Abstract
Background
Nursing is a notoriously high-stress occupation emotionally taxing and physically draining, with a high incidence of burnout. In addition to the damaging effects of stress on nurses’ health and well being, stress is also a major contributor to attrition and widespread shortages in the nursing profession. Although there exist promising in-person interventions for addressing the problem of stress among nurses, the experience of our group across multiple projects in hospitals has indicated that the schedules and workloads of nurses can pose problems for implementing in-person interventions, and that web-based interventions might be ideally suited to addressing the high levels of stress among nurses.
Purpose
The purpose of this study was to evaluate the effectiveness of the web-based BREATHE: Stress Management for Nurses program.
Methods
The randomized controlled trial was conducted with 104 nurses in five hospitals in Virginia and one hospital in New York. The primary outcome measure was perceived nursing-related stress. Secondary measures included symptoms of distress, coping, work limitations, job satisfaction, use of substances to relieve stress, alcohol consumption, and understanding depression and anxiety.
Results
Program group participants experienced significantly greater reductions than the control group on the full Nursing Stress Scale, and six of the seven subscales. No other significant results were found. Moderator analysis found that nurses with greater experience benefitted more.
Conclusion
Using a web-based program holds tremendous promise for providing nurses with the tools they need to address nursing related stress.
Keywords: Nurses’ Stress, Stress Management, Web-Based Intervention
Background
With nearly 4 million nurses in the U.S., nursing represents the largest sector of the health care professions and an indispensable component of the health care system (IOM, 2010). Although nurses are responsible for the health of millions of Americans on a daily basis, they suffer from high rates of stress that not only threaten their health and well-being, but which also have a significant impact on productivity and retention and ultimately on the quality of patient care (Kimball & O’Neill, 2002; Milliken et al., 2007; Aiken et al., 2002; Laschinger et al., 2001).
Several studies conducted over the past 25 years have found that nursing is a high-stress occupation and that higher stress among nurses is associated with poorer health and absenteeism (Erickson & Grove, 2007; McCrane et al., 1987; Schaeffer & Peterson, 1992, Kimball & O’Neill, 2002). The amount of stress and burnout experienced by nurses appears to be both a function of the work environment and nurses’ coping resources. The way a stressful event is perceived is dependent on the individual’s characteristics, resiliency, and coping skills (Wakim, 2014). Many sources of nurses’ stress have been identified, including shift work, death of patients, heavy work load, feelings of powerlessness, management styles, and ill-designed jobs and work environments (Burke & Greenglass, 2001; Laschinger et al., 2001; Ruggiero, 2003; Upenieks, 2003; Cohen-Katz et al., 2005).
A considerable body of research strongly suggests that workplace stress management interventions are effective at reducing stress (Richardson & Rothstein, 2008; Milliken et al., 2007). A meta-analysis by Richardson and Rothstein (2008) found that stress interventions (N = 36) had a medium to large effect on psychological, physiological, and organizational outcomes (overall effect size was .52), with cognitive-behavioral interventions producing the largest effects, followed by relaxation interventions. Studies of stress management programs conducted specifically for nurses indicate that cognitive-behavioral and relaxation techniques can be effective in helping nurses cope with and reduce personal stress (Milliken et al., 2007; Pipe et al., 2009; Cohen-Katz et al., 2005). The findings of other studies have also underscored the roles of hospital environment and management style in determining nurses’ stress levels, suggesting that stress management interventions should address issues at the organizational/management level as well as the personal level (Ruggiero, 2003; Laschinger et al., 2001).
However, virtually all of these interventions require multiple in-person trainer-led sessions, typically conducted in groups. Convening groups at scheduled times can be an impediment to implementing interventions with any occupational group (Cook & Schlenger, 2002; Snow et al., 2003; Billings et al., 2008), but it is especially problematic for nurses whose duties require an unusual amount of mobility and immediate responsiveness to patient needs (Chesak et al, 2015; Hersch et al., 2009). To address this issue, there is now accumulating evidence that web-based programs can be effective (and cost-effective) approaches to workforce health promotion and disease prevention (Webb et al., 2010; Wantland et al., 2004; Rothert et al., 2006). Importantly, web-based programs do not require the convening of groups at mutually convenient times and places, but can be delivered to users at the time and place of their choosing, requiring only access to the Internet.
Purpose
The current study was undertaken to test the effectiveness of a web-based stress management intervention created specifically for nurses and the situations that they experience. The BREATHE: Stress Management for Nurses program was designed to provide nurses with the information and tools they need to manage the myriad of stressors that can impact their work life. The web-based program provides a mechanism for nurses to access the intervention at times and places convenient to their busy and often stressful schedules. Influenced by feedback from nurses in focus groups and feasibility tests, the program includes sections on how stress impacts the body; assessing stress and identifying stressors; practical stress management tools addressing changing one’s views of stressors, changing one’s response to stressors, or changing the stressful situation; promoting effective communication skills; taking time to grieve; and depression and anxiety. A randomized controlled trial was conducted to test this web-based program with a sample of hospital-based nurses to determine if the program could help reduce the perceived stress associated with nursing and improve other coping and work practices. It was hypothesized that participants receiving the web-based program (experimental group) would experience greater reductions in nursing related stress when compared to participants in the wait-list control condition. It was further hypothesized that there would be greater reductions in symptoms of distress, using substances to relieve stress, alcohol consumption, and work limitations and greater increases in coping strategies, understanding depression and anxiety, and job satisfaction for participants in the experimental group when compared to control group participants.
Methods
Design
The web-based BREATHE: Stress Management for Nurses program was tested with nurses in six hospitals (five hospitals from a suburban Virginia hospital system and one located in New York City). The study was a pretest-posttest randomized controlled trial in which participants were randomly assigned to a group condition. Participation was voluntary and all protocols and procedures were approved by the study team’s Institutional Review Board (IRB) and the Institutional Review Boards of the participating hospitals. Those expressing interest in participating were asked to complete a pretest survey and, upon completion, were randomly assigned to either the experimental group (receiving access to the BREATHE web-based program) or to a wait-list control group. All participants were given access to the BREATHE program following completion of the posttest questionnaire.
