Abstract
Background:
Reperfusion of large vessel occlusions in acute stroke can improve patient outcomes. The purposes of this study were to assess the safety and efficacy of the Penumbra 5MAX ACE catheter for revascularization of large vessels and to compare its cost to the cost of stent retrievers.
Methods:
In this retrospective, single-center case review study, data were captured on consecutive patients treated with the Penumbra 5MAX ACE as first-line therapy during an 11-month period. Good functional outcome was defined as a modified Rankin Scale score of ≤2 at discharge. Results were directly compared with previously published data for stent retrievers, and length of stay was analyzed in relation to revascularization.
Results:
The 31 patients studied had a mean age of 66.3 ± 17.8 years and a mean National Institutes of Health Stroke Scale score of 19.4 ± 5.7. Intravenous tissue recombinant plasminogen activator therapy was initiated in 35.5% (11/31) of patients. A Thrombolysis in Cerebral Infarction (TICI) grade of 2b-3 reperfusion after endovascular therapy was achieved in 26/31 (83.9%) of cases; TICI grade 3 was achieved in 19/31 (61.3%) patients. The average time from groin puncture to TICI grade 2b-3 reperfusion was 40 minutes. The average estimated cost for aspiration with the 5MAX ACE alone was $4,916 per case compared with an estimated cost of $9,620 if a stent retriever was used as the primary device. Our actual average cost per case, including all adjunctive devices used in the neurointerventional procedure, was $6,997. Good functional outcome was achieved in 19/31 (61.3%) patients. Two patients experienced symptomatic intracerebral hemorrhage (6.5%), and 1 (3.2%) patient died. The length of stay was significantly shorter among patients with TICI grade 2b-3 reperfusion compared to patients with TICI grade <2 (6.8 ± 5.34 days vs 15.8 ± 11.32 days, respectively; P<0.05).
Conclusion:
These findings suggest that direct aspiration with the large-bore 5MAX ACE catheter can be considered a first-line approach to mechanical thrombectomy for large vessel occlusions. Our results demonstrated high rates of successful reperfusion in a timely manner with excellent clinical outcomes, although our sample size was small. In addition, this direct-aspiration technique has important cost-savings potential compared to stent retrievers.
Keywords: Intracranial thrombosis, ischemia, reperfusion, stroke, thrombectomy
INTRODUCTION
Acute ischemic stroke is the fourth leading cause of death in the United States and is also the leading cause of long-term disability in the country.1,2 Strokes attributable to large vessel occlusion or proximal vessel occlusion have a poor prognosis if allowed to follow their natural course, but with early revascularization treatment, patient outcomes have improved and mortality has decreased.3,4 Much has been published about the advances in techniques for mechanical approaches to revascularization of large vessel occlusion,5,6 and in 2015, intraarterial treatment to achieve revascularization was demonstrated to be safe while improving outcomes.7 The purpose of this study was to assess the safety and effectiveness of achieving revascularization of proximal or large vessel occlusion using the Penumbra 5MAX ACE catheter with ADAPT (A Direct Aspiration First Pass Technique). Also, because care must be provided in a cost-effective manner in today's medical environment, we also compared the cost of the Penumbra 5MAX ACE catheter with the cost of stent retrievers.
METHODS
A retrospective review of the medical records from September 2013 to July 2014 was conducted of all patients with large vessel occlusion strokes who were treated with mechanical thrombectomy using ADAPT and the recently introduced (June 2013) 5MAX ACE catheter (Penumbra, Inc.) as first-line therapy. Patient selection for endovascular treatment of large vessel occlusion acute stroke at our institution is based on noncontrast computed tomography (CT), CT angiogram, and whole brain 320-slice CT perfusion imaging, regardless of time of onset. This study was conducted after institutional review board approval, and informed consent was obtained from patients or their legal representatives in accordance with the Helsinki Declaration of 1975, as revised in 2005.
