Abstract
Background:
Blood loss during total knee arthroplasty (TKA) may require blood transfusions that are associated with increased risk, morbidity, and cost. Multiple techniques exist to reduce blood loss in TKA, including the use of a tourniquet and tranexamic acid (TXA). While multiple studies suggest that TXA is effective in reducing blood loss, the use of a tourniquet is more controversial. We studied the combined effect of TXA with a limited-use tourniquet on blood loss and complications in the setting of primary TKA.
Methods:
A retrospective review of a prospectively gathered arthroplasty database from a single institution was performed. We compared our limited-use cohort data with the published results of randomized controlled trials evaluating the effectiveness of tourniquets used during the entire TKA procedure.
Results:
Fifty-one procedures from our institution's database met the inclusion criteria. TXA (administered in a single 15-mg/kg dose) with limited tourniquet use (a mean duration of 26.3 minutes) resulted in an average intraoperative estimated blood loss of 94.7 mL. The mean decrease in hemoglobin from the preprocedure baseline to postoperative day 1 was 2.6 ± 0.9 g/dL (P<0.001), and only 2 of the 51 procedures required a blood transfusion. When compared to recent randomized controlled trials, the 51 procedures demonstrated lower levels of blood loss, similar operative time, and no increase in morbidity or mortality.
Conclusion:
Our study results suggest that using TXA in combination with a tourniquet during the cementation portion only of a TKA provides a reasonable operative time and low intraoperative blood loss without increasing perioperative morbidity or complications.
Keywords: Arthroplasty–replacement–knee, blood transfusion, tourniquets, tranexamic acid
INTRODUCTION
Total knee arthroplasty (TKA) is among the most commonly performed elective procedures in the United States.1 Its prevalence has increased dramatically during the past several decades because of increases in obesity, the size of the aging population, and utilization.1 The desire to stay active among members of the modern population may be responsible for the rise in per capita utilization. TKA may be associated with significant blood loss for which blood transfusion might be necessary.2 Transfusion rates as high as 60% have been reported.1 Allogeneic blood transfusion, despite current testing parameters, carries significant potential risks1,3,4 and costs.1,5 Risks include mismatch attributable to clerical error, infection, and immunologic reactions caused by the transfusion or contaminants.1,3,4 Costs associated with TKA-related intraoperative blood loss and allogeneic transfusions include the costs of the blood units, of longer hospital stays, and of readmissions for transfusion-related complications.1,5
A pneumatic tourniquet is commonly used during TKA to reduce intraoperative blood loss and to improve visualization.1,2,6-8 The pneumatic tourniquet has also been shown to reduce operative time and to improve cement interdigitation.2,6-8 A 2009 survey of the members of the American Association of Hip and Knee Surgeons reported that 95% used a tourniquet during TKA.9 However, the clinical role of the tourniquet in TKA remains controversial2,8,10,11 because of the potential deleterious effects of prolonged pneumatic tourniquet use2,8,11-19 that can be devastating.1,2,8,11,12,17-32 Intraoperatively, the use of a tourniquet during trial reduction and patellofemoral tracking has been associated with an increased risk of lateral release, secondary to a tethered quadriceps mechanism.2,13-15 Postoperatively, limb pain,2 swelling,12 stiffness,8,19 delay of muscle-power recovery,12 subcutaneous limb fat necrosis,2,16 and wound hematoma leading to persistent wound drainage and subsequent increased infection risk2,31 have all been reported. Less common complications associated with prolonged pneumatic tourniquet use during TKA include nerve palsy mediated or modulated by compression neuropraxia,8,11,20,21,32,33 compartment syndrome,12,33 rhabdomyolysis,2,8,24 renal failure,8,24 direct vascular injury,11,22,26-28 deep vein thrombosis (DVT),2,8,11,25,27,30 pulmonary embolism (PE),1,8,11,23,25,29 acute pulmonary edema, and cardiac arrest immediately following tourniquet release.8,17-19 Last, prolonged tourniquet use during TKA may interfere with postoperative functional recovery and affect overall patient knee range of motion and clinical success.8,11,17-19
While some studies have shown that a tourniquet is effective in reducing intraoperative blood loss,30,34,35 others have failed to demonstrate this benefit.10,36,37
Tranexamic acid (TXA), a synthetic lysine analogue and competitive inhibitor of plasminogen at its lysine-binding site for fibrin,38,39 has been used successfully in numerous nonorthopedic surgical procedures to decrease blood loss.40-48 In the United States, initial interest in the use of TXA in the field of joint arthroplasty focused on primary and revision total hip arthroplasty46,47,49-51 because of the high potential for blood loss during these procedures. After demonstrating a significant decrease in blood loss and need for blood transfusion46,47,51 with primary and revision total hip arthroplasty procedures, TXA became commonly used in TKA.52,53
The literature is largely unclear regarding best-practice use of the pneumonic tourniquet and TXA.9,34-37,46-48,51-58 Consequently, the goal of this investigation was to determine whether the limited use of a pneumatic tourniquet in conjunction with the use of TXA would alter operative time, intraoperative blood loss, transfusion rate, and complication rates when compared with the use of a pneumatic tourniquet throughout the procedure.