Procedures
Recruitment information was provided to nurses through a number of communication strategies depending on the hospital. Communication methods included posting the information on the hospital Intranet, announcing the study at new nursing orientations, sending emails to nurses, and posting the study flyer on the units. Nurses interested in participating were instructed to contact the study team directly and were provided additional information about the nature of the study. To be eligible for the study, nurses had to be 21 years of age or older and work at one of the participating hospitals. Interested participants were told that they would receive $25 for completing each of the two study questionnaires and be entered into a drawing in which one participant would receive either $200 or $500 (depending on the hospital; the respective hospital IRBs set the drawing amount) during each questionnaire round. Nurses who expressed continued interest provided the study team with an email address which was used to send a personalized link to the online pretest questionnaire, which included the consent document.
After reading the consent document, nurses were given the option of consenting or declining participation. Nurses were not able to continue with the questionnaire until they acknowledged and indicated that they consented to participate. Two nurses declined to participate at the point of the consent document and ten additional nurses who initially expressed interest in the study and received the pretest link did not complete the questionnaire. A hard copy of the consent document was emailed to participants after they completed the pretest questionnaire.
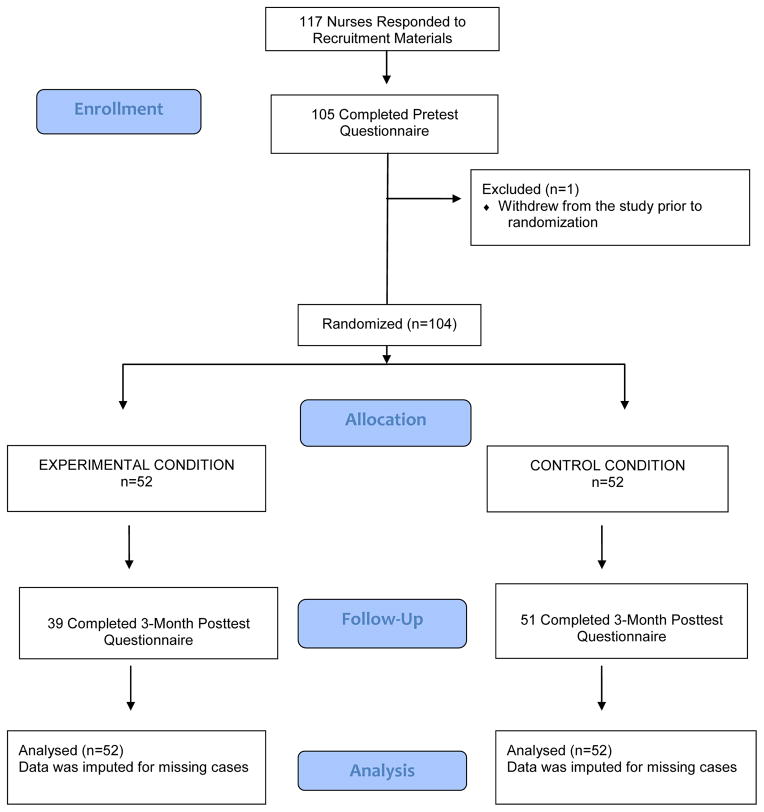
One hundred and seventeen nurses contacted the study team in response to the initial recruitment announcement and were sent a link to the online survey, 105 of whom completed the baseline survey. One participant subsequently withdrew from the study leaving a total sample size of 104 participants (See Figure 1).
Figure 1.
Consort Diagram
Randomization was conducted using a block randomized design with blocks of 4 and 6. The 0 and 1 within each block were random and the order of the group of 4 and the group of 6 was random. Randomization occurred after each participant completed the pretest questionnaire. The online questionnaire site was checked every day to determine who completed the pretest each day and individuals were assigned to the next condition on the randomization table as they completed the questionnaire. Once randomization was complete, participants were notified of the condition to which they were assigned (no blinding procedures were employed) and were informed of next steps; experimental group participants were sent a link to the BREATHE program along with a randomly generated username and password and instructions for using the program. Control group participants were told that their access to the program would be delayed until the end of the test period.
Participants could complete the online questionnaires and, for those in the program condition, access the online program on work time or at home. The program incorporated a responsive web design that allowed the program to be viewed on a desktop or laptop computer, tablet, or smartphone. Participants in the experimental group could access the web-based program at any time during the three-month test period, both at work or outside work (e.g., at home). A “project update” email was sent to all participants at one-month post randomization. For the experimental group, the emails included a reminder to use the program. For the control group, the email included information about when the second questionnaire would be available. In addition, the project staff was always available to answer questions by telephone and email if participants had any difficulty accessing the program. The data collection started on April 22, 2014 (first participant enrolled) and ended on February 16, 2015 (last participant completed posttest). Individual access to the program by experimental participants was limited to the three-month test period for the purposes of the study. No discernable secular events of note occurred during the test period. At the end of the three-month test period and prior to administering the follow-up questionnaire, access to the program was temporarily suspended. Three months after randomization, participants were sent an email with the link to the posttest questionnaire. After the posttest questionnaire was complete and all data were collected, all participants received access to the program.
Participant Characteristics
Study participants were 104 nurses employed either by one of five hospitals included in a suburban Virginia hospital system (n=36) or a large metropolitan hospital in New York (n=68). Demographic characteristics of the sample are noted in Table 1. Participants ranged in age from 22 to 65 (mean = 41), 87.5% were female, and 65% identified as Caucasian. Forty-four percent were never married and 50% were either married or living with a partner. Fifty-seven percent of participants had a BSN and 21% had a MSN. The nurses’ experience ranged from those that had been a nurse less than 1 year (8%) to those that had been a nurse for more than 25 years (30%); 34% worked on a medical or surgical floor; 8 participants (8%) identified themselves as Advanced Practice Nurses and 10 participants (10%) identified themselves as Clinical Nurse Managers. A comparison of the experimental and control group participants on demographics and outcome variables at baseline revealed no significant differences between the groups, indicating that randomization was successful.
Table 1.
