Abstract
This article evaluates the short-term outcomes of students attending the National Alliance on Mental Illness’ Ending the Silence presentations, delivered across three high schools in a Northern California school district.
One-half of all individuals who have experienced a mental illness report that their symptoms first began in adolescence (Kessler et al., 2005). Although one in five adolescents in the United States meet criteria for a serious mental disorder (Merikangas et al., 2010), less than one-third obtain mental health treatment (Merikangas et al., 2011). Mental illness stigma has been found to be present at an early age (Chandra and Minkovitz, 2006; Wahl, 2002) and has been posited as a major barrier to treatment (Corrigan, 2004). A number of studies evaluating interventions aimed at reducing mental illness stigma among children and adolescents have been conducted (Corrigan et al., 2012; Yamaguchi, Mino, and Uddin, 2011). These stigma and discrimination reduction (SDR) interventions typically involve an educational presentation in the classroom that may include an opportunity for contact with a person who has experienced mental health challenges. Contact usually involves a presenter sharing his or her experiences of recovering from a mental illness. A common goal of SDR interventions is not only to increase awareness of common mental health problems and to reduce stigma, but to foster greater acceptance and social inclusion of individuals who experience mental health challenges (Corrigan et al., 2012; Yamaguchi, Mino, and Uddin, 2011).
The National Alliance on Mental Illness (NAMI), a mental health education, advocacy, research, and service organization, developed such an educational presentation targeting high school students. Ending the Silence (ETS) is a 50-minute interactive presentation designed to teach high school students about mental illness, treatment, and how to help those in need of support, including friends, family, or themselves. The goal of ETS is “to create a generation of students equipped to eradicate the stigma associated with mental illness through education and advocacy” (NAMI, 2012). ETS components include a slide presentation, short videos, a presenter who shares his or her story about recovering from a mental illness (specifically referencing experiences as a student), and a question-and-answer period. Students are also provided with a resource card with contact information for mental health agencies and a list of symptoms and signs of mental illness. In addition, postcards are mailed to parents that inform them about the program and services provided by their local NAMI Affiliate.
Relying on funds from the Mental Health Services Act (Proposition 63), which levied a 1-percent tax on incomes over $1 million to expand mental health services, the California Mental Health Services Authority (CalMHSA) oversees three statewide prevention and early intervention initiatives focusing on mental illness stigma and discrimination reduction (SDR), suicide prevention, and student mental health. ETS is one of the programs funded under the SDR initiative. This paper evaluates the short-term outcomes of students attending ETS presentations delivered across three high schools in a Northern California school district. This comprises a small subset of the 704 ETS presentations delivered throughout the state of California under the SDR initiative, as reported by NAMI as of January 2015.* This evaluation provides preliminary information regarding the program's efficacy, which is valuable given that there have been no prior evaluations of ETS. Another NAMI program, In Our Own Voice, which was developed for broader community audiences, was found to increase mental health literacy among female high school students but did not decrease stigmatizing attitudes (Pinto-Foltz, Logsdon, and Myers, 2011). This evaluation assessed whether ETS, which has been specifically tailored for high school audiences, is effective across a wide array of outcomes.
Methods
A total of three ETS presentations were included in this study. Each presentation was delivered at a different high school, with one occurring during an assembly (191 students) and the other two during classroom time (59 students). This resulted in a total of 250 students who completed surveys before and after the presentation (i.e., pre- and post-test, respectively). Participants' mean age was 15.93 (SD = 1.32) and 57 percent were female, 37 percent male, and 6 percent other. With respect to students' racial/ethnic background, 29 percent were Latino, 39 percent non-Latino White, 7 percent non-Latino African American, 9 percent non-Latino Asian American, 1 percent non-Latino Hawaiian/Pacific Islander, 14 percent multiracial, and <1 percent listed another race. Approximately one-third of participants (31 percent) reported speaking a language other than English at home. NAMI worked with schools to ensure that passive parental consent and student assent were obtained. None of the parents or respondents refused to participate, but students who were missing a pre-test (N = 31) or post-test (N = 56) assessment were dropped from the analyses.