Data on age, sex, and presentation National Institutes of Health Stroke Scale (NIHSS) score were recorded. The NIHSS lists 11 specific abilities that are scored on numerical scales, with 0 indicating normal function and higher scores indicating some level of impairment. The maximum possible score is 42, and the minimum score is 0. Groin puncture time, reperfusion time, Thrombolysis in Cerebral Infarction (TICI) grade flow before and after the procedure, and procedural complications were also recorded. The TICI grading system is a tool for determining the response to thrombolytic therapy for ischemic stroke. The grades range from 0 (no perfusion) to 3 (complete perfusion). TICI subcategory grade 2b indicates complete filling of all of the expected vascular territory but with slower than normal filling. Follow-up data in the form of the modified Rankin Scale (mRS) score at discharge was also obtained from the medical records. The mRS is used to measure the degree of disability in carrying out daily activities for people who have had a stroke or have some other neurological disability. The scale is scored from 0 (no disability) to 6 (death). Higher scores indicate greater disability.
Thrombectomy cases using ADAPT with the 5MAX ACE were selected based on vessel size and the interventionalist's opinion that the catheter was the proper size for the occluded vessel. Patients with distal lesions (M2 or further) or with small caliber proximal vessels for which the 5MAX ACE was considered too large were not treated with the device, and hence, are not included in this discussion.
However, all patients in whom the following technique was used during the specified time frame are included in the study cohort. The technique involves an 8 French groin sheath through which a NeuronMAX 088 access catheter (Penumbra, Inc.) is advanced over a Davis diagnostic catheter (Torcon NB Advantage Catheter; Cook Medical) and an angled Glidewire (Terumo) into the internal carotid or vertebral artery of the affected side. Once in position, the 5MAX ACE aspiration catheter is advanced to the proximal segment of the thrombus with the aid of either a 3MAX aspiration catheter or a Velocity microcatheter (Penumbra, Inc.) with the support of a Fathom microwire (Boston Scientific Corporation). Whether to use a 3MAX or a Velocity microcatheter was the operator's decision (twice the 5MAX ACE was advanced over a Fathom microwire alone). Direct aspiration using the Penumbra reperfusion system (ADAPT) was the first-line therapy. If unsuccessful despite at least 2 attempts or if thrombus fragmentation was identified, additional small aspiration catheters or adjunctive thrombectomy devices were used.