Participant Characteristics at Baseline
| Control | Program | |
|---|---|---|
| Gender | ||
| Male | 9 (17%) | 4 (8%) |
| Female | 43 (83%) | 48 (92%) |
| Race | ||
| Black or African American | 6 (12%) | 2 (4%) |
| Caucasian | 31 (60%) | 35 (67%) |
| American Indian/Alaska Native | 1 (2%) | 0 |
| Asian | 11 (21%) | 10 (19%) |
| Other | 2 (4%) | 5 (10%) |
| Multiracial | 2 (4%) | 0 |
| Latino | ||
| Yes | 3(6%) | 6 (12%) |
| No | 48 (92%) | 46 (88%) |
| Prefer not to answer | 1 (2%) | 0 |
| Age | ||
| 22–26 | 15 (29%) | 7 (13%) |
| 27–31 | 2 (4%) | 7 (13%) |
| 32–36 | 7 (13%) | 5 (10%) |
| 37–41 | 3 (6%) | 7 (13%) |
| 42–46 | 4 (8%) | 2 (4%) |
| 47–51 | 5 (10%) | 9 (17%) |
| 52–56 | 11 (21%) | 5 (10%) |
| 57–61 | 5 (10%) | 8 (15%) |
| 62–66 | 0 | 2 (4%) |
| Marital Status | ||
| Single | 23 (44%) | 23 (44%) |
| Married | 23 (44%) | 27 (52) |
| Divorced/Separated | 3 (6%) | 2 (4%) |
| Widowed | 1 (2%) | 0 |
| Living with Partner | 2 (4%) | 0 |
| Highest Level of Nursing Education | ||
| Diploma (RN) | 7 (13%) | 13 (25%) |
| BSN | 32 (62%) | 27 (52%) |
| MSN | 11 (21%) | 11 (21%) |
| PhD | 2 (4%) | 0 |
| DNP | 0 | 1 (2%) |
| Clinical Nurse Manager | 5 (10%) | 5 (10%) |
| Advance Practice Nurse | 4 (8%) | 4 (8%) |
| Years in Nursing | ||
| < 1 | 5 (10%) | 3 (6%) |
| 1–5 | 16 (31%) | 12 (23%) |
| 6–10 | 6 (12%) | 7 (13%) |
| 11–15 | 1 (2%) | 4 (8%) |
| 16–20 | 5 (10%) | 4 (%) |
| 21–25 | 4 (8%) | 6 (12%) |
| >25 | 15 (29%) | 16 (31%) |
| Years at Current Hospital | ||
| < 1 | 14 (27%) | 9 (17%) |
| 1–5 | 15 (29%) | 15 (29%) |
| 6–10 | 8 (15%) | 11 (21%) |
| 11–15 | 2 (4%) | 6 (12%) |
| 16–20 | 3 (6%) | 2 (4%) |
| 21–25 | 3 (6%) | 3 (6%) |
| >25 | 7 (13%) | 6 (12%) |
| Work Setting | ||
| ICU | 11 (21%) | 5 (10%) |
| CCU | 2 (4%) | 2 (4%) |
| Med/Surgery/Unit/Floor | 18 (51%) | 17 (49%) |
| OR/Perioperative | 0 | 5 (10% |
| Emergency Department | 6 (12%) | 3 (6%) |
| NICU | 1 (2%) | 1 (2%) |
| Maternal/Child Health | 1 (2%) | 2 (4%) |
| Other | 13 (25%) | 17 (33%) |
Intervention
The web-based BREATHE: Stress Management for Nurses program consists of seven modules for nurses and an additional module for Nurse Managers. Participants who completed the pretest were asked if they were a Nurse Manager and depending on their response, they were provided a username corresponding to their role. That is, if a nurse indicated they were not a Nurse Manager, only the seven modules for nurses were visible in the program (the Nurse Manager module was not visible). When Nurse Managers accessed the program, they saw the seven nurse modules plus an additional module created specifically for Nurse Managers. The seven universal modules are: Welcome and Introduction (includes information on the stresses of nursing, and how stress impacts the body and affects daily life); Assess Your Stress (provides assessments and feedback on personal stress and coping levels); Identify Stressors (helps users recognize the symptoms of stress and their personal stressors and includes a tool for tracking their stress); Manage Stress (provides a number of different stress management strategies and tools); Avoid Negative Coping (addresses the problem of using alcohol and drugs to manage stress); and Your Mental Health (focuses on depression and anxiety and when to seek additional counseling). The Manager’s Role includes additional information for Nurse Managers on identifying workplace stressors and reducing stress through positive management practices. The program was developed through a series of steps which included focus groups with nurses to help craft the look, feel, and content of the program; discussions with experts in the field; and content review and refinement among the project staff and the technical development staff. The program includes interactive exercises, downloadable tools, real story videos from nurses, and other audio/visual content.
Experimental group participants were encouraged to use the BREATHE program as often as they wanted over a three-month period. Program utilization, including the number of times the program was accessed and the number of minutes spent in the program, was tracked by the research team.
Measures
The 30-minute online self-report questionnaire contained the following measures:
Demographics
Demographic questions included ten items assessing respondents’ gender, age, race, ethnicity, marital status, education, nurse manager status, work setting, years in nursing, and years at the hospital.
Nursing Stress Scale (NSS)
This widely used measure is designed to assess seven sources of work-related stress specific to nursing (Gray-Toft and Anderson 1981). Subscales of this measure include: Death and Dying, Conflict with Physicians, Inadequate Preparation, Lack of Support, Conflict with Other Nurses, Work Load, and Uncertainty Concerning Treatment. The NSS provides a total stress score as well as scores on each of seven subscales designed to measure the frequency with which the seven major sources of nursing stress are experienced by the respondent (Full Scale Alpha = .90).
Symptoms of Distress
This measure is a 15-item scale developed by Orioli et al. (1991). Each item describes a physical or emotional symptom of distress (muscle tension, nervousness, etc.) with a four-point response scale indicating the frequency with which the symptom was felt in the past 30 days, ranging from 1 (Nearly Every Day) to 4 (Never). A higher score = less stress (Alpha = .86).
Coping with Stress
This measure contains twelve items assessing the type of strategies one uses to cope with difficult situations and events (Orioli et al., 1991). Questions are answered on a 4-point scale ranging from 1 (Never) to 4 (Almost Always); higher score = better coping. Typical questions include: “I often put things aside for a while to get perspective on them,” and“I decide certain problems are not worth worrying about” (Alpha = .70).
Work Limitations Questionnaire (WLQ)
This measure was developed and validated by Lerner and associates (2001), and contains four separate scales: a five item scale assessing difficulty meeting time and scheduling demands (Alpha = .73), a six item scale measuring a person’s ability to perform job tasks, concentration and focus (Alpha = .76), a three item scale assessing interpersonal job demands (Alpha = .77), and a five item scale measuring a person’s ability to keep up with the quality and quantity demands of their job (Alpha = .85). Instructions asked the extent to which stress made it difficult for the user to engage in the activities noted.
