Abstract
Objectives
To characterize factors contributing to physical resilience in older cancer survivors, as demonstrated by resistance to decline or recovery (resilience).
Materials and Methods
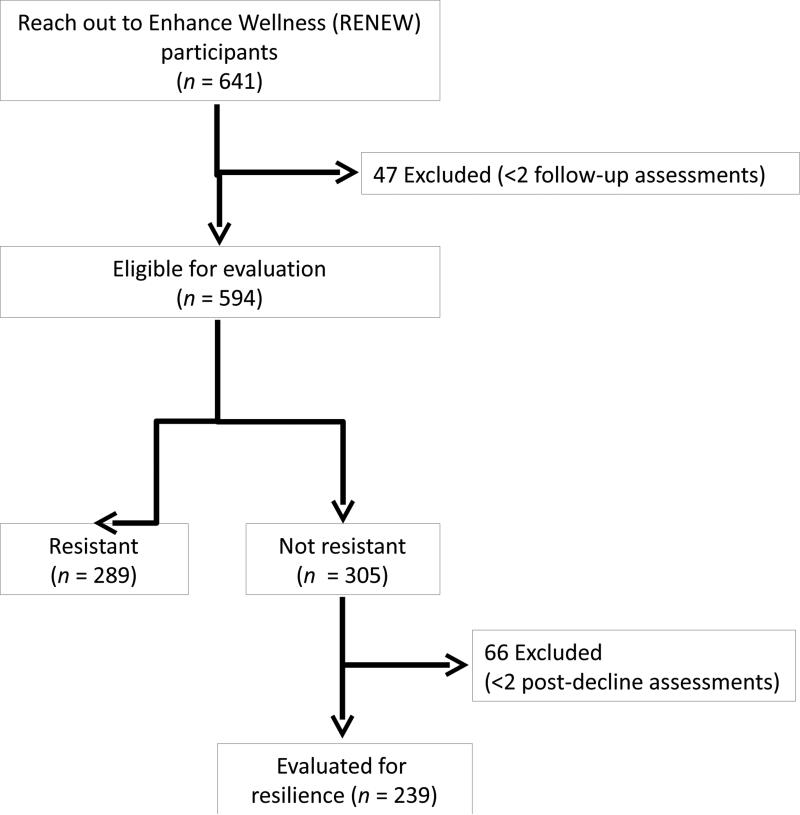
We conducted a secondary analysis of data from a randomized controlled trial of cancer survivors ≥ 65 years old and ≥ 5 years from cancer diagnoses. Physical function was assessed quarterly over 2 years, with Short-Form 36 physical function subscale. Participants with ≥ 2 follow-up assessments (n=594) were evaluated for physical resilience: 1) Resistance was defined as lack of any decline, where decline was a drop of ≥ 13 points, and 2) resilience (i.e., recovery) was defined as regaining ≥ 50% of lost function, subsequent to decline.
Results
Mean age was 73.1 years and 89.1% were Caucasian. Forty-nine percent (n=289) were resistant to decline in function; these individuals were younger, had higher education and income, were more likely to be Caucasian, and had higher baseline physical function (mean difference [MD] 7.8 points, 95% CI 5.0-10.8) and general health (MD 7.5 points, 95% CI 4.9-10.1). Fifty-seven percent (n=137 of 239) demonstrated resilience, with 91.2% (n=125) recovering within 6 months of declines; these participants had higher baseline physical function (MD 6.6 points, 95% CI 1.8-11.4), but similar pre-decline function. More participants who were resistant, and more who showed resilience, reported high self-efficacy and social support.
Conclusions
The majority of older cancer survivors exhibited physical resilience; this was associated with high baseline health, physical function, self-efficacy, and social support. Assessing and targeting psychosocial factors may be important for interventions seeking to promote physical resilience.
Keywords: physical resilience, functional decline, resistance, recovery, cancer survivors
INTRODUCTION
There are currently over 8 million U.S. cancer survivors who are 65 years or older, and this population is increasing rapidly, given aging of the population, higher incidence of cancer among older individuals, and improved overall survival (1–3). The National Cancer Institute and the Institute of Medicine have declared that improving oncology care for older adults is a national priority; in particular, we need to more robustly address functional outcomes and quality of life during and after oncology interventions (1–3). Physical resilience is an emerging concept that addresses the person-level ability to resist or recover from new declines in physical function (4). Greater understanding of factors contributing to physical resilience among older adults could enable efforts to improve function and health for older cancer survivors. In a recent systematic review, we found few studies that explicitly evaluated physical resilience (4).