METHODS
Patients
After Institutional Review Board approval was obtained, a search of the prospectively gathered arthroplasty database was conducted at the participating institution. All adult patients who underwent routine primary unilateral TKA (current procedural terminology [CPT] code 27447) by the senior author (A.D.R.) between April 30, 2013, and December 8, 2014, for osteoarthritis (OA) or rheumatoid arthritis (RA) were identified for inclusion in this retrospective cohort study. Patients who had undergone revision TKA, distal third femoral replacement TKA, or same-setting bilateral TKA; patients requiring computer assist or other electronic devices; and patients who had undergone previous intraarticular or periarticular open reduction and internal fixation were not included. Our search revealed a total of 70 patients.
Patients having preoperative gross deformities, severe contractures, or constrained TKA—a total of 21 patients—were excluded. A total of 51 knees, 29 right and 22 left, in 49 patients met the inclusion criteria. Two patients received bilateral knee arthroplasty in separate procedures.
All patients had their TKA performed by the senior author (A.D.R.) under general anesthesia and received a single dose of TXA, 15 mg/kg intravenously. All of the procedures were done through a midline skin incision and medial parapatellar arthrotomy. Tourniquet use was limited to the period of cementation. In all patients, the tourniquet was inflated after the extremity was exsanguinated, just prior to cementation, and deflated when the bone cement had cured. Intraoperative blood loss was estimated by addition of the volume of blood noted on the sponges to the volume collected in the suction canisters and subtraction of the amount of irrigation fluid used. Suction drains, cell savers, and autologous blood were not used. To further characterize postprocedural blood loss, hemoglobin levels were measured preprocedure and on postoperative day (POD) 1.
Data Collection
We individually reviewed patient medical records and operative reports. Data collected for the study included the anesthesia technique, TXA dose and route of administration, tourniquet inflation duration and pressure, operative time (from incision to completion of wound closure), intraoperative blood loss, hemoglobin levels (preoperatively and on POD 1), length of stay, and number of units of packed red blood cells transfused. All complications were noted, including surgical-site infections, delayed wound healing, readmission within 30 days for surgical complications, DVT, and PE. Patients were screened for DVT and PE only if clinically indicated.
Historical Control Selection
Electronic databases (PubMed, MEDLINE, and Embase) were searched by 2 independent researchers (Y.A.M. and A.D.R.) to identify studies published from January 2009 to June 2015. The keywords used in the search were total knee arthroplasty or total knee replacement and blood loss, tourniquet, and randomized controlled trial (RCT). Reference lists of the relevant papers were thoroughly searched for any further relevant studies. Only studies including a minimum of 25 patients in each arm were included. Eight RCTs that included the use of a tourniquet met the inclusion criteria and were included in the analysis from which root studies were reviewed and raw data were extracted.
Statistical Analysis
The statistical program SPSS v.19 (IBM) was used to analyze the data. Basic descriptive statistics are reported as means ± SD in addition to the median, minimal, and maximal values for continuous variables, and proportions and frequencies are reported for categorical variables. Paired t tests were used to examine changes in hemoglobin levels at POD 1 compared to preprocedure hemoglobin level. A P value <0.05 was used to determine statistical significance.
RESULTS
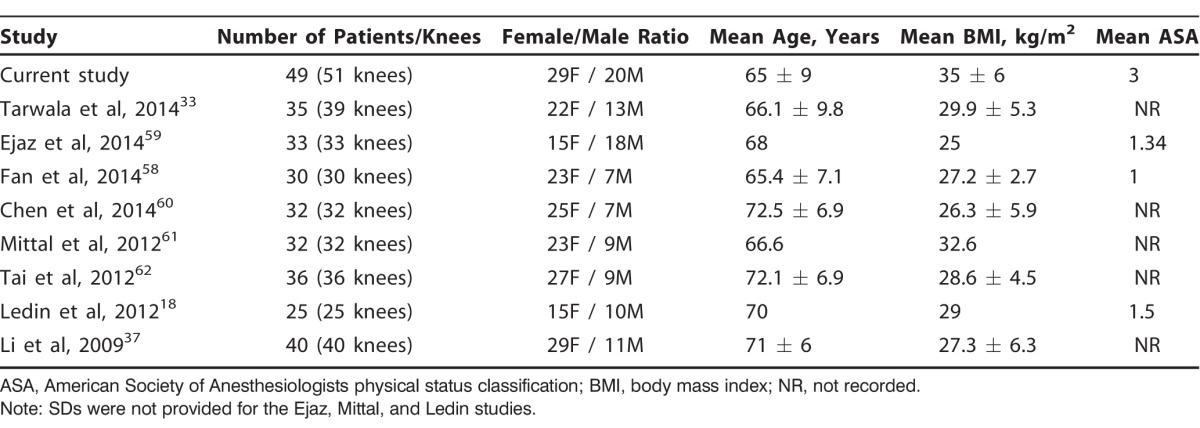
Patient demographics and comorbidities are described in Table 1. The average age of the patients at time of surgery was 65 ± 9 years (range, 50-83 years). A total of 51 procedures/knees in 49 patients (20 males and 29 females) were included in the investigation. The majority of procedures (50 of 51) were for the treatment of OA, with 1 procedure related to RA. We examined the demographics of our patient cohort in relation to published comparison studies that included patients for whom the tourniquet was inflated throughout the procedure, from incision to wound closure (Table 2).18,33,37,58-62 The patient characteristics in the published studies were comparable to the patient characteristics in our cohort.
