Abstract
Background and Purpose
The long-term effectiveness of both operative and non-operative management approaches for Chronic Exertional Compartment Syndrome of the lower legs (CECS) is moderate at best. Positive outcomes have recently been reported on modifying running technique in individuals with CECS. The purpose of this case series was to evaluate a training program aimed at changing marching technique in individuals with CECS, based on principles that aim to eliminate heel strike and decrease impact during foot strike.
Study Design
Case series.
Methods
Six service members with CECS underwent a five-week training program aimed at modifying marching technique. The program was comprised of foot/lower leg strengthening exercises, perception drills, and treadmill/outdoor marching bouts. Self-assessed leg condition, march endurance performance, and kinematic/kinetic measurements were assessed at baseline (T0), post-treatment (T5), and nine months post-intervention (T40).
Results
Moderate to fair pre- to post improvements on the self-assessed leg condition outcomes were demonstrated for most participants (4% to 73% improvements). These scores continued to improve until the 9 months follow-up. Marching performance improved during the intervention period in all but one subject, ranging from 6% to 38% improvement in marching time. Kinematic and kinetic data showed pre- to post-intervention changes that were reflective of the marching technique modification in most subjects. Post-intervention pain profiles of participants during marching showed that, in most subjects, the onset of leg pain was delayed compared to baseline.
Conclusions
A five-week intervention aimed at altering marching technique has demonstrated moderately promising results in a group of service members with CECS of the lower legs who had previously undergone other conservative management interventions without success. Due to the relatively small sample size and the variability in subject outcomes, further research is warranted.
Level of Evidence
4
Keywords: Chronic exertional compartment syndrome, lower leg, marching technique
INTRODUCTION
Lower extremity overuse injuries are a widespread problem in the military, commonly occurring in new recruits and infantry soldiers.1 Physical training and sports related activities account for up to 90% of all injuries and 80% of those injuries are considered overuse in nature.2,3,4 One of the overuse injuries consistent with the military lifestyle is chronic exertional compartment syndrome (CECS).5 This condition is classically prevalent with activities such as running and marching while carrying a load.6
CECS is an obstinate and theoretically multi-factorial musculoskeletal injury.4,7 The classic symptom of CECS is a complaint of increasing lower leg pain during physical exertion, cramping, burning or aching in nature, and often leading to premature cessation of activity.7 Neurological symptoms, such as numbness or muscle weakness in the lower legs, are only present in some cases and vary depending on which nerve is involved.8 Physical signs and symptoms at rest are often absent. Amateur athletes who are hampered in their training activities by CECS often modify, decrease, or even stop these activities in an effort to avoid CECS symptoms.4,9 Unfortunately, the military operational tempo does not allow for significant modifications of training activities. Eventually, this may lead to chronicity of the problem and eventual attrition from military duty.
The long-term effectiveness of conservative treatment interventions such as orthotics, massage, and stretching remains less than optimal.10,11,12 Surgical management by means of a fasciotomy, in which the fascia is cut to relieve Intra-Compartmental Pressure (ICP), has proven to be a somewhat effective treatment approach in CECS management.11,13 However, up to 17% of subjects undergoing fasciotomy experience less than favorable outcomes, such as decreased sensation or hypersensitivity over the incision site, numbness at the lateral lower leg, ankle pain, and reoccurrence of symptoms.10,14,15 Moreover, there are risks and complications associated with surgery, such as hemorrhage, infection, or nerve damage, and a significant hiatus from activity; not to mention the burden that postoperative rehabilitation has on military readiness.8,15 The prognosis, in terms of returning to an adequate level of military infantry readiness, is moderate at best.16,17 This gives reason to further investigate effective conservative management approaches.
As an alternative to surgical interventions, Diebal et al10,18 have recently reported positive outcomes in U.S. military members diagnosed with CECS by modifying their running technique. A six-week training program was used to implement a forefoot running technique in order to eliminate heel strike and have the foot contact the ground as close to under the general center of mass as possible. This program led to decreased post-exercise ICP values, significant reductions in pain and disability, and improved performance outcomes on run tests. More importantly, surgical intervention was avoided for all subjects at the one-year follow-up. If a modification of running technique shows therapeutic benefits for subjects with CECS, potentially a modification of marching/walking technique could elicit the same results. This may be relevant for civilian athletes participating in long distance walking events who also suffer from fatigue-related overuse leg injuries.19,20
The rationale for this type of intervention is that most runners have a habitual heel strike pattern, with a long stride length, slow cadence, and an excessive dorsiflexion of the ankle at ground contact. This places the runner in a position of terminal knee extension and ankle dorsiflexion at landing, which results in marked increased eccentric activity of the anterior compartment muscles of the lower leg, in particular the tibialis anterior muscle. Ultimately, the combination of knee extension and ankle dorsiflexion may lead to CECS symptoms in repetitive movements such as running.21 In order to eliminate the terminal knee extension and ankle dorsiflexion position at heel contact, a forefoot running technique is suggested. This method focuses on changing running style from a heel strike pattern toward a forefoot strike pattern (i.e., landing on the ball of foot), by performing various drills and exercises to get the runner to contact the ground with the foot as close to under the center of mass as possible. Instructions include decreasing stride length by increasing cadence (to 180 steps per minute) and pulling the foot from the ground with the hamstring muscles, thereby eliminating push off with the gastroc-soleus muscles. These adaptations have been shown to decrease weight acceptance rates, minimize ground contact time and vertical displacement, and eliminate the rearfoot strike that causes the eccentric loading of the anterior compartment musculature of the lower leg.10,22,23,24,25
Following the studies by Diebal et al,10,18 a series of case reports have been conducted to evaluate the effectiveness of the forefoot running intervention strategy in Dutch service members with CECS.25 In 19 subjects, a 6-week forefoot running intervention performed in both center-based and home-based training settings led to decreased post-running lower leg ICP values and improved run performance (distance). The pain and disability typically associated with CECS were significantly reduced.