Previous work has shown that older adults generally demonstrate substantial variation in overall trajectories of physical function and health, in addition to important fluctuations over time for each individual (5–7). While many older individuals experience episodes of functional disability, these are often followed by recovery (8,9). Factors associated with recovery have included baseline cognitive function, physical activity and function, chronic health conditions, and sensory impairments (8–10). For older cancer survivors, it is unknown whether similar patterns of decline and recovery occur, or if similar factors are associated with resistance to decline or recovery. Cancer survivors have lower general health and physical functioning than those without a history of cancer (11–13), and thus, cancer survivors may have decreased capacity to resist further functional decline, or recover after new declines. Moreover, considering the history of severe illness and often complex treatments experienced by older cancer survivors, factors important for physical resilience in the general older population may be more or less relevant for this at-risk group.
In order to address these important questions, we conducted a secondary analysis of data collected over a 2-year period in the Reach out to Enhance Wellness (RENEW) study, a randomized controlled trial aimed at improving physical function in older, overweight and obese cancer survivors (14,15). Primary RENEW study results have been published, showing that the diet and exercise intervention successfully reduced the decrease in physical function at 12 months, compared with wait-listed controls (14). First, we determined which RENEW participants were resistant to decline (i.e. lacked any new, meaningful declines) as measured by the 36-item Medical Outcomes Study Short-Form (SF36) physical function subscale. We compared pertinent characteristics between individuals who were resistant vs. those who exhibited declines. Then, we looked for resilience among those who had declined, and summarized key characteristics for those who were resilient, compared to those who were not.
MATERIALS AND METHODS
Study Design and Participants
RENEW was conducted from July 1, 2005 through May 17, 2007, and tested a set of behavioral interventions to improve diet and exercise for overweight and obese cancer survivors, 65 years or older, and a minimum of 5 years out from their cancer diagnoses (prostate, breast, or colorectal); detailed study protocol and eligibility criteria have been published elsewhere (14,15). Briefly, the behavioral intervention was delivered over 12 months and consisted of 15 telephone-based counseling sessions, automated telephone prompts, and personalized workbooks and newsletters. Participants were randomized to intervention (n=319) or wait-listed control (n=322), with control individuals receiving the intervention during the second year. The original primary outcome was self-reported physical function at 12 months, as assessed by the SF36 physical function subscale and self-reported lower extremity functioning. During the 2-year period, all study participants were assessed every 3 months for physical function, self-efficacy for diet and exercise (both endurance and strength), and self-reported physical activity.
In order to have sufficient data to evaluate physical resilience, we selected participants who had a minimum of 2 follow-up assessments for examining resistance, and at least 2 follow-up assessments post-decline (see decline definition below) for recovery.
Ethical Approval
All study procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The RENEW study was approved by all participating institutional review boards and informed consent was obtained from all individual participants in RENEW.
Resistance to Decline and Resilience
We first examined resistance to decline in function by determining which participants had no decline during the follow-up period, using the SF36 physical function subscale. The SF36 is a previously validated and widely employed instrument for measuring health and quality of life; it has established mental health and physical function components (16,17). We calculated the difference between SF36 physical function scores and the average of 2 preceding consecutive assessments, and set a minimum threshold of 13 points for meaningful decline. Previous work has shown that a change of 6.5 points in SF36 physical function scores to be clinically relevant (17); thus, in order to increase the likelihood of capturing important new changes in physical function, rather than random variability, we set the required minimum change to be twice this minimally clinically important difference. The change in SF36 function meeting this threshold is termed the “decline amount,” and the average of 2 preceding assessments, the “pre-decline function.”
Next, we evaluated participants who had declines, in order to determine if they recovered, thus demonstrating resilience. To identify stable and clinically meaningful recovery, we required that participants regain 50% or more of the decline amount, on at least 2 consecutive post-decline assessments. For those who demonstrated resilience, we also evaluated who had complete recovery (i.e., regaining at least 90% of the decline amount), compared with partial recovery (i.e., 50-89% of the decline).