Measures
Where possible, measures were drawn or adapted from previous studies conducted with youth populations in which changes occurred in response to an SDR intervention, thus indicating the items' ability to detect such shifts (Livingston et al., 2013; Pinfold et al., 2005; Rahman et al., 1998; Schulze et al., 2003; Spagnolo, Murphy, and Librera, 2008; Watson, Miller, and Lyons, 2005; Watson et al., 2004; Yap and Jorm, 2012). The survey included items on the following domains: attitudes and emotional responses toward people with mental health problems, intentions to seek help for mental health symptoms and provide support to others experiencing symptoms, and knowledge about mental illness. Participant perceptions of the presentation were also assessed, including the perceived cultural sensitivity of the program and level of involvement in the narrative or stories shared about experiences of recovering from a mental illness. Narrative involvement has been shown to increase responsiveness to information designed to educate and/or persuade (Green and Brock, 2000). Descriptions of all of the measures are provided alongside the presentation of results.
Analyses
We examined whether participants' average scores or percentage of endorsement of survey items changed significantly from pre-test to post-test.** As is conventional in social science research, a p-value less than 0.05 (i.e., p < 0.05) was considered a statistically significant change from pre- to post-test.
Results
Perceptions of the Presentation
Overall, 74 percent of the students reported that attending the presentation was a positive experience and more than one-half expressed getting experientially involved with what it might feel like to have a mental health challenge (see Figure 1). Approximately two-thirds felt that the presentation taught them how to respond to peers with a mental health challenge who are from a different culture. Although 78 percent said they would recommend the presentation to someone of their own culture, only about one-quarter considered the presentation as being culturally sensitive to their own background. Latino students were significantly more likely to rate the presentation as being culturally sensitive to their background than non-Latino White students (30 percent and 17 percent, respectively; p < 0.01; not shown in figure).
Figure 1.
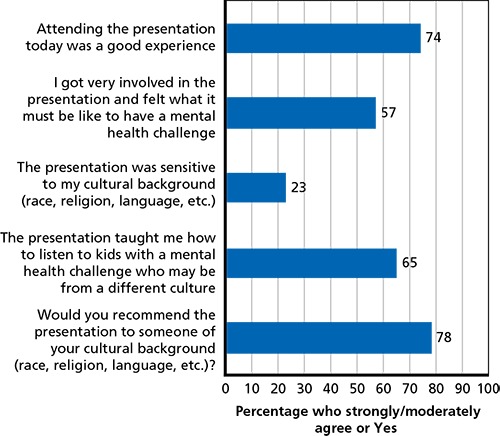
Perceptions of the Presentation
Attitudes Toward People with Mental Health Problems
The following attitudinal items were assessed: social distance (i.e., degree of willingness to interact with a person with a mental health problem), blame, perceived dangerousness, and beliefs about the acceptability of individuals with a mental illness serving as a child care provider. This latter item was included given that issues related to individuals with mental health problems' proximity to family and children have been found to elicit particularly negative responses (Pescosolido et al., 2013).
In Figure 2, pre- and post-test responses to questions on social distance (first five items) and blame (last item) are provided. Significant positive shifts in social distance occurred from pre- to post-test. Specifically, after attending the presentation, participants expressed greater willingness to extend an invitation to their house, work on a project, and go on a date with a hypothetical student with a mental health problem. In contrast, no significant changes occurred in students' feelings about being in class with, or being seen talking with, a student with a mental health problem. In addition, no significant shifts occurred in blaming the student for his or her mental health problem.
Figure 2.
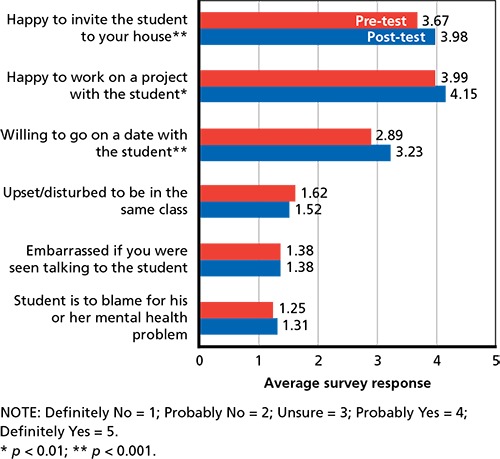
Changes in Social Distance and Blame from Pre- to Post-Presentation
As shown in Figure 3, some students' other attitudes toward people with mental illness significantly improved after the presentation. Perceptions of people with mental illness as dangerous or as unfit to take on a job caring for children significantly decreased from pre-test to post-test.
Figure 3.