Unfortunately, a substantial subset of recruits and infantry soldiers with CECS report that their lower leg complaints are caused and prolonged by (forced) marching activities, as opposed to running activities. In an effort to resolve this dilemma, a five-week training program was constructed aimed at changing marching technique, while integrating movement principles derived from a forefoot running technique. The purpose of this study was to evaluate a training program based on principles that aim to eliminate heel strike and decrease impact during foot strike aimed at changing marching technique in military service members with CECS.
METHODS
Subjects
From January to April 2014, military service members from the Royal Netherlands Army, diagnosed with CECS by a general surgeon of the Central Military Hospital in Utrecht, The Netherlands, were sent to the Military Sports Medical Center in Utrecht to be assessed for inclusion. To be included in this study, subjects had to report a two-month history of recurrent anterior and/or lateral leg pain and tightness in one or both legs that was exacerbated with marching activities. Pain had to occur in the first 15 minutes of marching and had to lead to the termination of the marching activity. In addition, all symptoms had to completely resolve within 15 minutes after the cessation of marching activity. The physical examination findings had to be normal at rest (i.e., full ankle and knee range of motion and strength and full functional ability to squat and hop without symptoms). Finally, the intracompartmental pressure at one minute after a standardized exercise protocol had to be above 35 mmHg in at least one anterior compartment. Exclusion criteria included: a history of previous fasciotomy or other lower extremity surgery, any condition that would cause lower extremity swelling, creatine supplementation in the previous two months, any injury that would affect marching tolerance besides CECS, a current use of nonsteroidal anti-inflammatory drugs (NSAID's) that would interfere with test outcomes, and co-interventions such as other exercise therapy modalities in the two weeks preceding the baseline measurements through the post-intervention measurements of this study. Each participant was given a verbal and written explanation of the study protocol and provided informed consent prior to testing.
Pre-Intervention Measurements (T0)
Intracompartmental Pressure Measurements and Biometry
To objectify and confirm the clinical diagnosis of CECS, one-minute post-exercise ICPs of the anterior compartments were measured, following a standardized treadmill run test protocol as described by Zimmermann et al.27 Baseline measurements included biometric parameters: body height, body weight, fat percentage (skinfold measurement28), waist circumference, and blood pressure. Measurements were performed by the same (experienced) practitioner to avoid inter-rater reliability issues.
Self-assessed Leg Condition and Physical Activity
Participants filled out the following self-report questionnaires:
The Single Assessment Numeric Evaluation (SANE),10 a one-item question rating the lower leg condition on a 0-100 scale, with 100 being normal.
The Lower Leg Outcome Survey (LLOS),10 a 20-item scale questionnaire that specifically evaluates leg conditions such as CECS, with a range of scores between 0-60, a score of 60 being normal.
The Subject Specific Complaints (PSC) questionnaire,29 in which, from a list of different daily activities, subjects had to select the one to three most important activities that were hampered by their leg complaints in the past week, and rate them on a 100 mm visual analogue scale (VAS).
The validated Short Questionnaire to Assess Health Enhancing Physical Activity (SQUASH),30 measuring the degree of daily physical activity (subdivided into following categories: commuting activities, work activities, household activities, leisure time activities, and sports activities), and expressed as activity scores per week.
Marching Performance and Kinematic/Kinetic Measurements
Approximately one week after the ICP measurements were taken in the hospital, participants performed a baseline marching test on an instrumented treadmill (Zebris FDM-T, GmbH, Isny im Allgäu; calibrated in January 2014) at the Sports Medical Center. During the test, participants wore shorts, a t-shirt, military boots, and carried a backpack containing 21 kg of total weight. After a five-minute treadmill warm-up without a backpack at 4.5 km/h, participants started marching at 5.0 km/h. Treadmill speed was increased every 10 minutes by 0.5km/h for up to 60 minutes of marching. Kinematic data (i.e., step length, cadence, time of load change from heel to forefoot during the stance phase) and kinetic data (i.e., maximum force in heel area) were collected for one minute in the second minute of each stage; data from the last complete stage was reported. Verbal pain scores on a 0-10 scale were gathered at the end of each minute during the whole marching test. The test was aborted when participants reached 60 minutes of marching, when they reported a pain score of seven or more (out of 10) in at least one of four lower leg regions (anteriomedial, anteriolateral, posteriomedial, and posteriolateral), or when they asked to stop due to reaching their cardiorespiratory limit. Verbal pain scores were also asked at one, five, and 10 minutes following marching cessation.