Because the neurointerventionists at our institution have been using this method primarily rather than stent retrievers, a direct comparison of the 2 techniques at our institution would be unfair and poorly powered in the stent retriever arm. Therefore, we compared our results to published series on stent retrievers by other experienced authors.7,8
Successful reperfusion was defined by postprocedure TICI flow of grade 2b or 3. Good functional outcome was defined as an mRS score of 0-2 at discharge. Symptomatic intracerebral hemorrhage (sICH) was defined as hematoma associated with a worsening NIHSS score of 4 points or more.
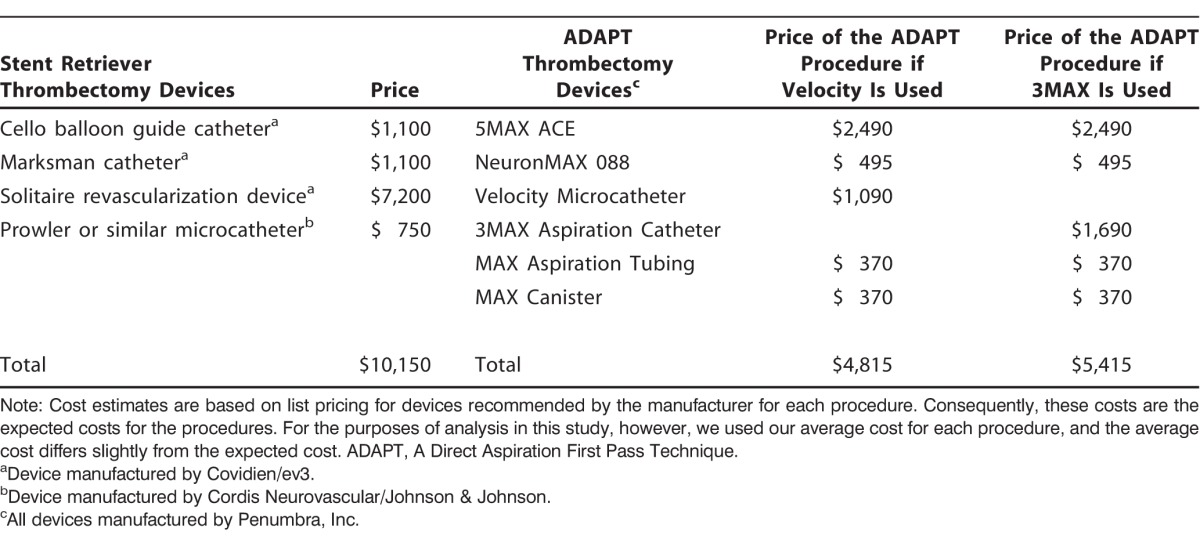
The expected cost of the devices was totaled for each case using market/list prices to eliminate the variability of pricing among different institutions (a methodology that has been used in other publications for device cost analysis)9 and compared with what the cost would have been for an uncomplicated case using the Solitaire stent retriever device (Covidien/ev3). Costs for the Penumbra system aspiration cases included the cost of all reperfusion catheters (the 5MAX ACE plus any other adjunctive tools if required), 6 French long sheath (NeuronMAX), as well as coaxial delivery catheters (3MAX or Velocity), canister, and aspiration tubing. Costs for the Solitaire stent retriever cases used as first-line therapy included the cost of balloon guide catheter, microcatheter, and stent retriever (as recommended by parent company). Using device list prices, price estimates for comparison are shown in Table 1. Sheaths, microwires, diagnostic catheters, and closure devices were not included in the cost analysis as they are used in the same fashion for both techniques. As noted, the costs shown in Table 1 are the expected costs based on list prices. For the purposes of analysis in this study, however, we used our average cost for each procedure, and the procedures' total average costs differ slightly from the total expected costs.
Table 1.
Thrombectomy Options: Cost Comparison
The data obtained were compared with previously published data: the Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN)7 and the North American Solitaire Stent Retriever Acute Stroke (NASA) Registry.8 The effect of successful revascularization on length of stay was compared using the Tukey honest significant difference (HSD) test.
RESULTS
Demographics
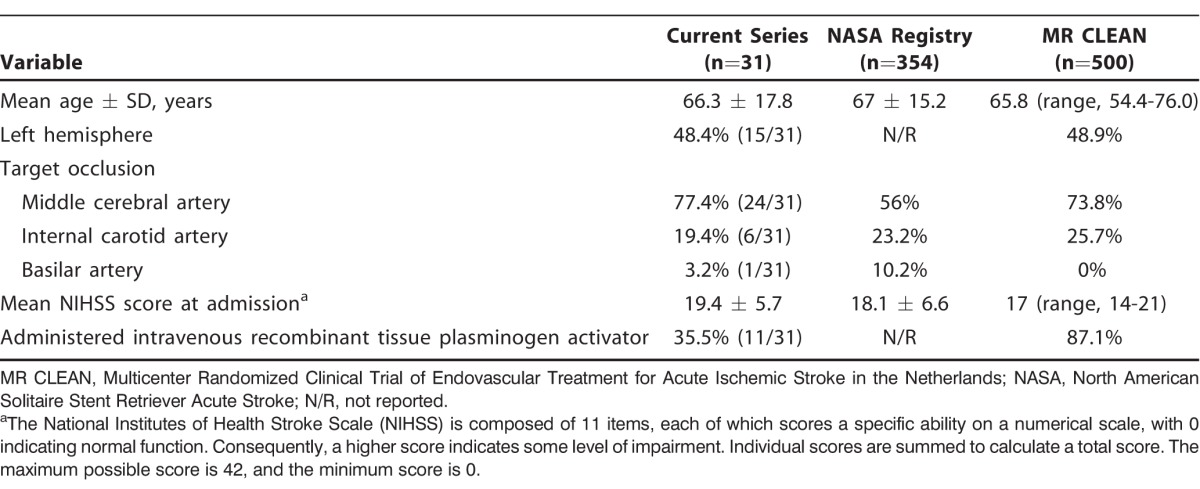
A total of 31 patients were included in our study. All were treated with the 5MAX ACE catheter as the primary tool for mechanical thrombectomy. The patients' mean age was 66.3 years ± 17.8, and their mean admission NIHSS score was 19.4 ± 5.7 (Table 2). The target occlusion was located in the proximal middle cerebral artery in 24 (77.4%) patients, in the internal carotid artery in 6 (19.4%) patients, and in the basilar artery in 1 (3.2%) patient. Eleven (35.5%) patients had received intravenous recombinant tissue plasminogen activator.