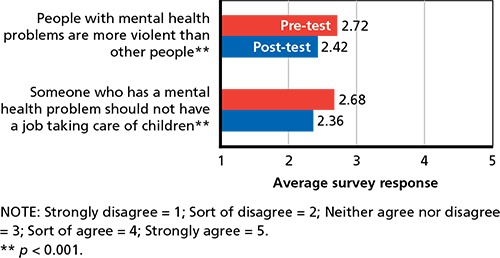
Changes in Attitudes Toward People with Mental Illness from Pre- to Post-Presentation
Emotional Responses to Individuals with Mental Health Challenges
Some theories posit that emotional reactions like fear and anger are the basis for prejudice against groups that appear different or dissimilar (Cottrell and Neuberg, 2005). To assess for such responses, participants were asked how they would feel having the student with a mental health problem at their school. Participants were provided with a list of emotions and instructed to check off any that applied. At pre-test, only a small proportion endorsed negative emotions (see Figure 4). Less than 5 percent of participants reported feeling angry, scared, or disgusted; nonetheless, all were reduced post-presentation. Approximately one-third to one-half of participants expressed feeling interested, calm, or caring at pre-test, and significant increases were observed for all of these emotions after the performance. While nearly all changes in emotional responses were quite small—between 1 and 2 percentage points—a more substantial change was observed for pity. Thirty-six percent of participants reported feeling sorry for the student with a mental health problem at pre-test, and this decreased by six percentage points at post-test. Although pity has been associated with increased willingness to provide help, it has also been linked to perceptions of people with mental illness as incompetent; therefore, decreases in pity may be interpreted as a positive result (Corrigan and Fong, 2014).
Figure 4.
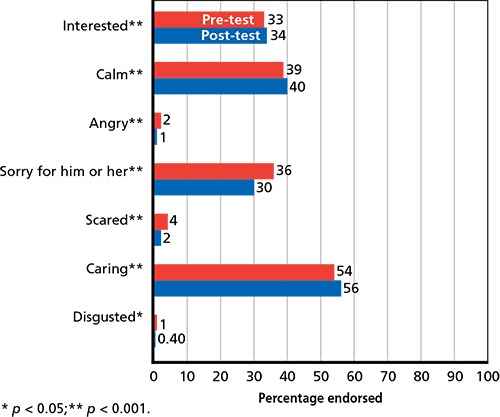
Emotional Responses to a Student with a Mental Health Problem at School
Help-Seeking and Support-Giving Intentions
No significant changes were observed for the help-seeking and support-giving items (see Figure 5). On average, participants endorsed “sort of” agreeing that they would tell an adult if they had a mental health problem or if a friend had a mental health problem. With respect to whether participants would provide emotional support to a friend with a mental health problem, levels of agreement were slightly lower, with responses on average falling between “neither agree/disagree” and “sort of agree.”
Figure 5.
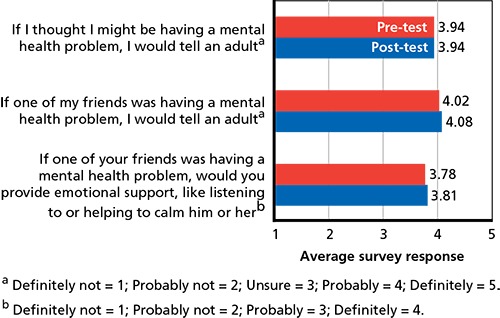
Help-Seeking and Support-Giving Intentions
Knowledge
Knowledge related to mental health problems increased in all areas assessed (see Figure 6). Across a set of true/false questions, the percentage of participants providing correct answers significantly increased from pre-test to post-test. At pre-test, most respondents knew the symptoms of ADHD and depression; nonetheless, significant gains were observed at post-test. There were also substantial gains in knowledge about the prevalence of mental illness and in the ability of those with mental illness to engage in normal activities. Most notable were the increases related to treatment effectiveness, knowledge of which nearly doubled.
Figure 6.
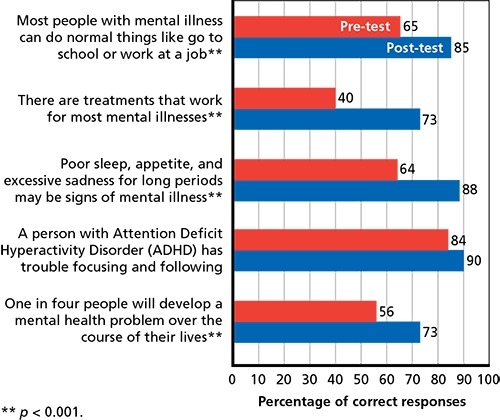
Knowledge Questions about Mental Illness
Discussion
This study investigated the effects of ETS, a high school educational presentation aimed at reducing mental illness stigma, increasing mental health knowledge, and equipping students to secure support for themselves or others should mental health needs arise. ETS had a significant immediate impact on several stigma indicators. After the presentation, participants reported being more willing to extend an invitation to one's house, to work on a project, and to go on a date with a student who has a mental health problem. In addition, perceptions of people with mental health problems as violent or as unfit for child care jobs also significantly diminished after the presentation. These findings are promising, given that some of the most negatively held attitudes involve concerns about the dangerousness of individuals with a mental health problem and their engagement with vulnerable populations (Pescosolido et al., 2013).