Intervention
Immediately after informed consent was obtained, two weeks preceding the first training session, participants were instructed on core stability and strengthening exercises for the feet and lower legs. These exercises were used to prepare the lower body for the new marching technique. A training schedule and log was utilized to increase subject compliance with performing these exercises at home on a daily basis prior to the initiation of the marching program. Participants were instructed to continue these exercises every other day throughout the five-week training period. Prior to the first marching session, a physical therapist examined all participants to ensure that all physical findings were still within normal limits before starting the marching activities. The first training session was also used to provide a detailed rationale to the subject regarding the concepts used in the intervention program.
After these preliminary events, a five-week training program aimed at altering marching technique was provided by a team of specialists, which included a physical therapist, a human movement scientist, and a medical student. The aims of the marching program were to train the participants to march with a higher cadence, shorter strides, and relaxed foot and lower leg muscles, in order to decrease the work load of the anterior compartment musculature when marching. Appendices 1 to 5 present the intervention protocol and typical examples of the exercises and drills used in this study.
Five weeks of training was chosen as the optimal intervention length, based on previous experiences within the sports medical center with treating lower leg subjects using marching activities [W. Zimmermann, unpublished data, 2010-2013]. The training program consisted of 11 training sessions of 90 minutes each in a five-week period. Six trainings sessions took place at the research center. For the remaining five training sessions, participants exercised at their own military base or at home, utilizing a training log that contained descriptions of each exercise as well as the training protocol.
Training sessions consisted of the following elements (Appendices 2-5): waist-down joint flexibility exercises; perception drills (focusing on issues such as perception of body weight and pressure on the ball of the foot, vertical joint alignment, and falling forward); marching bouts on the treadmill; outdoor marching bouts on track and dirt roads. Time spent on exercises and drills remained constant (approx. 50 minutes), whereas the intensity and the amount of time spent on marching sessions increased throughout the program (from 20 up to 35 minutes). All training sessions were concluded with 10 minutes of regular stretching exercises for the muscles of the lower legs tailored to the needs of the subject.
For proprioceptive purposes, all exercises and drills were performed barefoot. Participants performed the first few training sessions barefoot, followed by training sessions with running shoes, military boots, and military boots with additional gear (military uniform, backpack), respectively. Both verbal and written information about how to lace up military boots was provided by an orthopedic shoe technician at the first training session. Lacing military boots too tightly, especially around the distal lower leg, may potentially obstruct blood flow and increase CECS complaints.
Besides verbal cues (e.g., “take shorter strides”, “increase step frequency”, “relax the foot”, “don't bend at the waist”), a digital metronome (training center) or a metronome-app (home based) was used to pace the cadence at 125 to 130 steps per minute. This pace interval was based on previous experiences with treadmill marching activities in CECS subjects at the laboratory. At several training sessions, an EMG device (BTS FREEWALK, Brooklyn NY, USA) was used as a monitoring device to provide participants real-time visual feedback of the activity of their tibialis anterior muscles during marching. Additionally, throughout the training program, marching time and speed were gradually increased.
Post-intervention Measurements (T5, T40)
In the fifth week, one week after the last training session, all baseline measurements (i.e., biometry, questionnaire, marching test) were repeated (T5). The protocols were identical to those used to obtain the baseline measurements, i.e., marching tests were executed using identical speed increments and termination criteria as previously described. A Global Rating of Change (GROC)31 was also collected following the five week intervention. The GROC is a 15-point scale to measure the subjects’ perceived change and overall improvement, from ‘a very great deal worse’ (score −7) to ‘a very great deal better’ (score + 7).
Nine months post-intervention (T40), participants were asked to fill in a follow-up questionnaire consisting of the SANE, LLOS, PSC, SQUASH, and GROC, as well as answer additional questions regarding (medical) treatment activities in the post-intervention period.
Statistics
Descriptive analyses were used to describe possible pre- to post-differences (T0–T5 and T0–T40) in outcomes. No statistical testing was used considering the design and sample size of the study.
RESULTS
Subject characteristics
From February to June 2014, six male subjects were enrolled in the study: two air mobile infantry soldiers, two mounted infantry soldiers, one marine, and one signal service member. Table 1 presents baseline clinical characteristics of each included subject. Mean baseline and post-intervention values for biometry (weight, body fat, blood pressure) and level of physical activity are displayed in Table 2.
Table 1.