Use of Substances for Stress Relief
Three individual items were developed by the study team which asked users to indicate the extent to which they used alcohol, prescription drugs as prescribed, or used prescription drugs in ways other than as prescribed to relieve stress.
Drinking Quantity and Frequency
Drinking quantity and frequency was measured by four separate items which asked users whether they have had a drink in the past 12 months, the number of drinking days in the past 30 days, the number of drinks consumed on drinking days, and the number of days in which users consumed five or more drinks on the same occasion.
Understanding Depression and Anxiety
Developed by the study team, this measure included six items designed to assess the extent to which users understood and internalized the information presented in the Your Mental Health section of the program (Alpha = .58)
Nurses Job Satisfaction Scale
Nurses’ satisfaction with their job was assessed with the 24-item Nurse Satisfaction Scale, developed by Ng (1993). The scale measures the respondent’s satisfaction with seven work factors: administration, co-workers, career, patient care, relation with supervisor, nursing education, and communications. (Alpha = .84).
Analysis
There were fourteen participants who did not respond at posttest. Of these participants, thirteen were in the treatment group, representing a significant difference between conditions. While the overall attrition rate was 13.4% (14/104), the experimental group attrition rate was 25% (13/52). A number of strategies were employed to address this difference and to ensure that any significant group differences in outcome measures were not due to this differential attrition. First, we conducted an attrition analysis to determine if there was a failure of randomization. Results revealed that there were no significant differences between the two groups on any of the pretest measures or demographic variables, indicating that randomization with respect to the study variables had been successful. Next, we examined which pretest or demographic variables predicted posttest missingness (i.e., attrition). We found that the following participants were less likely to respond to the posttest measure: those who reported greater number of days in which they had five or more drinks on the same occasion at pretest, those who reported more drinks per day at pretest, and those who had lower scores on the understanding of depression and anxiety measure at pretest.
Using these variables, we also conducted a logistic regression, predicting posttest non-response (i.e., a 0 or 1 outcome variable) with these three variables as a set as well as the “Group” (i.e., experimental condition) variable. We did so to examine whether these other variables collectively explained the differential attrition across groups. Results of this analysis revealed that experimental condition remained a significant predictor of non-response beyond (i.e., in addition to) these variables, indicating that drinking status and understanding of mental health issues did not “carry” the effects of the experimental condition.
Given these findings, we conducted multiple imputation for missing values of all outcome variables, using the Markov chain Monte Carlo (MCMC) approach (Schafer, 1997). To ensure robustness, we generated several imputation models (i.e., included different sets of variables) to create multiply-imputed data sets. For each model, we generated 25 multiply-imputed data sets. We then conducted the primary analyses on each of the 25 datasets (i.e., conducted analyses using one imputation model using the corresponding imputed 25 datasets, then using another imputed 25 datasets, etc.). For all outcomes, conclusions were identical across imputation models. Thus, we only report the results for each outcome for a single imputation model here the one we viewed as most conservative. This imputation model included baseline demographic characteristics, group assignment, the corresponding baseline (pretest) measure, the interaction between group assignment and pretest scores on that measure, and the variables noted above that predicted attrition.
The primary analyses followed intent-to-treat principles, including all participants irrespective of protocol violations and events arising from post randomization (Friedman et al, 2010). The analyses (i.e., tests of program effectiveness) consisted of a series of multiple regressions (one for each outcome variable) conducted in Mplus using the imputed datasets described above. Mplus automatically generates the correct standard errors associated with multiply-imputed data. In addition to including group (i.e., experimental condition), we also entered the following variables as covariates in each equation: pretest scores for that outcome, program dosage (i.e., time in program), and the interaction between group and pretest scores. These analyses are identical to Analysis of Covariance [ANCOVA] in ANOVA terminology.
To further corroborate the conclusions from these analyses and to explore the impact of the multiple imputation, we also conducted ANCOVAs in SPSS (using listwise deletion). The conclusions from those analyses mirrored the ones from the Mplus analyses, suggesting that the imputation, although allowing for the inclusion of more data, did not lead to appreciably different study results.
Results
Primary Outcome Measures
Table 2 presents the results of the regression analyses using the imputed data testing the differential improvement on the self-reported outcome measures.
Table 2.
Program Results on Dependent Measures
| Baseline | Follow-up | Regression Analyses | |||||
|---|---|---|---|---|---|---|---|
| Outcome Measure | Experimental Mean (sd) | Control Mean (sd) | Experimental Mean (sd) | Control Mean (sd) | SE | t | p-value |
| Nursing Stress: Full Scale | 2.243 (.46) | 2.273 (.43) | 2.072 (.38) | 2.350 (.49) | .085 | −2.954 | .003 |
| Nursing Stress: Death and Dying | 2.102 (.54) | 2.143 (.58) | 2.004 (.50) | 2.275 (.70) | .106 | −2.244 | .025 |
| Nursing Stress: Conflict with Physicians | 2.285 (.59) | 2.290 (.61) | 2.064 (.51) | 2.297 (.56) | .104 | −2.108 | .035 |