Table 2.
Revascularization and Outcomes
TICI grade 2b-3 reperfusion was achieved in 26 (83.9%) patients, while TICI grade 3 was attained in 19 (61.3%) patients. Of the 83.9% of patients who achieved TICI grade 2b-3, successful revascularization by aspiration with the Penumbra system was performed in 84.6% (22/26) of the patients.
In a further breakdown of devices used to achieve TICI grade 2b-3, 73.1% (19/26) of patients achieved reperfusion with ADAPT and the 5MAX ACE catheter alone, 15.4% (4/26) of patients required the addition of a separator or smaller aspiration catheter, and 11.5% (3/26) of patients required the addition of a stent retriever.
Overall, rescue therapy was used in 35.5% (11/31) of the patient cohort. In one case, rescue therapy was used when the 5MAX ACE could not be advanced past the ophthalmic segment of the internal carotid artery to reach the thrombus. The rescue techniques used were the Penumbra separator (n=5), smaller aspiration catheters (n=6), and stent retrievers (n=5). Some cases required more than one rescue therapy tool. A noteworthy observation is that 7 of our first 15 cases required additional devices (rescue) compared to only 4 in the last 16 cases, suggesting a short learning curve for using this new device. In the 5 cases in which TICI grade 2b-3 was not achieved, rescue therapy with stent retrievers was attempted in 2/5 (40%) of the cases, smaller aspiration catheters were used in 2/5 (40%), and the last case was aborted because of contrast extravasation during the procedure.
The average time from groin puncture to TICI grade 2b-3 reperfusion was 40 minutes (Table 3). Good functional outcome was reported in 19 (61.3%) patients. The mean discharge mRS score was 2.3 ± 1.8. Thirteen patients were discharged to home (41.9%), 11 to rehabilitation (35.5%), 2 to a nursing