Abstract
Background:
Many studies report a positive association between smoking and mental illness. However, the literature remains mixed regarding the direction of this association. We therefore conducted a systematic review evaluating the association of smoking and depression and/or anxiety in longitudinal studies.
Methods:
Studies were identified by searching PubMed, Scopus, and Web of Science and were included if they: (1) used human participants, (2) were longitudinal, (3) reported primary data, (4) had smoking as an exposure and depression and/or anxiety as an outcome, or (5) had depression and/or anxiety as the exposure and smoking as an outcome.
Results:
Outcomes from 148 studies were categorized into: smoking onset, smoking status, smoking heaviness, tobacco dependence, and smoking trajectory. The results for each category varied substantially, with evidence for positive associations in both directions (smoking to later mental health and mental health to later smoking) as well as null findings. Overall, nearly half the studies reported that baseline depression/anxiety was associated with some type of later smoking behavior, while over a third found evidence that a smoking exposure was associated with later depression/anxiety. However, there were few studies directly supporting a bidirectional model of smoking and anxiety, and very few studies reporting null results.
Conclusions:
The literature on the prospective association between smoking and depression and anxiety is inconsistent in terms of the direction of association most strongly supported. This suggests the need for future studies that employ different methodologies, such as Mendelian randomization (MR), which will allow us to draw stronger causal inferences.
Implications:
We systematically reviewed longitudinal studies on the association of different aspects of smoking behavior with depression and anxiety. The results varied considerably, with evidence for smoking both associated with subsequent depression and anxiety, and vice versa. Few studies supported a bidirectional relationship, or reported null results, and no clear patterns by gender, ethnicity, clinical status, length to follow-up, or diagnostic test. Suggesting that despite advantages of longitudinal studies, they cannot alone provide strong evidence of causality. Therefore, future studies investigating this association should employ different methods allowing for stronger causal inferences to be made, such as MR.
Introduction
The high co-occurrence of smoking and mental illness is a major public health concern, and smoking accounts for much of the reduction in life expectancy associated with mental illness.1 Many studies report a positive association between smoking and mental illness, with smoking rates increasing with the severity of the disease.2,3 Individuals with mental illness also tend to start smoking at an earlier age, smoke more heavily, and are more addicted to cigarettes than the general population. For example, a recent survey suggests that 42% of all cigarettes consumed in England are consumed by those with mental illness, although this includes substance use disorders.4 Additionally, while cigarette consumption in the general population has shown a sustained decrease over the past 20 years, consumption among smokers with mental illness has remained relatively unchanged.1 There is therefore a pressing need to understand the mechanisms underlying the high rate of smoking in people with mental illness. Here, we focus specifically on the relationship between cigarette smoking and depression and anxiety.
Currently, there are several hypotheses that have been proposed to explain the high rates of smoking in people with depression and anxiety. The self-medication hypothesis postulates that individuals turn to smoking to alleviate their symptoms5–7 and therefore suggests that symptoms of depression and anxiety may lead to smoking. An alternative hypothesis is that smoking may lead to depression or anxiety, through effects on an individual’s neurocircuitry that increases susceptibility to environmental stressors. Animal models indicate that prolonged nicotine exposure dysregulates the hypothalamic–pituitary–adrenal system, resulting in hypersecretion of cortisol and alterations in the activity of the associated monoamine neurotransmitter system, whose function is to regulate reactions to stressors,8 an effect that appears to normalize after nicotine withdrawal.9 The association between smoking and depression/anxiety may also be bidirectional, with occasional smoking initially used to alleviate symptoms, but in fact worsening them over time.10 Finally, there may in fact be no causal relationship between smoking and depression/anxiety. Instead, the association may be a product of shared risk factors (eg, common genetic influences)10,11 or confounding. Smokers may also report that cigarettes alleviate their symptoms due to the misattribution of withdrawal relief. Given the short half-life of nicotine that results in withdrawal symptoms (including mood symptoms) after a short period of abstinence, smokers may misattribute the relief of short-term withdrawal as reflecting a genuine anxiolytic effect of smoking.7 That is, withdrawal symptoms of increased anxiety and negative affect may be misattributed as reflecting genuine mood symptoms, which would lead to the impression that smoking improves mood.
We are therefore presented with multiple different hypotheses regarding whether there is a causal relationship between smoking and depression/anxiety and if so, what the direction of causality underlying this relationship is. While experimental studies are generally not possible, for both practical and ethical reasons, longitudinal studies may help inform our understanding of the causal relationship between smoking and depression/anxiety by clarifying the temporal association. Our study aimed to systematically review the literature comprising longitudinal studies of the associations between smoking and depression/anxiety and conduct meta-analyses where possible. To the best of our knowledge, this is the first systematic review of this literature.
Methods
Identification of Studies
We searched PubMed, Scopus, and Web of Science up until August 1, 2015 using the following search terms: depressi*, anxi*, smok*, tobacco, nicotine, cigarette, caus*, cohort, prospective, longitudinal. The term animal* was specified for exclusion. Two authors (MF and AT) reviewed the electronic abstracts, selecting the full-text articles to be included.
Selection Criteria
Studies were included in the review if they met the following criteria: (1) human participants, (2) smoking as the exposure variable and depression and/or anxiety as the outcome variable, or vice versa (depression and/or anxiety as the exposure variable and smoking as the outcome variable), (3) longitudinal study design, and (4) reported primary data not previously reported elsewhere. Studies involving cessation, withdrawal, suicide, or trauma, which recruited participants who were pregnant or diagnosed with a psychiatric illness other than depression or anxiety, or included participants with depression and anxiety comorbid with another psychiatric illness were excluded. Studies not utilizing a validated diagnostic test for depression or anxiety were excluded. Studies investigating the association of parental smoking on offspring outcomes were also excluded, as were all experimental studies (eg, randomized controlled trials of smoking cessation interventions). RCTs as well as secondary analyses of randomized controlled trials were excluded.
Data Extraction
The following information was extracted from each of the included studies, by one author (MF): type of depression/anxiety (major depression, generalized anxiety disorder, mixed major depression, and generalized anxiety disorder), method of measuring depression/anxiety (self-report via diagnostic test, clinical interview, or physician diagnosis) and scale used (continuous or categorical), smoking behavior (age of smoking onset, smoking status, heaviness of smoking, tobacco dependence, smoking trajectory), sample size, mean age of participants and sex distribution of participants, population sampled (eg, general or clinical), and length of follow up. A 100% data check was performed by the same author (MF) and a 10% data check was independently performed by another author (MG) to identify data extraction errors. Any errors identified were resolved by mutual consent.
Rationale for not Conducting Meta-analysis
A meta-analysis was not conducted as, even within the general population samples available, there was substantial heterogeneity (age, location, covariates used, time to follow up, and number of times and frequency of outcomes sampled). Additionally, the studies included were not limited to only those examining an a priori hypothesis of mental health and smoking; studies were included if they contained the desired outcome and exposure variables within their data set.
Results
Characteristics of Included Studies
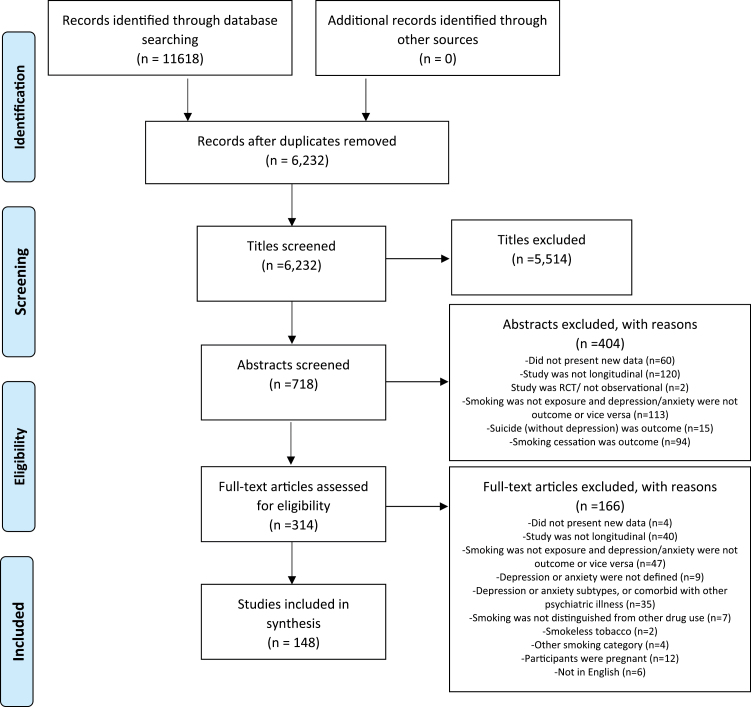
Of the 6232 abstracts reviewed, 5514 were excluded on the basis of title and 404 after reviewing the abstract. In total, 314 articles were retrieved and assessed for eligibility, and 148 met inclusion criteria (Figure 1). Details of included studies are provided in Supplementary Table S1 and details of excluded full-text studies in Supplementary Table S2.
