Abstract
The dramatic evolution in information and communication technologies (ICTs) online and on smartphones has led to rapid innovations in behavioral health care. To assist the U.S. Air Force in developing a strategy for use of ICTs, the authors reviewed the scientific literature on their use to prevent and treat behavioral health conditions, such as major depression, posttraumatic stress disorder, and alcohol misuse. There is currently little scientific evidence supporting additional investment in ICT-based psychosocial programs for resilience or prevention of posttraumatic stress symptoms, depression, or anxiety. Instead, preventive interventions might prioritize problems of alcohol misuse and intimate partner violence. ICT applications that play a role in the treatment process may be used for patient education and activation, to improve decisionmaking by clinicians, to provide a therapy, to improve adherence to treatment, or to maintain treatment gains over time. However, partly due to the rapid pace of development of the technology, there is little or no evidence in the literature regarding the efficacy of the most recently developed types of ICTs, in particular those using smartphones. Despite the lack of solid research evidence to date, ICTs hold promise in addressing the challenges of mental health care. One promising avenue is development of reliable methods for patient-clinician communication between therapy sessions; another is Internet-based cognitive behavioral therapy. The authors recommend that the Air Force should take an incremental approach to adopting the use of ICTs—one that involves a program of measurement-based implementation and process and outcome monitoring rather than urgent dissemination.
The growth in information and communication technologies (ICTs) has led to rapid innovation in methods for providing behavioral health care, a wide field of services including prevention and treatment of both substance use and psychiatric disorders. Innovations range from updating and enhancing older technologies, such as electronic health records and telemedicine, to the thousands of mental health—related applications now available on smartphones. These innovations have created new opportunities to improve the quality of mental health care, expand access to mental health information, enable new methods for providing care, encourage patient adherence to treatment, and even reduce the stigma often associated with seeking treatment.
The challenge, however, lies in determining what functions ICTs should fill in mental health service delivery and gaining insight into the effectiveness of the many available tools. While thousands of apps are available, there is little guidance available to users or mental health professionals about which tools and programs are the most promising. A growing gap exists between the availability of ICTs and scientific evidence to inform the use of these tools in mental health service delivery. Addressing this gap is particularly important to the U.S. military in light of recent involvement in the prolonged armed conflicts in Iraq and Afghanistan and the subsequent focus on behavioral health consequences for U.S. military personnel.
ICTs may represent a strategic opportunity to improve access to mental health information and assistance. Motivated by a desire to better understand this landscape and, particularly, the research supporting the use of ICTs for providing mental health care, the U.S. Air Force Surgeon General asked RAND Project AIR FORCE to conduct a literature review about the use of ICTs to help answer the following questions:
When is their use most effective?
Do they improve the quality and effectiveness of care?
Can they improve patient adherence to treatment?
What are the costs and benefits?
What considerations must be given to incorporating these methods into military care options?
This study provides the results of that review.
RAND used a commonly referenced public health model of the clinical process for providing mental health care as an organizing construct for the use of ICTs (Figure 1). The foundation of the model is universal prevention interventions that address the entire population. Next are targeted prevention interventions that aim to reach people who are known to have a high risk of or predisposition toward mental health problems that could lead to adverse outcomes. Clinical interventions, represented by the top of the triangle, include all the treatment provided in the formal health care system to individuals with clinical conditions. RAND addressed the use of ICTs in each of these settings.
Figure 1.
Public Health Model for ICT Uses in Behavioral Health
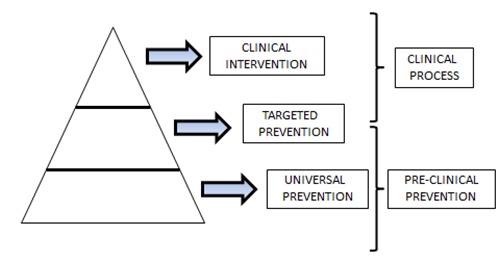
SOURCE: Adapted from Frieden, 2010.
Prevention
Prevention is a preclinical or clinical activity that involves averting some aspect of an illness before it occurs. The literature suggests potential strategies for applying ICTs to universal prevention (efforts that address the entire population without respect to individuals' preexisting level of risk, including personalized assessment of behavioral health risk factors) and targeted prevention (efforts focused on a specific at-risk group, including delivery of information tailored to individuals with particular health risks). Preventive ICTs use such new technological forms as online education, supportive therapies, the use of email or text-based communication while deployed, and smartphone or video-linked social support tools. Potential applications include depression, anxiety, posttraumatic stress symptoms (PTSS), substance misuse, and intimate partner problems.
