Abstract
Background:
Upper extremity surgery is commonly performed in the ambulatory setting and is associated with moderate to severe postoperative pain.
Methods:
Patients scheduled for upper extremity orthopedic surgery with a peripheral nerve block were randomized to receive either an ultrasound-guided single-injection supraclavicular block or ultrasound-guided median, ulnar, and radial nerve blocks (forearm blocks) performed at the level of the mid to proximal forearm with liposomal bupivacaine (Exparel) combined with a short-acting supraclavicular block. A sham block was performed in an attempt to blind enrollees in the control group. We administered the EuroQol 5D-5L questionnaire preoperatively and on postoperative days 1-3 and considered the results the primary outcome of our investigation. Block procedure times, postanesthesia care unit (PACU) length of stay, instances of nausea/vomiting, need for narcotic administration, and patient satisfaction were also assessed.
Results:
We observed no significant differences in postoperative EuroQol scores between the 2 groups and no significant differences in patient demographics, PACU length of stay, or side effects in the PACU. In some instances, the short-acting supraclavicular block resolved in the PACU, and these patients reported higher pain scores and required titration of analgesics prior to discharge.
Conclusion:
Larger prospective studies are needed to determine the safety and efficacy of liposomal bupivacaine in patients undergoing upper extremity surgery. Liposomal bupivacaine is currently only approved for local anesthetic infiltration use.
Keywords: Anesthetics–local, brachial plexus block, nerve block, orthopedics, pain–postoperative, ulnar nerve
INTRODUCTION
Upper extremity orthopedic surgery is associated with moderate to severe postoperative pain.1,2 Because these surgeries are commonly performed as outpatient procedures, attempts to optimize analgesia and minimize opioid-related side effects are the cornerstones of postoperative patient management. Ultrasound-guided regional anesthesia techniques are safe and effective approaches to avoid a general anesthetic as well as opioid-related side effects while providing excellent postoperative analgesia.3
However, these techniques also have limitations. Single-injection brachial plexus blocks—even with current long-acting local anesthetics—are associated with a relatively short duration of analgesia (<18 hours).3 Although continuous perineural brachial plexus catheters may be placed to prolong analgesia, instances of migration, leaking, dislodgement, infection, and inappropriate quantity of drug delivery have been reported with indwelling catheters.4 Both long-acting brachial plexus single-injection and continuous catheter techniques may result in prolonged numbness or motor weakness, resulting in patient and provider dissatisfaction and injury risk to the insensate extremity.5,6
Injection of local anesthetic around the ulnar, median, and radial nerves at the level of the forearm (forearm blocks) is a safe and effective technique to achieve anesthesia or analgesia of the hand.5-8 This approach to perineural blockade has been associated with a lower incidence of upper extremity weakness compared to proximal brachial plexus blocks.5-7 The ideal regional anesthetic technique provides dense intraoperative anesthesia, postoperative analgesia, and minimization of motor block.6 Dufeu et al combined a short-acting brachial plexus block with single-injection forearm blocks using a long-lasting local anesthetic in a series of patients undergoing hand surgery.6 In their case series, the blocks were limited in duration (<12 hours), and a substantial portion of patients reported suboptimal pain control.
Liposomal bupivacaine (Exparel) is an encapsulated formulation of bupivacaine designed for slow, continuous release and prolonged analgesia.9,10 Because, at the time of this writing, it is only approved by the US Food and Drug Administration for wound infiltration, its use via another route is considered off-label and should be reserved for investigational use.9,10 We hypothesized that a forearm block performed with liposomal bupivacaine in patients undergoing orthopedic surgery would result in prolonged analgesia with minimization of motor block.
METHODS
The study protocol was reviewed and approved by the Ochsner Institutional Review Board, and written informed consent was obtained from all subjects. The trial was registered on clinicaltrials.gov (identifier NCT02058303) prior to patient enrollment.