Participant Characteristics
Complete descriptions of RENEW study measurements have been published elsewhere (14,15). Briefly, baseline characteristics included age, sex, race, educational status, annual income, years since cancer was first diagnosed, a variety of medical conditions and symptoms, body mass index (kg/m2) and current smoking. Complete SF36 responses were also obtained at baseline and yearly, providing mental health and general health scores, in addition to physical function. Baseline and follow-up self-efficacy for exercise were measured with 2 questions: “How sure are you that you could do exercises to make your legs stronger for 15 minutes, 3 days a week?” and “How sure are you that you could walk or do another type of endurance exercise for 30 minutes, 5 or more days a week?”; the 5 response categories ranged from “Very Sure” to “Very Unsure.” Social support for exercise was assessed with the question “To what extent would your friends and family support your efforts to increase your amount of exercise?” and 5 response categories ranging from “Not at all” to “Extremely.” Hospitalizations and diagnoses of cancer, whether new or recurrences, were reported by participants at quarterly assessments for adverse events.
Statistical Analyses
After determining who were resistant to decline and who were resilient, we performed bivariate comparisons of participant characteristics. We used 2-sample t-tests to compare these groups on continuously measured data (e.g., age and SF36 scores) and symptom counts. For categorical data, we employed χ2 tests of homogeneity for unordered categories (e.g., sex, race, and types of cancer diagnosed) and Cochran-Armitage tests for trend for ordinal categories (e.g., annual income and self-efficacy for exercise). We defined statistical significance as p-value less than 0.05, from 2-tailed tests. All analyses were performed in R version 3.0.2.
RESULTS
Overall, 594 (92.7% of total trial participants, see Figure) were eligible for evaluation of resistance to functional decline and resilience, with most (n=472, 76.1%) having complete follow-up over the 2-year study period. Our study sample had a mean age of 73.1 years (SD=5.1), were mostly Caucasian (n=529, 89.1%) and were on average 8.6 years (SD=2.7) from their cancer diagnosis, consistent with previously reported data for the total RENEW cohort (14). About half of participants were resistant to functional decline during study follow-up, and these individuals were significantly younger, had higher educational attainment and annual income, and were more likely to be Caucasian (Table 1). Additionally, participants who were resistant to decline had better health at baseline, with significantly higher physical function (mean difference [MD] 7.8 points, 95% CI 5.0-10.8) and general health (MD 7.5 points, 95% CI 4.9-10.1), and lower symptom counts (MD 1.5, 95% CI 0.9-2.0, Table 1). Also, individuals who were resistant had significantly lower prevalence of cardiovascular conditions, including hypertension (47.4% vs. 60.3%, p=0.002) and peripheral circulation problems (22.5% vs. 34.8%, p=0.001). There were no statistically significant differences in types of cancer diagnoses or years since cancer diagnosis. When we examined types of cancer therapy, fewer of those who were resistant had received radiation therapy (37.7% vs. 51.8%, p <0.001), whereas there were no differences in proportions of participants who had received chemotherapy or underwent surgery. There were no significant differences in self-reported diagnoses of cancer during follow-up (4.3% among those who were resistant vs. 2.8% of those who were not, p=0.32). Participants who were resistant also reported higher baseline self-efficacy and social support for exercise (p-values 0.008 for endurance exercise self-efficacy, 0.003 for strength exercise self-efficacy, and <0.001 for social support, see Table 1). A small proportion of those who were not resistant (i.e., had new declines) reported hospitalizations during the period spanning 6 months before and 1 month after the observed decline (n=34, 11.1%). Additionally, among those who were not resistant, nearly half (n=146, 47.9%) experienced declines while they were actively receiving RENEW study interventions to promote physical activity.
Figure.
Selection of Participants for Evaluation of Physical Resilience.
Table 1.