home (6.5%), 2 to a skilled nursing facility (6.5%), and 1 to hospice (3.2%). One patient was transferred to another institution (3.2%), and we were not able to obtain information on the final discharge disposition. The transfer was done at the request of the family so that the patient could be cared for closer to their home. One (3.2%) patient died.
Table 3.
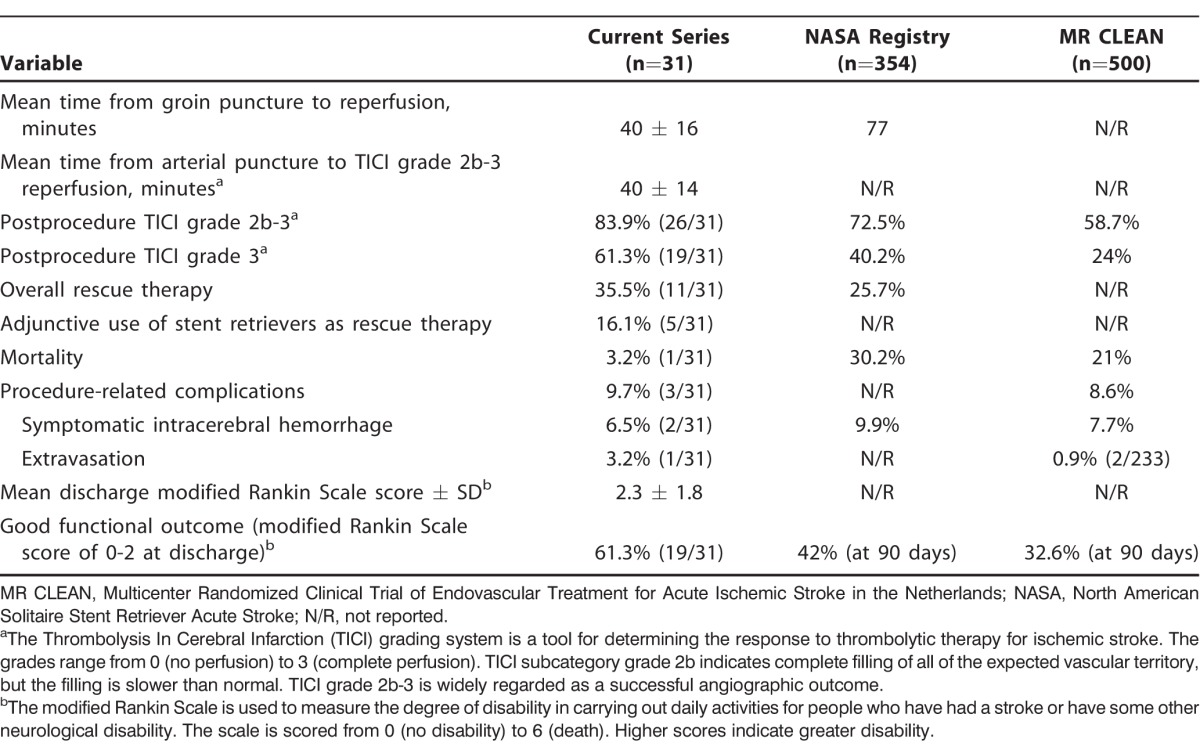
The average length of stay increased as the reperfusion grade decreased: TICI grade 3 = 5.7 ± 3.65 days, TICI grade 2b = 9.14 ± 8.33 days, and TICI grade <2b = 15.8 ± 11.32 days. These findings are statistically significant when compared based on angiographic outcome using the Tukey HSD test (TICI grade 2b-3 vs TICI grade <2b: 6.8 ± 5.34 days vs 15.8 ± 11.32 days, P<0.05).
Regarding procedure-related complications, 2 patients experienced sICH (6.5%), and 1 patient suffered extravasation of contrast (3.2%). Procedure-related complications were similar in all series: current series 9.7%; MR CLEAN 8.6%; NASA Registry 9.9% (the NASA Registry only reports sICH as procedure-related complications).
Cost Comparison
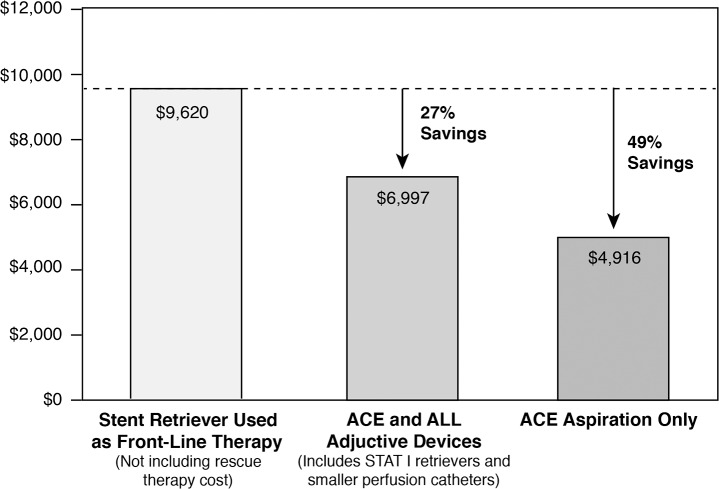
Our average cost for aspiration with the 5MAX ACE alone was $4,916. In contrast, our average cost when a stent retriever is used as the primary device is $9,620, so aspiration with the 5MAX ACE alone can save 49% in potential costs. However, these average costs do not reflect the increased cost of rescue therapy tools that are used in approximately 26% of stent retriever cases according to the NASA Registry.8 In our study, the average cost of all cases, including all adjunctive devices, was $6,997 per patient. Compared with the cost of using a stent retriever as primary device, this average cost illustrates a potential savings of approximately 26% (Figure).
Figure.