Table 1.
Patient Demographics and Comorbidities
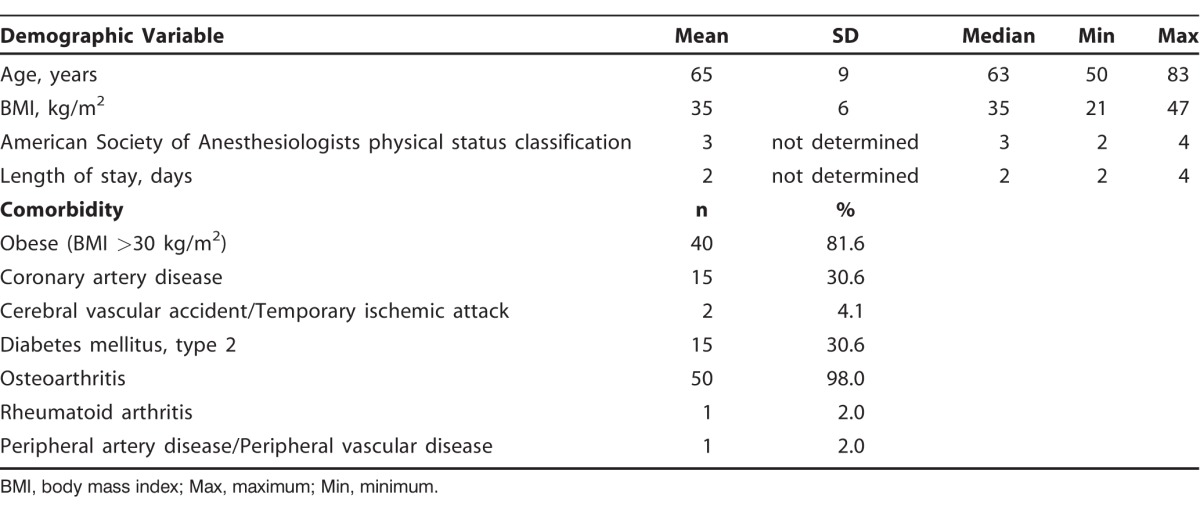
Table 2.
Demographics of Patients Receiving Limited Tourniquet Use Plus Tranexamic Acid During Total Knee Arthroplasty in Relation to Historical Comparison Studies
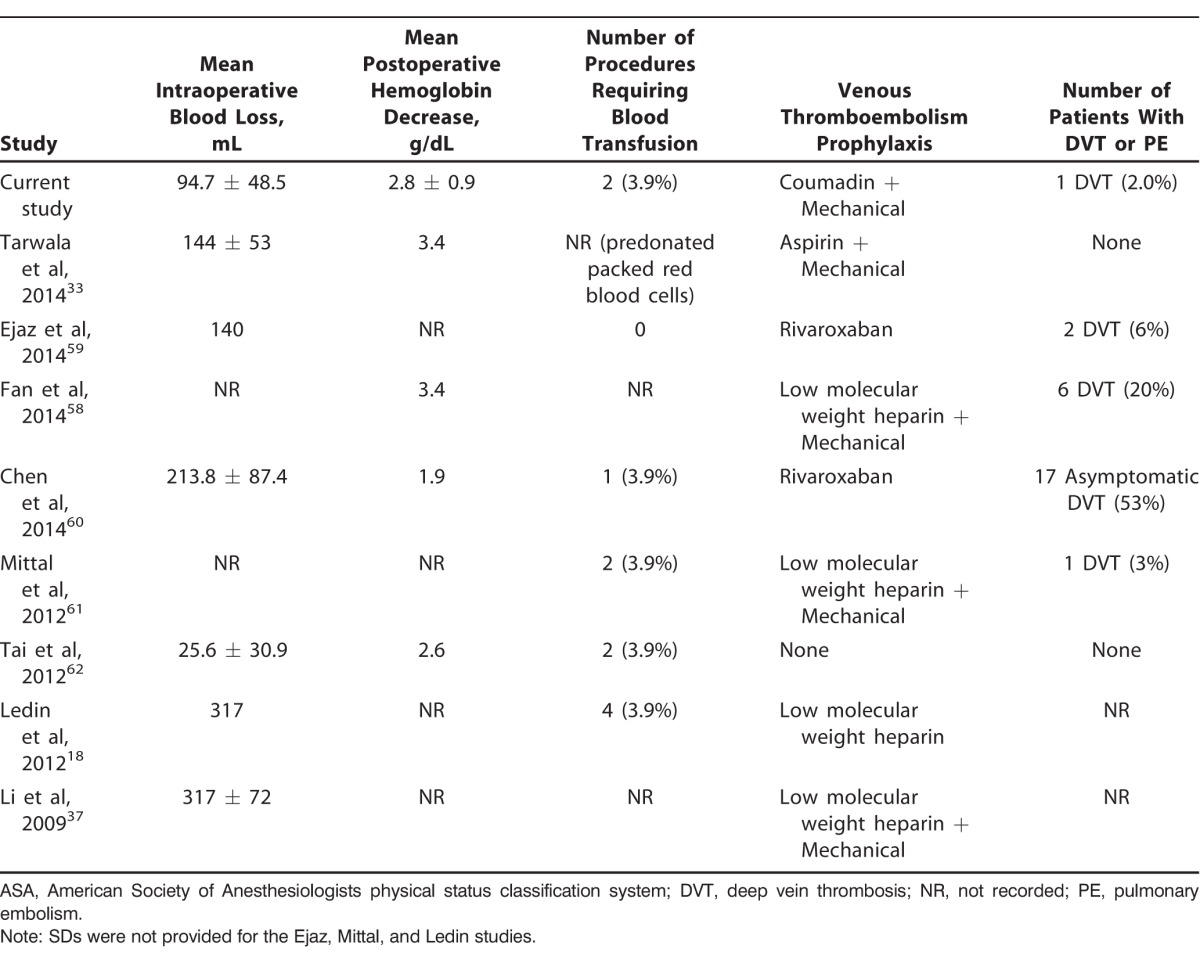
Data on the mean duration of procedure and tourniquet inflation time for our study cohort are presented in Table 3. Our operative variables and results were also comparable to published controls (Tables 4 and 5). Our mean duration of procedure was 116 minutes, which is within the range reported in the