Emotional responses are considered an integral component of stigma that may influence behaviors toward people with mental health problems (Link et al., 2004), yet this is an understudied aspect of stigma (Angermeyer, Holzinger, and Matschinger, 2010; Corrigan and Fong, 2014). In this study, only a very small percentage of participants harbored negative emotional responses such as anger, pity, fear, or disgust toward individuals with mental health problems before the presentation. Still, small but significant pre-post reductions in fear were observed, while more-substantial reductions in pity and gains across all of the positive emotional responses were observed (e.g., calm, interested, caring). To the authors' knowledge, this is one of the few studies to examine the impact of an educational presentation on the emotional reactions of high school students to someone experiencing mental health challenges.
In keeping with the goal of increasing mental health knowledge, participants exhibited significant immediate gains in their understanding of the prevalence of mental health problems, signs and symptoms of mental illness, the effectiveness of treatment, and recovery. Lack of mental health knowledge has been identified as a major barrier to help-seeking among youths (Gulliver, Griffiths, and Christensen, 2010) and has been associated with increased societal stigma and discrimination (Evans-Lacko et al., 2012; Rüsch et al., 2011). Improving mental health literacy among youth is seen as a critical step in facilitating early identification of mental illness and access to treatment (Kelly, Jorm, and Wright, 2007; Wilson, 2007).
Despite the demonstrated improvements in mental illness stigma and knowledge, similar gains were not achieved for help-seeking and support-giving intentions. Though on average, participants held relatively positive help-seeking and support-giving intentions at pre-test, these domains remained unmoved by the presentation at post-test. Given that participants started off with positive intentions, there may not have been as much room to make improvements on this front. Moreover, help-seeking and support-giving may be more challenging to influence. In a review of mental health educational interventions for youth, only five of 23 studies had assessed awareness of one's own mental health problems or help-seeking intentions (Yamaguchi, Mino, and Uddin, 2011). Of those, only two studies yielded positive outcomes, indicating a need to examine the impact of educational interventions on help-seeking. Further, of the few studies that have investigated whether interventions can enhance support provision by youth, significant positive effects have not been demonstrated (Livingston et al., 2013; Stuart, 2006). Additional study is needed to understand the extent to which educational interventions can equip youth to provide support to peers who are facing mental health challenges.
The majority of participants viewed the presentation as a good experience and more than one-half reported engaging in the experience of what it feels like to have a mental health challenge. However, participants expressed mixed views with respect to the degree to which the presentation was culturally sensitive. Only a quarter of participants rated the presentation as culturally sensitive, yet most would recommend ETS to someone of their own culture. Further study is needed to understand what aspects of ETS participants did not consider to be culturally sensitive and how this may have influenced outcomes.
Findings should be considered in light of certain study limitations. Although pre-post changes are examined, we note that these findings may in part be related to participants completing the pre-test, which may have heightened their attention to key parts of the presentation. In addition, we only examined short-term outcomes immediately after the presentation. Whether the positive shifts in stigma are maintained in the long term is unknown, and further investigation is warranted. Few studies have assessed the long-term outcomes of educational interventions among high school students, and there is some evidence that maintaining follow-up gains in knowledge and attitudes can be challenging (Yamaguchi et al., 2011). Our study examined only three ETS presentations, which further limits the findings. Results may be unique to the particular speakers or audiences involved.
Conclusion
Our findings indicate that ETS, as presented in the three school settings included within this evaluation, can result in immediate and substantial improvements in mental health knowledge, as well as in positive shifts in emotional responses and attitudes toward people with mental health challenges. ETS may be an important addition to the catalogue of programs provided by NAMI, particularly with respect to the provision of stigma reduction interventions within high school settings.
This research was conducted in RAND Health, a division of the RAND Corporation.
Notes
Permission for the ETS evaluation could only be secured from the school district and the schools included in this study within the time frame of the evaluation period.
Paired t-tests and chi-square tests were used to examine pre-post changes in mean scores and percentage of endorsement, respectively.