Baseline subject characteristics.
| Subject no. | Age (yrs) | Height (cm) | Duration of complaints (months) | Location of complaints* | Type of complaints† | Previous Treatments‡ |
|---|---|---|---|---|---|---|
| 1 | 22 | 178.5 | 9 | Left = Right | CECS | A,B,C,D,E,F |
| 2 | 19 | 172.5 | 36 | Left = Right | CECS > MTSS | A,B,C,E,F |
| 3 | 18 | 179.0 | 6 | Left < Right | CECS > MTSS | A,B,E,F |
| 4 | 19 | 171.5 | 18 | Left < Right | CECS | A,B,C |
| 5 | 21 | 173.5 | 15 | Left > Right | CECS | A,B |
| 6 | 27 | 187.5 | 24 | Left < Right | CECS > MTSS | A,B,C,E |
CECS = Chronic Exertional Compartment Syndrome; MTSS = Medial Tibial Stress Syndrome
- * Left = Right means same level of CECS symptoms in both leg; Left < Right means CECS symptoms more pronounced in right lower leg; Left > Right means CECS symptoms more pronounced in left lower leg
- † CECS > MTSS means: mainly CECS, some MTSS symptoms
- ‡ Previous treatment modalities: A = Rest; B = Physical therapy; C = Orthotics/modified shoes; D = Compression stockings; E = Shockwave; F = Dry-needling
Table 2.
Baseline (T0), 5-week post-intervention (T5), and 10-month follow-up (T40) measurements of biometry and physical activity for the six subjects. Mean values ± SD are presented.
| T0 | T5 | T40 | |
|---|---|---|---|
| Weight (kg) | 74.5 ± 3.6 | 74.8 ± 3.4 | – |
| Body fat (%) | 15.5 ± 3.7 | 15.8 ± 3.8 | – |
| BPS (mmHg) | 132 ± 8 | 134 ± 7 | – |
| BPD (mmHg) | 71 ± 8 | 71 ± 7 | – |
| SQUASH (activity score) | 8047 ± 4720 | – | 14413 ± 4561 |
BPS = Systolic blood pressure; BPD = Diastolic blood pressure; SQUASH = Short Questionnaire to Assess Health-enhancing physical activity score
For most subjects, the onset of CECS symptoms could be traced back to basic military training and the duration of their complaints ranged from six months up to three years. Three subjects had minor symptoms of medial tibial stress syndrome (MTSS) along with their CECS complaints, although CECS was seen as the primary affliction. All subjects had already undergone several treatment modalities, ranging from rest to specific physical therapy (e.g., stretching, Shockwave therapy). None of the previous treatments were successful in diminishing their CECS complaints. Exaggerated stride lengths and a significant heel strike during marching were observed in all subjects at the baseline marching test. At baseline, only one of the six subjects succeeded in finishing the 60-minute marching test. This individual had the longest period without physical activities prior to inclusion in the study (12 weeks) compared to the other study subjects (1 to 6 weeks).
Treatment compliance
The treatment period was comprised of five consecutive weeks and included six center-based training sessions and five home-based training sessions. Four out of six subjects fully complied with the treatment protocol. One subject performed only four of the five home-based training sessions due to operational activities, and the post-intervention measurements were delayed by one week in another subject due to a rescheduled vacation.
Pre- to post-intervention results
All but one participant (Subject 5 from Table 1) showed moderate to fair improvements from pre- to post-intervention on the self-assessed leg condition outcome tool. Table 3 displays the overall group results: + 4% to + 33% for SANE, + 4% to + 33% for LLOS and −13% to −73% for PSC. These improvements correspond to the reported post-intervention GROC scores: + 3 (‘somewhat better’) in two subjects, + 4 (‘moderately better) in one subject, + 5 (‘quite a bit better’) in two subjects, and +6 (‘a great deal better’) in one subject. Only minor pre- to post-intervention changes in biometric and blood pressure values were seen in the study group. The three subjects diagnosed with a combination of CECS and MTSS reported that they were not hindered by their MTSS symptoms during the treatment period.
Table 3.
Baseline (T0), 5-week post-intervention (T5), and 10-month follow-up (T40) measurements of self-assessed leg condition for the six subjects. Mean values ± SD are presented.
| T0 | T5 | T40 | |
|---|---|---|---|
| SANE | 66.7 ± 6.1 | 73.3 ± 19.1 | 86.7 ± 9.8 |
| LLOS | 44.3 ± 5.8 | 51.2 ± 5.6 | 53.8 ± 6.0 |
| PSC1 | 70.5 ± 26.9 | 37.3 ± 15.0 | 22.5 ± 16.7 |
| PSC2 | 64.0 ± 27.3 | 28.7 ± 29.0 | 19.2 ± 25.2 |
| PSC3 | 36.0 ± 27.9 | 26.5 ± 29.5 | 18.5 ± 40.2 |
SANE = Single Assessment Numeric Evaluation (range 0 to 100); LLOS = Lower Leg Outcome Survey (range 0 to 60); PSC = Patient Specific Complaints survey (3 items, range per item 0 to 100)
Marching performance improved during the five-week intervention period in all but one subject (Subject 5 from Table 1), ranging from 6% to 38% increase in marching duration. Table 4 presents the mean group results across all subjects. Moreover, kinematic and kinetic data showed pre- to post-intervention changes that were reflective of the marching technique modification (i.e., shorter strides, higher cadence, decreased loading of the heel at ground contact) in all but two subjects (Subjects 1 and 5).
Table 4.