Figure 1.
Identification of independent studies for inclusion in systematic review.
Studies ranged in sample size from 59 to 90 627 participants and in length of follow up from 2 months to 36 years. Of the 148 included studies, 99 (67%) recruited male and female participants, 16 (11%) recruited only females and 7 (5%) recruited only males, while 26 (18%) did not report the sex of the participants. In addition, 101 studies (70%) sampled participants from the general population, 15 (10%) from clinical populations, and 16 (10%) from particular ethnic groups, while 16 (10%) had other selection criteria (see Supplementary Table S2).
Unless otherwise stated, the associations described refer to a positive relationship between smoking and depression/anxiety (ie, smoking is associated with increased depression/anxiety, or increased depression/anxiety is associated with increased smoking).
Smoking Categories
Studies were categorized based on the basis of the smoking behavior(s) they assessed: smoking onset, smoking status, smoking heaviness, tobacco dependence, and smoking trajectory. Studies with measures of daily or weekly cigarette use were included in the smoking heaviness category. Studies that were able to establish the onset of smoking from an initially nonsmoking population were included in the smoking onset category. Studies that measured tobacco dependence, for example, through the DSM-IV 12 or the Fagerström Test for Nicotine Dependence,13 were included in the tobacco dependence category. Studies that tracked the different paths of cigarette smoking uptake and use in a cohort were included in the smoking trajectory category, and studies that defined smokers in purely categorical terms (eg, current, former, and never) were included in the smoking status category. Table 1 summarizes the directions of associations investigated within the studies in each smoking category.
Table 1.
Directions of Associations Investigated by Smoking Category
| Category | Depression | Anxiety | Comorbid depression and anxiety | ||||||
|---|---|---|---|---|---|---|---|---|---|
| MH into smoking | Smoking into MH | Bidirectional | MH into smoking | Smoking into MH | Bidirectional | MH into smoking | Smoking into MH | Bidirectional | |
| Smoking onset | 13 | 0 | 1 | 4 | 0 | 2 | 5 | 0 | 1 |
| Smoking status | 29 | 40 | 8 | 0 | 4 | 1 | 1 | 7 | 0 |
| Smoking heaviness | 9 | 7 | 2 | 1 | 1 | 0 | 0 | 1 | 0 |
| Tobacco dependence | 12 | 2 | 1 | 6 | 0 | 0 | 5 | 1 | 0 |
| Smoking trajectory | 7 | 2 | 0 | 1 | 0 | 0 | 1 | 1 | 0 |
| Any smoking category | 70 | 51 | 12 | 12 | 5 | 3 | 12 | 10 | 1 |
The number of studies investigating each direction(s) of association for each smoking category is shown. Studies investigating multiple directions are repeated within smoking category. Please note these only include directions investigated and differ from the overall findings within smoking groups detailed in Figure 2. MH = mental health outcome.
Smoking Onset
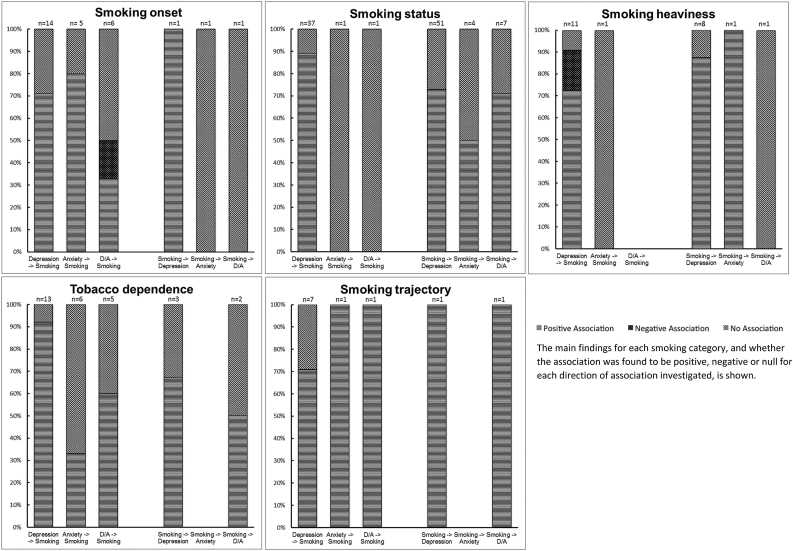
A total of 14 studies investigated the association of baseline depression with subsequent smoking onset, of which 10 (71%) found evidence to support this association,14–23 while four (29%) found no evidence of an association.24–27 Five studies investigated the association of baseline anxiety on smoking onset, of which four (80%) found evidence to support an association with increased risk of smoking onset24,28–30 and one (20%) found no evidence of an association.21 Six studies investigated the association of comorbid depression and anxiety with later smoking onset, of which two (33%) found evidence to support this association,31,32 while one (17%) reported comorbid depression and anxiety was associated with reduced risk of smoking onset33 and three (50%) found no evidence of an association.34–36 One study investigated the association of smoking onset with later depression, finding evidence for this association.15 One study investigated the association of smoking onset with later anxiety, finding no evidence for this association.21 Additionally one study investigated the association of smoking onset with later comorbid depression and anxiety, finding no evidence for this association.31 These findings are summarized in Figure 2.
Figure 2.
Main outcomes by smoking category.
Smoking Status
A total of 37 studies investigated the association of baseline depression with subsequent smoking status, of which 33 (89%) found evidence to support this association,21,37–66 while four (11%) found no evidence of an association.67–70 One study investigated the association of anxiety with later smoking status, finding evidence of an association.28 One study investigated the association of comorbid depression and anxiety with later smoking status, finding no evidence of an association.71
A total of 51 studies investigated the association of smoking status with later depression, of which 37 (73%) found evidence to support this association,21,25,47,57,65,70,72–102 while 14 (27%) found no evidence of this association.28,38,48,64,69,103–111 Four studies investigated the association of smoking status with later anxiety, of which two (50%) found evidence to support this association,28,112 while two (50%) found no evidence of an association.21,103 Seven studies investigated the association of smoking status with later comorbid depression and anxiety, of which five (71%) found evidence to support this association,35,113–116 while two (29%) found no evidence of an association.117,118 These findings are summarized in Figure 2.
Smoking Heaviness
A total of 11 studies investigated the association of baseline depression with subsequent heaviness of smoking, of which eight (73%) found evidence that depression was associated with heavier rates of smoking,22,119–125 while two (18%) found that depression was associated with reduced heaviness of smoking26,126 and one (09%) found no evidence of an association.127 One study investigated the association of baseline anxiety with subsequent smoking heaviness and found no evidence of an association.124 Eight studies investigated the association of heaviness of smoking with later depression, of which seven (88%) found evidence to support this association,11,82,95,102,125,127,128 while one (13%) found no evidence of an association.129 One study investigated the association of heaviness of smoking with later anxiety and found evidence to support this association.130 One study investigated the association of heaviness of smoking with later comorbid depression and anxiety, finding no evidence of an association.117 These findings are summarized in Figure 2.
Tobacco Dependence
A total of 13 studies investigated the association of baseline depression with subsequent tobacco dependence, of which 12 (92%) found evidence to support this association29,120,131–140 while one (8%) found no evidence of an association.141 Six studies investigated the association of baseline anxiety with later tobacco dependence, of which two (33%) found evidence to support this association,140,142 while four (67%) found no evidence of an association.132,137,139,143 Five studies investigated baseline comorbid depression and anxiety with subsequent tobacco dependence, of which three (60%) found evidence to support this association, 144–146 while two (40%) found no evidence of an association.35,147 Three studies investigated the association of tobacco dependence with later depression, of which two (67%) found evidence to support this association,6,132 while one (33%) found no evidence of an association.148 Two studies investigated the association of tobacco dependence with later comorbid depression and anxiety, of which one (50%) found evidence to support this association,149 while one (50%) found no evidence of an association.147 These findings are summarized in Figure 2.
Smoking Trajectory
A total of seven studies investigated the association of baseline depression with smoking trajectory, of which one (14%) reported that depressive symptoms were associated with accelerated cigarette use,150 three (43%) reported that depressive symptoms were associated with early smoking onset,17,43,151 one reported that depressive symptoms were associated with late onset smoking152 and two (29%) found no evidence of an association.153,154. One study reported evidence of an association of baseline anxiety with early and late onset smoking patterns.155 Another study reported evidence of an association of baseline comorbid depression and anxiety with late onset smoking as opposed to experimental smoking.156 One study reported that individuals in (smoking) starter and maintaining groups were more likely to be depressed at follow up compared with nonsmoking groups.157 Finally, one study reported evidence that early onset smokers developed depression and anxiety approximately five years earlier than late onset smokers.158 These findings are summarized in Figure 2.