historical comparison studies (70.0-120.8 minutes). Our mean intraoperative estimated blood loss, a less precise measure, was 94.7 mL ± 48.5 mL, and this value is lower than the blood loss reported in all of the published RCTs used for comparison, except for the study published by Tai et al62 who reported a mean intraoperative blood loss of 25.6 ± 30.9 mL (Table 5).
Table 3.
Procedure Characteristics
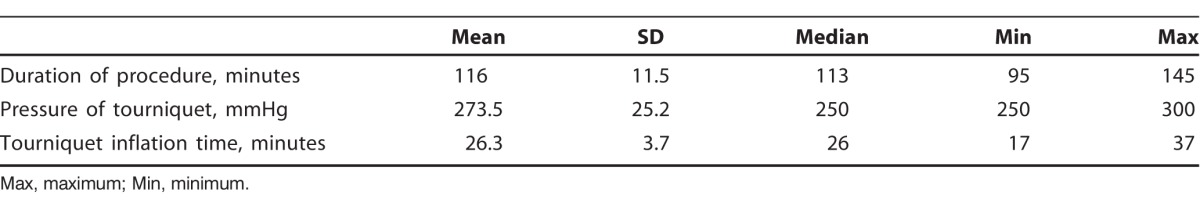
Table 4.
Procedure Characteristics in Our Study Cohort in Relation to Historical Comparison Studies
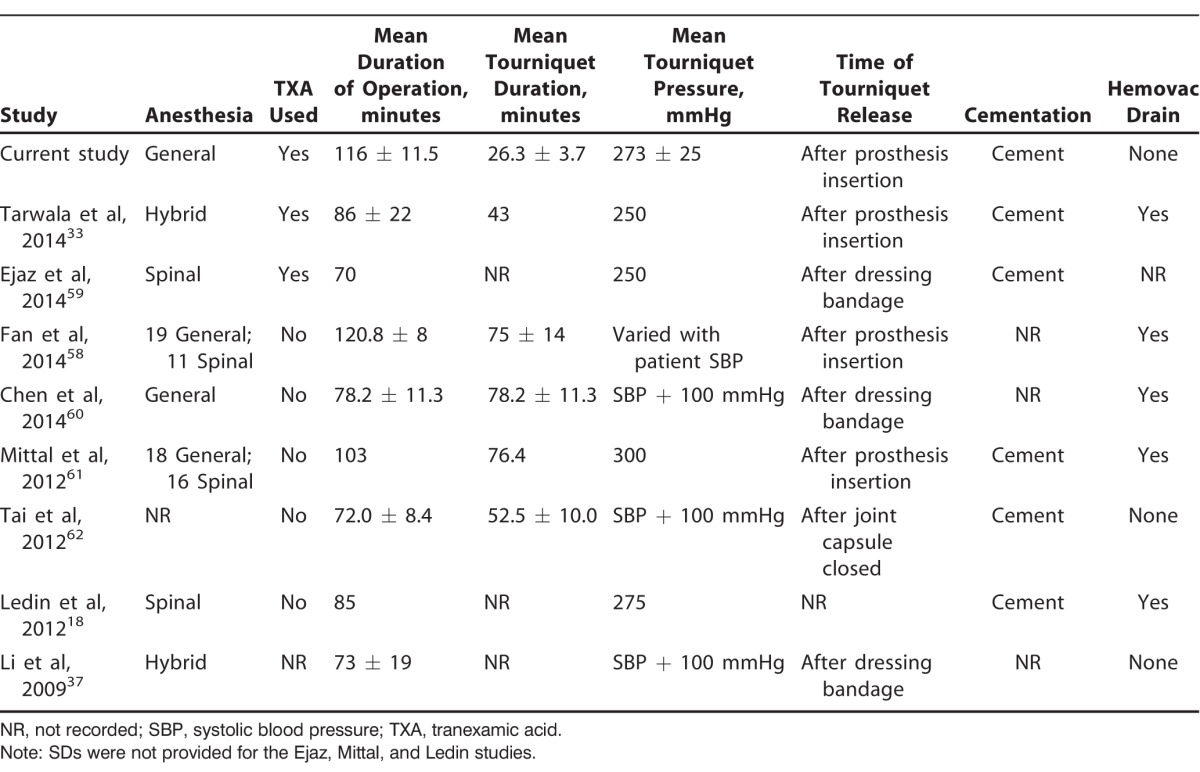
Table 5.
