Abstract
Background:
Falls and their consequences are significant concerns for older adults, caregivers, and health care providers. Identification of fall risk is crucial for appropriate referral to preventive interventions. Falls are multifactorial; no single measure is an accurate diagnostic tool. There is limited information on which history question, self-report measure, or performance-based measure, or combination of measures, best predicts future falls.
Purpose:
First, to evaluate the predictive ability of history questions, self-report measures, and performance-based measures for assessing fall risk of community-dwelling older adults by calculating and comparing posttest probability (PoTP) values for individual test/measures. Second, to evaluate usefulness of cumulative PoTP for measures in combination.
Data Sources:
To be included, a study must have used fall status as an outcome or classification variable, have a sample size of at least 30 ambulatory community-living older adults (≥65 years), and track falls occurrence for a minimum of 6 months. Studies in acute or long-term care settings, as well as those including participants with significant cognitive or neuromuscular conditions related to increased fall risk, were excluded. Searches of Medline/PubMED and Cumulative Index of Nursing and Allied Health (CINAHL) from January 1990 through September 2013 identified 2294 abstracts concerned with fall risk assessment in community-dwelling older adults.
Study Selection:
Because the number of prospective studies of fall risk assessment was limited, retrospective studies that classified participants (faller/nonfallers) were also included. Ninety-five full-text articles met inclusion criteria; 59 contained necessary data for calculation of PoTP. The Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS) was used to assess each study's methodological quality.
Data Extraction:
Study design and QUADAS score determined the level of evidence. Data for calculation of sensitivity (Sn), specificity (Sp), likelihood ratios (LR), and PoTP values were available for 21 of 46 measures used as search terms. An additional 73 history questions, self-report measures, and performance-based measures were used in included articles; PoTP values could be calculated for 35.
Data Synthesis:
Evidence tables including PoTP values were constructed for 15 history questions, 15 self-report measures, and 26 performance-based measures. Recommendations for clinical practice were based on consensus.
Limitations:
Variations in study quality, procedures, and statistical analyses challenged data extraction, interpretation, and synthesis. There was insufficient data for calculation of PoTP values for 63 of 119 tests.
Conclusions:
No single test/measure demonstrated strong PoTP values. Five history questions, 2 self-report measures, and 5 performance-based measures may have clinical usefulness in assessing risk of falling on the basis of cumulative PoTP. Berg Balance Scale score (≤50 points), Timed Up and Go times (≥12 seconds), and 5 times sit-to-stand times (≥12) seconds are currently the most evidence-supported functional measures to determine individual risk of future falls. Shortfalls identified during review will direct researchers to address knowledge gaps.
Keywords: accidental falls, community-dwelling older adults, functional assessment
INTRODUCTION
As many as one-third of older adults fall at least once over the course of a year.1 Falls and fear of falling contribute to restricted activity as a strategy to reduce perceived risk of subsequent falls.2 Resultant secondary deconditioning may actually increase risk of falling.3 Fall-related injuries (eg, hip fractures and head injury) contribute to increasing care costs for older adults.4 Fall risk-reduction programs have received significant funding in public health initiatives.5 Nonetheless, accurately identifying those requiring intervention to reduce fall risk is challenging for health professionals caring for older adults.6
Susceptibility to falls results from an interaction of multiple factors: reduced efficacy of postural responses,7 diminished sensory acuity,8 impaired musculoskeletal,9 neuromuscular,9 and/or cardiopulmonary systems,10 deconditioning associated with inactivity,11 depression and low balance self-efficacy,12 polypharmacy,13 and a host of environmental factors.14 The multifactorial nature of fall risk complicates identification of those most at risk.15 Consequently, fall risk assessment tools are as plentiful as contributing factors (Table 1). Given the number of tests and measures available for fall risk assessment, how do clinicians select the best “diagnostic” tool(s) to examine their client's risk of falling? How does a given test or measure change degree of clinical certainty that a future fall is likely? Calculation of posttest probability (PoTP) allows a clinician to determine how much risk has shifted from a pretest probability of approximately 30% (the prevalence of fall among community-dwelling older adults).1,16,17 The first step in determining a measure's PoTP begins with consideration of its diagnostic accuracy, as indicated by sensitivity (Sn) and specificity (Sp).
Table 1. Measures Used as Search Terms and Additional Measures Identified During Review of Retrieved Articlesa.
| Includedb | Excludedc |
|---|---|
| Measures used as search terms | |
Self-report measures
Performance-based measures
|
Self-report measures
|
| Additional measures derived from article review | |
History questions
Self-report measures
Performance-based measures
|
Self-report measures
Performance-based measures
|
aIn order for a measure to be included in analysis, data extracted from research articles about the measure had to include number of participants who did/did not fall, the value of a threshold or cut score for the measure, and/or reported sensitivity and specificity values, such that posttest probability (PoTP) could be calculated.
bSufficient information for calculation of PoTP.
cInsufficient information for CALCULATION of PoTP.
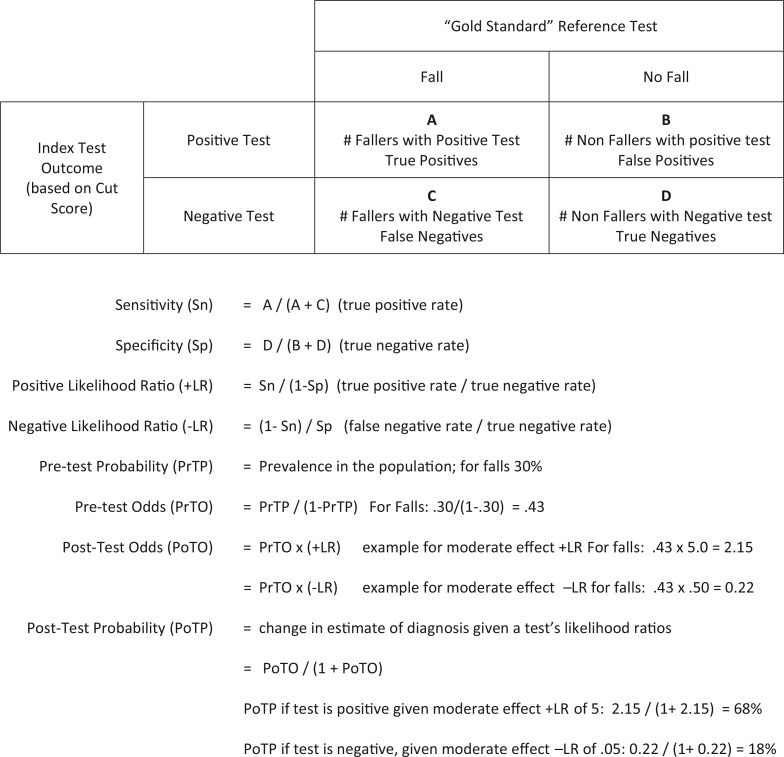
To determine diagnostic accuracy, a measure (index test) is compared with a gold standard or reference event (ie, a fall event).16 This comparison is based on a “cut point” that defines positive and negative test results. A 2×2 table can be constructed to classify participants by fall status and clinical test results on the basis of the defined “cut point” (Figure 1). Sn is calculated by dividing the number of persons who fell and have a positive test results by the total number of fallers: the test's true positive rate. High Sn indicates the test correctly identifies most people with the diagnosis; therefore, a negative result in a test with high Sn helps to rule out the diagnosis. Sp is calculated by dividing the number of persons who did not fall and have a negative test result by the total number of nonfallers: the test's true negative rate. High Sp indicates that the test correctly identifies most people who did not fall; therefore, a positive result on a test with high Sp helps to identify those most likely to fall. Few tests or measures achieve both high Sn and Sp values.
Figure 1.
Usefulness of a 2 × 2 table for interpreting test results. In this systematic review and meta-analysis, data about each test from multiple studies were combined to calculate an overall sensitivity and specificity values, and positive (+ LR) and negative (− LR) likelihood ratios. On the basis of consistent epidemiological evidence, pretest probability for future falls was set at 30%. Calculation of pretest odds from pretest probability, followed by calculation of posttest odds, allows estimation of posttest probability. Assuming a moderate effect + LR of 5 and − LR of 0.5, posttest probability after a positive test would increase from 30% to 68%. Assuming a moderate effect − LR of 0.5, posttest probability after a negative test would decrease from 30% to 18%. When test results are positive, the size of the increase in posttest probability beyond pretest predictive toward 100% determines how much “more sure” the clinician can be that an older adult would likely experience a future fall. When test results are negative, how much posttest probability decreases toward 0 from pretest value determines how much “more sure” that an older individual would not be likely to fall.
Sn and Sp values are used to calculate a measure's positive and negative likelihood ratios (+LR, −LR).16,17 The formula for calculation of LR is shown in Figure 1. An LR indicates what the expected test result would be in persons with the condition of interest compared with those without the condition. Both positive (+LR >1.0) and negative (−LR <1.0) likelihood ratios can be calculated for any test (see Figure 1). A +LR indicates the clinical usefulness of a positive test result: the larger the +LR value above 1.0, the more valuable the positive test result.16,17 The −LR indicates the usefulness of a negative test result: the smaller the value below 1.0, the more valuable the negative test result.16,17
Likelihood ratios are then used to calculate pre- and posttest odds, which serve as indicators of strength of association between exposure (test result as indicator of fall risk) and outcome (fall event). Pretest odds (PrTO) are calculated by dividing prevalence (pretest probability) by its inverse: for falls this would be 30%/(1%-30%), a value of 0.43. Posttest odds (PoTO) are developed by multiplying PrTO by the measure's +LR (for positive tests results) and −LR (for negative test results).
Finally, the informative PoTP, which indicates the degree of change in surety of diagnosis given a test's likelihood ratios, can be calculated. The pretest probability (PrTP) of falling for community-living older adults is estimated as 30%,1 with a PrTO of 0.43. Using these values and example LRs, we can calculate the PoTO and PoTP for an older adult on the basis of a positive and a negative test result (see Figure 1). If our fall-risk test has a moderate +LR of 5 and a moderate −LR of 0.5, a positive test result (high risk) would result in a PoTP of falling for this individual of 68%. A negative test result (low risk) would result in a PoTP of falling for this individual of 18%. Both values are substantially different from PrTP of 30%. For the clinician, this information enhances determination of who would/would not benefit from a more in-depth examination and intervention to reduce risk of falling.16,17
In clinical medicine, when no single diagnostic test has PoTP large enough to cross threshold for intervention, the results of several tests are combined to calculate a cumulative PoTP value.16 In effect, the PoTP of one test becomes the pretest probability for the next test. If both pretest probability (as in falls risk of 30%) and a test/measures' likelihood ratio values are moderate, as in most measures of balance and risk of falls, the cumulative PoTP can be thought of as increasing surety.16,17 Two or more positive tests with a high cumulative PoTP value (above the baseline PrTP of 30%) suggest the individual is at high risk of experiencing falls, and supports the need for intervention. Two or more negative tests leading to substantially lower PoTP (below the baseline PrTP of 30%) would indicate lower risk of future falls. Mixed results (some positive, some negative) are more challenging to interpret.
Physical therapists, like other health professionals, collect information about an individual's health and functional status is several ways: by asking questions about medical history (eg, do you remember falling in the last 6 months?), by administering self-report measures (eg, fear of falling scales or depression scales), and by using performance-based tests (eg, Berg Balance Scale, walking speed, or Timed Up and Go test). Combining multiple sources of information assists the diagnostic process to identify issues that can be addressed by intervention.18 It is not clear what history questions, self-report measures, or performance-based measures best identify those community-living older adults at risk of falling.
Although there have been systematic reviews of individual measures (eg, the Timed Up and Go19 and the Berg Balance Scale20), no reviews that provided measure-to-measure comparison of predictive properties for tools used to assess risk of falling were identified in the literature. The Academy of Geriatric Physical Therapists charged a team of 10 researchers and clinicians to undertake such a systematic review. This was to provide support of the work of another group charged to develop a clinical practice guideline for management of falls in later life. This systematic review has 2 aims: (1) to evaluate the predictive ability of fall risk assessment tools for community-dwelling older adults by calculating and comparing PoTP values, and (2) to explore usefulness of cumulative PoTP using test results from multiple measures. The measure-to-measure comparison and consolidation of findings will assist clinicians in selection of measures as well as in clinical decision making about need for intervention to prevent falls. It will also inform researchers where evidence about ability of a measure's ability to predict falls is lacking and needs further investigation.
METHODS
The Institute of Medicine Guidelines for Systematic Review,21 the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines,22 and the Cochrane Handbook of Systematic Reviews of Diagnostic Test Accuracy23 served as resources for this systematic review and meta-analysis.
A fall was defined as an event in which an older adult unintentionally came to rest on the ground or other lower supporting surface, unrelated to a medical incident or to an overwhelming external physical force.6 Risk was defined using the World Health Organization's (WHO) definition: the probability that an unwanted health event (eg a future fall) will occur was used.24 For older adults, fall risk is always present and cannot be reduced to zero, although many risk factors for falls are modifiable.
In this review, fall status (prospectively or retrospectively) was the gold standard to which the various index measures where compared. Based on the literature, a 6-month period was deemed sufficient time for fall occurrence. On the basis of anticipation that the number of prospective studies of fall risk assessment would be small, a decision was made to include retrospective studies tracking previous falls over at least a 6-month period as well. Although retrospective recall of falls may be somewhat inaccurate, given the high number of retrospective studies of falls in the literature, the combination of prospective and retrospective data provides “best available” evidence at the present time.
DATA SOURCES AND SEARCHES
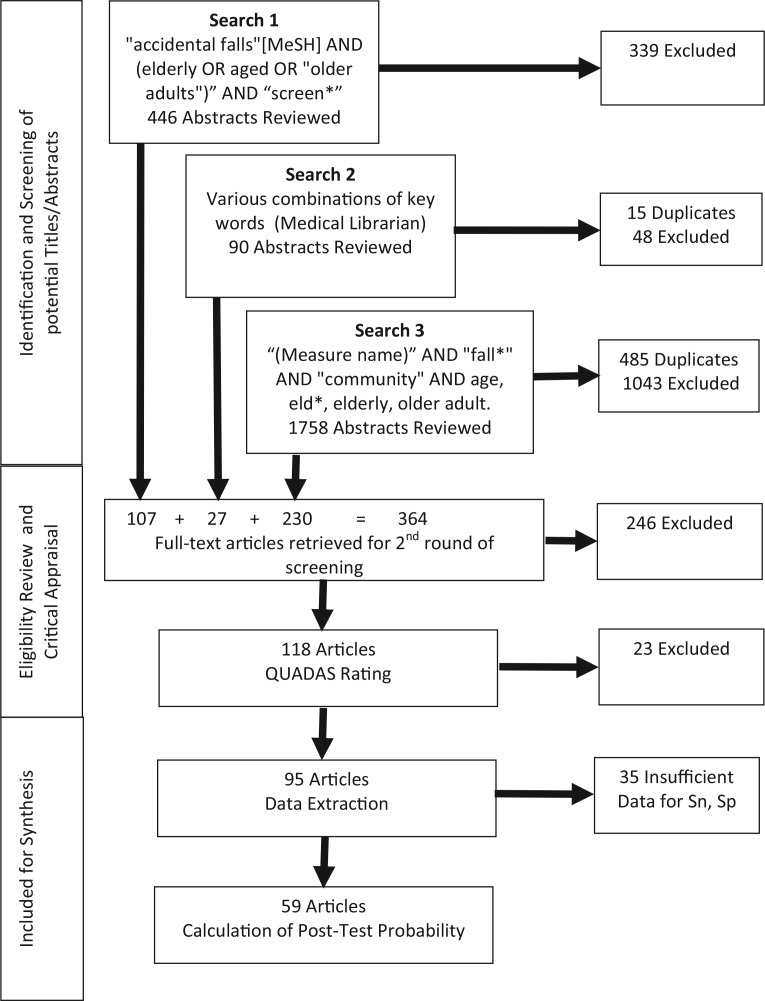
MEDLINE and CINAHL databases were searched, as those most likely to index geriatric, gerontology, and rehabilitation research literature. Search strategies (key words) and results are summarized in the PRISMA flow diagram of Figure 2. The first search did not yield the number or type of articles needed for a comprehensive review. A medical librarian carried out a second search by combining key words in various groupings. Unfortunately, search strings were not recorded and could not be accurately reformulated. To enhance search rigor, a third search was undertaken using names of specific measures gathered from websites (Rehabilitation Measures Database,25 PTNow,26 and the American Physical Therapy Association's Guide to Physical Therapist Practice18) and the team's clinical experience as search terms. References from retrieved articles were also reviewed. This multisearch strategy ensured that the combined final search results were as comprehensive as possible.
Figure 2.
PRISMA diagram for the systematic review process. A total of 2294 abstracts were reviewed; these included 500 duplicates and 1430 that did not immediately meet inclusion criteria. A total of 364 full-text articles were retrieved, examined, and appraised: an additional 269 did not meet inclusion criteria. Data were extracted from the remaining 95 articles; 57 of these contained information necessary for calculation of posttest probability.
Study Selection
To be included in the review, each study had to (1) include a study sample of 30 or more independently ambulatory (with/without assistive device) community-dwelling adults 65 years or older; (2) collect falls data for at least a 6-month period, either following study enrollment (prospective studies) or recall falls before the study enrollment (retrospective); (3) focus on evaluating risk of future falls and/or differentiating characteristics of fallers versus nonfallers; (4) use fall status (none, one, and/or recurrent) as an outcome variable (prospective) or classification variable (retrospective); and (5) be published in English, in a peer-reviewed journal between January 1990 and September 2013. The start date for the search was the year 1990 as the point in time that commonly used measures began to be developed (eg, Functional Reach in 1990); the end date was September 2013, when data examination began.
Studies were excluded from the review if they included (1) persons younger than 65 years; (2) participants with cognitive dysfunction, or with orthopedic or neurological diagnoses associated with elevated fall risk; (3) data from acute care, postacute care, or extended care settings; (4) little evidence of how falls were defined or documented; or (5) equipment unavailable in most physical therapy settings, such as force plates, computerized motion analysis, or other technology-based assessment systems.