Comparison of average costs for aspiration with the 5MAX ACE alone vs the 5MAX ACE plus adjunctive devices when needed vs the use of a stent retriever as first-line therapy.
DISCUSSION
This initial clinical experience supports considering the use of the 5MAX ACE catheter as first-line therapy for large vessel occlusion in acute ischemic stroke. Our analysis suggests that direct aspiration with a large bore catheter first using ADAPT6 may represent an important potential cost-saving approach to vessel revascularization that in our experience results in high rates of reperfusion with rapid procedural times, enabling excellent clinical outcomes with acceptable safety.
Regarding angiographic and technical outcomes, the percentage of our patients showing reperfusion to TICI grade 2b-3—83.9%—is higher than the percentages reported in the NASA Registry (72.5%)8 and in the MR CLEAN study (58.7%).7 Reperfusion to TICI grade 3 in 61.3% of our patients is also higher than the rates reported in the NASA Registry (40.2%) and MR CLEAN (24%) and is comparable to a 2014 publication describing the ADAPT FAST technique that achieved reperfusion to TICI grade 3 in 61% of subjects treated with the 5MAX ACE catheter and 41% of those treated with the 5MAX.10 We believe that the larger lumen of the 5MAX ACE catheter may lead to higher TICI grade 3 rates compared with the 5MAX.
Our mean time to reperfusion of 40 minutes using the 5MAX ACE is similar to the report of 36 minutes published in 201410 for a study using a similar technique, while in the NASA Registry,8 the average time to revascularization is approximately 77 minutes using stent retrievers as first-line therapy.
Good functional outcome (mRS score ≤2) was seen in 61.3% of our patients, a finding that compares favorably with the 32.6% of patients with good functional outcomes reported in MR CLEAN7 and the 42% in the NASA Registry.8 In our cohort, 24 (77.4%) patients were discharged to home or rehabilitation, another indicator of a satisfactory outcome. Our sICH rate of 6.5% is comparable to the 9.9% in the NASA Registry and the 7.7% in MR CLEAN.7,8 The death rate in our group was 3.2% vs 30.2% in NASA registry and 21% in MR CLEAN.7,8
The purpose of the cost analysis is to provide a basic understanding of the relative procedural device costs between ADAPT using the 5MAX ACE catheter and stent retrievers in practice. Hospital administrators are acutely aware of device costs for procedures. Both endovascular and open surgeons are being tasked to reduce costs and to justify inclusion of new products, sometimes by omitting other products, as in the authors' experience.
We do not warrant that our cost analysis defines cost effectiveness because such a determination requires a complete evaluation of the patient's care.11 However, device costs are a major cost in the treatment of large vessel occlusions and are the only costs that the interventionalist may completely control.
A study by Turk et al provides support for our cost-saving findings.11 In a single-center retrospective study of mechanical thrombectomy, the average device cost of $15,798 for a stent retriever (the Solitaire or Trevo) with local aspiration was significantly higher than the $10,263 cost of the traditional Penumbra system and the $7,421 cost for ADAPT.11 Their data thus showed a 53% cost savings with ADAPT compared to a stent retriever with local aspiration, consistent with our data showing a potential 49% cost savings with ADAPT. These investigators included all costs, whereas we did not include the costs of wires, diagnostic catheters, sheaths, or closure devices. In our study, the potential cost savings for our institution was approximately 26% when we added all cases together, including all rescue therapy costs, and compared the cost with the cost of successful revascularization with a stent retriever as the only tool. If we consider that rescue therapy is required in at least 26% of stent retriever cases,8 the cost savings could be much greater than our estimate.
Despite our small sample size, our data show that good angiographic results correlate with shorter length of stay. Shorter hospitalizations have the potential to produce additional cost savings in the treatment of large vessel occlusion strokes. The authors believe that improvement in cerebral perfusion—not the actual device that was used to perform the successful thrombectomy—reduces length of stay.