Complications in Our Study Cohort in Relation to Historical Comparison Studies
In our cohort, the mean decrease in hemoglobin from the preprocedure baseline to POD 1 was 2.8 g/dL ± 0.9 g/dL with hemoglobin levels at POD 1 (11.5 g/dL ± 1.4 g/dL) significantly decreased in comparison to baseline values (14.1 g/dL ± 1.2 g/dL, P<0.001) (Figure). Hemoglobin values on discharge were not significantly different than those measured on POD 1. The mean hemoglobin drop in the published comparison studies ranged from 1.9-3.4 mg/dL. This change is similar to the mean hemoglobin drop of 2.8 mg/dL noted in our study on POD 1; however, the timing of these published levels varied in some instances beyond POD 1.
Figure 1.
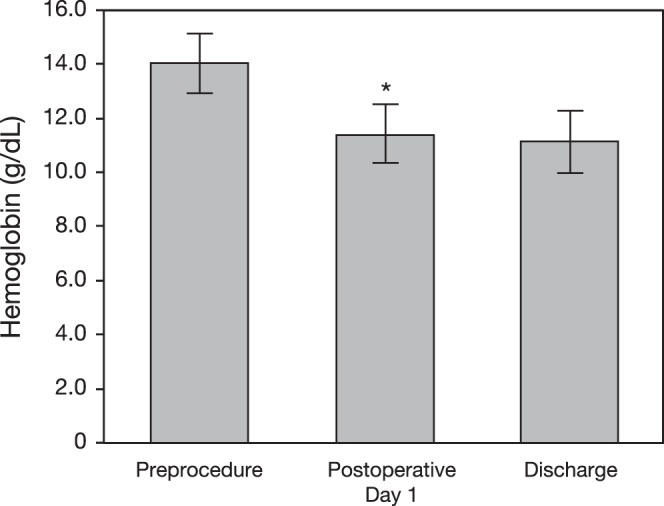
Mean hemoglobin preprocedure, on postoperative day 1, and on discharge. *The mean decrease in hemoglobin from the preprocedure baseline to postoperative day 1 was 2.6 ± 0.9 g/dL (P<0.001).
Of our 51 procedures, only 2 (3.9%) required blood transfusions during the perioperative period, with each patient receiving 2 units each. No surgical-site infections were reported in our patient cohort. One patient developed a PE after surgery. No patients required readmission for surgery-related postoperative complications or surgical revision.
DISCUSSION
The results of this investigation revealed that the use of TXA in combination with a tourniquet for only cementation provided reasonable operative time and low intraoperative blood loss without increasing perioperative morbidity or complications.
Our study findings concur with findings published by Tarwala et al33 in that the use of limited tourniquet along with TXA in the performance of TKA is as effective as using a tourniquet throughout the entire procedure as it relates to operative time, intraoperative blood loss, and need for blood transfusion. Two metaanalyses of randomized studies comparing tourniquet use throughout an entire case vs no tourniquet at all found differences only in total blood loss.2,63 More recently, 2 studies comparing the use of a tourniquet just for cementation of the implants with tourniquet use during the entire operation found no important clinical differences between the 2 methods.33,58
Our study has several limitations. First, it is a retrospective review. Second, we reviewed only 51 knee operations all performed by a single surgeon. Third, the majority of our patients were obese; therefore, our results may not be applicable to all populations. Finally, the study has no true control group to provide baseline blood loss levels for TKA without a tourniquet and without TXA.
From 1999-2009, the reported number of TKA cases performed annually in the United States doubled.64 Such an increase may be at least partially attributed to rising obesity rates, as well as to improved imaging and longer life expectancy.65,66 Increasing numbers of patients who require TKA and the high economic burden of this procedure will require techniques such as we have described for surgical and anesthetic management.67-72
CONCLUSION
Our investigation results demonstrate that using TXA in combination with a tourniquet for only cementation provides reasonable operative time and low intraoperative blood loss without increasing perioperative morbidity or complications.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, and Practice-Based Learning and Improvement.