Bidirectional Studies
Sixteen (11%) of the 148 included studies investigated the association between smoking behavior and mental health bidirectionally (ie, both the association between baseline mental health and later smoking behavior and baseline smoking behavior and later mental health). Of these, seven (44%) reported evidence in support of a bidirectional relationship between depression and smoking15,21,47,57,65,125,132 and one (9%) reported evidence in support of a bidirectional relationship between anxiety and smoking.28
Sex Differences
A total of eight studies (7% of all studies including both males and females) reported that the relationship between smoking and depression/anxiety differed between males and females. Two studies reported that depression was associated with subsequent smoking behavior only in males,23,64 while one study reported depression was associated with subsequent smoking only in females66 and one study reported that anxiety was associated with later smoking behavior only in females.140 Additionally, one study reported evidence that smoking status in men was associated with later depression,101 and two studies reported evidence that smoking status had a stronger association with later depression in females than males.97,157 Finally, one study reported a bidirectional relationship between smoking and depression that was only observed in females.57
Clinical Studies
Five studies investigated participants with cardiovascular problems. One study reported evidence that depression was associated with subsequent smoking behavior.44 The other four reported that smoking status was associated with later depression.80,83,87,88 Other studies of clinical populations generally reported evidence of an association between smoking and the onset of depression.
Ethnic Differences
Five studies recruited participants of East Asian descent (China, Japan, and South Korea), with two studies reporting evidence that depression was associated with later smoking behavior 41,48 and one study reporting no evidence of an association.70 Additionally, two studies reported evidence for an association between smoking status and later depression,70,99 while two studies reported no evidence that smoking status was associated with subsequent depression.48,108 Three studies recruited African American participants, with two studies reporting evidence that depression was associated with later smoking behavior,54,64 one study reporting no evidence that depression was associated with subsequent smoking onset,153 and one study reporting no evidence that smoking was associated with the onset of depression.64 Four studies recruited both African American and Hispanic participants, with three studies reporting that depression and anxiety were associated with subsequent smoking trajectories,43,131,156 while one study reported that smoking heaviness was associated with the onset of anxiety.130 Other studies of specific ethnic groups generally reported evidence of an association between smoking and later depression and anxiety.
Additional Analyses
No clear pattern of results was apparent when studies with different lengths of follow up were considered separately (see Supplementary Table S3). Additionally, the findings did not vary substantially between studies using different tests (interview vs. self-diagnostic test) or scales (continuous vs. categorical) to diagnose depression or anxiety (see Supplementary Table S4).
Discussion
In general, the findings across the studies in our systematic review were inconsistent. Nearly half of the studies reported that baseline depression or anxiety was associated with some type of later smoking behavior, whether it be the onset of smoking itself, increased smoking heaviness, or the transition from daily smoking into dependence. These findings support a self-medication model, suggesting that individuals smoke to alleviate psychiatric symptoms.5,6 However, over a third of the studies found evidence for a relationship in the opposite direction whereby smoking exposure at baseline was associated with later depression or anxiety, supporting the alternative hypothesis that prolonged smoking increases susceptibility to depression and anxiety.8,9 Of course, these two putative causal pathways are not mutually exclusive, but interestingly there were relatively few studies reporting evidence for a bidirectional model relationship between smoking and depression and anxiety. One possible reason for this is that many studies only measured or analyzed the variables in the direction of their a priori hypothesis. For example, studies examining factors for depression in later life measured smoking as a possible factor but typically did not analyze the association of baseline depression with later smoking. Moreover, few studies reported null results; often these were only included alongside positive results relating to another outcome. Additionally, it is possible the associations observed between smoking and mental health are a result of shared genetic and environmental factors.6
There are a number of limitations that should be considered when interpreting these results. First, the studies included in this review varied substantially in population sampled, with some recruiting from the general population and others selectively recruiting by sex, ethnicity, clinical population, or some other characteristic (eg, at-risk adolescents). This introduced substantial heterogeneity into the review, thus making meta-analysis inappropriate. The substantial heterogeneity between study populations could be responsible for the inconsistent results observed, and future reviews should consider analyzing different populations individually. Second, there was also substantial variation in study designs, including the length of follow up (between 2 months and 36 years) and confounders adjusted for. Measurement of depression or anxiety was based on a wide range of different diagnostic tests, with different cutoffs for determining clinical status. Sample size also varied substantially between studies, ranging from 59 to 90 627, suggesting that some smaller studies may be inadequately powered. This may lead to an increased likelihood of false positives since, among statistically significant findings, power declines the ratio of true positives to false positives decreases.159 This is because while 5% of null associations will be falsely declared as significant (assuming a 5% alpha level), the number of true positives correctly identified will decline as power declines (eg, from 80% of true associations correctly declared as significant in high powered studies to, say, only 20% in low powered studies).159 However, it is also worth noting that very large samples may detect statistically significant associations that are unlikely to be of clinical or population health importance.
Third, we only included published studies, and while the inclusion of unpublished studies may increase the likelihood of including lower quality work that has not been peer reviewed, it may also decrease publication bias, in which studies are only published if they have positive results. By expanding our search to include non-published studies, it is possible we may have found more instances of null results. Fourth, we did not investigate whether quality of the individual studies was related to the nature of the results reported. However, this would be challenging, given the diversity of study designs among the included studies. Fifth, while we were able to categorize and investigate a range of different smoking behaviors, the same level of detail was not available for depression and anxiety. Future reviews should investigate individual symptomology (eg, negative affect, somatic features, etc.) and their relationship with smoking behavior, as previous research has indicated that specific symptoms may be differentially associated with smoking motivations and tobacco withdrawal.160–162 However, this analysis was not possible with the data reviewed here. Sixth, we only focused on depression, anxiety, or comorbid depression and anxiety. However, several studies identified during screening included depression or anxiety subtypes (eg, post-traumatic stress disorder or social anxiety). These were excluded in order to maximize comparability among included studies. Future studies should explore whether there is a more consistent pattern of relationship between smoking behavior and other diagnostic categories. However, given the disparate results, we observed in our more focused review, it is perhaps unlikely that clear relationships will emerge.
Despite the advantages of longitudinal studies, they cannot by themselves provide strong evidence of causality. However, applying latent variable mixture modeling to establish group-based trajectories, as some studies identified did, may help to identify different patterns within the data that may have otherwise gone unnoticed. Rather than clustering individuals into simply “smokers” and “nonsmokers,” mixture modeling can identify various groups such as “experimenters,” “early onset,” “late onset,” “stable,” or “late escalating” smokers.163 This approach could provide insight into the type or critical age of smokers vulnerable to mental illness, or vice versa. It’s likely that our review did not yield more of these studies, as we did not include “trajectory” in our search terms. Future reviews should include an exhaustive search, including a variety of terms such as mixture modeling, latent class analysis, and latent trajectory analysis in addition to the term trajectory.
Additionally, future studies should therefore employ methods that enable stronger causal inference, such as Mendelian randomization (MR).164 This approach uses genetic polymorphisms that have been previously shown to be robustly associated with one of the exposures of interest; for example, the CHRNA5-A3-B4 gene cluster is associated with smoking quantity and tobacco dependence165,166 and has been used in a number of MR studies.160 It is based on the principle that an individual inherits a random assortment of genes from their parents, and these genes should not be associated with potential confounders.10 Therefore, in theory, a robust genetic influence to a particular exposure (eg, smoking) would be comparable to a randomized trial in which individuals are assigned to a high- or low-exposure group.164 In addition, environmental factors cannot affect the genes that an individual is born with, so analyses are not subject to reverse causality or residual confounding. Two studies that have used MR have found no evidence to support a causal association between smoking and depression and anxiety,117,167 while another found evidence to suggest that smoking was associated with lower odds of depression during pregnancy.168 The results of these studies suggest that observational findings of an association of smoking status with later psychological distress may be a result of shared vulnerability, residual confounding, or reverse causality (eg, psychological distress associated with later smoking behavior).167 However, this review yielded the most findings in the direction of psychological distress associated with later smoking behavior. This review found slightly more evidence to support a direction of psychological distress predicting later smoking behavior, which is not inconsistent with these MR studies.167,168 However, while both depression and anxiety are highly heritable,169,170 genomewide association studies have not identified genetic variants robustly and strongly associated with these outcomes.171 Therefore, it is not currently possible to use MR to examine whether depression and anxiety are associated with smoking behavior, although this is likely to change in the near future as larger genomewide association studies of depression and anxiety emerge. Until such genomewide association studies emerge, it is not possible to directly test the causal hypothesis in this direction.