Our goal was to compare the postoperative analgesia and health outcomes (as measured by the EuroQol 5D-5L questionnaire [used with permission of the EuroQol Group]) in patients receiving a single-injection brachial plexus supraclavicular block or a short-acting supraclavicular block plus perineural injections of liposomal bupivacaine around the median, ulnar, and radial nerves at the level of the forearm in patients undergoing hand and wrist surgery. We administered the EuroQol 5D-5L questionnaire preoperatively and on postoperative days 1-3 and considered the results the primary outcome of our investigation.
Patients scheduled for upper extremity orthopedic surgery were invited to participate in the study. Exclusion criteria included refusal, known or suspected local anesthetic allergy, preexisting neurologic deficits of the upper extremity, or daily use of opioids for >2 weeks prior to the surgical procedure. A member of the research pharmacy team randomized the patients by listing the designated group in opaque envelopes that were opened immediately prior to block placement.
The EuroQol 5D-5L was administered prior to block performance and then daily for 3 days postoperatively. The EuroQol 5D-5L is a validated and standardized questionnaire used to describe overall health status and is applicable to a wide range of patient populations.11,12 The EuroQol evaluates 5 dimensions of daily life: mobility (walking about), self-care (washing or dressing), usual activities (work, study, housework, family, or leisure activities), pain/discomfort, and anxiety/depression. The potential responses to these inquiries are “no problems,” “slight problems,” “moderate problems,” “severe problems,” and “unable” (inability to perform the desired activity) for the mobility, self-care, and usual activities dimensions; similar choices are available for the pain/discomfort and anxiety/depression dimensions. Furthermore, the EuroQol includes a self-reported global health analog score ranging from 0 (very poor health) to 100 (excellent health).
All blocks were performed in a designated block area prior to the surgery by staff anesthesiologists with expertise in ultrasound-guided regional anesthesia or fellows under their direct supervision. Block procedure time was defined as the duration of time from the initial placement of the ultrasound probe to the conclusion of the perineural injection(s). A blinded research assistant assessed sensory blockade in the various nerve distributions of the arm via pinprick at 5-, 10-, 20-, and 30-min intervals after the block procedure. A score of 2 was recorded if the patient had full sensation to pinprick, while 1 and 0 indicated decreased and absent sensation, respectively.
Control Group Procedure
Patients randomized to the control group received an ultrasound-guided supraclavicular block. After administration of intravenous sedation and skin cleansing with chlorhexidine gluconate/alcohol (ChloraPrep), an S-Nerve Ultrasound System (SonoSite) L25× 13-6 MHz probe was placed in the supraclavicular region, and a 22-gauge, 5-cm Stimuplex needle (B. Braun Medical, Inc.) was used to deposit 30 mL of 0.5% bupivacaine incrementally around targeted neural structures using an in-plane technique.
To further blind patients and the research assistant, a sham block was performed in this group. After skin cleansing and sham ultrasound imaging of the ipsilateral forearm, 3 mL of 0.9% saline was injected subcutaneously. Sham block procedure times were not included in the statistical analyses.
Liposomal Bupivacaine Group Procedure
Patients randomized to the liposomal bupivacaine group received perineural injections of 1.3% liposomal bupivacaine around the median, ulnar, and radial nerves at the level of the forearm and similarly received an ultrasound-guided supraclavicular block, but a short-acting local anesthetic (mepivacaine) was used.
After administration of intravenous sedation and skin preparation with chlorhexidine gluconate/alcohol, an S-Nerve Ultrasound System L25× 13-6 MHz probe was used to identify the median, radial, and ulnar nerves in the proximal forearm. Once the nerves were identified, a 22-gauge, 5-cm Stimuplex needle was inserted using an in-plane technique, and 5 mL of 1.3% liposomal bupivacaine was injected around each respective nerve for a total of 15 mL.
After the forearm blocks were completed, the supraclavicular region was cleansed with chlorhexidine gluconate/alcohol, and an S-Nerve Ultrasound System L25× 13-6 MHz probe was used to inject 30 mL of 1.5% mepivacaine around the targeted neural structures using a 22-gauge, 5-cm Stimuplex needle.