Abstracts of all 2294 articles identified in the searches were retrieved and reviewed. Interrater reliability was addressed in a multistep training process. First, each researcher in the team reviewed the same set of 10 abstracts, applying inclusion and exclusion criteria. Next, all participated in a series of conference calls, and discussed the review process until consensus was reached for the set of 10 abstracts. By the review of the 10th abstract, the team reached a 95% agreement rate before discussion. Next, teams of 2 reviewers were assigned sets of 100 abstracts, and charged to reach agreement on inclusion/exclusion criteria in their sets. To reduce potential reviewer bias, reviewers were paired differently for each set of 100 abstracts, until all were reviewed. At the end of the abstract review process, 364 full-text articles were retrieved. Retrieved full-text articles were rescreened on the basis of inclusion/exclusion criteria before quality review and data extraction; an additional 246 failed to meet inclusion criteria, leaving 118 articles for quality assessment.
Quality Assessment
We used the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) Critical Appraisal Tool to evaluate methodological quality and risk of bias of retrieved studies.27 QUADAS is composed of 14 questions designed to assess validity, potential for bias, and methodological soundness of diagnostic studies. Items are scored as yes, no, unsure, or not applicable. Total criterion score is calculated as: 100 × (#yes responses)/(14 − # not applicable responses). Criterion scores were reported for all included studies. Interrater reliability was addressed as in the abstract review process. First, each researcher independently rated the same 5 articles using the QUADAS tool. This was followed by conference calls to discuss the rating process, and until consensus on rating of these 5 articles. There was 92% agreement by evaluation of the fifth article. Two person teams then rated sets of 20 articles with the goal of reaching consensus. Agreement about the QUADAS score between team members ranged from 90% to 97%. During quality assessment, 23 more articles failed to meet inclusion criteria, leaving 95 for data extraction
Data Extraction
The American Physical Therapy Association Section on Research's Evaluation Database to Guide Effectiveness (EDGE) Task Force data extraction form28 was used to record data extracted from each article. It was modified slightly to include level of evidence for studies of diagnostic accuracy as defined by Australia's National Health and Medical Research Council.29 Level of evidence for this project was defined as follows: Level I included prospective studies with QUADAS 75 or more as Level I evidence; Level II included prospective studies with QUADAS less than 75. Retrospective studies were classified as Level III, regardless of the QUADAS score.
Each researcher independently extracted data from sets of retrieved articles. Interrater reliability was determined by a second independent data extraction of a subset of 25 of the 90 remaining articles. Agreement ranged from 93% to 97% on the comparison of data extraction records for these 25 articles. The study coordinator performed a third reviewed to correct data when there was disagreement. Extracted data were combined into a summary Excel spreadsheet so that measures could be sorted by name.
Data Synthesis and Analysis
After sorting of data by measure name, reviewer teams used extracted data to construct individual evidence tables for each test/measure. The study coordinator reviewed these tables for accuracy. When number of fallers/nonfallers and number above and below cut point values were available, or if Sn and Sp were provided, 2×2 tables were constructed so that Sn, Sp, LRs, odds ratios and PoTP could be calculated.16,17 Fifty-nine of 95 articles (prospective evidence Level I n = 27; Level II n = 5; retrospective evidence Level III n = 27) contained information necessary for calculation of PoTP. Finally, 3 cumulative evidence tables were created on the basis of type of data collected: medical history questions (Table 2), self-report measures (Table 3), and performance-based measures (Table 4). These 3 tables summarized best evidence available from January 1990 to September 2013, and allowed direct comparison between measures.
Table 2. Summary of Findings for Determining Risk of Falls During Patient Medical History Component of the Physical Therapy Examinationa.
| History Questions | Author | Level | QUADAS Score | Study Type, mo | Fall Defined | Age, Mean (SD) | Fallers, N | Nonfallers, N | Cut Point | Fallers With +Test | Non Fallers With −Test | Difference P | Sn (CI95), % | Sp (CI95), % | +LR (CI95) | −LR (CI95) | Posttest Probability, % | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| If +Test | If −Test | |||||||||||||||||
| Activities of daily living (ADL) Not independent Self-report dichotomous |
Kwan et al30 | I | 84.6 | Pro (24) | Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | 2 IADL depend | 14 | 157 | NR | 16 (9-26) | 90 (85-94) | 1.7 (0.9-3.2) | 0.9 (0.8-1.0) | 42 | 28 |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | Any ADL depend | 12 | 52 | NR | 20 (11-33) | 90 (79-96) | 2.0 (0.8-4.9) | 0.9 (0.8-1.0) | 46 | 28 | |
| Tinetti et al32 | I | 76.9 | Pro (12) | Any fall | 76.9 (5.3) | 546 | 557 | Any ADL depend | 364 | 251 | ANOVA P < .05 | 67 (62-71) | 45 (41-49) | 1.2 (1.1-1.3) | 0.7 (0.6-0.9) | 34 | 23 | |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | Any ADL depend | 7 | 100 | NR | 9 (4-18) | 96 (90-99) | 2.3 (0.7-7.7) | 1.0 (0.9-1.0) | 50 | 30 | |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | Bathing depend | 74 | 44 | OR = 2.4 P = .003 |
64 (54-73) | 58 (46-69) | 1.5 (1.1-2.0) | 0.6 (0.5-0.9) | 39 | 20 | |
| Walking outside | 51 | 51 | OR = 1.6 P = .12 |
44 (35-53) | 67 (55-77) | 1.3 (0.9-2.0) | 0.8 (0.7-1.1) | 36 | 26 | |||||||||
| Dressing depend | 34 | 60 | OR = 1.6 P = .20 |
29 (21-38) | 79 (68-87) | 1.4 (0.8-2.3) | 0.9 (0.8-1.1) | 38 | 28 | |||||||||
| Transfer depend | 13 | 75 | OR = 9.5 P = .01 |
11 (6-18) | 99 (93-100) | 8.5 (1.1-64) | 0.9 (0.8-1.0) | 78 | 28 | |||||||||
| Stairs depend | 31 | 72 | OR = 2.2 P = .05 |
27 (19-36) | 95 (87-99) | 5.1 (1.9-14) | 0.8 (0.7-0.9) | 69 | 26 | |||||||||
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | Any ADL depend | 37 | 258 | χ2 P < .001 |
47 (36-58) | 87 (83-90) | 3.6 (2.5-5.2) | 0.6 (0.5-0.8) | 61 | 20 | |
| Flemming36 | III | 69.2 | Retro (4) | Any fall | 78.7 (7.2) | 40 | 267 | Any ADL depend | 37 | 75 | χ2 P = .005 |
93 (79-98) | 29 (23-34) | 1.3 (1.2-1.4) | 0.3 (0.1-0.8) | 36 | 11 | |
| Summary: Posttest probability of falling if positive for requiring ADL assistance (excluding Coll-Planas 2007 walking, dressing, transfer, stairs; to avoid duplication of subjects) | 1006 | 1533 | Any ADL depend | 545 | 937 | NA | 54 (51-57) | 61 (59-64) | 1.4 (1.3-1.5) | 0.8 (0.7-0.8) | 38 | 26 | ||||||
| Age | Stalenhoef et al37 | I | 84.6 | Retro (12) | Any fall | M: 77.2 (4.9) W: 78.5 (5.2) |
207 | 104 | ≥80 | 84 | 63 | NR | 41 (34-48) | 61 (51-70) | 1.0 (0.8-1.4) | 1.0 (0.9-1.2) | 30 | 30 |
| Yamada and Iscihashi38 | I | 84.6 | Retro (12) | Any fall | 80.5 (5.6) | 59 | 112 | ≥80 | 34 | 41 | NR | 58 (44-70) | 37 (28-46) | 0.9 (0.7-1.2) | 1.2 (0.8-1.7) | 28 | 34 | |
| LeClerc et al39 | II | 76.9 | Pro (6) | ≥2 falls | F: 79.5 (6.6) NF: 79.0 (6.9) |
99 | 769 | ≥75 | 72 | 185 | P > .05 | 73 (63-81) | 24 (21-27) | 1.0 (0.8-1.1) | 1.1 (0.8-1.6) | 30 | 32 | |
| Sohng et al40 | III | 92.3 | Retro (12) | Any fall | 73.3 (6.1) | 148 | 203 | ≥75 | 50 | 118 | NR | 34 (26-42) | 58 (51-65) | 0.8 (0.6-1.1) | 1.1 (1.0-1.3) | 23 | 32 | |
| Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | ≥80 | 11 | 10 | NR | 32 (17-51) | 79 (69-87) | 1.5 (0.8-2.9) | 0.9 (0.7-1.1) | 39 | 28 | |
| Summary: Posttest probability of falling if >80 y of age | 547 | 1269 | >80 | 251 | 471 | NA | 46 (42-50) | 37 (34-40) | 0.7 (0.7-0.8) | 1.5 (1.3-1.6) | 23 | 39 | ||||||
| Ambulatory assistive device use Self-report and observation |
Sai et al42 | I | 92.3 | Pro (12) | Any fall | 76.7 (6.1) | 95 | 42 | Yes | 30 | 40 | χ2 P < .05 |
32 (22-42) | 95 (84-99) | 6.6 (1.7-26.0) | 0.7 (0.6-0.8) | 74 | 23 |
| Brauer et al43 | I | 84.6 | Pro (6) | Any fall | 71 (5) | 35 | 65 | Yes | 2 | 60 | χ2 P > .05 |
6 (1-19) | 92 (83-97) | 0.7 (0.2-3.6) | 1.0 (0.9-1.1) | 23 | 30 | |
| Kwan et al30 | I | 84.6 | Pro (24) | Any fall | 74.9 (6.4) | 86 | 174 | Yes | 15 | 165 | NR | 17 (10-27) | 95 (90-98) | 3.4 (1.5-7.4) | 0.9 (0.8-1.0) | 59 | 28 | |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | Yes | 15 | 50 | NR | 28 (16-42) | 86 (75-94) | 2.0 (0.9-4.4) | 0.8 (0.7-1.0) | 46 | 28 | |
| Tinetti et al32 | I | 84.6 | Pro (12) | Any fall | 76.9 (5.3) | 546 | 557 | Yes | 80 | 512 | ANOVA P < .05 |
15 (12-18) | 92 (89-94) | 1.9 (1.3-2.6) | 0.9 (0.9-1.0) | 45 | 28 | |
| Yamada and Iscihashi38 | I | 84.6 | Pro (12) | Any fall | 80.5 (5.6) | 59 | 112 | Yes | 5 | 99 | χ2 P = .61 |
9 (3-19) | 88 (81-94) | 0.7 (0.3-2.0) | 1.0 (0.0-1.2) | 23 | 30 | |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | Yes | 12 | 93 | NR | 15 (8-25) | 90 (83-95) | 1.5 (0.7-3.2) | 0.9 (0.8-1.1) | 39 | 28 | |
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | Yes | 45 | 223 | χ2 P < .001 |
56 (44-67) | 75 (70-80) | 2.2 (1.7-2.9) | 0.6 (0.5-0.8) | 49 | 20 | |
| Shumway-Cook et al44 | III | 84.5 | Retro (6) | Any fall | F: 86.2 (6.4) NF: 78.4 (5.8) |
15 | 15 | Yes | 12 | 15 | NR | 80 (52-96) | 100 (78-100) | NA | 0.2 (0.1-0.6) | NA | 8 | |
| Desai et al45 | III | 76.9 | Retro (12) | Any fall | F 81.5 (6.9) NF 79.4 (5.5) |
47 | 25 | Yes | 35 | 7 | χ2 P > .05 |
74 (60-86) | 28 (12-49) | 1.0 (0.8-1.4) | 0.9 (0.4-2.0) | 30 | 28 | |
| Huang46 | III | 76.9 | Retro (12) | Any fall | 76 (NR) | 199 | 197 | Yes | 92 | 138 | χ2 P < .001 |
46 (39-53) | 70 (63-76) | 1.5 (1.2-2.0) | 0.8 (0.7-0.9) | 39 | 26 | |
| Shumway-Cook et al47 | III | 76.9 | Retro (6) | ≥2 falls | 78.7 (7.2) | 22 | 22 | Yes | 5 | 22 | χ2 P < .05 |
23 (8-45) | 100 (85-100) | NA | 0.8 (0.6-1.0) | NA | 26 | |
| Flemming36 | III | 69.2 | Pro (4) | Any fall | 78.7 (7.2) | 40 | 267 | Yes | 37 | 77 | χ2 P = .004 |
93 (80-98) | 29 (24-35) | 1.3 (1.2-1.5) | 0.3 (0.1-0.8) | 36 | 11 | |
| Summary: Posttest probability of falling if ambulatory assistive device use | 1362 | 1935 | Yes | 385 | 1501 | NA | 28 (26-31) | 78 (76-79) | 1.3 (1.1-1.4) | 0.9 (0.9-1.0) | 36 | 26 | ||||||
| Alcohol consumption Self-report (yes/no) |
Sai et al42 | I | 92.3 | Pro (12) | Any fall | 76.7 (6.1) | 95 | 42 | Yes | 46 | 18 | NR | 48 (38-59) | 43 (28-59) | 0.9 (0.6-1.2) | 1.2 (0.8-1.8) | 28 | 34 |
| Bongue et al48 | I | 84.6 | Pro (12) | 70.7 (4.6) | 563 | 1196 | Yes | 509 | 101 | NR | 90 (88-93) | 8 (7-10) | 1.0 (1.0-1.0) | 1.1 (0.8-1.5) | 30 | 32 | ||
| Swanenburg et al49 | I | 76.9 | Pro (12) | ≥2 falls | 73.7 (7) | 85 | 185 | Daily | 27 | 154 | NR | 32 (22-43) | 83 (77-88) | 1.9 (1.2-3.0) | 0.8 (0.7-1.0) | 45 | 26 | |
| LeClerc et al39 | II | 76.9 | Pro (6) | ≥2 falls | F: 79.5 (6.6) NF: 79.0 (6.9) |
769 | 99 | Yes | 155 | 78 | χ2 P > .05 |
20 (17-23) | 79 (69-86) | 1.0 (0.6-1.4) | 1.0 (0.9-1.1) | 30 | 30 | |
| Sohng et al40 | III | 92.3 | Retro (12) | Any fall | 73.3 (6.1) | 148 | 203 | Yes | 61 | 111 | χ2 P = .44 |
41 (33-50) | 55 (48-62) | 0.9 (0.7-1.2) | 1.1 (0.9-1.3) | 28 | 32 | |
| Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | Yes | 11 | 49 | NR | 32 (17-51) | 61 (49-71) | 0.8 (0.5-1.4) | 1.1 (0.8-1.5) | 28 | 32 | |
| Huang46 | III | 76.9 | Retro (12) | Any fall | F: 81.3 (5.1) NF: 79.7 (4.3) |
200 | 201 | Yes | 18 | 175 | χ2 P > .05 |
9 (5-14) | 87 (82-91) | 0.7 (0.4-1.2) | 1.1 (1.0-1.1) | 23 | 32 | |
| Summary: Posttest probability of falling if history of alcohol consumption | 1894 | 2007 | Yes | 827 | 686 | NA | 44 (41-46) | 34 (32-36) | 0.7 (0.6-0.7) | 1.7 (1.6-1.8) | 23 | 42 | ||||||
| Depression Self-report (yes/no) |
Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | Yes | 16 | 48 | NR | 27 (16-40) | 83 (71-91) | 1.6 (0.8-3.2) | 0.9 (0.7-1.1) | 41 | 28 |
| Difficulty walking or missteps Self-report | Srygley et al50 | I | 84.6 | Pro | Any fall | 76.4 (4.3) | 68 | 198 | ≥2 missteps | 9 | 177 | NR | 13 (6-24) | 89 (84-93) | 1.3 (0.6-2.6) | 1.0 (0.9-1.1) | 36 | 30 |
| Sohng et al40 | III | 92.3 | Retro (12) | Any fall | 73.3 (6.1) | 148 | 203 | Difficulty walking | 71 | 128 | χ2 P = .05 |
48 (40-56) | 63 (56-70) | 1.3 (1.0-1.7) | 0.8 (0.7-1.0) | 36 | 23 | |