Baseline (T0) and 5-week post-intervention (T5) measurements of marching performance and kinetics/kinematics for the six subjects. Kinematic and kinetic parameters are presented as averages of left and right leg of a normalized gait cyle.
| Performance | T0 (Mean ± SD) | T5 (Mean ± SD) |
|---|---|---|
| March time (min:s) | 38:07 ± 11:06 | 41:40 ± 9:49 |
| Step length (cm) | 85.4 ± 5.1 | 81.4 ± 4.2 |
| Cadence (steps/min) | 124 ± 11 | 130 ± 10 |
| Fmax (N) | 965 ± 48 | 965 ± 58 |
| Time H-FF (%) | 42.9 ± 6.8 | 40.8 ± 9.0 |
| PH-max (N/cm2) | 39.3 ± 1.8 | 38.0 ± 3.2 |
Fmax = Vertical reaction force; Time H-FF = Load change from heel to forefoot in percentage of total stance phase time; PH-max = Maximum heel pressure
Figure 1 demonstrates the lower leg pain profiles for each subject during the marching test at pre- and post-intervention measurements. In all but two subjects (Subjects 5 and 6), the onset of pain in the bilateral compartments of the lower legs was delayed at the post-intervention measurements compared to baseline. Subject 5 showed an earlier onset of pain for his left leg post-treatment, which may have been the result of a substantially longer rest period prior to baseline. Subject 6 did not show pre- to post- intervention differences.
Figure 1.
Pain profiles of subjects during pre-intervention marching test (grey line) and five-week post-intervention measurement (black line). Subjects’ lateral compartment pain scores are presented, on a verbal 0-10 scale, for both lower legs. Subjects reported pain levels each minute of the test till marching cessation (cross). Subject numbers (1 to 6) correspond to those presented in Table 1.
Nine-Month Follow-up Results
Due to logistical reasons, the follow-up periods varied between participants, ranging from 33 to 44 weeks (9 months on average). Each participant showed improvements in their self-reported outcomes at the end of the follow-up period, compared with the post-intervention measurements (Table 3). These additional improvements were consistent with the follow-up GROC scores: + 1 (‘a tiny bit better’) in one subject, + 5 (‘quite a bit better’) in one subject, + 6 (‘a great deal better’) in two subjects, and +7 (‘a very great deal better’) in two subjects. As shown in Table 2, the activity scores per week also showed an increase at the follow-up measurement compared to the baseline values: from 8,047 points ± 4,720 to 14,413 points ± 4,561. All subjects improved their levels of physical activity at work. Three participants decreased the time spent on sports activities (mainly strength and conditioning training) for this reason.
Results from additional questions at the follow-up measurement regarding the nine-month follow-up period showed that three participants continued exercising their legs on their own terms, one participant was trained by a physical trainer, and two participants (Subject 4 with post-treatment GROC score + 5, and Subject 6 with post-treatment GROC score + 4) underwent a fasciotomy five months and four months post-treatment, respectively, with an accompanying rehabilitation program. Without surgical release, both subjects were judged to be not enough physically assessable to continue their military career. All but Subject 6 continued using the marching principles that were taught during the study in their marching activities during follow-up; four of them used the training schedule that was issued to them at the post-treatment measurement. One participant (Subject 4) used medication for his lower leg symptoms during the follow-up period. No participant reported other lower leg complaints during follow-up.
DISCUSSION
A five-week treatment program aimed at changing marching technique was studied in a group of six Dutch military service members with CECS of the lower legs. The study hypothesis was that the marching intervention would lead to increased marching performance/tolerance and decreased pain levels due to reduced muscular demand in the anterior compartments of the lower legs. Although not universal, on average, small post-treatment improvements were found for the self-assessed lower leg condition outcomes, marching performance, and accompanying lower leg pain profiles. Kinematic and kinetic data showed changes that reflected the marching technique modification. The self-assessed outcomes continued to improve in all subjects in the months following the end of the intervention, during which two of them proceeded to undergo fasciotomy.
To the authors’ knowledge, this is the first study to focus on modification of marching technique as a potentially beneficial conservative treatment for CECS. In a comprehensive systematic review on prevention strategies for training-related injuries in military and other active populations, Bullock et al3 listed “manipulation of running stride length” among the intervention strategies without sufficient evidence to recommend such an intervention. In more recent studies, promising findings have been reported regarding the reduction in joint loading at foot strike via step rate manipulation in running activities.32,33 Diebal et al10,18 have reported on the therapeutic effects of a six-week running intervention using similar principles (e.g., shortening stride length, increasing cadence) in the U.S. Army. Pain and disability typically associated with CECS were greatly reduced up to one year after intervention, avoiding fasciotomy in all subjects. These findings were largely confirmed in a similar running intervention study in Dutch service members with CECS.26
It is well understood that differences exist between running and marching kinetics and kinematics. Compared to marching/walking, running is characterized by faster speeds, longer strides, and greater impact forces. The most prominent characteristic of running is the double float phase, where neither foot is in contact with the ground; thereby leaving more room for manipulating stride length and changing foot strike patterns (e.g., from rearfoot to forefoot). A forefoot strike is virtually impossible while walking, especially at higher speeds. Nonetheless, it was noticed in this study that subject instruction on marching at an increased cadence (i.e., shorter strides) could be effective in itself in reducing the negative impact of CECS, especially when combined with the instruction to leave the foot in a relaxed position during the swing phase. It was observed that all participants initially had the tendency to hold their ankles in a pronounced dorsiflexed state throughout the gait cycle. The study findings indicate that short- and mid-term improvements in marching performance and self-assessed lower leg condition may occur even with relatively small and seemingly insignificant changes in kinematic parameters (4 cm mean decrease in stride length and 6 steps/min mean increase in cadence, see Table 4).