| Nursing Stress: Inadequate Preparation | 2.180 (.53) | 2.231 (.58) | 1.982 (.47) | 2.207 (.59) | .107 | −1.952 | .051 |
| Nursing Stress: Lack of Support | 1.884 (.60) | 2.032 (.62) | 1.750 (.66) | 2.021 (.58) | .115 | −1.487 | .137 |
| Nursing Stress: Conflict with Other Nurses | 2.182 (.71) | 2.077 (.68) | 1.855 (.55) | 2.328 (.70) | .125 | −4.167 | .000 |
| Nursing Stress: Work Load | 2.666 (.61) | 2.741 (.56) | 2.558 (.59) | 2.832 (.58) | .110 | −2.297 | .022 |
| Nursing Stress: Uncertainty Concerning Treatment | 2.186 (.64) | 2.203 (.62) | 2.003 (.45) | 2.211 (.55) | .096 | −2.139 | .032 |
| Symptoms of Distress: Full Scale | 2.793 (.47) | 2.799 (.52) | 2.968 (.51) | 2.840 (.54) | .081 | 1.536 | .125 |
| Symptoms of Distress: Physical Symptoms | 2.551 (.63) | 2.760 (.60) | 2.660 (.70) | 2.689 (.66) | .108 | 1.186 | .236 |
| Symptoms of Distress: Behavioral Symptoms | 3.248 (.46) | 3.188 (.53) | 3.404 (.46) | 3.286 (.48) | .095 | .942 | .346 |
| Symptoms of Distress: Emotional Symptoms | 2.675 (.60) | 2.599 (.67) | 2.891 (.63) | 2.681 (.66) | .101 | 1.679 | .093 |
| Coping with Stress: Full Scale | 2.013 (.33) | 2.030 (.29) | 1.949 (.39) | 1.992 (.31) | .063 | −.617 | .537 |
| Coping with Stress: Situation Mastery | 2.231 (.39) | 2.211 (.43) | 2.232 (.40) | 2.243 (.35) | .076 | −.284 | .776 |
| Coping with Stress: Adaptability | 2.017 (.37) | 2.036 (.38) | 1.877 (.51) | 1.963 (.40) | .083 | −.972 | .331 |
| Work Limitations: Time and Scheduling Demands | 3.929 (.73) | 4.022 (.71) | 4.078 (.92) | 3.908 (.79) | .015 | −.282 | .778 |
| Work Limitations: Focus and Concentration Demands | 4.042 (.62) | 4.075 (.65) | 4.305 (.73) | 3.964 (.82) | .090 | .245 | .806 |
| Work Limitations: Interpersonal Demands | 4.387 (.47) | 4.177 (.82) | 4.340 (.68) | 4.222 (.74) | .150 | .313 | .754 |
| Work Limitations: Quality and Quantity Demands | 4.045 (.66) | 3.866 (.86) | 4.193 (.89) | 4.001 (.77) | .162 | .520 | .603 |
| Understanding Depression and Anxiety | 3.246 (.52) | 3.354 (.45) | 3.470 (.38) | 3.357 (.47) | .108 | 1.569 | .117 |
| Using Alcohol to Relieve Stress | 1.808 (.86) | 1.885 (.93) | 1.738 (.86) | 1.912 (.99) | .127 | −.880 | .379 |
| Using Prescription Drugs as Prescribed to Relieve Stress | 1.135 (.56) | 1.212 (.57) | 1.104 (.48) | 1.112 (.47) | .092 | .246 | .806 |
| Using Prescription Drugs Not as Prescribed to Relieve Stress | 1.019 (.14) | 1.058 (.30) | 1.020 (.11) | 1.038 (.28) | .024 | .511 | .609 |
| Drank in the past 12 Months | .885 (.32) | .885 (.32) | .876 (.32) | .886 (.31) | .037 | −.271 | .787 |
| Number of Drinking Days in Past 30 Days | 5.326 (6.66) | 4.306 (4.83) | 4.452 (5.89) | 4.918 (4.65) | .686 | −1.612 | .107 |
| Number of Drinks Per Drinking Day in Past 30 Days | 1.649 (1.34) | 1.704 (1.32) | 1.513 (1.19) | 1.455 (1.04) | .208 | .413 | .680 |
| Number of Days Having 5 or More Drinks on One Occasion in Past 30 Days | .556 (1.67) | .466 (1.28) | .282 (.78) | .353 (.76) | .126 | −.847 | .397 |
Notes. SE = standard error for group effect. t = t-value for group effect. sd = Standard Deviation
Nursing Related Stress (Nursing Stress Scale)
The experimental group showed significantly greater improvement than the control group on the primary outcome measure of nurses’ stress. Significant differences were found between the experimental and control groups on the full Nursing Stress Scale (t = -2.95; p=.00) and six of the seven subscales including stress related to issues of Death and Dying (t=−2.24, p=.03), Conflict with Physicians (t=−2.11, p=.04), Inadequate Preparation (t=−1.95, p=.05), Conflict with Other Nurses (t=−4.17, p=.00), Work Load (t=−2.30, p=.02), and Uncertainty Concerning Treatment (t=−2.14, p=.03). The only subscale where there were no significant differences between groups was stress related to issues of Lack of Support (t=−1.49; ns).
Other Outcome Measures
No other significant differences were found for the secondary outcome measures including Symptoms of Distress, Coping with Stress, Work Limitations, Nurses Job Satisfaction, Understanding Depression and Anxiety, Using Substances to Relieve Stress, or Alcohol Quantity and Frequency.
Program Utilization
Every time an experimental group participant logged into the BREATHE program using the unique identifier, data were collected on the time the user was active in the program and the pages that were accessed. As noted in Table 3, the majority of program group participants logged into the program 1–3 times. Ten participants in the experimental group never logged into the program. The average number of logins for those who logged in at least once was 2.5. The average amount of time spent in the BREATHE program was 43 minutes.
Table 3.
Program Utilization
| Utilization | Number | Percentage |
|---|---|---|
|
| ||
| Logins | ||
| 0 | 10 | 19.2% |
| 1 | 15 | 28.8% |
| 2 | 8 | 15.4% |
| 3 | 10 | 19.2% |
| 4 | 4 | 7.7% |
| 5 | 4 | 7.7% |
| 8 | 1 | 1.9% |
| Time in Program | ||
| (For participants who logged in at least once) | ||
| 17 | 40.5% | |
| Less than 20 minutes | 14 | 33.3% |
| 20 to 1 hour | 6 | 14.3% |
| 1 to 2 hours | 5 | 11.9% |
| Over 2 hours | ||
Moderator Effects
To determine whether program effects on the nurses’ stress outcome differed based on participant demographics, a series of moderator analyses were performed on all outcome measures. No interactions were detected between condition and race, marital status, nursing education, site, or years at current hospital. There was, however, a statistically significant moderating effect of years of nursing on nurses’ stress. Specifically, results showed that the program had a greater impact on reducing nursing related stress for nurses with more experience (that is, having been a nurse for more years).
We also examined the relationship between utilization as measured by “minutes in program” and the impact of the program on nursing related stress. Results of that analysis showed that participants who spent more time appeared to benefit more (p = .076), that is, had greater reduction in nursing related stress, though that relationship was not significant at p =.05 level.