| Summary: Posttest probability of falling if self-reported difficulty walking | 216 | 401 | Difficulty walking | 80 | 305 | NA | 37 (931-44) | 76 (72-80) | 1.6 (1.2-2.0) | 0.8 (0.7-0.9) | 41 | 26 | ||||||
| Fear of falling Self-report (yes/no) |
Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | Yes | 33 | 63 | OR = 1.9 P = .07 |
28 (20-38) | 83 (73-91) | 1.7 (0.9-3.0) | 0.9 (0.7-1.0) | 42 | 28 |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | Yes | 20 | 47 | NR | 34 (22-47) | 81 (69-90) | 1.8 (0.9-3.4) | 0.8 (0.7-1.0) | 44 | 26 | |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | Yes | 11 | 97 | NR | 14 (7-24) | 93 (87-97) | 2.1 (0.9-5.2) | 0.9 (0.8-1.0) | 47 | 28 | |
| Swanenburg et al49 | I | 76.9 | Pro (12) | ≥2 falls | 73.7 (7) | 85 | 185 | Yes | 24 | 149 | NR | 28 (19-39) | 81 (74-86) | 1.5 (0.9-2.3) | 0.9 (0.8-1.0) | 39 | 28 | |
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | Yes | 48 | 219 | χ2 P < .001 |
60 (48-70) | 70 (68-79) | 2.3 (1.7-2.9) | 0.6 (0.4-0.7) | 50 | 20 | |
| Keskin et al51 | III | 84.6 | Retro | Any fall | F: 68 (3) NF: 70 (5) | 12 | 19 | Yes | 5 | 18 | χ2 P = 02 |
42 (15-72) | 95 (74-100) | 7.9 (1.1-60) | 0.6 (0.4-1.0) | 77 | 20 | |
| Flemming36 | III | 69.2 | Retro (4) | Any fall | 78.7 (7.2) | 40 | 267 | Yes | 24 | 165 | χ2 P = .009 |
60 (43-75) | 62 (56-68) | 1.6 (1.2-2.1) | 0.7 (0.4-1.0) | 41 | 23 | |
| Summary: Posttest probability of falling if self-report of fear of falling | 471 | 1006 | Yes | 165 | 758 | NA | 35 (31-40) | 75 (73-78) | 1.4 (1.2-1.7) | 0.9 (0.8-0.9) | 38 | 28 | ||||||
| Health status Self-reported (fair or poor) |
Kwan et al30 | I | 84.6 | Pro (24) | Any fall | 74.9 (6.4) | 86 | 174 | ≤ fair | 69 | 49 | IRR = 1.55 P = NR |
80 (70-88) | 28 (22-35) | 1.1 (1.0-1.3) | 0.7 (0.4-1.1) | 32 | 23 |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | ≤ fair | 12 | 38 | NR | 20 (11-33) | 66 (52-78) | 0.6 (0.3-1.1) | 1.2 (2.0-1.1) | 20 | 34 | |
| Iinattiniemi et al52 | II | 69.2 | Pro (11) | Any fall | F: 88(3) NF: 88 (2) | 273 | 282 | ≤ fair | 49 | 242 | χ2 P = .22 |
18 (14-23) | 86 (81-90) | 1.3 (0.9-1.9) | 1.0 (0.9-1.0) | 36 | 30 | |
| Summary: Posttest probability of falling if health is rated fair or poor | 418 | 514 | ≤ fair | 130 | 329 | NA | 31 (27-36) | 64 (60-68) | 0.9 (0.7-1.0) | 1.1 (1.0-1.2) | 28 | 32 | ||||||
| History of falling Self-report | Aoyama et al53 | I | 92.3 | Pro (6) | Any fall | 80.5 (5.7) | 25 | 33 | Any fall | 18 | 13 | NR | 72 (51-88) | 39 (23-58) | 1.2 (0.8-1.7) | 0.7 (0.3-1.5) | 34 | 23 |
| Herman et al54 | I | 92.3 | Pro (24) | Any fall | 76.3 (6.1) | 131 | 131 | Any fall | 46 | 116 | χ2 P < .001 |
35 (27-44) | 89 (82-93) | 3.1 (1.8-5.2) | 0.7 (0.6-0.8) | 57 | 23 | |
| Lindeman et al55 | I | 92.3 | Pro (12) | Any fall | F: 68.8 (6.0) NF: 66.5 (5.8) |
30 | 26 | Any fall | 19 | 20 | χ2 P = .003 |
63 (43-80) | 77 (56-91) | 2.7 (1.3-5.8) | 0.5 (0.3-0.8) | 54 | 18 | |
| Sai et al42 | I | 92.3 | Pro (12) | Any fall | 76.7 (6.1) | 95 | 42 | Any fall | 54 | 26 | OR = 3.8 P < .05 |
57 (46-67) | 62 (46-76) | 1.5 (1.0-2.3) | 0.7 (0.5-1.0) | 39 | 23 | |
| Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | Any fall | 236 | 965 | NR | 42 (38-46) | 81 (78-83) | 2.2 (1.9-2.5) | 0.7 (0.7-0.8) | 49 | 23 | |
| Brauer et al43 | I | 84.6 | Pro (6) | Any fall | 71 (5) | 35 | 65 | Any fall | 19 | 49 | χ2 P < .05 |
54 (37-71) | 75 (63-85) | 2.2 (1.3-3.7) | 0.6 (0.4-0.9) | 49 | 20 | |
| Kwan et al30 | I | 84.6 | Pro (24) | Any fall | 74.9 (6.4) | 86 | 174 | Any fall | 33 | 135 | NR | 38 (28-50) | 78 (71-84) | 1.7 (1.2-2.5) | 0.8 (0.7-1.0) | 42 | 26 | |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | Any fall | 34 | 58 | NR | 58 (44-70) | 100 (93-100) | NA | 0.4 (0.3-0.6) | NA | 15 | |
| Panzer et al56 | I | 84.6 | Pro (12) | ≥2 falls | F: 80.1 (6.2) NF: 75.1 (6.5) |
39 | 23 | ≥2 falls | 23 | 6 | χ2 P = .24 |
59 (42-74) | 26 (10-48) | 0.8 (0.6-1.1) | 1.6 (0.7-3.4) | 26 | 41 | |
| Stalenhoef et al37 | I | 84.6 | Pro (9) | ≥2 falls | M: 77.2 (4.9) W: 78.5 (5.2) |
46 | 192 | Any fall | 7 | 133 | OR = 3.0 | 15 (6-29) | 69 (62-75) | 0.5 (0.3-1.0) | 0.6 (0.5-0.7) | 68 | 20 | |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | Any fall | 93 | 31 | OR = 1.8 P = .002 |
80 (72-87) | 41 (30-53) | 1.4 (1.1-1.7) | 0.5 (0.3-0.8) | 38 | 18 | |
| LeClerc et al39 | I | 76.9 | Pro (6) | ≥2 falls | F: 79.5 (6.6) NF: 79.0 (6.9) |
99 | 769 | ≥2 falls | 65 | 496 | χ2 P < .001 |
66 (55-75) | 65 (61-68) | 1.9 (1.6-2.2) | 0.5 (0.4-0.7) | 45 | 18 | |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | Any fall | 31 | 89 | NR | 40 (29-51) | 86 (77-92) | 2.8 (1.6-4.7) | 0.7 (0.6-0.9) | 55 | 23 | |
| Swanenburg et al49 | I | 76.9 | Pro (12) | ≥2 falls | 73.7 (7) | 85 | 185 | ≥2 falls | 23 | 173 | NR | 27 (18-38) | 93 (89-96) | 4.2 (2.2-8.0) | 0.8 (0.7-0.9) | 64 | 26 | |
| Buatois et al57 | II | 69.2 | Pro (18) | ≥2 falls | 70.1 (4.4) | 96 | 903 | ≥2 falls | 53 | 743 | χ2 P < .001 |
55 (45-65) | 82 (80-85) | 3.1 (2.5-3.9) | 0.5 (0.4-0.7) | 57 | 18 | |
| Flemming36 | II | 69.2 | Pro (4) | Any fall | 78.7 (7.2) | 40 | 267 | Any fall | 27 | 152 | χ2 P = .004 |
68 (51-81) | 57 (51-63) | 1.6 (1.2-2.0) | 0.6 (0.4-0.9) | 41 | 20 | |
| Gerdhem et al58 | II | 69.2 | Pro (12) | Any fall | F: 75 (NR) NF: NR |
232 | 746 | Any fall | 103 | 585 | OR = 2.9 P < .05 |
44 (38-51) | 78 (75-81) | 2.1 (1.7-2.5) | 0.7 (0.6-0.8) | 47 | 23 | |
| Iinattiniemi et al52 | II | 69.2 | Pro (11) | Any fall | F: 88 (3) NF: 88 (2) |
273 | 282 | ≥2 falls | 88 | 243 | χ2 P < .01 |
32 (27-38) | 86 (82-90) | 2.3 (1.7-3.3) | 0.8 (0.7-0.9) | 50 | 26 | |
| Myers et al59 | III | 86.5 | Retro (12) | Any fall | 74.5 (8.3) | 17 | 20 | Any fall | 14 | 15 | χ2 P < .01 |
82 (57-96) | 75 (51-91) | 3.3 (1.5-7.3) | 0.2 (0.1-0.7) | 59 | 8 | |
| Summary: Posttest probability of falling if history of previous fall/s | 2109 | 5292 | Any fall | 906 | 4047 | NA | 43 (41-45) | 77 (75-78) | 1.8 (1.7-2.0) | 0.8 (0.7-0.8) | 44 | 26 | ||||||
| History of imbalance Self-report |
Shumway-Cook et al44 | III | 76.9 | Retro (6) | ≥2 falls | 78.7 (7.2) | 22 | 22 | Yes | 21 | 9 | χ2 P = .0002 |
95 (77-100) | 59 (36-79) | 2.3 (1.4-3.9) | 0.1 (0.0-0.5) | 50 | 4 |
| Limited physical activity or exercise Self-report | Kwan et al30 | I | 84.6 | Pro (24) | Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | Avoid stairs | 54 | 97 | NR | 63 (52-73) | 56 (48-63) | 1.4 (1.1-1.8) | 0.7 (0.5-0.9) | 38 | 23 |
| Swanenburg et al49 | I | 76.9 | Pro (12) | 2+ falls | 73.7 (7) | 85 | 185 | Sedentary | 8 | 171 | NR | 9 (4-18) | 92 (88-96) | 1.2 (.5-2.8) | 1.0 (0.9-1.1) | 30 | 30 | |
| Tinetti et al32 | I | 84.6 | Pro (12) | Any fall | 76.9 (5.3) | 546 | 557 | Walk <3 blocks/d | 329 | 288 | ANOVA P < .05 |
60 (56-64) | 52 (48-56) | 1.3 (1.1-1.4) | 0.8 (0.7-0.9) | 36 | 26 | |
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | <3 h | 58 | 164 | χ2 P < .001 |
72 | 55 | 1.6 | 0.5 | 41 | 18 | |
| Sohng et al40 | III | 92.3 | Retro (12) | Any fall | 73.3 (6.1) | 148 | 203 | Stayed home | 42 | 138 | NR | 28 (21-36) | 68 (61-74) | 0.9 (0.6-1.2) | 1.1 (0.9-1.2) | 26 | 32 | |
| Karlsson et al60 | III | 77.9 | Retro (12) | ≥2 falls | 75 (NR) | 2049 | 8928 | No exercise | 1443 | 3108 | Regression P < .01 |
70 (68-72) | 35 (34-36) | 1.1 (1.1-1.1) | 0.8 (0.8-0.9) | 32 | 26 | |
| No HHW | 738 | 6071 | Regression P < .01 |
36 (34-38) | 70 (69-71) | 1.2 (1.1-1.3) | 0.9 (0.9-0.9) | 34 | 28 | |||||||||
| Iinattiniemi et al52 | III | 69.2 | Retro (11) | Any fall | 88 (2) | 273 | 282 | Sedentary | 81 | 219 | χ2 P = .06 |
30 (24-35) | 78 (72-82) | 1.3 (1.0-1.8) | 0.9 (0.8-1.0) | 36 | 28 | |
| Rosengren et al61 | III | 64.2 | Retro (12) | Any fall | F: 74.8 (NR) NF: 73.7 (NR) |
1918 | 8912 | No exercise | 1283 | 2683 | χ2 P = .2 |
67 (65-69) | 30 (29-31) | 1.0 (0.9-1.0) | 1.1 (1.0-1.2) | 30 | 32 | |
| No HHW | 683 | 6042 | χ2 P = .004 |
37 (33-38) | 68 (67-69) | 1.1 (1.0-1.2) | 0.9 (0.9-1.0) | 32 | 28 | |||||||||
| Summary: Posttest probability of falling if self-report of limited habitual physical activity (excluding Karslon and Rosengren HHW to avoid duplication of subjects) | 5186 | 19 538 | Limited physical activity | 3298 | 6867 | NA | 64 (2-65) | 35 (34-36) | 1.0 (1.0-1.0) | 1.0 (1.0-1.1) | 30 | 30 | ||||||
| Nocturia, incontinence, urinary urgency, or difficulty Self-report | Stewart et al62 | III | 84.6 | Retro (12) | Any fall | W: 79.9 (4.6) M: 80.0 (4.2) |
254 | 1254 | ≥2 nocturia | 141 | 688 | OR = 1.8 P = .03 |
56 (49-62) | 55 (52-58) | 1.2 (1.1-1.4) | 0.8 (0.7-0.9) | 34 | 26 |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | ≥2 nocturia | 46 | 48 | OR = 1.1 P = .64 |
40 (31-49) | 63 (51-74) | 1.1 (0.7-1.6) | 1.0 (0.8-1.2) | 32 | 30 | |
| Bongue et al48 | I | 84.6 | PRO (12) | Any fall | 70.7 (4.6) | 563 | 1196 | Yes | 108 | 1066 | OR = 1.9 P = NR |
19 (16-23) | 89 (87-91) | 1.8 (1.4-2.2) | 0.9 (0.9-1.0) | 44 | 28 | |
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | Yes | 19 | 254 | χ2 P = .05 |
23 (15-34) | 86 (81-89) | 1.6 (1.0-2.6) | 0.9 (0.8-1.0) | 41 | 28 | |
| Huang46 | III | 76.9 | Retro (12) | Any fall | F: 81.3 (5.1) NF: 79.7 (4.3) |
195 | 202 | Yes | 66 | 160 | χ2 P < .001 |
34 (27-41) | 79 (73-85) | 1.6 (1.2-2.3) | 0.8 (0.7-0.9) | 41 | 26 | |
| de Rekeneire et al63 |
III | 69.2 | Retro (12) | Any fall | Range: 70-79 | 652 | 2398 | Yes | 314 | 1537 | χ2 P < .01 |
48 (44-52) | 64 (62-66) | 1.3 (1.2-1.5) | 0.8 (0.8-0.9) | 36 | 26 | |
| Flemming36 | III | 69.2 | Retro (4) | Any fall | 78.7 (7.2) | 40 | 267 | Yes | 16 | 195 | χ2 P = .09 |
40 (25-57) | 73 (67-78) | 1.5 (1.0-1.3) | 0.8 (0.6-1.1) | 39 | 26 | |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | Yes | 57 | 46 | OR = 1.5 P = NR |
49 (40-59) | 61 (49-72) | 1.2 (0.9-1.7) | 0.8 (0.7-1.1) | 60 | 26 | |
| Iinattiniemi et al52 | III | 69.2 | Retro (11) | Any fall | 88 (2) | 273 | 282 | Yes | 30 | 267 | χ2 P = .01 |
11 (8-15) | 95 (91-97) | 2.1 (1.1-3.8) | 0.9 (0.9-1.0) | 47 | 28 | |
| Summary: Posttest probability if any urinary difficulty | 2290 | 6048 | Any urinary difficulty | 797 | 14 261 | NA | 35 (33-37) | 70 (69-72) | 1.2 (1.1-1.3) | 0.9 (0.9-1.0) | 34 | 26 | ||||||
| Pain Self-report | Kwan et al30 | I | 84.6 | Pro (24) | Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | Significant | 45 | 134 | NR | 47 (36-58) | 74 (67-80) | 1.8 (1.3-2.5) | 0.7 (0.6-0.9) | 44 | 23 |
| Polypharmacy ≥4 medications, self-report | Peeters et al64 | I | 93.3 | Pro (37) | ≥2 falls | F: 76.9 (6.9) NF: 74.9 (7.3) |
325 | 1004 | ≥4 meds | 96 | 777 | χ2 P = .01 |
30 (25-35) | 77 (75-80) | 1.3 (1.1-1.6) | 0.9 (0.8-1.0) | 36 | 28 |
| Kwan et al30 | I | 84.6 | Pro (24) | ≥2 falls | 74.9 (6.4) | 86 | 174 | ≥4 meds | 33 | 135 | NR | 38 (28-49) | 78 (71-84) | 1.7 (1.2-2.5) | 0.8 (0.7-1.0) | 42 | 26 | |
| Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | ≥4 meds | 14 | 150 | NR | 16 (9-26) | 86 (80-91) | 1.2 (0.6-1.2) | 1.0 (0.9-1.1) | 34 | 30 | |||||
| Brauer et al43 | I | 84.6 | Pro (6) | Any fall | 71 (5) | 35 | 65 | ≥3 meds | 7 | 45 | χ2 P > .05 |
20 (8-37) | 69 (57-80) | 0.7 (0.2-1.4) | 1.2 (0.9-1.5) | 23 | 34 | |
| Muir et al31 | I | 84.6 | Pro (12) | Any fall | 79.7 (5.3) | 59 | 58 | ≥4 meds | 48 | 13 | NR | 81 (69-90) | 22 (13-35) | 1.1 (0.9-1.3) | 0.8 (0.4-1.7) | 32 | 26 | |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | ≥5 meds | 74 | 32 | OR = 1.2 P = .06 |
64 (54-73) | 42 (31-54) | 1.1 (0.9-1.4) | 0.9 (0.6-1.3) | 32 | 28 | |
| Swanenburg et al49 | I | 76.9 | Pro (12) | ≥2 falls | 73.7 (7) | 85 | 185 | ≥4 meds | 54 | 110 | NR | 64 (52-74) | 59 (52-67) | 1.6 (1.2-2.0) | 0.6 (0.5-0.8) | 41 | 20 | |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | ≥4 meds | 64 | 35 | NR | 82 (72-90) | 34 (25-44) | 1.2 (1.0-1.5) | 0.5 (0.3-0.9) | 34 | 18 | |
| LeClerc et al39 | I | 76.9 | Pro (6) | ≥2 falls | F: 79.6 (6.6) NF: 79.0 (6.9) |
99 | 769 | ≥4 meds | 91 | 99 | χ2 P > .05 |
92 (85-96) | 13 (11-15) | 1.1 (1.0-1.1) | 0.6 (0.3-1.3) | 32 | 20 | |
| Buatois et al57 | II | 69.2 | Pro (18) | ≥2 falls | 70.1 (4.4) | 96 | 903 | ≥4 meds | 52 | 569 | χ2 P = .001 |
54 (44-64) | 63 (60-67) | 1.5 (1.2-1.8) | 0.7 (0.6-0.9) | 39 | 23 | |
| Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | ≥6 meds | 10 | 47 | NR | 29 (15-48) | 58 (47-69) | 0.7 (0.4-1.3) | 1.2 (0.9-1.6) | 23 | 34 | |
| Sai et al42 | III | 92.3 | Retro (12) | Any fall | 76.7 (6.1) | 95 | 42 | ≥4 meds | 35 | 35 | NR | 37 (27-47) | 83 (69-93) | 2.2 (1.2-4.6) | 0.8 (0.6-0.9) | 49 | 26 | |
| Perracini et al65 | III | 84.6 | Retro (12) | Any fall | F-LA 87/MA 79 NF-La 78/MA 76 |
68 | 54 | ≥5 meds | 41 | 30 | χ2 P = .03 |
60 (48-72) | 56 (41-69) | 1.4 (1.0-1.9) | 0.7 (0.5-1.0) | 38 | 23 | |
| Shumway-Cook et al47 | III | 84.5 | Retro (6) | Any fall | F: 86.2 (6.4) NF: 78.4 (5.8) |