REFERENCES
- 1. Levine BR, Haughom B, Strong B, Hellman M, Frank RM. Blood management strategies for total knee arthroplasty. J Am Acad Orthop Surg. 2014. June; 22 6: 361- 371. doi: 10.5435/JAAOS-22-06-361. [DOI] [PubMed] [Google Scholar]
- 2. Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011. July; 19 7: 1121- 1130. doi: 10.1007/s00167-010-1342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kirkley SA, Cowles J, Pellegrini VD, Harris CM, Boyd AD, Blumberg N. Blood transfusion and total joint replacement surgery: T helper 2 (TH2) cytokine secretion and clinical outcome. Transfus Med. 1998. September; 8 3: 195- 204. [DOI] [PubMed] [Google Scholar]
- 4. Klein HG. How safe is blood, really? Biologicals. 2010. January; 38 1: 100- 104. doi: 10.1016/j.biologicals.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 5. Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010. August; 113 2: 482- 495. doi: 10.1097/ALN.0b013e3181e08e97. [DOI] [PubMed] [Google Scholar]
- 6. Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2010. March; 17 2: 141- 147. doi: 10.1016/j.knee.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 7. Whitehead DJ, MacDonald SJ. TKA sans tourniquet: let it bleed: opposes. Orthopedics. 2011. September 9; 34 9: e497- e499. doi: 10.3928/01477447-20110714-44. [DOI] [PubMed] [Google Scholar]
- 8. Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014. March 6; 9 1: 13 doi: 10.1186/1749-799X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berry DJ, Bozic KJ. Current practice patterns in primary hip and knee arthroplasty among members of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010. September; 25 6 Suppl: 2- 4. doi: 10.1016/j.arth.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 10. Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg. 2001. February; 44 1: 33- 38. [PMC free article] [PubMed] [Google Scholar]
- 11. Lohmann-Jensen R, Holsgaard-Larsen A, Emmeluth C, Overgaard S, Jensen C. The efficacy of tourniquet assisted total knee arthroplasty on patient-reported and performance-based physical function: a randomized controlled trial protocol. BMC Musculoskelet Disord. 2014. March 29; 15: 110 doi: 10.1186/1471-2474-15-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wakai A, Winter DC, Street JT, Redmond PH. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001. Sep-Oct; 9: 345- 351. [DOI] [PubMed] [Google Scholar]
- 13. Komatsu T, Ishibashi Y, Otsuka H, Nagao A, Toh S. The effect of surgical approaches and tourniquet application on patellofemoral tracking in total knee arthroplasty. J Arthroplasty. 2003. April; 18 3: 308- 312. [DOI] [PubMed] [Google Scholar]
- 14. Lombardi AV, Jr, Berend KR, Mallory TH, Dodds KL, Adams JB. The relationship of lateral release and tourniquet deflation in total knee arthroplasty. J Knee Surg. 2003. October; 16 4: 209- 214. [PubMed] [Google Scholar]
- 15. Husted H. Toftgaard Jensen T. Influence of the pneumatic tourniquet on patella tracking in total knee arthroplasty: a prospective randomized study in 100 patients. J Arthroplasty. 2005. September; 20 6: 694- 697. [DOI] [PubMed] [Google Scholar]
- 16. Tamvakopoulos GS, Toms AP, Glasgow M. Subcutaneous thigh fat necrosis as a result of tourniquet control during total knee arthroplasty. Ann R Coll Surg Engl. 2005. September; 87 5: W11- W13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang FJ, Xiao Y, Liu YB, Tian X, Gao ZG. Clinical effects of applying a tourniquet in total knee arthroplasty on blood loss. Chin Med J (Engl). 2010. November; 123 21: 3030- 3033. [PubMed] [Google Scholar]
- 18. Ledin H, Aspenberg P, Good L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012. October; 83 5: 499- 503. doi: 10.3109/17453674.2012.727078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu D, Graham D, Gillies K, Gillies RM. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res. 2014. December; 26 4: 207- 213. doi: 10.5792/ksrr.2014.26.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Newman RJ. Metabolic effects of tourniquet ischaemia studied by nuclear magnetic resonance spectroscopy. J Bone Joint Surg Br. 1984. May; 66 3: 434- 440. [DOI] [PubMed] [Google Scholar]
- 21. Sapega AA, Heppenstall RB, Chance B, Park YS, Sokolow D. Optimizing tourniquet application and release times in extremity surgery. A biochemical and ultrastructural study. J Bone Joint Surg Am. 1985. February; 67 2: 303- 314. [PubMed] [Google Scholar]
- 22. Irving GA, Noakes TD. The protective role of local hypothermia in tourniquet-induced ischaemia of muscle. J Bone Joint Surg Br. 1985. March; 67 2: 297- 301. [DOI] [PubMed] [Google Scholar]
- 23. McGrath BJ, Hsia J, Epstein B. Massive pulmonary embolism following tourniquet deflation. Anesthesiology. 1991. March; 74 3: 618- 620. [DOI] [PubMed] [Google Scholar]
- 24. Palmer SH, Graham G. Tourniquet-induced rhabdomyolysis after total knee replacement. Ann R Coll Surg Engl. 1994. November; 76 6: 416- 417. [PMC free article] [PubMed] [Google Scholar]