Discussion
Results of this randomized controlled trial provide evidence of the benefits of using a web-based program to help hospital-based nurses manage the stress often associated with nursing. Nurses who received access to the BREATHE program showed significant improvement in perceived nursing related stress. In addition to showing significant improvement in perceived stress as measured by the overall Nursing Stress Scale (NSS), nurses showed reductions in specific areas of nursing stress including the stress related to Death and Dying, Conflict with Physicians, Inadequate Preparation, Conflict with Other Nurses, Work Load, and Uncertainty Concerning Treatment. These subareas are particularly important as the BREATHE program specifically focuses on areas of nursing stress that nurses could address either by changing the way they view the stressor, changing how they respond to stress or, when possible, changing the stressful situation. For example, three of the stress management skills sections involve learning assertive communication, conflict resolution, and problem solving strategies that can reduce the stress associated with different interactions with other nurses or physicians. In addition, the section entitled “Taking Time to Grieve” tackles head on the stress surrounding death and dying and provides nurses with strategies they can use to alleviate that stress. In the course of their clinical work, nurses are frequently required to cope with the processes surrounding patient deaths. Nurses’ personal attitudes towards death and dying can influence the quality of care they provide especially during the terminal stages of a person’s life. Faced with emotional issues such as the reality of death, nurses need skills and experience to manage such fears. Programs such as BREATHE which aim to address this issue and provide exercises on grieving and coping with the demands of caring for dying patients can serve to both minimize this stress and improve overall care of terminal and critically ill patients (Peters et al., 2013; Deffner & Bell 2005).
Results of this study also point to the importance of interventions that are aimed at improving work relations among nurses since conflict with other nurses and physicians is a significant source of stress (Tabak & Orit, 2007). Perceptions of stresses associated with conflict with other nurses and conflict with physicians were significantly improved following administration of the BREATHE program which specifically addresses communication skills in this area. Additionally, the nurse mangers module of BREATHE provides information on reducing stress through positive management practices and better communication with staff nurses. Identifying and addressing the communication needs of nurses has been associated with the promotion of individual growth, retention, and work satisfaction (Wakim, 2014). An essential element for nursing management is to create an environment in which open communication is encouraged and co-worker support is fostered because worker criticisms and conflicts are often the cause of stress (Lavoie-Tremblay et al., 2010). Nursing unit managers and their teams are confronted with complex health care issues and managers need the skills to promote supportive and adaptive work environments. Chronic exposure to stress and work complexity can negatively affect nurse managers’ health, their decision-making processes and potentially threaten both patient and organizational outcomes (Van Bogaert, 2014). Further, stresses emanating from the physical and social environment such as role ambiguity and poor communications with leadership have been significantly associated with increased levels of emotional exhaustion (Stordeur et al., 2001). Providing nurses with communication skills and reinforcing the need to ask for help when needed appears to help both the perception of stress and physical consequences such as exhaustion and burnout.
It was surprising that perceived stress from a lack of social support did not show significant improvements following the intervention. Social support among nurses in the form of positive interpersonal exchanges with coworkers and supervisors is associated with enhanced security, mutual respect, and positive feelings - which all help to reduce stress (Jennings, 2008). One explanation for this finding is that nurses in this study did not experience high levels of stress from a lack of social support. Baseline numbers for nurses experiencing this type of stress were low (lowest among all the subscales), and while there were decreases in this type of stress following the intervention, there was reduced ability for improvement and the changes were minor.
Secondary outcome measures which included symptoms of distress and job satisfaction and using alcohol or substances to relieve stress showed no significant effects of the web-based program. It may be that the relatively short intervention and brief follow-up period were not sufficient to achieve the desired improvements in these types of outcome measures. Future studies could benefit from longer intervention and follow-up periods to more adequately test program effects.
The moderating effect of years in nursing on nurses’ stress following the intervention is an interesting finding and worthy of further investigation. A study looking at the moderating effects of negative outcomes of stress among nurses, found a significant relationship with age, but not with years in nursing (Kath et al., 2012). Results of this study, however, showed that the program had a greater impact on reducing nursing related stress for nurses with more experience (having been a nurse for more years). A recent study found interesting associations between years of nursing and response to stressful situations (Galdikiene et al., 2014). In this study a significant correlation was found between length of work experience and the responses to dealing with issues of death and dying and conflict with physicians. The nurses with longer work experience in health care mentioned that the most stressful situations were caring for dying patients and having conflicts with physicians, which were also areas impacted with the current intervention. The reasons why the program had greater impact on nurses with more experience could be due to ways in which information is processed in relation to experience. A study by Daley (1999) reported that novice nurses tend to primarily learn through the content delivered in formal training, whereas in contrast, expert nurses supplement formal learning with a mature knowledge base that they have developed over a period of years.
These results mirror findings for in-person workplace stress management interventions that focus on cognitive-behavioral and relaxation strategies (Milliken et al., 2007; Pipe et al., 2009; Cohen-Katz et al., 2005).
The cognitive behavioral aspects of the program include instructing users about reactions to stress that are counterproductive and strategies designed to help users replace dysfunctional ways of thinking with more positive ways of coping. The program also provided examples of stressful situations and how to use cognitive restructuring techniques to change interpretations and perceptions of stressful events, the importance of which has been discussed elsewhere (Bamber, 2006). Numerous studies have indicated that cognitive behavioral therapy is effective in modifying dysfunctional cognitions and improving an individual's ability to deal with stressful events (Mok et al., 2014; Moeini et al., 2011; Granath et al., 2006). As cognitive behavioral therapy focuses on modifying dysfunctional cognitions and promoting the adoption of appropriate behaviors for coping with stress and emergent situations, it can be especially effective for addressing the stress experienced by nurses (Brunero et al., 2008; Orly et al., 2010).
The results of this study need to be considered with regard to limitations. The primary limitation is the small sample size, which makes it difficult to generalize the effectiveness of the intervention beyond our population. The sample size may also have made it difficult to detect significant relationships between the intervention and the outcomes of interest. A second limitation is the degree of program utilization. Several nurses in the experiment group did not access the program, thereby diluting observed differences between the experimental and control groups. The reasons why these nurses did not access the program is worthy of further consideration as is exploring ways in which utilization could have been bolstered. It is encouraging, however, that despite the small sample size and limited utilization the results clearly revealed that the intervention had beneficial effects on nurses' perception of stress lending additional support to the findings that programs focusing on personnel support can be an effective workplace stress management approach for nurses (Mimura & Griffiths, 2003). Lastly, the study was only able to assess the relatively short-term (three months) impact of the BREATHE program on self-reported measures of perceived stress, distress and coping. Additional studies would benefit from a longer posttest data collection period and the inclusion of biological measures such as cortisol to test the effects of stress management interventions on objective measures of stress.