Two subjects showed relatively low compliance to marching technique modification: Subject 1 reported a slightly higher level of lower leg complaints at the post-intervention measurement, likely due to participation in snowboarding activities in the preceding week. Subject 5 entered the study after a relatively long period of rest, with no marching activities whatsoever, compared with the other participants. His CECS symptoms gradually started to increase throughout the treatment period, which may explain both the decline in self-assessed leg condition and lower compliance to the new marching technique at the post-intervention measurement.
The individual pain profiles suggest that this five-week intervention enables less development of pain while marching at progressive speeds, although it may not completely prevent the development of CECS complaints during a marching bout. Still, this delay in the onset of and progression of pain may be of value for recruits and soldiers who are subject to unit events that involve regular marching activities. However, as shown in two of the participants, even successful modification of marching technique with regard to pain reports may not prevent a surgical release in the long run, despite a favorable post-treatment pain profile or global rating of change score.
All findings must be seen in the light of weaknesses in the study design concerning the small sample size, lack of control group, and relatively short follow-up period. This study was built around a case series, for which patients were referred by the military hospital within a limited time frame. The total number of subjects participating in this (pilot) study was limited mainly due to logistic constraints in terms of staff capacity and facilities.
CONCLUSIONS
The results of this case series indicate that a five-week intervention aimed at altering elements of marching technique may be beneficial in individuals with long-lasting lower leg CECS complaints who have previously undergone other conservative management interventions without success. The relatively small sample size and the variability in subject outcomes within the program, demonstrate the necessity for follow up (controlled) studies with larger cohorts of subjects.
APPENDIX 1.
Protocol of the Treatment Intervention Program
| Session | Location | Exercises |
|---|---|---|
| Week -1 | Research center |
|
| Week 1: Wednesday | Research center |
|
| Week 1: Friday | Research center |
|
| Week 2: Monday | Research center |
|
| Week 2: Wednesday | Home base |
|
| Week 2: Friday | Research center |
|
| Week 3: Monday | Research center |
|
| Week 3: Wednesday | Home base |
|
| Week 3: Friday | Research center |
|
| Week 4: Monday | Home base |
|
| Week 4: Wednesday | Home base |
|
| Week 4: Friday | Research center |
|
| Week 5: Monday | Home base |
|
| Week 5: Wednesday | Research center |
|
APPENDIX 2.
Lower Leg Strengthening Exercises
|
Foot Arch Exercise (‘doming’) Instruction: Press the underneath side of the small knuckles of the toes down into the floor, making the main knuckles closest to the foot raise up like a dome. The toes need to stay long and straight, without curling under. |
 |
||||
|
Towel grab with toes Instruction: Curl a towel in the pointed direction, only using the toes. |
 |
||||
|
Toe spreading Instruction: Spread all toes as far as possible and hold for a few seconds. |
 |
||||
|
Calf raises Instruction: Lift the heels until standing on the toes |
 |
||||
| Example of a training schedule (every second or third day): | |||||
| Week | Frequency | Doming | Towel grab | Toe spreading | Calf raises |
| 1 | 2x | 10 reps | 3 x 5 reps | 5 reps | 3 x 5 reps |
| 2 | 2x | 13 reps | 3 x 8 reps | 8 reps | 3 x 8 reps |
| 3 | 3x | 13 reps | 3 x 8 reps | 8 reps | 3 x 8 reps |
| 4 | 3x | 15 reps | 3 x 13 reps | 10 reps | 3 x 13 reps |
APPENDIX 3.
Core Strengthening Exercises
|
Body Squats Instruction: Bend the knees, allowing the body to sink towards the ground as if sitting in a chair, not further than with the thighs parallel to the floor. |
 |
||||
|
Dynamic plank Instruction: From a starting position with the forearms to the ground and the body in a straight line, move the hips down and up, holding at each position for a few seconds. |
 |
||||
|
Dynamic bridge Instruction: Leaning on hands and heels, move the hips up and down, holding at each position for a few seconds. |
 |
||||
|
Side bridge Instruction: Leaning on left forearm and outside of the foot, move the hips up, holding for a few seconds, and down, holding for a few seconds. Change position to right forearm and repeat the exercise. |
 |
||||
| Example of a training schedule (every second or third day): | |||||
| Week | Frequency | Body squats | Dynamic plank | Dynamic bridge | Side bridge |
| 1 | 2x | 3 x 5 reps | 3 x 3 reps | 3 x 3 reps | 2* x 3 x 3 reps |
| 2 | 2x | 3 x 8 reps | 3 x 4 reps | 3 x 4 reps | 2* x 3 x 4 reps |
| 3 | 3x | 3 x 12 reps | 3 x 5 reps | 3 x 5 reps | 2* x 3 x 5 reps |
| 4 | 3x | 3 x 15 reps | 3 x 6 reps | 3 x 6 reps | 2* x 3 x 6 reps |
| * 1x left, 1x right | |||||
APPENDIX 4.