15 | 15 | ≥4 meds | 2 | 15 | NR | 13 (2-40) | 100 (78-100) | NA | 0.9 (0.7-1.1) | NA | 28 | |
| Huang46 | III | 76.9 | Retro (12) | Any fall | F: 81.3 (5.1) NF: 79.7 (4.3) |
190 | 190 | ≥4 meds | 78 | 129 | χ2 P < .05 |
41 (34-48) | 70 (63-76) | 1.4 (1.0-1.8) | 0.9 (0.7-1.0) | 38 | 28 | |
| Flemming36 | III | 69.2 | Retro (4) | Any fall | 78.7 (7.2) | 40 | 267 | ≥4 meds | 34 | 71 | χ2 P = .12 |
85 (70-94) | 27 (21-32) | 1.2 (1.0-1.3) | 0.6 (0.3-1.2) | 34 | 20 | |
| Summary: Posttest probability of falling if taking ≥4 medications of any kind | 1507 | 4161 | ≥4 meds | 733 | 2292 | NA | 48 (46-51) | 55 (54-57) | 1.1 (1.0-1.2) | 0.9 (0.9-1.0) | 32 | 28 | ||||||
| Psychoactive medications Self-report (yes/no) | Beauchet et al66 | I | 92.3 | Pro (12) | Any fall | 84.8 (5.2) | 54 | 133 | Any | 30 | 67 | χ2 P = .46 |
56 (41-69) | 50 (42-59) | 1.1 (0.8-1.5) | 0.9 (0.6-1.3) | 32 | 28 |
| Peeters et al64 | I | 93.3 | Pro (37) | ≥2 falls | F: 76.9 (6.9) NF: 74.9 (7.3) |
325 | 1004 | Any | 67 | 877 | χ2 P < .001 |
21 (16-26) | 89 (86-90) | 1.8 (1.4-2.4) | 0.9 (0.8-1.0) | 44 | 28 | |
| Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | Any | 135 | 1030 | NR | 24 (21-27) | 86 (84-88) | 1.7 (1.4-2.1) | 0.9 (0.8-0.9) | 42 | 28 | |
| Kwan et al30 | I | 84.6 | Pro (24) | Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | Any | 7 | 165 | NR | 8 (3-16) | 95 (90-98) | 1.6 (0.6-4.1) | 1.0 (0.9-1.0) | 41 | 30 | |
| Peeters et al67 | I | 84.6 | Pro (36) | Any Fall | 1F: 74.9 (6.4) ≥2F: 77.0 (6.9) NF: 74.8 (6.2) |
740 | 597 | Any | 81 | 535 | χ2 P < .001 |
11 (9-13) | 90 (87-92) | 1.1 (0.8-1.4) | 1.0 (1.0-1.0) | 32 | 30 | |
| Tinetti et al32 | I | 84.6 | Pro (12) | Any fall | 76.9 (5.3) | 546 | 557 | Any | 89 | 512 | ANOVA P < .05 |
16 (13-20) | 92 (89-94) | 2.0 (1.4-2.8) | 0.9 (0.9-1.0) | 46 | 28 | |
| LeClerc et al39 | II | 76.9 | Pro (6) | ≥2 falls | F: 79.5 (6.6) NF: 79.0 (6.9) |
99 | 769 | Any | 50 | 406 | χ2 P > .05 |
51 (40-61) | 53 (49-56) | 1.1 (0.9-1.3) | 0.9 (0.8-1.2) | 32 | 28 | |
| Buatois et al57 | II | 69.2 | Pro (18+) | ≥2 falls | 70.1 (4.4) | 96 | 903 | Any | 19 | 812 | χ2 P = .06 |
20 (12-29) | 95 (88-92) | 2.0 (1.3-3.1) | 0.9 (0.8-1.0) | 46 | 28 | |
| Hellstrom et al35 | III | 100 | Retro (6) | Any fall | 81.7 (4.8) | 81 | 297 | Any | 62 | 218 | χ2 P < .02 |
77 (66-85) | 73 (68-78) | 2.9 (2.3-3.6) | 0.3 (0.2-0.5) | 55 | 11 | |
| Huang46 | III | 76.9 | Retro (12) | Any fall | F: 81.3 (5.1) NF: 79.7 (4.3) |
194 | 198 | Any | 44 | 176 | χ2 P < .05 |
23 (17-29) | 87 (81-91) | 1.7 (1.1-2.7) | 0.9 (0.8-1.0) | 42 | 28 | |
| de Rekeneire et al63 |
III | 69.2 | Retro (12) | Any fall | Range: 70-79 | 652 | 2398 | Any | 48 | 2288 | χ2 P = .01 |
7 (5-10) | 95 (95-96) | 1.6 (1.2-2.2) | 1.0 (0.9-1.0) | 41 | 30 | |
| Iinattiniemi et al52 | III | 69.2 | Retro (11) | Any fall | 88 (2) | 273 | 282 | Any | 118 | 187 | χ2 P = .02 |
43 (37-49) | 66 (60-72) | 1.3 (1.0-1.6) | 0.9 (0.8-1.0) | 36 | 28 | |
| Summary: Posttest probability of falling if using any psychoactive medication | 3709 | 8508 | Any | 750 | 7269 | NA | 22 (19-22) | 85 (85-86) | 1.4 (1.3-1.5) | 0.9 (0.9-1.0) | 38 | 26 | ||||||
| Summary: Posttest probability of falling if using any psychoactive medication | 3709 | 8508 | Any | 750 | 7269 | NA | 22 (19-22) | 85 (85-86) | 1.4 (1.3-1.5) | 0.9 (0.9-1.0) | 38 | 26 | ||||||
Abbreviations: AD, use of any assistive device; ADL, activities of daily living; ANOVA, analysis of variance; AUC, area under the curve; CI95, 95% confidence interval; Depend, dependence; F, faller/persons who fell; Fall inj, fall with injury; HHW, heavy house work; IADL, instrumental activities of daily living; LA, less active; IRR, Incident Rate Ratio; M, men in the sample; MA, more active; −, negative; +, positive; NA, not applicable; NF, nonfaller/persons who did not fall; NR, not reported; OR, odds ratio; Pro, prospective; QUADAS, Quality Assessment Tool for Diagnostic Accuracy Studies; R, rural; Retro, retrospective; ROC, receiver operating characteristic curve; SD, standard deviation; Sn, sensitivity; Sp, specificity; U, urban; W, women in the sample.
aPosttest probabilities are based on an assumption of a 30% pretest probability for future falls.
Table 3. Summary of Findings for Determining Risk of Falls Using Self-Report Measures, Grouped by Construct Being Measureda.
| Self-Report Measure | Author | Level | QUADAS Score | Study Type, mo | Fall Defined | Age (SD) | Fallers, N | Nonfallers, N | Cut Point | Fallers With +Test | Nongallers With −Test | Difference P | Sn (CI95), % | Sp (CI95), % | +LR (CI95) | −LR (CI95) | Posttest Probability, % |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| If +Test | If −Test | |||||||||||||||||
| Measures of balance confidence and fear of falling | ||||||||||||||||||
| Activity-Specific Balance Confidence Scale 0%-100% Low: less confidence |
Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | <60 | 12 | 71 | NR | 35 (20-53) | 88 (78-94) | 2.9 (1.4-6.0) | 0.7 (0.6-1.0) | 55 | 23 |
| Balance Self-Perception Test Ordinal 0-60 points Low: less confidence |
Shumway-Cook et al44 | III | 76.9 | Retro (6) | ≥2 falls | F: 77.6 (7.8) NF: 74.6 (5.4) |
22 | 22 | ≤50 | 16 | 18 |
t test P = .01 |
73 (50-89) | 82 (60-95) | 4.0 (1.6-10) | 0.3 (0.2-0.7) | 63 | 11 |
| Falls Efficacy Scale International Ordinal 16-64 points High: more concern about falling |
Delbaere et al68 | I | 92.3 | Pro (12) | ≥2 falls | 77.9 (4.6) | 166 | 334 | >21 | 103 | 181 | OR = 1.3 P = .01 |
62 (54-69) | 54 (49-60) | 1.4 (1.2-1.6) | 0.7 (0.6-0.9) | 38 | 23 |
| Kwan et al30 | I | 84.6 | Pro (24) | Fall inj/≥2 falls | 74.9 (6.4) | 86 | 174 | ≥24 | 64 | 127 | NR | 74 (64-83) | 73 (66-79) | 2.8 (2.1-3.6) | 0.4 (0.2-0.5) | 54 | 14 | |
| Summary: posttest probability of falling on the basis of high FES-I score | 252 | 508 | ≥24 | 167 | 308 | NA | 66 (60-72) | 60 (56-65) | 1.7 (1.0-2.4) | 0.6 (0.1-0.2) | 42 | 20 | ||||||
| Falls Efficacy Scale-Modified Ordinal 0-10 rating on 14 items, averaged High: more concern |
Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | <6 | 6 | 76 | NR | 21 (8-41) | 94 (86-98) | 3.5 (1.1-10) | 0.8 (0.7-1.0) | 60 | 26 |
| Falls Risk Assessment Questionnaire Ordinal 0-16 points High: greater risk |
Flemming36 | III | 69.2 | Pro (3) | Any fall | F: 78.7 (7.2) NF: 78.6 (7.7) |
40 | 267 | >8 | 216 | 51 |
t test P < .001 |
75 (59-87) | 81 (76-85) | 3.9 (2.9-5.3) | 0.3 (0.2-0.5) | 63 | 11 |
| Measures of activities of daily living | ||||||||||||||||||
| Barthel index Ordinal 0-20 points Low: more disability |
Stalenhoef et al37 | I | 84.6 | Pro (9) | Any fall | M: 7.2 (4.9) F: 78.5 (5.2) |
2F 46 | 192 | <19 | 22 | 180 | OR = 3.3 P < .05 |
48 (38-59) | 94 (89-97) | 7.8 (4.3-14) | 0.6 (0.5-0.7) | 77 | 20 |
| Oars ADL Scale Ordinal 0-28 points Low: more disability |
Perracini et al65 | III | 84.6 | Retro (12) | Any fall | LA-F: 86.6 MA-F: 78.5 LA-NF: 77.6 MA-NF: 75.6 |
66 | 52 | >4 | 41 | 37 |
t-test LA, P = .004 MA, P = .18 |
62 (49-74) | 71 (57-83) | 2.2 (1.4-3.4) | 0.5 (0.4-0.7) | 49 | 18 |
| Measures of cognition | ||||||||||||||||||
| MMSE Ordinal 0-30 points Low: more impairment |
Beauchet et al66 | I | 92.3 | Pro (12) | Any fall | F: 85.7 (5.2) NF: 84.4 (5.3) |
54 | 133 | <25 | 34 | 64 |
t-test P > .05 |
63 (49-76) | 52 (43-61) | 1.3 (1.0-1.7) | 0.7 (0.5-1.1) | 36 | 23 |
| Shumway-Cook et al44 | III | 76.9 | Retro (6) | Any fall | F: 77.6 (7.8) NF: 74.6 (5.4) |
22 | 33 | NR | 10 | 27 | χ2 P = .02 |
45 (24-68) | 82 (65-93) | 2.5 (1.1-6.0) | 0.7 (0.4-1.0) | 52 | 23 | |
| Summary: Posttest probability of falling on the basis of low MMSE score | 76 | 166 | <25 | 44 | 91 | NA | 58 (46-69) | 55 (47-63) | 1.3 (1.0-1.7) | 0.8 (0.6-1.0) | 36 | 26 | ||||||
| Short-Orientation Memory Concentration Test Ordinal 0-28 points High: more impairment |
Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | ≥9 | 38 | 52 | OR = 1.1 P = .72 |
33 (24-42) | 68 (57-79) | 1.0 (0.7-1.6) | 1.0 (0.8-1.2) | 30 | 30 |
| Measures of depression | ||||||||||||||||||
| Center for Epidemiologic Studies Depression Scale Ordinal 0-60 points High: more depression |
Tinetti et al32 | I | 84.6 | Pro (12) | Any Fall | 76.9 (5.3) | 546 | 557 | ≥16 | 116 | 457 | ANOVA P < .05 |
21 (18-25) | 82 (79-85) | 1.2 (0.9-1.5) | 1.0 (0.9-1.0) | 34 | 30 |
| de Rekeneire et al63 |
III | 69.2 | Retro (12) | Any fall | Range: 70-79 | 652 | 2398 | ≥16 | 41 | 2292 | χ2 P < .05 |
6 (5-8) | 96 (95-96) | 1.4 (1.0-2.0) | 1.0 (1.0-1.0) | 38 | 30 | |
| Summary: Posttest probability if CES-D indicates depression | 1198 | 2955 | ≥16 | 157 | 2749 | NA | 13 (11-15) | 93 (92-94) | 1.9 (1.5-2.3) | 0.9 (0.9-1.0) | 45 | 28 | ||||||
| Geriatric Depression Scale-15 item Ordinal 0-15 points GDS-4-item Ordinal 0-4 points |
Beauchet et al66 | I | 92.3 | Pro (12) | Any fall | F: 85.7 (5.2) NF: 84.4 (5.3) |
54 | 133 | >4 | 11 | 118 | χ2 P = .003 |
20 (11-34) | 89 (82-94) | 1.8 (0.9-3.7) | 0.9 (0.8-1.0) | 44 | 28 |
| Kwan et al30 | I | 84.6 | Pro (24) | Any fall | 74.9 (6.4) | 86 | 174 | ≥6 | 28 | 146 | IRR = 1.82 P <.05 |
33 (23-44) | 84 (78-89) | 2.0 (1.3-3.2) | 0.8 (0.7-0.9) | 46 | 26 | |
| Iinattiniemi et al52 | II | 69.2 | Pro (11) | Any fall | F: 88 (3) NF: 88 (2) |
273 | 282 | >7 | 71 | 241 | χ2 P < .01 |
26 (21-32) | 85 (81-89) | 1.8 (1.3-2.5) | 0.9 (0.8-0.9) | 44 | 28 | |
| Summary: Posttest probability of falling based on GDS-15 Score | 413 | 589 | ≥7 | 110 | 505 | NA | 27 (22-31) | 86 (83-88) | 1.9 (1.5-2.4) | 0.9 (0.8-0.9) | 45 | 28 | ||||||
| Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | ≥1 | 198 | 872 | OR = 1.5 NR |
35 (31-39) | 73 (71-75) | 1.3 (1.1-1.5) | 0.9 (0.8-1.0) | 36 | 28 | |
| Coll-Planas et al34 | I | 76.9 | Pro (12) | Any fall | 82 (NR) | 116 | 76 | ≥1 | 55 | 46 | OR = 1.5 P = .23 |
48 (38-57) | 61 (49-72) | 1.2 (0.9-1.7) | 0.9 (0.7-1.1) | 34 | 28 | |
| Summary: Posttest probability of falling based on GSD-4 Score | 679 | 1272 | ≥1 | 253 | 918 | NA | 37 (34-41) | 72 (70-75) | 1.3 (1.2-1.5) | 0.9 (0.8-0.9) | 36 | 28 | ||||||
| Measures of physical activity | ||||||||||||||||||
| Longitudinal study of Aging Physical Activity Questionnaire LASA-PAQ Ordinal 0-30 points |
Peeters et al64 | I | 92.3 | Pro (36) | ≥2 falls | F: 76.8 (6.8) NF: 74.8 (6.3) |
325 | 1004 | No HHW | 173 | 611 | χ2 P < .05 |
63 (48-59) | 61 (58-64) | 1.4 (1.2-1.6) | 0.8 (0.7-0.9) | 38 | 26 |
| Peeters et al69 | 1 | 84.6 | Pro (12) | ≥2 falls | 77.9 (7.1) | 76 | 332 | >8 | 48 | 208 | ROC AUC = .65 | 63 (51-74) | 63 (57-68) | 1.7 (1.4-2.1) | 0.6 (0.4-0.8) | 42 | 20 | |
| SF-36 Physical Activity Subscale Ordinal 0-100 points |
Bohannon et al70 | III | 90 | Retro (24) | Any fall | F: 80.8 (7.2) NF: 78 (7.75) |
29 | 29 | <72.5 | 27 | 19 |
t test P < .001 |
93 (77-99) | 66 (46-82) | 2.7 (1.6-4.5) | 0.1 (0.0-0.4) | 54 | 4 |
| Measures of caregiver concern about fall risk | ||||||||||||||||||
| Subjective risk rating for specific tasks Ordinal 0-7 points |
Hashidate et al71 | III | 77.9 | Retro (12) | Any fall | 65 and older | 17 | 13 | ≥2 | 14 | 7 | χ2 P < .05 |
82 (57-96) | 54 (25-81) | 1.8 (1.0-3.3) | 0.3 (0.1-1.0) | 44 | 11 |
| Measures of overall health status | ||||||||||||||||||
| Sickness Impact Profile (SIP-68) Ordinal High = poor health |
Stalenhoef et al37 | I | 84.6 | Pro (9) | ≥2 falls | M: 77.2 (4.9) W: 78.5 (5.2) |
46 | 192 | ≥8 | 6 | 148 | OR = 2.5 P = NR |
13 (5-26) | 77 (70-83) | 0.6 (0.3-1.3) | 1.1 (1.0-1.3) | 20 | 3.2 |
| Self-rated health Ordinal 0-10 points |
Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | <5 | 8 | 64 | NR | 24 (11-41) | 79 (69-87) | 1.1 (0.5-2.4) | 1.0 (0.8-1.2) | 32 | 30 |
| <8 | 21 | 31 | NR | 62 (44-78) | 38 (28-50) | 1.0 (0.7-1.4) | 1.0 (0.6-1.7) | 30 | 30 | |||||||||
Abbreviations: ADL, activities of daily living; ANOVA, analysis of variance; AUC; CES-D, Center for Epidemiological Studies Depression; CI95, 95% confidence interval; F, fallers; fall inj, fall with injury;FES-I, Falls Efficacy Scale International; GDS, Geriatric Depression Scale; HHW, heavy house work; IRR; LA, less active; LASA-PAQ, Longitudinal Study of Aging Physical Activity Questionnaire; LR, likelihood ratio; MA, more active; MMSE, Mini-Mental State Questionnaire; NA, not applicable; NF, nonfallers; NR, not reported; −, negative; OARS, Older Adults Resources and Services; OR, odds ratio; +, positive; Pro, prospective; QUADAS, Quality Assessment Tool for Diagnostic Accuracy Studies; Retro, retrospective; R, rural; ROC; SD, standard deviation; SF-36, 36-item Short Form Health Survey; Sn, sensitivity; Sp, specificity; U, urban.
aPosttest probabilities are based on an assumption of a 30% pretest probability for future falls.