Characteristics of Participants Who were Resistant to Decline or Not
| Characteristics | Resistanta (n=289) | Not Resistanta (n=305) | p-valueb |
|---|---|---|---|
| Physical function | |||
| Baseline SF36 physical function, mean (SD) | 80.2 (17.8) | 72.4 (18.3) | <0.001 |
| Pre-decline physical functionc, mean (SD) | — | 75.1 (16.3) | — |
| Amount of decline in physical function, mean (SD) | — | 26.4 (13.8) | — |
| Time at decline, mean (SD), mo | — | 12.8 (5.7) | — |
| Demographics | |||
| Age, mean (SD), y | 72.6 (5.0) | 73.6 (5.1) | 0.02 |
| Female, No. (%) | 149 (51.6) | 173 (56.7) | 0.24 |
| Caucasian, No. (%) | 271 (93.8) | 258 (84.6) | <0.001 |
| Education, No. (%): | |||
| High school degree | 63 (21.8) | 88 (28.9) | |
| Vocational or some college | 98 (33.9) | 78 (25.6) | 0.04 |
| College degree or above | 111 (38.4) | 112 (36.7) | |
| Annual income, No. (%)d: | |||
| < $12,500 | 6 (2.1) | 16 (5.2) | |
| $12,500 - $30,000 | 69 (23.9) | 92 (30.2) | 0.006 |
| $30,001- $49,999 | 79 (27.3) | 80 (26.2) | |
| ≥ $50,000 | 108 (37.4) | 92 (30.2) | |
| Health | |||
| Baseline SF36 general health, mean (SD) | 76.2 (15.7) | 68.7 (16.4) | <0.001 |
| Baseline SF36 mental health, mean (SD) | 87.4 (10.0) | 85.2 (12.6) | 0.02 |
| Symptom count, mean (SD) | 3.6 (2.9) | 5.1 (3.5) | <0.001 |
| Body mass index, mean (SD), kg/m2 | 28.7 (3.4) | 29.5 (3.5) | 0.007 |
| Years since cancer diagnosis, mean (SD) | 8.7 (2.6) | 8.6 (2.8) | 0.816 |
| Cancer treatment, No. (%): | |||
| Chemotherapy | 70 (24.2) | 86 (28.2) | 0.31 |
| Radiation | 109 (37.7) | 158 (51.8) | <0.001 |
| Surgery | 258 (89.3) | 271 (88.9) | 0.97 |
| Smoking, No. (%) | 18 (6.2) | 14 (4.6) | 0.48 |
| Psychosocial factors | |||
| Baseline self-efficacy for strength exercise, No. (%): | |||
| Very sure or sure | 240 (83.0) | 225 (73.8) | |
| Somewhat sure | 38 (13.1) | 59 (19.3) | 0.003 |
| Unsure or very unsure | 11 (3.8) | 21 (6.9) | |
| Baseline self-efficacy for endurance exercise, No. (%): | |||
| Very sure or sure | 215 (74.4) | 191 (62.6) | |
| Somewhat sure | 40 (13.8) | 65 (21.3) | 0.008 |
| Unsure or very unsure | 34 (11.8) | 49 (16.1) | |
| Baseline social support for exercise, No. (%) | |||
| Very much or extremely | 238 (82.4) | 214 (70.2) | |
| Somewhat | 37 (12.8) | 64 (21.0) | <0.001 |
| Not at all or a little | 14 (4.8) | 26 (8.5) |
Abbreviations: SF36 = Medical Outcomes Study Short-Form 36 Survey
Resistant participants had no declines, where decline was defined as a minimum drop of 13 points from average physical function during 2 preceding assessments.
Comparison of characteristics between “Resistant” and “Not Resistant” groups. As appropriate, we used t-test, χ2 test (for unordered categorical data), or Cochran- Armitage test for trend (for ordered categorical data).
Average of physical function scores observed at 2 assessments immediately preceding decline.
Overall, 52 (8.7%) of participants had missing data for annual income--27 (9.3%) among those who were resistant and 25 (8.2%) for those who were not.
Of 305 participants who declined in function, 239 (78.4%, see Figure) had 2 or more post-decline assessments and thus, could be evaluated for resilience. Overall, the mean age was 73.7 years (SD=5.2) and 83.9% (n=202) were Caucasian. More than half recovered, and among these, 91.3% (n=115) did so within 6 months. There were no significant differences in age, race, education or income (Table 2). Those who showed resilience had higher physical function (MD 6.6 points, 95% CI 1.8-11.4) and lower symptom counts (MD 1.1, 95% CI 0.2-2.1) at baseline. They were also further out from their original cancer diagnoses (MD 0.7 years, 95% CI 0.01-1.4). However, baseline general and mental health, as well as pre-decline function, were similar between those who showed resilience vs. those who did not (Table 2). There were also no differences in chronic medical conditions, original cancer diagnoses, or types of therapy received. Interestingly, those who exhibited resilience had larger decline amounts (MD 4.5 points, 95% CI 1.1-7.9). Similar proportions of those who showed resilience vs. not were receiving the behavioral intervention at the time of decline in physical function (43.1% vs. 51.0%, p=0.26). Notably, among individuals who demonstrated resilience, a greater proportion had high baseline self-efficacy for endurance exercise and high social support (Table 2). Forty-one percent (n=56) had complete recovery (i.e., regained at least 90% of decline amount), and we found no significant differences in characteristics between these individuals and those with partial recoveries.