Intraoperative and Postoperative Care
Once transported to the operating room, patients were administered a propofol infusion for comfort and procedural sedation. Opioids, multimodal analgesic agents, or other anesthetics were not administered intraoperatively, so an inadequate block would not be masked. Instances of local anesthetic supplementation by the surgical team or conversion to general anesthesia were recorded. To minimize surgical blood loss, a padded upper extremity tourniquet was applied to the proximal arm and inflated to 250 mmHg in all of the control group patients and in all but one of the liposomal bupivacaine block group patients.
In the postanesthesia care unit (PACU), all patients were asked to rate their pain using a numerical rating scale (NRS) from 0-10, with 0 indicating no pain and 10 indicating the worst pain imaginable. The length of PACU stay and postoperative side effects were recorded.
Subjects were contacted via telephone daily for 3 days postoperatively to administer the EuroQol questionnaire and again 1 week after surgery to inquire about patient satisfaction (extremely satisfied, satisfied, neutral, dissatisfied, or very dissatisfied) as well as weakness, numbness, or tingling (symptoms suggestive of neurologic injury) in the blocked extremity.
Statistical Analysis
Categorical variables are presented as counts and percentages, with differences between the groups assessed using chi-square or Fisher exact tests. Continuous variables with skewed distributions were assessed using the Wilcoxon rank-sum test. We considered P values <0.05 statistically significant.
RESULTS
A total of 38 patients were enrolled in the study. Twenty-one patients in the control group and 16 patients in the liposomal bupivacaine group were included in the statistical analysis, and the results are shown in Tables 1-3. A 17th patient who was randomized to the liposomal bupivacaine group developed compartment syndrome postoperatively and was excluded from the analysis; this rare condition (unrelated to the study intervention) and the subsequent management are discussed elsewhere in the literature.13 No significant differences were identified in age, sex, and body mass index (Table 1).
Table 1.
Patient Characteristics
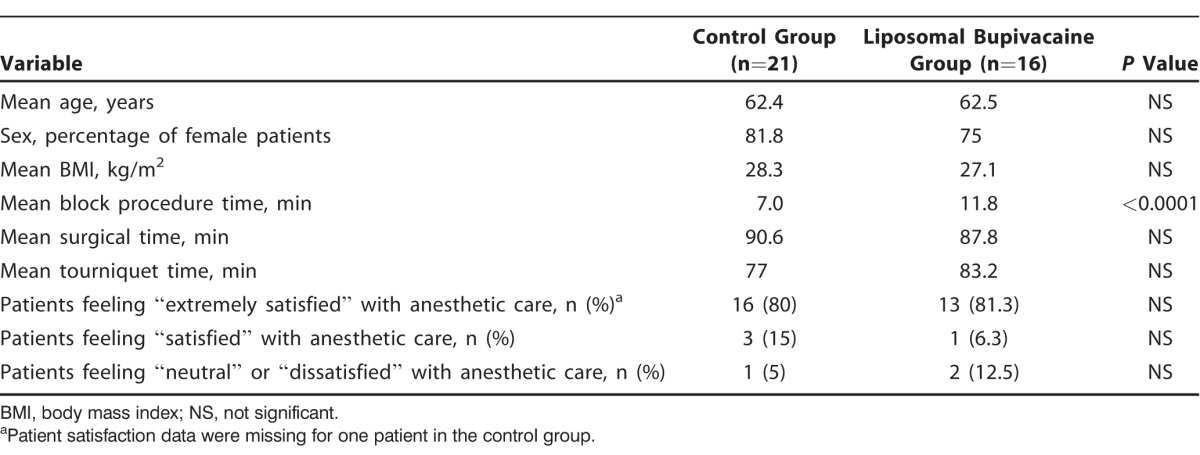
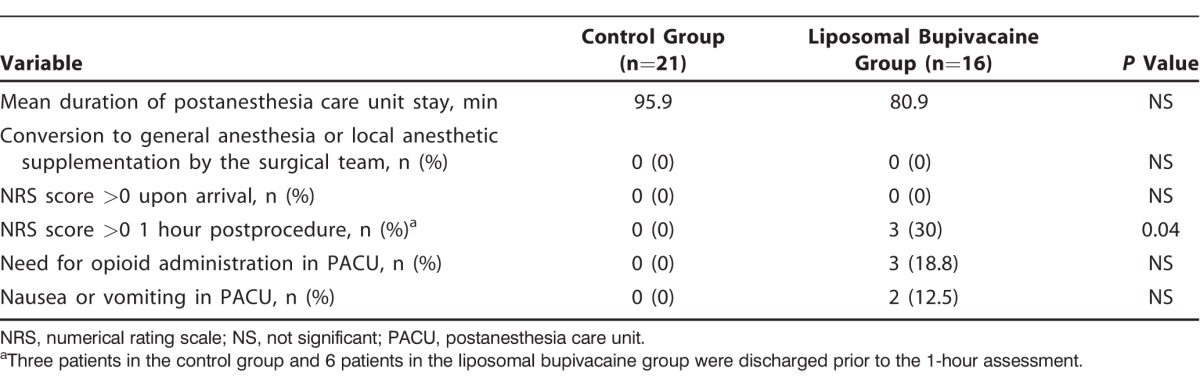
Table 3.