In summary, we found overall inconsistent findings regarding whether smoking leads to depression and anxiety, depression and anxiety results in smoking or increased smoking behavior, or there is a bidirectional relationship between the two. This conflicting evidence suggests the need for future studies to focus on different methodologies, such as MR, which will allow us to draw stronger causal inferences.
Supplementary Material
Supplementary Tables S1 to S4 can be found online at http://www.ntr.oxfordjournals.org
Funding
This work was supported by a University of Bristol postgraduate research scholarship to MF, and the Medical Research Council (MC_UU_12013/6).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors are members of the UK Centre for Tobacco and Alcohol Studies, a UKCRC Public Health Research: Centre of Excellence. Funding from British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, and the National Institute for Health Research, under the auspices of the UK Clinical Research Collaboration is gratefully acknowledged.
References
- 1. Royal College of Physicians RCoP. Smoking and Mental Health. London: RCP; 2013. [Google Scholar]
- 2. Farrell M, Howes S, Taylor C, et al. Substance misuse and psychiatric comorbidity: An overview of the OPCS National Psychiatric Morbidity Survey. Addictive Behav. 1998;23(6):909–918. doi:10.1016/S0306-4603(98)00075-6. [DOI] [PubMed] [Google Scholar]
- 3. Meltzer H, Gill B, Hinds K, Petticrew M. OPCS Surveys of Psychiatric Morbidity in Great Britain,Report 6: Economic Activity and Social Functioning of Residents With Psychiatric Disorders. London: HMSO; 1996. doi:10.5255/UKDA-SN-3585-1. [Google Scholar]
- 4. McManus S, Howard M, Campion J. Cigarette Smoking and Mental Health in England: Data From the Adult Psychiatric Morbidity Survey 2007; 2010. [Google Scholar]
- 5. Chaiton MO, Cohen JE, O’Loughlin J, Rehm J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health. 2009;9:356. doi:10.1186/1471-2458-9-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boden JM, Fergusson DM, Horwood LJ. Cigarette smoking and depression: tests of causal linkages using a longitudinal birth cohort. Br J Psychiatry. 2010;196:440–446. doi:10.1192/bjp.bp.109.065912. [DOI] [PubMed] [Google Scholar]
- 7. Taylor G, McNeill A, et al. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ. 2014;348:g1151. doi:10.1136/bmj.g1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Markou A, Kosten TR, Koob GF. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis. Neuropsychopharmacology. 1998;18:135–174. doi:10.1016/S0893-133X (97)00113-9. [DOI] [PubMed] [Google Scholar]
- 9. Rose JE, Behm FM, Ramsey C, Ritchie JC., Jr Platelet monoamine oxidase, smoking cessation, and tobacco withdrawal symptoms. Nicotine Tob Res. 2001;3:383–390. doi:10.1080/14622200110087277. [DOI] [PubMed] [Google Scholar]
- 10. Munafò MR, Araya R. Cigarette smoking and depression: a question of causation. Br J Psychiatry. 2010;196:425–426. doi:10.1192/bjp.bp.109.074880. [DOI] [PubMed] [Google Scholar]
- 11. Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression. A causal analysis. Arch Gen Psychiatry. 1993;50:36–43. doi:10.1001/archpsyc.1993.01820130038007. [DOI] [PubMed] [Google Scholar]
- 12. Diagnostic and Statistical Manual of Mental Disorders. 4th ed., Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 13. Fagerstrom KO, Heatherton TF, Kozlowski LT. Nicotine addiction and its assessment. Ear Nose Throat J. 1990;69:763–765. www.ncbi.nlm.nih.gov/pubmed/2276350 Accessed September 15, 2015. [PubMed] [Google Scholar]
- 14. Carvajal SC, Granillo TM. A prospective test of distal and proximal determinants of smoking initiation in early adolescents. Addict Behav. 2006;31:649–660. doi:10.1016/j.addbeh.2005.05.047. [DOI] [PubMed] [Google Scholar]
- 15. Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry. 1998;55:161–166. doi:10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- 16. Chen J, Li X, Zhang J, et al. The Beijing Twin Study (BeTwiSt): a longitudinal study of child and adolescent development. Twin Res Hum Genet. 2013;16:91–97. doi:10.1017/thg.2012.115. [DOI] [PubMed] [Google Scholar]
- 17. Fuemmeler B, Lee CT, Ranby KW, et al. Individual- and community-level correlates of cigarette-smoking trajectories from age 13 to 32 in a U.S. population-based sample. Drug Alcohol Depend. 2013;132:301–308. doi:10.1016/j.drugalcdep.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi:10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 19. Naicker K, Galambos NL, Zeng Y, Senthilselvan A, Colman I. Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Health. 2013;52:533–538. doi:10.1016/j.jadohealth.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 20. Weiss JW, Mouttapa M, Cen S, Johnson CA, Unger J. Longitudinal effects of hostility, depression, and bullying on adolescent smoking initiation. J Adolesc Health. 2011;48:591–596. doi:10.1016/j.jadohealth.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35:1602–1610. doi:10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- 22. Holahan CK, Holahan CJ, Powers DA, Hayes RB, Marti CN, Ockene JK. Depressive symptoms and smoking in middle-aged and older women. Nicotine Tob Res. 2011;13:722–731. doi:10.1093/ntr/ntr066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Killen JD, Robinson TN, Haydel KF, et al. Prospective study of risk factors for the initiation of cigarette smoking. J Consult Clin Psychol. 1997;65:1011–1016. doi:10.1037/0022-006X.65.6.1011. [DOI] [PubMed] [Google Scholar]
- 24. Senol Y, Donmez L, Turkay M, Aktekin M. The incidence of smoking and risk factors for smoking initiation in medical faculty students: cohort study. BMC Public Health. 2006;6:128. doi:10.1186/1471-2458-6-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Goodman E, Capitman J. Depressive symptoms and cigarette smoking among teens. Pediatrics. 2000;106:748–755. doi:10.1542/peds.106.4.748. [DOI] [PubMed] [Google Scholar]
- 26. O’Loughlin J, Karp I, Koulis T, Paradis G, DiFranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am J Epidemiol. 2009;170(5):585–597. doi: 10.1093/aje/kwp179. [DOI] [PubMed] [Google Scholar]
- 27. Wiesner M, Ittel A. Relations of pubertal timing and depressive symptoms to substance use in early adolescence. J Early Adolesc.2002;22(1):5–23. doi: 10.1177/0272431602022001001. [Google Scholar]
- 28. Cuijpers P, Smit F, Ten Have M, de Graaf R. Smoking is associated with first-ever incidence of mental disorders: a prospective population-based study. Addiction. 2007;102(8):1303–1309. doi: 10.1111/j.1360-0443.2007.01885.x. [DOI] [PubMed] [Google Scholar]
- 29. Swendsen J, Conway KP, Degenhardt L, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. J Abnorm Child Psychol. 2010;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998;88:1518–1522. doi: 10.2105/AJPH.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Escobedo LG, Reddy M, Giovino GA. The relationship between depressive symptoms and cigarette smoking in US adolescents. Addiction. 1998;93:433–440. doi: 10.1046/j.1360-0443.1998.93343311.x. [DOI] [PubMed] [Google Scholar]
- 33. Fischer JA, Najman JM, Williams GM, Clavarino AM. Childhood and adolescent psychopathology and subsequent tobacco smoking in young adults: findings from an Australian birth cohort. Addiction. 2012;107:1669–1676. doi: 10.1111/j.1360-0443.2012.03846.x. [DOI] [PubMed] [Google Scholar]
- 34. Leff MK, Moolchan ET, Cookus BA, et al. Predictors of smoking initiation among at risk youth: a controlled study. J Child Adolesc Subst Abuse. 2003;13(1):59–75. doi: 10.1300/J029v13n01_04. [Google Scholar]
- 35. Pedersen W, von Soest T. Smoking, nicotine dependence and mental health among young adults: a 13-year population-based longitudinal study. Addiction. 2009;104:129–137. doi: 10.1111/j.1360-0443.2008.02395.x. [DOI] [PubMed] [Google Scholar]