Table 2.
Characteristics of Participants who were Resilient or Not
| Characteristics | Resilienta (n=137) | Not Resilienta (n=102) | p-valueb |
|---|---|---|---|
| Physical function and recovery | |||
| Baseline SF36 physical function, mean (SD) | 74.5 (16.9) | 67.9 (19.8) | 0.01 |
| Pre-decline physical functionc, mean (SD) | 76.1 (17.3) | 72.7 (16.1) | 0.11 |
| Amount of decline in physical function, mean (SD) | 28.9 (16.0) | 24.4 (10.7) | 0.01 |
| Time at decline, mean (SD), mo | 10.6 (3.9) | 11.4 (4.3) | 0.17 |
| Recovered physical functiond, mean (SD) | 25.3 (15.0) | — | — |
| Time to recovery, No. (%): | |||
| 3 months | 106 (77.4) | — | — |
| 6 months | 19 (13.9) | — | — |
| 9 or more months | 12 (8.8) | — | — |
| Sociodemographics | |||
| Age, mean (SD), y | 73.3 (5.1) | 74.3 (5.3) | 0.15 |
| Female, No. (%) | 83 (60.6) | 58 (56.9) | 0.66 |
| Caucasian, No. (%) | 117 (85.4) | 85 (83.3) | 0.80 |
| Education, No. (%): | |||
| High school degree | 42 (29.1) | 23 (22.5) | |
| Vocational or some college | 36 (26.3) | 27 (26.5) | 0.54 |
| College degree or above | 48 (35.0) | 40 (39.2) | |
| Annual income, No. (%)e: | |||
| < $12,500 | 5 (3.6) | 7 (6.9) | |
| $12,500 - $30,000 | 51 (37.2) | 26 (25.5) | 0.50 |
| $30,001- $49,999 | 32 (24.4) | 29 (28.4) | |
| ≥ $50,000 | 38 (27.7) | 31 (30.4) | |
| Health | |||
| Baseline SF36 general health, mean (SD) | 69.5 (15.8) | 68.0 (17.0) | 0.38 |
| Baseline SF36 mental health, mean (SD) | 86.7 (11.5) | 83.4 (14.2) | 0.08 |
| Symptom count, mean (SD) | 4.9 (3.4) | 6.4 (3.9) | 0.02 |
| Body mass index, mean (SD), kg/m2 | 29.1 (3.4) | 29.9 (3.7) | 0.13 |
| Years since cancer diagnosis, mean (SD) | 8.4 (2.9) | 9.2 (2.6) | 0.047 |
| Cancer treatment, No. (%): | |||
| Chemotherapy | 43 (31.4) | 31 (30.4) | 0.98 |
| Radiation | 123 (89.8) | 90 (88.2) | 0.16 |
| Surgery | 77 (56.2) | 47 (46.1) | 0.87 |
| Smoking, No. (%) | 8 (5.8) | 5 (4.9) | 0.98 |
| Psychosocial factors | |||
| Baseline self-efficacy for strength exercise, No. (%): | |||
| Very sure or sure | 107 (78.1) | 68 (66.7) | |
| Somewhat sure | 20 (14.6) | 26 (25.5) | 0.10 |
| Unsure or very unsure | 10 (7.3) | 8 (7.8) | |
| Baseline self-efficacy for endurance exercise, No. (%): | |||
| Very sure or sure | 95 (69.3) | 55 (53.9) | |
| Somewhat sure | 25 (18.2) | 25 (24.5) | 0.04 |
| Unsure or very unsure | 17 (12.4) | 22 (21.6) | |
| Baseline social support for exercise, No. (%): | |||
| Very much or extremely | 104 (75.9) | 67 (65.7) | |
| Somewhat | 27 (19.7) | 22 (21.6) | 0.048 |
| Not at all or a little | 6 (4.4) | 12 (11.8) |
Abbreviations: SF36 = Medical Outcomes Study Short-Form 36 Survey
Resilient participants recovered after declines. Recovery was defined as regaining at least 50% of physical function lost during decline, and minimum recovery was observed on at least 2 consecutive assessments.