Table 4. Summary of Findings for Determining Risk of Falls Using Performance-Based Functional Measuresa.
| Functional Measure | Author | Level | QUADAS Score | Study Type, mo | Fall Defined | Age Mean (SD) | Fallers, N | Nonfallers, N | Cut Point | Fallers With +Test Mean (SD) |
Nonfallers With –Test Mean (SD) |
Difference P | Sn (CI95), % | Sp (CI95), % | +LR (CI95) | −LR (CI95) | Posttest Probability | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| If +Test | If −Test | |||||||||||||||||
| Alternate Step Test Continuous, s | Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 74 | 265 | ≥10 | 51 12.2 (4.6) |
95
10.8 (23.8) |
t test P = .007 |
69 (57-79) | 64 (58-70) | 1.9 (1.5-2.4) | 0.5 (0.3-0.7) | 45 | 18 |
| BBS Ordinal 0-56 points Low score: high risk |
LeClerc et al39 | I | 76.9 | Pro (6) | ≥2 falls | F: 79.5 (6.6) NF: 79.0 (6.9) |
99 | 769 | ≤30 | 19 39.4 (8.5) |
703 ] 43.9 (8.5) |
t test P > .05 |
19 (12-28) | 91 (89-93) | 2.2 (1.4-3.6) | 0.9 (0.8-1.0) | 49 | 28 |
| Muir et al31 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | ≤50 | 43 48.9 (9.1) |
62 52.0 (6.1) |
NR | 55 (43-66) | 60 (50-69) | 1.4 (1.0-1.9) | 0.8 (0.6-1.0) | 38 | 26 | |
| O'Brien et al73 | III | 76.9 | Retro (12) | Any fall | F: 76.0 (6.7) NF: 73.8 (4.1) |
13 | 23 | ≤45 | 7 45.0 (NR) |
23 55.0 (NR) |
MW-U P < .001 |
54 (25-81) | 100 (85-100) | NA | 0.5 (0.3-0.8) | NA | 18 | |
| Shumway-Cook et al44 | III | 76.9 | Retro (6) | ≥2 falls | F: 77.6 (7.8) NF: 74.6 (5.4) |
22 | 22 | ≤49 | 17 36.6 (11.1) |
19 52.6 (3.4) |
t test P < .001 |
77 (55-92) | 86 (65-97) | 5.7 (1.9-16.6) | 0.3 (0.1-0.6) | 71 | 11 | |
| Summary: Posttest probability of falling on the basis of BBS score ≤50 | 212 | 918 | ≤50 | 86 | 807 | NA | 41 (34-47) | 88 (85-90) | 3.4 (2.6-4.3) | 0.7 (0.6-0.80) | 59 | 23 | ||||||
| BBS and history of imbalance | Shumway-Cook et al44 | III | 76.9 | Retro (6) | ≥2 falls | F: 77.6 (7.8) NF: 74.6 (5.4) |
22 | 22 | ≤42/no or <51/yes |
20 | 18 | NR | 91 (71-99) | 82 (60-95) | 5.0 (2.0-12) | 0.1 (0.0-0.4) | 68 | 4 |
| Clinical Test of Sensory Organization and Balance Foam and dome continuous, sec Less time: higher risk |
Ricci et al74 | III | 69.2 | Retro (12) | ≥2 falls | ≥2F: 74.8 (7.3) NF: 74.5 (6.4) Single fallers not reported due to no difference between NF and single fallers in 5 of 6 conditions) |
32 | 32 | EO-Firm <30 s | 1 29.7 (1.7) |
32 30.0 (0.0) |
ANOVA P = .50 |
3 (1-16) | 100 (89-100) | NA | 1.0 (0.9-1.0) | NA | 30 |
| EC-Firm A <30 s | 5 27.9 (5.4) |
30 29.7 (1.1) |
ANOVA P = .08 |
16 (5-33) | 94 (79-99) | 2.5 (0.5-12) | 0.9 (0.8-1.1) | 52 | 28 | |||||||||
| Dome-FOAM <30 s | 7 26.8 (5.0) |
30 29.2 (4.4) |
ANOVA P = .18 |
22 (9-40) | 94 (78-99) | 3.5 (0.8-16) | 0.8 (0.7-1.0) | 60 | 26 | |||||||||
| EO-FOAM <30 s | 6 26.9 (5.0) |
32 30.0 (0.0) |
ANOVA P = .04 |
19 (7-36) | 100 (89-100) | NA | 0.8 (0.7-1.0) | NA | 26 | |||||||||
| EC-FOAM <30 s | 16 21.4 (11.4) |
26 26.2 (8.4) |
ANOVA P = .02 |
50 (32-68) | 81 (64-93) | 2.7 (1.2-6.0) | 0.6 (0.4-0.9) | 54 | 20 | |||||||||
| Dome-FOAM <30 s | 13 21.1 (11.8) |
26 26.9 (7.7) |
ANOVA P = .01 |
41 (24-49) | 81 (64-93) | 2.2 (0.9-5.0) | 0.7 (0.5-1.0) | 49 | 23 | |||||||||
| Dynamic gait index Ordinal (0-24) Low scores: higher risk |
Weiss et al75 | I | 76.9 | Pro (6) | ≥2 falls | F: 77.9 (5.1) NF: 78.8 (4.4) |
12 | 59 | NR | 4 | 58 | NR | 64 (41-83) | 98 (91-100) | 3.7 (5.2-26.9) | 0.7 (0.2-0.6) | 94 | 23 |
| III | 76.9 | Retro (6) | ≥2 falls | F: 77.9 (5.1) NF: 78.8 (4.4) |
32 | 39 | NR | 12 20.7 (3.3) |
35 22.2 (1.8) |
t-test P = .15 |
38 (21-56) | 90 (76-97) | 3.7 (1.3-10.3) | 0.7 (0.5-0.9) | 61 | 23 | ||
| Shumway-Cook et al44 | III | 76.9 | Retro (6) | ≥2 falls | F: 77.6 (7.8) NF: 74.6 (5.4) |
22 | 22 | 19 | 13 15.6 (5.7) |
11 20.6 (2.9) |
t test P = .001 |
59 (36-79) | 64 (41-83) | 1.6 (0.9-3.1) | 0.6 (0.4-1.2) | 41 | 20 | |
| Herman et al54 | III | 69.2 | Retro (12) | Any fall | 76.3 (NR) | 74 | 204 | ≤19 | 66 22.5 (1.8) |
6 23.0 (1.4) |
t test P = .03 |
90 (81-96) | 3 (1-6) | 0.9 (0.9-1.0) | 3.3 (1.1-9.4) | 28 | 59 | |
| Summary: Posttest probability of recurrent falls on the basis of DGI score ≤19 | 140 | 324 | ≤19 | 95 | 111 | NA | 68 (60-76) | 34 (29-40) | 1.0 (0.9-1.2) | 0.9 (0.7-.3)) | 30 | 28 | ||||||
|
Summary: Posttest probability of recurrent falls on the basis of DGI score ≤19 (excluding Herman 2009) |
66 | 120 | ≤19 | 29 | 107 | NA | 44 (32-57) | 89 (82-94) | 4.0 (2.3-7.3) | 0.6 (0.5-0.8) | 63 | 20 | ||||||
| Fullerton Advanced Balance Scale Ordinal 0-40 | Hernandez and Rose76 | III | 84.6 | Retro (12) | ≥2 falls | 77.0 (6.5) | 59 | 133 | 25 | 43 20 (7.3) |
69 25 (6.7) |
t test P = .19 |
73 (60-84) | 52 (43-61) | 1.5 (1.2-1.9) | 0.5 (0.3-0.8) | 39 | 18 |
| 5TSTS Continuous, s |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 80 | 282 | ≥12 s | 53 14.8 (6.2) |
127 12.5 (4.8) |
t test P < .001 |
66 (55-76) | 45 (39-51) | 1.2 (1.0-1.5) | 0.8 (0.5-1.1) | 34 | 25 |
| Buatois et al57 | II | 69.2 | Pro (≥18) | ≥2 falls | 70.1 (4.4) | 96 | 903 | ≥15 s | 58 | 582 | χ2 P < .001 |
60 (50-70) | 64 (61-68) | 1.7 (1.4-2.0) | 0.6 (0.5-0.8) | 42 | 20 | |
| Buatois et al77 | II | 46.2 | Pro (18) | ≥2 falls | 70 (4) | 183 | 1775 | ≥15 s | 101 | 1146 | NR | 55 (48-63) | 65 (62-67) | 1.6 (1.4-1.8) | 0.7 (0.6-0.8) | 41 | 23 | |
| Summary: Posttest probability of falling on the basis of 5TSTS time ≥12 s | 359 | 2960 | ≥12 | 212 | 1858 | NA | 59 (54-64) | 63 (61-65) | 1.6 (1.4-1.8) | 0.7 (0.6-0.7) | 41 | 20 | ||||||
| One time sit to stand Continuous, s |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 45 | 170 | ≥1 s | 22 1.0 (0.6) |
89 1.1 (0.6) |
t test P = .25 |
49 (34-64) | 52 (45-60) | 1.0 (07-1.4) | 1.0 (0.7-1.3) | 30 | 30 |
| 30-s Sit-to-Stand Test Continuous, s |
Cho et al78 | III | 69.2 | Retro (12) | Any fall | F: 72.1 (5.9) NF: 71.7 (5.1) |
31 | 55 | 15 times | 20 | 46 |
t test P = .001 |
65 (45-81) | 84 (71-92) | 3.9 (2.0-7.6) | 0.4 (0.3-0.7) | 63 | 15 |
| Ability to sit to stand without UE use Dichotomous (able/unable) |
de Rekeneire et al63 |
III | 69.2 | Retro (12) | Any fall | Range: 70-79 | 652 | 2398 | Unable | 35 | 2333 | χ2 P = .01 |
5 (4-7) | 97 (96-98) | 2.0 (1.3-3.0) | 1.0 (0.9-1.0) | 46 | 30 |
| Stride length Continuous, cm |
Van Swearingen et al79 | III | 92.3 | Retro (12) | ≥2 falls | 75.5 (7.3) | 53 | 31 | <87 | 34 76.1 (24.2) |
24 99.8 (23.5) |
t test P < .001 |
64 (50-77) | 77 (59-90) | 2.8 (1.4-5.6) | 0.5 (0.3-0.7) | 55 | 18 |
| Functional (anterior) reach Continuous, cm or inch |
Stalenhoef et al37 | I | 84.6 | Pro (9) | ≥2 falls | M: 77.2 (4.9) W: 78.5 (5.2) | 46 | 192 | ≤15 cm ≤5.9 in |
19 | 180 | OR = 2.0 | 41 (27-57) | 94 (89-97) | 6.6 (3.5-12.6) | 0.6 (0.5-0.8) | 74 | 20 |
| O'Brien et al73 | III | 76.9 | Retro (12) | Any fall | F: 76.0 (6.7) NF: 73.8 (4.1) |
13 | 23 | <22 cm <8.7 in |
8 22.2 (5.9) |
20 27.7 (4.9) |
MW-U P < .01 |
62 (32-86) | 87 (66-97) | 4.7 (1.5-14.7) | 0.4 (0.2-0.9) | 67 | 15 | |
| Summary: Posttest probability of falling on the basis of functional reach distance <22 cm | 59 | 215 | <22 cm | 27 | 200 | NA | 55 (40-69) | 93 (89-96) | 7.9 (4.6-13) | 0.5 (0.4-0.7) | 77 | 17 | ||||||
| Maximal step length (longest trial) (% height) continuous | Lindeman et al55 | I | 92.3 | Pro (12) | Any fall | F: 68.8 (6.0) NF: 66.5 (5.8) |
30 | 26 | <0.66 | 21 0.6 (01) |
18 0.7 (0.1) |
KS P = .03 | 70 (51-85) | 69 (48-86) | 2.3 (1.2-4.2) | 0.4 (0.2-0.8) | 50 | 15 |
| Maximal step length (mean 5 trials) (% height) continuous | <0.64 | 23 0.6 (0.1) |
16 0.7 (0.1) |
KS P = .02 |
77 (58-90) | 62 (41-80) | 2.0 (1.2-3.4) | 0.4 (0.2-0.8) | 46 | 15 | ||||||||
| Minimal chair height Continuous with physiological profile assessment |
Kwan et al80 | III | 84.6 | Retro (12) | Any fall | 74.9 (6.4) | 81 | 199 | NR | 52 | 131 | Wilks lambda P <.001 |
64 (53-75) | 66 (59-72) | 1.9 (1.5-2.4) | 0.5 (0.4-0.7) | 45 | 18 |
| Modified Gait Abnormality Rating Scale Ordinal 0-21 |
Van Swearingen et al79 | III | 92.3 | Retro (12) | ≥2 falls | 75.5 (7.3) | 53 | 31 | >9 | 33 9.3 (4.9) |
27 3.6 (3.5) |
t test P < .001 | 62 (48-75) | 87 (70-96) | 4.8 (1.9-12.3) | 0.4 (0.3-0.6) | 67 | 15 |
| mGARS >9 with PPT <15 Combined | mGARS >9 and PPT <15 | 48 | 27 | NR | 91 (79-97) | 87 (70-96) | 7.0 (2.8-17.6) | 0.1 (0.1-0.3) | 75 | 4 | ||||||||
| Performance-Oriented Mobility Assessment (POMA/Tinetti) Ordinal 0-28 points |
Topper et al81 | I | 92.3 | Pro (12) | Any fall | 83 (6) | 58 | 37 | NR | 54 | 33 | KW P = .03 ROC −0.62 |
93 (83-98) | 89 (75-97) | 8.6 (3.4-21.8) | 0.1 (0.0-0.2) | 79 | 4 |
| Panzer et al56 | I | 84.6 | Pro (12) | ≥2 falls | F: 80 (6) NF: 75 (7) |
27 | 47 | <26/28 | 14 | 47 | NR | 52 (32-71) | 100 (92-100) | NA | 0.5 (0.3-0.7) | NA | 18 | |
| Tinetti et al32 | I | 84.6 | Pro (12) | Any fall | 79.6 (5.2) | 546 | 557 | <12/22 <15/28 |
252 | 384 | ANOVA P < .05 |
46 (42-50) | 69 (65-73) | 1.5 (1.3-1.7) | 0.8 (0.7-0.9) | 39 | 26 | |
| Raiche et al82 | I | 76.9 | Pro (12) | Any fall | 80.0 (4.4) | 53 | 172 | <36/40 <25/28 |
37 | 83 | NR | 70 (56-82) | 48 (41-56) | 1.4 (1.1-1.7) | 0.6 (0.4-1.0) | 38 | 20 | |
| Avdic and Pecar83 | III | 61.5 | Retro (6) | ≥2 falls | 71.7 (5.6) | 21 | 56 | <17/26 <18/28 |
20 15.8 (7.3) |
49 23.1 (5.9) |
t-test P < .01 |
95 (76-100) | 88 (76-95) | 7.6 (3.8-15.3) | 0.5 (0.1-0.4) | 77 | 18 | |
| Summary: Posttest probability of falling on the basis of POMA score <25 | 705 | 869 | <25 | 377 | 596 | NA | 53 (50-57) | 69 (65-72) | 1.7 (1.5-1.9) | 0.7 (0.6-0.7) | 42 | 23 | ||||||
| Pick up 5-lb weight test Dichotomous (able/unable) |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 80 | 282 | Unable | 9 | 262 | χ2 P = .22 |
11 (5-20) | 93 (89-96) | 1.6 (0.8-2.4) | 1.0 (0.9-1.0) | 41 | 30 |
| 7-item PPT Ordinal 0-28 |
Van Swearingen et al79 | III | 92.3 | Retro (12) | ≥2 falls | 75.5 (7.3) | 53 | 31 | <15 | 42 11.8 (4.6) |
22 17.6 (4.0) |
t test P < .001 |
79 (66-89) | 71 (52-(86) | 2.7 (1.6-4.8) | 0.3 (0.2-0.5) | 54 | 11 |
| PPT <15 and mGARS >9 | mGARS >9 PPT <15 | 48 | 27 | NR | 91 (79-97) | 87 (70-96) | 7.0 (2.8-17.6) | 0.1 (0.1-0.3) | 75 | 4 | ||||||||
| PPA Continuous (z-score) −2 to +3 points Age-referenced |
Delbaere et al84 | I | 92.3 | Pro (12) | Any fall | 77.9 (4.6) | 166 | 334 | >0.6 | 116 | 148 | OR = 1.2 P = .04 |
70 (62-77) | 44 (39-50) | 1.3 (1.1-1.4) | 0.7 (0.5-0.9) | 36 | 23 |
| Kwan et al80 | III | 84.6 | Retro (12) | Any fall | F: 68 (3) NF: 70 (5) |
81 | 199 | NR | 46 2.0 (1.2) |
113 1.7 (1.3) |
t test P < .05 |
57 (45-68) | 57 (50-64) | 1.3 (1.0-1.7) | 0.8 (0.6-1.0) | 36 | 26 | |
| Summary: Posttest probability of falling on the basis of PPA score >0.6 | 247 | 533 | >0.6 | 162 | 261 | NA | 66 (59-71) | 49 (45-53) | 1.3 (1.1-1.5) | 0.7 (0.6-0.9) | 36 | 23 | ||||||
| SSWS Continuous, m/s |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 80 | 282 | <1.0 | 40 0.94 (0.26) |
192 1.03 (0.28) |
t test P = .003 |
50 (39-61) | 68 (62-73) | 1.6 (1.2-1.2) | 0.7 (0.6-0.9) | 41 | 23 |
| Vicarro et al85 | I | 76.9 | Pro (12) | Any fall | 74 (5.7) | 161 | 264 | < 1.0 | 126 | 72 | NR | 78 (71-84) | 27 (22-33) | 1.1 (1.0-1.2) | 0.8 (0.6-1.1) | 32 | 26 | |
| < 0.6 | 36 | 244 | NR | 22 (16-30) | 92 (89-95) | 2.9 (1.8-4.9) | 0.8 (0.8-0.9) | 55 | 26 | |||||||||
| DePasquale and Toscano86 | III | 92.3 | Retro (12) | Any fall | F: 83 (5.5) NF: 78 (7.8) |
29 | 29 | <1.2 | 19 1 (0.2) |
22 1.3 (0.2) |
t test P = .001 | 67 (46-82) | 76 (56-90) | 2.7 (1.4-5.5) | 0.5 (0.3-0.8) | 54 | 18 | |
| Van Swearingen et al79 | III | 92.3 | Retro (24) | ≥2 falls | 75.5 (7.3) | 53 | 31 | <0.6 | 38 0.50 (0.24) |
23 0.74 (0.25) |
t test P < .001 |
72 (58-83) | 74 (55-88) | 2.8 (1.5-5.2) | 0.4 (0.2-0.6) | 55 | 15 | |
| Summary: Posttest probability of falling on the basis of SSWS <1.0 (excluding Vicarro <0.6 to avoid duplication of participants) | 323 | 607 | <1.0 | 223 | 317 | NA | 69 (64-74) | 52 (48-56) | 1.5 (1.3-1.6) | 0.6 (0.5-0.7) | 39 | 20 | ||||||
| Summary: Posttest probability of falling on the basis of SSWS <0.6 (based on Vicarro <0.06 and Van Swearingen) | 214 | 295 | <0.06 | 74 | 267 | NA | 35 (28-42) | 91 (87-94) | 3.6 (2.5-5.4) | 0.7 (0.7-0.8) | 61 | 23 | ||||||
| Single-limb stance Dominant limb SLS/OLS Continuous, s |
Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | <12.7 | 343 | 587 | OR = 1.5 P < .05 |
61 (57-65) | 49 (46-52) | 1.2 (1.1-1.3) | 0.8 (0.7-0.9) | 34 | 26 |
| Muir et al33 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | <10 | 58 | 48 | RR: 1.58 P = .04 |
74 (63-84) | 46 (36-56) | 1.4 (1.1-1.7) | 0.6 (0.4-0.9) | 38 | 20 | |
| Buatois et al57 | II | 69.2 | Pro (18) | ≥2 falls | 70 (4) | 96 | 903 | <5 | 16 | 815 | χ2 P < .001 |
17 (9.8-26) | 90 (88-92) | 1.7 (1.1-2.8) | 0.9 (0.8-1.0) | 42 | 28 | |
| Buatois et al73 | II | 46.2 | Pro (18) | ≥2 falls | 70 (4) | 183 | 1775 | <5 | 29 | 1594 | NR | 35 (25-46) | 90 (88-91) | 3.4 (2.5-4.7) | 0.7 (0.6-0.9) | 59 | 23 | |
| DePasquale and Toscano86 | III | 92.3 | Retro (24) | Any fall | F: 83.6 (5.6) NF: 78 (7.8) |
29 | 29 | <6.5 | 14 3.2 (3.3) |
26 10.3 (9.6) |
t test P < .001 |
48 (29-64) | 90 (73-98) | 4.7 (1.5-14.5) | 0.6 (0.4-0.8) | 67 | 20 | |
| Summary: Posttest probability of falling on the basis of SLS time <12.7 (Bonge, Muir) | 641 | 1300 | <12.7 | 401 | 635 | NA | 63 (59-66) | 49 (47-52) | 1.2 (1.1-0.3) | 0.8 (0.7-0.9) | 34 | 26 | ||||||
| Summary: Posttest probability of falling on the basis of SLS time <6.5 (Buatois, DePasquale) | 308 | 2707 | <6.5 | 59 | 2435 | NA | 19 (15-24) | 90 (89-91) | 1.9 (1.5-2.5) | 0.9 (0.9-1.0) | 45 | 28 | ||||||
| Single-limb stance Alternatives Continuous, s |
Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | <7.6 | Non Dom 259 | Non Dom 781 | OR = 1.4 NR | 46 (42-50) | 65 (63-68) | 1.3 (1.2-1.5) | 0.8 (0.8-0.9) | 36 | 26 |
| UE mvt yes | UE mvt first 5 s 285 |
UE mvt first 5 s 714 | OR = 1.5 NR | 51 (46-55) | 60 (57-63) | 1.3 (1.1-1.4) | 0.8 (0.8-0.9) | 36 | 26 | |||||||||
| Spring Scale Test Continuous % body weight |
DePasquale and Toscano86 | III | 92.3 | Retro (24) | Any fall | F: 83.5 (5.5) NF: 78.0 (7.8) |
29 | 29 | <10% | 27 7.5 (1.4) |
28 12.3 (1.7) |
t test P = .001 |
93 (77-99) | 97 (82-100) | 27 (3.9-185) | 0.1 (0.0-0.3) | 92 | 4 |
| 8-Stair ascent time Continuous, s |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 80 | 282 | ≥5 | 43 5.9 (2.7) |
163 5.5 (2.6) |
t test P = .05 |
54 (42-65) | 58 (52-64) | 1.3 (1.0-1.6) | 0.8 (0.6-1.0) | 36 | 26 |
| 8-Stair descent time Continuous, s |
50 6.6 (3.5) |
155 5.7 (3.3) |
t test P = .01 |
63 (51-73) | 55 (49-61) | 1.4 (1.1-1.7) | 0.7 (0.5-0.8) | 38 | 23 | |||||||||
| # Steps in a half turn Continuous # steps |
Tiedemann et al72 |
I | 92.3 | Pro (12) | ≥2 falls | 80.4 (4.5) | 80 | 282 | ≥4 steps | 62 | 79 |
t test P = .08 |
78 (67-86) | 28 (23-34) | 1.1 (0.9-1.2) | 0.08 (0.5-1.3) | 32 | 26 |
| Tandem stance Continuous, s |
Muir et al31 | I | 76.9 | Pro (12) | Any fall | 79.9 (4.7) | 78 | 104 | <30 | 39 | 64 | NR | 50 (38-62) | 62 (52-71) | 1.3 (0.9-1.8) | 0.8 (0.6-1.1) | 36 | 26 |
| DePasquale and Toscano86 | III | 92.3 | Retro (24) | Any fall | F: 83.5 (5.5) NF: 78 (7.8) |
29 | 29 | <22 | 21 12.7 (10.8) |
22 23.9 (9.9) |
t test P = .001 | 72 (53-87) | 76 (56-90) | 3.0 (1.5-5.9) | 0.4 (0.2-0.7) | 56 | 15 | |
| Summary: Posttest probability of falling on the basis of tandem stance time | 107 | 133 | <30 | 60 | 86 | NA | 56 (46-66) | 65 (56-73) | 1.6 (1.2-2.1) | 0.7 (0.5-0.9) | 41 | 23 | ||||||
| Tandem walk (able/unable) | Sai et al42 | I | 92.3 | Pro (12) | Any fall | 76.7 (6.1) | 94 | 42 | Unable | 91 | 11 | NR | 96 (90-99) | 26 (14-42) | 1.3 (1.1-1.6) | 0.2 (0.1-0.5) | 36 | 8 |
| TUG Continuous, s Longer times: higher risk |
Beauchet et al66 | I | 92.3 | Pro (12) | Any Fall | 84.8 (5.2) | 54 | 133 | ≥20 | 44 27 (8.7) |
49 23 (7.9) |
χ2 P = .02 | 82 (69-91) | 37 (29-46) | 1.3 (1.1-1.6) | 0.5 (0.3-0.9) | 36 | 18 |
| Bongue et al48 | I | 84.6 | Pro (12) | Any fall | 70.7 (4.6) | 563 | 1196 | ≥11 | 193 | 894 | OR = 1.5 P < .05 |
34 (30-38) | 75 (72-77) | 1.4 (1.2-1.6) | 0.9 (0.8-0.9) | 38 | 28 | |
| Buatois et al57 | II | 69.2 | Pro (≥18) | ≥2 falls | 70.1 (4.4) | 96 | 903 | ≥12 | 12 | 836 | χ2 P < .001 | 13 (7-21) | 93 (91-94) | 1.7 (1.0-3.0) | 0.9 (0.9-1.0) | 42 | 28 | |
| Buatois et al77 | II | 46.2 | Pro (18) | ≥2 falls | 70 (4) | 183 | 1775 | ≥12 | 25 | 1650 | χ2 P < .05 | 15 (10-21) | 93 (92-94) | 2.1 (1.4-3.1) | 0.9 (0.9-10) | 47 | 28 | |
| LeClerc et al39 | II | 76.9 | Pro (6) | ≥2 falls | 79.5 (6.9) | 99 | 769 | ≥30 | 22 27.6 (17.2) |
631 23.5 (16.9) |
t test P < .05 | 25 (17-35) | 82 (80-85) | 1.4 (1.0-2.0) | 0.9 (0.8-1.1) | 38 | 28 | |
| DePasquale and Toscan86 | III | 92.3 | Retro (24) | Any fall | F: 83.5 (5.5) NF: 78.0 (7.8) |
29 | 29 | ≥7.4 | 23 9.2 (1.3) |
27 7.0 (0.9) |
t test P = .001 |
79 (60-92) | 93 (77-99) | 11.5 (2.0-44.4) | 0.2 (0.1-0.5) | 83 | 8 | |
| Payne et al41 | III | 92.3 | Retro (12) | Any fall | R: 75.5 (7.7) U: 76.0 (7.3) |
34 | 81 | >15 | 12 | 69 | NR | 35 (20-54) | 85 (76-92) | 2.4 (1.2-4.8) | 0.8 (0.6-1.0 | 51 | 26 | |
| Greany and DiFAbio87 | III | 84.6 | Retro (12) | Any fall | 82.6 (5.5) | 12 | 21 | ≥13.5 | 10 14.9 (3.1) |
16 12.5 (2.4) |
ANOVA P < .05 |
83 (52-98) | 76 (53-92) | 3.5 (1.6-7.8) | 0.2 (0.1-0.8) | 60 | 8 | |
| Huo88 | III | 84.6 | Retro (12) | Any fall | 66.3 (5.2) | 24 | 77 | ≥8 | 20 10.5 (2.9) |
47 8.3 (2.5) |
t test P < .01 | 83 (63-95) | 61 (49-72) | 2.1 (1.5-3.0) | 0.3 (0.1-0.7) | 47 | 11 | |
| Shumway-Cook et al47 | III | 84.6 | Retro (6) | ≥2 falls | F: 86.2 (6.4) NF: 78.4 (5.8) |
15 | 15 | >13.5 | 13 22.2 (9.3) |
13 8.4 (1.7) |
MANOVA P < .001 |
87 (60-98) | 87 (60-98) | 6.5 (1.8-24.0) | 0.2 (1.8-24.0) | 74 | 8 | |
| O'Brien et al73 | III | 76.9 | Retro (12) | Any fall | F: 76.0 (6.7) NF: 73.8 (4.1) |
13 | 23 | ≥20 | 8 21.5 (11.3) |
23 11.3 (2.4) |
MW-U P < .001 |
63 (32-86) | 100 (85-100) | NA | 0.4 (0.2-0.8) | NA | 15 | |
| Vicarro et al85 | III | 76.9 | Retro (12) | Any fall | 74 (5.6) | 161 | 264 | ≥15 | 42 | 242 | NR | 26 (19-34) | 92 (88-95) | 3.1 (1.9-5.0) | 0.8 (0.7-0.9) | 57 | 26 | |
| Summary: Posttest probability of falling if TUG time >0.74 s (based on DePasquale, Huo) | 53 | 106 | >7.4 | 43 | 32 | NA | 56 (46-66) | 65 (56-73) | 1.6 (1.2-1.2) | 0.7 (0.5-0.9) | 41 | 23 | ||||||
| Summary: Posttest probability of falling if TUG time ≥12 s (excluding DePasquale, Huo) | 1230 | 5180 | >12 | 381 | 4465 | NA | 31 (28-34) | 85 (84-86) | 2.1 (1.9-2.4) | 0.8 (0.8-0.8) | 47 | 25 | ||||||
| TUG Dual task |
Shumway-Cook et al47 | III | 84.6 | Retro (6) | ≥2 falls | F: 86.2 (6.4) NF: 78.4 (5.8) | 15 | 15 | DT-C >13.5 | 12 27.7 (11.6) |
14 9.7 (2.3) |
MANOVA P < .001 | 80 (52-96) | 93 (68-100) | 12.0 (1.8-87.1) | 0.2 (0.1-0.6) | 84 | 8 |
| DT-M >13.5 | 12 27.2 (11) |
14 9.7 (1.6) |
MANOVA P < .001 |
80 (52-96) | 93 (68-100) | 12.0 (1.8-81.1) | 0.2 (0.1-0.6) | 84 | 8 | |||||||||
Abbreviations: ANOVA, analysis of variance; BBS, Berg Balance Scale; CI95, 95% confidence interval; DGI, dynamic gait index; EC, eyes closed; EO, eyes open; F, fallers; Firm, tested while standing on firm supporting surface; FOAM, tested while standing on foam surface; KS, Kolmogorov-Smirnov test; KW, Kruskal-Wallis test; LR, likelihood ratio; MANOVA, multivariate analysis of variance; M, men; mGARS, Modified Gait Abnormality Rating Scale; Mvt, movement; MW-U, Mann-Whitney U test; NA, not applicable; NF, nonfallers; Non Dom, nondominant; NR, not reported; +, positive; −, negative; OR, odds ratio; Pro, prospective; PPA, Physiological Profile Assessment; PPT, Physical Performance Test; QUADAS, Quality Assessment Tool for Diagnostic Accuracy Studies; Retro, retrospective; Sn, sensitivity; Sp, specificity; SD, standard deviation; SSWS, self-selected walking speed; 5TSTS, 5 times sit to stand; TUG, Timed Up and Go; UE, upper extremity; W, women.
aPosttest probabilities are based on an assumption of a 30% pre-test probability for future falls.
When measures were supported by more than one study, data were combined to create larger samples more likely to be representative of the overall community-dwelling older adult population. The number of fallers and nonfallers, as well as the number of participants with positive and negative findings on the test of interest, was combined across studies, and composite prevalence, Sn, Sp, LR, and PoTP values were calculated.16,17 The resulting overall values for Sn, Sp, LR, and PoTP would likely be more accurate estimates of community-dwelling older adult population's true values, as demonstrated by narrow 95% confidence intervals.16,17
RESULTS
Information necessary to calculate Sn and Sp was available for 56 of the 112 included measures (50%). There were 15 questions related to medical history questions (Table 2), 15 self-report measures (Table 3), and 26 performance-based measures (Table 4) with data either about number of fallers and nonfallers having scores above and below cut score, or Sn and Sp, such that calculation of PoTP was possible.
Posttest Probability: Medical History Questions
Information collected during the medical history interview is used to screen clients and identify areas requiring further examination.18 As seen in Table 2, no medical history questions achieved both high Sn and Sp values for fall risk, typically being more specific than sensitive. LRs of several individual studies yielded PoTP of 50% or more. These included difficulty with activities of daily living (ADL),33,34 assistive device use,30,35,42 fear of falling,35,51 and previous fall history,33,37,43,48,49,52,54,55,57,59 The combined summary calculations, however, demonstrated small to moderate LRs and small change in PoTP. The medical history questions providing the largest increase in PoTP above PrTP of 30% included previous falls (PoTP= 44%), use of psychoactive medications (PoTP = 38%), requiring assistance for any ADL (PoTP = 38%), being fearful of falling (PoTP = 38%), and use of an ambulatory assistive device (PoTP = 36%). Five of these six questions (excluding fear of falling), when answered negatively, reduced PoTP to 26%. One study34 (Level I, prospective, n = 192) suggested that any reported difficulty with transfers (PoTP = 78%) or stairs (PoTP = 69%) should trigger further evaluation. Although less powerful, self-reported difficulty with walking might indicate possibility of future falls (PoTP = 41%).40,50 Although the literature suggests that advancing age (>80 years),37–41 poor self-reported health,30,31,52 and frequent alcohol consumption39,40,41,43,46,48,49 are risk factors for falls, these conclusions were not supported by summary PoTP values for either positive or negative test results. Evidence about polypharmacy was inconsistent across studies.
Posttest Probability: Self-Report Measures
Self-report measures, in the form of questionnaires, are often used to collect data before physical therapy examination.18 Some of these measures demonstrate clinical utility as fall risk tools (Table 3).
Positive test results for 4 ordinal measures of balance confidence/fear of falling substantially increased PoTP. Although data about the Falls Risk Assessment Questionnaire36 (>8 of 16 points; PoTP = 63%), the Balance Self-Perception Test44 (<50 of 60 points; PoTP = 63%), and the Activities Specific Balance Confidence Test41 (<90 of 100%; PoTP = 59%) look promising, results were based on a single study with small sample sizes. The Falls Efficacy Scale International (≥24; PoTP = 42%) is supported by 2 Level I prospective studies with moderate sample sizes,30,68 and may be more trustworthy.
Both positive and negative test results on ordinal measures of ADL appear to be informative. Scoring 19 points or less on the Barthel index resulted in a PoTP of 77%, whereas scoring 20 points or more resulted in a PoTP of 20% for multiple falls.37 This was derived from a single study with moderate sample size (n = 242). The Older Adults Resources and Services (OARS) ADL scale65 produced similar results. It should be noted that the OARS scale requires specialized training and more time to administer than the Barthel index.
Cognitive dysfunction, as measured by the Mini-Mental State Evaluation (MMSE) score less than 25, appears to shift PoTP slightly (38% if positive, 23% if negative) on the basis of 1 Level I66 and 1 Level III44 study, both with small sample sizes. Because cognitive dysfunction was one of the exclusion criteria for the review, the value of the MMSE as a fall risk tool may have been underestimated.