- 36. Hayatbakhsh R, Mamun AA, Williams GM, O’Callaghan MJ, Najman JM. Early childhood predictors of early onset of smoking: a birth prospective study. Addict Behav. 2013;38:2513–2519. doi: 10.1016/j.addbeh.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 37. Mendel JR, Berg CJ, Windle RC, Windle M. Predicting young adulthood smoking among adolescent smokers and nonsmokers. Am J Health Behav. 2012;36:542–554. doi: 10.5993/ajhb.36.4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Braithwaite RS, Fang Y, Tate J, et al. Do alcohol misuse, smoking, and depression vary concordantly or sequentially? A longitudinal study of HIV-infected and matched uninfected veterans in care. AIDS Behav. 2016;20:566–572. doi: 10.1007/s10461-015-1117-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Audrain-McGovern J, Lerman C, Wileyto EP, Rodriguez D, Shields PG. Interacting effects of genetic predisposition and depression on adolescent smoking progression. Am J Psychiatry. 2004;161:1224–1230. doi: 10.1176/appi.ajp.161.7.1224. [DOI] [PubMed] [Google Scholar]
- 40. Audrain-McGovern J, Rodriguez D, Rodgers K, Cuevas J. Declining alternative reinforcers link depression to young adult smoking. Addiction. 2011;106:178–187. doi: 10.1111/j.1360-0443.2010.03113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Black DS, Sussman S, Johnson CA, Milam J. Testing the indirect effect of trait mindfulness on adolescent cigarette smoking through negative affect and perceived stress mediators. J Subst Use. 2012;17(5–6):417–429. doi: 10.3109/14659891.2011.587092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bomba J, Modrzejewska R, Pilecki M, Ślosarczyk M. Adolescent depression as a risk factor for the development of mental disorders. A 15-year prospective follow-up. Arch Psychiatr Psychother.2004;6(1):5–14. http://www.archivespp.pl/uploads/APPv6n1p5Bomba.pdf Accessed September 15, 2015. [PubMed] [Google Scholar]
- 43. Brook JS, Balka EB, Ning Y, Whiteman M, Finch SJ. Smoking involvement during adolescence among African Americans and Puerto Ricans: risks to psychological and physical well-being in young adulthood. Psychol Rep. 2006;99:421–438. doi: 10.2466/pr0.99.2.421-438. [DOI] [PubMed] [Google Scholar]
- 44. Brummett BH, Babyak MA, Siegler IC, Mark DB, Williams RB, Barefoot JC. Effect of smoking and sedentary behavior on the association between depressive symptoms and mortality from coronary heart disease. Am J Cardiol. 2003;92:529–532. doi: 10.1016/S0002-9149(03)00719-7. [DOI] [PubMed] [Google Scholar]
- 45. Carvajal SC. Global positive expectancies in adolescence and health-related behaviours: longitudinal models of latent growth and cross-lagged effects. Psychol Health. 2012;27:916–937. doi: 10.1080/08870446.2011.633241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking. A national perspective. JAMA. 1990;264:1541–1545. doi: 10.1001/jama.1990.03450120053028. [PubMed] [Google Scholar]
- 47. Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104:1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Park S, Weaver TE, Romer D. Predictors of the transition from experimental to daily smoking among adolescents in the United States. J Spec Pediatr Nurs. 2009;14:102–111. doi: 10.1111/j.1744-6155.2009.00183.x. [DOI] [PubMed] [Google Scholar]
- 49. Clark HK, Ringwalt CL, Shamblen SR. Predicting adolescent substance use: the effects of depressed mood and positive expectancies. Addict Behav. 2011;36:488–493. doi: 10.1016/j.addbeh.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 50. Gritz ER, Prokhorov AV, Hudmon KS, et al. Predictors of susceptibility to smoking and ever smoking: a longitudinal study in a triethnic sample of adolescents. Nicotine Tob Res.2003;5(4):493–506. doi: 10.1080/1462220031000118568. [DOI] [PubMed] [Google Scholar]
- 51. Kandel DB, Davies M. Adult sequelae of adolescent depressive symptoms. Arch Gen Psychiatry. 1986;43:255–262. doi: 10.1001/archpsyc.1986.01800030073007. [DOI] [PubMed] [Google Scholar]
- 52. Knekt P, Raitasalo R, Heliövaara M, et al. Elevated lung cancer risk among persons with depressed mood. Am J Epidemiol. 1996;144:1096–1103. doi: 10.1093/oxfordjournals.aje.a008887. [DOI] [PubMed] [Google Scholar]
- 53. Leve LD, Harold GT, Van Ryzin MJ, Elam K, Chamberlain P. Girls’ tobacco and alcohol use during early adolescence: prediction from trajectories of depressive symptoms across two studies. J Child Adolesc Subst Abuse. 2012;21(3):254–272. doi: 10.1080/1067828x.2012.700853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: substance use outcomes across adolescence. J Abnorm Child Psychol. 1998;26:221–232. www.ncbi.nlm.nih.gov/pubmed/9650628 Accessed September 15, 2015. [DOI] [PubMed] [Google Scholar]
- 55. Prinstein MJ, La Greca AM. Childhood depressive symptoms and adolescent cigarette use: a six-year longitudinal study controlling for peer relations correlates. Health Psychol. 2009;28:283–291. doi: 10.1037/a0013949. [DOI] [PubMed] [Google Scholar]
- 56. Wickrama T, Wickrama KA. Heterogeneity in adolescent depressive symptom trajectories: implications for young adults’ risky lifestyle. J Adolesc Health. 2010;47:407–413. doi: 10.1016/j.jadohealth.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 57. Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Soc Sci Med. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 58. Coogan PF, Yu J, O’Connor GT, Brown TA, Palmer JR, Rosenberg L. Depressive symptoms and the incidence of adult-onset asthma in African American women. Ann Allergy Asthma Immunol. 2014;112:333–8.e1. doi: 10.1016/j.anai.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Byers AL, Vittinghoff E, Lui LY, et al. Twenty-year depressive trajectories among older women. Arch Gen Psychiatry. 2012;69:1073–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Franko DL, Striegel-Moore RH, Bean J, et al. Psychosocial and health consequences of adolescent depression in Black and White young adult women. Health Psychol. 2005;24:586–593. doi: 10.1037/0278-6133.24.6.586. [DOI] [PubMed] [Google Scholar]
- 61. Leiferman J. The effect of maternal depressive symptomatology on maternal behaviors associated with child health. Health Educ Behav. 2002;29:596–607. doi: 10.1177/109019802237027. [DOI] [PubMed] [Google Scholar]
- 62. Appleton KM, Woodside JV, Arveiler D, et al. Depression and mortality: artifact of measurement and analysis? J Affect Disord. 2013;151(2):632–638. doi: 10.1016/j.jad.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 63. Niemelä S, Sourander A, Pilowsky DJ, et al. Childhood antecedents of being a cigarette smoker in early adulthood. The Finnish ‘From a Boy to a Man’ Study. J Child Psychol Psychiatry. 2009;50:343–351. doi: 10.1111/j.1469-7610.2008.01968.x. [DOI] [PubMed] [Google Scholar]
- 64. Repetto PB, Caldwell CH, Zimmerman MA. A longitudinal study of the relationship between depressive symptoms and cigarette use among African American adolescents. Health Psychol. 2005;24:209–219. doi: 10.1037/0278-6133.24.2.209. [DOI] [PubMed] [Google Scholar]
- 65. Leung J, Gartner C, Hall W, Lucke J, Dobson A. A longitudinal study of the bi-directional relationship between tobacco smoking and psychological distress in a community sample of young Australian women. Psychol Med. 2012;42:1273–1282. doi: 10.1017/s0033291711002261. [DOI] [PubMed] [Google Scholar]
- 66. Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychol Addict Behav. 2008;22:186–197. doi: 10.1037/0893-164x.22.2.186. [DOI] [PubMed] [Google Scholar]
- 67. Audrain-McGovern J, Rodriguez D, Patel V, Faith MS, Rodgers K, Cuevas J. How do psychological factors influence adolescent smoking progression? The evidence for indirect effects through tobacco advertising receptivity. Pediatrics. 2006;117:1216–1225. doi: 10.1542/peds.2005-0808. [DOI] [PubMed] [Google Scholar]
- 68. van Gool CH, Kempen GI, Bosma H, van Boxtel MP, Jolles J, van Eijk JT. Associations between lifestyle and depressed mood: longitudinal results from the Maastricht Aging Study. Am J Public Health. 2007;97:887–894. doi: 10.2105/ajph.2004.053199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wang MQ, Fitzhugh EC, Turner L, Fu Q, Westerfield RC. Association of depressive symptoms and school adolescents’ smoking: a cross-lagged analysis. Psychol Rep. 1996;79:127–130. doi: 10.2466/pr0.1996.79.1.127. [DOI] [PubMed] [Google Scholar]
- 70. Kang E, Lee J. A longitudinal study on the causal association between smoking and depression. J Prev Med Public Health. 2010;43:193–204. doi: 10.3961/jpmph.2010.43.3.193. [DOI] [PubMed] [Google Scholar]
- 71. Ferdinand RF, Blüm M, Verhulst FC. Psychopathology in adolescence predicts substance use in young adulthood. Addiction. 2001;96:861–870. doi: 10.1046/j.1360-0443.2001.9668617.x. [DOI] [PubMed] [Google Scholar]