Comparison of characteristics between “Resilient” and “Not Resilient” groups. As appropriate, we used t-test, χ2 test (for unordered categorical data), or Cochran-Armitage test for trend (for ordered categorical data).
Average of physical function scores observed at 2 assessments immediately preceding decline.
Difference between function at decline and average of physical function scores meeting recovery criteria.
Among those assessed for recovery, 20 (8.3%) had missing data for annual income--11 (8.0%) among those who were resilient and 9 (8.8%) for those who were not.
DISCUSSION
In this analysis of data from the RENEW trial, we examined physical resilience, a newly emerging concept. Our findings show that within a 2-year period, a majority of this at-risk group demonstrated resistance to functional decline or resilience. Moreover, most of those showing resilience recovered within 6 months of their decline. While socio-demographic differences, such as race, education, and income, were significantly different for those who were resistant vs. not, these factors were not different for those who exhibited resilience vs. not. Baseline physical function and general health were higher, while symptom counts were lower, among those who were resistant. Baseline physical function also was higher and symptom counts lower among those who showed resilience. In accordance with our prior work, we separately considered resistance to functional decline and resilience because these could represent distinct processes within physical resilience as a whole (4), and our results here indicate that different factors may indeed contribute to maintaining vs. recovering physical function.
In our sample of older cancer survivors, we observed a substantial number of new clinically meaningful declines in physical functioning, along with high rates of clinically meaningful recovery, both consistent with previously published work for older, community-dwelling adults, that examined trajectories of new disability (i.e., dependency in activities of daily living) and recovery (8,9). Although we used a continuous score of general physical function, we observed fairly large changes during decline and recovery, which likely corresponded with changes in ability to perform self-care tasks. Interestingly, we also found that the average decline was higher for those who were resilient. It is unclear why those who exhibited resilience would have experienced greater declines in function; perhaps these changes were due to more acute stressors that also permitted greater opportunity for resolution and recovery. Or, maybe large declines in function were associated with quicker detection by family and healthcare providers, leading to more rapid help and treatment. Notably, a very small proportion of those who experienced declines reported hospitalizations, and there were no significant differences in the proportion who had been hospitalized between those who showed resilience vs. not. Thus, these results indicate that the RENEW cohort of older cancer survivors seemed able to successfully manage important declines in physical function without hospitalization.
Key characteristics that appeared important for both resistance and resilience included baseline physical function, symptom count, and psychosocial factors. These results are consistent with previous work showing that poorer physical performance and more disability at baseline were predictive of risk for decline and lack of or delayed recovery in the general population (8,9,18). In contrast, the relevance of psychosocial factors, such as self-efficacy and social support, has been less clear, particularly for predicting future functional outcomes. Some groups have reported that high self-efficacy and social support were associated with higher self-reported physical resilience, but resilience was assessed through recall of past responses to acute health stressors (19,20). On the other hand, studies that prospectively evaluated functional trajectories have not found consistent relationships between psychosocial factors and physical function (21,22). For example, Seeman et al. (21) examined changes in physical performance over 2.5 years for individuals with a variety of medical conditions, and found that social support was significantly associated with performance only for those with cardiovascular disease. In another study, Kempen et al. (22) evaluated difficulty with activities of daily living at 8 weeks, 5 and 12 months after fractures, and showed that social support was not significantly associated with recovery at any time-point, whereas general self-efficacy was associated with recovery at 8 weeks. Thus, our results lend support to the importance of social support and self-efficacy, by demonstrating their association with resistance and recovery for another group of at-risk older adults.
In addition to being associated with physical resilience and future functional outcomes, self-efficacy and social support may be important for understanding who is more likely to adopt new behaviors that would promote resilience. For at-risk individuals with low self-efficacy and/or social support, we may need targeted interventions for patient engagement and activation (23,24), promoting both self-confidence for adopting new behaviors and greater connection with community resources or other sources of support. There is some evidence that self-efficacy mediates the effect of physical activity on preserving physical function, and thus, may affect outcomes from clinical interventions focused on function and recovery (25). Therefore, interventions to improve self-efficacy and social support for exercise may offer opportunities for promoting physical resilience in older cancer survivors. In summary, improved understanding of the roles of self-efficacy and social support could help us to both predict who has higher risk for poor functional outcomes, and better match interventions to individual needs and strengths.