Perception Exercises
|
Perception Body Weight Drill (3x 10 s) Instruction: Lean forward towards the toes and backward towards the heel, thereby identifying where the pressure is located. |
 |
|
Bouncing in Place Drill (3x 10 s) Instruction: Bounce lightly on the ball of the feet without leaving the ground, brushing the ground with the heels. |
 |
|
Fall to Wall Drill (10 reps) Instruction: Fall from the hips, keeping the body in a straight line, with knees and ankles in the same position throughout the fall (lifting the heels). |
 |
| These drills have been derived from the Pose Method® Drills (Romanov, N. Dr. Nicholas Romanov's Pose Method of Running: A New Paradigm of Running. Pose Tech Corp; 2002) | |
APPENDIX 5.
Flexibility Exercises
|
Hip flexibility exercise I (10 reps) Instruction: Make rotational movements with the hips, both clockwise and anticlockwise, keeping the feet flat on the floor and keeping the head still. |
 |
|
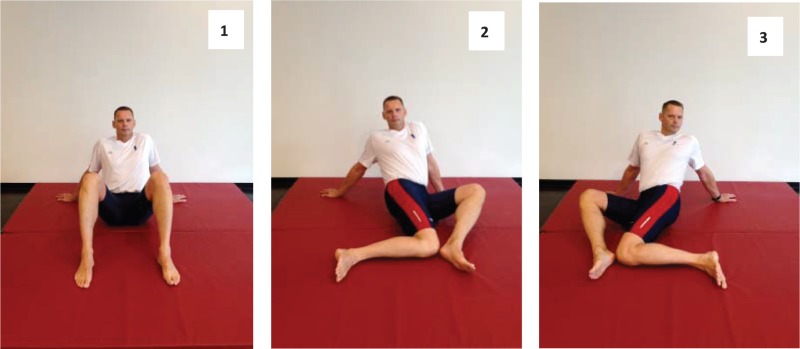
Hip flexibility exercise II (2x 5 reps) Instruction: On hands and feet (picture 1), touch the floor alternately with the left thigh (picture 2) and right thigh (picture 3), while turning on the feet. |
 |
|
Hip flexibility exercise III (2x 5 reps) Instruction: With bended knees (picture 1), rotate the legs inwardly and touching the floor alternately with the right knee (picture 2) and left knee (picture 3). |
 |
|
Hip-knee-ankle flexibility exercise (2x 5 reps) Instruction: On one leg, hold the foot in front of the body (picture 1), rotating the knee underneath the arm (pictures 2-3) to the front, with the foot behind the buttocks (picture 4), and back to the starting position. Additional support against a wall is allowed. |
 |
 |
|
Knee-ankle flexibility exercise (10 reps) Instruction: With the knees bent and touching each other, make circles both clockwise and anticlockwise, while keeping the feet flat on the ground. |
 |
REFERENCES
- 1.Sharma J, Greeves JP, Byers M, et al. Musculoskeletal injuries in British army recruits. BMC Musculoskeletal Disord. 2015;16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts A, Franklyn-Miller A. The validity of the diagnostic criteria used in chronic exertional compartment syndrome: A systematic review. Scand J Med Sci Sports. 2012;22(5):585-95. [DOI] [PubMed] [Google Scholar]
- 3.Bullock SH, Jones BH, Gilchrist J, et al. Prevention of physical training-related injuries: recommendations for the military and other active populations based on expedited systematic reviews. Am J Prev Med. 2010;38(1 Suppl):S158-81. [DOI] [PubMed] [Google Scholar]
- 4.Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surg. 2003;11(4):268-76. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann WO, Helmhout PH, Beutler A. Prevention and treatment of exercise related leg pain in young soldiers. J R Army Med Corps 2016, pre-publication online. [DOI] [PubMed] [Google Scholar]
- 6.Dharm-Datta S, Minden DF, Rosell PA, et al. Dynamic pressure testing for CECS in the UK military population. J R Army Med Corps 2013;159:114-118. [DOI] [PubMed] [Google Scholar]
- 7.Schubert AG. Exertional compartment syndrome: Review of the literature and proposed rehabilitation guidelines following surgical release. Int J Sports Phys Ther. 2001;6(2):126-41. [PMC free article] [PubMed] [Google Scholar]
- 8.Blackman PG. A review of chronic exertional compartment syndrome in the lower leg. Med Sci Sports Exerc. 2000;32(3 Suppl):S4-10. [DOI] [PubMed] [Google Scholar]
- 9.Barnes M. Diagnosis and management of chronic compartment syndromes: A review of the literature. Br J Sports Med. 1997;31(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diebal AR, Gregory R, Alitz C, et al. Forefoot running improves pain and disability associated with chronic exertional compartment syndrome. Am J Sports Med. 2012;40(5):1060-7. [DOI] [PubMed] [Google Scholar]
- 11.Tucker AK. Chronic exertional compartment syndrome of the leg. Curr Rev Musculoskelet Med. 2010;3(1-4):32-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farr D, Selesnick H. Chronic exertional compartment syndrome in a collegiate soccer player: A case report and literature review. Am J Orthop. 2008;37(7):374-7. [PubMed] [Google Scholar]
