. doi: 10.1083/jcb.97.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He M, Qin H, Poon TC, Sze SC, Ding X, Co NN, Ngai SM, Chan TF, Wong N. Hepatocellular carcinoma-derived exosomes promote motility of immortalized hepatocyte through transfer of oncogenic proteins and RNAs. Carcinogenesis. 2015;36:1008–1018. doi: 10.1093/carcin/bgv081. [DOI] [PubMed] [Google Scholar]
- Headley MB, Bins A, Nip A, Roberts EW, Looney MR, Gerard A, Krummel MF. Visualization of immediate immune responses to pioneer metastatic cells in the lung. Nature. 2016;531:513–517. doi: 10.1038/nature16985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedlund M, Stenqvist AC, Nagaeva O, Kjellberg L, Wulff M, Baranov V, Mincheva-Nilsson L. Human placenta expresses and secretes NKG2D ligands via exosomes that down-modulate the cognate receptor expression: evidence for immunosuppressive function. Journal of immunology. 2009;183:340–351. doi: 10.4049/jimmunol.0803477. [DOI] [PubMed] [Google Scholar]
- Hendrix A, Hume AN. Exosome signaling in mammary gland development and cancer. The International journal of developmental biology. 2011;55:879–887. doi: 10.1387/ijdb.113391ah. [DOI] [PubMed] [Google Scholar]
- Hendrix A, Maynard D, Pauwels P, Braems G, Denys H, Van den Broecke R, Lambert J, Van Belle S, Cocquyt V, Gespach C, et al. Effect of the secretory small GTPase Rab27B on breast cancer growth, invasion, and metastasis. Journal of the National Cancer Institute. 2010;102:866–880. doi: 10.1093/jnci/djq153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood JL, San RS, Wickline SA. Exosomes released by melanoma cells prepare sentinel lymph nodes for tumor metastasis. Cancer research. 2011;71:3792–3801. doi: 10.1158/0008-5472.CAN-10-4455. [DOI] [PubMed] [Google Scholar]
- Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic Mark M, Molina H, Kohsaka S, Di Giannatale A, Ceder S, et al. Tumour exosome integrins determine organotropic metastasis. Nature. 2015;527:329–335. doi: 10.1038/nature15756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hron G, Kollars M, Weber H, Sagaster V, Quehenberger P, Eichinger S, Kyrle PA, Weltermann A. Tissue factor-positive microparticles: cellular origin and association with coagulation activation in patients with colorectal cancer. Thrombosis and haemostasis. 2007;97:119–123. [PubMed] [Google Scholar]
- Hsu C, Morohashi Y, Yoshimura S, Manrique-Hoyos N, Jung S, Lauterbach MA, Bakhti M, Gronborg M, Mobius W, Rhee J, et al. Regulation of exosome secretion by Rab35 and its GTPase-activating proteins TBC1D10A-C. The Journal of cell biology. 2010;189:223–232. doi: 10.1083/jcb.200911018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X, Yuan T, Liang M, Du M, Xia S, Dittmar R, Wang D, See W, Costello BA, Quevedo F, et al. Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. European urology. 2015;67:33–41. doi: 10.1016/j.eururo.2014.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Song N, Ding Y, Yuan S, Li X, Cai H, Shi H, Luo Y. Pulmonary vascular destabilization in the premetastatic phase facilitates lung metastasis. Cancer research. 2009;69:7529–7537. doi: 10.1158/0008-5472.CAN-08-4382. [DOI] [PubMed] [Google Scholar]
- Iero M, Valenti R, Huber V, Filipazzi P, Parmiani G, Fais S, Rivoltini L. Tumour-released exosomes and their implications in cancer immunity. Cell death and differentiation. 2008;15:80–88. doi: 10.1038/sj.cdd.4402237. [DOI] [PubMed] [Google Scholar]
- Johnstone RM, Adam M, Hammond JR, Orr L, Turbide C. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes). The Journal of biological chemistry. 1987;262:9412–9420. [PubMed] [Google Scholar]