- 72. Albers AB, Biener L. The role of smoking and rebelliousness in the development of depressive symptoms among a cohort of Massachusetts adolescents. Prev Med. 2002;34:625–631. doi: 10.1006/pmed.2002.1029. [DOI] [PubMed] [Google Scholar]
- 73. Batterham PJ, Christensen H, Mackinnon AJ. Modifiable risk factors predicting major depressive disorder at four year follow-up: a decision tree approach. BMC Psychiatry. 2009;9:75. doi: 10.1186/1471-244x-9–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Buckner JC, Mandell W. Risk factors for depressive symptomatology in a drug using population. Am J Public Health. 1990;80:580–585. doi: 10.2105/ajph.80.5.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Choi WS, Patten CA, Gillin JC, Kaplan RM, Pierce JP. Cigarette smoking predicts development of depressive symptoms among U.S. adolescents. Ann Behav Med. 1997;19:42–50. doi: 10.1007/BF02883426. [DOI] [PubMed] [Google Scholar]
- 76. Colman I, Naicker K, Zeng Y, Ataullahjan A, Senthilselvan A, Patten SB. Predictors of long-term prognosis of depression. CMAJ. 2011;183:1969–1976. doi: 10.1503/cmaj.110676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol. 2008;76:173–183. doi: 10.1037/0022-006x.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. de Jonge P, Kempen GI, Sanderman R, et al. Depressive symptoms in elderly patients after a somatic illness event: prevalence, persistence, and risk factors. Psychosomatics. 2006;47:33–42. doi: 10.1176/appi.psy.47.1.33. [DOI] [PubMed] [Google Scholar]
- 79. Flensborg-Madsen T, von Scholten MB, Flachs EM, Mortensen EL, Prescott E, Tolstrup JS. Tobacco smoking as a risk factor for depression. A 26-year population-based follow-up study. J Psychiatr Res. 2011;45:143–149. doi: 10.1016/j.jpsychires.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 80. Gravely-Witte S, Stewart DE, Suskin N, Grace SL. The association among depressive symptoms, smoking status and antidepressant use in cardiac outpatients. J Behav Med. 2009;32:478–490. doi: 10.1007/s10865-009-9218-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Khaled SM, Bulloch AG, Williams JV, Hill JC, Lavorato DH, Patten SB. Persistent heavy smoking as risk factor for major depression (MD) incidence–evidence from a longitudinal Canadian cohort of the National Population Health Survey. J Psychiatr Res. 2012;46:436–443. doi: 10.1016/j.jpsychires.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 82. Klungsøyr O, Nygård JF, Sørensen T, Sandanger I. Cigarette smoking and incidence of first depressive episode: an 11-year, population-based follow-up study. Am J Epidemiol. 2006;163:421–432. doi: 10.1093/aje/kwj058. [DOI] [PubMed] [Google Scholar]
- 83. Koçer O, Wachter M, Zellweger M, Piazzalonga S, Hoffmann A. Prevalence and predictors of depressive symptoms and wellbeing during and up to nine years after outpatient cardiac rehabilitation. Swiss Med Wkly. 2011;141:w13242. doi: 10.4414/smw.2011.13242. [DOI] [PubMed] [Google Scholar]
- 84. Meng X, D’Arcy C. The projected effect of risk factor reduction on major depression incidence: a 16-year longitudinal Canadian cohort of the National Population Health Survey. J Affect Disord. 2014;158:56–61. doi: 10.1016/j.jad.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 85. Moon SS, Mo BC, Basham R. Adolescent depression and future smoking behavior: a prospective study. Child Adolesc Soc Work J. 2010;27(6):405–422. doi: 10.1007/s10560-010-0212-y. [Google Scholar]
- 86. Patten SB, Wang JL, Williams JV, Lavorato DH, Khaled SM, Bulloch AG. Predictors of the longitudinal course of major depression in a Canadian population sample. Can J Psychiatry. 2010;55:669–676. www.ncbi.nlm.nih.gov/pubmed/20964946 Accessed September 15, 2015. [DOI] [PubMed] [Google Scholar]
- 87. Schrader G, Cheok F, Hordacre AL, Guiver N. Predictors of depression three months after cardiac hospitalization. Psychosom Med. 2004;66:514–520. doi: 10.1097/01.psy.0000128901.58513.db. [DOI] [PubMed] [Google Scholar]
- 88. Schrader G, Cheok F, Hordacre AL, Marker J. Predictors of depression 12 months after cardiac hospitalization: the Identifying Depression as a Comorbid Condition study. Aust N Z J Psychiatry. 2006;40:1025–1030. doi: 10.1111/j.1440-1614.2006.01927.x. [DOI] [PubMed] [Google Scholar]
- 89. Silberg JL, Rutter M, D’Onofrio B, Eaves L. Genetic and environmental risk factors in adolescent substance use. J Child Psychol Psychiatry. 2003;44(5):664–676. doi: 10.1111/1469–7610.00153. [DOI] [PubMed] [Google Scholar]
- 90. Sweeting HN, West PB, Der GJ. Explanations for female excess psychosomatic symptoms in adolescence: evidence from a school-based cohort in the West of Scotland. BMC Public Health. 2007;7:298. doi: 10.1186/1471-2458-7-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Green BH, Copeland JR, Dewey ME, et al. Risk factors for depression in elderly people: a prospective study. Acta Psychiatr Scand. 1992;86:213–217. doi: 10.1111/j.1600-0447.1992.tb03254.x. [DOI] [PubMed] [Google Scholar]
- 92. Rodriguez D, Moss HB, Audrain-McGovern J. Developmental heterogeneity in adolescent depressive symptoms: associations with smoking behavior. Psychosom Med. 2005;67:200–210. doi: 10.1097/01.psy.0000156929.83810.01. [DOI] [PubMed] [Google Scholar]
- 93. Brook JS, Schuster E, Zhang C. Cigarette smoking and depressive symptoms: a longitudinal study of adolescents and young adults. Psychol Rep. 2004;95:159–166. doi: 10.2466/pr0.95.1.159-166. [DOI] [PubMed] [Google Scholar]
- 94. Stein JA, Newcomb MD, Bentler PM. Initiation and maintenance of tobacco smoking: changing personality correlates in adolescence and young adulthood. J Appl Soc Psychol.1996;26(2):160–187. doi: 10.1111/j.1559–1816.1996.tb01844.x. [Google Scholar]
- 95. Clyde M, Smith KJ, Gariepy G, Schmitz N. Assessing the longitudinal associations and stability of smoking and depression syndrome over a 4-year period in a community sample with type 2 diabetes. J Diabetes. 2014;7(1):95–101. doi: 10.1111/1753-0407.12141. [DOI] [PubMed] [Google Scholar]
- 96. Dugan SA, Bromberger JT, Segawa E, Avery E, Sternfeld B. Association between physical activity and depressive symptoms: midlife women in SWAN. Med Sci Sports Exerc. 2015;47:335–342. doi: 10.1249/mss.0000000000000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Duncan B, Rees DI. Effect of smoking on depressive symptomatology: a reexamination of data from the National Longitudinal Study of Adolescent Health. Am J Epidemiol. 2005;162:461–470. doi: 10.1093/aje/kwi219. [DOI] [PubMed] [Google Scholar]
- 98. Pasco JA, Williams LJ, Jacka FN, et al. Tobacco smoking as a risk factor for major depressive disorder: population-based study. Br J Psychiatry. 2008;193:322–326. doi: 10.1192/bjp.bp.107.046706. [DOI] [PubMed] [Google Scholar]
- 99. Tanaka H, Sasazawa Y, Suzuki S, Nakazawa M, Koyama H. Health status and lifestyle factors as predictors of depression in middle-aged and elderly Japanese adults: a seven-year follow-up of the Komo-Ise cohort study. BMC Psychiatry. 2011;11:20. doi: 10.1186/1471-244x-11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Almeida OP, Hankey GJ, Yeap BB, Golledge J, McCaul K, Flicker L. A risk table to assist health practitioners assess and prevent the onset of depression in later life. Prev Med. 2013;57:878–882. doi: 10.1016/j.ypmed.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 101. Korhonen T, Broms U, Varjonen J, et al. Smoking behaviour as a predictor of depression among Finnish men and women: a prospective cohort study of adult twins. Psychol Med. 2007;37:705–715. doi: 10.1017/s0033291706009639. [DOI] [PubMed] [Google Scholar]
- 102. Paffenbarger RS, Jr, Lee IM, Leung R. Physical activity and personal characteristics associated with depression and suicide in American college men. Acta Psychiatr Scand Suppl. 1994;377:16–22. doi: 10.1111/j.1600-0447.1994.tb05796.x. [DOI] [PubMed] [Google Scholar]
- 103. Gage SH, Hickman M, Heron J, et al. Associations of cannabis and cigarette use with depression and anxiety at age 18: findings from the Avon Longitudinal Study of Parents and Children. PLoS One. 2015;10:e0122896. doi: 10.1371/journal.pone.0122896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Aneshensel CS, Huba GJ. Depression, alcohol use, and smoking over one year: a four-wave longitudinal causal model. J Abnorm Psychol. 1983;92:134–150. doi: 10.1037/0021-843X.92.2.134. [DOI] [PubMed] [Google Scholar]