- 13.Scheltinga MR, Fijter MW de, Luiting MG. Minimally invasive fasciotomy in chronic exertional compartment syndrome and fascial hernias of the anterior lower leg: Short-and long-term results. Mil Med. 2006;171(5):399-403. [DOI] [PubMed] [Google Scholar]
- 14.Waterman BR, Laughlin M, Kilcoyne K, et al. Surgical treatment of chronic exertional compartment syndrome of the leg: failure rates and postoperative disability in an active subject population. J Bone Joint Surg Am. 2013;95(7):592-6. [DOI] [PubMed] [Google Scholar]
- 15.Howard JL, Mohtadi NG, Wiley JP. Evaluation of outcomes in subjects following surgical treatment of chronic exertional compartment syndrome in the leg. Clin J Sports Med. 2000;10(3):176-84. [DOI] [PubMed] [Google Scholar]
- 16.Zimmermann WO, Helmhout PH, Harts CC. [Guidelines for the prevention and treatment of overload injuries of the lower legs in young military service members.] Sport & Geneeskunde. 2015;1:6-19. [In Dutch] [Google Scholar]
- 17.Dunn JC, Waterman BR. Chronic exertional compartment syndrome of the leg in the military. Clin Sports Med. 2014;33(4):693-705. [DOI] [PubMed] [Google Scholar]
- 18.Diebal AR, Gregory R, Alitz C, et al. Effects of forefoot running on chronic exertional compartment syndrome: a case series. Int J Sports Phys Ther. 2011;6(4):312-21. [PMC free article] [PubMed] [Google Scholar]
- 19.Gefen A. Biomechanical analysis of fatigue-related foot injury mechanisms in athletes and recruits during intensive marching. Med Biol Eng Comput. 2002;40(3):302-10. [DOI] [PubMed] [Google Scholar]
- 20.Stolwijk NM, Duysens J, Louwerens JW, et al. Plantar pressure changes after long-distance walking. Med Sci Sports Exerc. 2010;42(12):2264-72. [DOI] [PubMed] [Google Scholar]
- 21.Tsintzas D, Ghosh S, Maffulli N, et al. The effect of ankle position on intracompartmental pressures of the leg. Acta Orthop Traumatol Turc. 2004;43(1):42-8. [DOI] [PubMed] [Google Scholar]
- 22.Romanov N, Fletcher G. Runners do not push off the ground but fall forwards via a gravitational torque. Sports Biomech. 2007;6(3):434-52. [DOI] [PubMed] [Google Scholar]
- 23.Daoud AI, Geissler GJ, Wang F. Foot strike and injury rates in endurance runners: A retrospective study. Med Sci Sports Exercise. 2012;44(7):1325-34. [DOI] [PubMed] [Google Scholar]
- 24.Dallam GM, Wilber RL, Jadelis K, et al. Effect of a global alteration of running technique on kinematics and economy. J Sports Sci. 2005;23(7):757-64. [DOI] [PubMed] [Google Scholar]
- 25.Arendse RE, Noakes TD, Azevedo LB, et al. Reduced eccentric loading of the knee with the pose running method. Med Sci Sports Exerc. 2004;36(2):272-77. [DOI] [PubMed] [Google Scholar]
- 26.Helmhout PH, Diebal AR, van der Kaaden L, et al. The effectiveness of a 6-week intervention program aimed at modifying running style in subjects with chronic exertional compartment syndrome: Results from a series of case studies. Orthop J Sports Med. 2015;3(3): 2325967115575691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmermann WO, Helmhout PH, Harts CC. [The treatment of MTSS and CECS in the Dutch military health care.] NMGT. 2014;67(3):72-82. [In Dutch] [Google Scholar]
- 28.Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77-97. [DOI] [PubMed] [Google Scholar]
- 29.Beurskens AJ, de Vet HC, Köke AJ, et al. A subject-specific approach for measuring functional status in low back pain. J Manipulative Physiol Ther. 1999;22(3):144-8. [DOI] [PubMed] [Google Scholar]
- 30.Wendel-Vos GC, Schuit AJ, Saris WH, et al. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol. 2003;56(12):1163-9. [DOI] [PubMed] [Google Scholar]
- 31.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989 Dec;10(4):407-15. [DOI] [PubMed] [Google Scholar]
- 32.Chumanov ES, Wille CM, Michalski MP, et al. Changes in muscle activation patterns when running step rate is increased. Gait Posture. 2012;36(2):231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heiderscheit BC. Gait retraining for runners: In search of the ideal. J Orthop Sports Phys Ther. 2011;41(12):909-10. [DOI] [PubMed] [Google Scholar]