Although the level of evidence from published and scientifically valid research trials supporting the preventive use of ICTs for these problems is scarce, some low-cost, low-risk opportunities exist. Education efforts are generally seen as a public good, and the demand for efficacy and safety data is low. Efforts to use the Internet, smartphone apps, and similar technologies to increase Air Force and family member understanding of mental health issues and reduce the mystery and stigma that surround them are responsible and well advised, but these efforts should be considered in light of the resources needed to sustain them. There is currently little scientific evidence supporting additional investment in ICT-based psychosocial programs for resilience or prevention of PTSS, depression, or anxiety. Instead, preventive interventions might prioritize problems of alcohol misuse and intimate partner violence (IPV). Given the unique features and needs of the Air Force population, any effort to implement preventive behavioral health ICTs will necessitate ongoing monitoring of program safety and effectiveness.
Clinical Treatment
The clinical process begins with the initial contact between a patient and a care provider. ICT interventions associated with the clinical process may be used for patient education and activation, to improve decisionmaking by clinicians, to provide a therapy, to improve adherence to treatment, or to maintain treatment gains over time. ICT applications that can be used to support the clinical process occupy a rapidly changing area of technology development, and research on the efficacy of specific ICT applications cannot keep up with their evolution. The literature is vast, but much of it is descriptive or based on uncontrolled observational studies, making it difficult to draw conclusions regarding how these tools might best be used.
Despite the lack of solid research evidence to date, ICTs hold promise in addressing the challenges of mental health care. ICTs offer an advance in convenience for providers and clinicians, which can be advantageous in the military, with its frequent moves and inflexible schedules. One promising avenue is development of reliable methods for patient-clinician communication between therapy sessions; another is Internet-based cognitive behavioral therapy. Even if off-the-shelf products are not available, the success described in the literature suggests that these should be priority target areas for Air Force efforts. How ICT applications developed for particular target populations might translate into a military environment is an area that will need further investigation and should be one component in developing an ICT implementation strategy. Cost trade-offs are another area that needs further study within the military community to determine what level of use justifies the investment.
Recommendations
ICTs offer a wide range of innovative techniques designed to improve access to behavioral health care and to improve the quality of care that is delivered. The evidence to date on effectiveness and efficiency of use is vast but uneven, and how these research results apply to the population of airmen in the U.S. Air Force is unclear. Much of the research focuses on the use of ICTs to extend services to individuals already in clinical treatment. Yet this research offers little insight into how those tools might scale up for use in preventive care that is targeted toward a far larger population. For this larger population, the available research is much more limited and fails to address such important concerns as safety, adverse effects, and inconsistent results. Furthermore, there is little or no evidence in the literature regarding the efficacy of some of the most recently developed types of ICTs, in particular those using smartphones.
Despite its limitations, the literature does offer constructive lessons and opportunities that can inform the development of a responsible strategy for implementing behavioral health ICTs. Our recommendations focus on ICT strategies for the Air Force rather than specific applications that can be immediately put into place. In our judgment, the Air Force should take an incremental approach to adopting the use of these tools—one that involves a program of measurement-based implementation and process and outcome monitoring rather than urgent dissemination. The most significant concerns surrounding a more aggressive approach to implementation are efficient use of resources and the safety, privacy, and applicability of existing behavioral health ICTs in the Air Force.
General Recommendations
We offer a number of general recommendations toward developing an effective Air Force strategy:
The Air Force should develop and adopt a coordinated interdisciplinary strategy for behavioral health ICT implementation. Just as important as the question of which ICTs should be used and how and where to use them is the strategy employed for managing emerging health technologies. In developing this strategy, the Air Force should work with an interdisciplinary mix of professionals with behavioral health, public health, information technology, mental health measurement, and health communications expertise.
The Air Force should develop standards and objectives for adapting ICTs to the unique Air Force context and implement a method for determining when the standard has been met before fielding a given ICT. Most available tools have been tested in a nonmilitary setting. Field testing in a military environment will be needed to reduce unintended organizational and health consequences and maximize benefits for the intended populations and individuals.