Secondary Outcome Measures
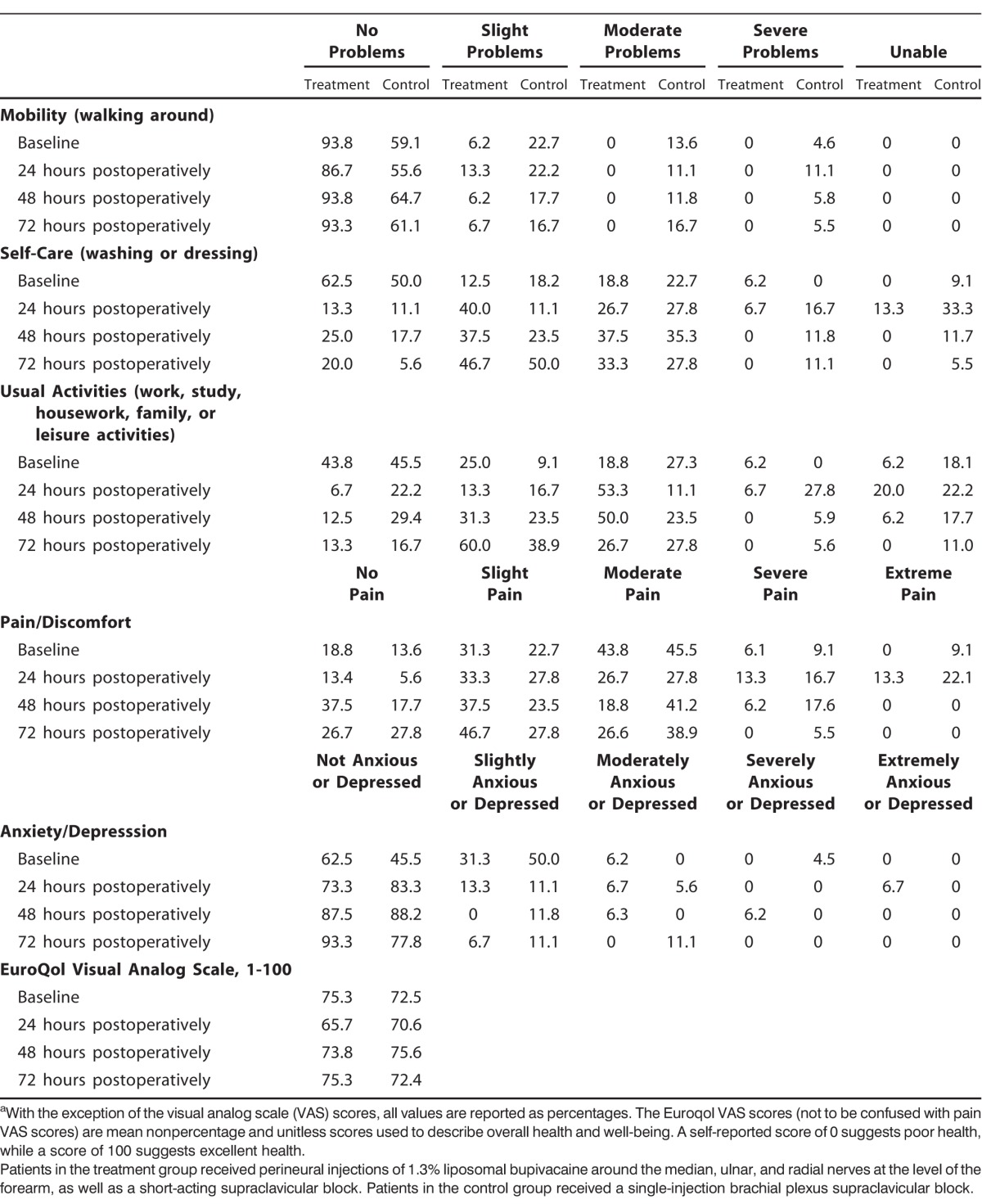
We considered the results of the EuroQol 5D-5L instrument the primary outcome of this investigation and report them in Table 2, using the percentage of patient responses for each item of the EuroQol questionnaire. No differences in the EuroQol visual analog scale scores, mobility, self-care, pain/discomfort, or anxiety/depression were identified at baseline or on postoperative days 1-3. Only 2 items reached statistical significance: a higher percentage of patients in the control group reported moderate problems with and inability to perform usual activities at baseline (both P=0.01) compared to patients in the liposomal bupivacaine group, but this difference was not statistically significant on postoperative days 1-3.
Table 2.
EuroQol 5D-5L Resultsa
Because 2 block procedures were performed, the mean block procedure time was longer in the liposomal bupivacaine group relative to the control group (11.8 min vs 7.0 min, respectively [P<0.0001]). We found no statistically significant differences between the groups in length of PACU stay, tourniquet or operative times, or patient satisfaction.
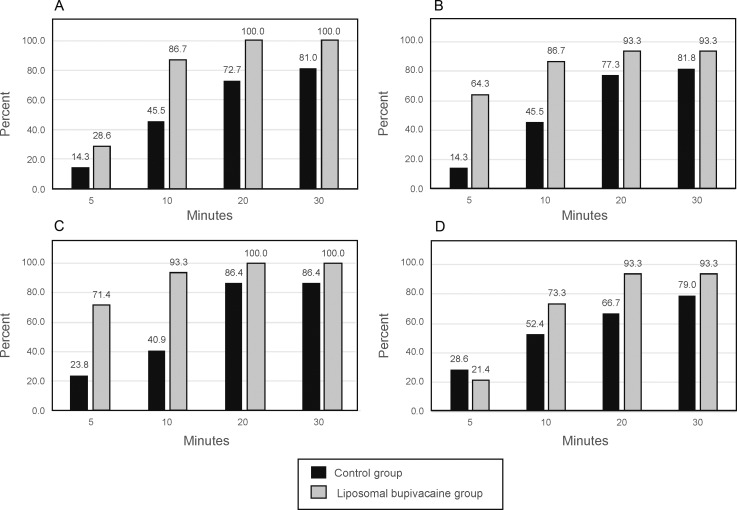
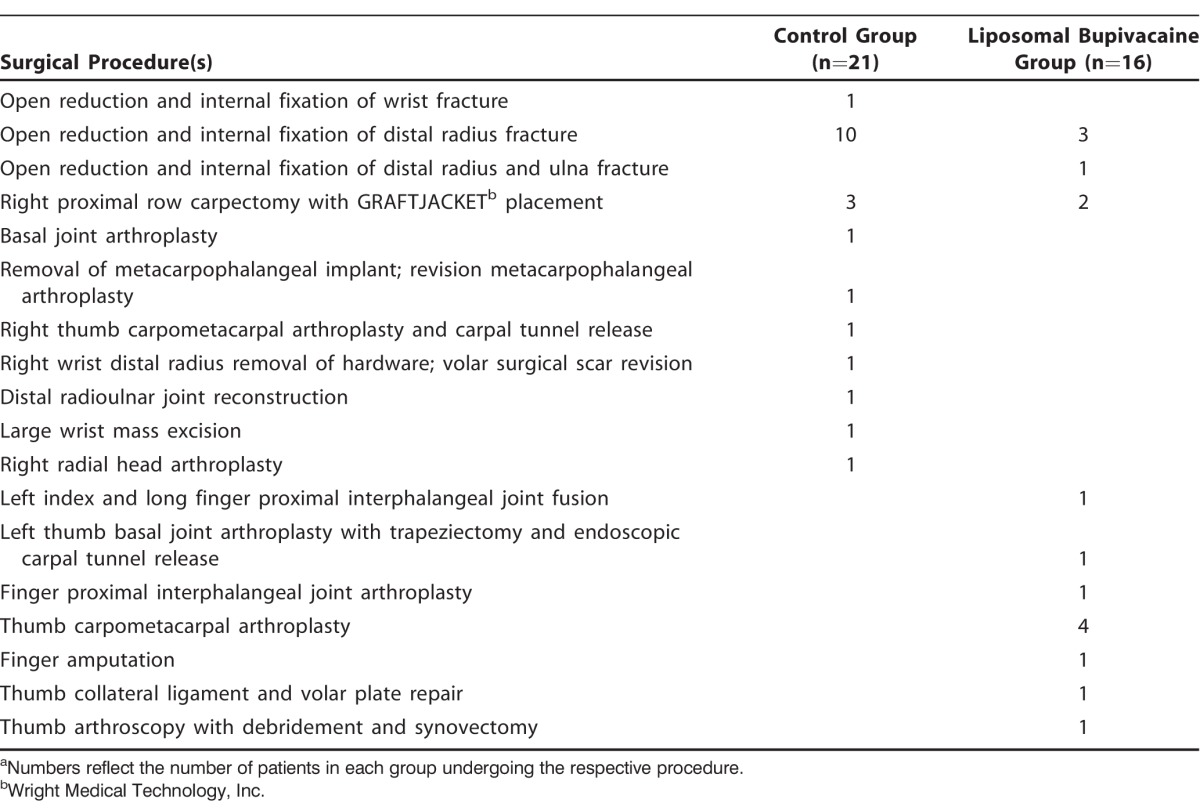