We also observed that characteristics associated with disadvantaged groups (i.e., Caucasian vs. minority race, education, and income) appeared relevant for resistance among older cancer survivors, but did not differ between those who showed resilience vs. not. While racial differences in risk for new disability were not identified in the general older adult population (8,9), more years of education had been previously associated with decreased risk for decline (8,26). It is possible that socioeconomic status preferentially affects one's risk for adverse events, but sufficient social support and community resources may promote recovery even for disadvantaged individuals. Indeed, our findings that self-efficacy and social support were higher for both those who demonstrated resistance and those with resilience, suggest that psychosocial resources may remain relevant for physical resilience among those who are at greater risk for decline.
There are several limitations to our study. First, physical functioning and health data, including hospitalizations, were self-reported. Second, our evaluation of resilience was limited to those participants who had available follow-up after their declines. Nearly 80% of those who declined had data for evaluation of recovery, but the 20% who had missing data may have been in worse (or better) health, thus biasing our results. However, both the proportion who recovered and the timing of recovery are consistent with previous results for the general population (8,9), thus minimizing concern for potential bias. Additionally, our sample was fairly high functioning, as demonstrated by overall high baseline SF36 scores for physical function, mental health, and general health. Furthermore, because RENEW participants were in relatively good health and an average of 8.6 years after their cancer diagnoses, these individuals probably had high physical functioning before (and perhaps after) their cancer treatments, although these data were not available. Thus, our study sample may be biased towards more resilient older cancer survivors. RENEW participants were also sufficiently motivated and concerned to enroll in a randomized trial for improving physical function. It is unclear if similar results would be found for those with poorer health or functioning after cancer treatments, or those with less motivation.
Despite these limitations, our results as a whole indicate that older cancer survivors have high physical resilience, with nearly half being resistant to declines over 2 years of follow-up, and the vast majority of those who declined demonstrating subsequent recovery. Future work is needed to address whether factors which appear to contribute to physical resilience (e.g., self-efficacy and social support) could be targeted for interventions that would enhance physical resilience among aging cancer survivors.
ACKNOWLEDGMENTS
Support for Wei Duan-Porter was provided by grant No. TPM 21-022 from the Department of Veteran Affairs Office of Academic Affiliations. The RENEW trial was supported by the National Institutes of Health grants CA106919 and P30AG028716. The sponsors had no role in any aspect of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHOR CONTRIBUTIONS
Study Concept: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, R Sloane, JF Pendergast, DC Snyder, MC Morey
Study Design: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, R Sloane, JF Pendergast, DC Snyder, MC Morey
Data Acquisition: R Sloane, W Demark-Wahnefried, DC Snyder, HJ Cohen, MC Morey
Quality Control of Data and Algorithms: W Duan-Porter, R Sloane, JF Pendergast
Data Analysis and Interpretation: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, R Sloane, JF Pendergast, DC Snyder, and MC Morey
Statistical Analysis: W Duan-Porter, R Sloane, JF Pendergast
Manuscript Preparation: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, MC Morey
Manuscript Editing: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, R Sloane, JF Pendergast, DC Snyder, MC Morey
Manuscript Review: W Duan-Porter, HJ Cohen, W Demark- Wahnefried, R Sloane, JF Pendergast, DC Snyder, MC Morey
DISCLOSURES AND CONFLICT OF INTEREST STATEMENTS
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis [Internet] Institute of Medicine; [2014 Dec 2]. Available from: http://www.iom.edu/Reports/2013/Delivering-High-Quality-Cancer-Care-Charting-a-New-Course-for-a-System-in-Crisis.aspx. [Google Scholar]
- 2.Hurria A, Naylor M, Cohen HJ. Improving the quality of cancer care in an aging population: recommendations from an IOM report. JAMA. 2013 Nov 6;310(17):1795–6. doi: 10.1001/jama.2013.280416. [DOI] [PubMed] [Google Scholar]