Two of 3 ordinal measures of depression appear to have potential to indicate risk of falling. Both the Geriatric Depression Scale-15 (GDS-15) score less than 6 (supported by 2 Level I30,66 and 1 Level II52 prospective studies) and the Center for Epidemiological Studies Depression (CES-D) score 16 or more32,63 yielded a PoTP of 45% if positive, and a PoTP of 28% if negative. The GDS-15 has fewer items and requires less time to complete. Although shorter, the GDS-434,48 was not as useful (PoTP = 36%) as the 15-item version.
Self-report measures of physical activity may also have clinical utility for fall risk assessment. A Level I study64 with moderate sample size suggests that the Longitudinal Study of Aging Physical Activity Questionnaire (LASA-PAQ) score of more than 8 may be useful for identifying those at risk for multiple falls (PoTP = 46% if positive, PoTP = 20% if negative). A single Level III study70 with small sample (n = 29) suggests that the Medical Outcome Short Form Health Survey (SF-36) Physical Activity Subscale score of less than 72.5 may be useful (PoTP = 54% if positive, PoTP = 20% if negative). Measures of caregiver concern71 and of overall health status41 were cited in single studies with small to moderate sample sizes. Neither demonstrated ability to identify fall risk.
Posttest Probability: Performance-Based Measures
Of the 28 performance-based measures included in the review, 17 were supported by a single study, 4 by 2 studies, and 7 by 3 or more studies (see Table 4). For most, Sp values were much higher than Sn values, indicating greater usefulness for ruling in risk of future falls than ruling them out. Although some PoTP values for the 20 measures evaluated by 1 or 2 studies looked promising, sample sizes tended to be small and confidence intervals for Sn, Sp, and LR values large. These measures require further investigation before recommendations on their use for predicting falls can be made with confidence. This discussion focuses on 7 measures supported by at least 3 studies. These allowed combining sample sizes, and resulted in smaller confidence intervals.16,17
The Berg Balance Scale (BBS) increased PoTP more than any other performance measure.31,39,44,73 A cut score of 50 points provides a PoTP of 59% for those who score 50 or less (a positive test) and from a PoTP of 23% for those who score 51 or more points (a negative test). These BBS results are based on 2 Level I prospective studies31,39 and 3 Level III retrospective studies44,73 with a combined sample size of 1130 older adults.
The single-task Timed Up and Go (TUG) test 12 seconds or more had a PoTP of 47% (positive test) and a PoTP of 25% if TUG time less than 12 seconds. TUG findings are based on 2 Level I48,66 and 3 Level II39,57,77 prospective studies, and 7 Level III41,47,73,85–88 retrospective studies with a combined sample of 6410 older adults.
Single-limb stance (SLS) also altered PoTP substantially: being unable to maintain the SLS potions for at least 6.5 seconds (positive test) yielded a PoTP of 45%. Exceeding this time (negative test) yields a PoTP of 28%. SLS findings are supported by 2 Level I27,44 and 2 Level II53,73 prospective studies, as well as 1 level III82 retrospective studies with a combined sample size of 3015 older adults.
For those requiring 12 seconds or more to complete the 5 times sit-to-stand test (5TSTS) (positive test), the PoTP = 41%. For those able to complete this task in less than 12 seconds (negative test), the PoTP = 20%. These findings are derived from data in 1 Level I72 and 2 Level II57,77 prospective studies with a combined sample of 3319 participants.
The Performance-Oriented Mobility Assessment (POMA, Tinetti) includes both balance and gait subscales. Because scoring methodology differed across retrieved articles, we cautiously extrapolated values on the basis of a range of possible from 0 to 28 points to be able to do study-to-study comparison. Scoring less than 25 points (positive test) increased PoTP to 42%. Scoring more than 25 points (negative test) decreased PoTP to 23%. POMA findings are derived from 4 Level I32,56,81,82 prospective studies and 1 Level III83 retrospective study with a combined sample size of 1374 participants.
Self-selected walking speed (SSWS) less than 1.0 m/s (positive test) resulted in a PoTP of 39%. An SSWS 1.0 m/s or more (negative test) resulted in a PoTP of 20%. This is based on 2 Level I72,85 prospective studies, and 2 Level III79,86 retrospective studies with a combined sample size of 1354 participants used to calculate these values. Two of these79,85 (combined sample size 509 participants) also considered an SSWS cut score of 0.6 m/s, reporting a PoTP of 61% for those walking 0.6 m/s or less (positive test), and a PoTP of 23% for those walking more than 0.6 m/s (negative test).
Results for the dynamic gait index were difficult to interpret because 1 of the 3 retrospective studies54 had a very poor Sp, reporting 198 of 204 participants with no history of falling scoring less than 19 points as cut point, but reporting a mean (standard deviation) of 22.5 (1.8). When this study was excluded from synthesis, the ability of the dynamic gait index to predicting recurrent (≥2) falls was a PoTP of 63% for those scoring 19 or less (positive test) and a PoTP of 20% for those scoring more than 19 (negative test). This finding should be interpreted with caution, however, because the combined sample size is only 186 older adults, and the confidence intervals for Sn, Sp, and LRs are wide.
Combining Measures for Cumulative Posttest Probability
Table 5 summarizes the measures with the largest PoTP for positive test results and the smallest PoTP for negative test results, as discussed in the previous sections. The following paragraphs explain how clinicians might calculate cumulative PoTP values when more than one measure has a positive test result.
Table 5. Summary of Clinically Useful Indicators of Risk of 1 or More Future Falls Based on a PrTP of 30%a.
| Category | Measure | Cut Point | +LR | −LR | PoTP, % If +Test | PoTP, % If −Test |
|---|---|---|---|---|---|---|
| Medical history questions | Any previous falls | Yes/no | 1.8 | 0.8 | 44 | 26 |
| Psychoactive medication | Yes/no | 1.4 | 0.8 | 38 | 26 | |
| Requiring any ADL assistance | Yes/no | 1.4 | 0.8 | 38 | 26 | |
| Self-report fear of falling | Yes/no | 1.4 | 0.9 | 38 | 28 | |
| Ambulatory assistive device use | Yes/no | 1.3 | 0.9 | 36 | 26 | |
| Self-report measures | Geriatric Depression Scale-15 | <6 points | 1.9 | 0.9 | 45 | 28 |
| Falls Efficacy Scale International | >24 points | 1.7 | 0.6 | 42 | 20 | |
| Performance-based functional measures | Berg Balance Scale | <50 points | 3.4 | 0.7 | 59 | 23 |
| Timed Up and Go Test | >11 s | 2.1 | 0.8 | 47 | 25 | |
| Single-limb stance eyes open | <6.5 s | 1.9 | 0.9 | 45 | 28 | |
| Five Times Sit-to-Stand Test | >12 s | 1.6 | 0.7 | 41 | 20 | |
| Self-selected walking speed | <1.0 m/s | 1.5 | 0.6 | 39 | 20 |
Abbreviations: +LR, positive likelihood ratio; −LR, negative likelihood ratio; PoTP, posttest probability; PrTP, pretest probability; +, test positive test result; −, test negative test result.
aTo the extent that tests are independent (unrelated) the PoTP of 1 positive test can be used as a new PrTP for the next positive test, etc., to develop a cumulative individualized risk estimate. Because the degree of relationship among tests is not clearly understood at this time, this strategy may inflate the cumulative risk estimate. Online resources such as www.easycalculation.com/statistics/post-test-probability.php can assist clinicians in quickly determining cumulative PoTP risk values.
Although no single medical history question emerged as a powerful diagnostic tool for identifying older adults at risk of future falls, queries about fall history, ADL difficulty, use of an ambulatory device, concern about falling, and use of psychoactive medication, in combination, are likely useful for initial screening. Yes responses to any of these questions can be used to identify those who would most benefit from a more comprehensive risk assessment for falls.6 If these questions are conceptually independent of each other, it may be appropriate to use one question's PoTP as the next test's PrTP to develop a cumulative estimate of PoTP.16,17 Clinicians can quickly calculate cumulative PoTP with online resources such as www.medcalc.org/calc/diagnostic_test.php (Sn, Sp, and LR) and https://www.easycalculation.com/statistics/post-test-probability.php (PoTP values).
As an example, during interview an older woman reports a previous fall, sleeping pill use, needing assistance with bathing, being fearful of falling, and use of a cane for ambulation. Assuming a PrTP of 30%, her cumulative PoTP would be calculated by using the largest PoTP as the next measure's PrTP, and multiplying by the test's +LR etc. It would increase to an individual PoTP of 44% on the basis of fall history, then to a cumulative PoTP of 52% on the basis of sleeping pill use, then to a cumulative PoTP of 60% because of self-reported fear of falling, and finally to a cumulative PoTP of 68% because she uses a cane to walk. This demonstrates a 2.4-fold increased risk from the original PrTP 30% value, and would support the need for more in-depth evaluation of balance and risk of falling. Conversely, the PoTP for an individual with no previous falls (individual PoTP = 26%), without psychoactive medication (cumulative PoTP = 22%), no ADL difficulty (cumulative PoTP = 18%), no fear of falling (cumulative PoTP = 17%), and no need of assistive device (cumulative PoTP = 16%) has been reduced by half from the PrTP of 30%. Education about home safety and value of activity may be sufficient to address this person's fall risk. Because these concepts are at least somewhat related, the cumulative PoTP may overestimate risk to some degree. The “cost” of referral for in-depth evaluation, even if the PoTP is somewhat inflated, is low when considered against the potential negative consequences of a future fall event.
No single self-report measure emerged as a strong predictor of future falls; however, adding the Fall Efficacy Scale-I (FES-I) and the GDS-15 as part of intake information for community-dwelling older adults may be useful. GDS-15 scores more than 6 (+LR = 1.9, PoTP = 45%) or less than 6 points (−LR = 0.9, PoTP = 28%) and FES-I scores 24 points or more (+LR = 1.7, PoTP = 42%) or below 24 points (−LR = 0.6, PoTP = 20%) may indicate whether further assessment is warranted. The use of cumulative PoTP may be most informative: a GDS score of more than 6 (individual PoTP 45%), and an FES-I score of less than 24 points (cumulative PoTP 58%), when combined with self-reported ADL difficulty (cumulative PoTP = 66%) and need for an assistive device (cumulative PoTP = 72%) certainly increases suspicion that a future fall will occur.
Performance-based measures demonstrated a stronger ability to predict future falls than either medical history questions or self-report measures. For screening purposes (where minimal time and equipment are desirable), adding SLS and SSWS to history questions may better determine who requires further examination: persons who cannot maintain SLS for at least 6.5 seconds (individual PoTP = 45%), who walk less than 1.0 m/s (cumulative PoTP = 55%), with previous falls (cumulative PoTP = 69%), self-reported fear of falling (cumulative PoTP = 76%), and who routinely use an assistive device (cumulative PoTP = 80%) would likely benefit from more comprehensive risk assessment.
For a more detailed risk assessment, the BBS and POMA contain similar test items, but the BBS has a larger range of possible scores and a more substantial impact on PoTP; therefore, the BBS appears to be more useful than POMA in determining risk of future falls. Although the BBS, TUG, and 5TSTS all contain at least one sit-to-stand task (and therefore are not fully independent), they are not identical. Combining test results would more clearly identify those individuals most in need of intervention, despite the risk of inflated cumulative PoTP. A BBS score of 50 points or less (individual PoTP = 59%) combined with a TUG time of 12 seconds or more (cumulative PoTP = 75%) and a 5TSTS time of 12 seconds or more (cumulative PoTP = 83%) would justify initiation of a program to reduce risk. A further benefit of performance-based measures is the ability to observe potentially modifiable underlying factors during testing (eg, lower extremity muscle performance, flexibility and range of motion, and eyes open/closed balance performance) that can be addressed to reduce overall risk of falling.
DISCUSSION
Given the large numbers of tests and measures available to assess risk falling (Table 1) and that falls in later life are multifactorial, identifying those older individuals living in the community who are most likely to fall is problematic. This systematic review identified the medical history questions, self-report measures, and performance-based measures for which evidence of predictive ability is strongest. Calculation of PoTP, assuming PrTP of 30% (on the basis of epidemiologic evidence), has permitted comparison of predictive ability for 56 measures. Of these, 5 medical history questions, 2 self-report measures, and 5 functional measures are supported by 3 or more high-quality prospective and retrospective studies.
Clinicians who incorporate questions about previous falls, psychoactive medication use, need for ADL assistance, a yes response to the question “are you concerned that you might fall?” and routine use of a cane or walker as part of their screening effort and intake strategy will have greater confidence in their ability to identify those individuals in need of in-depth assessment on the basis of calculation of cumulative PoTP values. For screening purposes, measuring single-limb stance with eyes open (<6.5 seconds) and/or self-selected walking speed (<1.0 m/s) will assist clinicians identifying those community-living older adults in need of in-depth evaluation. On the basis of current best-available evidence, in-depth assessment of fall risk should include several performance-based measures: BBS Score (<50 points), Time Up and Go (> 11 seconds), and 5 times sit to stand (>12 seconds) on the basis of their individual as well as cumulative PoTP values for positive and negative tests results. The addition of the self-report measures GDS-15 and FES-I can also enhance confidence in level of risk.
Strengths/Weaknesses
To our knowledge, this is the first systematic review and meta-analysis to use PoTP values to compare measures used to evaluate risk of falling. The search strategy was designed to be as inclusive as possible; however, it is limited to articles published through mid-2013. This cut-off date was a practical one: a point at which data extraction and synthesis could commence and be completed in a timely manner. Both of these activities required much more time and energy than anticipated. There is likely additional evidence published since September 2013; updating this work would be a worthwhile project for future researchers. The lack of information about the ordering search terms in the second search is unfortunate, as it threatens replication. The inclusion of retrospective (known groups) studies may have elevated the ability of some measures to “predict” falls; retrospective studies were included because of the limited number of prospective studies (more difficult and costly to carry out) available in the literature. Variation in study quality, methods, and analysis presented a significant challenge to the synthesis process. Of note is that one of the exclusion criteria was a sample including persons with significant cognitive dysfunction; as a result, information about MMSE's value as indicator of risk may be underestimated. Although inclusion criteria required studies with samples of age 65 years or more, there may be differences in pretest probability by decade of age that we were unable to account for.
Because falls are multifactorial, it is not surprising that no single test/measure was diagnostic on its own. A more in-depth understanding of relationships between history questions (fall history, assistive device use, self-reported concern about falling, ADL difficulty, and psychoactive medications), fear of falling as measured by the FES-I, depression as measured by the GDS-15, and the 5 performance measures (BBS, TUG, SLS, 5TSTS, and SSWS) would refine the ability to use the additive strategy we discussed earlier.
Meaning of Study
Assuming a literature-based PrTP of 30%, and on the basis of our systematic review, we have identified 5 dichotomous medical history questions, 2 informative self-report measures, and 5 performance-based measures with clinical usefulness in assessing risk of falling on the basis of calculation of cumulative PoTP values (Table 5). Incorporating these measures into screening and examination of older adults, and interpreting results on the basis of cumulative PoTP values, would likely enhance identification of those who do, or do not, require specific intervention to reduce risk of falling. The findings suggest that an effective screening strategy would combine the answers to the medical history questions with the ability to maintain SLS at least 6.5 seconds and to walk at a speed of at least 1.0 m/s. Client-specific cumulative PoTP values can be calculated, and need for further risk assessment determined. Although diagnostic studies in clinical medicine seek cumulative diagnostic PoTP approaching 100%, it is unlikely that combining these clinical measures will yield such certainty. However, given the negative consequences of falling in later life, a PoTP beyond the literature-based PrTP of 30% would be welcome. Physical therapists and others using these tests will need to determine the PoTP threshold needed to trigger intervention on the basis of their clinical judgment; a PoTP of 60% to 66%, for example, would suggest an individual as having a 2 in 3 chance of a future fall.
The use of the GDS-15 and a FES-I score as part of the physical therapy examination has the potential to contribute to fall risk assessment efforts. For those requiring in-depth risk assessment, the results of this meta-analysis suggest that the BBS score 50 points or less, TUG times 12 seconds or more, and 5TSTS times 12 seconds or more are currently the most evidence-supported performance-based measures to determine individual risk of future falls.
This cumulative, evidence-based, quantitative approach to multifactorial fall risk assessment would be valuable in required documentation to explain and support recommendations for further evaluation and intervention. This approach also provides a tool for patient/family education and for communication among interdisciplinary health care teams to explain level of risk and need for intervention. Finally, as level of risk decreases after intervention, this approach may be used for evaluation of outcome of intervention.
Unanswered Questions/Future Research
Researchers concerned with risk of falling, especially those who use receiver operating characteristics and area under the curve values, should be encouraged to always report cut-points, Sn, and Sp values, if not the number of participants who are “true positives” and “true negatives” (figure 1) in their manuscripts. In this way clinicians can more easily consider PoTP as they interpret an older individual's performance. Further study of the influence of advancing age and of level of physical activity on the risk of falling is certainly warranted. Consistency in how measures are implemented and scored across studies would enhance interpretation of collective results. Many of the measures included in the evidence tables looked promising as predictors of future falls, but were based on single studies with small sample sizes. It is important to investigate the usefulness of these measures, if only to narrow the range of possible indicators of fall risk to a smaller group. There are far too many measures being used to assess risk of falling in research and clinical practice: increasing the number of prospective studies would assist in narrowing the range of possible measures.
CONCLUSIONS
This systematic review and meta-analysis using individual-measure PoTP as well as cumulative, multitest PoTP identifies measures that, at this time, appear to be most informative about interpreting test results to quantify risk of falling. Combining 5 simple medical history questions (see Table 5) with 2 quickly implemented performance-based measures (single-limb stance <6.5 seconds, and self-selected walking speed <1.0 second) may be a useful way to identify persons most in need of a more in-depth examination of balance. Combining 3 performance measures (BBS score <50 points, TUG time >11 seconds, and 5 times sit-to-stand test >12 seconds) provides not only the opportunity to identify possible modifiable risk factors to inform intervention but also the means to quantify change in risk (PoTP) after intervention. The addition of 2 self-report measures (Geriatric Depression Scale <6 points and Falls Efficacy Scale International >24 points) provides additional insight into contributors to risk of falling as part of an in-depth examination and evaluation.