Summary and Conclusions
This project developed and tested a comprehensive web-based training program for hospital staff nurses and nursing management. The web-based program contains segments on identifying and assessing stress, stress management strategies and tools, and avoiding negative coping techniques. Overall, study findings indicate that the BREATHE web-based program can be an effective means of reducing nurses perceived stress related to issues of death and dying, conflict with physicians, inadequate preparation, conflict with other nurses, work load, and uncertainty concerning treatment. Results of the study hold promise for the use of BREATHE (or similar) web-based programs as an important occupationally-based intervention to help nurses gain the information and skills they need to manage many of the stressors associated with nursing.
Acknowledgments
This study was funded by a grant from the National Institutes of Health, National Institute on Nursing Research. Grant Number R44NR013348.
We would also like to acknowledge the following individuals for their contributions to the study:
Christine Althoff, RN, MSN, AOCNS, Inova Fairfax Hospital
Susanne T. Fehr, PhD, RN-BC, NE-BC; Nursing Resource Manager, Inova Alexandria Hospital
Debra Stanger, MSN, RN, NE-BC, Director of Nursing Outcomes/Magnet Program Director, Inova Loudoun Hospital
Mary G Gibbons, MSN, RN, NE-BC, Director of Outpatient Services, Inova Fair Oaks Hospital
Sara Phillippe, DNP, MSHCA, BSN, RN, NE-BC (Formerly of Inova Mount Vernon Hospital)
Footnotes
Conflict of Interest: The first two authors are owners in the research organization that owns the BREATHE: Stress Management for Nurses program which was tested in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rebekah K. Hersch, ISA Associates Inc..
Royer F. Cook, ISA Associates Inc..
Diane K. Deitz, ISA Associates Inc..
Seth Kaplan, George Mason University.
Daniel Hughes, Mount Sinai Medical Center
Mary Ann Friesen, Inova Health System.
Maria Vezina, Mount Sinai St.Luke's Hospital.
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Bamber MR. CBT for occupational stress in health professionals. Introducing a schema-based approach. New York: Routledge; 2006. [Google Scholar]
- Billings DW, Cook RF, Hendrickson A, Dove D. A web-based approach to managing stress and mood disorders in the workforce. Journal of Occupational and Environmental Medicine. 2008;50:960–968. doi: 10.1097/JOM.0b013e31816c435b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunero S, Cowan D, Fairbrother G. Reducing emotional distress in nurses using cognitive behavioral therapy: A preliminary program evaluation. Journal of Nursing Science. 2008;5:109–115. [Google Scholar]
- Burke RJ, Greenglass ER. Hospital restructuring and nursing staff well-being: The role of perceived hospital and union support. Anxiety, Stress & Coping: An International Journal. 2001;14(1):14–21. [Google Scholar]
- Chesak SS, Bhagra A, Schroeder DR, Foy DA, Cutshall SM, Sood A. Enhancing resilience among new nurses: Feasibility and efficacy of a pilot intervention. The Ochsner Journal. 2015;15:38–44. [PMC free article] [PubMed] [Google Scholar]
- Cohen-Katz J, Wiley S, Capuano T, Baker DM, Deitrick L, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part III. Holistic Nursing Practice. 2005;19:78–86. doi: 10.1097/00004650-200503000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Kimmel S, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part II: A quantitative and qualitative study. Holistic Nursing Practice. 2005;19:26–35. doi: 10.1097/00004650-200501000-00008. [DOI] [PubMed] [Google Scholar]
- Cook RF, Schlenger W. Prevention of substance abuse in the workplace: Review of research on the delivery of services. Journal of Primary Prevention. 2002;23(1):115–142. [Google Scholar]
- Daley B. Novice to expert: An explanation of how professionals learn. Adult Education Quarterly. 1999;49(4):1–17. [Google Scholar]
- Deffner JM, Bell SK. Nurses' death anxiety, comfort level during communication with patients and families regarding death, and exposure to communication education: a quantitative study. Journal of Nurses in Staff Development. 2005;21:19–23. doi: 10.1097/00124645-200501000-00005. [DOI] [PubMed] [Google Scholar]
- Erickson R, Grove W. Why emotions matter: Age, agitation and burnout among Registered Nurses. The Online Journal of Issues in Nursing. 2007;13(1) [Google Scholar]
- Friedman LM, Furberg CD, DeMets DL. Fundamentals of Clinical Trials. New York: Springer; 2010. [Google Scholar]
- Galdikiene N, Asikainen P, Balciunas S, Suominen T. Do nurses feel stressed? A perspective from primary health care. Nursing and Health Sciences. 2014;16:327–334. doi: 10.1111/nhs.12108. [DOI] [PubMed] [Google Scholar]
- Granath J, Igvarsson S, von Thiele U, Lundberg U. Stress management: A randomized study of cognitive behavioral therapy and yoga. Cognitive Behavioral Therapy. 2006;35(1):3–10. doi: 10.1080/16506070500401292. [DOI] [PubMed] [Google Scholar]
- Gray-Toft P, Anderson J. The Nursing Stress Scale: development of an instrument. Journal of Behavioral Assessment. 1981;3(1):11–23. [Google Scholar]
- Hersch R, Cook R, Hughes D, Leaf S, Billings D, Kaplan S. Final Report. Gaithersburg, MD: Center for Substance Abuse Prevention; 2009. Healthy WorkLife for Young Adults. [Google Scholar]
- IOM (Institute of Medicine) The Future of Nursing: Leading Change, Advancing Health. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- Jennings B. Work stress and burnout among nurses: Role of work environment and working conditions. In: Hughes RG, editor. Patient safety and quality: An evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- Kath LM, Stichler JF, Ehrhart MG. Moderators of the negative outcomes of nurse manager stress. Journal of Nursing Administration. 2012;42(4):215–221. doi: 10.1097/NNA.0b013e31824ccd25. [DOI] [PubMed] [Google Scholar]
- Kimball B, O’Neill E. Health Care’s Human Crisis: The American Nursing Shortage. Princeton, NJ: The Robert Wood Johnson Foundation; 2002. [Google Scholar]