- 3.Hurria A, Dale W, Mooney M, Rowland JH, Ballman KV, Cohen HJ, et al. Designing therapeutic clinical trials for older and frail adults with cancer: U13 conference recommendations. J Clin Oncol. 2014 Aug 20;32(24):2587–94. doi: 10.1200/JCO.2013.55.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, Colón-Emeric CS. Physical Resilience in Older Adults: Systematic Review and Development of an Emerging Construct. J Gerontol A Biol Sci Med Sci. 2016 Apr;71(4):489–95. doi: 10.1093/gerona/glv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkman LF, Seeman TE, Albert M, Blazer D, Kahn R, Mohs R, et al. High, usual and impaired functioning in community-dwelling older men and women: findings from the MacArthur Foundation Research Network on Successful Aging. J Clin Epidemiol. 1993 Oct;46(10):1129–40. doi: 10.1016/0895-4356(93)90112-e. [DOI] [PubMed] [Google Scholar]
- 6.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006 Jan;14(1):6–20. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- 7.Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: the Health and Retirement Study. J Am Geriatr Soc. 2009 Mar;57(3):511–6. doi: 10.1111/j.1532-5415.2008.02150.x. [DOI] [PubMed] [Google Scholar]
- 8.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004 Apr 7;291(13):1596–602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 9.Gill TM. Disentangling the disabling process: insights from the precipitating events project. Gerontologist. 2014 Aug;54(4):533–49. doi: 10.1093/geront/gnu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012 Jan 17;156(2):131–40. doi: 10.1059/0003-4819-156-2-201201170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003 Jan 1;58(1):M82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 12.Baker F, Haffer SC, Denniston M. Health-related quality of life of cancer and noncancer patients in Medicare managed care. Cancer. 2003 Feb 1;97(3):674–81. doi: 10.1002/cncr.11085. [DOI] [PubMed] [Google Scholar]
- 13.Baker F, Denniston M, Haffer SC, Liberatos P. Change in health-related quality of life of newly diagnosed cancer patients, cancer survivors, and controls. Cancer. 2009 Jul 1;115(13):3024–33. doi: 10.1002/cncr.24330. [DOI] [PubMed] [Google Scholar]
- 14.Morey MC, Snyder DC, Sloane R, Cohen HJ, Peterson B, Hartman TJ, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA. 2009 May 13;301(18):1883–91. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snyder DC, Morey MC, Sloane R, Stull V, Cohen HJ, Peterson B, et al. Reach out to ENhancE Wellness in Older Cancer Survivors (RENEW): design, methods and recruitment challenges of a home-based exercise and diet intervention to improve physical function among long-term survivors of breast, prostate, and colorectal cancer. Psychooncology. 2009 Apr;18(4):429–39. doi: 10.1002/pon.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993 Mar;31(3):247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Jr, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems: Results from the Medical Outcomes Study. JAMA. 1996 Oct 2;276(13):1039–47. [PubMed] [Google Scholar]
- 18.Boyd CM, Ricks M, Fried LP, Guralnik JM, Xue Q-L, Xia J, et al. Functional decline and recovery of activities of daily living in hospitalized, disabled older women: the Women's Health and Aging Study I. J Am Geriatr Soc. 2009 Oct;57(10):1757–66. doi: 10.1111/j.1532-5415.2009.02455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardy SE, Concato J, Gill TM. Resilience of community-dwelling older persons. J Am Geriatr Soc. 2004 Feb;52(2):257–62. doi: 10.1111/j.1532-5415.2004.52065.x. [DOI] [PubMed] [Google Scholar]
- 20.Resnick B, Galik E, Dorsey S, Scheve A, Gutkin S. Reliability and validity testing of the physical resilience measure. Gerontologist. 2011 Oct;51(5):643–52. doi: 10.1093/geront/gnr016. [DOI] [PubMed] [Google Scholar]
- 21.Seeman T, Chen X. Risk and protective factors for physical functioning in older adults with and without chronic conditions: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2002 May;57(3):S135–44. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- 22.Kempen GIJM, Ormel J, Scaf-Klomp W, Van Sonderen E, Ranchor AV, Sanderman R. The role of perceived control in the process of older peoples’ recovery of physical functions after fall-related injuries: a prospective study. J Gerontol B Psychol Sci Soc Sci. 2003 Jan;58(1):P35–41. doi: 10.1093/geronb/58.1.p35. [DOI] [PubMed] [Google Scholar]
- 23.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012 May;27(5):520–6. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood) 2015 Mar 1;34(3):431–7. doi: 10.1377/hlthaff.2014.0452. [DOI] [PubMed] [Google Scholar]
- 25.McAuley E, Szabo A, Gothe N, Olson EA. Self-efficacy: implications for physical activity, function, and functional limitations in older adults. Am J Lifestyle Med. 2011;5(4) doi: 10.1177/1559827610392704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004 Nov 3;292(17):2115–24. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]