Air Force behavioral health ICTs should be designed for monitoring aggregate use and intervention outcomes, including adverse or unintended effects. An advantage of ICTs, apart from their potential to improve health and prevent health problems, is the potential for transparent, built-in measurement features. Behavioral health ICTs are medical devices. In a manner consistent with continuous quality improvement programs in the clinical service delivery domain, establishing the ongoing safety and effectiveness of these ICT-based programs of care is necessary for ongoing, responsible use.
The study also details a number of specific recommendations regarding the use of ICTs in the prevention and treatment of behavioral health problems.
Prevention Recommendations
If the Air Force introduces ICTs for prevention, it should review existing ICTs provided to airmen across the Department of Defense (DoD), the services, and supporting private organizations to harmonize efforts with existing programs. There are ongoing efforts in a variety of military, governmental, and private sources. The potential for duplication of efforts is great without careful ongoing review, particularly because there is no comprehensive, up-to-date list of preventive behavioral health programs or ICTs.
The Air Force should seek and collate aggregate search engine data from Air Force and DoD websites aiming to provide preventive assistance to airmen and families. Search terms may be a simple, low-cost way of identifying the interests and needs of the Air Force population and enhancing web-based information resources for airmen and their families.
The Air Force should not use ICTs for the purpose of targeting traumatized units or individuals for “critical incident stress debriefings” or “psychological debriefings.” Extensive research relating to interventions to prevent PTSS and posttraumatic stress disorder (PTSD) is clear. These interventions, particularly when mandated, do not prevent PTSS symptoms, and there is no evidence to suggest that currently available technologies offer a new way forward in this preventive area.
The Air Force should consider adapting and implementing ICTs offering Internet-based, personalized single-session feedback for airmen at identified risk for future alcohol-related incidents. Alcohol misuse is a common problem in the military and a major factor in IPV and preventable and fatal injuries, including suicide. The Internet offers low-cost opportunities to deliver this preventive intervention in ways that are accountable and assess for general effectiveness.
The Air Force should consider the use of ICTs for universal and targeted prevention efforts relating to IPV. About half of airmen are married, and a much larger proportion are involved in intimate partner relationships. At least one universal preventive ICT approach, ePREP, is well studied and effective for preventing IPV.
Clinical Treatment Recommendations
The Air Force should adopt an Internet-based treatment program for depression and anxiety, tailored to the needs of the Air Force population. An Internet-based cognitive behavioral therapy program could fill a niche in the mental health care delivery system by providing a treatment option for airmen who are remote from treatment, highly mobile, or concerned about the stigma of attending a mental health clinic. Procedures for guaranteeing confidentiality of treatment, particularly if treatment enables patient-physician contact via smartphone, should be in place prior to the introduction of new Internet-based treatment programs.
The Air Force should monitor the future development of Internet-based treatments for substance misuse. Although no off-the-shelf programs in this area offer proven efficacy, there are a number of promising recently developed programs, such as brief interventions for alcohol misuse, that could prove valuable to the Air Force.
The Air Force should select smartphone apps that airmen can use to monitor their medication use and communicate with mental health clinicians between in-person visits. For both of these functions, evidence suggests that smartphone apps provide effective tools that make adherence to treatment more convenient. Given the large number of apps currently available, the selection of specific apps will require an extensive review of existing options and particular attention to the ability of clinicians to ensure the confidentiality of treatment-related information for their patients.
The rapidly changing field of ICT applications for mental health care promises to improve treatment systems in ways that address long-standing problems in both the civilian and military service systems. However, very few ICT applications have moved from promising to proven technologies. Only a small handful of ICT applications, notably those designed for Internet cognitive behavioral therapy, are supported by evidence-based research. Nonetheless, other ICTs appear to be promising based on the convenience and efficiency they add to established evidence-based treatments and evidence of their acceptability to patients and providers. Over time, the research literature and clinical experience with ICTs will grow, and consensus will form on which ICT applications are of greatest benefit to patients.
Footnotes
The research reported here was sponsored by the Air Force Surgeon General and conducted within the Manpower, Personnel, and Training and Program of RAND Project AIR FORCE.
Reference
- Frieden, T. R., “A Framework for Public Health Action: The Health Impact Pyramid,” American Journal of Public Health, Vol. 100, No. 4, 2010, pp. 590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]