References
- Angermeyer, Matthias C., Holzinger Anita, and Matschinger Herbert, “Emotional Reactions to People with Mental Illness,” Epidemiologia e Psichiatria Sociale, Vol. 19, No. 1, 2010, pp. 26–32. [DOI] [PubMed] [Google Scholar]
- Chandra, Anita, and Minkovitz Cynthia S., “Stigma Starts Early: Gender Differences in Teen Willingness to Use Mental Health Services,” Journal of Adolescent Health, Vol. 38, No. 6, 2006, pp. 754.e1–754.e8. [DOI] [PubMed] [Google Scholar]
- Corrigan, Patrick W., “How Stigma Interferes with Mental Health Care,” American Psychologist, Vol. 59, No. 7, 2004, p. 614. [DOI] [PubMed] [Google Scholar]
- Corrigan, Patrick W., and Fong Mandy W. M., “Competing Perspectives on Erasing the Stigma of Illness: What Says the Dodo Bird?” Social Science & Medicine, Vol. 103, 2014, pp. 110–117. [DOI] [PubMed] [Google Scholar]
- Corrigan, Patrick W., Morris Scott B., Michaels Patrick J., Rafacz Jennifer D., and Rüsch Nicholas, “Challenging the Public Stigma of Mental Illness: A Meta-Analysis of Outcome Studies,” Psychiatric Services, Vol. 63, No. 10, 2012, pp. 963–973. [DOI] [PubMed] [Google Scholar]
- Cottrell, Catherine A, and Neuberg Steven L., “Different Emotional Reactions to Different Groups: A Sociofunctional Threat-Based Approach to Prejudice,” Journal of Personality and Social Psychology, Vol. 88, No. 5, 2005, p. 770. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko, Sara, Brohan Elaine, Mojtabai Ramin, and Thornicroft Graham, (2012). “Association Between Public Views of Mental Illness and Self-Stigma Among Individuals with Mental Illness in 14 European Countries,” Psychological Medicine, Vol. 42, No. 8, 2012, pp. 1741–1752. [DOI] [PubMed] [Google Scholar]
- Green, Melanie C., and Brock Timothy C., “The Role of Transportation in the Persuasiveness of Public Narratives,” Journal of Personality and Social Psychology, Vol. 79, No. 5, 2000, p. 701. [DOI] [PubMed] [Google Scholar]
- Gulliver, Amelia, Griffiths Kathleen M., and Christensen Helen, “Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review,” BMC Psychiatry, Vol. 10, No. 1, 2010, p. 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, Claire M., Jorm Anthony F., and Wright Annemarie, “Improving Mental Health Literacy as a Strategy to Facilitate Early Intervention for Mental Disorders,” Medical Journal of Australia, Vol. 187 (Suppl. 7), 2007, pp. S26–S30. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Berglund P., Demler O., Jin R., Merikangas K. R., and Walters E. E., “Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication,” Archives of General Psychiatry, Vol. 62, No. 6, 2005, pp. 593–602. [DOI] [PubMed] [Google Scholar]
- Link, Bruce G., Yang Lawrence H., Phelan Jo C., and Collins Pamela Y., “Measuring Mental Illness Stigma,” Schizophrenia Bulletin, Vol. 30, No. 3, 2004, pp. 511–541. [DOI] [PubMed] [Google Scholar]
- Livingston, James D., Tugwell Andrew, Korf-Uzan Kimberly, Cianfrone Michelle, and Coniglio Connie, “Evaluation of a Campaign to Improve Awareness and Attitudes of Young People Towards Mental Health Issues,” Social Psychiatry and Psychiatric Epidemiology, Vol. 48, No. 6, 2013, pp. 965–973. [DOI] [PubMed] [Google Scholar]
- Merikangas, Kathleen Ries, He Jian-ping, Burstein Marcy, Swanson Sonja A., Avenevoli Shelli, Cui Lihong, Benjet Corina, Georgiades Katholiki, and Swendsen Joel, “Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A),” Journal of the American Academy of Child and Adolescent Psychiatry, Vol. 49, No. 10, 2010, pp. 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas, Kathleen Ries, Jian-ping He, Marcy Burstein, Joel Swendsen, Shelli Avenevoli, Brady Case, Katholiki Georgiades, Leanne Heaton, Sonja Swanson, and Mark Olfson, “Service Utilization for Lifetime Mental Disorders in U.S. Adolescents: Results of the National Comorbidity Survey—Adolescent Supplement (NCS-A),” Journal of the American Academy of Child and Adolescent Psychiatry, Vol. 50, No. 1, 2011, pp. 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAMI—See National Alliance on Mental Illness.