- Jung T, Castellana D, Klingbeil P, Hernández IC, Vitacolonna M, Orlicky DJ, Roffler SR, Brodt P, Zöller M. CD44v6 Dependence of Premetastatic Niche Preparation by Exosomes. Neoplasia. 2009;11:1093–IN1017. doi: 10.1593/neo.09822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlert C, Melo SA, Protopopov A, Tang J, Seth S, Koch M, Zhang J, Weitz J, Chin L, Futreal A, Kalluri R. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and p53 DNA in the serum exosomes of patients with pancreatic cancer. The Journal of biological chemistry. 2014;289:3869–3875. doi: 10.1074/jbc.C113.532267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keerthikumar S, Gangoda L, Liem M, Fonseka P, Atukorala I, Ozcitti C, Mechler A, Adda CG, Ang CS, Mathivanan S. Proteogenomic analysis reveals exosomes are more oncogenic than ectosomes. Oncotarget. 2015;6:15375–15396. doi: 10.18632/oncotarget.3801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JW, Wieckowski E, Taylor DD, Reichert TE, Watkins S, Whiteside TL. Fas ligand-positive membranous vesicles isolated from sera of patients with oral cancer induce apoptosis of activated T lymphocytes. Clinical cancer research : an official journal of the American Association for Cancer Research. 2005;11:1010–1020. [PubMed] [Google Scholar]
- King HW, Michael MZ, Gleadle JM. Hypoxic enhancement of exosome release by breast cancer cells. BMC cancer. 2012;12:421. doi: 10.1186/1471-2407-12-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal J, Arras G, Colombo M, Jouve M, Morath JP, Primdal-Bengtson B, Dingli F, Loew D, Tkach M, Thery C. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proceedings of the National Academy of Sciences of the United States of America. 2016;113:E968–977. doi: 10.1073/pnas.1521230113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal J, Tkach M, Thery C. Biogenesis and secretion of exosomes. Current opinion in cell biology. 2014;29:116–125. doi: 10.1016/j.ceb.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Kucharzewska P, Christianson HC, Welch JE, Svensson KJ, Fredlund E, Ringner M, Morgelin M, Bourseau-Guilmain E, Bengzon J, Belting M. Exosomes reflect the hypoxic status of glioma cells and mediate hypoxia-dependent activation of vascular cells during tumor development. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:7312–7317. doi: 10.1073/pnas.1220998110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai CP, Kim EY, Badr CE, Weissleder R, Mempel TR, Tannous BA, Breakefield XO. Visualization and tracking of tumour extracellular vesicle delivery and RNA translation using multiplexed reporters. Nature communications. 2015;6:7029. doi: 10.1038/ncomms8029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai CP, Mardini O, Ericsson M, Prabhakar S, Maguire CA, Chen JW, Tannous BA, Breakefield XO. Dynamic biodistribution of extracellular vesicles in vivo using a multimodal imaging reporter. ACS Nano. 2014;8:483–494. doi: 10.1021/nn404945r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakkaraju A, Rodriguez-Boulan E. Itinerant exosomes: emerging roles in cell and tissue polarity. Trends in cell biology. 2008;18:199–209. doi: 10.1016/j.tcb.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee TH, D'Asti E, Magnus N, Al-Nedawi K, Meehan B, Rak J. Microvesicles as mediators of intercellular communication in cancer--the emerging science of cellular ‘debris’. Semin Immunopathol. 2011;33:455–467. doi: 10.1007/s00281-011-0250-3. [DOI] [PubMed] [Google Scholar]