NRS scores in the PACU were similar upon arrival, although 3 patients in the liposomal bupivacaine group reported pain 1 hour after PACU arrival compared to no patients in the control group (P=0.04). Three patients in the liposomal bupivacaine group received narcotic analgesics in the PACU compared to none in the control group; this finding, however, was not statistically significant. Block onset was slightly faster in the liposomal bupivacaine group (Figure). No patient required conversion to general anesthesia, local anesthetic supplementation, or narcotic administration intraoperatively. We found no differences in postoperative nausea or vomiting between the 2 groups. Secondary outcomes and a list of surgical procedures are presented in Tables 3 and 4, respectively.
Figure.
Progression of sensory block. The graphs represent the (A) median nerve, (B) radial nerve, (C) ulnar nerve, and (D) musculocutaneous nerve of the forearm. Data are presented as the percentages of patients with an absence of sensation in the respective nerve at the specified times after the block procedure.
Table 4.
List of Surgical Proceduresa
No surgical or anesthetic complications were identified, and all patients denied evidence of neurologic injury during telephone follow-up 1 week postprocedure.
DISCUSSION
We detected no clinically significant differences in EuroQol results between patients who received a single-injection brachial plexus block and patients who received a brachial plexus block plus perineural injections of liposomal bupivacaine around the median, ulnar, and radial nerves in a population undergoing upper extremity orthopedic surgery.
This investigation has several limitations. While the EuroQol has been validated across a wide variety of patient populations,11,12 patients may report similar scores for varying reasons. For example, a patient with a liposomal bupivacaine block may report an inability to perform usual activities because of numbness in the fingers or adherence to the surgeon's postoperative recommendations to keep the hand elevated and in a sling, while another patient may report an identical score because of poorly controlled pain or opioid-related side effects, such as sedation or nausea. We found no differences between the control and liposomal bupivacaine groups in EuroQol scores in any category during the postoperative period. Because the EuroQol questionnaire provides only descriptive values regarding health status, it cannot be used to determine whether an intervention caused the measured outcomes. Furthermore, some questions may not be entirely applicable to this study population (for example, mobility—depending on weight-bearing status—may be more relevant to someone undergoing lower extremity surgery). A similar study using a larger sample size, different instrument, or a different surgical population may yield different results and should be the subject of future inquiry. Nonetheless, the ease of administration and patient comprehension made the EuroQol a desirable measurement tool.