- 25. Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995. March; 77 2: 250- 253. [PubMed] [Google Scholar]
- 26. Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty. 1998. February; 13 2: 211- 216. [DOI] [PubMed] [Google Scholar]
- 27. Wakankar HM, Nicholl JE, Koka R, D'Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999. January; 81 1: 30- 33. [DOI] [PubMed] [Google Scholar]
- 28. Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001. Jul-Aug; 9 4: 253- 257. [DOI] [PubMed] [Google Scholar]
- 29. Nishiguchi M, Takamura N, Abe Y, Kono M, Shindo H, Aoyagi K. Pilot study on the use of tourniquet: a risk factor for pulmonary thromboembolism after total knee arthroplasty? Thromb Res. 2005; 115 4: 271- 276. [DOI] [PubMed] [Google Scholar]
- 30. Fukuda A, Hasegawa M, Kato K, Shi D, Sudo A, Uchida A. Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. 2007. October; 127 8: 671- 675. [DOI] [PubMed] [Google Scholar]
- 31. Butt U, Ahmad R, Aspros D, Bannister GC. Factors affecting wound ooze in total knee replacement. Ann R Coll Surg Engl. 2011. January; 93 1: 54- 56. doi: 10.1308/003588410X12771863937124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Olivecrona C, Blomfeldt R, Ponzer S, Stanford BR, Nilsson BY. Tourniquet cuff pressure and nerve injury in knee arthroplasty in a bloodless field: a neurophysiological study. Acta Orthop. 2013. April; 84 2: 159- 164. doi: 10.3109/17453674.2013.782525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tarwala R, Dorr LD, Gilbert PK, Wan Z, Long WT. Tourniquet use during cementation only during total knee arthroplasty: a randomized trial. Clin Orthop Relat Res. 2014. January; 472 1: 169- 174. doi: 10.1007/s11999-013-3124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harvey EJ, Leclerc J, Brooks CE, Burke DL. Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997. April; 12 3: 291- 296. [DOI] [PubMed] [Google Scholar]
- 35. Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. 2002; 26 5: 306- 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. 2000. February; (371):169-177. [DOI] [PubMed] [Google Scholar]
- 37. Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009. October; 33 5: 1263- 1268. doi: 10.1007/s00264-008-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Prentice CR. Basis of antifibrinolytic therapy. J Clin Pathol Suppl (R Coll Pathol). 1980; 14: 35- 40. [PMC free article] [PubMed] [Google Scholar]
- 39. Mannucci PM. Hemostatic drugs. N Engl J Med. 1998. July 23; 339 4: 245- 253. [DOI] [PubMed] [Google Scholar]
- 40. Shore-Lesserson L, Reich DL, Vela-Cantos F, Ammar T, Ergin MA. Tranexamic acid reduces transfusions and mediastinal drainage in repeat cardiac surgery. Anesth Analg. 1996. July; 83 1: 18- 26. [DOI] [PubMed] [Google Scholar]
- 41. Dalmau A, Sabaté A, Acosta F, et al. Tranexamic acid reduces red cell transfusion better than epsilon-aminocaproic acid or placebo in liver transplantation. Anesth Analg. 2000. July; 91 1: 29- 34. [DOI] [PubMed] [Google Scholar]
- 42. Ickx BE, van der Linden PJ, Melot C, et al. Comparison of the effects of aprotinin and tranexamic acid on blood loss and red blood cell transfusion requirements during the late stages of liver transplantation. Transfusion. 2006. April; 46 4: 595- 605. [DOI] [PubMed] [Google Scholar]
- 43. Henry DA, Carless PA, Moxey AJ, et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2007. Oct 17;(4):CD001886. [DOI] [PubMed] [Google Scholar]
- 44. Colomina MJ, Bagó J, Vidal X, Mora L, Pellisé F. Antifibrinolytic therapy in complex spine surgery: a case-control study comparing aprotinin and tranexamic acid. Orthopedics. 2009. February; 32 2: 91. [PubMed] [Google Scholar]
- 45. Henry D, Carless P, Fergusson D, Laupacis A. The safety of aprotinin and lysine-derived antifibrinolytic drugs in cardiac surgery: a meta-analysis. CMAJ. 2009. January 20; 180 2: 183- 193. doi: 10.1503/cmaj.081109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br. 2011. January; 93 1: 39- 46. doi: 10.1302/0301-620X.93B1.24984. [DOI] [PubMed] [Google Scholar]
- 47. Wind TC, Barfield WR, Moskal JT. The effect of tranexamic acid on transfusion rate in primary total hip arthroplasty. J Arthroplasty. 2014. February; 29 2: 387- 389. doi: 10.1016/j.arth.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 48. Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W. Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res. 2009. March; 123 5: 687- 696. doi: 10.1016/j.thromres.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 49. Gill JB, Rosenstein A. The use of antifibrinolytic agents in total hip arthroplasty: a meta-analysis. J Arthroplasty. 2006. September; 21 6: 869- 873. [DOI] [PubMed] [Google Scholar]
- 50. Gill JB, Chase E, Rosenstein A. The use of tranexamic acid in revision total hip arthroplasty: a pilot study. Curr Orthop Pract. 2009. April; 20 2: 152- 156. doi: 10.1097/BCO.0b013e318191ebc0. [Google Scholar]