- 105. Julian LJ, Tonner C, Yelin E, et al. Cardiovascular and disease-related predictors of depression in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2011;63:542–549.doi: 10.1002/acr.20426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Munafò MR, Hitsman B, Rende R, Metcalfe C, Niaura R. Effects of progression to cigarette smoking on depressed mood in adolescents: evidence from the National Longitudinal Study of Adolescent Health. Addiction. 2008;103:162–171.doi: 10.1111/j.1360-0443.2007.02052.x. [DOI] [PubMed] [Google Scholar]
- 107. Strong C, Juon HS, Ensminger ME. Long-term effects of adolescent smoking on depression and socioeconomic status in adulthood in an urban African American cohort. J Urban Health. 2014;91:526–540. doi: 10.1007/s11524-013-9849-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Takeuchi T, Nakao M, Yano E. Relationship between smoking and major depression in a Japanese workplace. J Occup Health. 2004;46:489–492. doi: 10.1539/joh.46.489. [DOI] [PubMed] [Google Scholar]
- 109. Weyerer S, Eifflaender-Gorfer S, Wiese B, et al. Incidence and predictors of depression in non-demented primary care attenders aged 75 years and older: results from a 3-year follow-up study. Age Ageing. 2013;42:173–180. doi: 10.1093/ageing/afs184. [DOI] [PubMed] [Google Scholar]
- 110. Clark C, Haines MM, Head J, et al. Psychological symptoms and physical health and health behaviours in adolescents: a prospective 2-year study in East London. Addiction. 2007;102:126–135. doi: 10.1111/j.1360-0443.2006.01621.x. [DOI] [PubMed] [Google Scholar]
- 111. Anstey KJ, von Sanden C, Sargent-Cox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. Am J Geriatr Psychiatry. 2007;15:497–505. doi: 10.1097/JGP.0b013e31802e21d8. [DOI] [PubMed] [Google Scholar]
- 112. Moylan S, Gustavson K, Karevold E, et al. The impact of smoking in adolescence on early adult anxiety symptoms and the relationship between infant vulnerability factors for anxiety and early adult anxiety symptoms: the TOPP Study. PLoS One. 2013;8:e63252. doi: 10.1371/journal.pone.0063252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Boyes AW, Girgis A, D’Este CA, Zucca AC, Lecathelinais C. Prevalence and predictors of the short-term trajectory of anxiety and depression in the first year after a cancer diagnosis: a population-based longitudinal study. J Clin Oncol. 2013. doi: 10.1200/jco.2012.44.7540. [DOI] [PubMed] [Google Scholar]
- 114. Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women - Population-based longitudinal study. Br J Psychiatry. 2006;189:547–555. doi: 10.1192/bjp.bp.106.022558. [DOI] [PubMed] [Google Scholar]
- 115. Wagena EJ, van Amelsvoort LG, Kant I, Wouters EF. Chronic bronchitis, cigarette smoking, and the subsequent onset of depression and anxiety: results from a prospective population-based cohort study. Psychosom Med. 2005;67:656–660. doi: 10.1097/01.psy.0000171197.29484.6b. [DOI] [PubMed] [Google Scholar]
- 116. Fergusson DM, Boden JM, Horwood LJ. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2011;46:933–942. doi: 10.1007/s00127-010-0268-1. [DOI] [PubMed] [Google Scholar]
- 117. Bjørngaard JH, Gunnell D, Elvestad MB, et al. The causal role of smoking in anxiety and depression: a Mendelian randomization analysis of the HUNT study. Psychol Med. 2013;43:711–719. doi: 10.1017/s0033291712001274. [DOI] [PubMed] [Google Scholar]
- 118. Clark DB, Cornelius J. Childhood psychopathology and adolescent cigarette smoking: a prospective survival analysis in children at high risk for substance use disorders. Addict Behav. 2004;29:837–841. doi: 10.1016/j.addbeh.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 119. Brook DW, Brook JS, Zhang C. Joint trajectories of smoking and depressive mood: associations with later low perceived self-control and low well-being. J Addict Dis. 2014;33:53–64. doi: 10.1080/10550887.2014.882717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Fergusson DM, Goodwin RD, Horwood LJ. Major depression and cigarette smoking: results of a 21-year longitudinal study. Psychol Med. 2003;33:1357–1367. doi: 10.1017/S0033291703008596 [DOI] [PubMed] [Google Scholar]
- 121. Maslowsky J, Schulenberg JE, Zucker RA. Influence of conduct problems and depressive symptomatology on adolescent substance use: developmentally proximal versus distal effects. Dev Psychol. 2014;50:1179–1189. doi: 10.1037/a0035085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. van Gool CH, Kempen GI, Penninx BW, Deeg DJ, Beekman AT, van Eijk JT. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Age Ageing. 2003;32:81–87. doi: 10.1093/ageing/32.1.81. [DOI] [PubMed] [Google Scholar]
- 123. Whitbeck LB, Yu M, McChargue DE, Crawford DM. Depressive symptoms, gender, and growth in cigarette smoking among indigenous adolescents. Addict Behav. 2009;34:421–426. doi: 10.1016/j.addbeh.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Lekka NP, Lee KH, Argyriou AA, Beratis S, Parks RW. Association of cigarette smoking and depressive symptoms in a forensic population. Depress Anxiety. 2007;24:325–330. doi: 10.1002/da.20235. [DOI] [PubMed] [Google Scholar]
- 125. Windle M, Windle RC. Depressive symptoms and cigarette smoking among middle adolescents: prospective associations and intrapersonal and interpersonal influences. J Consult Clin Psychol. 2001;69:215–226. doi: 10.1037//0022-006X.69.2.215. [PubMed] [Google Scholar]
- 126. Patten CA, Hurt RD, Offord KP, et al. Relationship of tobacco use to depressive disorders and suicidality among patients treated for alcohol dependence. Am J Addict. 2003;12:71–83. doi: 10.1111/j.1521-0391.2003.tb00541.x. [PubMed] [Google Scholar]
- 127. Beal SJ, Negriff S, Dorn LD, Pabst S, Schulenberg J. Longitudinal associations between smoking and depressive symptoms among adolescent girls. Prev Sci. 2013;15(4):506–515. doi: 10.1007/s11121-013-0402-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Galambos N, Leadbeater B, Barker E. Gender differences in and risk factors for depression in adolescence: a 4-year longitudinal study. Int J Beh Dev. 2004;28(1):16–25. doi: 10.1080/01650250344000235. [Google Scholar]
- 129. Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- 130. Okeke NL, Spitz MR, Forman MR, Wilkinson AV. The associations of body image, anxiety, and smoking among Mexican-origin youth. J Adolesc Health. 2013.doi: 10.1016/j.jadohealth.2013.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Brook JS, Brook DW, Zhang C. Psychosocial predictors of nicotine dependence in Black and Puerto Rican adults: a longitudinal study. Nicotine Tob Res. 2008;10(6):959–967. doi: 10.1080/14622200802092515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Breslau N, Kilbey MM, Andreski P. Nicotine dependence and major depression. New evidence from a prospective investigation. Arch Gen Psychiatry. 1993;50:31–35. doi:10.1001/archpsyc.1993.01820130033006. [DOI] [PubMed] [Google Scholar]
- 133. Hamdi NR, Iacono WG. Lifetime prevalence and co-morbidity of externalizing disorders and depression in prospective assessment. Psychol Med. 2014;44:315–324. doi: 10.1017/s0033291713000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Karp I, O’Loughlin J, Hanley J, Tyndale RF, Paradis G. Risk factors for tobacco dependence in adolescent smokers. Tob Control. 2006;15:199–204. doi: 10.1136/tc.2005.014118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Kleinjan M, Wanner B, Vitaro F, Van den Eijnden RJ, Brug J, Engels RC. Nicotine dependence subtypes among adolescent smokers: examining the occurrence, development and validity of distinct symptom profiles. Psychol Addict Behav. 2010;24:61–74. doi: 10.1037/a0018543. [DOI] [PubMed] [Google Scholar]
- 136. Racicot S, McGrath JJ, Karp I, O’Loughlin J. Predictors of nicotine dependence symptoms among never-smoking adolescents: a longitudinal analysis from the Nicotine Dependence in Teens Study. Drug Alcohol Depend. 2013;130:38–44. doi: 10.1016/j.drugalcdep.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. DiFranza JR, Savageau JA, Fletcher K, et al. Susceptibility to nicotine dependence: the Development and Assessment of Nicotine Dependence in Youth 2 study. Pediatrics. 2007;120:e974–e983. doi: 10.1542/peds.2007-0027. [DOI] [PubMed] [Google Scholar]