ACKNOWLEDGMENTS
The GeriEDGE Team expresses gratitude to Alice Bell, PT, DPT, GCS, Mindy Oxman Renfro, PT, PhD, and Poonam Pardesanay, PT, PhD, who contributed to the GeriEDGE effort in the first year of our project.
Footnotes
This project was supported in part by a development grant from the Department of Practice, American Physical Therapy Association (APTA) ($7500) and the Academy of Geriatric Physical Therapy ($2500). Several members of the workgroup attended the APTA Workshop on Development of Evidence-Based Documents/Clinical Practice Guidelines (July 2013 and July 2014).
Portions of this work were presented at American Physical Therapy Association's Combined Sections Meeting 2014 and 2015.
The authors declare no conflicts of interest.
Robert Wellmon was the Decision Editor.
REFERENCES
- 1.Stevens JA. Falls among older adults—risk factors and prevention strategies. Falls Free: Promoting a National Falls Prevention Action Plan. Washington, DC: The National Council on the Aging; 2005. [Google Scholar]
- 2.Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2014;23(1):72–86. [DOI] [PubMed] [Google Scholar]
- 3.Allison LK, Painter JA, Emory A, et al. Participation restriction, not fear of falling, predicts actual balance and mobility abilities in rural community-dwelling older adults. J Geriatr Phys Ther. 2013;36(1):13–23. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Older Adults Falls Data & Statistics. http://www.cdc.gov/homeandrecreationalsafety/Falls/data.html. Accessed May 8, 2014
- 5.Albert SM, King J, Boudreau R, et al. Primary prevention of falls: effectiveness of a statewide program. Am J Pub Health. 2014;104(5):e77–e84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevention of Falls in Older Persons. AGS/BGS Clinical Practice Guideline. http://www.medcats.com/FALLS/frameset.htm. Accessed May 9, 2014.
- 7.Cohen RG, Nutt JG, Horak FB. Errors in postural preparation lead to increased choice reaction times for step initiation in older adults. J Gerontol Biol Sci Med Sci. 2011;66A(6):705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhital A, Pey T, Stanford MR. Visual loss and falls: a review. Eye. 2010;24(10):1437–1446. [DOI] [PubMed] [Google Scholar]
- 9.Daly RM, Rosengren BE, Alwis G, et al. Gender specific age-related changes in bone density, muscle strength and functional performance in the elderly: a-10 year prospective population-based study. BMC Geriatr. 2013;13(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mertz KJ, Lee DC, Sui X, et al. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related Falls. Am J Prev Med. 2010;39(1):15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kabeshova A, Annweiler C, Fantino B, et al. A regression tree for identifying combinations of fall risk factors associated to recurrent falling: a cross-sectional elderly population-based study. Aging Clin Exp Res. 2014;26(3):331–336 [DOI] [PubMed] [Google Scholar]
- 12.Quach L, Yang FM, Berry SD, et al. Depression, antidepressants, and falls among community-dwelling elderly people: the MOBILIZE Boston study. J Gerontol Biol Sci Med Sci. 2013;68(12):1575–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeland KN, Thompson AN, Zhao Y, et al. Medication use and associated risk of falling in a geriatric outpatient population. Ann Pharmacother. 2012;46(9):1188–1192. [DOI] [PubMed] [Google Scholar]
- 14.Letts L, Moreland J, Richardson J, et al. The physical environment as a fall risk factor in older adults: systematic review and meta-analysis of cross-sectional and cohort studies. Australian Occup Ther J. 2010;57(1):51–64. [DOI] [PubMed] [Google Scholar]
- 15.Delbaere K, Close JC, Heim J, et al. A multifactorial approach to understanding fall risk in older people. J Am Geriatr Soc. 2010;58(9):1679–1685. [DOI] [PubMed] [Google Scholar]
- 16.Strauss SE, Glasziou P, Richardson WS, Haynes RB. eds. Diagnosis and screening. Evidence-Based Medicine: How to Practice and Teach It. 4th ed. Edinburgh UK: Churchill Livingstone/Elsevier; 2011:137–167. [Google Scholar]
- 17.Mayer D. Bayes' theorem, predictive values, post-test probabilities, and interval likelihood ratios. Essential Evidence-Based Medicine. 2nd ed. New York, NY: Cambridge University Press; 2009:261–276. [Google Scholar]
- 18.American Physical Therapy Association. Guide to Physical Therapist Practice 3.0. Alexandria, VA: American Physical Therapy Association; 2014. http://guidetoptpractice.apta.org./ Accessed February 13, 2014. [Google Scholar]
- 19.Barry E, Galvin R, Keogh C, et al. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults? A systematic review and meta- analysis. BMC Geriatr. 2014;14:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neuls PD, Clark TL, Van Heuklon NC, et al. Usefulness of the Berg Balance Scale to predict falls in the elderly. J Geriatr Phys Ther 2011;34(1):3–10. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: The National Academies Press; 2011 [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Macaskill P, Gatsonis C, Deeks JJ, et al. Analyzing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C. eds. Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy, Version 1.0 The Cochrane Collaboration; 2010. http://srdta.cochrane.org/. Accessed May 15, 2013. [Google Scholar]
- 24.Murray C, Lopez A, eds. World Health Report 2002: Reducing Risks and Promoting Health Lifestyle. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 25.Center for Rehabilitation Research. Rehabilitation Measures Database. Chicago IL: Rehabilitation of Chicago; www.rehabmeasures.org. Accessed October 1, 2013. [Google Scholar]
- 26.PTNow. American Physical Therapy Association, Alexandria VA. www.ptnow.org. Accessed October 1, 2013.
- 27.Whiting P, Rutjes A, Reitsma J, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.EDGE Taskforce, Section on Research, APTA. Towards optimal practice: what can we gain from assessment of patient progress with standardized outcome measures? http://www.ptresearch.org/article/14/edge-taskforce. Accessed May 11, 2014.
- 29.Cloleman K, Norris S, Weston A, et al. NHMRC Additional Levels of Evidence and Grades for Recommendations for Developers of Guidelines. Australia: National Health & Medical Research Council; 2009. [Google Scholar]
- 30.Kwan MM, Lin SI, Close JC, Lord SR. Depressive symptoms in addition to visual impairment, reduced strength and poor balance predict falls in older Taiwanese people. Age Ageing. 2012:41(5):606–612. [DOI] [PubMed] [Google Scholar]
- 31.Muir S, Berg K, Chesworth B, et al. Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community dwelling older adults: a prospective study. J Geriatr Phys Ther. 2010:33(4):165–172. [PubMed] [Google Scholar]
- 32.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(1):1214–1221. [DOI] [PubMed] [Google Scholar]
- 33.Muir S, Berg K, Chesworth B, Klar N, Speechley M. Balance impairment as a risk factor for falls in community-dwelling older adults who are high functioning: a prospective study. Phys Ther. 2010;90(3):338–347. [DOI] [PubMed] [Google Scholar]
- 34.Coll-Planas L, Kron M, Sander S, et al. Accidental falls among community-dwelling older adults: improving the identification process of persons at risk by nursing staff. Z Gerontol Geriatr. 2006;39(4):277–282. [DOI] [PubMed] [Google Scholar]
- 35.Hellstrom K, Sandstrom M, Wagert PH, et al. Fall related self-efficacy in instrumental activities of daily living is associated with falls in older community-living people. Phys Occup Ther Geriatr. 2013;31(2):128–139. [Google Scholar]
- 36.Flemming P. Utilization of a screening tool to identify homebound older adults at risk for falls: validity and reliability. Home Health Care Serv Q. 2006;25(3–4):1–26. [DOI] [PubMed] [Google Scholar]
- 37.Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemol. 2002;55:1088–1094. [DOI] [PubMed] [Google Scholar]
- 38.Yamada M, Iscihashi N. Predicting the probability of falls in community-dwelling elderly individuals using the trail-walking test. Environ Health Prev Med. 2010:15(6):386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.LeClerc B, Begin C, Cadieux E, et al. A classification and regression tree for predicting recurrent falling among community-dwelling seniors using home-care services. Can J Public Health. 2009;100(4):263–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sohng KY, Moon JS, Song HH, et al. Risk factors for falls among community dwelling elderly in Korea. J Korean Acad Nurs. 2004;34(8):1483–1490. [DOI] [PubMed] [Google Scholar]
- 41.Payne MW, Perkin TR, Payne WL. Incidence of falls by rural elders compared with their urban counterparts. Can J Rural Med. 2003;8(1):25–32. [Google Scholar]
- 42.Sai AJ, Gallagher JC, Smith LM, Logsdon S. Fall predictors in the community dwelling elderly: a cross sectional and prospective study. J Musculoskel Neuronal Interact. 2010;10(2):142–150. [PubMed] [Google Scholar]
- 43.Brauer SG, Burn YR, Galley P. A prospective study of laboratory and clinical measures of postural stability to predict community-dwelling fallers. J Gerontol Biol Sci Med Sci. 2000;55(8):469–476. [DOI] [PubMed] [Google Scholar]
- 44.Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997:77(8):812–819. [DOI] [PubMed] [Google Scholar]
- 45.Desai A, Goodman V, Kapadia N, et al. Relationship between dynamic balance measures and functional performance in community-dwelling elderly people. Phys Ther. 2010;90(5):748–760. [DOI] [PubMed] [Google Scholar]
- 46.Huang HC. A checklist for assessing the risk of falls among the elderly. J Nurs Res. 2004;12(2):131–142. [DOI] [PubMed] [Google Scholar]
- 47.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther. 2000;80(9):896–890. [PubMed] [Google Scholar]
- 48.Bongue B, Dupre C, Beauchet O, et al. A screening tool with five risk factors was developed for fall-risk prediction in community-dwelling elderly. J Clin Epidemiol. 2011;64(10):1152–1160. [DOI] [PubMed] [Google Scholar]
- 49.Swanenburg J, de Bruin ED, Uebelhart D, Mulder T. Falls prediction in elderly people: a 1-year prospective study. Gait Posture. 2010;31(3):317–321. [DOI] [PubMed] [Google Scholar]
- 50.Srygley JM, Herman T, Giladi N, Hausdorff JM. Self-report of missteps in older adults: a valid proxy of fall risk? Arch Phys Med Rehabil. 2009;90(5):786–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keskin D, Borman P, Ersoz M, et al. The risk factors related to falling in elderly females. Geriatr Nurs. 2008;29(1):58–63. [DOI] [PubMed] [Google Scholar]
- 52.Iinattiniemi S, Jokelainen J, Luukinen H. Falls risk among a very old home dwelling population. Scan J Primary Health Care. 2009;27(1):25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aoyama M, Suzuki Y, Onishi J, Kuzuya M. Physical and functional factors in activities of daily living that predict falls in community-dwelling older women. Geriatr Gerontol Int. 2011;11(3):348–357. [DOI] [PubMed] [Google Scholar]
- 54.Herman T, Inbar-Borovsky N, Brozgol, et al. The dynamic gait index in healthy older adults; the role of stair climbing, fear of falling, and gender. Gait Posture. 2009;29(2):237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lindemann U, Lundin-Olsson L, Hauer K, et al. Maximum step length as a potential screening tool for falls in non-disabled older adults living in the community. Aging Clin Exp Res. 2008;20(5):394–399. [DOI] [PubMed] [Google Scholar]
- 56.Panzer VP, Wakefield DB, Hall CB, Wolfson LI. Mobility assessment: sensitivity and specificity of measurement sets in older adults. Arch Phys Med Rehabil. 2011;92(6):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Buatois S, Perret-Guillaume C, Gueguen R, et. el. A simple clinical scale to stratify risk of recurrent and older falls in community-dwelling adults aged 65 years. Phys Ther. 2010;90(4):550–560. [DOI] [PubMed] [Google Scholar]
- 58.Gerdhem P, Ringsberg KA, Akesson K, Obrant KJ. Clinical history and biologic age predicted falls better than objective functional tests. J Clin Epidemiol. 2005;58(3):226–232. [DOI] [PubMed] [Google Scholar]
- 59.Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) scale. J Gerontol Biol Sci Med Sci. 1998;53A(4):M287–M294. [DOI] [PubMed] [Google Scholar]
- 60.Karlsson MK, Ribom E, Nilsson JA, et al. Inferior physical performance tests in 10,998 men in the MrOS study is associated with recurrent falls. Age Ageing. 2012;41(6);740–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rosengren BE, Ribom EL, Nilsson JA, et al. Inferior physical performance test results of 10,988 men in the MrOS study is associated with high fracture risk. Age Ageing. 2012;41(3):339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stewart RB, Moore MT, May FE, et al. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992;40(12):1217–1220. [DOI] [PubMed] [Google Scholar]
- 63.deRekeneire N, Visser M, Peila R, et al. Is a fall just a fall: correlates of falling in healthy older persons: the Health, Aging, and Body Composition Study. J Am Geriatr Soc. 2003;51(6):841–846. [DOI] [PubMed] [Google Scholar]
- 64.Peeters GM, Verweij LM, van Schoor NM, et al. Which types of activities are associated with risk of recurrent falling in older persons? J Gerontol Biol Sci Med Sci. 2010;65(7):743–751. [DOI] [PubMed] [Google Scholar]
- 65.Perracini M, Teixeira LR, Ramos JL, et al. Fall-related factors among less and more active older outpatients. Rev Bras Fisoter. 2012;16(2):166–172. [DOI] [PubMed] [Google Scholar]
- 66.Beauchet O, Allali G, Anweiler C, et al. Does change in gait while counting backward predict an occurrence of a first fall in older adults? Gerontology. 2008;54(4)217–223. [DOI] [PubMed] [Google Scholar]
- 67.Peeters GM, van Schoor NM, Pluijm SM, et al. Is there a U-shaped association between physical activity and falling in older persons? Osteoporosis Int. 2010;21(7):1189–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Delbaere K, Close JC, Brodaty P, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. Br Med J. 2010;341:c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peeters GM, Pluijm SF, van Schoor NM, et al. Validation of the LASA fall risk profile for recurrent falling in older recent fallers. J Clin Epidemiol. 2010;63(11):1242–1248. [DOI] [PubMed] [Google Scholar]
- 70.Bohannon RW, DePasquale L. Physical functioning scale of the short form (SF) 36; internal consistency and validity with older adults. J Geriatr Phys Ther. 2010;33(1):16–18. [PubMed] [Google Scholar]
- 71.Hashidate H, Shimada H, Shiomi T, Sasamoto N. Usefulness of the subjective risk rating of specific tasks for falls in frail elderly people. J Phys Ther Sci. 2011;23(3):519–524. [Google Scholar]
- 72.Tiedemann A, Shimada H, Sherrington C, et al. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37(4):430–435. [DOI] [PubMed] [Google Scholar]
- 73.O'Brien K, Pickles B, Culham E. Clinical measures of balance in community-dwelling elderly female fallers and nonfallers. Physiother Can. 1998;50(3):212–217. [Google Scholar]
- 74.Ricci NA, Goncalves DF, Coimbra AM, Coimbra IB. Sensory interaction on static balance: a comparison concerning the history of falls of community-dwelling elderly. Geriatr Gerontol Int. 2009;9(2):165–171. [DOI] [PubMed] [Google Scholar]
- 75.Weiss A., Brozgol M, Dorfman M, et al. Does the evaluation of gait quality during daily life provide insight into fall risk? A novel approach using 3-day accelerometer recordings. Neurorehabil Neural Repair. 2013:27(8):742–752. [DOI] [PubMed] [Google Scholar]
- 76.Hernandez D, Rose DJ. Predicting which older adults will or will not fall using the Fullerton Advanced Balance scale. Arch Phys Med Rehabil. 2006;89(12);2309–2315. [DOI] [PubMed] [Google Scholar]
- 77.Buatois S, Manckoundia P, Gueguen R, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56(8):1575–1577. [DOI] [PubMed] [Google Scholar]
- 78.Cho KH, Bok SK, Kim YJ, Hwag SL. Effect of lower limb strength on falls and balance of the elderly. Ann Rehabil Med. 2012;36(3):386–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Van Swearingen JM, Paschal KA, Bonino P, Chen TW. Assessing recurrent fall risk of community-dwelling frail older veterans using specific tests of mobility and the physical performance test of function. J Gerontol Biol Sci Med Sci. 1998;53A(6):M457–M464. [DOI] [PubMed] [Google Scholar]
- 80.Kwan MM, Lin SI, Chen CH, et al. Minimal chair height standing ability is independently associated with falls in Taiwanese older people. Arch Phys Med Rehabil. 2011;92(7):1080–1085. [DOI] [PubMed] [Google Scholar]
- 81.Topper LK, Maki BE, Holliday PJ. Are activity-based assessments of balance and gait in the elderly predictive of risk of falling and/or type of fall? J Am Geriatr Soc. 1993;41(5);479–487. [DOI] [PubMed] [Google Scholar]
- 82.Raiche M, Herbert R, Prince F, Corriveau H. Screening older adults at risk of falling with the Tinetti balance scale. The Lancet. 2000;356(9234):1001–1002. [DOI] [PubMed] [Google Scholar]
- 83.Avdic D, Pecar D. Significance of specificity of B-POMA test and fall risk factor in the third age of life. Bos J Basic Med Sci. 2006;6(1):50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Delbaere K, Close JC, Mikolaizak AS, et al. The falls efficacy scale international (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39(2):210–216. [DOI] [PubMed] [Google Scholar]
- 85.Vicarro LJ, Perera S, Studenski SA. Is the timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc. 2011;59(5):887–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.DePasquale L, Toscano L. The spring scale test; a reliable and valid tool for explaining fall history. J Geriatr Phys Ther. 2009;32(4):159–167. [PubMed] [Google Scholar]
- 87.Greany JF, DiFAbio RP. Models to predict fall history and fall risk for community-dwelling elderly. Phys Occup Ther Geriatr. 2010;28(3):280–296. [Google Scholar]
- 88.Huo M. An approach to assessment of the fall risk for the elderly by probe reaction time during walking. J Phys Ther Sci. 2009:21(4):311–316. [Google Scholar]