- Lener T, Gimona M, Aigner L, Borger V, Buzas E, Camussi G, Chaput N, Chatterjee D, Court FA, Del Portillo HA, et al. Applying extracellular vesicles based therapeutics in clinical trials - an ISEV position paper. Journal of extracellular vesicles. 2015;4:30087. doi: 10.3402/jev.v4.30087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Ma YY, Wang J, Zeng XF, Li R, Kang W, Hao XK. Exosomal microRNA-141 is upregulated in the serum of prostate cancer patients. OncoTargets and therapy. 2016;9:139–148. doi: 10.2147/OTT.S95565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao J, Liu R, Shi YJ, Yin LH, Pu YP. Exosome-shuttling microRNA-21 promotes cell migration and invasion-targeting PDCD4 in esophageal cancer. International journal of oncology. 2016;48:2567–2579. doi: 10.3892/ijo.2016.3453. [DOI] [PubMed] [Google Scholar]
- Liu C, Yu S, Zinn K, Wang J, Zhang L, Jia Y, Kappes JC, Barnes S, Kimberly RP, Grizzle WE, Zhang HG. Murine mammary carcinoma exosomes promote tumor growth by suppression of NK cell function. J Immunol. 2006;176:1375–1385. doi: 10.4049/jimmunol.176.3.1375. [DOI] [PubMed] [Google Scholar]
- Liu Y, Gu Y, Han Y, Zhang Q, Jiang Z, Zhang X, Huang B, Xu X, Zheng J, Cao X. Tumor exosomal RNAs promote lung pre-metastatic niche formation by activating alveolar epithelial TLR3 to recruit neutrophils. Cancer cell. 2016;30 doi: 10.1016/j.ccell.2016.06.021. [DOI] [PubMed] [Google Scholar]
- Liu Y, Zhao L, Li D, Yin Y, Zhang CY, Li J, Zhang Y. Microvesicle-delivery miR-150 promotes tumorigenesis by up-regulating VEGF, and the neutralization of miR-150 attenuate tumor development. Protein & cell. 2013;4:932–941. doi: 10.1007/s13238-013-3092-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logozzi M, De Milito A, Lugini L, Borghi M, Calabro L, Spada M, Perdicchio M, Marino ML, Federici C, Iessi E, et al. High levels of exosomes expressing CD63 and caveolin-1 in plasma of melanoma patients. PloS one. 2009;4:e5219. doi: 10.1371/journal.pone.0005219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luga V, Zhang L, Viloria-Petit AM, Ogunjimi AA, Inanlou MR, Chiu E, Buchanan M, Hosein AN, Basik M, Wrana JL. Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell. 2012;151:1542–1556. doi: 10.1016/j.cell.2012.11.024. [DOI] [PubMed] [Google Scholar]
- Matsumura T, Sugimachi K, Iinuma H, Takahashi Y, Kurashige J, Sawada G, Ueda M, Uchi R, Ueo H, Takano Y, et al. Exosomal microRNA in serum is a novel biomarker of recurrence in human colorectal cancer. British journal of cancer. 2015;113:275–281. doi: 10.1038/bjc.2015.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, LeBleu VS, Mittendorf EA, Weitz J, Rahbari N, et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature. 2015;523:177–182. doi: 10.1038/nature14581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo SA, Sugimoto H, O'Connell JT, Kato N, Villanueva A, Vidal A, Qiu L, Vitkin E, Perelman LT, Melo CA, et al. Cancer exosomes perform cell-independent microRNA biogenesis and promote tumorigenesis. Cancer cell. 2014;26:707–721. doi: 10.1016/j.ccell.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello M, Minciacchi VR, de Candia P, Yang J, Posadas E, Kim H, Griffiths D, Bhowmick N, Chung LW, Gandellini P, et al. Large oncosomes mediate intercellular transfer of functional microRNA. Cell cycle. 2013;12:3526–3536. doi: 10.4161/cc.26539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse MA, Garst J, Osada T, Khan S, Hobeika A, Clay TM, Valente N, Shreeniwas R, Sutton MA, Delcayre A, et al. A phase I study of dexosome immunotherapy in patients with advanced non-small cell lung cancer. Journal of translational medicine. 2005;3:9. doi: 10.1186/1479-5876-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazarenko I, Rana S, Baumann A, McAlear J, Hellwig A, Trendelenburg M, Lochnit G, Preissner KT, Zoller M. Cell surface tetraspanin Tspan8 contributes to molecular pathways of exosome-induced endothelial cell activation. Cancer research. 2010;70:1668–1678. doi: 10.1158/0008-5472.CAN-09-2470. [DOI] [PubMed] [Google Scholar]