- 51. Kazemi SM, Mosaffa F, Eajazi A, et al. The effect of tranexamic acid on reducing blood loss in cementless total hip arthroplasty under epidural anesthesia. Orthopedics. 2010. January; 33 1: 17 doi: 10.3928/01477447-20091124-30. [DOI] [PubMed] [Google Scholar]
- 52. Eubanks JD. Antifibrinolytics in major orthopaedic surgery. J Am Acad Orthop Surg. 2010. March; 18 3: 132- 138. [PubMed] [Google Scholar]
- 53. Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2012. July 3; 94 13: 1153- 1159. doi: 10.2106/JBJS.K.00873. [DOI] [PubMed] [Google Scholar]
- 54. Barsoum WK, Klika AK, Murray TG, Higuera C, Lee HH, Krebs VE. Prospective randomized evaluation of the need for blood transfusion during primary total hip arthroplasty with use of a bipolar sealer. J Bone Joint Surg Am. 2011. March 16; 93 6: 513- 518. doi: 10.2106/JBJS.J.00036. [DOI] [PubMed] [Google Scholar]
- 55. Seo JG, Moon YW, Park SH, Kim SM, Ko KR. The comparative efficacies of intra-articular and IV tranexamic acid for reducing blood loss during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013. August; 21 8: 1869- 1874. doi: 10.1007/s00167-012-2079-2. [DOI] [PubMed] [Google Scholar]
- 56. Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000. July 1; 7 3: 151- 155. [DOI] [PubMed] [Google Scholar]
- 57. Marulanda GA, Krebs VE, Bierbaum BE, et al. Hemostasis using a bipolar sealer in primary unilateral total knee arthroplasty. Am J Orthop (Belle Mead NJ). 2009. December; 38 12: E179- E183. [PubMed] [Google Scholar]
- 58. Fan Y, Jin J, Sun Z, et al. The limited use of a tourniquet during total knee arthroplasty: a randomized controlled trial. Knee. 2014. December; 21 6: 1263- 1268. doi: 10.1016/j.knee.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 59. Ejaz A, Laursen AC, Kappel A, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014. August; 85 4: 422- 426. doi: 10.3109/17453674.2014.931197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Chen S, Li J, Peng H, Zhou J, Fang H, Zheng H. The influence of a half-course tourniquet strategy on peri-operative blood loss and early functional recovery in primary total knee arthroplasty. Int Orthop. 2014. February; 38 2: 355- 359. doi: 10.1007/s00264-013-2177-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mittal R, Ko V, Adie S, et al. Tourniquet application only during cement fixation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg. 2012. June; 82 6: 428- 433. doi: 10.1111/j.1445-2197.2012.06083.x. [DOI] [PubMed] [Google Scholar]
- 62. Tai TW, Chang CW, Lai KA, Lin CJ, Yang CY. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012. December 19; 94 24: 2209- 2215. doi: 10.2106/JBJS.K.00813. [DOI] [PubMed] [Google Scholar]
- 63. Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Fismer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. 2012. March; 27 3: 331- 340. doi: 10.1016/j.arth.2011.04.046. [DOI] [PubMed] [Google Scholar]
- 64. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. April; 89 4: 780- 785. [DOI] [PubMed] [Google Scholar]
- 65. Losina E, Katz JN. Total knee arthroplasty on the rise in younger patients: are we sure that past performance will guarantee future success? Arthritis Rheum. 2012. February; 64 2: 339- 341. doi: 10.1002/art.33371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Mehrotra C, Remington PL, Naimi TS, Washington W, Miller R. Trends in total knee replacement surgeries and implications for public health, 1999-2000. Public Health Rep. 2005. May-Jun; 120 3: 278- 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fleischut PM, Eskreis-Winkler JM, Gaber-Baylis LK, et al. Variability in anesthetic care for total knee arthroplasty: an analysis from the anesthesia quality institute. Am J Med Qual. 2015. Mar-Apr; 30 2: 172- 179. doi: 10.1177/1062860614525989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Escobar A, Quintana JM, Bilbao A, et al. Development of explicit criteria for prioritization of hip and knee replacement. J Eval Clin Pract. 2007. June; 13 3: 429- 434. [DOI] [PubMed] [Google Scholar]
- 69. Frankel L, Sanmartin C, Conner-Spady B, et al. Osteoarthritis patients' perceptions of “appropriateness” for total joint replacement surgery. Osteoarthritis Cartilage. 2012. September; 20 9: 967- 973. doi: 10.1016/j.joca.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 70. Total knee replacements on the rise, despite high costs. Harv Health Lett. 2012. December; 38 2: 8. [PubMed] [Google Scholar]
- 71. Bhandari M, Smith J, Miller LE, Block JE. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord. 2012; 5: 89- 94. doi: 10.4137/CMAMD.S10859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Robinson JC, Pozen A, Tseng S, Bozic KJ. Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am. 2012. September 19; 94 18: 1693- 1698. [DOI] [PubMed] [Google Scholar]