Forearm blocks may not provide adequate coverage for all upper extremity surgeries because they have variable coverage of the thumb and do not provide adequate coverage of the wrist and forearm.6,7 Although the median, ulnar, and radial nerves were blocked with liposomal bupivacaine, the musculocutaneous nerve and medial antebrachial cutaneous nerves were not blocked. Therefore, patients who have surgery in these areas are likely to report pain after resolution of the surgical (mepivacaine) block, even with functional forearm blocks. In a recently completed prospective study, we confirmed that forearm blocks appear to best provide anesthetic and analgesic coverage for hand and non-thumb finger surgery.14 Because of the lack of coverage in the aforementioned nerve distributions, a supraclavicular block is recommended in addition to the median, ulnar, and radial nerve blocks to avoid patient discomfort or a need for conversion to general anesthesia in patients undergoing surgery in the thumb, wrist, or forearm or when prolonged upper arm tourniquet times are anticipated. As can be inferred from Table 4, most of the procedures in both groups involved areas outside of the median, radial, and ulnar nerve distributions. The incomplete coverage of the forearm blocks, coupled with the subjective and variable nature of reporting pain severity, likely accounted for the absence of differences in pain scores on the EuroQol. Despite these inherent limitations, these blocks were chosen because of their motor-sparing properties and benign side effect profiles.5-7
Our sample size may have been inadequate to identify minor differences in patient outcomes or rare adverse events. Despite the absence of adverse events in our investigation, the results may not be generalizable to other brachial plexus blocks. We do not know if the addition of a musculocutaneous nerve block in addition to the radial, ulnar, and median nerve blocks would result in improved postoperative analgesia or EuroQol scores. An alternative approach would have been to conduct a 3-arm trial using short-acting (mepivacaine) supraclavicular blocks in all groups and comparing 0.5% bupivacaine, liposomal bupivacaine, and a sham injection for radial, ulnar, and median nerve blocks for postoperative analgesia. Further research is warranted to determine the safety of forearm and proximal brachial plexus block approaches using liposomal bupivacaine.
Sunderland et al15 found that patients who received a single-injection brachial plexus block for wrist fracture surgery were 3 times more likely to have unplanned use of healthcare resources (such as urgent clinic or emergency room visits) compared to patients who underwent general anesthesia without a nerve block 48 hours postoperatively. Furthermore, 41% of these patients reported their pain to be “excruciating,” “severe,” or “extreme” during this time period. The explanation for these findings is multifactorial but may be related to relative underdosing of opioids and other analgesics, resolution of the block during evening hours resulting in unanticipated pain at home, and patient expectations.15 A theoretical benefit of the liposomal bupivacaine forearm injections is that the primary (mepivacaine) block may resolve in the PACU, allowing providers to titrate opioids and other analgesic agents (if needed) in a monitored medical setting to manage postoperative pain. Further research, particularly large-scale studies, are needed to determine if perineural injections of liposomal bupivacaine result in improved use of healthcare resources.
CONCLUSION
We were unable to detect any differences in self-reported EuroQol scores in a small group of patients undergoing painful upper extremity surgery with a single-injection brachial plexus block or short-acting single-injection brachial plexus block with perineural injections of liposomal bupivacaine around the median, ulnar, and radial nerves at the level of the forearm. Liposomal bupivacaine is only approved for surgical wound infiltration at this time.
ACKNOWLEDGMENTS
We would like to thank the Ochsner Health System Publishing Services team and Dr Lauren V. Soberón for proofreading this submission. We also thank Barbara Siede, MS, from Ochsner Health System Medical Illustration Services for her assistance in the labeling and preparation of our image.