- Ogata-Kawata H, Izumiya M, Kurioka D, Honma Y, Yamada Y, Furuta K, Gunji T, Ohta H, Okamoto H, Sonoda H, et al. Circulating exosomal microRNAs as biomarkers of colon cancer. PloS one. 2014;9:e92921. doi: 10.1371/journal.pone.0092921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ono M, Kosaka N, Tominaga N, Yoshioka Y, Takeshita F, Takahashi RU, Yoshida M, Tsuda H, Tamura K, Ochiya T. Exosomes from bone marrow mesenchymal stem cells contain a microRNA that promotes dormancy in metastatic breast cancer cells. Science signaling. 2014;7:ra63. doi: 10.1126/scisignal.2005231. [DOI] [PubMed] [Google Scholar]
- Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, Moita CF, Schauer K, Hume AN, Freitas RP, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nature cell biology. 2010;12:19–30. doi: 10.1038/ncb2000. sup pp 11-13. [DOI] [PubMed] [Google Scholar]
- Paget S. The distribution of secondary growths in cancer of the breast. 1889. Cancer metastasis reviews. 1989;8:98–101. [PubMed] [Google Scholar]
- Pan BT, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell. 1983;33:967–978. doi: 10.1016/0092-8674(83)90040-5. [DOI] [PubMed] [Google Scholar]
- Pap E, Pallinger E, Falus A, Kiss AA, Kittel A, Kovacs P, Buzas EI. T lymphocytes are targets for platelet- and trophoblast-derived microvesicles during pregnancy. Placenta. 2008;29:826–832. doi: 10.1016/j.placenta.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Peinado H, Aleckovic M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, Hergueta-Redondo M, Williams C, Garcia-Santos G, Ghajar C, et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nature medicine. 2012;18:883–891. doi: 10.1038/nm.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peinado H, Lavotshkin S, Lyden D. The secreted factors responsible for pre-metastatic niche formation: old sayings and new thoughts. Seminars in cancer biology. 2011;21:139–146. doi: 10.1016/j.semcancer.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Pelloski CE, Ballman KV, Furth AF, Zhang L, Lin E, Sulman EP, Bhat K, McDonald JM, Yung WK, Colman H, et al. Epidermal growth factor receptor variant III status defines clinically distinct subtypes of glioblastoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25:2288–2294. doi: 10.1200/JCO.2006.08.0705. [DOI] [PubMed] [Google Scholar]
- Pfeffer SR, Grossmann KF, Cassidy PB, Yang CH, Fan M, Kopelovich L, Leachman SA, Pfeffer LM. Detection of Exosomal miRNAs in the Plasma of Melanoma Patients. Journal of clinical medicine. 2015;4:2012–2027. doi: 10.3390/jcm4121957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteryaev D, Datta S, Ackema K, Zerial M, Spang A. Identification of the switch in early-to-late endosome transition. Cell. 2010;141:497–508. doi: 10.1016/j.cell.2010.03.011. [DOI] [PubMed] [Google Scholar]
- Psaila B, Lyden D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer. 2009;9:285–293. doi: 10.1038/nrc2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pucci F, Garris C, Lai CP, Newton A, Pfirschke C, Engblom C, Alvarez D, Sprachman M, Evavold C, Magnuson A, et al. SCS macrophages suppress melanoma by restricting tumor-derived vesicle-B cell interactions. Science. 2016 doi: 10.1126/science.aaf1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rak J. Microparticles in cancer. Seminars in thrombosis and hemostasis. 2010;36:888–906. doi: 10.1055/s-0030-1267043. [DOI] [PubMed] [Google Scholar]