- 138. Kendler KS, Gardner CO. Monozygotic twins discordant for major depression: a preliminary exploration of the role of environmental experiences in the aetiology and course of illness. Psychol Med. 2001;31:411–423. doi: 10.1017/S0033291701003622. [DOI] [PubMed] [Google Scholar]
- 139. Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 140. Kandel DB, Hu M-C, Griesler PC, Schaffran C. On the development of nicotine dependence in adolescence. Drug Alcohol Depend. 2007;91(1):26–39. doi: 10.1016/j.drugalcdep.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Tully EC, Iacono WG, McGue M. Changes in genetic and environmental influences on the development of nicotine dependence and major depressive disorder from middle adolescence to early adulthood. Dev Psychopathol. 2010;22:831–848. doi: 10.1017/s0954579410000490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Goodwin RD, Fergusson DM, Horwood LJ. Association between anxiety disorders and substance use disorders among young persons: results of a 21-year longitudinal study. J Psychiatr Res. 2004;38(3):295–304. doi: 10.1016/j.jpsychires.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 143. Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40:1086–1093. doi: 10.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- 144. Goodwin RD, Kim JH, Weinberger AH, Taha F, Galea S, Martins SS. Symptoms of alcohol dependence and smoking initiation and persistence: a longitudinal study among US adults. Drug Alcohol Depend. 2013;133:718–723. doi: 10.1016/j.drugalcdep.2013.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. McKenzie M, Olsson CA, Jorm AF, Romaniuk H, Patton GC. Association of adolescent symptoms of depression and anxiety with daily smoking and nicotine dependence in young adulthood: findings from a 10-year longitudinal study. Addiction. 2010;105:1652–1659. doi: 10.1111/j.1360-0443.2010.03002.x. [DOI] [PubMed] [Google Scholar]
- 146. Patton GC, Coffey C, Carlin JB, Sawyer SM, Wakefield M. Teen smokers reach their mid twenties. J Adolesc Health. 2006;39:214–220. doi: 10.1016/j.jadohealth.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 147. Griesler PC, Hu MC, Schaffran C, Kandel DB. Comorbidity of psychiatric disorders and nicotine dependence among adolescents: findings from a prospective, longitudinal study. J Am Acad Child Adolesc Psychiatry. 2008;47:1340–1350. doi: 10.1097/CHI.0b013e318185d2ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Hu MC, Griesler P, Schaffran C, Kandel D. Risk and protective factors for nicotine dependence in adolescence. J Child Psychol Psychiatry. 2011;52:1063–1072. doi: 10.1111/j.1469-7610.2010.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Jamal M, Willem Van der Does AJ, Cuijpers P, Penninx BW. Association of smoking and nicotine dependence with severity and course of symptoms in patients with depressive or anxiety disorder. Drug Alcohol Depend. 2012;126:138–146. doi: 10.1016/j.drugalcdep.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 150. Hooshmand S, Willoughby T, Good M. Does the direction of effects in the association between depressive symptoms and health-risk behaviors differ by behavior? A longitudinal study across the high school years. J Adolesc Health. 2012;50:140–147. doi: 10.1016/j.jadohealth.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 151. Audrain-McGovern J, Rodriguez D, Tercyak KP, Cuevas J, Rodgers K, Patterson F. Identifying and characterizing adolescent smoking trajectories. Cancer Epidemiol Biomarkers Prev. 2004;13:2023–2034. www.ncbi.nlm.nih.gov/pubmed/15598757 Accessed September 15, 2015. [PubMed] [Google Scholar]
- 152. Saules KK, Pomerleau CS, Snedecor SM, et al. Relationship of onset of cigarette smoking during college to alcohol use, dieting concerns, and depressed mood: results from the Young Women’s Health Survey. Addict Behav. 2004;29:893–899. doi: 10.1016/j.addbeh.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 153. White HR, Violette NM, Metzger L, Stouthamer-Loeber M. Adolescent risk factors for late-onset smoking among African American young men. Nicotine Tob Res. 2007;9:153–161. doi: 10.1080/14622200601078350. [DOI] [PubMed] [Google Scholar]
- 154. Juon HS, Ensminger ME, Sydnor KD. A longitudinal study of developmental trajectories to young adult cigarette smoking. Drug Alcohol Depend. 2002;66:303–314. doi: 10.1016/S0376-8716(02)00008-X. [DOI] [PubMed] [Google Scholar]
- 155. Hu MC, Griesler PC, Schaffran C, Wall MM, Kandel DB. Trajectories of criteria of nicotine dependence from adolescence to early adulthood. Drug Alcohol Depend. 2012;125:283–289. doi: 10.1016/j.drugalcdep.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Brook JS, Ning Y, Brook DW. Personality risk factors associated with trajectories of tobacco use. Am J Addict. 2006;15(6):426–433. doi: 10.1080/10550490600996363. [DOI] [PubMed] [Google Scholar]
- 157. Steuber TL, Danner F. Adolescent smoking and depression: which comes first? Addict Behav. 2006;31:133–136. doi: 10.1016/j.addbeh.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 158. Jamal M, Does AJ, Penninx BW, Cuijpers P. Age at smoking onset and the onset of depression and anxiety disorders. Nicotine Tob Res. 2011;13:809–819.doi: 10.1093/ntr/ntr077. [DOI] [PubMed] [Google Scholar]
- 159. Button KS, Ioannidis JP, Mokrysz C, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–376. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]
- 160. Mickens L, Greenberg J, Ameringer KJ, Brightman M, Sun P, Leventhal AM. Associations between depressive symptom dimensions and smoking dependence motives. Eval Health Prof. 2011;34:81–102. doi: 10.1177/0163278710383562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Leventhal AM, Ameringer KJ, Osborn E, Zvolensky MJ, Langdon KJ. Anxiety and depressive symptoms and affective patterns of tobacco withdrawal. Drug Alcohol Depend. 2013;133:324–329. doi: 10.1016/j.drugalcdep.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Leventhal AM, Zvolensky MJ, Schmidt NB. Smoking-related correlates of depressive symptom dimensions in treatment-seeking smokers. Nicotine Tob Res. 2011;13:668–676. doi: 10.1093/ntr/ntr056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Heron J, Hickman M, Macleod J, Munafo MR. Characterizing patterns of smoking initiation in adolescence: comparison of methods for dealing with missing data. Nicotine Tob Res. 2011;13(12):1266–1275. doi: 10.1093/Ntr/Ntr161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Gage SH, Smith GD, Zammit S, Hickman M, Munafò MR. Using Mendelian randomisation to infer causality in depression and anxiety research. Depress Anxiety. 2013;30:1185–1193. doi: 10.1002/da.22150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Furberg H, Ostroff J, Lerman C, Sullivan PF. The public health utility of genome-wide association study results for smoking behavior. Genome Med. 2010;2:26. doi: 10.1186/gm147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Ware JJ, van den Bree M, Munafò MR. From men to mice: CHRNA5/CHRNA3, smoking behavior and disease. Nicotine Tob Res. 2012;14:1291–1299. doi: 10.1093/ntr/nts106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Taylor AE, Fluharty ME, Bjørngaard JH, et al. Investigating the possible causal association of smoking with depression and anxiety using Mendelian randomisation meta-analysis: the CARTA consortium. BMJ Open. 2014;4:e006141. doi: 10.1136/bmjopen-2014–006141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Lewis SJ, Araya R, Smith GD, et al. Smoking is associated with, but does not cause, depressed mood in pregnancy—a Mendelian randomization study. PLoS One. 2011;6(7). doi: 10.1371/journal.pone.0021689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Hamet P, Tremblay J. Genetics and genomics of depression. Metabolism. 2005;54(5 Suppl 1):10–15. doi: 10.1016/j.metabol.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 170. Norrholm SD, Ressler KJ. Genetics of anxiety and trauma-related disorders. Neuroscience. 2009;164:272–287. doi: 10.1016/j.neuroscience.2009.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Major Depressive Disorder Working Group of the Psychiatric GWAS Consortium , Ripke S, Wray NR, et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry. 2013;18(4):497–511. doi: 10.1038/mp.2012.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.