- National Alliance on Mental Illness, NAMI Ending the Silence Presenter Manual, 2012.
- Pescosolido, Bernice A., Medina Tait R., Martin Jack K., and Scott Long J., “The ‘Backbone’ of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness,” American Journal of Public Health, Vol. 103, No. 5, 2013, pp. 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinfold, V., Stuart H., Thornicroft G., and Arboleda-Flórez J., (2005). “Working with Young People: The Impact of Mental Health Awareness Programs in Schools in the UK and Canada,” World Psychiatry, Vol. 4 (Suppl. 1), 2005, pp. 48–52. [Google Scholar]
- Pinto-Foltz, Melissa D., Cynthia Logsdon M., and Myers John A., “Feasibility, Acceptability, and Initial Efficacy of a Knowledge-Contact Program to Reduce Mental Illness Stigma and Improve Mental Health Literacy in Adolescents,” Social Science & Medicine, Vol. 72, No. 12, 2011, pp. 2011–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, A., Mubbashar M. H., Gater R., and Goldberg D., “Randomised Trial of Impact of School Mental-Health Programme in Rural Rawalpindi, Pakistan,” Lancet, Vol. 352, No. 9133, 1998, pp. 1022–1025. [DOI] [PubMed] [Google Scholar]
- Rüsch, Nicolas, Evans-Lacko Sara E., Henderson Claire, Flach Clare, and Thornicroft Graham, “Knowledge and Attitudes as Predictors of Intentions to Seek Help for and Disclose a Mental Illness,” Psychiatric Services, Vol. 62, No. 6, 2011, pp. 675–678. [DOI] [PubMed] [Google Scholar]
- Schulze, B., Richter-Werling M., Matschinger H., and Angermeyer M. C., “Crazy? So what! Effects of a School Project on Students' Attitudes Towards People with Schizophrenia,” Acta Psychiatrica Scandinavica, Vol. 107, No. 2, 2003, pp. 142–150. [DOI] [PubMed] [Google Scholar]
- Spagnolo, A. B., Murphy A. A., and Librera L. A., “Reducing Stigma by Meeting and Learning from People with Mental Illness,” Psychiatric Rehabilitation Journal, Vol. 31, No. 3, 2008, pp. 186–193. [DOI] [PubMed] [Google Scholar]
- Stuart, Heather, “Reaching Out to High School Youth: The Effectiveness of a Video-Based Antistigma Program,” Canadian Journal of Psychiatry, Vol. 51, No. 10, 2006, pp. 647. [DOI] [PubMed] [Google Scholar]
- Wahl, Otto E., “Children's Views of Mental Illness: A Review of the Literature,” Psychiatric Rehabilitation Skills, Vol. 6, No. 2, 2002, pp. 134–158. [Google Scholar]
- Watson, A. C., Miller F. E., and Lyons J. S., “Adolescent Attitudes Toward Serious Mental Illness,” The Journal of Nervous and Mental Disease, Vol. 193, No. 11, 2005, pp. 769–772. [DOI] [PubMed] [Google Scholar]
- Watson, A. C., Otey E., Westbrook A. L., Gardner A. L., Lamb T. A., Corrigan P. W., and Fenton W. S., “Changing Middle Schoolers' Attitudes About Mental Illness Through Education,” Schizophrenia Bulletin, Vol. 30, No. 3, 2004, pp. 563–572. [DOI] [PubMed] [Google Scholar]
- Wilson, Coralie J., “When and How Do Young People Seek Professional Help for Mental Health Problems?” The Medical Journal of Australia, Vol. 187 (Suppl.), 2007, pp. S35–S39. [DOI] [PubMed] [Google Scholar]
- Yamaguchi, S., Mino Y., and Uddin S., “Strategies and Future Attempts to Reduce Stigmatization and Increase Awareness of Mental Health Problems Among Young People: A Narrative Review of Educational Interventions,” Psychiatry and Clinical Neurosciences, Vol. 65, No. 5, 2011, pp. 405–415. [DOI] [PubMed] [Google Scholar]
- Yap, Marie Bee Hui, and Jorm Anthony Francis, “Young People's Mental Health First Aid Intentions and Beliefs Prospectively Predict Their Actions: Findings from an Australian National Survey of Youth,” Psychiatry Research, Vol. 196, Nos. 2–3, 2012, pp. 315–319. [DOI] [PubMed] [Google Scholar]