One limitation of this study is the lack of a comparison group of stent retriever cases performed at the same institution. Because the current protocol shared by the 2 neurointerventionalists is to start with ADAPT, stent retrievers are used primarily for smaller arteries, for tortuous anatomy, and as rescue therapy following thromboaspiration. Another limitation is the lack of blinded core laboratory adjudication of angiographic endpoints; a metaanalysis of trial data on angiographic evaluation of aneurysms has shown that local centers may overestimate their results.12 Furthermore, our study is limited to a single center, which makes the results potentially less generalizable, and the data analysis is retrospective rather than prospective. While the sample size is small compared to the data emerging from multicenter randomized controlled trials, this report of a relatively new device shows the potential for important cost savings while maintaining a high degree of clinical effectiveness. Although the preponderance of currently available trial data is based on stent retrievers, the authors believe that ADAPT deserves continued consideration as first-line therapy and should be studied further with a randomized, prospective cost-benefit analysis to guide future recommendations for acute stroke care.
CONCLUSION
This single-center retrospective review of mechanical thrombectomy cases using the large bore 5MAX ACE catheter and ADAPT suggests that it should be considered as a first-line approach for treatment for large vessel occlusions. This technique resulted in high rates of successful reperfusion, rapid reperfusion times, and excellent clinical outcomes with important potential cost savings compared to the first-line use of stent retrievers.
ACKNOWLEDGMENTS
Both authors have participated as speakers/educators for the Penumbra, Inc. speakers' bureau.
Some of the data discussed in the manuscript were presented on November 7, 2014, at the Society of Vascular Interventional Neurology 7th Annual Meeting in Hollywood, FL.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012. October 10; 61 6: 1- 51. [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015. January 27; 131 4: e29- e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3. Wasiewski WW, Johnston KC. Clinical trials, devices, unproven treatments, and clinical equipoise. Stroke. 2009. June; 40 6: e441- e442. doi: 10.1161/STROKEAHA.108.531939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gralla J, Brekenfeld C, Mordasini P, Schroth G. Mechanical thrombolysis and stenting in acute ischemic stroke. Stroke. 2012. January; 43 1: 280- 285. doi: 10.1161/STROKEAHA.111.626903. [DOI] [PubMed] [Google Scholar]
- 5. Spiotta AM, Chaudry MI, Hui FK, Turner RD, Kellogg RT, Turk AS. Evolution of thrombectomy approaches and devices for acute stroke: a technical review. J Neurointerv Surg. 2015. January; 7 1: 2- 7. doi: 10.1136/neurintsurg-2013-011022. [DOI] [PubMed] [Google Scholar]
- 6. Turk AS, Spiotta A, Frei D, et al. Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014. April 1; 6 3: 231- 237. doi: 10.1136/neurintsurg-2013-010713. [DOI] [PubMed] [Google Scholar]
- 7. Berkhemer OA, Fransen PS, Beumer D, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015. January 1; 372 1: 11- 20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 8. Zaidat OO, Castonguay AC, Gupta R, et al. North American Solitaire Stent Retriever Acute Stroke registry: post-marketing revascularization and clinical outcome results. J Neurointerv Surg. 2014. October; 6 8: 584- 588. doi: 10.1136/neurintsurg-2013-010895. [DOI] [PubMed] [Google Scholar]
- 9. Milburn J, Pansara AL, Vidal G, Martinez RC. Initial experience using the Penumbra coil 400: comparison of aneurysm packing, cost effectiveness, and coil efficiency. J Neurointerv Surg. 2014. March; 6 2: 121- 124. doi: 10.1136/neurintsurg-2012-010587. [DOI] [PubMed] [Google Scholar]
- 10. Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014. May; 6 4: 260- 264. doi: 10.1136/neurintsurg-2014-011125. [DOI] [PubMed] [Google Scholar]
- 11. Turk AS, Turner R, Spiotta A, et al. Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015. September; 7 9: 666- 670. doi: 10.1136/neurintsurg-2014-011282. [DOI] [PubMed] [Google Scholar]
- 12. Rezek I, Mousan G, Wang Z, Murad MH, Kallmes DF. Effect of core laboratory and multiple-reader interpretation of angiographic images on follow-up outcomes of coiled cerebral aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2013. July; 34 7: 1380- 1384. doi: 10.3174/ajnr.A3398. [DOI] [PMC free article] [PubMed] [Google Scholar]