Ochsner Health System received an unrestricted research grant from Pacira Pharmaceuticals in 2013. This grant was used for administrative costs and to purchase the study medications. Pacira Pharmaceuticals had no role in study design, statistical analysis, or manuscript preparation. Otherwise, the authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1. McGrath B, Elgendy H, Chung F, Kamming D, Curti B, King S. Thirty percent of patients have moderate to severe pain 24 hr after ambulatory surgery: a survey of 5,703 patients. Can J Anaesth. 2004. November; 51 9: 886- 891. [DOI] [PubMed] [Google Scholar]
- 2. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013. April; 118: 934- 944. doi: 10.1097/ALN.0b013e31828866b3. [DOI] [PubMed] [Google Scholar]
- 3. Hadzic A. Textbook of Regional Anesthesia and Acute Pain Management. 1st ed. New York: McGraw-Hill Professional; 2007. [Google Scholar]
- 4. Candiotti K. Liposomal bupivacaine: an innovative nonopioid local analgesic for the management of postsurgical pain. Pharmacotherapy. 2012. September; 32(9 Suppl);19S-26S. doi: 10.1002/j.1875-9114.2012.01183.x. [DOI] [PubMed] [Google Scholar]
- 5. Lam NC, Charles M, Mercer D, et al. A triple-masked, randomized controlled trial comparing ultrasound-guided brachial plexus and distal peripheral nerve block anesthesia for outpatient hand surgery. Anesthesiol Res Pract. 2014; 2014: 324083 doi: 10.1155/2014/324083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dufeu N, Marchand-Maillet F, Atchabahian A, et al. Efficacy and safety of ultrasound-guided distal blocks for analgesia without motor blockade after ambulatory hand surgery. J Hand Surg Am. 2014. April; 39 4: 737- 743. doi: 10.1016/j.jhsa.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 7. Soberón JR, Bhatt NR, Nossaman BD, Duncan SF, Patterson ME, Sisco-Wise LE. Distal peripheral nerve blockade for patients undergoing hand surgery: a pilot study. Hand (N Y). 2015. June; 10 2: 197- 204. doi: 10.1007/s11552-014-9680-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liebmann O, Price D, Mills C, et al. Feasibility of forearm ultrasonography-guided nerve blocks of the radial, ulnar, and median nerves for hand procedures in the emergency department. Ann Emerg Med. 2006. November; 48 5: 558- 562. [DOI] [PubMed] [Google Scholar]
- 9. Exparel (bupivacaine liposome injectable suspension) [package insert]. Parsippany, NJ: Pacira Pharmaceuticals, Inc 2011. [Google Scholar]
- 10. Ilfeld BM. Liposome bupivacaine in peripheral nerve blocks and epidural injections to manage postoperative pain. Expert Opin Pharmacother. 2013. December; 14 17: 2421- 2431. doi: 10.1517/14656566.2013.844791. [DOI] [PubMed] [Google Scholar]
- 11. EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990. December; 16 3: 199- 208. [DOI] [PubMed] [Google Scholar]
- 12. Brooks R. EuroQol: the current state of play. Health Policy. 1996. July; 37 1: 53- 72. [DOI] [PubMed] [Google Scholar]
- 13. Soberón JR, Jr, Sisco-Wise LE, Dunbar RM. Compartment syndrome in a patient treated with liposomal bupivacaine (Exparel). J Clin Anesth. 2016. June; 31: 1- 4. doi: 10.1016/j.jclinane.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 14. Soberón JR, Jr, Crookshank JW, 3rd, Nossaman BD, Elliott CE, Sisco-Wise LE, Duncan SF. Distal peripheral nerve blocks in the forearm as an alternative to proximal brachial plexus blockade in patients undergoing hand surgery: a prospective and randomized pilot study. J Hand Surg Am. 2016. Aug 11 doi: 10.1016/j.jhsa.2016.07.092. [DOI] [PubMed] [Google Scholar]
- 15. Sunderland S, Yarnold CH, Head SJ, et al. Regional versus general anesthesia and the incidence of unplanned health care resource utilization for postoperative pain after wrist fracture surgery: results from a retrospective quality improvement project. Reg Anesth Pain Med. 2016. Jan-Feb; 41 1: 22- 27. doi: 10.1097/AAP.0000000000000325. [DOI] [PubMed] [Google Scholar]