- Rana S, Malinowska K, Zoller M. Exosomal tumor microRNA modulates premetastatic organ cells. Neoplasia. 2013;15:281–295. doi: 10.1593/neo.122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raposo G, Nijman HW, Stoorvogel W, Liejendekker R, Harding CV, Melief CJ, Geuze HJ. B lymphocytes secrete antigen-presenting vesicles. The Journal of experimental medicine. 1996;183:1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. The Journal of cell biology. 2013;200:373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratajczak J, Wysoczynski M, Hayek F, Janowska-Wieczorek A, Ratajczak MZ. Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication. Leukemia. 2006;20:1487–1495. doi: 10.1038/sj.leu.2404296. [DOI] [PubMed] [Google Scholar]
- Ridder K, Sevko A, Heide J, Dams M, Rupp AK, Macas J, Starmann J, Tjwa M, Plate KH, Sultmann H, et al. Extracellular vesicle-mediated transfer of functional RNA in the tumor microenvironment. Oncoimmunology. 2015;4:e1008371. doi: 10.1080/2162402X.2015.1008371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runz S, Keller S, Rupp C, Stoeck A, Issa Y, Koensgen D, Mustea A, Sehouli J, Kristiansen G, Altevogt P. Malignant ascites-derived exosomes of ovarian carcinoma patients contain CD24 and EpCAM. Gynecologic oncology. 2007;107:563–571. doi: 10.1016/j.ygyno.2007.08.064. [DOI] [PubMed] [Google Scholar]
- Saadeldin IM, Kim SJ, Choi YB, Lee BC. Improvement of cloned embryos development by co-culturing with parthenotes: a possible role of exosomes/microvesicles for embryos paracrine communication. Cellular reprogramming. 2014;16:223–234. doi: 10.1089/cell.2014.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadeldin IM, Oh HJ, Lee BC. Embryonic-maternal cross-talk via exosomes: potential implications. Stem cells and cloning : advances and applications. 2015;8:103–107. doi: 10.2147/SCCAA.S84991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safaei R, Larson BJ, Cheng TC, Gibson MA, Otani S, Naerdemann W, Howell SB. Abnormal lysosomal trafficking and enhanced exosomal export of cisplatin in drug-resistant human ovarian carcinoma cells. Molecular cancer therapeutics. 2005;4:1595–1604. doi: 10.1158/1535-7163.MCT-05-0102. [DOI] [PubMed] [Google Scholar]
- Sanchez CA, Andahur EI, Valenzuela R, Castellon EA, Fulla JA, Ramos CG, Trivino JC. Exosomes from bulk and stem cells from human prostate cancer have a differential microRNA content that contributes cooperatively over local and premetastatic niche. Oncotarget. 2016;7:3993–4008. doi: 10.18632/oncotarget.6540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savina A, Fader CM, Damiani MT, Colombo MI. Rab11 promotes docking and fusion of multivesicular bodies in a calcium-dependent manner. Traffic. 2005;6:131–143. doi: 10.1111/j.1600-0854.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- Shtam TA, Kovalev RA, Varfolomeeva EY, Makarov EM, Kil YV, Filatov MV. Exosomes are natural carriers of exogenous siRNA to human cells in vitro. Cell communication and signaling : CCS. 2013;11:88. doi: 10.1186/1478-811X-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidhu SS, Mengistab AT, Tauscher AN, LaVail J, Basbaum C. The microvesicle as a vehicle for EMMPRIN in tumor-stromal interactions. Oncogene. 2004;23:956–963. doi: 10.1038/sj.onc.1207070. [DOI] [PubMed] [Google Scholar]
- Sierko E, Wojtukiewicz MZ. Inhibition of platelet function: does it offer a chance of better cancer progression control? Seminars in thrombosis and hemostasis. 2007;33:712–721. doi: 10.1055/s-2007-991540. [DOI] [PubMed] [Google Scholar]
- Simons M, Raposo G. Exosomes--vesicular carriers for intercellular communication. Curr Opin Cell Biol. 2009;21:575–581. doi: 10.1016/j.ceb.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Skog J, Wurdinger T, van Rijn S, Meijer DH, Gainche L, Sena-Esteves M, Curry WT, Jr., Carter BS, Krichevsky AM, Breakefield XO. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nature cell biology. 2008;10:1470–1476. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squadrito ML, Baer C, Burdet F, Maderna C, Gilfillan GD, Lyle R, Ibberson M, De Palma M. Endogenous RNAs modulate microRNA sorting to exosomes and transfer to acceptor cells. Cell reports. 2014;8:1432–1446. doi: 10.1016/j.celrep.2014.07.035. [DOI] [PubMed] [Google Scholar]
- Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. The American journal of medicine. 2006;119:60–68. doi: 10.1016/j.amjmed.2005.06.058. [DOI] [PubMed] [Google Scholar]
- Stenqvist AC, Nagaeva O, Baranov V, Mincheva-Nilsson L. Exosomes secreted by human placenta carry functional Fas ligand and TRAIL molecules and convey apoptosis in activated immune cells, suggesting exosome-mediated immune privilege of the fetus. Journal of immunology. 2013;191:5515–5523. doi: 10.4049/jimmunol.1301885. [DOI] [PubMed] [Google Scholar]
- Suetsugu A, Honma K, Saji S, Moriwaki H, Ochiya T, Hoffman RM. Imaging exosome transfer from breast cancer cells to stroma at metastatic sites in orthotopic nude-mouse models. Advanced drug delivery reviews. 2013;65:383–390. doi: 10.1016/j.addr.2012.08.007. [DOI] [PubMed] [Google Scholar]
- Sung BH, Ketova T, Hoshino D, Zijlstra A, Weaver AM. Directional cell movement through tissues is controlled by exosome secretion. Nature communications. 2015;6:7164. doi: 10.1038/ncomms8164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taraboletti G, D'Ascenzo S, Borsotti P, Giavazzi R, Pavan A, Dolo V. Shedding of the matrix metalloproteinases MMP-2, MMP-9, and MT1-MMP as membrane vesicle-associated components by endothelial cells. The American journal of pathology. 2002;160:673–680. doi: 10.1016/S0002-9440(10)64887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauro BJ, Mathias RA, Greening DW, Gopal SK, Ji H, Kapp EA, Coleman BM, Hill AF, Kusebauch U, Hallows JL, et al. Oncogenic H-ras reprograms Madin-Darby canine kidney (MDCK) cell-derived exosomal proteins following epithelialmesenchymal transition. Molecular & cellular proteomics : MCP. 2013;12:2148–2159. doi: 10.1074/mcp.M112.027086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DD, Gercel-Taylor C. MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecologic oncology. 2008;110:13–21. doi: 10.1016/j.ygyno.2008.04.033. [DOI] [PubMed] [Google Scholar]
- Thakur BK, Zhang H, Becker A, Matei I, Huang Y, Costa-Silva B, Zheng Y, Hoshino A, Brazier H, Xiang J, et al. Double-stranded DNA in exosomes: a novel biomarker in cancer detection. Cell research. 2014;24:766–769. doi: 10.1038/cr.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thery C, Ostrowski M, Segura E. Membrane vesicles as conveyors of immune responses. Nature reviews Immunology. 2009;9:581–593. doi: 10.1038/nri2567. [DOI] [PubMed] [Google Scholar]
- Thomas GM, Panicot-Dubois L, Lacroix R, Dignat-George F, Lombardo D, Dubois C. Cancer cell-derived microparticles bearing P-selectin glycoprotein ligand 1 accelerate thrombus formation in vivo. The Journal of experimental medicine. 2009;206:1913–1927. doi: 10.1084/jem.20082297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilley RE, Holscher T, Belani R, Nieva J, Mackman N. Tissue factor activity is increased in a combined platelet and microparticle sample from cancer patients. Thrombosis research. 2008;122:604–609. doi: 10.1016/j.thromres.2007.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trajkovic K, Hsu C, Chiantia S, Rajendran L, Wenzel D, Wieland F, Schwille P, Brugger B, Simons M. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319:1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- Trams EG, Lauter CJ, Salem N, Jr., Heine U. Exfoliation of membrane ecto-enzymes in the form of micro-vesicles. Biochimica et biophysica acta. 1981;645:63–70. doi: 10.1016/0005-2736(81)90512-5. [DOI] [PubMed] [Google Scholar]
- Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nature cell biology. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- van der Pol E, Boing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacological reviews. 2012;64:676–705. doi: 10.1124/pr.112.005983. [DOI] [PubMed] [Google Scholar]
- van Niel G, Porto-Carreiro I, Simoes S, Raposo G. Exosomes: a common pathway for a specialized function. Journal of biochemistry. 2006;140:13–21. doi: 10.1093/jb/mvj128. [DOI] [PubMed] [Google Scholar]
- Wahlgren J, De LKT, Brisslert M, Vaziri Sani F, Telemo E, Sunnerhagen P, Valadi H. Plasma exosomes can deliver exogenous short interfering RNA to monocytes and lymphocytes. Nucleic acids research. 2012;40:e130. doi: 10.1093/nar/gks463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Ding X, Nan L, Wang Y, Wang J, Yan Z, Zhang W, Sun J, Zhu W, Ni B, et al. Investigation of the roles of exosomes in colorectal cancer liver metastasis. Oncology reports. 2015;33:2445–2453. doi: 10.3892/or.2015.3843. [DOI] [PubMed] [Google Scholar]
- Webber J, Steadman R, Mason MD, Tabi Z, Clayton A. Cancer exosomes trigger fibroblast to myofibroblast differentiation. Cancer research. 2010;70:9621–9630. doi: 10.1158/0008-5472.CAN-10-1722. [DOI] [PubMed] [Google Scholar]
- Wolf P. The nature and significance of platelet products in human plasma. British journal of haematology. 1967;13:269–288. doi: 10.1111/j.1365-2141.1967.tb08741.x. [DOI] [PubMed] [Google Scholar]
- Wolfers J, Lozier A, Raposo G, Regnault A, Thery C, Masurier C, Flament C, Pouzieux S, Faure F, Tursz T, et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nature medicine. 2001;7:297–303. doi: 10.1038/85438. [DOI] [PubMed] [Google Scholar]
- Xiang X, Liu Y, Zhuang X, Zhang S, Michalek S, Taylor DD, Grizzle W, Zhang HG. TLR2-mediated expansion of MDSCs is dependent on the source of tumor exosomes. The American journal of pathology. 2010;177:1606–1610. doi: 10.2353/ajpath.2010.100245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J, May L, Milsom C, Anderson GM, Weitz JI, Luyendyk JP, Broze G, Mackman N, Rak J. Contribution of host-derived tissue factor to tumor neovascularization. Arteriosclerosis, thrombosis, and vascular biology. 2008;28:1975–1981. doi: 10.1161/ATVBAHA.108.175083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu JL, May L, Lhotak V, Shahrzad S, Shirasawa S, Weitz JI, Coomber BL, Mackman N, Rak JW. Oncogenic events regulate tissue factor expression in colorectal cancer cells: implications for tumor progression and angiogenesis. Blood. 2005;105:1734–1741. doi: 10.1182/blood-2004-05-2042. [DOI] [PubMed] [Google Scholar]
- Zhang L, Zhang S, Yao J, Lowery FJ, Zhang Q, Huang WC, Li P, Li M, Wang X, Zhang C, et al. Microenvironment-induced PTEN loss by exosomal microRNA primes brain metastasis outgrowth. Nature. 2015;527:100–104. doi: 10.1038/nature15376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Fong MY, Min Y, Somlo G, Liu L, Palomares MR, Yu Y, Chow A, O'Connor ST, Chin AR, et al. Cancer-secreted miR-105 destroys vascular endothelial barriers to promote metastasis. Cancer cell. 2014;25:501–515. doi: 10.1016/j.ccr.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitvogel L, Regnault A, Lozier A, Wolfers J, Flament C, Tenza D, Ricciardi-Castagnoli P, Raposo G, Amigorena S. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell-derived exosomes. Nature medicine. 1998;4:594–600. doi: 10.1038/nm0598-594. [DOI] [PubMed] [Google Scholar]
- Zomer A, Maynard C, Verweij FJ, Kamermans A, Schafer R, Beerling E, Schiffelers RM, de Wit E, Berenguer J, Ellenbroek SI, et al. In Vivo imaging reveals extracellular vesicle-mediated phenocopying of metastatic behavior. Cell. 2015;161:1046–1057. doi: 10.1016/j.cell.2015.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]