- Laschinger HKS, Finegan J, Shamian J, Wilk P. Impact of structural and psychological empowerment on job strain in nursing work settings: Expanding Kanter’s model. Journal of Nursing Administration. 2001;31:260–272. doi: 10.1097/00005110-200105000-00006. [DOI] [PubMed] [Google Scholar]
- Lavoie-Tremblay MM, Leclerc E, Marchionni C, Drevniok U. The needs and expectations of Generation Y nurses in the workplace. Journal of Nurses in Staff Development. 2010;26(1):2–8. doi: 10.1097/NND.0b013e3181a68951. [DOI] [PubMed] [Google Scholar]
- Lerner DJ, Amick BC, III, Rogers WH, Malspeis S, Bungay K. The work limitations questionnaire: a self-administered instrument for assessing on-the-job work disability. Medical Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- McCrane EW, Lambert VA, Lambert CE. Work, stress, hardiness and burnout among hospital staff nurses. Nurse Res. 1987;36:374–378. [PubMed] [Google Scholar]
- Milliken TF, Clements PT, Tillman HJ. The impact of stress management on nurse productivity and retention. Nursing Economics. 2007;25:203–210. [PubMed] [Google Scholar]
- Mimura C, Griffiths P. The effectiveness of current approaches to workplace stress management in the nursing profession: an evidence based literature review. Occupational and Environmental Medicine. 2003;60(1):10–5. doi: 10.1136/oem.60.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeini B, Hazavehei SM, Hosseini Z, Aghamolaei T, Moghimbeigi A. The impact of cognitive-behavioral stress management training program on job stress in hospital nurses: Applying PRECEDE model. Journal of Research in Health Sciences. 2011;11(2):114–20. [PubMed] [Google Scholar]
- Mok ALF, Chau JPC, Chan DWK, Ip WY. The effectiveness of cognitive behavioral interventions in reducing stress among nurses working in hospitals: a systematic review protocol. [Accessed online 11/3/2015];JBI Database of Systematic Reviews and Implementation Reports. 2014 12(7) at: http://joannabriggslibrary.org/index.php/jbisrir/article/view/1601/2049. [Google Scholar]
- Orioli EM, Jaffe DT, Scott CD. Developed by Essi Systems. New York: Newmarket Press; 1991. StressMap: Personal diary edition. The ultimate stress management, self-assessment, and coping guide. [Google Scholar]
- Orly S, Rivka B, Dorit SE. The impact of cognitive behavioral intervention on SOC, perceived stress and mood states of nurses. Procedia Social and Behavioral Science. 2010;2:928–932. [Google Scholar]
- Ng S. A job satisfaction scale for nurses. New Zealand Journal of Psychology. 1993;22:87–91. [Google Scholar]
- Peters L, Cant R, Payne S, O’Connor M, McDermott F, Hood K, Morphet J, Shimoinaba K. How death anxiety impacts nurses’ caring for patients at the end of life: A review of literature. The Open Nursing Journal. 2013;7:14–21. doi: 10.2174/1874434601307010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pipe TB, Bortz JJ, Dueck M, Pendergast D, Buchda V, Summers J. Nurse leader mindfulness meditation program for stress management: A randomized controlled trial. Journal of Nursing Administration. 2009;39:130–137. doi: 10.1097/NNA.0b013e31819894a0. [DOI] [PubMed] [Google Scholar]
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: A meta-analysis. Journal of Occupational Health Psychology. 2008;13:69–93. doi: 10.1037/1076-8998.13.1.69. [DOI] [PubMed] [Google Scholar]
- Rothert K, Strecher VJ, Doyle LA, Caplan WM, Joyce JS, Jimison HB, et al. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity. 2006;14(2):266–272. doi: 10.1038/oby.2006.34. [DOI] [PubMed] [Google Scholar]
- Ruggiero JS. Health, work variables, and job satisfaction among nurses. Journal of Nursing Administration. 2003;35:254–263. doi: 10.1097/00005110-200505000-00009. [DOI] [PubMed] [Google Scholar]
- Schaefer KM, Peterson K. Effectiveness of coping strategies among critical care nurses. Dimensions of Critical Care Nursing. 1992;11(1):28–34. doi: 10.1097/00003465-199201000-00005. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- Snow DL, Swan SC, Wilton L. A workplace coping-skills intervention to prevent alcohol abuse. In: Bennett J, Lehman WEK, editors. Beyond drug testing: Innovative approaches to dealing with employee substance abuse. Washington, DC: American Psychological Association; 2003. pp. 57–96. [Google Scholar]
- Stordeur S, D'Hoore W, Vandenberghe C. Leadership, organizational stress, and emotional exhaustion among hospital nursing staff. Journal of Advanced Nursing. 2001;35(4):533–542. doi: 10.1046/j.1365-2648.2001.01885.x. [DOI] [PubMed] [Google Scholar]
- Tabak N, Orit K. Relationship between how nurses resolve their conflicts with doctors, their stress and job satisfaction. Journal of Nursing Management. 2007;15(3):321–31. doi: 10.1111/j.1365-2834.2007.00665.x. [DOI] [PubMed] [Google Scholar]
- Upenieks VV. The interrelationship of organizational characteristics of magnet hospitals, nursing leadership, and nursing job satisfaction. Health Care Manager. 2003;22:83–98. doi: 10.1097/00126450-200304000-00002. [DOI] [PubMed] [Google Scholar]
- Van Bogaert P, Adriaenssens J, Dilles T, Martens D, Van Rompaey B, Timmermans O. Impact of role-, job- and organizational characteristics on Nursing Unit Managers’ work related stress and well-being. Journal of Advanced Nursing. 2014:2622–2633. doi: 10.1111/jan.12449. [DOI] [PubMed] [Google Scholar]
- Wakim N. Occupational stressors, stress perception levels, and coping styles of medical surgical RNs: a generational perspective. Journal of Nursing Administration. 2014;44(12):632–9. doi: 10.1097/NNA.0000000000000140. [DOI] [PubMed] [Google Scholar]
- Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, Mcghee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. Journal of Medical Internet Research. 2004 Nov 10;6(4) doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb T, Joseph J, Yardley L, Michie S. Using the Internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12(1):e:4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]